An Autonomous Wireless Health Monitoring System Based on Heartbeat and Accelerometer Sensors
Abstract
1. Introduction
- (i)
- A new design of a wearable AWHMS is presented based on a WBSN with high measurement accuracy and a long communication range based on the GSM network.
- (ii)
- The accuracy of patient heart rate measurement was improved, and the normal and abnormal patient heart rate functions were identified based on the abnormal heart rate detection (AHRD) algorithm.
- (iii)
- Patient falls were accurately detected based on a new proposed algorithm that combines an acceleration threshold and activity/inactivity counter (TB-AIC).
- (iv)
- The performance of heart rate measurement and fall detection was confirmed based on statistical analysis.
- (v)
- The results of the current work were compared with those of similar previous studies in terms of accuracy, sensitivity, and specificity to validate the performance of the proposed AWHMS.
2. Related Work
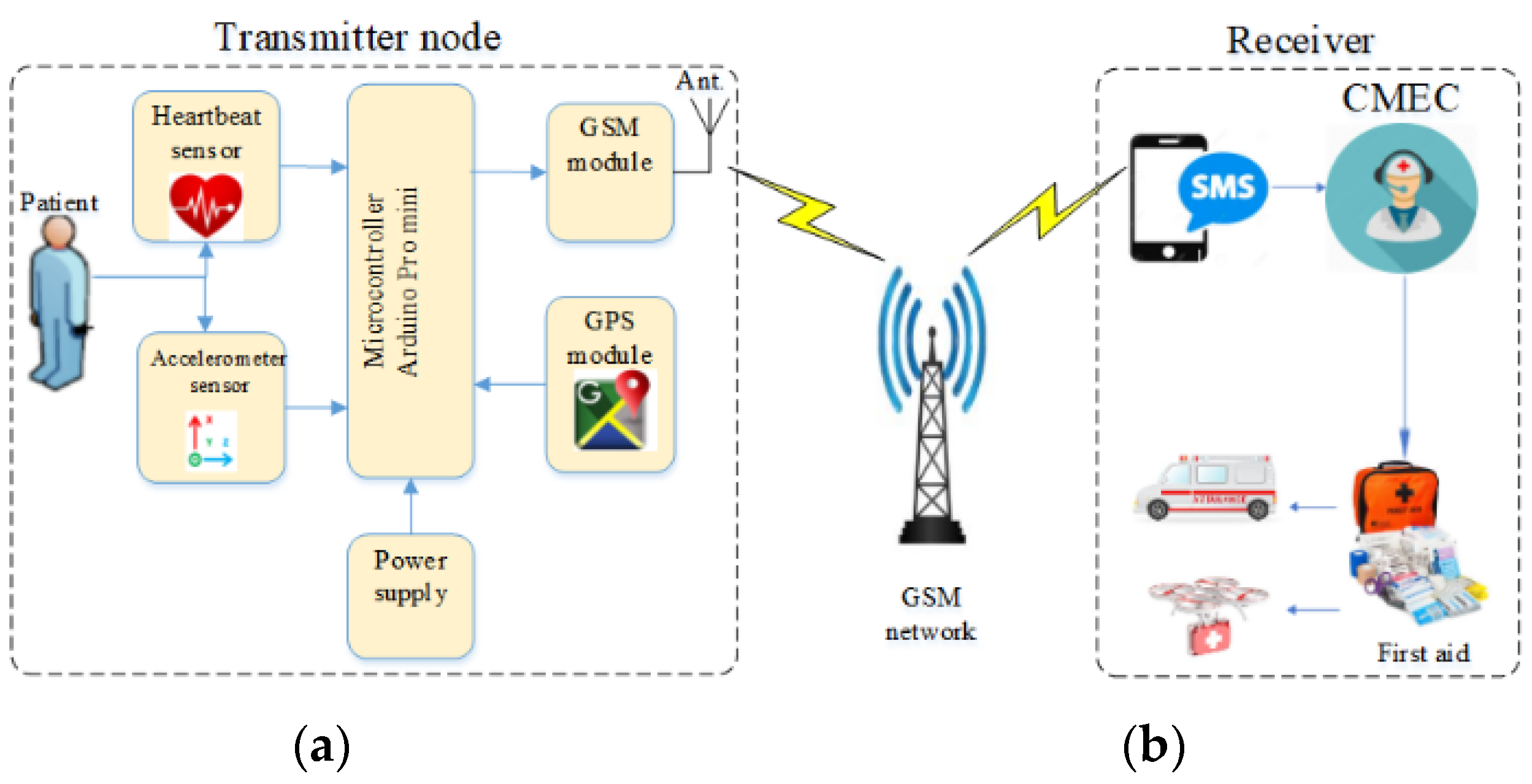
3. System Architecture
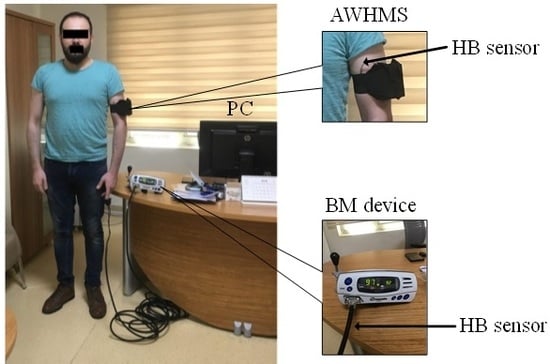
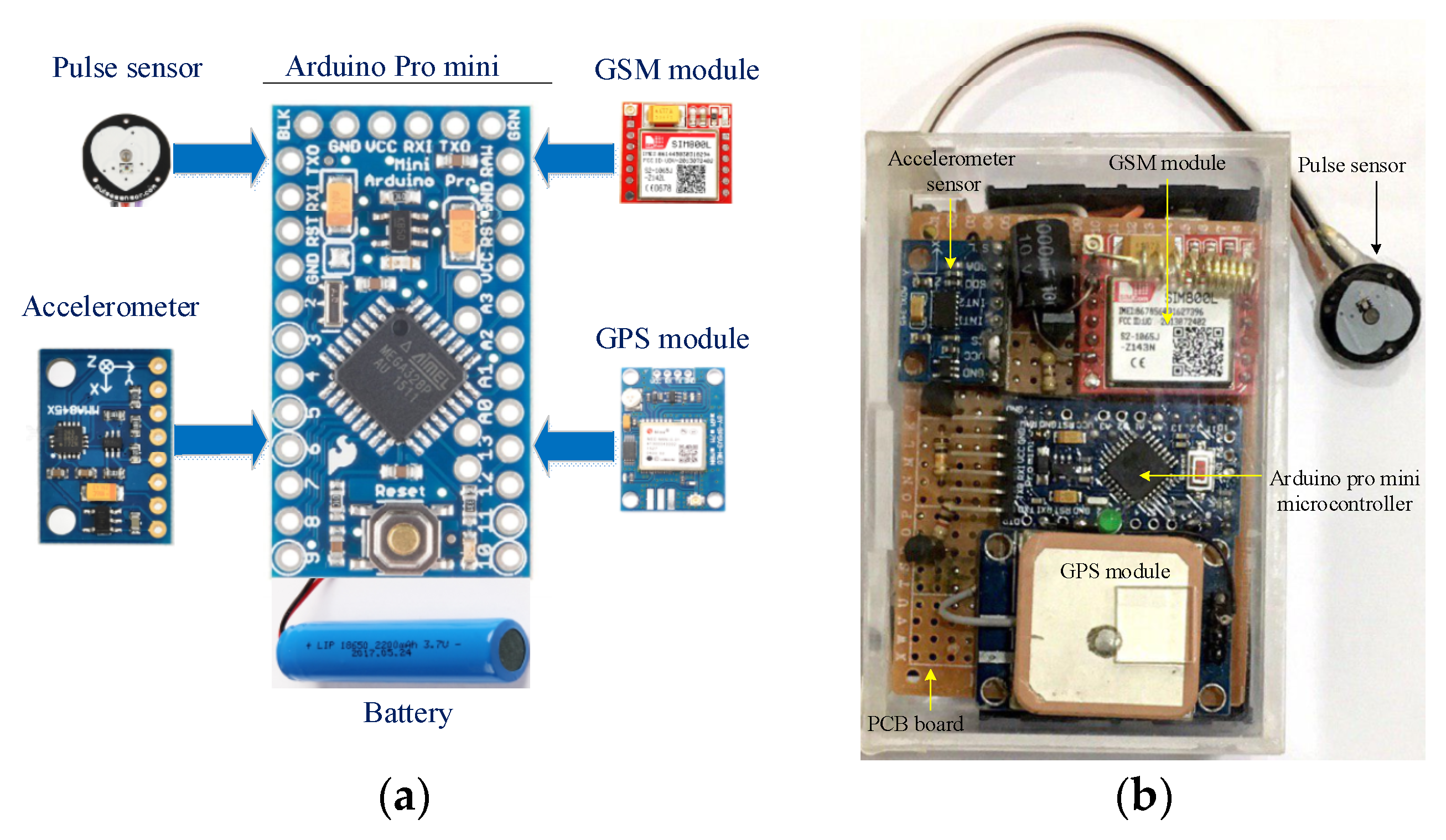
3.1. Hardware of AWHMS
3.1.1. Accelerometer
3.1.2. Heartbeat Sensor
3.1.3. Microcontroller
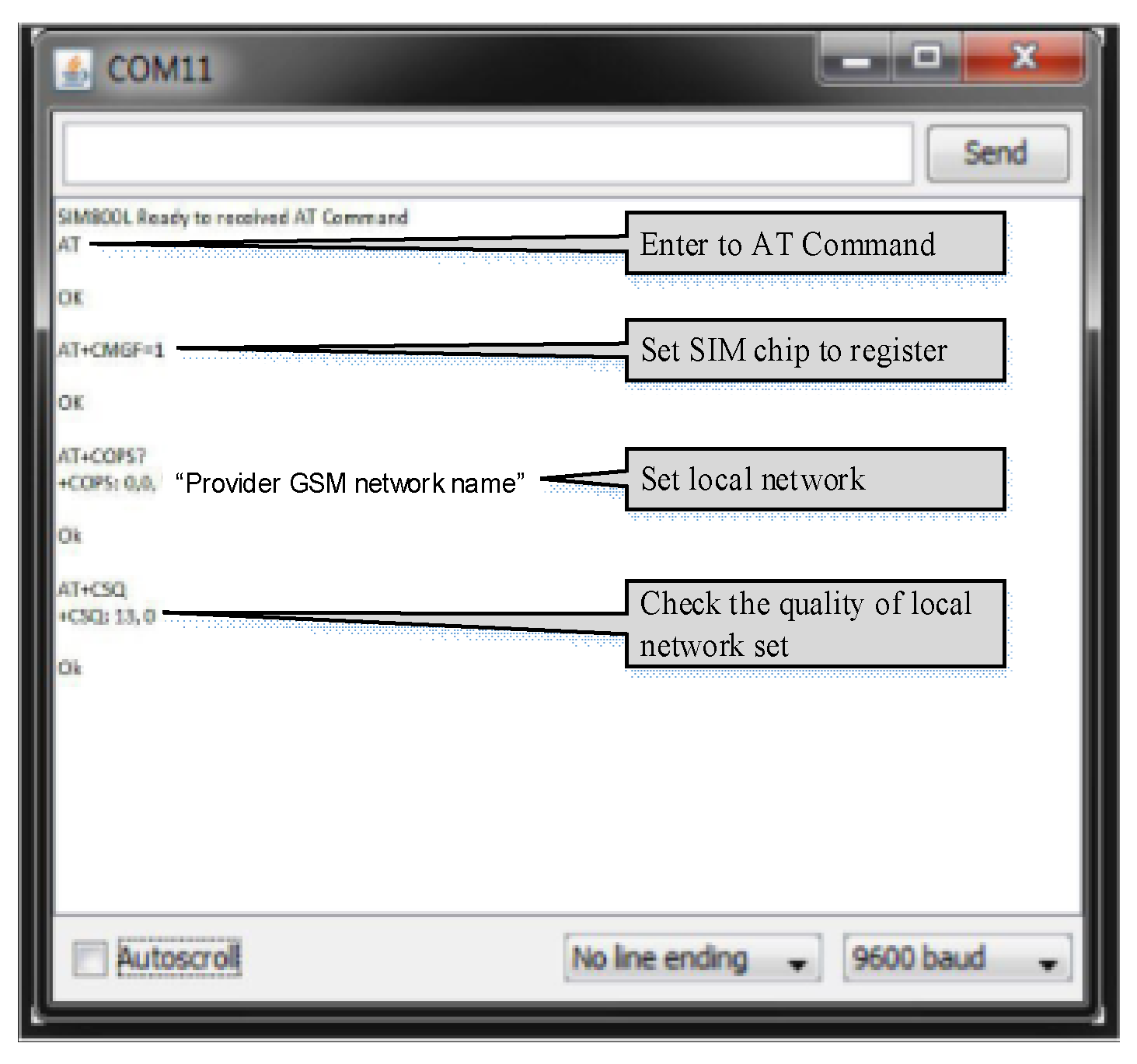
3.1.4. GSM Module and Smartphone
3.1.5. GPS Module
3.2. Proposed Algorithm
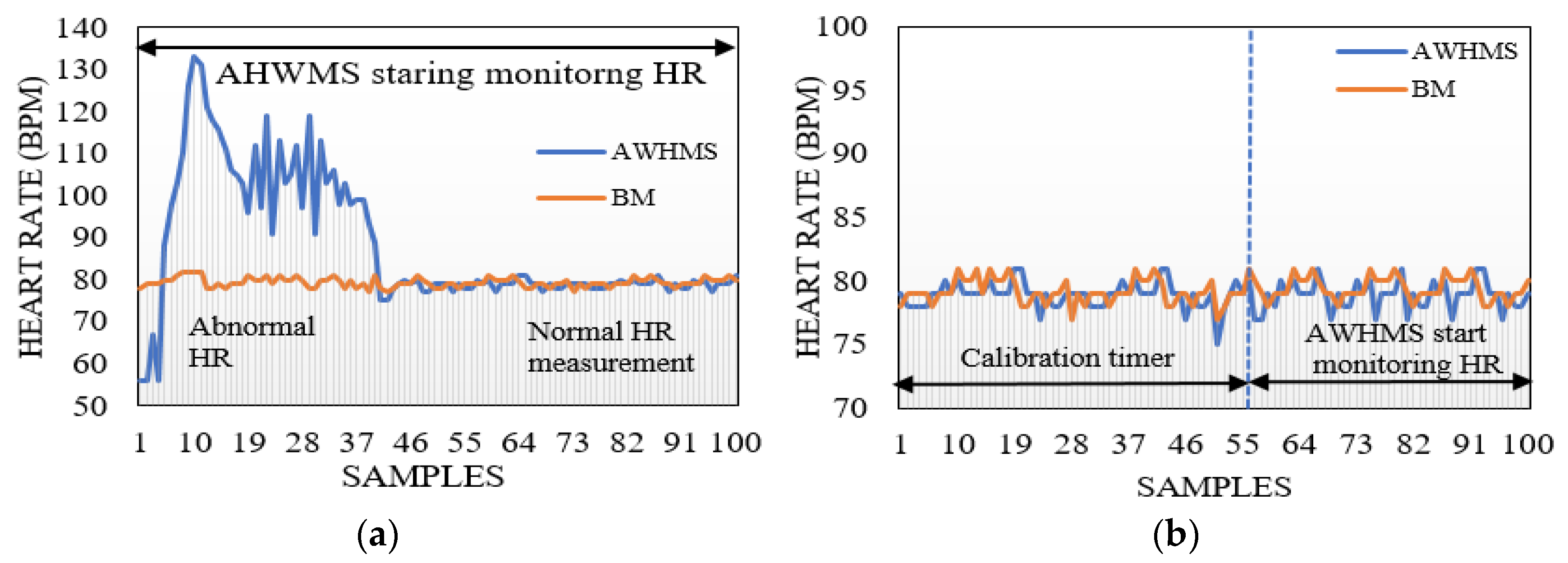
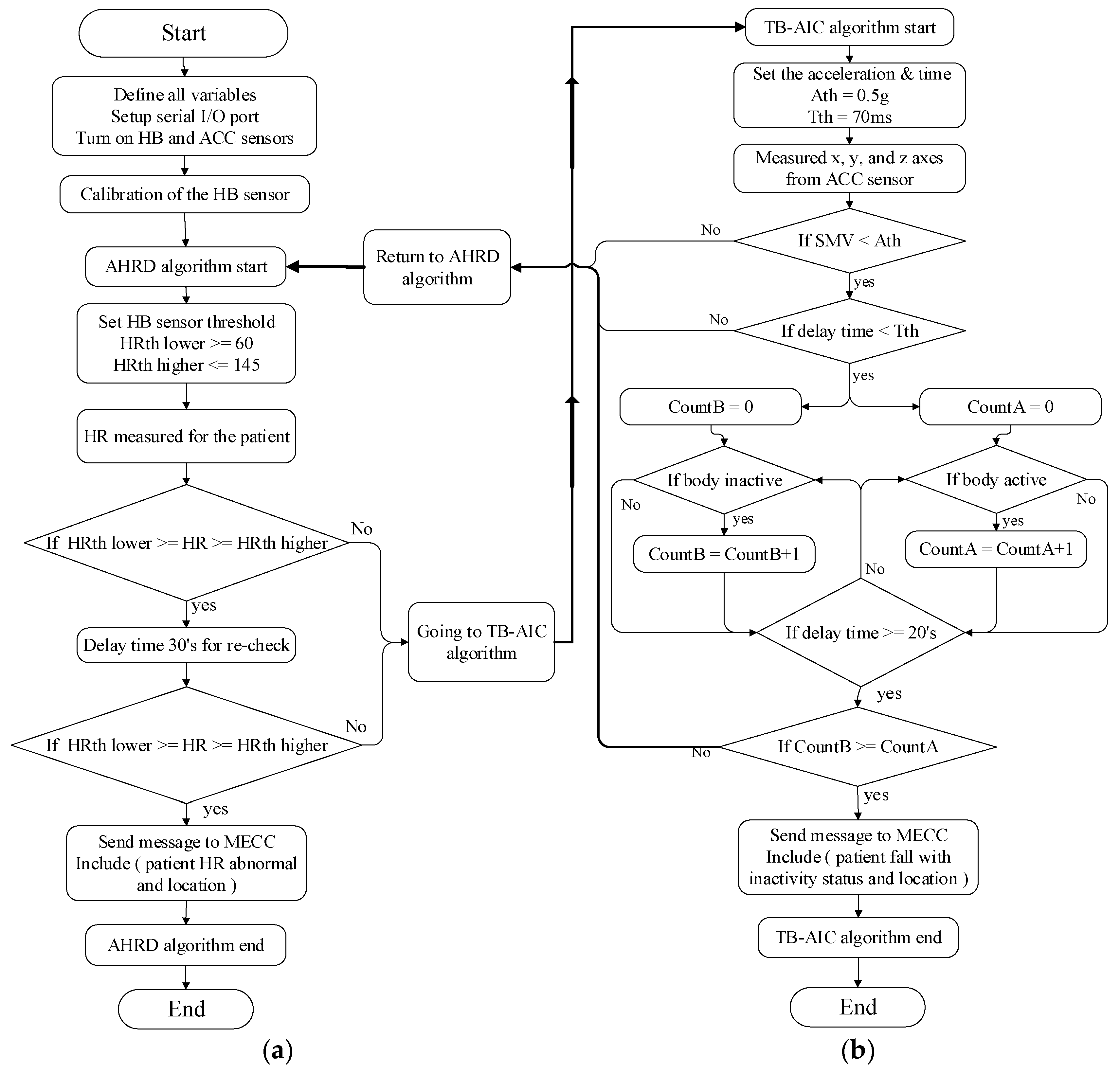
3.2.1. Abnormal HR Detection (AHRD) Algorithm
3.2.2. Fall Detection Algorithm (TB-AIC)
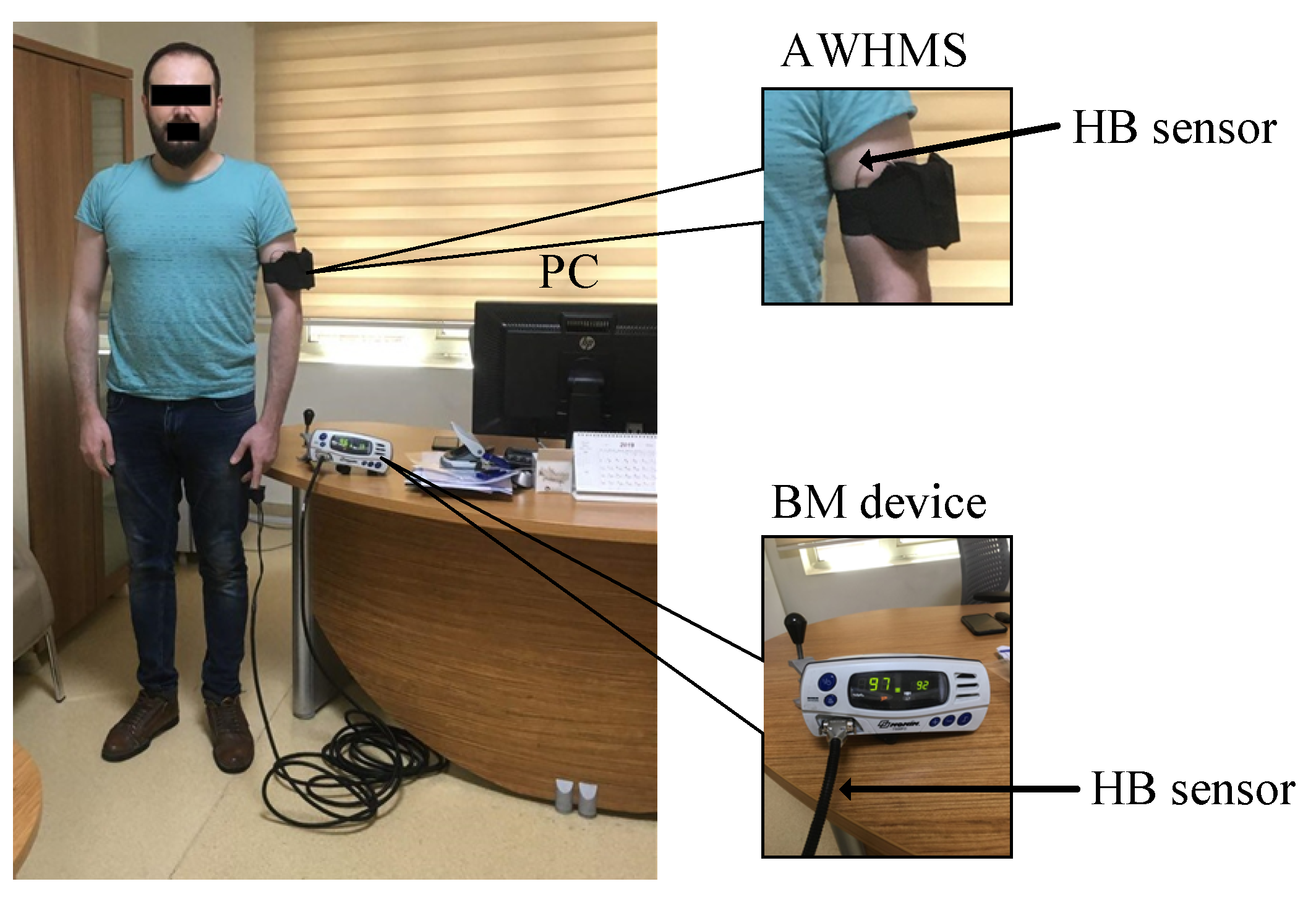
