Potential Toxicity of Medicinal Plants Inventoried in Northeastern Morocco: An Ethnobotanical Approach
Abstract
1. Introduction
2. Results and Discussion
2.1. Demographic Profile of the Informants
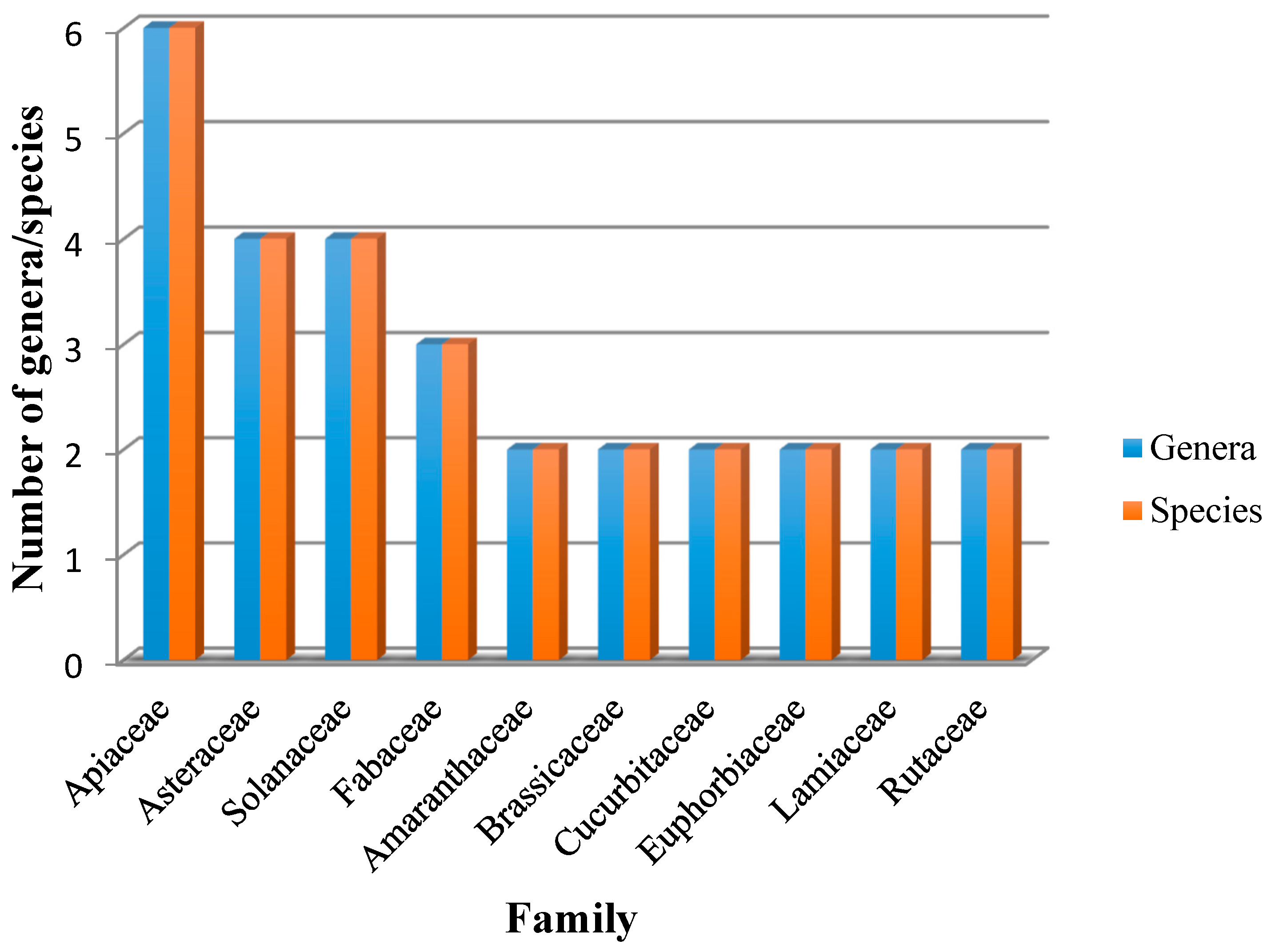
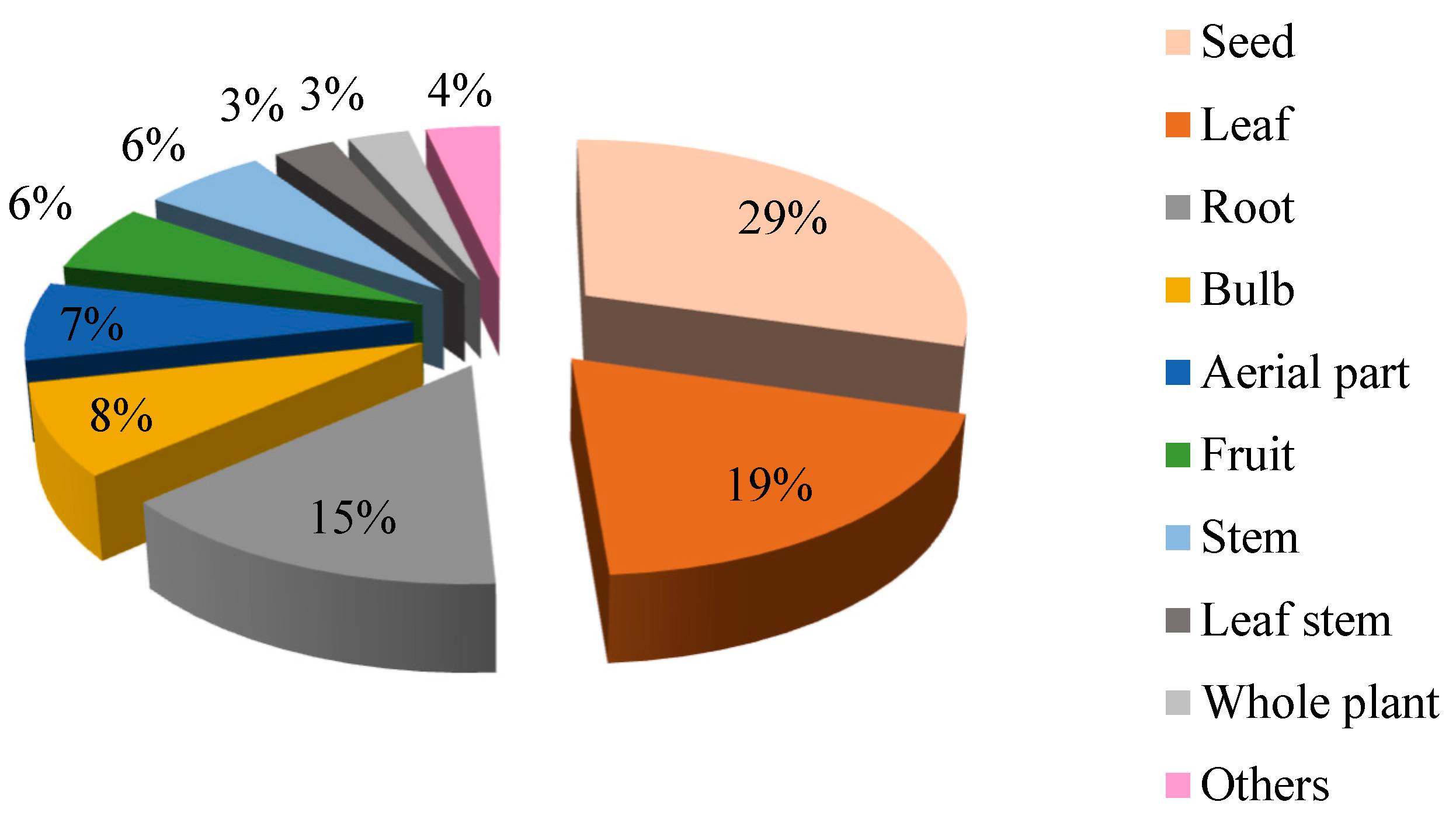
2.2. Floristic Characteristics of Poisonous Plants
2.3. Traditional Knowledge of Poisonous Herbs
2.4. Quantitative Analysis of Data
2.4.1. Informant Consensus Factor (ICF)
2.4.2. Fidelity Level (FL)
- -
- Concerning the death category, the most important species were Solanum sodomaeum L. (Fl = 100%), Nerium oleander L. (Fl = 77.14%), and Citrullus colocynthis (L.) Schrad. (Fl = 66%).
- -
- For the digestive category, Mentha spicata L. (Fl = 100%), Arisarum vulgare O. Targ. Tozz. (Fl = 100%), Morus alba L. (Fl = 100%), Viscum album L. (Fl = 100%), and Ruta montana (L.) L. (Fl = 80%).
- -
- The most common plants in the cardiovascular category were Petroselinum crispum (Mill.) Fuss (Fl = 100%), Citrus x aurantium L. (Fl = 80%), and Salvia officinalis L. (Fl = 80%).
- -
- For the neurological category, the plant with the highest Fl (100%) were Ephedra altissima Desf., Papaver somniferum L., Datura stramonium L., and Anastatica hierochuntica L.
- -
- Crocus sativus L. was reported with Fl of 100% for the general and unspecified category.
- -
- For the skin category, we found Urtica dioica L. (Fl = 87.5%) was the most important.
- -
- For the female genital category, Glycine max (L.) Merr. (Fl = 50%) was the most important.
- -
- Peganum harmala L. and Cannabis sativa L. for the digestive category;
- -
- Nerium oleander L. for the cardiovascular and eye categories;
- -
- Glycine max (L.) Merr. for the neurological category;
- -
- Peganum harmala L. for the female genital category;
- -
- Allium sativum L. for the skin category;
- -
- Carlina gummifera (L.) Less. and Cannabis sativa L. for the respiratory category; and
- -
- Trigonella foenum-graecum L. for endocrine, metabolic and nutritional, blood, blood forming organs, and immune mechanism.
3. Materials and Methods
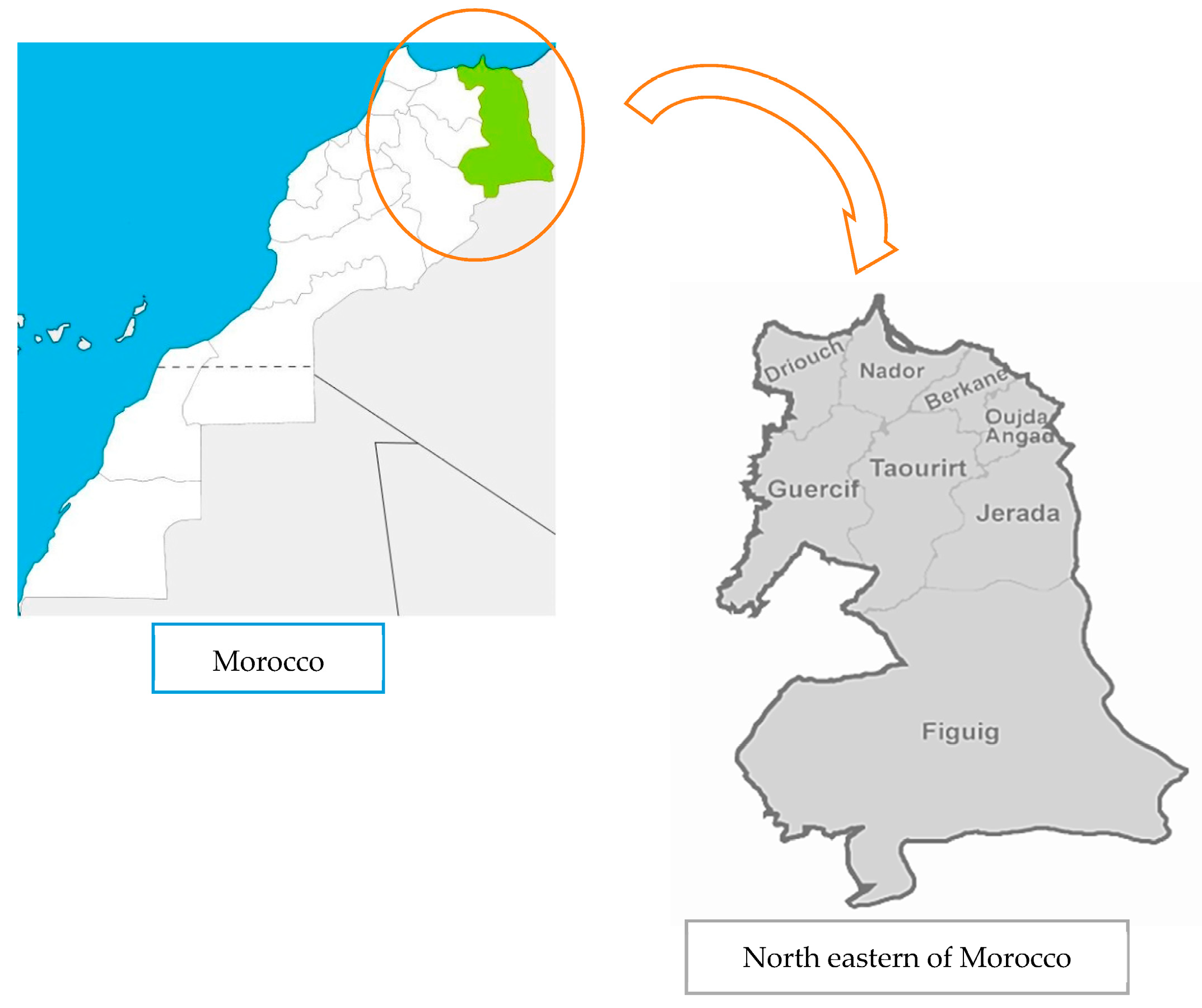
3.1. Study Area
3.2. Ethnobotanical Data Collection
3.3. Plant Collection and Identification
3.4. Analysis of Ethnomedicinal Data
3.4.1. Informant Consensus Factor (ICF)
3.4.2. Fidelity level (FL)
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Perrino, E.V.; Valerio, F.; Gannouchi, A.; Trani, A. Ecological and Plant Community Implication on Essential Oils Composition in Useful Wild Officinal Species: A Pilot Case Study in Apulia (Italy). Plants 2021, 10, 574. [Google Scholar] [CrossRef]
