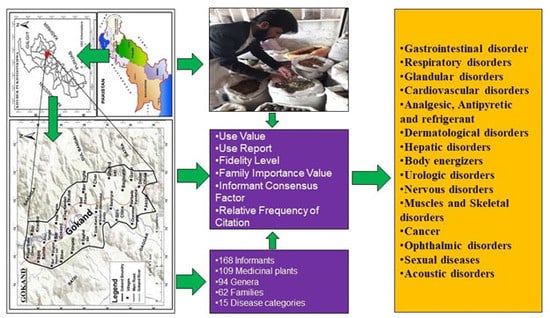
Quantitative Ethnobotanical Study of Indigenous Knowledge on Medicinal Plants Used by the Tribal Communities of Gokand Valley, District Buner, Khyber Pakhtunkhwa, Pakistan
Abstract
1. Introduction
2. Materials and Methods
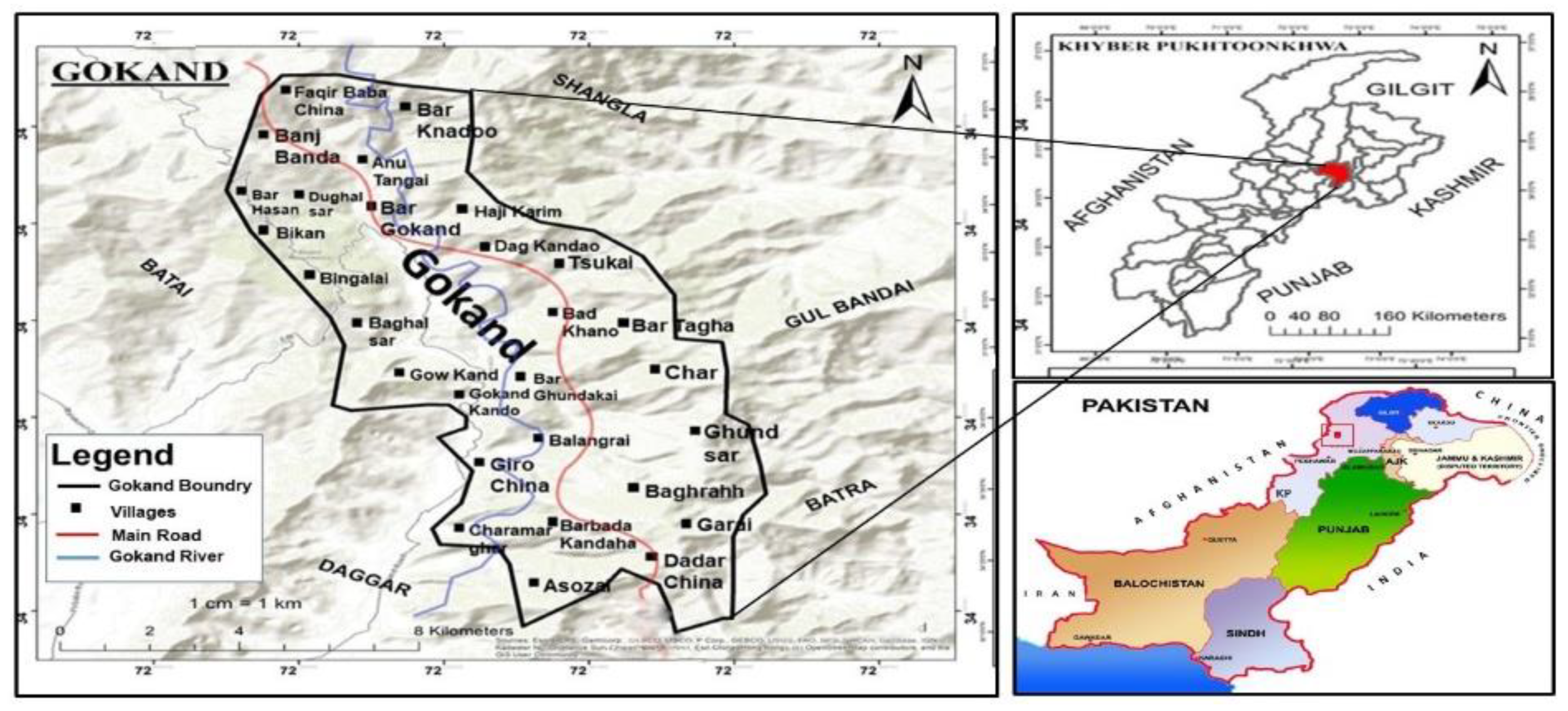
2.1. Study Area and Climate
2.2. Data Collection
2.3. Demographic Data of Local Participants
2.4. Plant Collection and Identification
2.5. Statistical Data Analysis
2.5.1. Use Value
2.5.2. Relative Frequency of Citation and Use Reports
2.5.3. Fidelity Level
2.5.4. Informant Consensus Factor
2.5.5. Family Importance Value
2.6. Conservation Status
3. Results
3.1. Medicinal Plant Taxonomy and Growth Forms
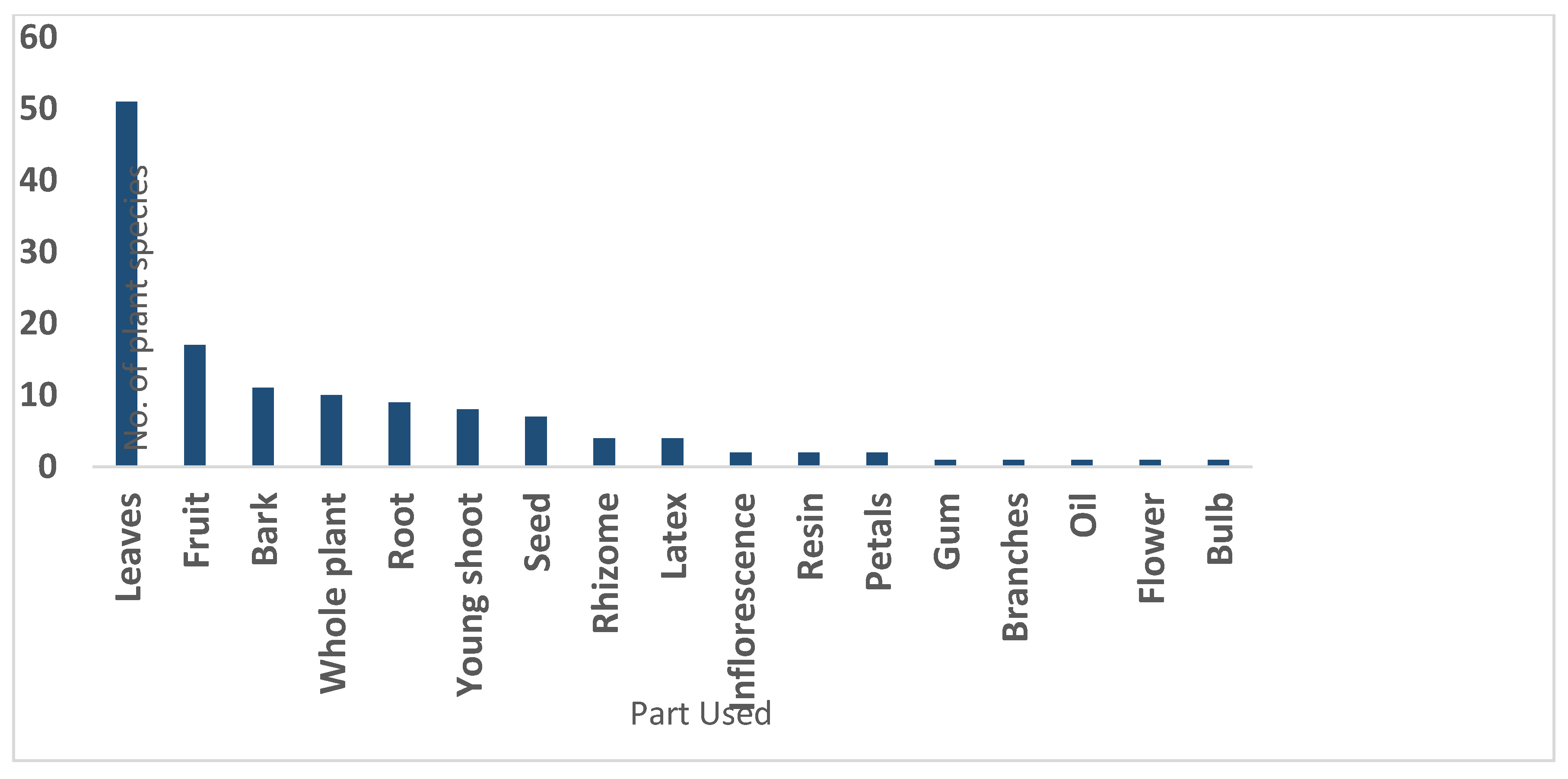
3.2. Plant Parts Used and Preparation of Remedies
3.3. Availability and Mode of Administration
3.4. Quantitative Ethnomedicinal Data Analysis
3.4.1. Use Value
3.4.2. Relative Frequency of Citation and Use Report
3.4.3. Fidelity Level
3.4.4. Informant Consensus Factor
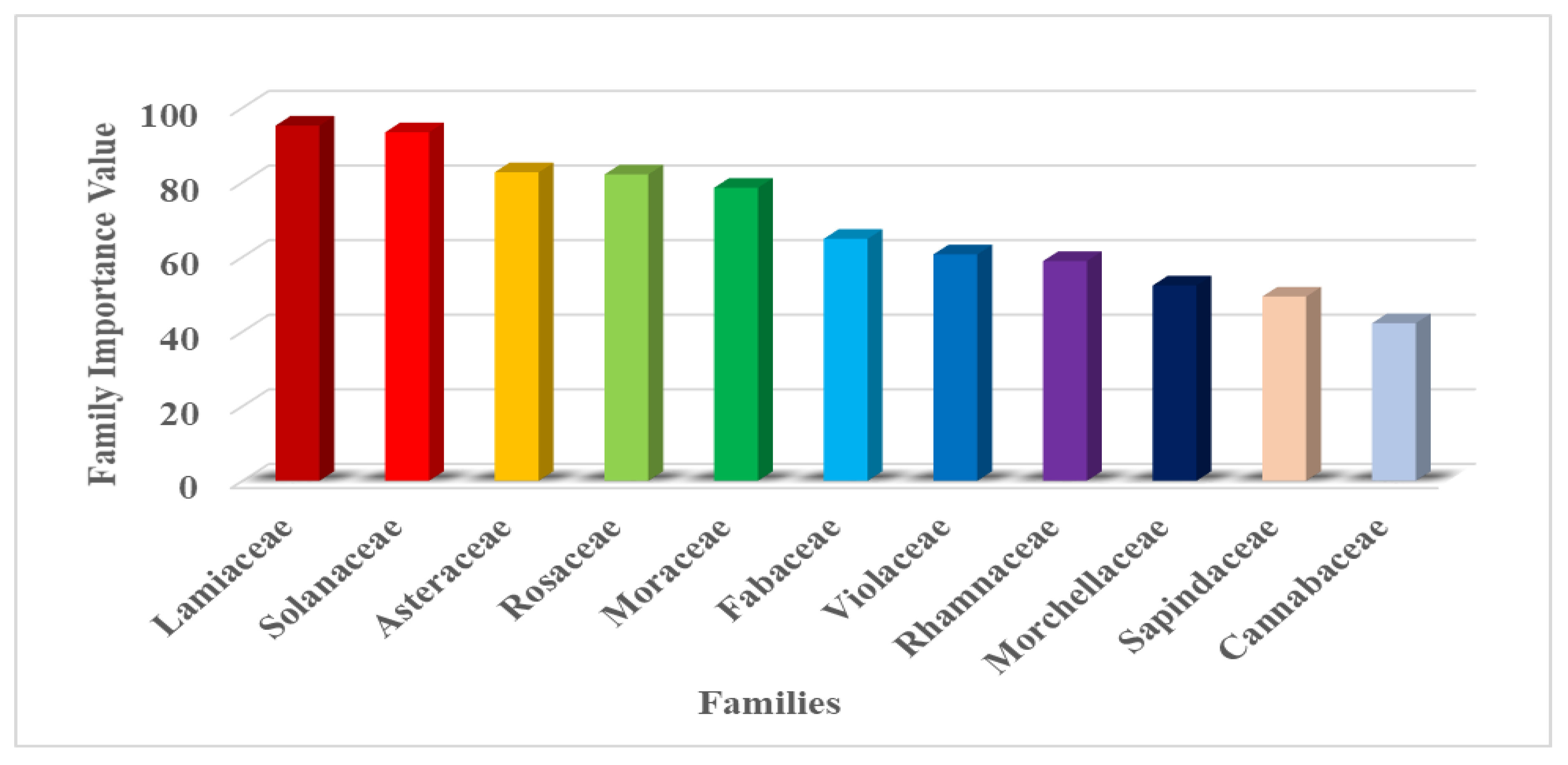
3.4.5. Family Importance Value (FIV)
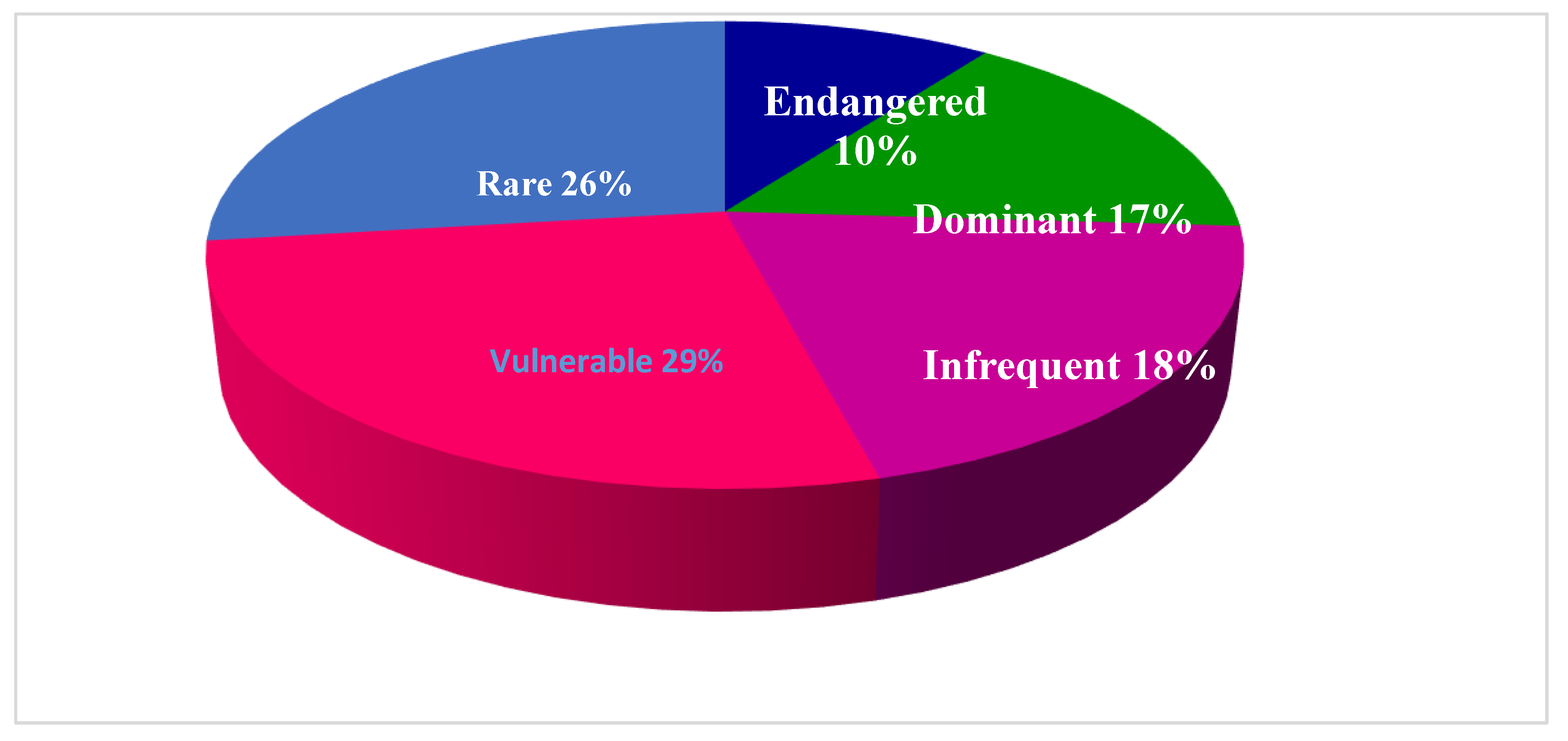
3.5. Conservation Status of the Medicinal Flora
4. Discussion
4.1. Ethnopharmacological Relevance
4.2. Novelty and Future Impacts
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Abbas, W.; Hussain, W.; Hussain, W.; Badshah, L.; Hussain, K.; Pieroni, A. Traditional wild vegetables gathered by four religious groups in Kurram District, Khyber Pakhtunkhwa, North-West Pakistan. Genet. Resour. Crop Evol. 2020, 67, 1521–1536. [Google Scholar] [CrossRef]
- Asase, A.; Kadera, M. Herbal medicines for child healthcare from Ghana. J. Herb. Med. 2014, 4, 24–36. [Google Scholar] [CrossRef]
- Giday, K.; Lenaerts, L.; Gebrehiwot, K.; Yirga, G.; Verbist, B.; Muys, B.X. Ethnobotanical study of medicinal plants from degraded dry afromontane forest in northern Ethiopia: Species, uses and conservation challenges. J. Herb. Med. 2017, 6, 96–104. [Google Scholar] [CrossRef]
- Hussain, W.; Hussain, J.; Ali, R.; Khan, I.; Shinwari, Z.K.; Nascimento, I.A. Tradable and conservation status of medicinal plants of Kurram Valley. Parachinar, Pakistan. J. Appl. Pharmac. Sci. 2012, 2, 66–70. [Google Scholar] [CrossRef][Green Version]
- Kpodar, M.S.; Lawson-Evi, P.; Bakoma, B.; Eklu-Gadegbeku, P.; Agbonon, A.; Aklikokou, A.; Gbeassor, M. Ethnopharmacological survey of plants used in the treatment of diabetes mellitus in south of Togo (Maritime Region). J. Herb. Med. 2015, 5, 147–152. [Google Scholar] [CrossRef]
- Hao, D.-C.; Xiao, P.-G. Pharmaceutical resource discovery from traditional medicinal plants: Pharmacophy- logeny and pharmacophylogenomics. Chin. Herb. Med. 2020, 9, 11. [Google Scholar] [CrossRef]
- Wagh, V.V.; Jain, A.K. Ethnopharmacological survey of plants used by the Bhil and Bhilala ethnic community in dermatological disorders in Western Madhya Pradesh, India. J. Herb. Med. 2020, 19, 100234. [Google Scholar] [CrossRef]
- Adeniyi, A.; Asase, A.; Ekpe, P.K.; Asitoakor, B.K.; Adu-Gyamfi, A.; Avekor, P.Y. Ethnobotanical study of medicinal plants from Ghana; confirmation of ethnobotanical uses, and review of biological and toxicological studies on medicinal plants used in Apra Hills Sacred Grove. J. Herb. Med. 2018, 14, 76–87. [Google Scholar] [CrossRef]
- Hayta, S.; Polat, R.; Selvi, S. Traditional uses of medicinal plants in Elazığ (Turkey). J. Ethnopharmacol. 2014, 155, 171–184. [Google Scholar] [CrossRef]
- Umair, M.; Altaf, M.; Abbasi, A.M. An ethnobotanical survey of indigenous medicinal plants in Hafizabad district, Punjab-Pakistan. PLoS ONE 2017, 12, e0177912. [Google Scholar] [CrossRef]