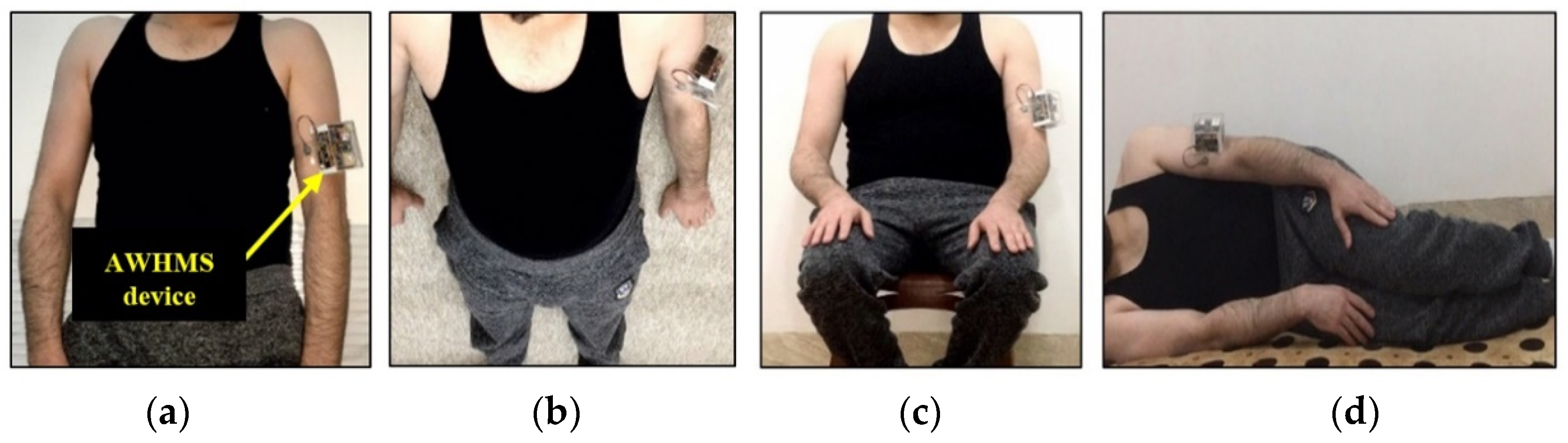
4. Experiment Configuration
4.1. Heartbeat Sensor
4.2. ACC Sensor
5. Parameter Measurements
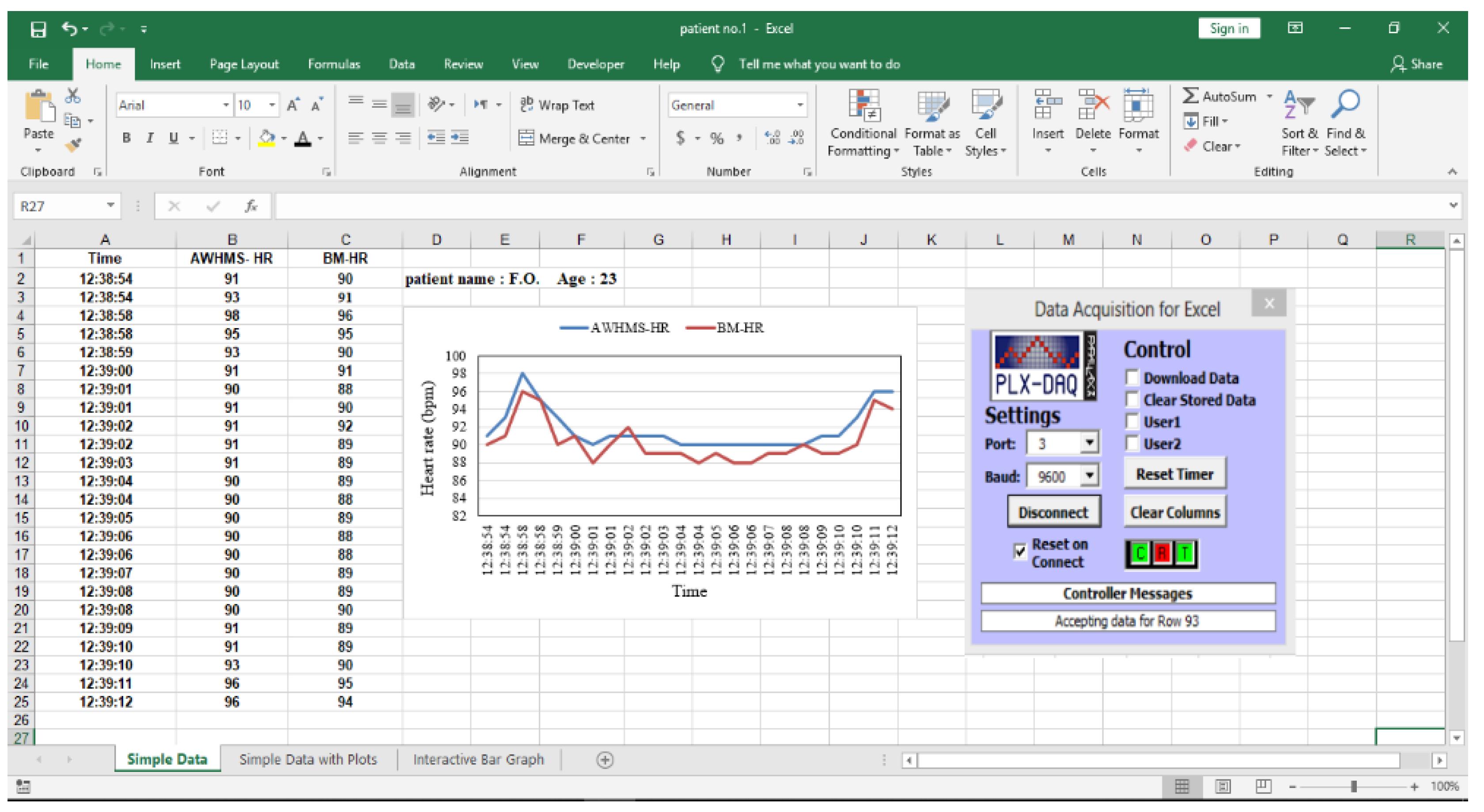
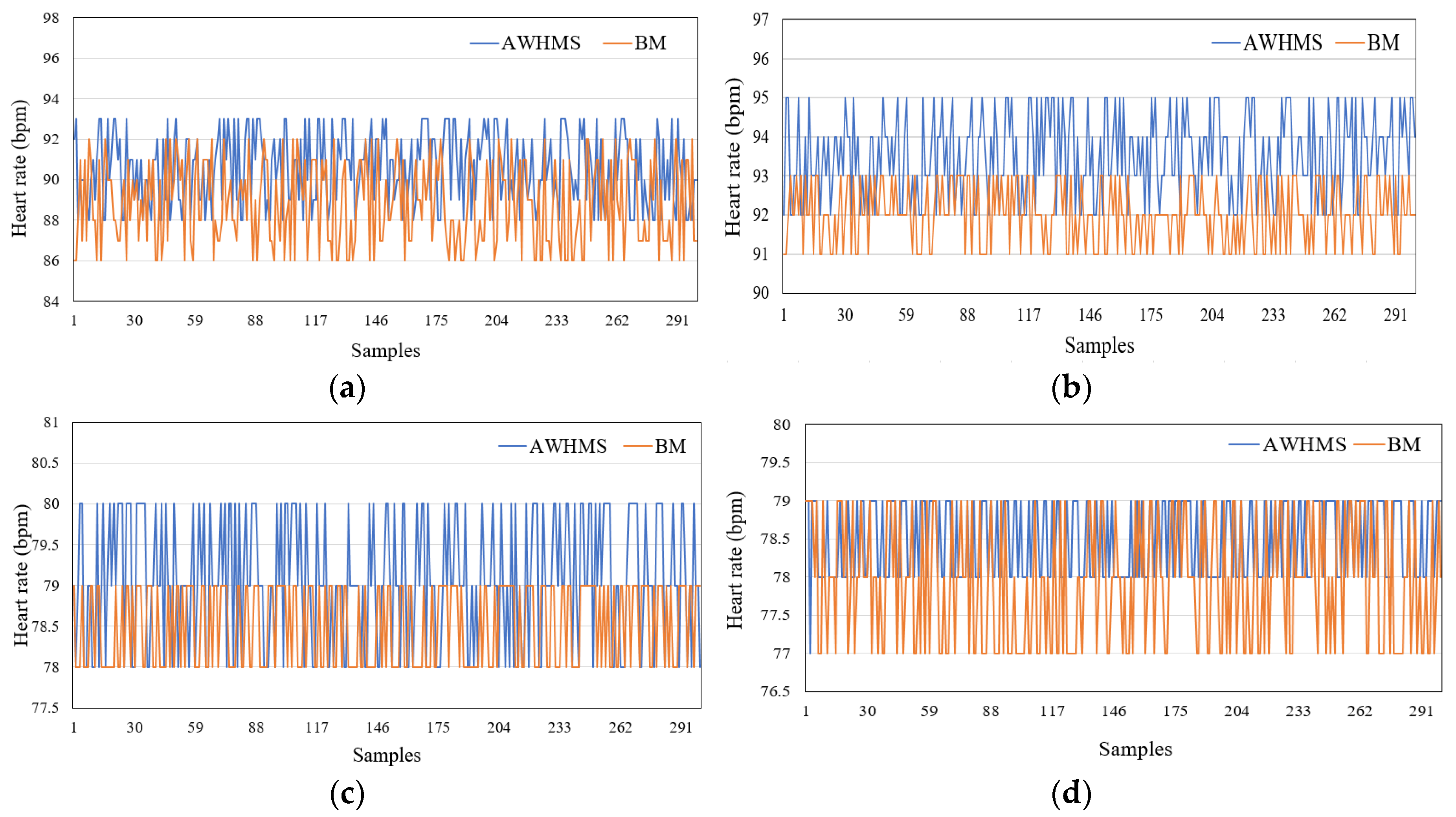
5.1. HR Measurements
5.2. Accelerometer Measurement
6. Results and Discussions
6.1. HR Measurement Validation
6.1.1. Accuracy
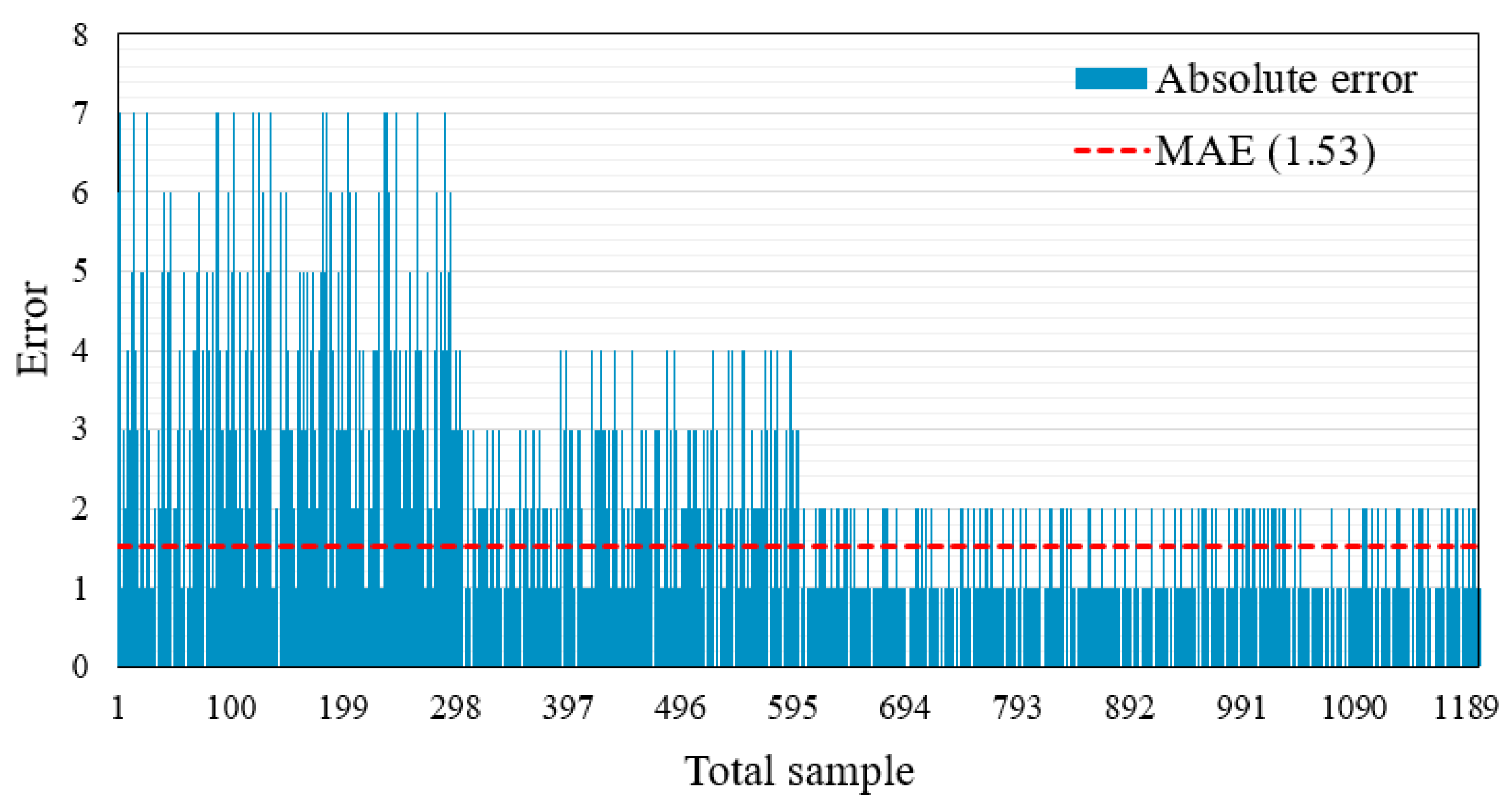
6.1.2. Error Test
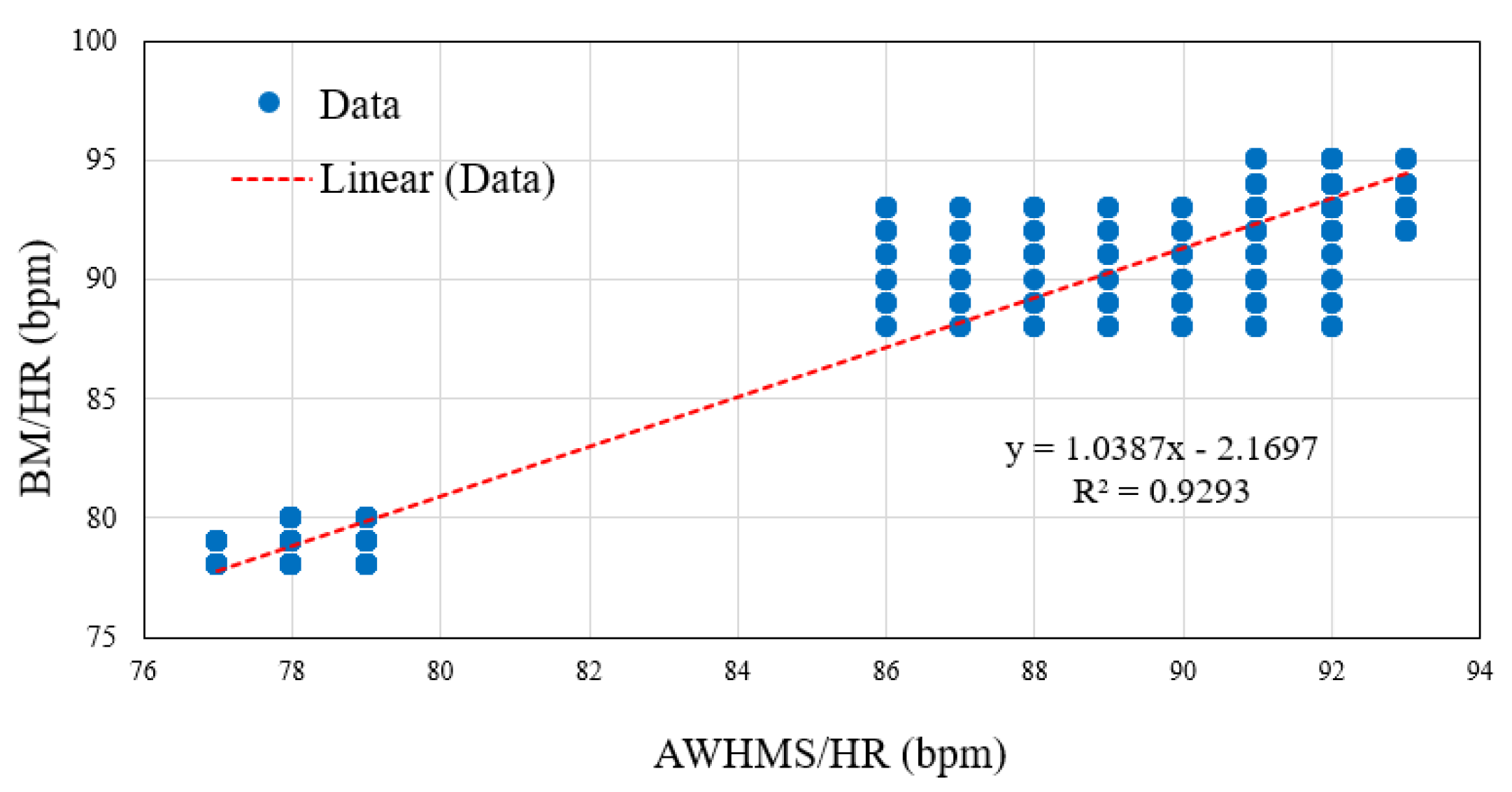
6.1.3. Correlation Coefficient Test
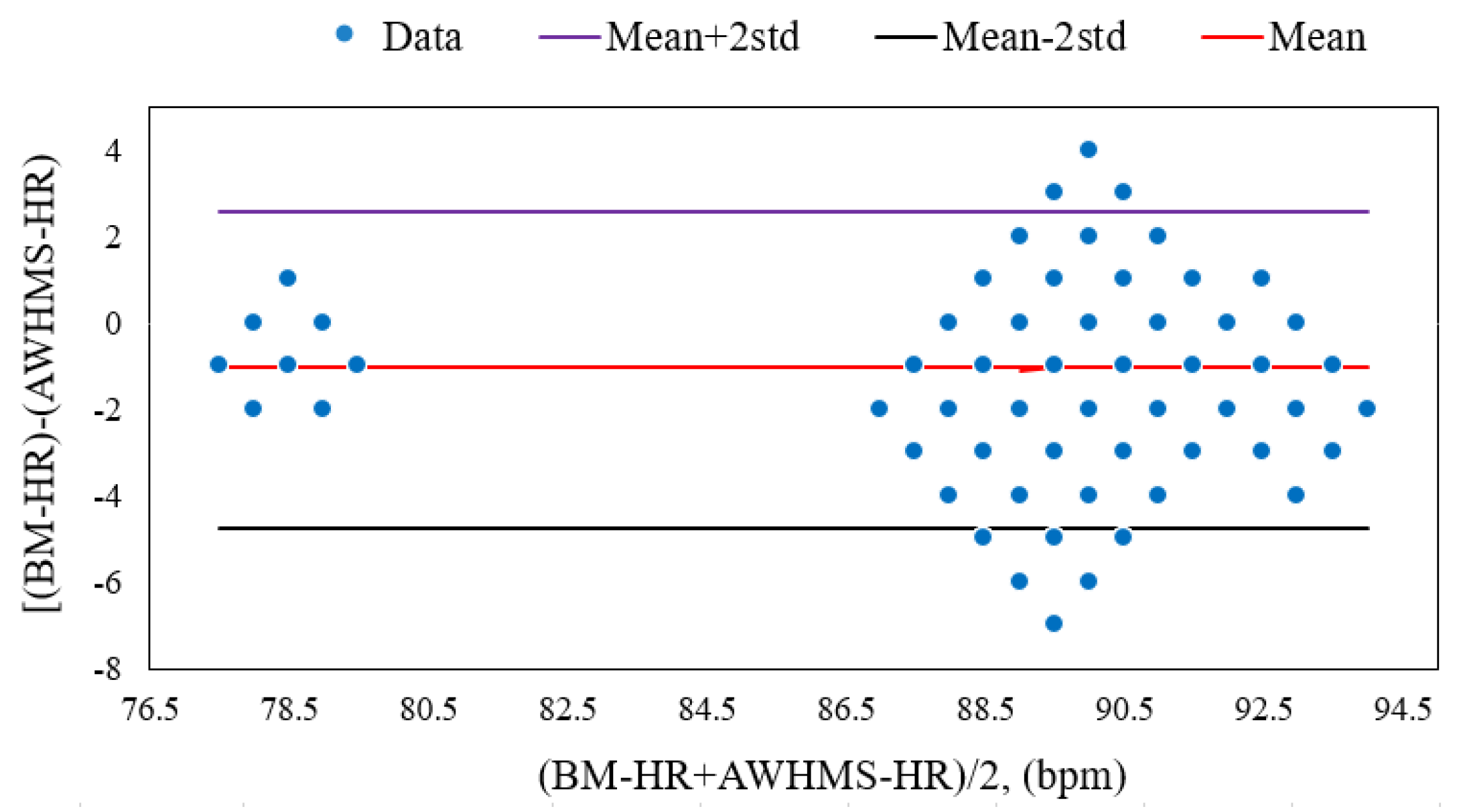
6.1.4. Bland–Altman Plot
6.2. Performance Validation of the Accelerometer Measurements
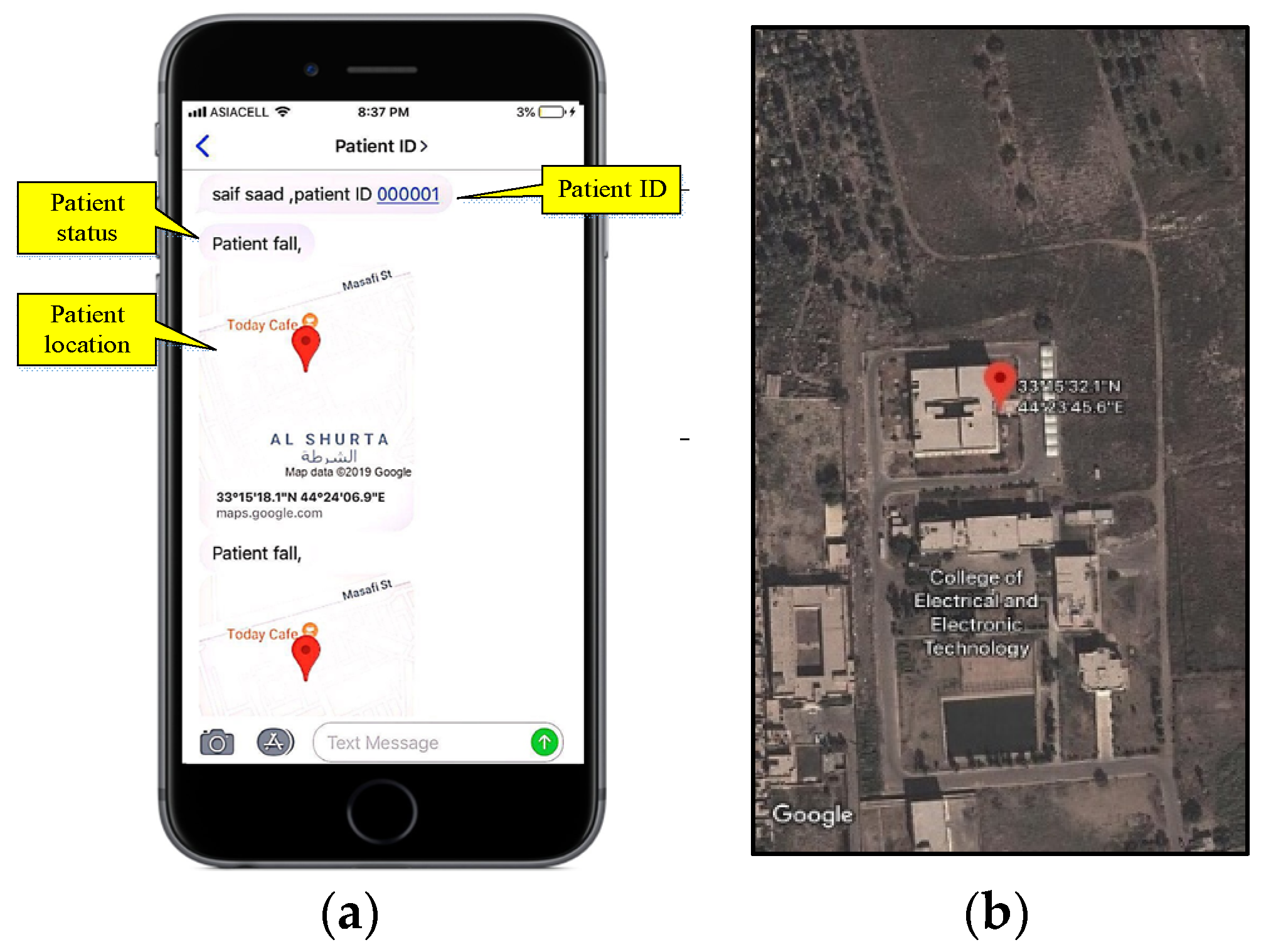
6.3. Test Data Delivery
7. Comparison with Previous Results
8. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| ACC | Accelerometer |
| ADL | Activities of daily living |
| AHRD | Abnormal heart rate detection |
| Ath | Acceleration threshold |
| AWHMS | Autonomous wireless health monitoring system |
| BM | Benchmark |
| CDC | Centers for Disease Control and Prevention |
| CHMM | Coupled hidden Markov module |
| FD | Fall detection |
| FDA | Food and Drug Administration |
| FD-NOLS | Fall detection for non-line of sight |
| FN | False negative |
| FP | False positive |
| GNSS | Global navigation satellite system |
| GPS | Global positioning system |
| GSM | Global system for mobile communications |
| HB | Heartbeat |
| HMM | Hidden Markov module |
| HR | Heart rate |
| HRth | Heart rate threshold |
| HUM | Humidity |
| LED | Light emitting diode |
| MAE | Mean absolute error |
