A Multi-Scale Geographically Weighted Regression Approach to Understanding Community-Built Environment Determinants of Cardiovascular Disease: Evidence from Nanning, China
Abstract
1. Introduction
2. Materials and Methods
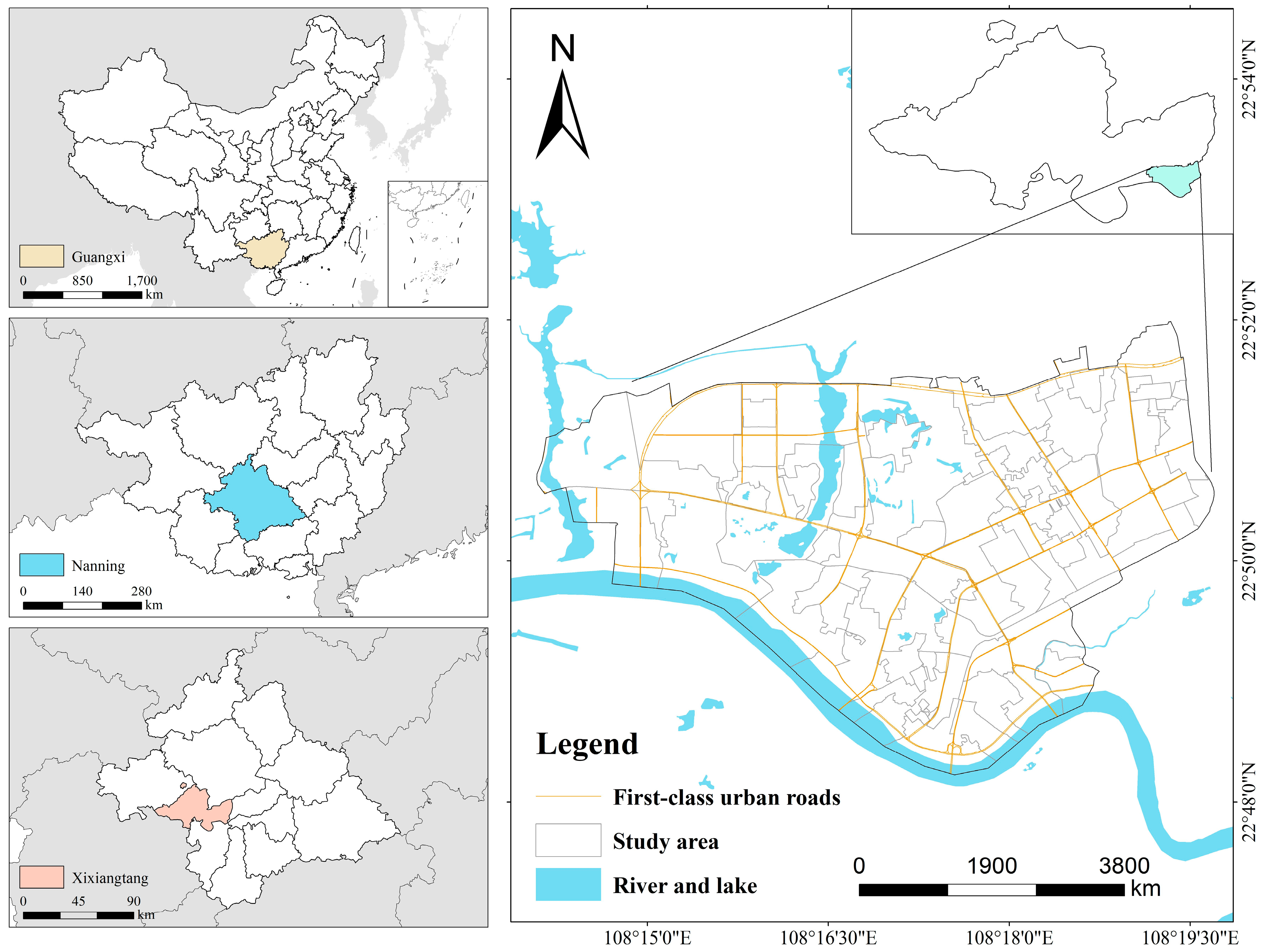
2.1. Study Area Overview
2.2. Data Description
2.2.1. Cardiovascular Patient Data
2.2.2. Built Environment Data
2.2.3. Variables and Definitions
2.3. Research Methods
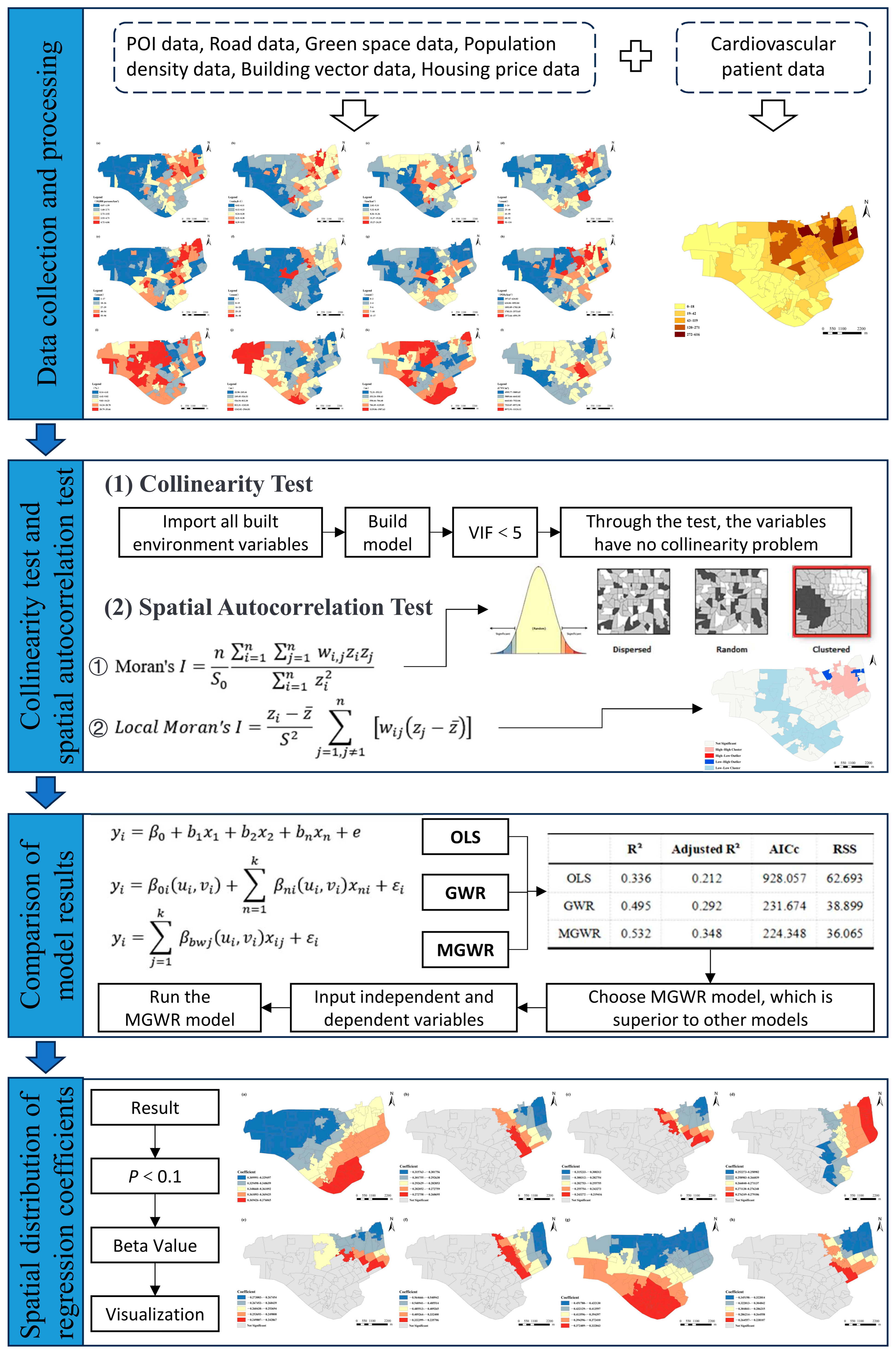
2.3.1. Research Framework
2.3.2. Spatial Autocorrelation Testing
2.3.3. Ordinary Least Squares (OLS)
2.3.4. Geographically Weighted Regression (GWR)
2.3.5. Multi-Scale Geographically Weighted Regression (MGWR)
3. Results
