Abstract
Bangladesh is a malaria endemic country. There are 13 districts in the country bordering India and Myanmar that are at risk of malaria. The majority of malaria morbidity and mortality cases are in the Chittagong Hill Tracts, the mountainous southeastern region of Bangladesh. In recent years, malaria burden has declined in the country. In this study, we reviewed and summarized published data (through 2014) on the use of geospatial technologies on malaria epidemiology in Bangladesh and outlined potential contributions of geospatial technologies for eliminating malaria in the country. We completed a literature review using “malaria, Bangladesh” search terms and found 218 articles published in peer-reviewed journals listed in PubMed. After a detailed review, 201 articles were excluded because they did not meet our inclusion criteria, 17 articles were selected for final evaluation. Published studies indicated geospatial technologies tools (Geographic Information System, Global Positioning System, and Remote Sensing) were used to determine vector-breeding sites, land cover classification, accessibility to health facility, treatment seeking behaviors, and risk mapping at the household, regional, and national levels in Bangladesh. To achieve the goal of malaria elimination in Bangladesh, we concluded that further research using geospatial technologies should be integrated into the country’s ongoing surveillance system to identify and better assess progress towards malaria elimination.
1. Introduction
Malaria is a major public health problem in many developing countries, including Bangladesh. In 2012, the official number of laboratory confirmed malaria cases in the country was 29,522 with 11 confirmed malaria deaths [1]. Thirteen million people are living in malaria risk areas in 13 of the country’s 64 administrative districts [2]. The Bangladesh National Malaria Control Program (NMCP), which is responsible for overseeing malaria control activities at the national level, has had some success in controlling malaria with a reduction in prevalence of all malaria in the country by 65% (95% CI: 65-66) between 2008 and 2012 [1,3]. Between 2008 and 2012, the NMCP, through the support of the Global Fund, implemented in the 13 endemic districts, malaria control programs, including test and treat and the distribution of long lasting insecticide-treated nets (LLINs) [1]. During this timeframe, the prevalence rate in these 13 endemic districts decreased from 6.2 cases per 1000 population in 2008 to 2.1 cases per 1000 population in 2012 [1]. This steep decline in malaria prevalence has been attributed to the increase distribution of LLINs [1]. After successful implementation of its malaria control program in certain regions of the country, Bangladesh has started to eliminate malaria in eight of the 13 malaria endemic districts (Figure 1).
Bangladesh’s malaria control activities have been integrated into the government’s general health services system; however, this system relies mostly on passive case detection in health facilities and with community health workers at the community level. This delivery system still faces many challenges, including inadequate accessibility to proper treatment; lack of trained health workers; and marginalized, at-risk populations with limited education [4]. In addition, there are a limited number of health facilities in the country that are equipped to manage severe malaria cases. The country’s overall surveillance and vector control programs have been insufficient to eliminate malaria from these at-risk populations particularly in the endemic regions of the country.
Geospatial technology, which has been used successfully in other malaria control programs in developing countries, includes Geographic Information System (GIS), Global Positioning System (GPS), and remote sensing (RS) [5]. GIS is defined as an organized collection of computer hardware and software, and geographic data to efficiently capture, store, update, manipulate, analyze, and display all forms of geographically referenced information [5]. With GIS it is possible to analyze differences in multiple spatial data layers related to the geographic position of a phenomenon, its attributes, and spatial relationships and to create new spatial information not available by studying the data layers separately. GPS provides users with navigation, position and timing services captured through satellite transmission [6]. Used in conjunction with GIS, this technology provides real-time data collection with accurate position information that can be used to analyze geospatial information. RS, an earth-observing instrument on satellite platforms, provides information on landscape features and climatic factors, and can be used to associate these factors with the risk of vector-borne diseases. Geospatial technologies have been used extensively in malaria risk mapping and malaria control throughout the world [7]. Providing accurate malaria risk maps can effectively guide the allocation of malaria resources and interventions in developing countries [8].