| MAPE | Mean absolute percentage error |
| MECC | Medical emergency call center |
| MSE | Mean square error |
| PC | Personal computer |
| PCB | Printed circuit board |
| PLX-DAQ | Parallax data acquisition software |
| PPG | Photoplethysmography |
| RMSE | Root mean square error |
| SEMG | Surface electromyography |
| SMV | Sum magnitude vectors |
| SpO2 | Oximeter saturation |
| Std | Standard deviation |
| SVM | Support vector machine |
| TB-AIC | threshold based and activity/inactivity counter |
| TBM | Threshold based method |
| TBM-MD | Threshold based method with Madgwick’s decomposition |
| TEMP | Temperature |
| TN | True negative |
| TP | True positive |
| Tth | Time threshold |
| VSMS | Vital signs monitoring system |
| WBSN | Wireless body area sensor network |
References
- Harbouche, A.; Djedi, N.; Erradi, M.; Ben-Othman, J.; Kobbane, A. Model driven flexible design of a wireless body sensor network for health monitoring. Comput. Netw. 2017, 129, 548–571. [Google Scholar] [CrossRef]
- Fajkus, M.; Nedoma, J.; Martinek, R.; Vasinek, V.; Nazeran, H.; Siska, P. A non-invasive multichannel hybrid fiber-optic sensor system for vital sign monitoring. Sensors 2017, 17, 111. [Google Scholar] [CrossRef] [PubMed]
- Amin, R.; Islam, S.H.; Biswas, G.P.; Khan, M.K.; Kumar, N. A robust and anonymous patient monitoring system using wireless medical sensor networks. Futur. Gener. Comput. Syst. 2018, 80, 483–495. [Google Scholar] [CrossRef]