3.1. Spatial Distribution and Clustering Characteristics of Cardiovascular Patients
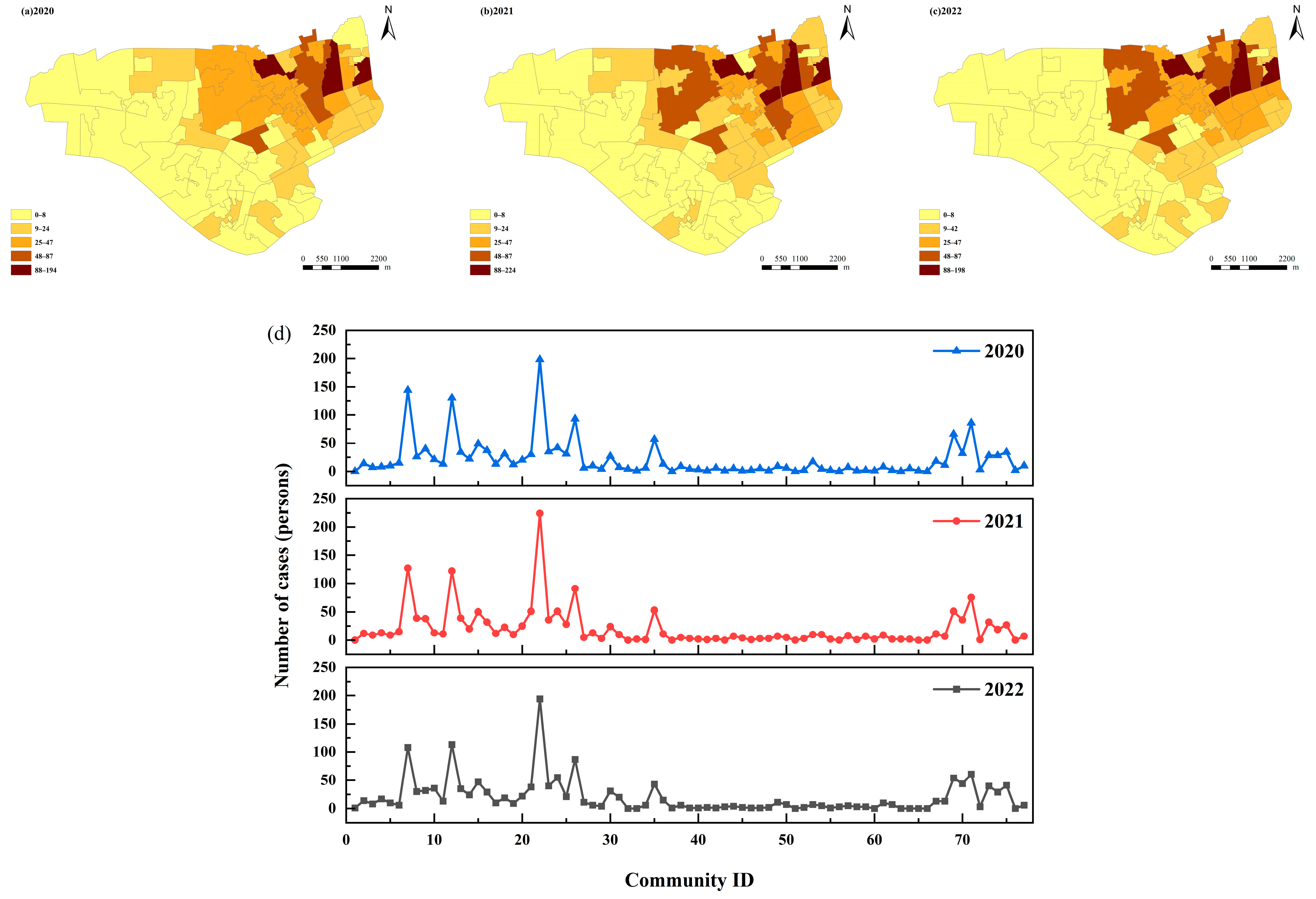
3.1.1. Spatial Distribution
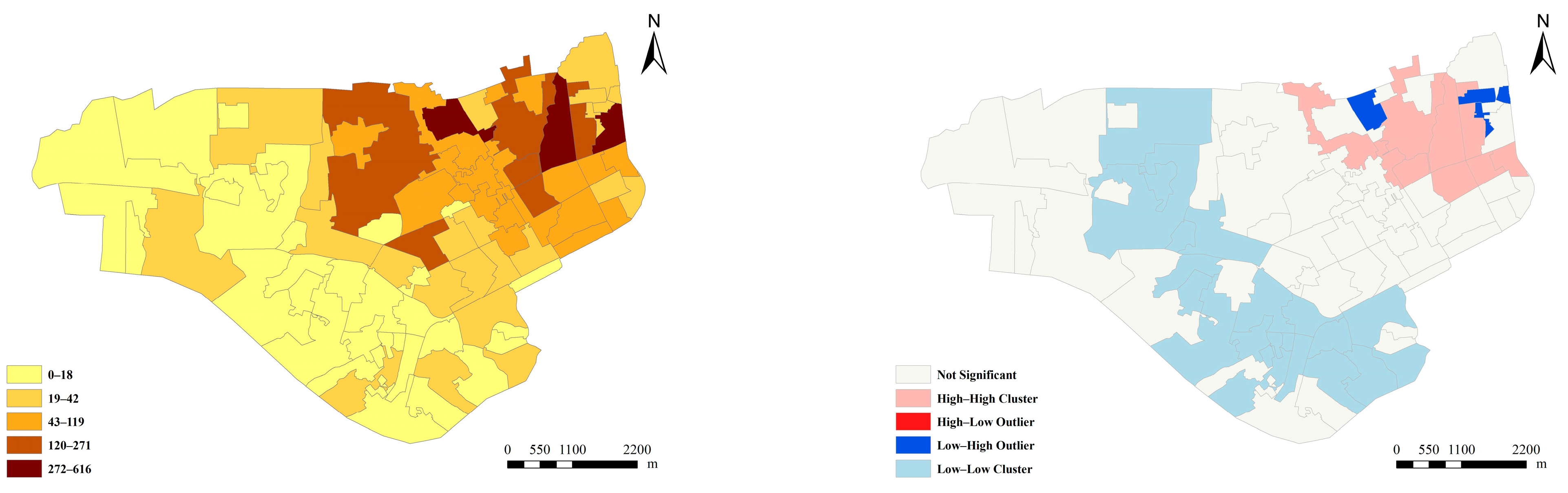
3.1.2. Spatial Clustering Characteristics of Cardiovascular Patients at the Community Level
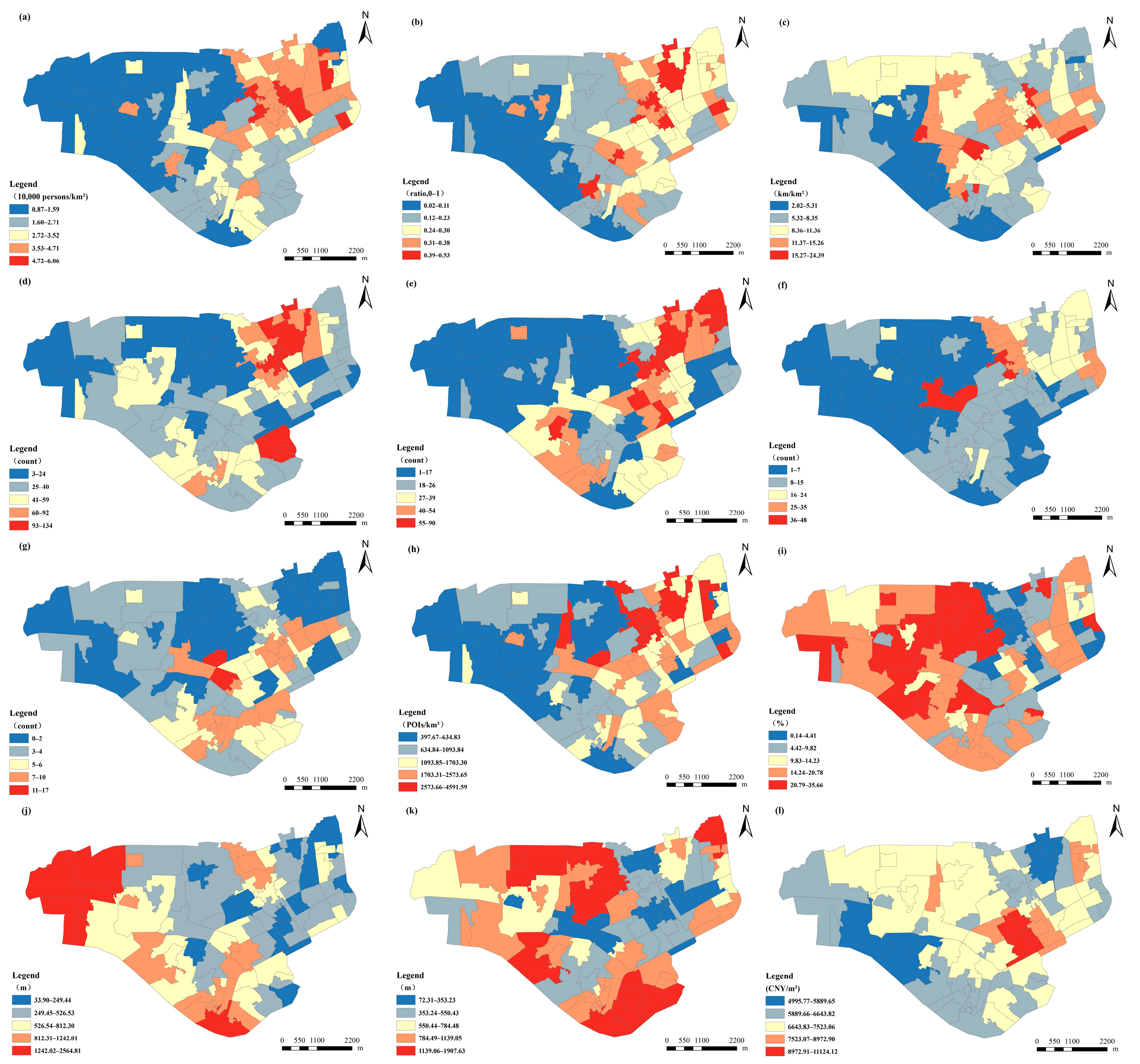
3.2. Spatial Distribution Characteristics of the Built Environment
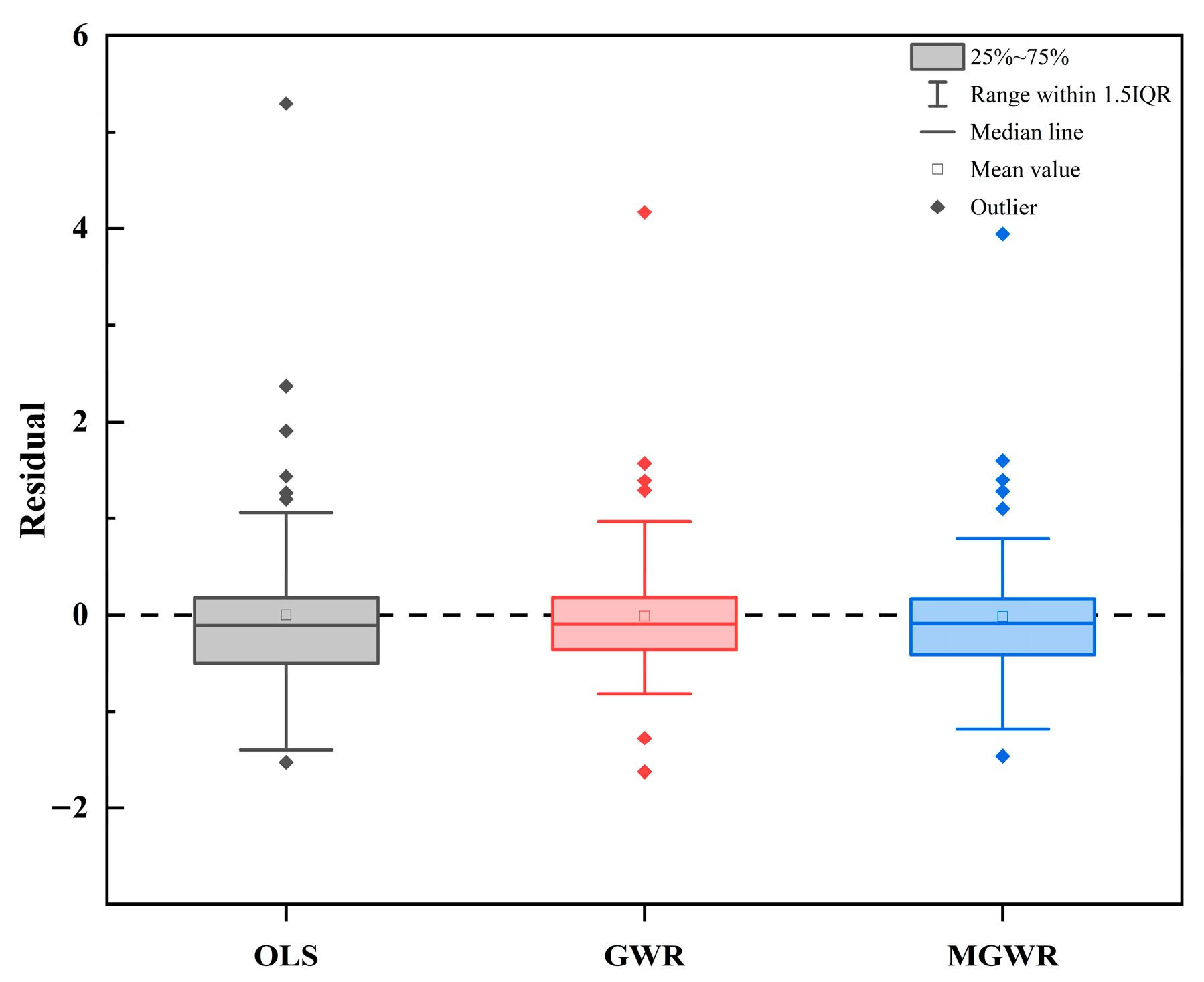
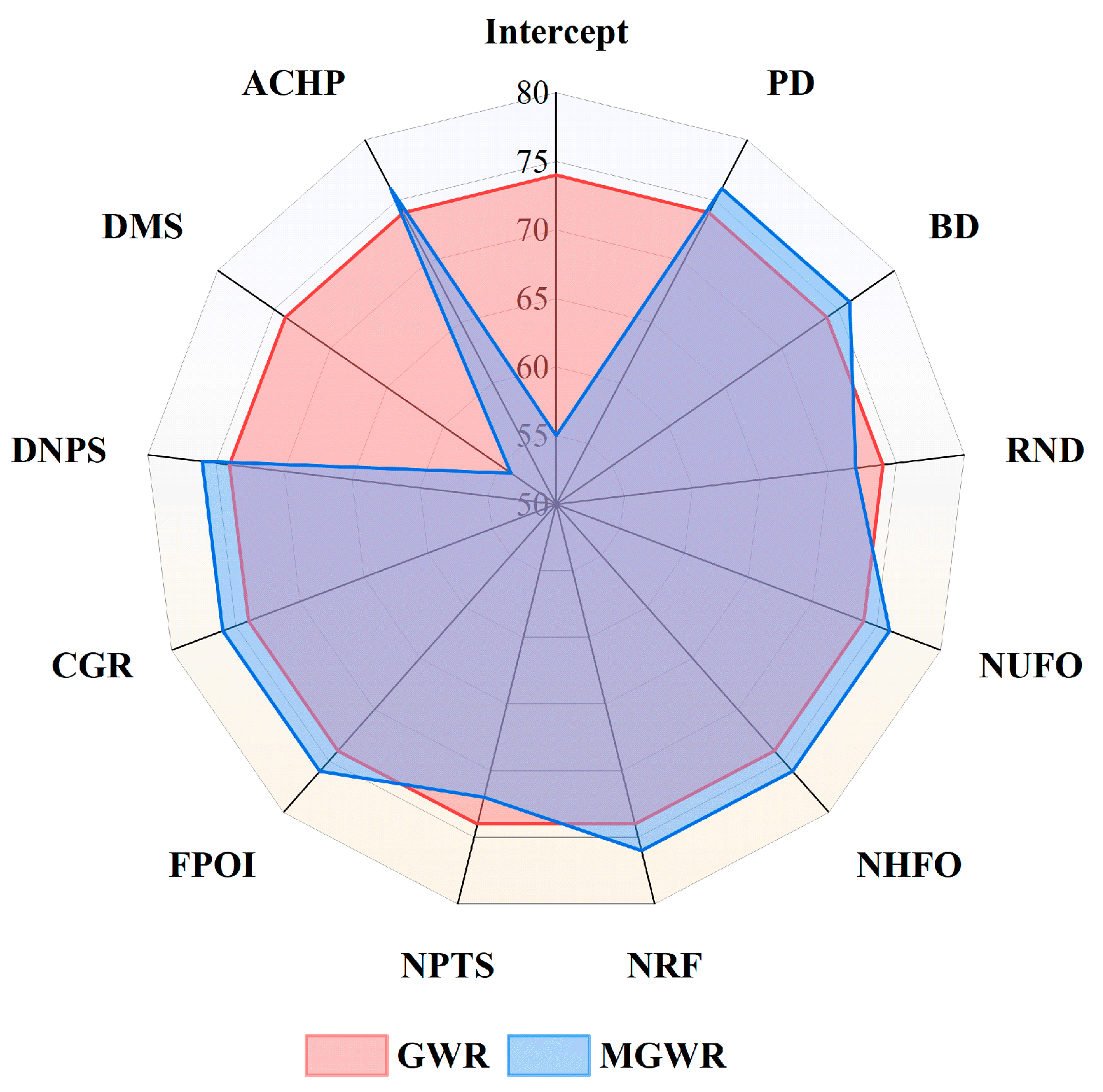
3.3. Model Comparison Results
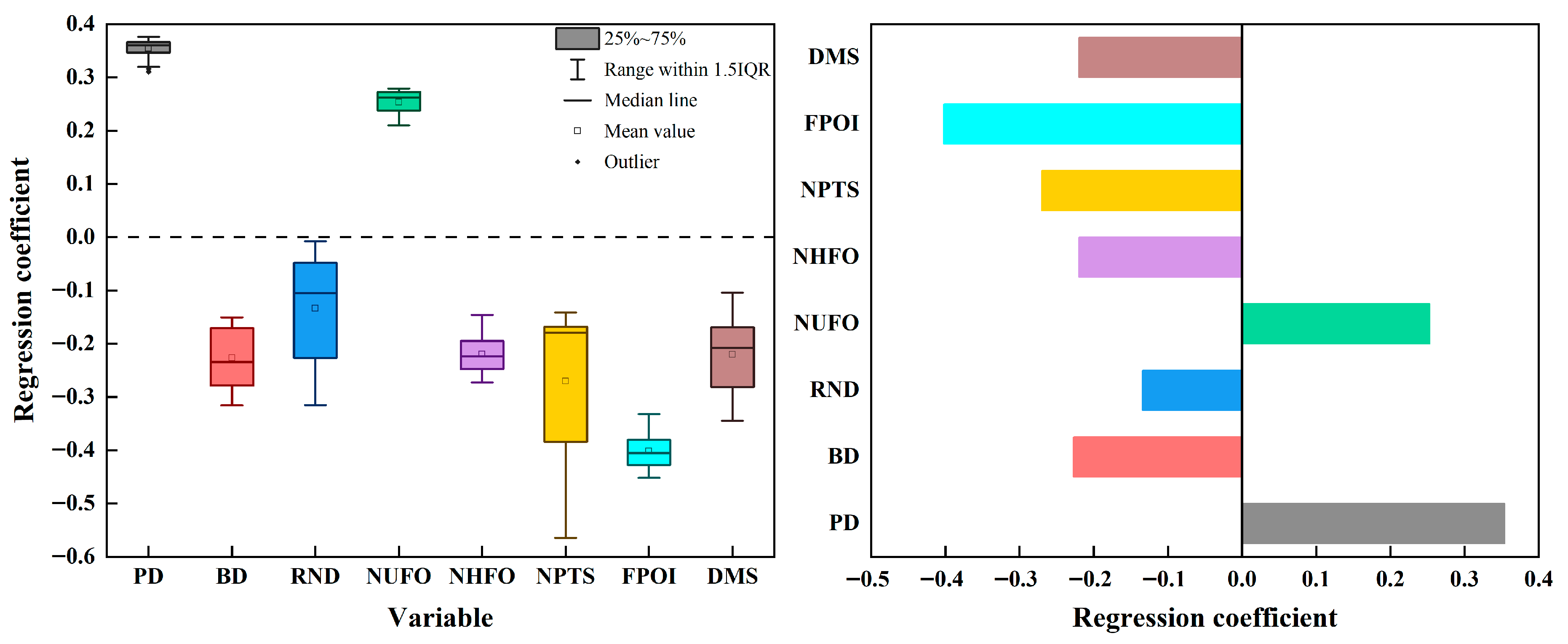
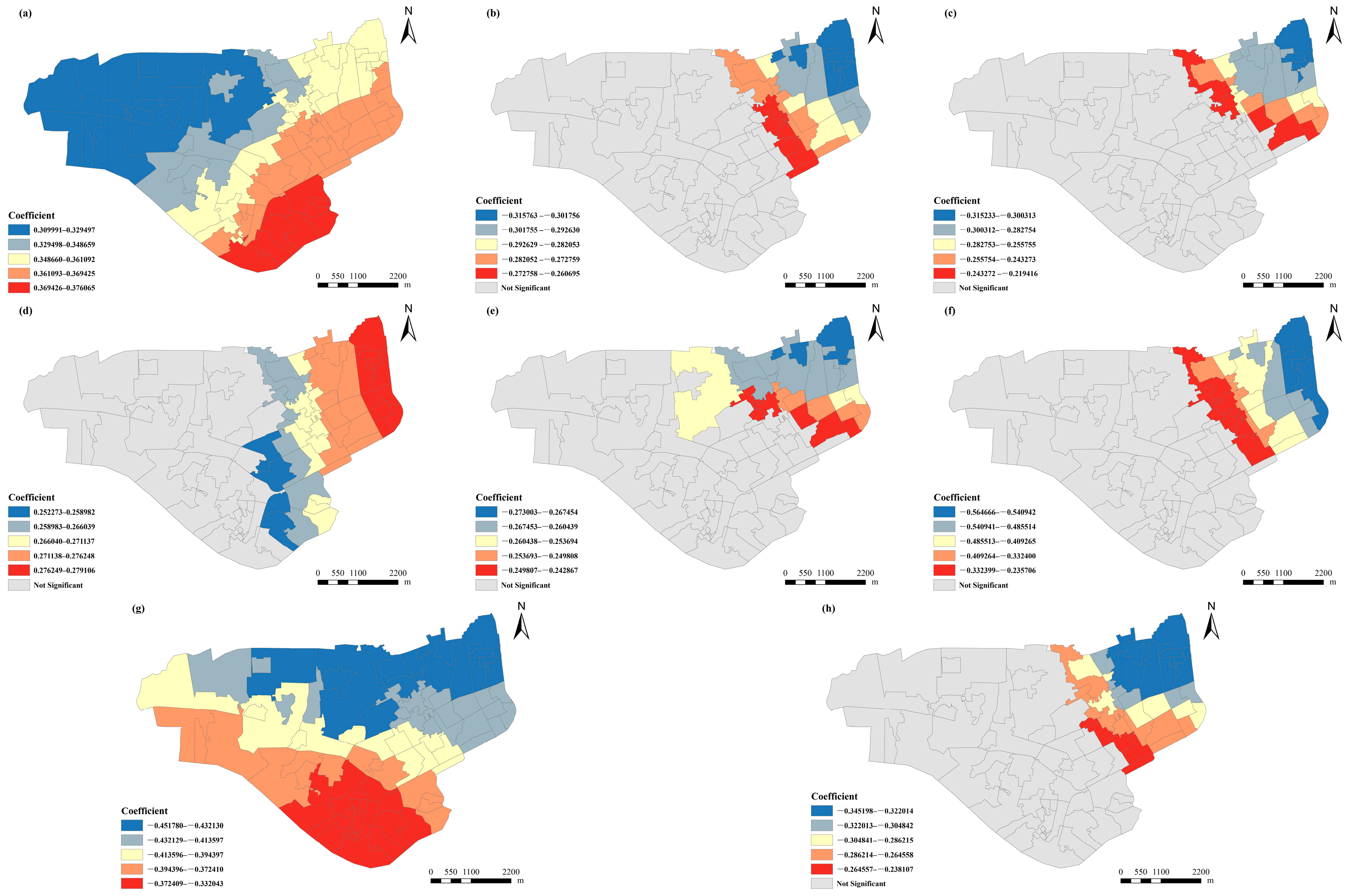
3.4. Spatial Heterogeneity Analysis of Influencing Factors
4. Discussion
4.1. Key Findings
4.2. Policy Implications
4.3. Limitations and Future Research Directions