- Ekor, M. The growing use of herbal medicines: Issues relating to adverse reactions and challenges in monitoring safety. Front. Pharmacol. 2014, 7, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Mahomoodally, F.; Suroowan, S.; Sreekeessoon, U. Adverse reactions of herbal medicine a quantitative assessment of severity in Mauritius. J. Herb. Med. 2018. [Google Scholar] [CrossRef]
- Kayani, S.; Ahmad, M.; Zafar, M.; Sultana, S.; Khan, M.P.Z.; Ashraf, M.A.; Hussain, J.; Yaseen, G. Ethnobotanical uses of medicinal plants for respiratory disorders among the inhabitants of Gallies–Abbottabad, Northern Pakistan. J. Ethnopharmacol. 2014, 156, 47–60. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, K.S.; Hamid, A.; Nawaz, F.; Hameed, M.; Ahmad, F.; Deng, J.; Akhtar, N.; Wazarat, A.; Mahroof, S. Ethnopharmacological studies of indigenous plants in Kel village, Neelum Valley, Azad Kashmir, Pakistan. J. Ethnobiol. Ethnomed. 2017, 13, 68. [Google Scholar] [CrossRef] [PubMed]
- Ong, H.G.; Kim, Y.D. Quantitative ethnobotanical study of the medicinal plants used by the Ati Negrito indigenous group in Guimaras Island, Philippines. J. Ethnopharmacol. 2014, 157, 228–242. [Google Scholar] [CrossRef] [PubMed]
- Rashid, N.; Gbedomon, R.C.; Ahmad, M.; Salako, V.K.; Zafar, M.; Malik, K. Traditional knowledge on herbal drinks among indigenous communities in Azad Jammu and Kashmir, Pakistan. J. Ehnobiol. Ethnomed. 2018, 14, 16. [Google Scholar] [CrossRef] [PubMed]
- Shinwari, Z.K.; Qaisar, M. Efforts on conservation and sustainable use of medicinal plants of Pakistan. Pak. J. Bot. 2011, 43, 5–10. [Google Scholar]
- Hussain, S.; Malik, F.; Khalid, N.; Qayyum, M.A.; Riaz, H. Alternative and traditional medicines systems in Pakistan: History, Regulation, Trends, Usefulness, Challenges, Prospects and Limitations. In A Compendium of Essays on Alternative Therapy; InTech: London, UK, 2012; p. 67. [Google Scholar]
- Kanwal, H.; Sherazi, B.A. Herbal medicine: Trend of practice, perspective, and limitations in Pakistan. Asian Pac. J. Health Sci. 2017, 4, 6–8. [Google Scholar] [CrossRef]
- Petrakoua, K.; Iatroub, G.; Lamari, F.N. Ethnopharmacological survey of medicinal plants traded in herbal markets in the Peloponnisos, Greece. J. Herb. Med. 2020, 19, 100305. [Google Scholar] [CrossRef]
- Farooq, A.; Amjad, M.S.; Ahmad, K.; Altaf, M.; Umair, M.; Abbasi, M.A. Ethnomedicinal knowledge of the rural communities of Dhirkot, Azad Jammu and Kashmir, Pakistan. J. Ethnobiol. Ethnomed. 2019, 15, 45. [Google Scholar] [CrossRef]
- Hussain, W.; Badshah, L.; Ullah, M.; Ali, M.; Ali, A.; Hussain, F. Quantitative study of medicinal plants used by the communities residing in Koh-e-Safaid Range, northern Pakistani-Afghan borders. J. Ethnobiol. Ethnomed. 2018, 14, 30. [Google Scholar] [CrossRef] [PubMed]
- Kangl, A.; Moon, S.K.; Cho, S.Y.; Park, S.U.; Jung, W.S.; Park, J.M.; Ko, C.N.; Cho, K.H.; Kwon, S. Herbal medicine treatments for essential tremor: A retrospective chart review study. J. Herb. Med. 2020, 19, 100295. [Google Scholar] [CrossRef]
- Eddouks, M.; Bidi, A.; El-Bouhali, B.; Hajji, L.; Zeggwagh, N.A. Antidiabetic plants improving insulin sensitivity. J. Pharm. Pharmacol. 2014, 66, 1197–1214. [Google Scholar] [CrossRef] [PubMed]
- Malik, K.; Ahmad, M.; Zafar, M.; Ullah, R.; Mahmood, H.M.; Parveen, B.; Rashid, N.; Sultana, S.; Shah, S.N. An ethnobotanical study of medicinal plants used to treat skin diseases in northern Pakistan. BMC Compl. Altern. Medici. 2019, 19, 210. [Google Scholar] [CrossRef] [PubMed]