- Fouad, H.; Farouk, H. Heart rate sensor node analysis for designing internet of things telemedicine embedded system. Cogent Eng. 2017, 4, 1–12. [Google Scholar] [CrossRef]
- Mezghani, N.; Ouakrim, Y.; Islam, M.R.; Yared, R.; Abdulrazak, B. Context aware adaptable approach for fall detection bases on smart textile. In Proceedings of the 2017 IEEE EMBS International Conference on Biomedical & Health Informatics (BHI), Orlando, FL, USA, 16–19 February 2017. [Google Scholar]
- Wang, Z.; Zhao, C.; Qiu, S. A system of human vital signs monitoring and activity recognition based on body sensor network. Sens. Rev. 2014, 34, 42–50. [Google Scholar] [CrossRef]
- Kantoch, E.; Augustyniak, P.; Markiewicz, M.; Prusak, D. Monitoring activities of daily living based on wearable wireless body sensor network. In Proceedings of the 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Chicago, IL, USA, 26–30 August 2014. [Google Scholar]
- Kakria, P.; Tripathi, N.K.; Kitipawang, P. A Real-Time Health Monitoring System for Remote Cardiac Patients Using Smartphone and Wearable Sensors. Int. J. Telemed. Appl. 2015, 2015, 373474. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.; Chen, X.; Shen, M. A framework for daily activity monitoring and fall detection based on surface electromyography and accelerometer signals. IEEE J. Biomed. Health. Inform. 2013, 17, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Sikder, F.; Sarkar, D. Log-sum distance measures and its application to human-activity monitoring and recognition using data from motion sensors. IEEE Sens. J. 2017, 17, 4520–4533. [Google Scholar] [CrossRef]