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CVD | Cardiovascular Disease |
| GBD | Global Burden of Disease |
| WHO | World Health Organization |
| OLS | Ordinary least squares |
| GWR | Geographically weighted regression |
| MGWR | Multi-scale geographically weighted regression |
| POI | Points of interest |
| VIF | Variance inflation factor |
| NCC | Number of Cardiovascular Cases |
| PD | Population Density |
| BD | Building Density |
| RND | Road Network Density |
| LUME | Land Use Mix Entropy |
| NUFO | Number of Unhealthy Food Outlets |
| NHFO | Number of Healthy Food Outlets |
| NRF | Number of Recreational Facilities |
| NPTS | Number of Public Transport Stations |
| FPOI | Facility POI Density |
| CGR | Community Green Space Ratio |
| DNPS | Distance to Nearest Park or Square |
| DBS | Distance to Nearest Bus Stop |
| DMS | Distance to Nearest Metro Station |
| ACHP | Average Community Housing Price |
| RSS | Residual sum of squares |
| GIS | Geographic Information Systems |
| HH | high–high clusters |
| LL | low–low clusters |
| HL | high–low clusters |
| LH | low–high clusters |
References
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update from the GBD 2019 study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef] [PubMed]
- Non-Communicable Disease. Available online: https://www.who.int/zh/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 27 November 2024).