- Singh, B.; Singh, B.; Kishor, A.; Singh, S.; Bhat, M.N.; Surmal, O.; Musarella, C.M. Exploring Plant-Based Ethnomedicine and Quantitative Ethnopharmacology: Medicinal Plants Utilized by the Population of Jasrota Hill in Western Himalaya. Sustainability 2020, 12, 7526. [Google Scholar] [CrossRef]
- Aziz, M.A.; Ullah, Z.; Pieroni, A. Wild Food Plant Gathering among Kalasha, Yidgha, Nuristani and Khowar Speakers in Chitral, NW Pakistan. Sustainability 2020, 12, 9176. [Google Scholar] [CrossRef]
- Omwenga, E.O.; Hensel, A.; Shitandi, A.; Goycoolea, F.M. Ethnobotanical Survey of Traditionally Used Medicinal Plants for Infections of Skin, Gastrointestinal Tract, Urinary Tract and the Oral Cavity in Borabu Sub-County, Nyamira County, Kenya. J. Ethnopharmacol. 2015, 176, 508–514. [Google Scholar] [CrossRef] [PubMed]
- El-hilaly, J.; Hmammouchi, M.; Lyoussi, B. Ethnobotanical Studies and Economic Evaluation of Medicinal Plants in Taounate Province (Northern Morocco). J. Ethnopharmacol. 2003, 86, 149–158. [Google Scholar] [CrossRef]
- Tahraoui, A.; El-hilaly, J.; Israili, Z.H.; Lyoussi, B. Ethnopharmacological Survey of Plants Used in the Traditional Treatment of Hypertension and Diabetes in South-Eastern Morocco (Errachidia Province). J. Ethnopharmacol. 2007, 110, 105–117. [Google Scholar] [CrossRef]
- Eddouks, M.; Maghrani, M.; Lemhadri, A.; Ouahidi, M.; Jouad, H. Ethnopharmacological Survey of Medicinal Plants Used for the Treatment of Diabetes Mellitus, Hypertension and Cardiac Diseases in the South-East Region of Morocco (Tafilalet). J. Ethnopharmacol. 2002, 82, 97–103. [Google Scholar] [CrossRef]
- Bellakhdar, J.; Claisse, R.; Fleurentin, J.; Younos, C. Repertory of Standard Herbal Drugs in the Moroccan Pharmacopoea. J. Ethnopharmacol. 1991, 35, 123–143. [Google Scholar] [CrossRef]
- Alami Merrouni, I.; Elachouri, M. Anticancer Medicinal Plants Used by Moroccan People: Ethnobotanical, Preclinical, Phytochemical and Clinical Evidence. J. Ethnopharmacol. 2021, 266, 113435. [Google Scholar] [CrossRef]
- Fakchich, J.; Elachouri, M. Ethnobotanical Survey of Medicinal Plants Used by People in Oriental Morocco to Manage Various Ailments. J. Ethnopharmacol. 2014, 154, 76–87. [Google Scholar]
- Ziyyat, A.; Legssyer, A.; Mekhfi, H.; Dassouli, A.; Serhrouchni, M. Phytotherapy of Hypertension and Diabetes in Oriental Morocco. J. Ethnopharmacol. 1997, 58, 45–54. [Google Scholar] [CrossRef]
- Mordeniz, C. Integration of Traditional and Complementary Medicine into Evidence-Based Clinical Practice. In Traditional and Complementary Medicine; IntechOpen: London, UK, 2019; pp. 1–8. [Google Scholar]