- Gia, T.N.; Tcarenko, I.; Sarker, V.K.; Rahmani, A.M.; Westerlund, T.; Liljeberg, P.; Tenhunen, H. IoT-based fall detection system with energy efficient sensor nodes. In Proceedings of the IEEE Nordic Circuits and Systems (Norcas’16), Copenhagen, Denmark, 1–2 November 2016. [Google Scholar]
- Aguiar, B.; Rocha, T.; Silva, J.; Sousa, I. Accelerometer-based fall detection for smartphones. In Proceedings of the 2014 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Lisboa, Portugal, 11–12 June 2014. [Google Scholar]
- Depari, A.; Flammini, A.; Bellagente, P.; Sisinni, E.; Crema, C.; Vezzoli, A. Virtual Respiratory Rate Sensors: An Example of a Smartphone-Based Integrated and Multiparametric mHealth Gateway. IEEE Trans. Instrum. Meas. 2017, 66, 2456–2463. [Google Scholar]
- Wu, F.; Zhao, H.; Zhao, Y.; Zhong, H. Development of a Wearable-Sensor-Based Fall Detection System. Int. J. Telemed. Appl. 2015, 2015, 576364. [Google Scholar] [CrossRef]
- Wang, J.; Zhang, Z.; Li, B.; Lee, S.; Sherratt, R. An enhanced fall detection system for elderly person monitoring using consumer home networks. IEEE Trans. Consum. Electron. 2014, 60, 23–29. [Google Scholar] [CrossRef]
- Delahoz, Y.S.; Labrador, M.A. Survey on fall detection and fall prevention using wearable and external sensors. Sensors 2014, 14, 19806–19842. [Google Scholar] [CrossRef] [PubMed]
- Panicker, N.V.; Kumar, A.S. Design of a telemonitoring system for detecting falls of the elderly. In Proceedings of the 2015 International Conference on Green Computing and Internet of Things (ICGCIoT), Noida, India, 14 January 2016. [Google Scholar]