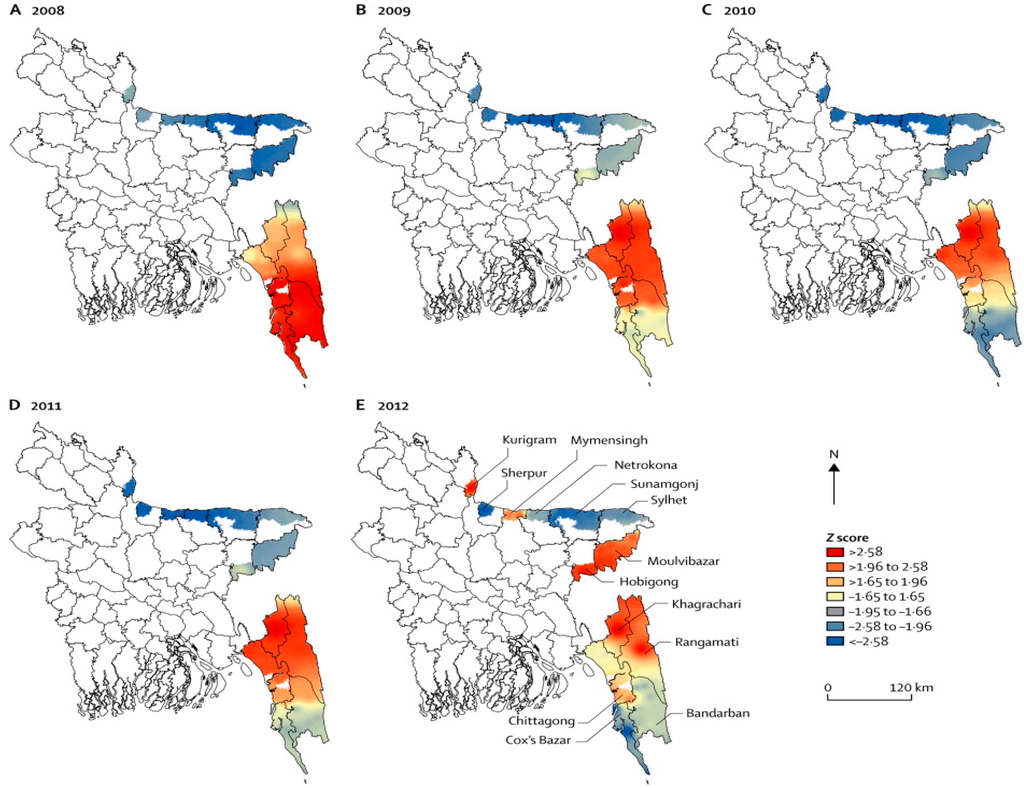
Figure 1.
Malaria prevalence in Bangladesh in 2008, and progress in malaria control from 2009 to 2012 *. * For 2009–2012, red areas show the regions with the largest decreases in malaria prevalence. (Z-score: A statistically positive Z-score indicates high rates and a negative Z-score indicates of low rates).
Geospatial technology has been previously implemented in Bangladesh to develop risk mapping in parts of the country. In this study, we investigated the recent progress of malaria mapping in Bangladesh with GIS, GPS, and RS, and identified potential future applications and contributions of geospatial technologies to eliminate malaria in the country.
2. Materials and Methods
2.1. Study Area
Approximately 98% of all malaria morbidity and mortality cases reported in Bangladesh are located in 13 malaria endemic districts along the India and Myanmar borders. These districts are situated in densely forested, hilly areas with an average altitude of 500 meters above sea level. Eight of the districts, which are considered hyperendemic, are located in the country’s northern region. The three districts with the highest malaria prevalence rates are Bandarban, Khagrachari, and Rangamati districts, located in the southwestern area of the country, in the Chittagong Hill Tracts (CHT) region, home to 1.3 million people [1,2,3]. CHT topographically encompasses hilly forests, lakes, rivers, canals, and waterfalls that provide an excellent breeding ground for Anopheline species, the vector responsible for carrying malaria parasites. Of the 35 Anopheline species found in the country, at least 26 were reported to be present in the CHT region in recent times. More than 10 of these vectors have been implicated, through laboratory testing, with the malaria parasite [9]. Historically, Anopheles minimus and An. Baimaii [10] were the most abundant and efficient vectors in the area. Due to habitat destruction (deforestation) for the expansion of human settlements and the introduction of irrigation systems among the farmlands, these two species have declined in abundance and have been replaced by a number of plain land vector species (Anopheles philippinensis, An. vagus, An. anularis, An. aconitus, An. sundaicus) [11,12].
2.2. Data Search
We researched the PubMed database for studies on the use of geospatial technology to study malaria in Bangladesh through to June 2014 (Box 1). The following search terms were used: “Malaria, Bangladesh”. The results in PubMed showed there were 218 journal articles listed; however, only 17 of 218 articles included GIS, GPS, and RS in their studies on malaria epidemiology and risk mapping in Bangladesh (Table 1). Five studies included all 13 endemic districts of the country while other studies focused specifically on the districts with the highest malaria endemic rates with five studies in Bandarban, six in Rangamati, and two in the Khagrachari district.