- Kharchoufa, L.; Bouhrim, M.; Bencheikh, N.; El Assri, S.; Amirou, A.; Yamani, A.; Choukri, M.; Mekhfi, H.; Elachouri, M. Acute and subacute toxicity studies of the aqueous extract from Haloxylon scoparium pomel (Hammada scoparia (pomel)) by oral administration in Rodents. BioMed Res. Int. 2020. [Google Scholar] [CrossRef] [PubMed]
- Ekor, M. The Growing Use of Herbal Medicines: Issues Relating to Adverse Reactions and Challenges in Monitoring Safety. Front. Neurol. 2014, 4, 177. [Google Scholar] [CrossRef] [PubMed]
- Kharchoufa, L.; Merrouni, I.A.; Yamani, A.; Elachouri, M. Profile on Medicinal Plants Used by the People of North Eastern Morocco: Toxicity Concerns. Toxicon 2018, 154, 90–113. [Google Scholar] [CrossRef] [PubMed]
- Najem, M.; Daoudi, A.; Bouiamrine, E.H.; Ibijbijen, J.; Nassiri, L. Biodiversity of Poisonous Medicinal Plants Solicited in the Traditional Phytotherapy of the Central Middle Atlas -Morocco. Ethnobot. Res. Appl. 2019, 18, 1–22. [Google Scholar] [CrossRef]
- Bhatia, H.; Manhas, R.K.; Kumar, K.; Magotra, R. Traditional Knowledge on Poisonous Plants of Udhampur District of Jammu and Kashmir, India. J. Ethnopharmacol. 2014, 152, 207–216. [Google Scholar] [CrossRef]
- Yahyaoui, O.; El Ouaaziz, N.A.; Sammama, A.; Kerrouri, S.; Bouabid, B.; Lrhorfi, L.A.; Zidane, L.; Bengueddour, R. Etude Ethnobotanique: Plantes Médicinales Commercialisées à La Province de Laâyoune; Identification et Utilisation. Int. J. Innov. Appl. Stud. 2015, 12, 533–541. [Google Scholar]
- Musa, M.S.; Abdelrasool, F.E.; Elsheikh, E.A.; Ahmed, L.A.M.N.; Mahmoud, A.L.E.; Yagi, S.M. Ethnobotanical Study of Medicinal Plants in the Blue Nile State, South-Eastern Sudan. J. Med. Plants Res. 2011, 5, 4287–4297. [Google Scholar]
- Eddouks, M.; Ajebli, M.; Hebi, M. Ethnopharmacological Survey of Medicinal Plants Used in Daraa-Tafilalet Region (Province of Errachidia), Morocco. J. Ethnopharmacol. 2017, 198, 516–530. [Google Scholar] [CrossRef] [PubMed]
- Barkaoui, M.; Katiri, A.; Boubaker, H.; Msanda, F. Ethnobotanical Survey of Medicinal Plants Used in the Traditional Treatment of Diabetes in Chtouka Ait Baha and Tiznit (Western Anti-Atlas), Morocco. J. Ethnopharmacol. 2017, 198, 338–350. [Google Scholar] [CrossRef]
- Mechchate, H.; Es-safi, I.; Jawhari, F.z.; Bari, A.; Grafov, A.; Bousta, D. Ethnobotanical Survey about the Management of Diabetes with Medicinal Plants Used by Diabetic Patient in Region of Fez-Meknes, Morocco. Ethnobot. Res. Appl. 2020, 19. [Google Scholar] [CrossRef]
- Rodríguez, J.F.; López, A.V.; Núñez, D.R.; Franzi, A.V.; Castro, C.O. De Investigación y Divulgación Del Conocimiento Etnobiológico En Castilla-La Mancha. Sabuco Rev. Estud. Albacet. 2008, 6, 137–156. [Google Scholar]
- Bellakhdar, J. La Pharmacopee Marocaine Traditionnelle: Medecine Arabe Ancienne et Savoirs Populaires; IBIS Press: Newburyport, MA, USA, 1997. [Google Scholar]