- Wang, Y.; Wang, J. Modelling and prediction of global non-communicable diseases. BMC Public Health 2020, 20, 822. [Google Scholar] [CrossRef] [PubMed]
- Lai, K.Y.; Webster, C.; Gallacher, J.E.J.; Sarkar, C. Associations of Urban Built Environment with Cardiovascular Risks and Mortality: A Systematic Review. J. Urban Health 2023, 100, 745–787. [Google Scholar] [CrossRef]
- Bhatnagar, A. Environmental Determinants of Cardiovascular Disease. Circ. Res. 2017, 121, 162–180. [Google Scholar] [CrossRef]
- Pinter-Wollman, N.; Jelić, A.; Wells, N.M. The impact of the built environment on health behaviours and disease transmission in social systems. Philos. Trans. R. Soc. B Biol. Sci. 2018, 373, 20170245. [Google Scholar] [CrossRef]
- Malambo, P.; Kengne, A.P.; De Villiers, A.; Lambert, E.V.; Puoane, T. Built Environment, Selected Risk Factors and Major Cardiovascular Disease Outcomes: A Systematic Review. PLoS ONE 2016, 11, e0166846. [Google Scholar] [CrossRef]
- Cardiovascular Disease. Available online: https://www.who.int/zh/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 27 November 2024).
- Dummer, T.J. Health geography: Supporting public health policy and planning. CMAJ Can. Med. Assoc. J. Medicale Can. 2008, 178, 1177–1180. [Google Scholar] [CrossRef]
- Mayer, J.D. Geography, ecology and emerging infectious diseases. Soc. Sci. Med. (1982) 2000, 50, 937–952. [Google Scholar] [CrossRef]
- Garber, M.D.; Benmarhnia, T.; de Nazelle, A.; Nieuwenhuijsen, M.; Rojas-Rueda, D. The epidemiologic case for urban health: Conceptualizing and measuring the magnitude of challenges and potential benefits. F1000Research 2025, 13, 950. [Google Scholar] [CrossRef] [PubMed]
- Breslow, L. Social ecological strategies for promoting healthy lifestyles. Am. J. Health Promot. 1996, 10, 253–257. [Google Scholar] [CrossRef]
- Bronfenbrenner, U. Toward an experimental ecology of human development. Am. Psychol. 1977, 32, 513. [Google Scholar] [CrossRef]
- McLeroy, K.R.; Bibeau, D.; Steckler, A.; Glanz, K. An ecological perspective on health promotion programs. Health Educ. Q. 1988, 15, 351–377. [Google Scholar] [CrossRef] [PubMed]
- Stokols, D. Establishing and maintaining healthy environments: Toward a social ecology of health promotion. Am. Psychol. 1992, 47, 6. [Google Scholar] [CrossRef] [PubMed]
- Putrik, P.; de Vries, N.K.; Mujakovic, S.; van Amelsvoort, L.; Kant, I.; Kunst, A.E.; van Oers, H.; Jansen, M. Living Environment Matters: Relationships Between Neighborhood Characteristics and Health of the Residents in a Dutch Municipality. J. Community Health 2015, 40, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Jing, Y.; Xu, X.; Zhang, X.; Liu, Y.; He, H.; Chen, F.; Liu, Y. Spatial scale analysis for the relationships between the built environment and cardiovascular disease based on multi-source data. Health Place 2023, 83, 103048. [Google Scholar] [CrossRef]
- Chandrabose, M.; den Braver, N.R.; Owen, N.; Sugiyama, T.; Hadgraft, N. Built Environments and Cardiovascular Health: REVIEW AND IMPLICATIONS. J. Cardiopulm. Rehabil. Prev. 2022, 42, 416–422. [Google Scholar] [CrossRef]
- Liu, M.; Patel, V.R.; Salas, R.N.; Rice, M.B.; Kazi, D.S.; Zheng, Z.; Wadhera, R.K. Neighborhood Environmental Burden and Cardiovascular Health in the US. JAMA Cardiol. 2024, 9, 153–163. [Google Scholar] [CrossRef]
- Hu, K.; Wang, S.; Fei, F.; Song, J.; Chen, F.; Zhao, Q.; Shen, Y.; Fu, J.; Zhang, Y.; Cheng, J.; et al. Modifying temperature-related cardiovascular mortality through green-blue space exposure. Environ. Sci. Ecotechnology 2024, 20, 100408. [Google Scholar] [CrossRef]
- Fletcher, D.H.; Likongwe, P.J.; Chiotha, S.S.; Nduwayezu, G.; Mallick, D.; Uddin Md, N.; Rahman, A.; Golovátina-Mora, P.; Lotero, L.; Bricker, S.; et al. Using demand mapping to assess the benefits of urban green and blue space in cities from four continents. Sci. Total Environ. 2021, 785, 147238. [Google Scholar] [CrossRef]
- Nieuwenhuijsen, M.J. Influence of urban and transport planning and the city environment on cardiovascular disease. Nat. Rev. Cardiol. 2018, 15, 432–438. [Google Scholar] [CrossRef]
- Makhlouf, M.H.E.; Motairek, I.; Chen, Z.; Nasir, K.; Deo, S.V.; Rajagopalan, S.; Al-Kindi, S.G. Neighborhood Walkability and Cardiovascular Risk in the United States. Curr. Probl. Cardiol. 2023, 48, 101533. [Google Scholar] [CrossRef] [PubMed]
- Griffin, B.A.; Eibner, C.; Bird, C.E.; Jewell, A.; Margolis, K.; Shih, R.; Slaughter, M.E.; Whitsel, E.A.; Allison, M.; Escarce, J.J. The relationship between urban sprawl and coronary heart disease in women. Health Place 2013, 20, 51–61. [Google Scholar] [CrossRef]
- Laverty, A.A.; Mindell, J.S.; Webb, E.A.; Millett, C. Active Travel to Work and Cardiovascular Risk Factors in the United Kingdom. Am. J. Prev. Med. 2013, 45, 282–288. [Google Scholar] [CrossRef]
- Ewing, R.; Cervero, R. Does Compact Development Make People Drive Less? The Answer is Yes. J. Am. Plan. Assoc. 2017, 83, 19–25. [Google Scholar] [CrossRef]
- Patterson, R.; Webb, E.; Hone, T.; Millett, C.; Laverty, A.A. Associations of Public Transportation Use With Cardiometabolic Health: A Systematic Review and Meta-Analysis. Am. J. Epidemiol. 2019, 188, 785–795. [Google Scholar] [CrossRef]
- Stevenson, M.; Thompson, J.; de Sá, T.H.; Ewing, R.; Mohan, D.; McClure, R.; Roberts, I.; Tiwari, G.; Giles-Corti, B.; Sun, X.; et al. Land use, transport, and population health: Estimating the health benefits of compact cities. Lancet 2016, 388, 2925–2935. [Google Scholar] [CrossRef]
- Kwan, S.C.; Ismail, R.; Ismail, N.H.; Mohamed, N. An ecological study of the relationship between urban built environment and cardiovascular hospital admissions (2004–2016) in an Asian developing country. Soc. Sci. Med. 2021, 276, 113868. [Google Scholar] [CrossRef]
- Tamosiunas, A.; Grazuleviciene, R.; Luksiene, D.; Dedele, A.; Reklaitiene, R.; Baceviciene, M.; Vencloviene, J.; Bernotiene, G.; Radisauskas, R.; Malinauskiene, V.; et al. Accessibility and use of urban green spaces, and cardiovascular health: Findings from a Kaunas cohort study. Environ. Health 2014, 13, 20. [Google Scholar] [CrossRef]
- Garg, P.K.; Platt, J.M.; Hirsch, J.A.; Hurvitz, P.; Rundle, A.; Biggs, M.L.; Psaty, B.M.; Moore, K.; Lovasi, G.S. Association of neighborhood physical activity opportunities with incident cardiovascular disease in the Cardiovascular Health Study. Health Place 2021, 70, 102596. [Google Scholar] [CrossRef] [PubMed]
- Alter, D.A.; Eny, K. The Relationship Between the Supply of Fast-food Chains and Cardiovascular Outcomes. Can. J. Public Health 2005, 96, 173–177. [Google Scholar] [CrossRef]
- Liu, Y.J.; Wang, X.Q.; Zhang, G.; Zhao, Q.; Cheng, Y.X.; Liu, S.; Yang, B.X.; Luo, D.; Liu, Q.; Zou, H. The association between food environments and cardiovascular disease outcomes: A systematic review. Heart Lung 2024, 68, 359–366. [Google Scholar] [CrossRef]