Box 1. Literature search for data on the use of geospatial technology to study malaria in Bangladesh.
- Period searched: through to June 2014
- Source: PubMed databases
- Search terms: (“Bangladesh”) AND (“malaria”)
- Articles found: 218
- Inclusion criterion: Referral to any article using GIS/RS/GPS to study malaria in Bangladesh
- Articles retained for evaluation after detailed review: 17 [1,2,4,8,13,14,15,16,17,18,19,20,21,22,23,24,25]

Table 1.
Malaria risk mapping studies in Bangladesh, 1992–2012.
| Geospatial Application | |||||||
|---|---|---|---|---|---|---|---|
| Study Area | Ref. # | Study Year | Sample Size | GIS | GPS | RS | Findings of the Study |
| 13 districts | [1] | 2008–2012 | - | √ | Malaria mapping of Bangladesh from 2008 to 2012 showing a decrease in the country’s prevalence rates (65%). | ||
| 13 districts | [2] | 2007 | - | √ | Findings reported statistically significant positive associations between the incidence of reported P. vivax and P. falciparum cases and rainfall and maximum temperature. | ||
| Rangamati | [4] | 2009 | 5322 | √ | √ | Housing materials, household densities, education levels, and proximity to the regional urban center, were found to be effective predictors of treatment-seeking preferences for malaria. | |
| 13 districts | [8] | 2007 | 9750 | √ | √ | √ | Bayesian modeling found statistically significant correlation between malaria prevalence and rainfall, temperature, and elevation as major factors influencing spatiotemporal patterns. |
| Khagrachari | [13] | 2007 | 750 | √ | √ | √ | Risk mapping used to predict areas of high and low malaria prevalence based on risk factors that included age and location of fragmented forests. |
| Khagrachari | [14] | 2007 | 750 | √ | √ | √ | Proximity (3 km) to water proved significant as a risk factor for malaria. |
| Rangamati | [15] | 2009 | 1400 | √ | √ | √ | Hot-spot clustering of cases with statistically significant risk factors between malaria positivity and ethnicity, forest cover, altitude, treatment preference, floor construction, and household density. |
| Rangamati | [16] | 2009–2010 | 1634 | √ | √ | √ | Identified malaria hotspots and with risk factors of low bed net ratio, home construction material, and high density of homes. |
| Rangamati | [17] | 2009 | 5322 | √ | √ | Mapping of treatment seeking behaviors showed place of preference for malaria treatment were government health facilities if it was located 2 km from government health facilities preferred drug vendors. | |
| Bandarban | [18] | 2010–2012 | 24,074 | √ | √ | Risk factors for malaria were higher among jhum cultivators than non-cultivators living in the same household. | |
| All Bangladesh | [19] | 1992–2001 | - | √ | VCI and TCI were strong predictors of malaria risk in Bangladesh. | ||
| Bandarban | [20] | 1992–2004 | - | √ | Estimated epidemic risks can be achieved using VHI and high summer TCI. | ||
| Bandarban | [21] | 2009–2010 | 20,563 | √ | √ | Mapping of symptomatic & asymptomatic cases with high clustering within CHT; 80% of cases occurred during the rainy season. | |
| Rangamati | [22] | 2009 | 1400 | √ | √ | Age, ethnicity, proximity to forest, household density, and elevation were significant risk factors for malaria with 44.12% households living in areas with ≥10% prevalence rates. | |
| 13 districts | [23] | 2007 | 9750 | √ | √ | Malaria risk mapping of CHT with unequal distribution of prevalence rates -Khagrachari (15.25%), Bandarban (10.97%), and Rangamati (7.42%). | |
| Bandarban | [24] | 2010–2013 | 1753 | √ | √ | Higher risk of P. falciparum infection in pregnant women than other adults with asymptomatic infections. | |
| Bandarban | [25] | 2009–2012 | 4782 | √ | √ | Cases were geographically limited to hotspots with 80% infections occurring in one third of the population; incidence rates were highly seasonal with 85.8% of cases during rainy season (May–October). | |
VCI: Vegetation Condition Indices; TCI: Temperature Condition Index
3. Results and Discussion
3.1. Results
Through June 2014, there were 17 published studies that have used geospatial technologies (GIS, GPS and/or RS) to understand and predict malaria risks [1,2,8,13,14,15,16,17,18,19,20,21], develop malaria risk maps, [21,22] and provide findings for targeted interventions strategies in Bangladesh. To supply feedback to the NMCP, national malaria risk maps were produced [2,23]. Long-term average monthly rainfalls and minimum/maximum temperatures ranges were interpolated, and elevation and vegetation coverage data were obtained using satellite imagery. GIS was also employed to develop maps of posterior distributions of predicted prevalence [13]. In one study, environmental variables were extracted from RS data to predict malaria risk at the national level [8]. Since 2008, the NMCP has confirmed a reduction of malaria in all endemic districts including CHT, which reported prevalence rate above 10%, the highest in the country [1,23].