- Sher, H.; Aldosari, A.; Ali, A.; De Boer, H.J. Economic benefits of high value medicinal plants to Pakistani communities: An analysis of current practice and potential. J. Ethnobiol. Ethnomed. 2014, 10, 71. [Google Scholar] [CrossRef]
- Fatima, A.; Ahmad, M.; Zafar, M.; Yaseen, G.; Khan, M.P.Z.; Butt, M.A.; Sultana, S. Ethnopharmacological relevance of medicinal plants used for the treatment of oral diseases in Central Punjab-Pakistan. J. Herb. Med. 2017. [Google Scholar] [CrossRef]
- Kasilo, O.M.; Trapsida, J.M.; Ngenda, M.C.; Lusamba-Dikassa, P.S. World Health Organization. An overview of the traditional medicine situation in the African region. Afr. Health Monit. 2010, 4, 7–15. [Google Scholar]
- Mwangia, V.I.; Mumob, R.M.; Nyachieoa, A.; Onkoba, N. Herbal medicine in the treatment of poverty associated parasitic diseases: A case of sub-Saharan Africa. J. Herb. Med. 2017, 10, 1–7. [Google Scholar] [CrossRef]
- Hussain, W.; Ullah, M.; Dastagir, G.; Badshah, L. Quantitative ethnobotanical appraisal of medicinal plants used by inhabitants of lower Kurram, Kurram agency, Pakistan. Avic. J. Phyt. 2018, 8, 313. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6204146/ (accessed on 22 February 2020).
- Mahmood, A.; Malik, R.N.; Shinwari, Z.K. Indigenous knowledge of medicinal plants from Gujranwala district, Pakistan. J. Ethnopharmacol. 2013, 148, 714–723. [Google Scholar] [CrossRef]
- Haq, F.; Ahmad, H.; Alam, M. Traditional uses of medicinal plants of Nandiar Khuwarr catchment (district Battagram), Pakistan. J. Med. Plants Res. 2011, 5, 39–48. [Google Scholar]
- Aziz, M.A.; Khan, A.H.; Adnan, M.; Ullah, H. Traditional uses of medicinal plants used by Indigenous communities for veterinary practices at Bajaur Agency, Pakistan. J. Ehnobiol. Ethnomed. 2018, 14, 11. [Google Scholar] [CrossRef] [PubMed]
- Dilshad, S.M.R.; Rehman, N.U.; Ahmad, N.; Iqbal, A. Documentation of ethnoveterinary practices for mastitis in dairy animals in Pakistan. Pak. Vet. J. 2010, 30, 167–171. [Google Scholar]
- Shaheen, S.; Ramzan, S.; Haroon, N.; Hussain, K. Ethnopharmacological and systematic studies of selected medicinal plants of Pakistan. Pak. J. Sci. 2014, 66, 175–180. Available online: https://www.researchgate.net/publication/263451852 (accessed on 14 April 2020).
- Umair, M.; Altaf, M.; Bussmann, R.W.; Abbasi, A.M. Ethnomedicinal uses of the local flora in Chenab riverine area, Punjab province Pakistan. J. Ehnobiol. Ethnomed. 2019, 15, 7. [Google Scholar] [CrossRef] [PubMed]
- Ullah, N. Medicinal Plants of Pakistan: Challenges and Opportunities. Int. J. Complement. Alt. Med. 2017, 6, 00193. [Google Scholar] [CrossRef]
- Shinwari, Z.K. Medicinal plants research in Pakistan. J. Med. Plants Res. 2010, 4, 161–176. [Google Scholar]
- Usman ghani, K. Reshaping of Eastern Medicine in Pakistan. RADS J. Pharm. Pharmaceut. Sci. 2017, 5, 1–3. [Google Scholar]
- Shah, A.H.; Khan, S.M.; Shah, A.H.; Mehmood, A.; Rehman, I.U.; Ahmad, H. Cultural usesof plants among Basikhel tribe of District Tor Ghar, Khyber Pakhtunkhwa, Pakistan. Pak. J. Bot. 2015, 47, 23–41. [Google Scholar]
- Zaman, S.U.; Ali, K.; Khan, W.; Ali, M.; Jan, T.; Nisar, M. Ethno-botanical and geo-referenced profiling of medicinal plants of Nawagai Valley, District Buner (Pakistan). Biosyst. Divers. 2018, 26, 56–61. [Google Scholar] [CrossRef]
- Hamayun, M. Ethnobotanical studies of some useful shrubs and trees of District Buner, NWFP, Pakistan. Ethnobot. Leafl. 2003, 2003, 12. Available online: https://opensiuc.lib.siu.edu/ebl/vol2005/iss1/43 (accessed on 24 March 2020).