- Diez Roux, A.V.; Mujahid, M.S.; Hirsch, J.A.; Moore, K.; Moore, L.V. The Impact of Neighborhoods on CV Risk. Glob. Heart 2016, 11, 353–363. [Google Scholar] [CrossRef]
- Yitshak-Sade, M.; James, P.; Kloog, I.; Hart, J.E.; Schwartz, J.D.; Laden, F.; Lane, K.J.; Fabian, M.P.; Fong, K.C.; Zanobetti, A. Neighborhood Greenness Attenuates the Adverse Effect of PM2.5 on Cardiovascular Mortality in Neighborhoods of Lower Socioeconomic Status. Int. J. Environ. Res. Public Health 2019, 16, 814. [Google Scholar] [CrossRef]
- Malpezzi, S. Hedonic Pricing Models: A Selective and Applied Review. Wis.-Madison CULER Work. Pap. 2002, 10, 67–89. [Google Scholar] [CrossRef]
- Wei, H.; Chen, Y.; Chen, B.; Shi, S.; Tu, Y.; Xu, B. Built environments, communities, and housing price: A data-model integration approach. Appl. Geogr. 2024, 166, 103270. [Google Scholar] [CrossRef]
- National Center for Cardiovascular Diseases The Writing Committee of the Report on Cardiovascular Health Diseases in China. Report on Cardiovascular Health and Diseases in China 2023: An Updated Summary. Biomed. Environ. Sci. 2024, 37, 949–992. [Google Scholar] [CrossRef]
- Liu, M.; Meijer, P.; Lam, T.M.; Timmermans, E.J.; Grobbee, D.E.; Beulens, J.W.J.; Vaartjes, I.; Lakerveld, J. The built environment and cardiovascular disease: An umbrella review and meta-meta-analysis. Eur. J. Prev. Cardiol. 2023, 30, 1801–1827. [Google Scholar] [CrossRef] [PubMed]
- Yang, B.-Y.; Guo, Y.; Morawska, L.; Bloom, M.S.; Markevych, I.; Heinrich, J.; Dharmage, S.C.; Knibbs, L.D.; Lin, S.; Yim, S.H.-L.; et al. Ambient PM1 air pollution and cardiovascular disease prevalence: Insights from the 33 Communities Chinese Health Study. Environ. Int. 2019, 123, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Dalton, A.M.; Jones, A.P. Residential neighbourhood greenspace is associated with reduced risk of cardiovascular disease: A prospective cohort study. PLoS ONE 2020, 15, e0226524. [Google Scholar] [CrossRef] [PubMed]
- Thacher, J.D.; Poulsen, A.H.; Raaschou-Nielsen, O.; Hvidtfeldt, U.A.; Brandt, J.; Christensen, J.H.; Khan, J.; Levin, G.; Münzel, T.; Sørensen, M. Exposure to transportation noise and risk for cardiovascular disease in a nationwide cohort study from Denmark. Environ. Res. 2022, 211, 113106. [Google Scholar] [CrossRef] [PubMed]
- Koohsari, M.J.; McCormack, G.R.; Nakaya, T.; Oka, K. Neighbourhood built environment and cardiovascular disease: Knowledge and future directions. Nat. Rev. Cardiol. 2020, 17, 261–263. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.Y.; Choi, J.; Lee, S.; Choi, B.Y. Objectively Measured Built Environments and Cardiovascular Diseases in Middle-Aged and Older Korean Adults. Int. J. Environ. Res. Public Health 2021, 18, 1861. [Google Scholar] [CrossRef]
- Li, M.; Li, W.; Investigators, P. Associations of built environment characteristic using NEWS questionnaires with major cardiovascular diseases and all-cause mortality. Eur. Heart J. 2023, 44, ehad655.2573. [Google Scholar] [CrossRef]
- Patino, J.E.; Hong, A.; Duque, J.C.; Rahimi, K.; Zapata, S.; Lopera, V.M. Built environment and mortality risk from cardiovascular disease and diabetes in Medellín, Colombia: An ecological study. Landsc. Urban Plan. 2021, 213, 104126. [Google Scholar] [CrossRef]
- Pereira, G.; Foster, S.; Martin, K.; Christian, H.; Boruff, B.J.; Knuiman, M.; Giles-Corti, B. The association between neighborhood greenness and cardiovascular disease: An observational study. BMC Public Health 2012, 12, 466. [Google Scholar] [CrossRef]
- Brunsdon, C.; Fotheringham, A.S.; Charlton, M.E. Geographically Weighted Regression: A Method for Exploring Spatial Nonstationarity. Geogr. Anal. 1996, 28, 281–298. [Google Scholar] [CrossRef]
- Fotheringham, A.S.; Yang, W.; Kang, W. Multiscale geographically weighted regression (MGWR). Ann. Am. Assoc. Geogr. 2017, 107, 1247–1265. [Google Scholar] [CrossRef]
- Main Data Bulletin of the Seventh National Population Census in Xixiangtang District, Nanning City. Available online: http://xxtq.gov.cn/sj/sjgb/t5032802.html (accessed on 28 March 2025).
- Shi, Q.; Liu, M.; Marinoni, A.; Liu, X. UGS-1m: Fine-grained urban green space mapping of 34 major cities in China based on the deep learning framework. Earth Syst. Sci. Data Discuss. 2022, 2022, 555–577. [Google Scholar] [CrossRef]
- Chen, Y.; Xu, C.; Ge, Y.; Zhang, X.; Zhou, Y.n. A 100 m gridded population dataset of China’s seventh census using ensemble learning and big geospatial data. Earth Syst. Sci. Data 2024, 16, 3705–3718. [Google Scholar] [CrossRef]
- Li, X.; Zhou, L.; Liu, X.; Dun, Q.; Ma, L.; Zou, Y. Community built environment and the associated ischemic heart disease risk: Evidence from multi-source data in Wuhan, China. J. Transp. Health 2022, 25, 101371. [Google Scholar] [CrossRef]
- ŞENER, R.; Türk, T. Spatiotemporal analysis of cardiovascular disease mortality with geographical information systems. Appl. Spat. Anal. Policy 2021, 14, 929–945. [Google Scholar] [CrossRef]
- Li, Z.; Shang, Y.; Zhao, G.; Yang, M. Exploring the multiscale relationship between the built environment and the metro-oriented dockless bike-sharing usage. Int. J. Environ. Res. Public Health 2022, 19, 2323. [Google Scholar] [CrossRef] [PubMed]
- Mansour, S.; Al Kindi, A.; Al-Said, A.; Al-Said, A.; Atkinson, P. Sociodemographic determinants of COVID-19 incidence rates in Oman: Geospatial modelling using multiscale geographically weighted regression (MGWR). Sustain. Cities Soc. 2021, 65, 102627. [Google Scholar] [CrossRef] [PubMed]
- Fotheringham, A.S.; Charlton, M.E.; Brunsdon, C. Geographically weighted regression: A natural evolution of the expansion method for spatial data analysis. Environ. Plan. A 1998, 30, 1905–1927. [Google Scholar] [CrossRef]
- Oshan, T.M.; Li, Z.; Kang, W.; Wolf, L.J.; Fotheringham, A.S. mgwr: A Python implementation of multiscale geographically weighted regression for investigating process spatial heterogeneity and scale. ISPRS Int. J. Geo-Inf. 2019, 8, 269. [Google Scholar] [CrossRef]
- Carnegie, E.R.; Inglis, G.; Taylor, A.; Bak-Klimek, A.; Okoye, O. Is Population Density Associated with Non-Communicable Disease in Western Developed Countries? A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 2638. [Google Scholar] [CrossRef] [PubMed]
- Chandrabose, M.; Owen, N.; Giles-Corti, B.; Turrell, G.; Carver, A.; Sugiyama, T. Urban Densification and 12-Year Changes in Cardiovascular Risk Markers. J. Am. Heart Assoc. 2019, 8, e013199. [Google Scholar] [CrossRef]
- Su, J.G.; Apte, J.S.; Lipsitt, J.; Garcia-Gonzales, D.A.; Beckerman, B.S.; de Nazelle, A.; Texcalac-Sangrador, J.L.; Jerrett, M. Populations potentially exposed to traffic-related air pollution in seven world cities. Environ. Int. 2015, 78, 82–89. [Google Scholar] [CrossRef]
- Borck, R.; Schrauth, P. Population density and urban air quality. Reg. Sci. Urban Econ. 2021, 86, 103596. [Google Scholar] [CrossRef]