There were four published studies based in CHT that used satellite images for land cover classification, risk mapping, and GIS mapping to investigate spatial relationships between malaria and risk factors. In addition, GIS and GPS were used to understand malaria incidence and prevalence rates with both active and passive surveillance at the individual and household levels. In another study, in the Bandarban District, a cohort framework of over 4000 households was established and mapped for a longitudinal study [21]. Four studies prepared risk maps in the same district focusing on pregnant women and jhum cultivators—subsistent farmers that use slash and burn methods of farming [18,24]. There were six malaria risk mapping studies conducted in Rajasthali, a sub-district of Rangamati district, which in 2007 had the highest (36%) malaria prevalence rates in the country [23]. All households (n = 5322) studied in this sub-district were mapped using GPS and a household census was conducted collecting socio-demographic information, linking this data to geocoded household locations [4]. In addition, all health facilities and providers were mapped including the locations of community health workers, satellite clinics, hospitals, and drug stores [4]. Spatial models were explored in these different studies using ArcGIS, SaTScan, SAGA, and WinBugs mapping software. SAGA was used to extract topographical wetness (a measure of the extent of flow accumulation at the given point of the topographic surface) and elevation for all households surveyed in the Rangamati district. Satellite images using Advanced Spaceborne Thermal Emission and Reflection Radiometer digital elevation models was used to create water flow direction, accumulation, watershed, stream network, and stream link layers. Using cross-sectional and longitudinal data from these studies, spatial modeling of treatment seeking behaviors [17] and risk maps [8,13,16] were established and used to determine the progress and challenges to the NMCP.
3.2. Discussion
Geospatial technologies have been used for malaria risk mapping in Bangladesh since 2006 with the updating of these maps in 2008 and 2012 by the NMCP in collaboration with other research institutions [1,23]. Bangladesh has also developed spatial models for treatment seeking behavior, hydrological and prediction analysis using geostatistical modeling. Findings have confirmed that Bangladesh is closer to malaria elimination than ever before. The implementation of risk mapping with the NMCP, focusing particularly on targeted interventions in high risk areas in CHT, could provide decision makers crucial information for their elimination strategies [16].
While GIS, GPS and RS have all shown to be beneficial in providing data for malaria elimination strategies in both Bangladesh and other developing countries, improvements are still needed in the data collection process and dissemination of findings from the different malaria studies. Using household surveys, malaria hot-spots (the clustering of high malaria incidence cases) data, and more readily available spatial malaria databases along with a better understanding by decision makers on the usages and capabilities of these spatial analytical methods, can lead to more successful malaria elimination strategies [26]. The use of GIS and GPS systems connected to mobile phones [27] can also aid in malaria case detection and delivery of health services particularly in remote areas of CHT where tracking and analyzing malaria prevalence data can often be difficult [28]. With changing malaria epidemiology and reduced burden of malaria throughout the country, Bangladesh needs to focus on CHT region elimination strategies to address malaria hot-spots efficiently and effectively as well as reduce malaria importation, insecticide resistance, drug resistance [29], and the mapping of asymptomatic carrier [24]. Geospatial technology can provide the necessary data to assist in these elimination strategies.
Bangladesh NMCP has an extensive network of community health workers in all endemic districts but travel is often challenging in certain areas because of the difficult terrain and dense forest cover with few roads and limited waterways, which is often the only way to travel in these remote regions during the wet season. Thus, people living in these isolated areas are often deprived of many essential health services including proper malaria prevention and treatment methods. Careful planning using geospatial technologies to locate hot-spots particularly in the endemic districts of Bangladesh will be crucial in achieving malaria elimination goals in a cost effective way by focusing resourcing in areas with high prevalence rates (Table 2).