- Thomas, E.; Vandebroek, I.; Sanca, S.; Van Damme, P. Cultural Significance of Medicinal Plant Families and Species among Quechua Farmers in Apillapampa, Bolivia. J. Ethnopharmacol. 2009, 122, 60–67. [Google Scholar] [CrossRef]
- Huai, H.; Dong, Q.; Liu, A. Ethnomedicinal Analysis of Toxic Plants from Five Ethnic Groups in China. Ethnobot. Res. Appl. 2010, 8, 169–179. [Google Scholar] [CrossRef]
- Pomilio, A.B.; Falzoni, E.M.; Vitale, A.A. Toxic Chemical Compounds of the Solanaceae. Nat. Prod. Commun. 2008, 3, 593–628. [Google Scholar] [CrossRef]
- Al-qura, S. Ethnobotanical Survey of Folk Toxic Plants in Southern Part of Jordan. Toxicon 2005, 46, 119–129. [Google Scholar] [CrossRef]
- Bnouham, M.; Zahra Merhfour, F.; Elachoui, M.; Legssyer, A.; Mekhfi, H.; Lamnaouer, D.; Ziyyat, A. Toxic Effects of Some Medicinal Plants Used in Moroccan Traditional Medicine. Moroc. J. Biol. 2006, 23, 21–30. [Google Scholar]
- Yamani, A.; Bunel, V.; Antoine, M.; Husson, C.; Stévigny, C.; Duez, P.; Elachouri, M.; Nortier, J. Substitution between Aristolochia and Bryonia Genus in North-Eastern Morocco: Toxicological Implications. J. Ethnopharmacol. 2015, 166, 250–260. [Google Scholar] [CrossRef]
- Audi, J.; Belson, M.; Patel, M.; Schier, J.; Osterloh, J. Ricin Poisoning. JAMA 2005, 294, 2342–2351. [Google Scholar] [CrossRef]
- WHO. International Classification of Primary Care, Second Edition (ICPC-2). Available online: https://www.who.int/classifications/icd/adaptations/icpc2/en/ (accessed on 15 January 2020).
- RGPH. Recensement Général de La Population et de l’Habitat Au. 2014. Available online: https://www.rgph2014.hcp.ma (accessed on 25 November 2020).
- Fennane, M.; Ibn Tatou, M.; Mathez, J.; Ouyahya, A.; El Oualidi, J. Flore Pratique Du Maroc. Manuel de Determination Des Plantes Vasculaires. Vol 1. Ptéridophyta, Gymnospermae, Angiospermae(Lauraceae, Neuradaceae); Travaux de l’institut Scientifique Série Botanique: Rabat, Morocco, 1999. [Google Scholar]
- Fennane, M.; Ibn Tattou, M.; Ouyahya, A.; El Oualidi, J. Flore Pratique Du Maroc. Manuel de Determination Des Plantes Vasculaires. Vol. 2–Angiospermae (Leguminosae-Lentibulariaceae); Travaux de l’institut Scientifique Série Botanique: Rabat, Morocco, 2007. [Google Scholar]
- Fennane, M.; Tattou, M.I.; Ouyahya, A.; El Oualidi, J. Flore Pratique Du Maroc. Manuel de Determination Des Plantes Vasculaires. Vol. 3–Dicotylédones (p.p),Monocotylédones; Travaux de l’institut Scientifique Série Botanique: Rabat, Morocco, 2014. [Google Scholar]
- The Plant Lis. Available online: thttp://www.theplantlist.org/ (accessed on 11 December 2020).