- Khan, A.; Gilani, S.S.; Hussain, F.; Durrani, M.J. Ethnobotany of Gokand valley, District Buner, Pakistan. Pak. J. Biol. Sci. 2003, 6, 363–369. [Google Scholar] [CrossRef]
- Ali, S.I.; Nasir, Y.J. (Eds.) 1989–1992. Flora of Pakistan. No. 191-193. Islamabad, Karcahi.
- Ali, S.I.; Qaiser, M. (Eds.) 1993–2015. Flora of Pakistan. No. 194-221. Islamabad, Karachi.
- Nasir, E.; Ali, S.I. (Eds.) 1970–1989. Flora of West Pakistan. No. 1-131. Islamabad, Karachi.
- Ferreira, F.S.; Brito, S.V.; Ribeiro, S.C.; Almeido, W.O.; Alves, R.R.N. Zootherapeutics utilized by residents of the community Poco Dantas, Crato-CE, Brazil. J. Ethnobiol. Ethnomed. 2009, 5, 21. [Google Scholar] [CrossRef] [PubMed]
- Vitalini, S.; Iriti, M.; Puricelli, C.; Ciuchi, D.; Segale, A.; Fico, G. Traditional knowledge on medicinal and food plants used in Val San Giacomo (Sondrio, Italy)—An alpine ethnobotanical study. J. Ethnopharmacol. 2013, 145, 517–529. [Google Scholar] [CrossRef]
- Yaseen, G.; Ahmad, M.; Sultana, S.; Alharrasi, A.S.; Hussain, J.; Zafar, M. Ethnobotany of medicinal plants in the Thar Desert (Sindh) of Pakistan. J. Ethnopharmacol. 2015, 163, 43–59. [Google Scholar] [CrossRef]
- Idm’hand, E.; Msanda, F.; Cherifi, K. Ethnobotanical study and biodiversity of medicinal plants used in the Tarfaya Province, Morocco. Acta Ecol. Sinica. 2020, 40, 134–144. [Google Scholar] [CrossRef]
- Heinrich, M.; Ankli, A.; Frei, B.; Weimann, C.; Sticher, O. Medicinal plants in Mexico: Healers’ consensus and cultural importance. Soc. Sci. Med. 1998, 47, 1859–1871. [Google Scholar] [CrossRef]
- Anonymous. IUCN Red List Categories and Criteria: Version 3.1; IUCN Species Survival Commission IUCN: Gland, Switzerland; Cambridge, UK, 2001. [Google Scholar]
- Oliver, S.J. The role of traditional medicine practice in primary health care within aboriginal Australia: A review of the literature. J. Ehnobiol. Ethnomed. 2013, 9, 46. [Google Scholar] [CrossRef]
- Kamalebo, H.M.; Malale, H.N.S.W.; Ndabaga, C.M.; Degreef, J.; Kesel, A.D. Uses and importance of wild fungi: Traditional knowledge from the Tshopo province in the Democratic Republic of the Congo. J. Ehnobiol. Ethnomed. 2018, 14, 13. [Google Scholar] [CrossRef]
- Barkatullah, I.M.; Rauf, A.; Hadda, T.B.; Mubarak, M.S.; Patel, S. Quantitative ethnobotanical survey of medicinal flora thriving in Malakand Pass Hills, Khyber PakhtunKhwa, Pakistan. J. Ethnopharmacol. 2015, 169, 335–346. [Google Scholar] [CrossRef]
- Shah, S.A.; Shah, N.A.; Ullah, S.; Alam, M.M.; Badshah, H.; Ullah, S.; Mumtaz, A.S. Documenting the indigenous knowledge on medicinal flora from communities residing near Swat River (Suvastu) and in high mountainous areas in Swat-Pakistan. J. Ethnopharmacol. 2016, 182, 67–79. [Google Scholar] [CrossRef]
- Kidane, L.; Gebremedhin, G.; Beyene, T. Ethnobotanical study of medicinal plants in Ganta Afeshum District, Eastern Zone of Tigray, Northern Ethiopia. J. Ethnobiol. Ethnomed. 2018, 14, 64. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, X.-M.-A.; Bun, S.-S.; Ollivier, E.; Dang, T.-P.-T. Ethnobotanical study of medicinal plants used by K’Ho-Cil people for treatment of diarrhea in Lam Dong Province, Vietnam. J. Herb. Med. 2020, 19, 10032. [Google Scholar] [CrossRef]
- Abbasi, A.M.; Shah, M.H.; Khan, M.A. Wild Edible Vegetables of Lesser Himalayas: Ethnobotanical and Nutraceutical Aspects; Springer: Cham, Switzerland, 2015; Volume 1. [Google Scholar]
- Tuasha, N.; Petros, B.; Asfaw, Z. Medicinal plants used by traditional healers to treat malignancies and other human ailments in Dalle District, Sidama Zone, Ethiopia. J. Ethnobiol. Ethnomed. 2018, 14, 15. [Google Scholar] [CrossRef] [PubMed]
- Ouelbani, R.; Bensari, S.; Mouas, T.N.; Khelifi, D. Ethnobotanical investigations on plants used in folk medicine in the regions of Constantine and Mila (North-East of Algeria). J. Ethnopharmacol. 2016, 194, 196–218. [Google Scholar] [CrossRef]
- Ahmad, M.; Zafar, M.; Shahzadi, N.; Yaseen, G.; Murphey, T.M.; Sultana, S. Ethnobotanical importance of medicinal plants traded in Herbal markets of Rawalpindi-Pakistan. J. Herb. Med. 2017, 11, 78–89. [Google Scholar] [CrossRef]
- Sabir, S.; Arshad, M.; Hussain, M.; Sadaf, H.M.; Imran, M.; Yasmeen, F.; Chaudhari, S.K. A probe into biochemical potential of Aconitum violaceum: A medicinal plant from Himalaya. Asi. Pacific J. Trop. Dis. 2016, 6, 502–504. [Google Scholar] [CrossRef]
- Abbas, Z.; Khan, S.M.; Abbasi, A.M.; Pieroni, A.; Ullah, Z.; Iqbal, M.; Ahmad, Z. Ethnobotany of the Balti community, Tormik valley, Karakorum range, Baltistan, Pakistan. J. Ehnobiol. Ethnomed. 2016, 12, 38. [Google Scholar] [CrossRef]
- Günes, S.; Savran, A.; Paksoy, M.Y.; Kosar, M.; Cakılcıoglu, U. Ethnopharmacological survey of medicinal plants in Karaisalı and its surrounding (Adana-Turkey). J. Herbal Med. 2017. [Google Scholar] [CrossRef]
- Ko, H.J.; Oh, S.K.; Jin, J.H.; Son, K.H.; Kim, H.P. Inhibition of Experimental Systemic Inflammation (Septic Inflammation) and Chronic Bronchitis by New Phytoformula BL Containing Broussonetia papyrifera and Lonicera japonica. Biomol. Ther. 2012, 21, 66–71. [Google Scholar] [CrossRef][Green Version]
- Asghari, G.; Akbari, M.; Asadi-Samani, M. Phytochemical analysis of some plants from Lamiaceae family frequently used in folk medicine in Aligudarz region of Lorestan province. Marmara Pharmaceut. J. 2017, 21, 506–514. [Google Scholar] [CrossRef]
- Mehmood, A.; Murtaza, G. Phenolic contents, antimicrobial and antioxidant activity of Olea ferruginea Royle (Oleaceae). BMC Complement. Altern. Med. 2018, 18, 173. [Google Scholar] [CrossRef] [PubMed]
- Semerdjieva, I.B.; Zheljazkov, V.D. Chemical Constituents, Biological Properties, and Uses of Tribulus terrestris: A Review. Natur. Prod. Communi. 2019, 14, 1934578X19868394. [Google Scholar] [CrossRef]
- Nair, A.R.; Praveen, N. Biochemical and phytochemical variations during the growth phase of Withania somnifera (L.) Dunal. J. Pharmaco. Phytoch. 2019, 8, 1930–1937. [Google Scholar]
- Asati, A.K.; Sahoo, H.B.; Sahu, S.; Dwivedi, A. Phytochemical and pharmacological profile of Cannabis sativa L. Int. J. Ind. Herbs Drugs. 2017, 2, 37–45. [Google Scholar]
- Sarwar, W. Pharmacological and phytochemical studies on Acacia modesta Wall; A review. J. Phytopharmac. 2016, 5, 160–166. [Google Scholar]
- Yeşil, Y.; İnal, İ. Traditional knowledge of wild edible plants in Hasankeyf (Batman Province, Turkey). Acta Soc. Bot. Pol. 2019, 88, 3633. [Google Scholar] [CrossRef]