Table 2.
Recommended Geospatial Technologies to use toward Malaria Elimination in Bangladesh.
| Geospatial Technology | Recommended Applications |
|---|---|
| GIS | Create malaria risk map at the lowest administrative level and update malaria maps each month. |
| GPS | Locate hospitals, health facilities, clinics, and households to create malaria information systems for improved mapping of risk areas. |
| Mobile Telecommunication Systems | Target interventions using surveillance data, satellite imagery, and mobile phone call records to improve coordination of services. |
| Spatiotemporal Cluster Detection | Analyze malaria cases in each month, detect spatio-temporal clustering, and locate hotspots. |
| Geostatistics | Detect spatial auto-correlation, prediction, and modeling for cost effective interventions. |
| Ecological Niche Models | Prepare malaria vector distribution maps, ecological suitability, predict vector distribution maps to locate vector-breeding areas and determine the indoor residual spraying strategies. |
| Bayesian methods | Interpolate, predict, and develop models using multiple malaria risk factors. |
| Spatially Explicit Mathematical Models | Create hierarchical models, hierarchical linear regression models, and mixed linear regressions to predict current and future malaria risk scenarios. |
With the abundance of malaria vector breeding sites in the CHT region of the country, RS can be used to look at vector’s oviposition site/breeding ground and thereby predict their abundance. There has been a proliferation of some vector species in this region with an increase in standing water, particularly during the rainy seasons, from deforestation for agricultural purposes, providing more breeding sites for the mosquitos [30]. It has been noted that during the dry and malaria off-seasons, cases were found clustered around natural streams and canals in the CHT region [25]. Locating land use patterns across the vector breeding sites and using remotely sensed climatic environmental factors, particularly temperature, humidity, and rainfall as they correlate to malaria outbreaks, could provide useful information on the planning of vector control in this region. This same approach was applied in Indonesia and revealed malaria vector abundance in certain areas where malaria control programs were then implemented with much success [31]. The topographic variable can also be remotely-sensed to predict malaria vector’s breeding site in malaria endemic areas [32].
It should be noted that Bangladesh performed much better in malaria mapping of its endemic areas compared to its neighboring malaria endemic countries, India and Myanmar. Countries engage in malaria control [33,34,35,36] and elimination [37] may learn from Bangladeshi experiences. Spatial analytical studies have shown a higher incidence of malaria in areas adjacent to these international borders [26]. To sustain recent gains in malaria elimination, the Bangladesh NMCP should look at cross-border movement between Bangladesh and India and Myanmar. The mapping of malaria prevalence as well as surveying for household movement along the borders can also be used to identify hotspots in these areas.
Based on the findings of these studies, the following are recommendations for the NMCP to implement to further the malaria elimination program in Bangladesh: identify high-risk malaria zones to determine spatial distribution; combine surveillance with GIS and weather pattern database to determine geographic and climate risks [21]; conduct further studies to understand malaria transmission among impacted populations during high transmission season; develop strategies to interrupt transmission in low transmission settings [18]; use mass screening in stable hot-spot areas to identify asymptomatic reservoirs and provide treatment to reduce the malaria burden [16]; promote malaria test and treatment services particularly among vulnerable populations, such as children under five years and jhum cultivators [18]; monitor asymptomatic malaria particularly among pregnant women living in low-intensity malaria transmission areas [24]; target interventions at fine spatial scales for malaria control programs; improve equity of access to interventions [15]; improve collaboration between researchers using geostatistical techniques and malaria control managers; target high malaria transmission areas [8] to provide more GPS, GIS, and RS strategies to characterize spatial heterogeneity with malaria risk at a fine scale and identify high risk areas that have not been studied [19]; and lastly focus on interventions to be targeted and timed according to risk profiles of endemic areas [38].
4. Conclusions
Bangladesh has made significant advancements in malaria reduction and has successfully used geospatial technologies at various levels for risk mapping and targeted interventions in the 13 malaria endemic districts. However, with the continued reduction in malaria burden along with the country’s goal of elimination, this technology should be prioritized by the NMCP in their elimination strategy. More effort should be made by the NMCP to incorporate these strategies with improved surveillance systems, particularly in the remote areas of the CHT region, to detect and address malaria hotspots. Incorporating malaria ecology with spatial data along with malaria incidence maps, land usage maps, and population distributions can be helpful for decision makers to establish elimination strategies in these malaria endemic areas. Rapid advances in technology and analytical methods have allowed the development of spatial decision support systems, which can improve the elimination programs by enabling more accurate and timely resource allocation in high-risk areas. Geospatial technologies can play an important role in identifying inequities in health services in endemic areas of the country. GIS, GPS and RS are proven powerful tools that can provide important data and should be integrated with active and passive surveillance systems to achieve malaria elimination in Bangladesh.