- Heinrich, M.; Ankli, A.; Frei, B.; Weimann, C.; Sticher, O. Medicinal Plants in Mexico: Healers’ Consensus and Cultural Importance. Soc. Sci. Med. 1998, 47, 1859–1871. [Google Scholar] [CrossRef]
- Gazzaneo, L.R.S.; de Lucena, R.F.P.; de Albuquerque, U.P. Knowledge and Use of Medicinal Plants by Local Specialists in an Region of Atlantic Forest in the State of Pernambuco (Northeastern Brazil). J. Ethnobiol. Ethnomed. 2005, 1, 1–8. [Google Scholar] [CrossRef]
- Srithi, K.; Balslev, H.; Wangpakapattanawong, P.; Srisanga, P.; Trisonthi, C. Medicinal Plant Knowledge and Its Erosion among the Mien (Yao) in Northern Thailand. J. Ethnopharmacol. 2009, 123, 335–342. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.; Manhas, R.K.; Magotra, R. Ethnoveterinary Remedies of Diseases among Milk Yielding Animals in Kathua, Jammu and Kashmir, India. J. Ethnopharmacol. 2012, 141, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Friedman, J.; Yaniv, Z.; Dafnib, A.; Palewitcha, D. A Preliminary Classification of the Healing Potential of Medicinal Plants, Based on a Rational Analysis of an Ethnopharmacological Field Survey among Bedouins in the Negev Desert, Israel. J. Ethnopharmacol. 1986, 16, 275–287. [Google Scholar] [CrossRef]
| Socio-Demographic Variables | Sample | |
|---|---|---|
| Number | Percentage (%) | |
| District | ||
| Oujda | 161 | 41.70 |
| Berkane | 137 | 32.90 |
| Jerada | 88 | 25.38 |
| Function | ||
| Ordinary inhabitant | 345 | 89.37 |
| Herbalists | 41 | 10.63 |
| Habitat | ||
| Urban | 154 | 39.89 |
| Rural | 232 | 60.10 |
| Age (Years) | ||
| <30 | 56 | 14.50 |
| 30–60 | 241 | 62.43 |
| 60–80 | 74 | 19.17 |
| >80 | 15 | 3.88 |
| Gender | ||
| Male | 125 | 32.38 |
| Female | 261 | 67.61 |
| Study Level | ||
| Illiterate | 166 | 43 |
| Primary | 99 | 25.64 |
| High school | 56 | 14.50 |
| University | 65 | 16.83 |
| Family Scientific Name | Local Name | Herbaceous Life Form/Voucher Number | Rout of Administration | Traditional Uses | Poisonous Part | Toxic Signs | NC |
|---|---|---|---|---|---|---|---|
| Amaranthaceae | |||||||
| Dysphania ambrosioides (L.) Mosyakin & Clemants | Mkhinza | Herb/HUMPOM571 | Internal and external uses | Headache, migraine, fever | Leaf Aerial part | Madness, dizziness, death (oral), gallbladder toxicity | 7 |
| Haloxylon scoparium Pomel | Ramt | Herb/HUMPOM572 | Internal uses | Diabetes, scorpion bite | Aerial part | Vomiting, abdominal pain, pain general | 3 |
| Amarillydaceae | |||||||
| Allium sativum L. | Thouma | Herb/HUMPOM573 | Food, cold, hypertension, asthma, cough, dental pain, ear pain, digestive, antibiotic, weight loss, hair strengthening, immunity, eczema, influenza, hemorrhoids, gum disease | Bulb | Hypotension, stomach-ache, allergy, nephrotoxicity, stomach burning | 22 | |
| Anacardiaceae | |||||||
| Pistacia lentiscus L. | Dro/meska | Tree/HUMPOM574 | Internal uses | Uterus cancer, diabetes, gastro-intestinal disorders | Leaf, fruit | Constipation, skin irritation | 2 |
| Apiaceae | |||||||
| Conium maculatum L. | Ziyyata | Herb/HUMPOM575 | Internal uses | Cold | Fruit, seed | Neurological problems, abdominal pain, vomiting | 4 |
| Coriandrum sativum L. | Kosbare, Kessbour | Herb/HUM-POM576 | Internal and external uses | Food, mouth ulcers, frequent urination | Leaf, seeds, leafy stem | Forgetting, sleep, dizziness, neurological problems, allergy | 5 |
| Ferula communis L. | Kelkha L-klekh Fasoukh | Herb/HUMPOM577 | Internal and external uses | Cold, food, magic, anthelmintic, female sterility. | Stem, resin | Abortion, irritation, death, pain general, neurological toxicity | 7 |
| Foeniculum vulgare Mill. | Bassbass | Herb/HUMPOM578 | Internal and external uses | Abdominal pain, intestine, maternal milk. | Seed | Dizziness, hypotension, facial pills | 3 |
| Petroselinum crispum (Mill.) Fuss | Maâdnousse | Herb/HUMPOM579 | Internal and external uses | Food, hypertension, hair | Leaf | Hypotension | 2 |
| Thapsia garganica L. | Deryas | Herb/HUMPOM580 | Internal uses | Antispasmodic, rheumatism, women sterility, cough | Root | Abortion (animal), vomiting and diarrhea | 4 |
| Apocynaceae | |||||||
| Nerium oleander L. | Dafla | Shrub/HUMPOM581 | External uses | Stop nose bleeds, tonsillitis, swollen gums, cold, headache, teeth, rheumatism, sedative, mumps, influenza, jaundice, ear infections, mouth-ulcers, diabetes, torticollis, irritable bowel syndrome, skin problems | Whole plant | Death (oral), increased heart rate and irregularity, toxic to eyes, abdominal, pain, stomachache, digestive system disorders | 35 |
| Araceae | |||||||
| Arisarum vulgare O. Targ. Tozz. | Tabgouga | Herb/HUMPOM582 | External and internal uses | Emetic, purgative, dermatological problems | Tuber | Mouth inflammation, intestinal pain, vomiting, hepatotoxicity | 2 |
| Araliaceae | |||||||
| Hedera helix L. | Louwaya | Shrub/HUMPOM583 | External uses | Rheumatism, skin abscesses | Leaf, fruit | Death (oral) | 2 |
| Aristolochiaceae | |||||||