- Aziz, K.; Tarapiah, S.; Ismail, S.H.; Atalla, S. Smart real-time healthcare monitoring and tracking system using GSM/GPS technologies. In Proceedings of the 2016 3rd MEC International Conference on Big Data and Smart City, Muscat, Oman, 15–16 March 2016. [Google Scholar]
- Siregar, B.; Andayani, U.; Bahri, R.P.; Fahmi, F. Real-time monitoring system for elderly people in detecting falling movement using accelerometer and gyroscope. J. Phys. Conf. Ser. 2018, 978, 012110. [Google Scholar] [CrossRef]
- Hsieh, S.L.; Chen, C.C.; Wu, S.H.; Yue, T.W. A wrist-worn fall detection system using accelerometers and gyroscopes. In Proceedings of the 11th IEEE International Conference on Networking, Sensing and Control, Miami, FL, USA, 7–9 April 2014. [Google Scholar]
- Nosrati, M.; Tavassolian, N. High-Accuracy Heart Rate Variability Monitoring Using Doppler Radar Based on Gaussian Pulse Train Modeling and FTPR Algorithm. IEEE Trans. Microw. Theory Tech. 2018, 66, 556–567. [Google Scholar] [CrossRef]
- Gharghan, S.K.; Mohammed, S.L.; Al-Naji, A.; Abu-AlShaeer, M.J.; Jawad, H.M.; Jawad, A.M.; Chahl, J. Accurate fall detection and localization for elderly people based on neural network and energy-efficient wireless sensor network. Energies 2018, 11, 2866. [Google Scholar] [CrossRef]
- Lithium Polymer Battery Safety Data Sheet. Available online: https://system.na3.netsuite.com (accessed on 5 March 2019).