Acknowledgments
This work was funded in part by the Emerging Pathogens Institute at the University of Florida and the College of Liberal Arts and Sciences, as part of the University of Florida Preeminence Initiative.
Author Contributions
K.E.K. and U.H. conceived the study design, analyzed data and drafted the manuscript. M.Z.H. and M.S.A. contributed in writing and critically reviewed the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Haque, U.; Overgaard, H.J.; Clements, A.C.; Norris, D.E.; Islam, N.; Karim, J.; Roy, S.; Haque, W.; Kabir, M.; Smith, D.L.; et al. Malaria burden and control in Bangladesh and prospects for elimination: An epidemiological and economic assessment. Lancet Glob. Health 2014, 2, e98–e105. [Google Scholar] [CrossRef] [PubMed]
- Reid, H.L.; Haque, U.; Roy, S.; Islam, N.; Clements, A.C. Characterizing the spatial and temporal variation of malaria incidence in Bangladesh, 2007. Malar. J. 2012, 11. [Google Scholar] [CrossRef] [PubMed]
- National Malaria Control Program About NMCP in Bangladesh. Available online: http://www.Nmcp.Info/nmcp.Aspx (accessed on 9 June 2014).
- Haque, U.; Hashizume, M.; Sunahara, T.; Hossain, S.; Ahmed, S.M.; Haque, R.; Yamamoto, T.; Glass, G.E. Progress and challenges to control malaria in a remote area of Chittagong hill tracts, Bangladesh. Malar. J. 2010, 9. [Google Scholar] [CrossRef] [PubMed]
- What is a GIS? Available online: http://www.Volusia.Org/gis/whatsgis.Htm (accessed on 11 September 2014).
- GPS. Available online: http://www.Gps.Gov/systems/gps/ (accessed on 28 May 2014).
- Bautista, C.T.; Chan, A.S.; Ryan, J.R.; Calampa, C.; Roper, M.H.; Hightower, A.W.; Magill, A.J. Epidemiology and spatial analysis of malaria in the northern Peruvian Amazon. Am. J. Trop. Med. Hyg. 2006, 75, 1216–1222. [Google Scholar] [PubMed]
- Reid, H.; Haque, U.; Clements, A.C.A.; Tatem, A.J.; Vallely, A.; Ahmed, S.M.; Islam, A.; Haque, R. Mapping malaria risk in Bangladesh using bayesian geostatistical models. Am. J. Trop. Med. Hyg. 2010, 83, 861–867. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.S.; Chakma, S.; Khan, W.A.; Glass, G.E.; Mohon, A.N.; Elahi, R.; Norris, L.C.; Podder, M.P.; Ahmed, S.; Haque, R.; et al. Diversity of anopheline species and their plasmodium infection status in rural Bandarban, Bangladesh. Parasit. Vector 2012, 5. [Google Scholar] [CrossRef]
- Khan, A.Q.; Talibi, S.A. Epidemiological assessment of malaria transmission in an endemic area of East Pakistan and the significance of congenital immunity. Bull. World Health Organ. 1972, 46, 783–792. [Google Scholar] [PubMed]
- Elias, M.; Dewan, R.; Ahmed, R. Vectors of malaria in Bangladesh. J. Prev. Soc. Med. 1982, 1, 20–28. [Google Scholar]
- Alam, M.; Khan, M.; Chaudhury, N.; Deloer, S.; Nazib, F.; Bangali, A.; Haque, R. Prevalence of anopheline species and their plasmodium infection status in epidemic-prone border areas of Bangladesh. Malar. J. 2010, 9. [Google Scholar] [CrossRef] [PubMed]
- Haque, U.; Magalhaes, R.J.S.; Reid, H.L.; Clements, A.C.A.; Ahmed, S.M.; Islam, A.; Yamamoto, T.; Haque, R.; Glass, G.E. Spatial prediction of malaria prevalence in an endemic area of Bangladesh. Malar. J. 2010, 9. [Google Scholar] [CrossRef] [PubMed]