| Aristolochia fontanesii Boiss. & Reut. | Baraztem | Shrub/HUMPOM584 | External and internal uses | Cancer, skin infection, intestinal parasites, diabetes | Root, whole plant | Nephrotoxicity, hepatotoxicity, vomiting, dizziness, indigestion, death | 15 |
| Asparagaceae | |||||||
| Drimia maritima (L.) Stearn | Bes’al ed-dib Bassila | Herb/HUMPOM585 | External and internal uses | Detoxification, dental pain, abdominal pain | Bulb | Diarrhea, death, dizziness, nausea, vomiting | 6 |
| Asteraceae | |||||||
| Carlina gummifera (L.) Less. | Addad | Herb/HUMPOM586 | External and internal uses | Headache, respiratory system, sterility, rheumatism, skin diseases, mouth pain, freckles on the face, whiten the teeth, facilitates childbirth, hair loss. | Root | Vomiting, diarrhea, swilling, death, digestive disorders | 25 |
| Warionia saharae Benth. & Coss. | Affessass | Herb/HUMPOM587 | External and internal uses | Softens and strengthens hair, Gastroenteritis | Leafy stem | Nephrotoxicity | 2 |
| Artemisia arborescens (Vaill.) L. | Chiba | Herb/HUMPOM588 | External and internal uses | Hypoglycemic, otitis | Aerial part | Diarrhea, dizziness, convulsion | 2 |
| Launaea arborescens (Batt.) Murb. | Mmû-lbeyna | Shrub HUMPOM589 | Internal uses | Hypoglycemic, respiratory problems | Latex | Death | 2 |
| Boraginaceae | |||||||
| Borago officinalis L. | Lsan tawr El hricha | Herb/HUMPOM590 | External uses | Knee pains | Root | Death (oral) | 2 |
| Brassicaceae | |||||||
| Anastatica hierochuntica L. | Lkmicha, Keff-maryam, Tamkelt | Herb/HUMPOM591 | Internal uses | Strengthen the uterus | Leafy stem | Neurological disorders, sleep disturbance | 2 |
| Brassicaceae | |||||||
| Lepidium sativum L. | Hab rachad | Herb/HUMPOM592 | Internal and external uses | Hair, anemia, cough, intestinal gas, strengthen hair, regulates the menstrual cycle, maternal milk | Seed | Indigestion, diuresis, abortion, dizziness hepatotoxicity, hypertension | 8 |
| Cannabaceae | |||||||
| Cannabis sativa L. | Lkif | Herb/HUMPOM593 | External uses | Hair loss, hair lengthening and thickening, against dandruff, strengthen hair, calming | Leaf, seed | Ecstasy, hepatotoxicity madness, sedation, neurological toxicity, respiratory problems, dizziness, lose consciousness, neurological toxicity, death | 26 |
| Caryophyllaceae | |||||||
| Herniaria cinerea DC. | Harasst lahjar | Herb/HUMPOM594 | Internal uses | Kidney stones | Aerial part | Hypertension | 2 |
| Cucurbitaceae | |||||||
| Bryonia cretica subsp. dioica (Jacq.) Tutin | Aneb dib | Herb/HUMPOM595 | Internal and external uses | Hair loss, urinary tract infection | Whole plant | Harmful to pregnant woman, toxic for people with stomach diseases | 2 |
| Citrullus colocynthis (L.) Schrad. | H’adej Handa’al | Herb/HUMPOM596 | Internal and external uses | Cancer, diabetes, detoxification, diuretic | Fruit | Death (high doses), abortion, diarrhea vomiting | 9 |
| Cupressaceae | |||||||
| Tetraclinis articulata (Vahl) Mast. | Ar-âr | Tree/HUMPOM597 | Internal and external uses | Colds, headache, skin diseases | Leaf | Neurotoxicity | 2 |
| Ephedraceae | |||||||
| Ephedra altissima Desf. | Laâlenda | Shrub/HUMPOM598 | Internal uses | Cancer | Aerial part | Dizziness | 3 |
| Euphorbiaceae | |||||||
| Euphorbia resinifera O. Berg | Takiwt Takawt | Shrub/HUMPOM599 | Internal and external uses | Hair care, diabetes | Seed | Death | 2 |
| Fabaceae | |||||||
| Glycine max (L.) Merr. | Soja | Herb/HUMPOM600 Shrub/ | Internal uses | To weight gain, against menopause, appetite increases female hormones, hypertension colon | Seed | Sterility, sedation, sleep, diarrhea, blocks absorption of nutrients (high dose), colic, nausea, constipation, hypertension | 2 |
| Retama monosperma (L.) Boiss. | Rtem | HUMPOM601 | External uses | Magic, hypoglycemia | Stem | Death (high doses), abortion | 12 |
| Trigonella foenum-graecum L. | Lhelba | Herb/HUMPOM602 | Internal uses | Anemia, appetite, weight gain, blood detoxification, digestive system, facilitate food absorption, cold, antiparasitic | Seeds | Jaundice, harmful to pregnant woman, renal pain, hypertension, gastrointestinal diseases, nausea, decreases immunity, stomachache (in high doses), abortion | 12 |
| Gentianaceae | |||||||
| Centaurium erythraea Rafn. | Gosset l-hayya, Marraret al-hench | Herb/HUMPOM603 | Internal uses | Infertility, skin diseases | Seed | Nausea and dizziness | 2 |
| Hypericaceae | |||||||
| Hypericum perforatum L. | Hachicht lkalb | Herb/HUMPOM604 | Internal and external uses | Asthma, varicose veins | Flower | Death, nephrotoxicity, dermatological problems | 4 |
| Iridaceae | |||||||
| Crocus sativus L. | Za’fran lhor | Herb/HUMPOM605 | Internal uses | Digestion, anemia, asthma, cough | Stigma | Hypotension, dry mouth, allergic reaction (flushing of the face) | 2 |
| Lamiaceae | |||||||
| Mentha spicata L. | Naana’a | Herb/HUMPOM606 | Internal and external uses | Stomachache, lose weight, heart problems, cosmetic | Leaf Aerial part | Intestinal gas, colon bloating | 8 |