- Pittet, V.; Burnand, B.; Yersin, B.; Carron, P.N. Trends of pre-hospital emergency medical services activity over 10 years: A population-based registry analysis. BMC Health Serv. Res. 2014, 14, 380. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Liu, Y.; Jiang, M. Review on emergency medical response against terrorist attack. Mil. Med. Res. 2014, 1, 9. [Google Scholar] [CrossRef] [PubMed]
- Pernini, L.; Palma, L.; Pierleoni, P.; Valenti, S.; Pellegrini, M.; Belli, A. A High Reliability Wearable Device for Elderly Fall Detection. IEEE Sens. J. 2015, 15, 4544–4553. [Google Scholar]
- Rihana, S.; Mondalak, J. Wearable fall detection system. In Proceedings of the 2016 3rd Middle East Conference on Biomedical Engineering, Beirut, Lebanon, 6–7 October 2016. [Google Scholar]
- Ning, J. Detecting Human Falls with a 3-Axis Digital Accelerometer. Analog. Dialogue 2009, 43, 3. [Google Scholar]
- Malmivuo, P.; Malmivuo, J.; Plonsey, R. Bioelectromagnetism: Principles and Applications of Bioelectric and Biomagnetic Fields; Oxford University Press: New York, NY, USA, 1995; pp. 588–595. Available online: http://www.bem.fi/book/book.pdf (accessed on 4 March 2019).
- Butca, C.G.; Suciu, G.; Ochian, A.; Fratu, O.; Halunga, S. Wearable sensors and cloud platform for monitoring environmental parameters in e-health applications. In Proceedings of the 2014 11th International Symposium on Electronics and Telecommunications, Timisoara, Romania, 14–15 November 2014. [Google Scholar]
- Arduino. Available online: https://cdn.sparkfun.com/datasheets/Dev/Arduino/Boards/ProMini16MHzv1.pdf (accessed on 4 March 2019).
- Ali, A.S.; Zanzinger, Z.; Debose, D.; Stephens, B. Open Source Building Science Sensors (OSBSS): A low-cost Arduino-based platform for long-term indoor environmental data collection. Build. Environ. 2016, 100, 114–126. [Google Scholar] [CrossRef]
- Sim800l. Available online: https://img.filipeflop.com/files/download/Datasheet_SIM800L.pdf (accessed on 4 March 2019).
- Leu, F.; Ko, C.; You, I.; Choo, K.K.R.; Ho, C.L. A smartphone-based wearable sensors for monitoring real-time physiological data. Comput. Electr. Eng. 2018, 65, 376–392. [Google Scholar] [CrossRef]
- U-blox NEO-M8: U-blox Concurrent GNSS Modules—Data Sheet. Available online: https://www.u-blox.com/sites/default/files/NEO-M8-FW3_DataSheet_%28UBX-15031086%29.pdf (accessed on 8 March 2019).
- Grigulo, J.; Becker, L.B. Experimenting Sensor Nodes Localization in WSN with UAV Acting as Mobile Agent. In Proceedings of the 2018 IEEE 23rd International Conference on Emerging Technologies and Factory Automation, Turin, Italy, 4–7 September 2018. [Google Scholar]
- Skoglund, M.; Petig, T.; Vedder, B.; Eriksson, H.; Schiller, E.M. Static and dynamic performance evaluation of low-cost RTK GPS receivers. In Proceedings of the 2016 IEEE Intelligent Vehicles Symposium, Gothenburg, Sweden, 19–22 June 2016. [Google Scholar]
- Ostchega, Y.; Porter, K.S.; Hughes, J.; Dillon, C.F.; Nwankwo, T. Resting pulse rate reference data for children, adolescents, and adults: United States, 1999–2008. Natl. Health Stat. Rep. 2011, 41, 1–16. [Google Scholar]
- Pirbhulal, S.; Zhang, H.; Wu, W.; Mukhopadhyay, S.C.; Zhang, Y.T. Heartbeats Based Biometric Random Binary Sequences Generation to Secure Wireless Body Sensor Networks. IEEE Trans. Biomed. Eng. 2018, 65, 2751–2759. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.; Seo, J.O.; Jebelli, H.; Lee, S.H. Feasibility analysis of heart rate monitoring of construction workers using a photoplethysmography (PPG) sensor embedded in a wristband-type activity tracker. Autom. Constr. 2016, 71, 372–381. [Google Scholar] [CrossRef]
- Physical Activity Basics, Physical Activity, CDC. Available online: https://www.cdc.gov/physicalactivity/basics/index.htm (accessed on 7 June 2019).
- Ventricular Fibrillation: Treatment, Causes, and Symptoms. Available online: https://www.medicalnewstoday.com (accessed on 6 July 2019).
- Abnormal Heart Rhythms: Causes, Symptoms and Diagnosis. Available online: https://www.healthline.com (accessed on 4 July 2019).
- Model 7500 | Nonin. Available online: https://www.nonin.com/support/7500/ (accessed on 4 March 2019).
- Model 7500 Series. Available online: https://www.nonin.com/wp-content/uploads/2018/09/Spec-Sheet-Model-7500.pdf (accessed on 4 March 2019).
- PAR Hospital Erbil. Available online: http://parhospital.org/ (accessed on 7 March 2019).
- El Ghzizal, A.; Motahhir, S.; Derouich, A.; El Hammoumi, A.; Chalh, A. Low-cost virtual instrumentation of PV panel characteristics using Excel and Arduino in comparison with traditional instrumentation. Renew. Wind Water Sol. 2018, 5, 3. [Google Scholar]
- Smaldone, C.J.; Chabot, E.; Sun, Y. Impact of Placement of Facial PPG Sensor on Pulse-Rate Monitoring Accuracy. In Proceedings of the 43rd Annual Northeast Bioengineering Conference, Newark, NJ, USA, 2 March 2017. [Google Scholar]
- Saha, A.; Das, S.; Suresh, M.; Raj Kiran, V.; Dey, N. FPGA based self-vibration compensated two dimensional non-contact vibration measurement using 2D position sensitive detector with remote monitoring. Meas. J. Int. Meas. Confed. 2017, 111, 271–278. [Google Scholar] [CrossRef]
- Yuan, X.; Li, J.N.; Fang, Z. Hardware Design of Fall Detection System Based on ADXL345 Sensor. In Proceedings of the 2015 8th International Conference on Intelligent Computation Technology and Automation, Nanchang, China, 14–15 June 2015. [Google Scholar]
- Fakhri, A.B.; Gharghan, S.K.; Mohammed, S.L. Statistical validation of patient vital signs based on energy-efficient wireless sensor network monitoring system. ARPN J. Eng. App. Sci. 2018, 13, 8258–8270. [Google Scholar]
- Lu, G.; Yang, F. Limitations of oximetry to measure heart rate variability measures. Cardiovasc. Eng. 2009, 9, 119–125. [Google Scholar] [CrossRef]
- Lu, G.; Yang, F.; Taylor, J.A.; Stein, J.F. A comparison of photoplethysmography and ECG recording to analyse heart rate variability in healthy subjects. J. Med. Eng. Technol. 2009, 33, 634–641. [Google Scholar] [CrossRef]
- Schäfer, A.; Vagedes, J. How accurate is pulse rate variability as an estimate of heart rate variability? A review on studies comparing photoplethysmographic technology with an electrocardiogram. Int. J. Cardiol. 2013, 166, 15–29. [Google Scholar] [CrossRef]
- Zhang, H.; Safaei, F.; Tran, L.C. A Novel Cooperation-Based Network Coding Scheme for Walking Scenarios in WBANs. Wirel. Commun. Mob. Comput. 2017, 2017, 6267579. [Google Scholar] [CrossRef]
- Theodorsson, E.; Dahlqvist, S.; Attvall, S.; Sandgren, U.; Skrtic, S.; Lind, M.; Pivodic, A.; Ólafsdóttir, A.F. A Clinical Trial of the Accuracy and Treatment Experience of the Flash Glucose Monitor FreeStyle Libre in Adults with Type 1 Diabetes. Diabetes Technol. Ther. 2017, 19, 164–172. [Google Scholar]
- Social Research Methods Knowledge Base—Correlation. Available online: https://socialresearchmethods.net/kb/statcorr.php (accessed on 30 March 2019).