- Vallée, A. Association between socio-economic status and estimated atherosclerotic cardiovascular disease risk: Results from a middle-aged population-based study. Public Health 2023, 221, 1–9. [Google Scholar] [CrossRef]
- Dragano, N.; Bobak, M.; Wege, N.; Peasey, A.; Verde, P.E.; Kubinova, R.; Weyers, S.; Moebus, S.; Möhlenkamp, S.; Stang, A.; et al. Neighbourhood socioeconomic status and cardiovascular risk factors: A multilevel analysis of nine cities in the Czech Republic and Germany. BMC Public Health 2007, 7, 255. [Google Scholar] [CrossRef]
- Ye, X.; Tan, H.; Zhang, Y.; Zhang, L.; Zhang, Z. Research on Convenience Index of Urban Life Based on POI Data. J. Phys. Conf. Ser. 2020, 1646, 012073. [Google Scholar] [CrossRef]
- Chen, X.; Wang, N.; Tang, H. Influence of High-Density Community Spaces on the Walking Activity of Older Adults: A Case Study of Macau Peninsula. Buildings 2025, 15, 1505. [Google Scholar] [CrossRef]
- Rydin, Y.; Bleahu, A.; Davies, M.; Dávila, J.D.; Friel, S.; De Grandis, G.; Groce, N.; Hallal, P.C.; Hamilton, I.; Howden-Chapman, P.; et al. Shaping cities for health: Complexity and the planning of urban environments in the 21st century. Lancet 2012, 379, 2079–2108. [Google Scholar] [CrossRef] [PubMed]
- Daniel, M.; Paquet, C.; Auger, N.; Zang, G.; Kestens, Y. Association of fast-food restaurant and fruit and vegetable store densities with cardiovascular mortality in a metropolitan population. Eur. J. Epidemiol. 2010, 25, 711–719. [Google Scholar] [CrossRef]
- Victor, A.; Silva, R.d.C.R.; Silva, N.d.J.; Ferreira, A.; Barreto, M.L.; Campello, T. Influence of Unhealthy Food Environment on Premature Cardiovascular Disease Mortality in Brazil: An Ecologic Approach. Am. J. Prev. Med. 2023, 64, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Srour, B.; Fezeu, L.K.; Kesse-Guyot, E.; Allès, B.; Méjean, C.; Andrianasolo, R.M.; Chazelas, E.; Deschasaux, M.; Hercberg, S.; Galan, P. Ultra-processed food intake and risk of cardiovascular disease: Prospective cohort study (NutriNet-Santé). BMJ (Clin. Res. Ed.) 2019, 365, l1451. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Liu, S.; Li, M.; He, X.; Zhou, C. The Effect of High-Density Built Environments on Elderly Individuals’ Physical Health: A Cross-Sectional Study in Guangzhou, China. Int. J. Environ. Res. Public Health 2021, 18, 10250. [Google Scholar] [CrossRef]
- Ermagun, A.; Levinson, D. “Transit makes you short”: On health impact assessment of transportation and the built environment. J. Transp. Health 2017, 4, 373–387. [Google Scholar] [CrossRef]
- Lin, H.; Zhang, X.; Hu, Y.; Zhang, S. Unacknowledged health costs of subway transportation: Commuting time dominant environmental inequality in PM2.5 exposure. J. Transp. Health 2024, 38, 101865. [Google Scholar] [CrossRef]
- Liu, W.-T.; Ma, C.-M.; Liu, I.J.; Han, B.-C.; Chuang, H.-C.; Chuang, K.-J. Effects of commuting mode on air pollution exposure and cardiovascular health among young adults in Taipei, Taiwan. Int. J. Hyg. Environ. Health 2015, 218, 319–323. [Google Scholar] [CrossRef]
- Makram, O.M.; Nwana, N.; Nicolas, J.C.; Gullapelli, R.; Pan, A.; Bose, B.; Parekh, T.; Al-Kindi, S.; Yahya, T.; Hagan, K. Favorable neighborhood walkability is associated with lower burden of cardiovascular risk factors among patients within an integrated health system: The Houston Methodist Learning Health System Outpatient Registry. Curr. Probl. Cardiol. 2023, 48, 101642. [Google Scholar] [CrossRef] [PubMed]
- de Courrèges, A.; Occelli, F.; Muntaner, M.; Amouyel, P.; Meirhaeghe, A.; Dauchet, L. The relationship between neighbourhood walkability and cardiovascular risk factors in northern France. Sci. Total Environ. 2021, 772, 144877. [Google Scholar] [CrossRef]
- Chen, X.; Peng, S.; Liang, W.; Gan, S.; Xu, Y.; Xiang, H. Association between community walkability and hypertension: Evidence from the Wuhan Chronic Disease Cohort Study. Environ. Res. 2024, 263, 120071. [Google Scholar] [CrossRef]
- Howell, N.A.; Tu, J.V.; Moineddin, R.; Chu, A.; Booth, G.L. Association Between Neighborhood Walkability and Predicted 10-Year Cardiovascular Disease Risk: The CANHEART (Cardiovascular Health in Ambulatory Care Research Team) Cohort. J. Am. Heart Assoc. 2019, 8, e013146. [Google Scholar] [CrossRef]
- Sarkar, C.; Webster, C.; Gallacher, J. Association between adiposity outcomes and residential density: A full-data, cross-sectional analysis of 419 562 UK Biobank adult participants. Lancet Planet. Health 2017, 1, e277–e288. [Google Scholar] [CrossRef]
- Chiu, M.; Rezai, M.-R.; Maclagan, L.C.; Austin, P.C.; Shah, B.R.; Redelmeier, D.A.; Tu, J.V. Moving to a Highly Walkable Neighborhood and Incidence of Hypertension: A Propensity-Score Matched Cohort Study. Environ. Health Perspect. 2016, 124, 754–760. [Google Scholar] [CrossRef]
- Li, Y.; Mallinson, P.A.C.; Bhan, N.; Turner, C.; Bhogadi, S.; Sharma, C.; Aggarwal, A.; Kulkarni, B.; Kinra, S. Neighborhood physical food environment and cardiovascular risk factors in India: Cross-sectional evidence from APCAPS. Environ. Int. 2019, 132, 105108. [Google Scholar] [CrossRef] [PubMed]
- Sigala, E.G.; Chrysohoou, C.; Barkas, F.; Liberopoulos, E.; Sfikakis, P.P.; Faka, A.; Tsioufis, C.; Pitsavos, C.; Panagiotakos, D. The interplay between sex, lifestyle factors and built environment on 20-year cardiovascular disease incidence; the ATTICA study (2002–2022). Front. Cardiovasc. Med. 2025, 11, 1467564. [Google Scholar] [CrossRef] [PubMed]
- Paquet, C.; Orschulok, T.P.; Coffee, N.T.; Howard, N.J.; Hugo, G.; Taylor, A.W.; Adams, R.J.; Daniel, M. Are accessibility and characteristics of public open spaces associated with a better cardiometabolic health? Landsc. Urban Plan. 2013, 118, 70–78. [Google Scholar] [CrossRef]
- Zhong, J.; Liu, W.; Niu, B.; Lin, X.; Deng, Y. Role of built environments on physical activity and health promotion: A review and policy insights. Front. Public Health 2022, 10, 950348. [Google Scholar] [CrossRef]
- Ngom, R.; Gosselin, P.; Blais, C.; Rochette, L. Type and Proximity of Green Spaces Are Important for Preventing Cardiovascular Morbidity and Diabetes—A Cross-Sectional Study for Quebec, Canada. Int. J. Environ. Res. Public Health 2016, 13, 423. [Google Scholar] [CrossRef]
- Labib, S.; Lindley, S.; Huck, J.J. Spatial dimensions of the influence of urban green-blue spaces on human health: A systematic review. Environ. Res. 2020, 180, 108869. [Google Scholar] [CrossRef] [PubMed]
- Palacios, J.; Eichholtz, P.; Kok, N.; Aydin, E. The impact of housing conditions on health outcomes. Real Estate Econ. 2021, 49, 1172–1200. [Google Scholar] [CrossRef]
- Grewal, A.; Hepburn, K.J.; Lear, S.A.; Adshade, M.; Card, K.G. The impact of housing prices on residents’ health: A systematic review. BMC Public Health 2024, 24, 931. [Google Scholar] [CrossRef] [PubMed]