| Salvia officinalis L. | Salmia | Shrub/HUMPOM607 | Internal | Diabetes, balance female hormones, painful menstrual periods, influenza, pain killer, digestive system | Aerial part Leaf | Fever, nausea | 5 |
| Molluginaceae | |||||||
| Corrigiola litoralis L. | Serghina | Herb/HUMPOM608 | External uses | Cosmetic | Root Leaf | Diarrhea (oral), abdominal pain | 2 |
| Moraceae | |||||||
| Morus alba L. | Toute | Tree/HUMPOM609 | Internal uses | Anemia, cough | Fruit | Mouth inflammation (high doses) | 2 |
| Myristicaceae | |||||||
| Myristica fragrans Houtt | Lgouza | Tree/HUMPOM610 | Internal uses | Food | Fruit | Dizziness | 2 |
| Nitrariaceae | |||||||
| Peganum harmala L. | Harmel | Herb/HUMPOM611 | Internal and external uses | Headache, cold, hair care, constipation, fever, anorexia, diarrhea, abortion, lengthening hair, arthritis, rheumatism, diabetes, magic, bad spirit, facilitation of childbirth | Seed Aerial part Leaf | Neurological disorders vomiting, abortion hepatoxicity, eye irritations, death, dizziness | 23 |
| Solanaceae | |||||||
| Solanum sodomaeum L. | Matichat lahmir | Shrub/HUMPOM612 | External uses | Rheumatism | Berries | Death | 2 |
| Papaveraceae | |||||||
| Papaver somniferum L. | Kherkhacha | Herb/HUMPOM613 | Internal uses | Calming, sedative | Fruit | Neurological disorders | 6 |
| Ranunculaceae | |||||||
| Nigella sativa L. | Sanouj | Herb/HUMPOM614 | Internal uses | Respiratory infections, cold, diabetes, digestive disease, muscle stiffness | Seed | Dizziness (high doses), irritations, hepatotoxicity | 5 |
| Rhamnaceae | |||||||
| Ziziphus lotus (L.) Lam. | Sedr-Nbeg | Shrub/HUMPOM615 | Internal uses | Digestive disease, diabetes | Root | Bladder toxicity | 2 |
| Rosaceae | |||||||
| Prunus dulcis (Mill.) D.A.Webb | Louz lmor | Tree/HUMPOM616 | Internal and external uses | Hypertension, diabetes, fever, hair care | Seed Fruit | Hypotension (>3 seeds), fever, death (high doses) | 5 |
| Rutaceae | |||||||
| Citrus x aurantium L. | Ranje | Tree/HUMPOM617 | Internal uses | Hypertension, fever, cod, diarrhea, cosmetic, increase blood flow and circulation | Fruit Leaf pulp | Hypoglycemia, abortion, cardiac problem, hypertension | 5 |
| Ruta montana (L.) L. | Fijel | Herb/HUMPOM618 | Internal and external uses | Diarrhea, headache, fever, menstrual disorders, diabetes, bad spirit | Whole plant Leaf Aerial part | Diarrhea, vomiting Digestive disorders, nervous disorder | 5 |
| Santalaceae | |||||||
| Viscum album L. | Lenjbar | Tree/HUMPOM619 | Internal uses | Diarrhea, throat disorders | Seed | Constipation Hepatotoxicity | 2 |
| Solanaceae | |||||||
| Atropa Belladonna L. | Zbib lidur | Herb/HUMPOM620 | Internal uses | Stimulant and aphrodisiac, | Berries seed | Nervous disorder, colic, gastroenteritis, death | 5 |
| Datura stramonium L. | Chdeq jmel | Herb/HUMPOM621 | Internal uses | Headache, menstrual blood, sexual stimulant, sedative | Seed | Delirium, madness, hallucination | 4 |
| Hyoscyamus albus L. | Bounarjouf | Herb/HUMPOM622 | Internal and external uses | Skin infections, eczema, sedative | Seed Aerial part | Dizziness, hallucination | 2 |
| Thymelaeaceae | |||||||
| Daphne gnidium L. | Lezzâz | Herb/HUMPOM623 | external uses | Hair hydration, hair elongation | Leaf Aerial part | Dizziness, fainting eye irritation, skin problems | 10 |
| Euphorbiaceae | |||||||
| Ricinus communis L. | Kherouaa | Tree/HUMPOM624 | Internal and external uses | Abdominal pain, constipation, cosmetic (hair and face), detoxification, eyelash strengthening | Seed (oil) | Vomiting, eye pain, death, nausea | 10 |
| Urtica dioica L. | Lhoriga | Herb/HUMPOM625 | Internal and external uses | Menstrual pain, respiratory system diabetes, rheumatism, cold, kidneys | Aerial part Leaf | skin irritation, allergy, stomachache, skin problems | 8 |
| Ailments Categories | Ailments | Number of Reports | Number of Species | Informant Consensus Factor (ICF) |
|---|---|---|---|---|
| Death | Death | 94 | 18 | 0.81 |
| Urological | Kidneys problems, diuretic, bladder diseases | 14 | 4 | 0.76 |
| Neurological | Dizziness, delirium, madness, hallucination, migraine, headache, neurotoxicity, forgetting, sedation, lose consciousness, sleep disturbance, tonic-clonic seizures | 76 | 21 | 0.73 |
| Digestive | Vomiting, diarrhea, gastroenteritis, constipation, nausea, indigestion, stomachache, bloating, intestinal gas, absorption of nutrients, abdominal pain, mouth, liver problems, bile problems, jaundice, gallbladder | 95 | 32 | 0.67 |
| Skin | Skin irritation, itchy, inflammation, skin problems | 10 | 4 | 0.66 |
| Cardiovascular | Cardiac problems, hypertension, hypotension | 31 | 12 | 0.63 |
| Eye | Eye pain, eye irritation | 8 | 4 | 0.57 |
| Female Genital | Abortion, sterility | 18 | 10 | 0.47 |
| General and Unspecified | Fever, allergy, pain general | 11 | 8 | 0.30 |
| Endocrine, Metabolic and Nutritional | Hypoglycemia | 1 | 1 | 0 |
| Respiratory | Breathing problems | 2 | 2 | 0 |
| Blood, Blood Forming Organs and Immune Mechanism | Immune | 1 | 1 | 0 |
| Category of Illness | Name of Species | Fidelity Level (Fl %) |