- Valipour, A.; Abbasi-kesbi, R. A Heartbeat and Respiration Rate Sensor Based on a Phonocardiogram for Healthcare Applications. In Proceedings of the 2017 Iranian Conference on Electrical Engineering, Tehran, Iran, 2–4 May 2017. [Google Scholar]
- Neumayer, C.; Klinger, M.; Huk, I.; Nanobachvili, J.; Polanczyk, A. Artificial Circulatory Model for Analysis of Human and Artificial Vessels. Appl. Sci. 2018, 8, 1017. [Google Scholar]
- Zhang, Z.; Pi, Z.; Liu, B. TROIKA: A general framework for heart rate monitoring using wrist-type photoplethysmographic signals during intensive physical exercise. IEEE Trans. Biomed. Eng. 2015, 62, 522–531. [Google Scholar] [CrossRef]
- Baba, E.; Jilbab, A.; Hammouch, A. A health remote monitoring application based on wireless body area networks. In Proceedings of the 2018 International Conference on Intelligent Systems and Computer Vision, Fez, Morocco, 2–4 April 2018. [Google Scholar]
- Wang, C.; Lu, W.; Redmond, S.J.; Stevens, M.C.; Lord, S.R.; Lovell, N.H. A Low-Power Fall Detector Balancing Sensitivity and False Alarm Rate. IEEE J. Biomed. Health. Inform. 2018, 22, 1929–1937. [Google Scholar] [CrossRef] [PubMed]
- Lim, D.; Park, C.; Kim, N.H.; Kim, S.H.; Yu, Y.S. Fall-Detection Algorithm Using 3-Axis Acceleration: Combination with Simple Threshold and Hidden Markov Model. J. Appl. Math. 2014, 2014, 896030. [Google Scholar] [CrossRef]
- De Quadros, T.; Lazzaretti, A.E.; Schneider, F.K. A Movement Decomposition and Machine Learning-Based Fall Detection System Using Wrist Wearable Device. IEEE Sens. J. 2018, 18, 5082–5089. [Google Scholar] [CrossRef]
| Experiment | Stage 1 (ADL) | Stage 2 (Fall) |
|---|---|---|
| 1 | walking | forward fall, landing on knees |
| 2 | jumping | right fall, lying on the ground |
| 3 | running | forward fall, lying on the ground |
| 4 | lying on the bed | seated in bed, falling to the ground |
| 5 | descending stairs | forward fall, lying on the leg |
| 6 | running down the stairs | forward fall, lying on the hand |
| 7 | rapidly sitting down on a chair | backward fall from a seated position on a chair |
| Experiment | ADL (TN) | ADL (FP) | Fall (TP) | Fall (FN) |
|---|---|---|---|---|
| 1 | 16 | 0 | 16 | 0 |
| 2 | 16 | 0 | 16 | 0 |
| 3 | 16 | 0 | 16 | 0 |
| 4 | 16 | 0 | 15 | 1 |
| 5 | 16 | 0 | 16 | 0 |
| 6 | 15 | 1 | 16 | 0 |
| 7 | 16 | 0 | 16 | 0 |
| Total | 111 | 1 | 111 | 1 |
| Error | Group 1 (23–26 Years) | Group 2 (26–29) Years | Group 3 (61–63) Years | Group 4 (64–66) Years | Mean |
|---|---|---|---|---|---|
| MAE | 2.81 | 1.63 | 0.83 | 0.86 | 1.53 |
| MSE | 3.174 | 3.97 | 1.15 | 1.26 | 2.38 |
| RMSE | 1.781 | 1.99 | 1.08 | 1.12 | 1.49 |
| MAPE | 3.08 | 1.73 | 1.04 | 1.09 | 1.74 |
| Std | 2.105 | 1.197 | 0.713 | 0.735 | 1.188 |
| City | No. of Messages Sent | No. of Messages Received | Message Loss |
|---|---|---|---|
| Baghdad | 10 | 10 | 0 |
| Mosul | 10 | 10 | 0 |
| Erbil | 40 | 40 | 0 |
| Ref./Year | Fall Detection Algorithm | Wireless Technology | Sensor Type | Sensor Location | Accuracy (%) | Sensitivity (%) FD | Specificity (%) FD | |
|---|---|---|---|---|---|---|---|---|
| FD | Measurement | |||||||
| [9]/2013 | Entropy, HMM | Bluetooth | SEMG, ACC | Leg | >95 (Entropy) and >95 (HMM) | N/A | 95.33 | 97.66 |
| [6]/2014 | CHMM | Zigbee | ACC, Spo2, HB | Wrist, Chest Ankles | 94.8 (CHMM) | 88.75 (ECG) 93.75 (Spo2) | N/A | N/A |
| [7]/2014 | Threshold-based | Bluetooth | ACC, HB, Temp., Hum. | Chest | 97 (ACC) | 99.5(Temp.), 89.9 (Hum.), 95 (HR) | N/A | N/A |
| [12]/2014 | State machine | Smartphone | ACC | Pocket Belt | 97.5 (FD-Pocket), 97.6 (FD-Belt) | N/A | 96.6 (FD-Pocket) 97 (FDBelt) | 98.6 (FD-Pocket) 98.4 (FD-Belt) |
| [15]/2014 | Threshold-based | Zigbee | ACC, HB | N/A | 97.5 (classification) | N/A | 96.8 | 98.1 |
| [20]/2014 | Threshold-based | Zigbee | ACC Gyroscopes | Wrist | N/A | N/A | 95 | 96.7 |
| [8]/2015 | N/A | Bluetooth | HB, Temp. Blood pressure | Chest | N/A | >90 (all vital measurements) | N/A | N/A |
| [14]/2015 | Threshold-based | GSM | ACC | Belt | N/A | N/A | 97.1 | 98.3 |
| [63]/2015 | Threshold-based + HMM | Zigbee | ACC | N/A | 96.25 (FD) | N/A | 98.75 | 94.38 |
| [5]/2017 | Non-linear SVM | Bluetooth | Smart textiles | Belt | 98 (FD) | N/A | 97.5 | 98.5 |
| [10]/2017 | Log- Sum distance | Bluetooth | ACC | Ankles | 99 (Log-Sum distance) | N/A | N/A | N/A |
| [13]/2017 | N/A | Bluetooth | Heartbeat | Chest | N/A | 92.79(HR) | N/A | N/A |
| [21]/2018 | N/A | N/A | Heart rate | Chest | N/A | >90 (HR) | N/A | N/A |
| [22]/2018 | ANN | Zigbee | ACC, Tilt HB | Waist | 92.5 (FD-NLOS environment) | N/A | N/A | |
| [51]/2018 | N/A | Zigbee | HB, Spo2, Temp. | Wrist | N/A | 98.5 (HR), 98.6 (Spo2), 99.9 (Temp.) | N/A | N/A |
| [61]/2018 | N/A | nRF24L01+ | HB, Spo2 ECG, Breathing | N/A | N/A | Good (ECG and breathing), Excellent (SPO2 and HR) | N/A | N/A |
| [62]/2018 | Threshold-based | Zigbee | ACC Barometer | Neck | N/A | N/A | 91 | N/A |
| [64]/2018 | TBM, TBM-MD | N/A | ACC Gyroscopes Magnetometer | Wrist | 91.1 (TBM) 99 (TBM-MD) | N/A | 95.8 (TBM) 100 (TBM-MD) | 86.5 (TBM) 97.9 (TBM-MD) |
| Current work | TB-AIC | GSM | ACC, HB | Upper Arm | 99.11 (TB-AIC) | 98.75 (HR) | 99.12 (TB-AIC) | 99.12 (TB-AIC) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fakhrulddin, S.S.; Gharghan, S.K. An Autonomous Wireless Health Monitoring System Based on Heartbeat and Accelerometer Sensors. J. Sens. Actuator Netw. 2019, 8, 39. https://doi.org/10.3390/jsan8030039
Fakhrulddin SS, Gharghan SK. An Autonomous Wireless Health Monitoring System Based on Heartbeat and Accelerometer Sensors. Journal of Sensor and Actuator Networks. 2019; 8(3):39. https://doi.org/10.3390/jsan8030039
Chicago/Turabian StyleFakhrulddin, Saif Saad, and Sadik Kamel Gharghan. 2019. "An Autonomous Wireless Health Monitoring System Based on Heartbeat and Accelerometer Sensors" Journal of Sensor and Actuator Networks 8, no. 3: 39. https://doi.org/10.3390/jsan8030039
APA StyleFakhrulddin, S. S., & Gharghan, S. K. (2019). An Autonomous Wireless Health Monitoring System Based on Heartbeat and Accelerometer Sensors. Journal of Sensor and Actuator Networks, 8(3), 39. https://doi.org/10.3390/jsan8030039