| Variables | Categories | Number of Informants | Percentage | Sum of Reports |
|---|---|---|---|---|
| Gender ratio | Men | 47 | 27.976 | 588 |
| Women | 121 | 72.023 | 2709 | |
| Age | <20 | 15 | 8.928 | 107 |
| 21–40 | 33 | 19.642 | 217 | |
| 41–60 | 58 | 34.523 | 409 | |
| >60 | 62 | 36.904 | 2564 | |
| Educational Background | Illiterate | 67 | 39.88 | 1682 |
| Matric | 53 | 31.547 | 838 | |
| Intermediate | 26 | 15.476 | 352 | |
| Graduate | 17 | 10.119 | 300 | |
| Postgraduate | 5 | 2.976 | 125 | |
| Informant category | Farmer | 37 | 22.023 | 1455 |
| Elder (housewives and non-professional) | 33 | 19.642 | 930 | |
| Profession | Shepherd | 26 | 15.476 | 130 |
| Plant gatherer | 29 | 17.261 | 195 | |
| Healer | 14 | 8.333 | 453 | |
| Hunter | 15 | 8.928 | 85 | |
| Salesperson | 5 | 2.976 | 11 | |
| Dealer | 9 | 5.357 | 38 | |
| Life type | Urban area | 36 | 21.428 | - |
| Hilly area | 132 | 78.571 | - |
| Availability | Collection |
|---|---|
| 0 = Uncommon or very rare | 0 = More than 1000 kg/year |
| 1 = Less common or rare | 1 = Consumed from 500–1000 kg/year |
| 2 = Occasional | 2 = Consumed from 300–500 kg/year |
| 3 = Abundant | 3 = Consumed from 100–200 kg/year |
| Growth | Part used |
| 0 = Regrowth in more 3 years | 0 = Root/Whole |
| 1 = Regrowth within 3 years | 1 = Bark |
| 2 = Regrowth within 2 years | 2 = Seeds, Fruits |
| 3 = Regrowth within 1 year | 3 = Flowers |
| 4 = Regrowth in a season | 4 = Leaves/Gum/Latex |
| Total Score | |
| 0–4 | Endangered |
| 5–8 | Vulnerable |
| 9–12 | Rare |
| 13–14 | Infrequent |
| 15–16 | Dominant |
| Family | Botanical Name Local Name Voucher Number | Availability | Habit | Part(s) Used | Preparation of Remedies | ROA | Medicinal Uses | FC | RFC | UR | UV | FL | CS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pteridophytes | |||||||||||||
| Dryopteridaceae | Dryopteris juxtaposita Christ. Kwangai B.Sul.059.UOP | W | H | Young shoot | Juice | O | Bone weakness, dyspepsia | 43 | 0.255 | 22 | 0.51 | 65.11 | E |
| Equisetaceae | Equisetum arvense L. Bandaky B.Sul.061.UOP | W | H | Whole plant | Juice | O | Kidney stones | 26 | 0.154 | 11 | 0.42 | 57.69 | V |
| Pteridaceae | Adiantum capillus-veneris L. Sumbal B.Sul.025.UO | W | H | Whole plant | Decoction | O | Constipation, pneumonia, scorpion bite | 23 | 0.136 | 15 | 0.65 | 56.52 | E |
| Adiantum venustum D. Don Parsohan B.Sul.026.UOP | W | H | Whole plant | Decoction | O | Scorpion bite, constipation | 32 | 0.19 | 18 | 0.56 | 31.25 | V | |
| Angiosperm | |||||||||||||
| Acanthaceae | Justicia adhatoda L. Bekar B.Sul.071.UOP | W | S | Leaves | Decoction, poultice | O, top. | Wound, swelling, arthritis, headache | 30 | 0.178 | 13 | 0.43 | 50 | D |
| Acoraceae | Acorus calamus L. Skha waga B.Sul.024.UOP | W | H | Rhizome | Decoction | O | Menstrual cycle regularity, dyspepsia | 10 | 0.059 | 2 | 0.2 | 20 | R |
| Amaranthaceae | Achyranthes aspera L. Ghishkay B.Sul.022.UOP | W | H | Leaves | Juice | O | Stomachache, arthritis, diarrhea | 15 | 0.089 | 4 | 0.26 | 46.66 | I |
| Amaranthus viridis L. Chalwery B.Sul.032.UOP | W | H | Leaves | Juice, poultice, vegetable | O, top. | Urinary diseases, hair tonic | 12 | 0.071 | 5 | 0.41 | 33.33 | D | |
| Amaryllidaceae | Allium jacquemontii Kunth Oraky B.Sul.031.UOP | W | H | Leaves | Roast, decoction | O | Blood pressure, abdominal pain | 24 | 0.142 | 12 | 0.5 | 62.5 | R |
| Narcissus poeticus L. Gul-nargus B.Sul.082.UOP | W | H | Bulb | Juice | O | Allergy, pimples | 33 | 0.196 | 13 | 0.39 | 54.54 | C | |
| Anacardiaceae | Pistacia integerrima J.L. Stewart ex Brandis Kharawa B.Sul.094.UOP | W | T | Bark | Decoction | O | Hepatitis, loss of appetite | 43 | 0.255 | 22 | 0.51 | 65.11 | R |
| Apiaceae | Pimpinella diversifolia DC. Tarpakai B.Sul.091.UOP | W | H | Leaves | Decoction | O | Fever, stomachache, emphysema | 28 | 0.166 | 13 | 0.46 | 50 | V |
| Apocynaceae | Caralluma edulis (Edgew.) Benth. Ex Hook.f. Famanhy B.Sul.046.UOP | W | H | Whole plant | Decoction, powder | O | Anti-peristalsis, otitis media | 37 | 0.22 | 14 | 0.37 | 51.35 | R |
| Nerium oleander L. Ganderay B.Sul.084.UOP | C | S | Leaves | Roast | O | Anti-microbial, tooth ache | 21 | 0.125 | 10 | 0.47 | 66.66 | --- | |
| Araliaceae | Hedera helix L. Payo zela B.Sul.068.UOP | W | S | Leaves | Decoction | O | Diabetes, arthritis | 35 | 0.208 | 18 | 0.51 | 51.42 | V |
| Asclepiadaceae | Calotropis procera (Aiton) Dryand. Spalamy B.Sul.043.UOP | W | S | Leaves | Powder | O | Digestion, flatulence | 21 | 0.125 | 11 | 0.52 | 66.66 | E |
| Asparagaceae | Asparagus officinalis L. Tendory B.Sul.035.UOP | W | S | Root, young shoot | Juice | O | Fever, flatulence, kidney stones | 23 | 0.136 | 10 | 0.43 | 47.82 | V |
| Asparagus racemosus Willd. Gangra boty B.Sul.036.UOP | W | H | Leaves | Decoction | O, top. | Arthritis, skin diseases | 19 | 0.113 | 7 | 0.36 | 42.10 | V | |
| Asphodelaceae | Asphodelus tenuifolius Cav. Ogaky B.Sul.037.UOP | W | H | Leaves | Decoction | O | Blood pressure, tension | 38 | 0.226 | 17 | 0.44 | 55.26 | R |
| Asteraceae | Artemisia vulgaris L. Tarkha B.Sul.034.UOP | W | S | Root, leaves | Poultice | top. | Skin diseases, Intestinal worms | 38 | 0.226 | 18 | 0.47 | 47.36 | E |
| Cichorium intybus L. Harn B.Sul.051.UOP | W | S | Leaves | Decoction | O | Asthma, indigestion | 32 | 0.19 | 13 | 0.40 | 56.25 | V | |
| Senecio chrysanthemoides DC. Sra jaby B.Sul.107.UOP | W | H | Leaves, rhizome | Poultice | top. | Swelling, wound healing | 27 | 0.16 | 13 | 0.48 | 62.96 | I | |
| Sonchus asper L. Hill Shodapy B.Sul.110.UOP | W | H | Leaves | Decoction | O | Stomach problems, antipyretic | 15 | 0.089 | 5 | 0.33 | 40 | R | |
| Taraxacum officinale F.H. Wigg. Ziar guly B.Sul.114.UOP | W | H | Leaves, petals | Decoction | O | Cough, yellowness of skin eyes and urine | 18 | 0.107 | 8 | 0.44 | 38.88 | D | |
| Xanthium strumarium L. Ghishky B.Sul.126.UOP | W | S | Leaves, seeds | Decoction, Poultice | O, top. | Indigestion, diarrhea, smallpox | 9 | 0.053 | 3 | 0.33 | 22.22 | D | |
| Berberidaceae | Berberis lycium Royle Kwary B.Sul.039.UOP | W | S | Leaves, root, bark | Poultice, decoction | O, top. | Diabetic, wound healing, bone fracture, pain, diarrhea | 45 | 0.267 | 35 | 0.77 | 93.33 | V |
| Boraginaceae | Trichodesma indicum (L.) Lehm. Ghwa jaby B.Sul.118.UOP | W | H | Root | Poultice | top. | Anti-inflammatory, snake bite | 38 | 0.226 | 17 | 0.44 | 50 | R |