|---|---|---|
| Death | Solanum sodomaeum L. | 100.00% |
| Nerium oleander L. | 77.14% | |
| Citrullus colocynthis (L.) Schrad. | 66.00% | |
| Carlina gummifera (L.) Less. | 64.00% | |
| Prunus dulcis (Mill.) D.A.Webb | 60.00% | |
| Ferula communis L. | 57.14% | |
| Aristolochia fontanesii Boiss. & Reut. | 40.00% | |
| Cannabis sativa L. | 34.61% | |
| Drimia maritima (L.) Stearn | 33.33% | |
| Hypericum perforatum L. | 20.00% | |
| Peganum harmala L. | 17.39% | |
| Digestive | Mentha spicata L. | 100.00% |
| Arisarum vulgare O. Targ. Tozz. | 100.00% | |
| Morus alba L. | 100.00% | |
| Viscum album L. | 100.00% | |
| Ruta montana (L.) L. | 80.00% | |
| Thapsia garganica L. | 75.00% | |
| Haloxylon scoparium Pomel | 66.66% | |
| Artemisia arborescens (Vaill.) L. | 50.00% | |
| Bryonia cretica subsp. dioica (Jacq.) Tutin | 50.00% | |
| Pistacia lentiscus L. | 50.00% | |
| Ricinus communis L. | 50.00% | |
| Drimia maritima (L.) Stearn | 50.00% | |
| Carlina gummifera (L.) Less. | 44.00% | |
| Glycine max (L.) Merr. | 41.66% | |
| Citrullus colocynthis (L.) Schrad. | 33.00% | |
| Allium sativum L. | 31.18% | |
| Conium maculatum L. | 25.00% | |
| Trigonella foenum-graecum L. | 25.00% | |
| Aristolochia fontanesii Boiss. & Reut. | 20.00% | |
| Salvia officinalis L. | 20.00% | |
| Nigella sativa L. | 20.00% | |
| Nerium oleander L. | 17.14% | |
| Lepidium sativum L. | 12.50% | |
| Urtica dioica L. | 12.50% | |
| Peganum harmala L. | 8.69% | |
| Cannabis sativa L. | 7.69% | |
| Cardiovascular | Petroselinum crispum (Mill.) Fuss | 100.00% |
| Citrus x aurantium L. | 80.00% | |
| Salvia officinalis L. | 80.00% | |
| Allium sativum L. | 50.00% | |
| Nigella sativa L. | 20.00% | |
| Prunus dulcis (Mill.) D.A.Webb | 20.00% | |
| Trigonella foenum-graecum L. | 16.66% | |
| Lepidium sativum L. | 12.50% | |
| Nerium oleander L. | 2.85% | |
| Neurological | Ephedra altissima Desf. | 100.00% |
| Papaver somniferum L. | 100.00% | |
| Datura stramonium L. | 100.00% | |
| Anastatica hierochuntica L. | 100.00% | |
| Coriandrum sativum L. | 80.00% | |
| Conium maculatum L. | 75.00% | |
| Peganum harmala L. | 69.56% | |
| Cannabis sativa L. | 61.53% | |
| Daphne gnidium L. | 60.00% | |
| Nigella sativa L. | 60.00% | |
| Artemisia arborescens (Vaill.) L. | 50.00% | |
| Lepidium sativum L. | 37.00% | |
| Ruta montana (L.) L. | 20.00% | |
| Drimia maritima (L.) Stearn | 16.66% | |
| Ferula communis L. | 28.57% | |
| Glycine max (L.) Merr. | 8.33% | |
| Female Genitals | Glycine max (L.) Merr. | 50.00% |
| Citrus x aurantium L. | 40.00% | |
| Thapsia garganica L. | 25.00% | |
| Trigonella foenum-graecum L. | 25.00% | |
| Bryonia cretica subsp. dioica (Jacq.) Tutin | 20.00% | |
| Ferula communis L. | 14.28% | |
| Lepidium sativum L. | 12.50% | |
| Citrullus colocynthis (L.) Schrad. | 11.00% | |
| Peganum harmala L. | 8.69% | |
| Urological | Aristolochia fontanesii Boiss. & Reut. | 46.00% |
| Hypericum perforatum L. | 25.00% | |
| Trigonella foenum-graecum L. | 16.66% | |
| Lepidium sativum L. | 12.50% | |
| Allium sativum L. | 4.54% | |
| Skin | Urtica dioica L. | 87.50% |
| Pistacia lentiscus L. | 50.00% | |
| Daphne gnidium L. | 10.00% | |
| General and Unspecified | Crocus sativus L. | 100.00% |
| Haloxylon scoparium Pomel | 33.33% | |
| Coriandrum sativum L. | 20.00% | |
| Salvia officinalis L. | 20.00% | |
| Prunus dulcis (Mill.) D.A.Webb | 20.00% | |
| Ferula communis L. | 14.28% | |
| Allium sativum L. | 13.63% | |
| Eye | Daphne gnidium L. | 30.00% |
| Ricinus communis L. | 20.00% | |
| Nerium oleander L. | 2.85% | |
| Respiratory | Carlina gummifera (L.) Less. | 4.00% |
| Cannabis sativa L. | 3.84% | |
| Endocrine, Metabolic, and Nutritional | Citrus x aurantium L. | 20.00% |
| Trigonella foenum-graecum L. | 8.33% | |
| Blood, Blood Forming Organs, and Immune Mechanism | Trigonella foenum-graecum L. | 8.33% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kharchoufa, L.; Bouhrim, M.; Bencheikh, N.; Addi, M.; Hano, C.; Mechchate, H.; Elachouri, M. Potential Toxicity of Medicinal Plants Inventoried in Northeastern Morocco: An Ethnobotanical Approach. Plants 2021, 10, 1108. https://doi.org/10.3390/plants10061108
Kharchoufa L, Bouhrim M, Bencheikh N, Addi M, Hano C, Mechchate H, Elachouri M. Potential Toxicity of Medicinal Plants Inventoried in Northeastern Morocco: An Ethnobotanical Approach. Plants. 2021; 10(6):1108. https://doi.org/10.3390/plants10061108
Chicago/Turabian StyleKharchoufa, Loubna, Mohamed Bouhrim, Noureddine Bencheikh, Mohamed Addi, Christophe Hano, Hamza Mechchate, and Mostafa Elachouri. 2021. "Potential Toxicity of Medicinal Plants Inventoried in Northeastern Morocco: An Ethnobotanical Approach" Plants 10, no. 6: 1108. https://doi.org/10.3390/plants10061108
APA StyleKharchoufa, L., Bouhrim, M., Bencheikh, N., Addi, M., Hano, C., Mechchate, H., & Elachouri, M. (2021). Potential Toxicity of Medicinal Plants Inventoried in Northeastern Morocco: An Ethnobotanical Approach. Plants, 10(6), 1108. https://doi.org/10.3390/plants10061108