- Haque, U.; Huda, M.; Hossain, A.; Ahmed, S.M.; Moniruzzaman, M.; Haque, R. Spatial malaria epidemiology in Bangladeshi highlands. Malar. J. 2009, 8. [Google Scholar] [CrossRef] [PubMed]
- Haque, U.; Sunahara, T.; Hashizume, M.; Shields, T.; Yamamoto, T.; Haque, R.; Glass, G.E. Malaria prevalence, risk factors and spatial distribution in a hilly forest area of Bangladesh. PLoS One 2011, 6. [Google Scholar] [CrossRef] [PubMed]
- Haque, U.; Glass, G.E.; Bomblies, A.; Hashizume, M.; Mitra, D.; Noman, N.; Haque, W.; Kabir, M.M.; Yamamoto, T.; Overgaard, H.J. Risk factors associated with clinical malaria episodes in Bangladesh: A longitudinal study. Am. J. Trop. Med. Hyg. 2013, 88, 727–732. [Google Scholar] [CrossRef] [PubMed]
- Haque, U.; Scott, L.M.; Hashizume, M.; Fisher, E.; Haque, R.; Yamamoto, T.; Glass, G.E. Modelling malaria treatment practices in Bangladesh using spatial statistics. Malar. J. 2012, 11. [Google Scholar] [CrossRef] [PubMed]
- Galagan, S.R.; Prue, C.S.; Khyang, J.; Khan, W.A.; Ahmed, S.; Ram, M.; Alam, M.S.; Haq, M.Z.; Akter, J.; Streatfield, P.K.; et al. The practice of jhum cultivation and its relationship to plasmodium falciparum infection in the Chittagong hill districts of Bangladesh. Am. J. Trop. Med. Hyg. 2014, 91, 374–383. [Google Scholar] [CrossRef] [PubMed]
- Rahman, A.; Kogan, F.; Roytman, L. Short report: Analysis of malaria cases in Bangladesh with remote sensing data. Am. J. Trop. Med. Hyg. 2006, 74, 17–19. [Google Scholar] [PubMed]
- Rahman, A.; Krakauer, N.; Roytman, L.; Goldberg, M.; Kogan, F. Application of advanced very high resolution radiometer (AVHRR)-based vegetation health indices for estimation of malaria cases. Am. J. Trop. Med. Hyg. 2010, 82, 1004–1009. [Google Scholar] [CrossRef] [PubMed]
- Khan, W.A.; Sack, D.A.; Ahmed, S.; Prue, C.S.; Alam, M.S.; Haque, R.; Khyang, J.; Ram, M.; Akter, J.; Nyunt, M.M.; et al. Mapping hypoendemic, seasonal malaria in rural Bandarban, Bangladesh: A prospective surveillance. Malar. J. 2011, 10. [Google Scholar] [CrossRef] [PubMed]
- Haque, U.; Soares Magalhaes, R.J.; Mitra, D.; Kolivras, K.N.; Schmidt, W.P.; Haque, R.; Glass, G.E. The role of age, ethnicity and environmental factors in modulating malaria risk in Rajasthali, Bangladesh. Malar. J. 2011, 10. [Google Scholar] [CrossRef] [PubMed]
- Haque, U.; Ahmed, S.M.; Hossain, S.; Huda, M.; Hossain, A.; Alam, M.S.; Mondal, D.; Khan, W.A.; Khalequzzaman, M.; Haque, R. Malaria prevalence in endemic districts of Bangladesh. PLoS One 2009, 4, e6737. [Google Scholar] [CrossRef] [PubMed]
- Khan, W.A.; Galagan, S.R.; Prue, C.S.; Khyang, J.; Ahmed, S.; Ram, M.; Alam, M.S.; Haq, M.Z.; Akter, J.; Glass, G.; et al. Asymptomatic plasmodium falciparum malaria in pregnant women in the Chittagong hill districts of Bangladesh. PLoS One 2014, 9. [Google Scholar] [CrossRef] [PubMed]
- Glass, G.; Alam, M.S.; Khan, W.A.; Sack, D.A.; Sullivan, D.J. Spatial clustering of malaria cases during low-transmission season in Kuhalong, Bangladesh. In Proceedings of the 13th Ascon Conference, Dhaka, Bangladesh, 28 March 2011.