| Brassicaceae | Capsella bursa-pastoris (L.) Medik. Bambysa B.Sul.045.UOP | W | H | Leaves, root | Juice | O | Tension, anxiolytic | 33 | 0.196 | 12 | 0.36 | 45.45 | V |
| Nasturtium officinale R.Br. Talmera B.Sul.083.UOP | W | H | Root, young shoot | Juice, vegetable | O | Wound healing, toothache | 26 | 0.154 | 12 | 0.46 | 46.15 | D | |
| Buxaceae | Buxus wallichiana L. Shamshad B.Sul.042.UOP | W | S | Leaves | Powder, decoction | O, top. | Arthritis, bone fracture, purgative | 39 | 0.232 | 19 | 0.48 | 51.28 | V |
| Cactaceae | Opuntia dillenii (Ker Gawl.) Haw. Tohar B.Sul.086.UOP | W | H | Fruit | Juice | O | Anemia | 40 | 0.238 | 21 | 0.52 | 70 | D |
| Caesalpiniaceae | Cassiafistula L. Amaltas B.Sul.047.UOP | W | T | Fruit | Decoction | O | Constipation, skin infection, fever | 42 | 0.25 | 22 | 0.52 | 76.19 | R |
| Cannabaceae | Cannabis sativa L. Bang B.Sul.044.UOP | W | H | Leaves | Smoke, Poultice | Inhale | Sedative, narcotic, ulcer, pain killer | 34 | 0.202 | 16 | 0.47 | 70.58 | D |
| Celtis caucasica L. Tagha B.Sul.049.UOP | W | T | Bark, fruit | Decoction, Poultice | O, top. | Wound healing, burning | 37 | 0.22 | 17 | 0.45 | 54.05 | V | |
| Caryophyllaceae | Stellaria media L. Vill. Spin goly B.Sul.112.UOP | W | H | Leaves | Poultice | top. | Bone fracture | 32 | 0.19 | 10 | 0.31 | 40.62 | I |
| Celastraceae | Gymnosporia royleana Wall. Sor azghay B.Sul.067.UOP | W | S | Fruit | Direct | O | Blood purifier, gum pain | 28 | 0.166 | 10 | 0.35 | 39.28 | D |
| Chenopodiaceae | Chenopodium album L. Srmai B.Sul.050.UOP | W | H | Young shoot | Decoction | O | Hepatitis, constipation | 19 | 0.113 | 10 | 0.52 | 52.63 | R |
| Convolvulaceae | Convolvulus arvensis L. Prewatai B.Sul.053.UOP | W | H | Leaves | Powder | O | Pimple, acne, stomach problems | 10 | 0.059 | 4 | 0.4 | 30 | I |
| Cuscuta reflexa Roxb. Nary zaila B.Sul.054.UOP | W | H | Young shoot | Juice | O | Arthritis, blood purifier | 13 | 0.077 | 6 | 0.46 | 38.46 | I | |
| Dryopteridaceae | Dryopteris juxtaposita Christ. Kwangai B.Sul.059.UOP | W | H | Young shoot | Juice | O | Bone weakness, dyspepsia | 43 | 0.255 | 22 | 0.51 | 65.11 | E |
| Equisetaceae | Equisetum arvense L. Bandaky B.Sul.061.UOP | W | H | Whole plant | Juice | O | Kidney stones | 26 | 0.154 | 11 | 0.42 | 57.69 | V |
| Ericaceae | Conandrium arnotaimum L. Sra makha B.Sul.052.UOP | W | S | Whole plant | Decoction | O | Skin allergy | 30 | 0.178 | 15 | 0.5 | 60 | E |
| Rhododendron arboreum Sm. Gul-namaire B.Sul.099.UOP | W | S | Flower | Juice | O | Antipyretic | 27 | 0.16 | 14 | 0.51 | 59.25 | I | |
| Euphorbiaceae | Euphorbia helioscopia L. Mandanro B.Sul.062.UOP | W | H | Latex | Powder | O | Kidney stone, cholera | 23 | 0.136 | 12 | 0.52 | 69.56 | D |
| Euphorbia hirta L. Wrmago B.Sul.063.UOP | W | H | Latex | Poultice, juice | O, top. | Kidney stone, bronchitis, constipation | 30 | 0.178 | 15 | 0.5 | 60 | I | |
| Mallotus philippensis (Lam.) Müll.-Arg. Kambela B.Sul.072.UOP | W | T | Bark, seed | Juice, direct | O | Stomach pain | 16 | 0.095 | 8 | 0.5 | 56.25 | R | |
| Fabaceae | Acacia modesta Wall. Palosa B.Sul.021.UOP | W | T | Gum | Direct | O | Relaxant, hepatitis | 48 | 0.285 | 43 | 0.89 | 100 | R |
| Fabaceae | Indigofera gerardiana Wall Ghoreja B.Sul.069.UOP | W | S | Root | Direct | O | Stomach ache | 38 | 0.226 | 16 | 0.42 | 47.36 | V |
| Fabaceae | Robinia pseudoacacia L. Kikar B.Sul.100.UOP | C | T | Leaves, Inflorescence | Decoction, poultice | O, top. | Spasm, diabetes | 23 | 0.136 | 9 | 0.39 | 47.82 | --- |
| Fagaceae | Quercus incana Bartram Tor banj B.Sul.098.UOP | W | T | Bark | Powder, Poultice | O, top. | Bone fracture, urinary disorders | 40 | 0.238 | 20 | 0.5 | 65 | V |
| Fumariaceae | Fumaria indica (Hausskn.) Pugsley Papra B.Sul.066.UOP | W | H | Young shoot | Decoction, juice | O | Blood pressure, vomiting, fever, antispasmodic | 41 | 0.244 | 21 | 0.51 | 68.29 | D |
| Juglandaceae | Juglans regia L. Ghoz B.Sul.070.UOP | C | T | Bark | Decoction | O | Wound healing, cleaning teeth | 32 | 0.19 | 12 | 0.37 | 53.12 | -- |
| Lamiaceae | Ajuga bracteosa Wall. Ex Benth. Bote B.Sul.030.UOP | W | H | Whole plant | Decoction, juice | O | Antipyretic, Blood pressure | 20 | 0.119 | 8 | 0.4 | 30 | E |
| Mentha longifolia L. Welany B.Sul.074.UOP | W | H | Leaves | Powder, juice | O | Diarrhea, vomiting, abdominal pain | 46 | 0.273 | 38 | 0.82 | 95.65 | I | |
| Mentha piperata Stokes Podina B.Sul.075.UOP | W | H | Leaves | Powder, juice | O | Abdominal pain, indigestion, diarrhea, nausea | 42 | 0.25 | 21 | 0.5 | 73.80 | D | |
| Mentha spicata L. Podina B.Sul.076.UOP | W | H | Leaves | Juice, powder | O | Antipyretic, vomiting, hemorrhoid | 40 | 0.238 | 20 | 0.5 | 65 | I | |
| Otostegia limbata (Benth.) Boiss. Spin azghai B.Sul.087.UOP | W | S | Leaves | Direct, powder | O, top. | Teeth ache, wound healing | 12 | 0.071 | 6 | 0.5 | 58.33 | I | |
| Meliaceae | Azadirachta indica L. Meem B.Sul.038.UOP | W | T | Leaves | Decoction | O | Hepatitis, vermicide | 45 | 0.267 | 36 | 0.80 | 95.55 | V |
| Melia azedarach L. Tora bakyana B.Sul.073.UOP | W | T | Leaves, seeds | Decoction | O | Anti septic, Liver disease, laxative | 17 | 0.101 | 9 | 0.52 | 64.70 | R | |
| Menispermaceae | Tinospora cordifolia (Willd.) Miers Gelo B.Sul.116.UOP | W | H | Leaves, seeds | Powder | O | Antipyretic, liver disorders, diuretic | 38 | 0.226 | 19 | 0.5 | 68.42 | V |
| Moraceae | Broussonetia papyrifera (L.) Vent. Shah toot B.Sul.041.UOP | Inv | T | Leaves | Powder | O | Diarrhea | 13 | 0.077 | 6 | 0.46 | 38.46 | --- |
| Ficus carica L. Inza /B.Sul.064.UOP | W | T | Fruit, latex | Direct | O | Removal of wort, stomach disorders | 21 | 0.125 | 9 | 0.42 | 61.9 | V | |
| Ficus recemosa L. Ormal B.Sul.065.UOP | C | T | Latex, fruit | Direct | O, top. | Inflammation due to wasp bites | 35 | 0.208 | 17 | 0.48 | 68.57 | --- | |
| Morus alba L. Spen toot B.Sul.079.UOP | C | T | Fruit | Direct | O | Constipation, increase digestion | 30 | 0.178 | 13 | 0.43 | 60 | --- | |
| Morus nigra L. Tor too B.Sul.080.UOP | C | T | Fruit | Direct | O | Coughing, laxative, cooling agent | 33 | 0.196 | 16 | 0.48 | 66.66 | --- | |
| Myrsinaceae | Myrsine africana L. Marlorang B.Sul.081.UOP | W | S | Leaves, fruit | Direct | O | Against worms, abdominal pain | 29 | 0.172 | 11 | 0.37 | 51.72 | R |
| Wulfenia amherstiana L. Nar boty B.Sul.125.UOP | W | H | Leaves | Decoction | O | Hypertension, weakness | 18 | 0.107 | 9 | 0.5 | 61.11 | R | |
| Nitrariaceae | Peganum harmala L. Spelany B.Sul.090.UOP | W | H | Leaves | Direct | O | Obesity | 40 | 0.238 | 21 | 0.52 | 70 | V |
| Nyctaginaceae | Boerhavia diffusa L. nom. Cons. Zakhm boty B.Sul.040.UOP | W | H | Root | Poultice | top. | Skin inflammation, ulcer | 45 | 0.267 | 32 | 0.71 | 88.88 | R |
| Oleaceae | Olea ferruginea Wall. Ex Aitch. Khona B.Sul.085.UOP | W | T | Branches | Direct | Toothbrush | Toothache | 40 | 0.238 | 20 | 0.5 | 67.5 | R |
| Oxalidaceae | Oxalis corniculata L. Taroky B.Sul.088.UOP | W | H | Leaves | Juice, Poultice | O, top. | Removal of wort, stomach disorders, skin inflammation | 47 | 0.279 | 40 | 0.85 | 97.87 | D |
| Papaveraceae | Papaver rhoeas L. Zangaly khaskhash B.Sul.089.UOP | W | H | Seed | Decoction | O | Stomachache, indigestion | 37 | 0.22 | 19 | 0.51 | 67.56 | V |
| Phyllanthaceae | Andrachne cordifolia L. Chagzi panra B.Sul.033.UOP | W | S | Leaves | Decoction | O | Diabetes | 41 | 0.244 | 22 | 0.53 | 60.97 | R |
| Platanaceae | Platanus orientalis L. Cheenar B.Sul.095.UOP | C | T | Bark | Decoction | top. | Acne, pimple | 23 | 0.136 | 11 | 0.47 | 47.82 | --- |
| Poaceae | Cynodon dactylon (L.) Pers. Kabal B.Sul.055.UOP | W | H | Whole plant | Poultice | top. | Wound healing | 16 | 0.095 | 8 | 0.5 | 56.25 | D |
| Sorghum halepense (L.) Pers. Dadam B.Sul.111.UOP | W | H | Rhizome | Juice, powder | O, top. | Snake bite, anti-inflammatory | 12 | 0.071 | 3 | 0.25 | 33.33 | D | |
| Polygonaceae | Rumex dentatus L./Shalkhy/B.Sul.104.UOP | W | H | Leaves | Decoction, Poultice, vegetable | O, top. | Skin rash, wound healing | 30 | 0.178 | 15 | 0.5 | 56.66 | I |
| Rumex hastatus D. Don Taroky B.Sul.105.UOP | W | H | Leaves | Direct, juice, poultice | O, top. | Skin 1010late10, arthritis, purgative | 38 | 0.226 | 18 | 0.47 | 63.15 | V | |
| Portulacaceae | Portulaca oleracea L. Warkhary B.Sul.096.UOP | W | H | Young shoot | Vegetable, Roast | O | Constipation | 29 | 0.172 | 15 | 0.51 | 65.51 | D |
| Ranunculaceae | Aconitum violaceum Jacquem. Ex Stapf Zahar mora B.Sul.023.UOP | W | H | Roots | Juice, powder | O | Arthritis | 44 | 0.261 | 30 | 0.68 | 86.36 | E |
| Rhamnaceae | Sageretia theezans Brongn. Mamana B.Sul.106.UOP | W | S | Leaves | Juice | O | Jaundice | 43 | 0.225 | 22 | 0.51 | 67.44 | R |
| Ziziphus nummularia (Burm.f.) Wight and Arn. Ber B.Sul.128.UOP | W | S | Leaves, fruit | Decoction | O | Ulcer, skin infection | 19 | 0.113 | 8 | 0.42 | 57.89 | R | |
| Ziziphus oxyphylla Edgew. Elany B.Sul.129.UOP | W | S | Root, Fruit | Powder, decoction | O | Loss of appetite, constipation, diabetes | 37 | 0.22 | 18 | 0.48 | 64.86 | V | |
| Rosaceae | Duchesnea indica (Jacks.) Focke Zmaky toot B.Sul.060.UOP | W | H | Fruit | Decoction, direct | O | Sore throat, coughing | 16 | 0.095 | 7 | 0.43 | 50 | I |
| Pyrus pashia L. Tangy B.Sul.097.UOP | C | T | Fruit | Direct | O | Coughing, weakness | 30 | 0.178 | 14 | 0.46 | 56.66 | --- | |
| Rosa damascena Mill. Palwarai B.Sul.101.UOP | W | S | Petals | Juice | O | Diabetes | 37 | 0.22 | 19 | 0.51 | 54.05 | V | |
| Rosa webbiana Wall. Ex Royle Zangaly gulab B.Sul.102.UOP | W | S | inflorescence | Powder, direct | O | Memory stimulant, antispasmodic | 23 | 0.136 | 10 | 0.43 | 60.86 | I | |
| Rubus fruticosus G.N. Jones Karwara B.Sul.103.UOP | W | S | Fruit | Direct | O | Cooling agent | 32 | 0.19 | 12 | 0.37 | 46.87 | R | |
| Rutaceae | Zanthoxylum armatum DC. Dambara B.Sul.127.UOP | W | S | Fruit | Direct, powder | O | Gum pain, cooling agent, abdominal pain | 46 | 0.273 | 39 | 0.84 | 95.65 | V |
| Sapindaceae | Aesculus indica (Wall. Ex Cambess.) Hook. Jawaz B.Sul.027.UOP | C | T | Bark, seed | Direct, powder | O | Vermifuge | 40 | 0.238 | 23 | 0.57 | 65 | --- |
| Dodonaea viscosa (L.) Jacq. Ghorasky B.Sul.058.UOP | W | S | Leaves | Poultice | top. | Bone fracture, sprain, wound healing, | 43 | 0.255 | 26 | 0.60 | 79.06 | D | |
| Scrophulariacea | Verbascum thapsus L. Kharghogy B.Sul.119.UOP | W | H | Leaves | Juice | Eardrop | Otitis media | 16 | 0.095 | 8 | 0.5 | 56.25 | R |
| Simaroubaceae | Ailanthus altissima (Mill.) Swingle Spena bakanra B.Sul.029.UOP | W | T | Bark | Juice | O | Abdominal pain, skin irritation, pimples | 41 | 0.244 | 22 | 0.53 | 51.21 | I |
| Solanaceae | Datura innoxia Mill. Datora B.Sul.056.UOP | W | H | Leaves, fruit | Poultice | top. | Pimple, narcotic | 27 | 0.16 | 11 | 0.4 | 44.44 | R |
| Solanum nigrum L. Kachmachu B.Sul.108.UOP | W | H | Leaves, fruit | Juice, Poultice | O, top. | Gonorrhea, skin diseases | 41 | 0.244 | 21 | 0.51 | 68.29 | R | |
| Solanum surattense Burm. Marhaghon B.Sul.109.UOP | W | H | Root, leaves | Poultice, decoction, direct | O, top. | Bone fracture, bronchitis, antipyretic, | 43 | 0.255 | 25 | 0.58 | 76.74 | V | |
| Withania somnifera (L.) Dunal Kotelal B.Sul.124.UOP | W | H | Leaves | Powder, vegetable | O | Pneumonia, diuretic | 46 | 0.273 | 37 | 0.80 | 93.47 | I | |
| Tamaricaceae | Tamarix aphylla (L.) Karst. Ghaz B.Sul.113.UOP | C | T | Root, bark | Decoction | O, top. | Toothache, anti-inflammatory | 28 | 0.166 | 13 | 0.46 | 60.71 | --- |
| Taxaceae | Taxus fuana Nan Li and R.R. Mill Banrya B.Sul.115.UOP | W | T | Leaves, bark | Powder | O | Diabetes, hepatitis, pneumonia | 31 | 0.184 | 11 | 0.35 | 48.38 | V |
| Urticaceae | Debregeasia saeneb (Forssk.) Hepper Ajlai B.Sul.057.UOP | W | S | Leaves | Powder | top. | Dry skin, fatigue | 18 | 0.107 | 8 | 0.44 | 50 | R |
| Verbenaceae | Vitex negundo L. Marwandy B.Sul.123.UOP | W | S | Young shoot | Juice | O | Cramps, rheumatism | 27 | 0.16 | 13 | 0.48 | 59.25 | I |
| Violaceae | Viola canescens Wall. Banafsh /B.Sul.120.UOP | W | H | Leaves, rhizome | Poultice | top. | Arthritis, wound healing | 34 | 0.202 | 17 | 0.5 | 67.64 | V |
| Viola odorata L. Banafsha B.Sul.121.UOP | W | H | Leaves | Decoction | O, top. | Emphysema, itchy throat | 31 | 0.184 | 16 | 0.51 | 64.51 | V | |
| Viola serpens L. Boote B.Sul.122.UOP | W | H | Root | Juice | O | Jaundice, wound | 37 | 0.22 | 18 | 0.48 | 62.16 | E | |
| Zygophyllaceae | Tribulus terrestris L. Markundy B.Sul.117.UOP | W | H | Leaves | Juice | O | Tuberculosis, Sore throat | 13 | 0.077 | 6 | 0.46 | 53.84 | R |
| Gymnosperm | |||||||||||||
| Pinaceae | Cedrus deodara (Roxb.) G.Don/Ranzro/B.Sul.048.UOP | W | T | Oil, gum | Direct | O | Refrigerant, anti septic, antipyretic | 20 | 0.119 | 10 | 0.5 | 70 | E |