- Clement, A.C.; Reid, H.; Kelly, G.; Hay, S. Further shrinking the malaria map: How can geospatial science help to achieve malaria elimination? Lancet Infect. Dis. 2013, 13, 709–718. [Google Scholar] [CrossRef] [PubMed]
- Tatem, A.J.; Huang, Z.; Narib, C.; Kumar, U.; Kandula, D.; Pindolia, D.K.; Smith, D.L.; Cohen, J.M.; Graupe, B.; Uusiku, P.; et al. Integrating rapid risk mapping and mobile phone call record data for strategic malaria elimination planning. Malar. J. 2014, 13. [Google Scholar] [CrossRef] [PubMed]
- Prue, C.S.; Shannon, K.L.; Khyang, J.; Edwards, L.J.; Ahmed, S.; Ram, M.; Shields, T.; Hossain, M.S.; Glass, G.E.; Nyunt, M.M.; et al. Mobile phones improve case detection and management of malaria in rural Bangladesh. Malar. J. 2013, 12. [Google Scholar] [CrossRef] [PubMed]
- Haque, U.; Glass, G.E.; Haque, W.; Islam, N.; Roy, S.; Karim, J.; Noedl, H. Antimalarial drug resistance in Bangladesh, 1996–2012. Trans. R. Soc. Trop. Med. Hyg. 2013, 107, 745–752. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.S.; Chakma, S.; Al-Amin, H.M.; Elahi, R.; Mohon, A.N.; Khan, W.A.; Haque, R.; Glass, G.E.; Sack, D.A.; Sullivan, D.J.; et al. Role of artificial containers as breeding sites for anopheline mosquitoes in Malaria hypo endemic areas of rural Bandarban, Bangladesh: Evidence form a baseline survey. In Proceedings of the Astmh Conference 2012, Atlanta, GA, USA, 11–15 November 2012.
- Stoops, C.A.; Gionar, Y.R.; Shinta; Sismadi, P.; Rachmat, A.; Elyazar, I.F.; Sukowati, S. Remotely-sensed land use patterns and the presence of anopheles larvae (diptera: Culicidae) in Sukabumi, West Java, Indonesia. J. Vector. Ecol. 2008, 33, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Nmor, J.C.; Sunahara, T.; Goto, K.; Futami, K.; Sonye, G.; Akweywa, P.; Dida, G.; Minakawa, N. Topographic models for predicting malaria vector breeding habitats: Potential tools for vector control managers. Parasit. Vector 2013, 6. [Google Scholar] [CrossRef]
- Kamuliwo, M.; Chanda, E.; Haque, U.; Mwanza-Ingwe, M.; Sikaala, C.; Katebe-Sakala, C.; Mukonka, V.M.; Norris, D.E.; Smith, D.L.; Glass, G.E.; et al. The changing burden of malaria and association with vector control interventions in Zambia using district-level surveillance data, 2006–2011. Malar. J. 2013, 12. [Google Scholar] [CrossRef] [PubMed]
- Mukonka, V.M.; Chanda, E.; Haque, U.; Kamuliwo, M.; Mushinge, G.; Chileshe, J.; Chibwe, K.A.; Norris, D.E.; Mulenga, M.; Chaponda, M.; et al. High burden of malaria following scale-up of control interventions in Nchelenge district, Luapula province, Zambia. Malar. J. 2014, 13. [Google Scholar] [CrossRef] [PubMed]
- Chanda, E.; Mukonka, V.M.; Kamuliwo, M.; Macdonald, M.B.; Haque, U. Operational scale entomological intervention for malaria control: Strategies, achievements and challenges in Zambia. Malar. J. 2013, 12. [Google Scholar] [CrossRef] [PubMed]
- Chanda, E.; Govere, J.M.; Macdonald, M.B.; Lako, R.L.; Haque, U.; Baba, S.P.; Mnzava, A. Integrated vector management: A critical strategy for combating vector-borne diseases in South Sudan. Malar. J. 2013, 12. [Google Scholar] [CrossRef] [PubMed]
- Simon, C.; Moakofhi, K.; Mosweunyane, T.; Jibril, H.B.; Nkomo, B.; Motlaleng, M.; Ntebela, D.S.; Chanda, E.; Haque, U. Malaria control in Botswana, 2008–2012: The path towards elimination. Malar. J. 2013, 12. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Galagan, S.; Scobie, H.; Khyang, J.; Prue, C.S.; Khan, W.A.; Ram, M.; Alam, M.S.; Haq, M.Z.; Akter, J.; et al. Malaria hotspots drive hypoendemic transmission in the Chittagong hill districts of Bangladesh. PLoS One 2013, 8. [Google Scholar] [CrossRef] [PubMed]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).