| Pinus roxburghii Sarg. Nakhtar B.Sul.092.UOP | C | T | Bark, resin | Direct, decoction | O, top. | Antipyretic, urinary diseases, wound healing | 17 | 0.101 | 7 | 0.41 | 64.70 | --- | |
| Pinus wallichiana A.B. Jacks. Pewoch B.Sul.093.UOP | W | T | Resin, seeds | Direct | top. | Antipyretic, pimples | 13 | 0.077 | 5 | 0.38 | 53.84 | I | |
| Fungi | |||||||||||||
| Agaricaceae | Agaricus campestris L. Kharyray B.Sul.028.UOP | W | H | Whole plant | Decoction | O | Stimulant, Nutritive | 43 | 0.255 | 28 | 0.65 | 81.39 | V |
| Morchellaceae | Morchella deliciosa Fr. Ghuchy B.Sul.077.UOP | W | H | Whole plant | Decoction | O | Infertility, pain, anti-cholesteric | 42 | 0.25 | 23 | 0.54 | 71.42 | E |
| Morchella esculenta Fr. Ghuchy B.Sul.078.UOP | W | H | Whole plant | Decoction | O | Tonic, infertility | 46 | 0.273 | 40 | 0.86 | 100 | V | |
| Ailments Category | Nur. | % of Use Reports | Nt. | % of Species | Nur-Nt. | Nur-1 | FCI |
|---|---|---|---|---|---|---|---|
| Gastro-intestinal disorder | 137 | 18.792 | 75 | 68.8 | 62 | 136 | 0.45 |
| Respiratory disorders | 110 | 15.089 | 62 | 56.88 | 48 | 109 | 0.44 |
| Glandular disorders | 104 | 14.266 | 58 | 53.21 | 46 | 103 | 0.44 |
| Cardiovascular disorders | 82 | 11.248 | 47 | 43.11 | 35 | 81 | 0.43 |
| Analgesic, Antipyretic and Refrigerant | 51 | 6.995 | 35 | 32.11 | 16 | 50 | 0.32 |
| Dermatological disorders | 40 | 5.486 | 32 | 29.35 | 8 | 39 | 0.20 |
| Hepatic disorders | 33 | 4.526 | 27 | 24.77 | 6 | 32 | 0.18 |
| Body energizers | 30 | 4.115 | 26 | 23.85 | 4 | 29 | 0.13 |
| Urologic disorders | 27 | 3.703 | 22 | 20.18 | 5 | 26 | 0.19 |
| Nervous disorders | 25 | 3.429 | 20 | 18.34 | 5 | 24 | 0.20 |
| Muscles and Skeletal disorders | 22 | 3.017 | 19 | 17.43 | 3 | 21 | 0.14 |
| Cancer | 21 | 2.88 | 21 | 19.26 | 0 | 20 | 0.00 |
| Ophthalmic disorders | 19 | 2.606 | 17 | 15.59 | 2 | 18 | 0.11 |
| Sexual diseases | 17 | 2.331 | 16 | 14.67 | 1 | 16 | 0.06 |
| Acoustic disorders | 11 | 1.508 | 10 | 9.17 | 1 | 10 | 0.10 |
| Mean FCI | - | - | - | - | - | - | 0.226 |
| Family | No. of Genera | % of Etycontribution | No. of Species | % of Contribution | FIV |
|---|---|---|---|---|---|
| Asteraceae | 6 | 6.38 | 6 | 5.50 | 82.73 |
| Rosaceae | 4 | 4.25 | 5 | 4.58 | 82.14 |
| Lamiaceae | 3 | 3.19 | 5 | 4.58 | 95.23 |
| Moraceae | 3 | 3.19 | 5 | 4.58 | 78.57 |
| Solanaceae | 3 | 3.19 | 4 | 3.66 | 93.45 |
| Fabaceae | 3 | 3.19 | 3 | 2.75 | 64.87 |
| Pinaceae | 2 | 2.12 | 3 | 2.75 | 29.76 |
| Euphorbiaceae | 2 | 2.12 | 3 | 2.75 | 41.07 |
| Rhamnaceae | 2 | 2.12 | 3 | 2.75 | 58.92 |
| Violaceae | 1 | 1.06 | 3 | 2.75 | 60.71 |
| Amaranthaceae | 2 | 2.12 | 2 | 1.83 | 16.07 |
| Amaryllidaceae | 2 | 2.12 | 2 | 1.83 | 33.92 |
| Apocynaceae | 2 | 2.12 | 2 | 1.83 | 34.52 |
| Brassicaceae | 2 | 2.12 | 2 | 1.83 | 35.11 |
| Cannabaceae | 2 | 2.12 | 2 | 1.83 | 42.26 |
| Convolvulaceae | 2 | 2.12 | 2 | 1.83 | 13.69 |
| Ericaceae | 2 | 2.12 | 2 | 1.83 | 33.92 |
| Meliaceae | 2 | 2.12 | 2 | 1.83 | 36.9 |
| Myrsinaceae | 2 | 2.12 | 2 | 1.83 | 27.97 |
| Poaceae | 2 | 2.12 | 2 | 1.83 | 16.66 |
| Sapindaceae | 2 | 2.12 | 2 | 1.83 | 49.4 |
| Asparagaceae | 1 | 1.06 | 2 | 1.83 | 25 |
| Morchellaceae | 1 | 1.06 | 2 | 1.83 | 52.38 |
| Polygonaceae | 1 | 1.06 | 2 | 1.83 | 40.47 |
| Pteridaceae | 1 | 1.06 | 2 | 1.83 | 32.73 |
| Acanthaceae | 1 | 1.06 | 1 | 0.91 | 17.85 |
| Acoraceae | 1 | 1.06 | 1 | 0.91 | 5.95 |
| Agaricaceae | 1 | 1.06 | 1 | 0.91 | 25.59 |
| Anacardiaceae | 1 | 1.06 | 1 | 0.91 | 25.59 |
| Apiaceae | 1 | 1.06 | 1 | 0.91 | 16.66 |
| Araliaceae | 1 | 1.06 | 1 | 0.91 | 20.83 |
| Asclepiadaceae | 1 | 1.06 | 1 | 0.91 | 12.5 |
| Asphodelaceae | 1 | 1.06 | 1 | 0.91 | 22.61 |
| Berberidaceae | 1 | 1.06 | 1 | 0.91 | 26.78 |
| Boraginaceae | 1 | 1.06 | 1 | 0.91 | 22.61 |
| Buxaceae | 1 | 1.06 | 1 | 0.91 | 23.21 |
| Cactaceae | 1 | 1.06 | 1 | 0.91 | 23.8 |
| Caesalpiniaceae | 1 | 1.06 | 1 | 0.91 | 25 |
| Caryophyllaceae | 1 | 1.06 | 1 | 0.91 | 19.04 |
| Celastraceae | 1 | 1.06 | 1 | 0.91 | 16.66 |
| Chenopodiaceae | 1 | 1.06 | 1 | 0.91 | 11.3 |
| Dryopteridaceae | 1 | 1.06 | 1 | 0.91 | 25.59 |
| Equisetaceae | 1 | 1.06 | 1 | 0.91 | 15.47 |
| Fagaceae | 1 | 1.06 | 1 | 0.91 | 23.8 |
| Fumariaceae | 1 | 1.06 | 1 | 0.91 | 24.4 |
| Juglandaceae | 1 | 1.06 | 1 | 0.91 | 19.04 |
| Menispermaceae | 1 | 1.06 | 1 | 0.91 | 22.61 |
| Nitrariaceae | 1 | 1.06 | 1 | 0.91 | 23.80 |
| Nyctaginaceae | 1 | 1.06 | 1 | 0.91 | 26.78 |
| Oleaceae | 1 | 1.06 | 1 | 0.91 | 23.8 |
| Oxalidaceae | 1 | 1.06 | 1 | 0.91 | 27.97 |
| Papaveraceae | 1 | 1.06 | 1 | 0.91 | 22.02 |
| Phyllanthaceae | 1 | 1.06 | 1 | 0.91 | 24.4 |
| Platanaceae | 1 | 1.06 | 1 | 0.91 | 13.69 |
| Portulacaceae | 1 | 1.06 | 1 | 0.91 | 17.26 |
| Ranunculaceae | 1 | 1.06 | 1 | 0.91 | 26.19 |
| Rutaceae | 1 | 1.06 | 1 | 0.91 | 27.38 |
| Scrophulariaceae | 1 | 1.06 | 1 | 0.91 | 9.52 |
| Simaroubaceae | 1 | 1.06 | 1 | 0.91 | 24.4 |
| Tamaricaceae | 1 | 1.06 | 1 | 0.91 | 16.66 |
| Taxaceae | 1 | 1.06 | 1 | 0.91 | 18.45 |
| Urticaceae | 1 | 1.06 | 1 | 0.91 | 10.71 |
| Verbenaceae | 1 | 1.06 | 1 | 0.91 | 16.07 |
| Zygophyllaceae | 1 | 1.06 | 1 | 0.91 | 7.73 |
| Total | 94 | 100 | 109 | 100 | - |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sulaiman; Shah, S.; Khan, S.; Bussmann, R.W.; Ali, M.; Hussain, D.; Hussain, W. Quantitative Ethnobotanical Study of Indigenous Knowledge on Medicinal Plants Used by the Tribal Communities of Gokand Valley, District Buner, Khyber Pakhtunkhwa, Pakistan. Plants 2020, 9, 1001. https://doi.org/10.3390/plants9081001
Sulaiman, Shah S, Khan S, Bussmann RW, Ali M, Hussain D, Hussain W. Quantitative Ethnobotanical Study of Indigenous Knowledge on Medicinal Plants Used by the Tribal Communities of Gokand Valley, District Buner, Khyber Pakhtunkhwa, Pakistan. Plants. 2020; 9(8):1001. https://doi.org/10.3390/plants9081001
Chicago/Turabian StyleSulaiman, Sikandar Shah, Sheharyar Khan, Rainer W. Bussmann, Maroof Ali, Dildar Hussain, and Wahid Hussain. 2020. "Quantitative Ethnobotanical Study of Indigenous Knowledge on Medicinal Plants Used by the Tribal Communities of Gokand Valley, District Buner, Khyber Pakhtunkhwa, Pakistan" Plants 9, no. 8: 1001. https://doi.org/10.3390/plants9081001
APA StyleSulaiman, Shah, S., Khan, S., Bussmann, R. W., Ali, M., Hussain, D., & Hussain, W. (2020). Quantitative Ethnobotanical Study of Indigenous Knowledge on Medicinal Plants Used by the Tribal Communities of Gokand Valley, District Buner, Khyber Pakhtunkhwa, Pakistan. Plants, 9(8), 1001. https://doi.org/10.3390/plants9081001