- Sims, M.; Kershaw, K.N.; Breathett, K.; Jackson, E.A.; Lewis, L.M.; Mujahid, M.S.; Suglia, S.F.; FAHA On behalf of the American Heart Association Council on Epidemiology and Prevention and Council on Quality of Care and Outcomes Research. Importance of Housing and Cardiovascular Health and Well-Being: A Scientific Statement From the American Heart Association. Circ. Cardiovasc. Qual. Outcomes 2020, 13, e000089. [Google Scholar] [CrossRef]
| Variable | Definition | Abbreviation | Mean | Std. |
|---|---|---|---|---|
| Number of Cardiovascular Cases | Total number of cardiovascular cases in each community (persons) | NCC | 61.95 | 98.78 |
| Population Density | Population density within the residential community, calculated based on China’s 100 m census grid data (10,000 persons/km2) | PD | 3.12 | 1.22 |
| Building Density | Ratio of total building area to community area (ratio, 0–1) | BD | 0.26 | 0.1 |
| Road Network Density | Total road length within the community divided by community area (km/km2) | RND | 9.73 | 4 |
| Land Use Mix Entropy | Land use mix represented by entropy index (ratio, 0–1) | LUME | 0.23 | 0.04 |
| Number of Unhealthy Food Outlets | Number of convenience stores (including OK convenience stores) within a 500 m buffer zone around the community (count) | NUFO | 44.95 | 27.84 |
| Number of Healthy Food Outlets | Number of vegetable markets, fruit markets, and integrated markets within a 500 m buffer zone (count) | NHFO | 33.99 | 20.4 |
| Number of Recreational Facilities | Number of sports venues, swimming pools, chess rooms, fitness centers, etc., within a 500 m buffer zone (count) | NRF | 13.74 | 10.38 |
| Number of Public Transport Stations | Number of bus stops and metro stations within a 500 m buffer zone (count) | NPTS | 4.78 | 3.07 |
| Facility POI Density | Ratio of the number of various POI points to the community area (POIs/km2) | FPOI | 1607.58 | 900.3 |
| Community Green Space Ratio | Ratio of total green space area to community area (%) | CGR | 13.63 | 8.07 |
| Distance to Nearest Park or Square | Distance from the community to the nearest park or square (m) | DNPS | 648.93 | 461.72 |
| Distance to Nearest Bus Stop | Distance from the community to the nearest bus stop (m) | DBS | 244.23 | 124.31 |
| Distance to Nearest Metro Station | Distance from the community to the nearest metro entrance (m) | DMS | 762.68 | 434.21 |
| Average Community Housing Price | Average second-hand housing price within the community (CNY/m2) | ACHP | 7019.84 | 1117.32 |
| Variable | Summary Statistics | Multicollinearity Test | Spatial Autocorrelation | ||||
|---|---|---|---|---|---|---|---|
| Mean | Std. | Tolerance | VIF | Moran’s I | Z-Value | p-Value | |
| Number of Cardiovascular Cases | 61.950 | 98.780 | 0.274 | 3.654 | 0.280 | 4.984 | 0.000 |
| Population Density | 3.120 | 1.217 | 0.345 | 2.900 | 0.358 | 5.707 | 0.000 |
| Building Density | 0.26 | 0.099 | 0.648 | 1.544 | 0.214 | 3.512 | 0.000 |
| Road Network Density | 9.730 | 3.998 | 0.420 | 2.381 | 0.208 | 3.443 | 0.001 |
| Land Use Mix Entropy | 0.230 | 0.044 | 0.421 | 2.375 | 0.083 | 1.496 | 0.135 * |
| Number of Unhealthy Food Outlets | 44.950 | 27.835 | 0.444 | 2.254 | 0.430 | 6.930 | 0.000 |
| Number of Healthy Food Outlets | 33.990 | 20.400 | 0.511 | 1.958 | 0.338 | 5.432 | 0.000 |
| Number of Recreational Facilities | 13.740 | 10.379 | 0.611 | 1.637 | 0.398 | 6.426 | 0.000 |
| Number of Public Transport Stations | 4.780 | 3.070 | 0.202 | 4.945 | 0.304 | 4.973 | 0.000 |
| Facility POI Density | 1607.580 | 900.300 | 0.537 | 1.862 | 0.124 | 2.127 | 0.033 |
| Community Green Space Ratio | 13.630 | 8.070 | 0.723 | 1.383 | 0.156 | 2.614 | 0.009 |
| Distance to Nearest Park or Square | 648.930 | 461.720 | 0.656 | 1.524 | 0.312 | 5.143 | 0.000 |
| Distance to Nearest Bus Stop | 244.230 | 124.310 | 0.617 | 1.622 | 0.101 | 1.773 | 0.076 * |
| Distance to Nearest Metro Station | 762.680 | 434.210 | 0.600 | 1.665 | 0.530 | 8.382 | 0.000 |
| Average Community Housing Price | 7019.840 | 1117.320 | 0.274 | 3.654 | 0.651 | 10.543 | 0.000 |
| Model | R2 | Adjusted R2 | AICc | RSS | Moran’s I of Residuals for Each Model | ||
|---|---|---|---|---|---|---|---|
| Moran’s I | Z Value | p Value | |||||
| OLS | 0.336 | 0.212 | 928.057 | 62.693 | −0.023 | −0.173 | 0.863 |
| GWR | 0.495 | 0.292 | 231.674 | 38.899 | −0.066 | −0.981 | 0.327 |
| MGWR | 0.532 | 0.348 | 224.348 | 36.065 | −0.058 | −0.832 | 0.405 |
| Bandwidths | OLS | GWR | MGWR |
|---|---|---|---|
| Intercept | -- | 74 | 55 |
| Road Network Density | 72 (93.50%) | ||
| Number of Public Transport Stations | 72 (93.50%) | ||
| Distance to Nearest Metro Station | 54 (70.13%) | ||
| Other Built Environment Factors | 76 (98.70%) |
| Variable | Mean | Std. | Min | Median | Max | Number of Significant Samples | Proportion (%) |
|---|---|---|---|---|---|---|---|
| Intercept | 0.057 | 0.225 | −0.267 | 0.016 | 0.391 | 27 | 35.06 |
| Population Density | 0.354 | 0.017 | 0.31 | 0.36 | 0.376 | 77 | 100.00 |
| Building Density | −0.227 | 0.054 | −0.316 | −0.234 | −0.151 | 29 | 37.66 |
| Road Network Density | −0.134 | 0.096 | −0.315 | −0.105 | −0.008 | 22 | 28.57 |
| Number of Unhealthy Food Outlets | 0.253 | 0.022 | 0.21 | 0.262 | 0.279 | 45 | 58.44 |
| Number of Healthy Food Outlets | −0.22 | 0.034 | −0.273 | −0.224 | −0.146 | 24 | 31.17 |
| Number of Recreational Facilities | 0.179 | 0.024 | 0.136 | 0.181 | 0.22 | 0 | 0.00 |
| Number of Public Transport Stations | −0.27 | 0.144 | −0.565 | −0.179 | −0.141 | 29 | 37.66 |
| Facility POI Density | −0.402 | 0.032 | −0.452 | −0.405 | −0.332 | 77 | 100.00 |
| Community Green Space Ratio | −0.149 | 0.024 | −0.196 | −0.146 | −0.113 | 0 | 0.00 |
| Distance to Nearest Park or Square | −0.01 | 0.05 | −0.131 | 0.016 | 0.025 | 0 | 0.00 |
| Distance to Nearest Metro Station | −0.22 | 0.069 | −0.345 | −0.208 | −0.104 | 32 | 41.56 |
| Average Community Housing Price | 0.032 | 0.044 | −0.019 | 0.012 | 0.133 | 0 | 0.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the International Society for Photogrammetry and Remote Sensing. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Deng, S.; Zhu, S.; Chen, X.; Liang, J.; Zheng, R. A Multi-Scale Geographically Weighted Regression Approach to Understanding Community-Built Environment Determinants of Cardiovascular Disease: Evidence from Nanning, China. ISPRS Int. J. Geo-Inf. 2025, 14, 362. https://doi.org/10.3390/ijgi14090362
Deng S, Zhu S, Chen X, Liang J, Zheng R. A Multi-Scale Geographically Weighted Regression Approach to Understanding Community-Built Environment Determinants of Cardiovascular Disease: Evidence from Nanning, China. ISPRS International Journal of Geo-Information. 2025; 14(9):362. https://doi.org/10.3390/ijgi14090362
Chicago/Turabian StyleDeng, Shuguang, Shuyan Zhu, Xueying Chen, Jinlong Liang, and Rui Zheng. 2025. "A Multi-Scale Geographically Weighted Regression Approach to Understanding Community-Built Environment Determinants of Cardiovascular Disease: Evidence from Nanning, China" ISPRS International Journal of Geo-Information 14, no. 9: 362. https://doi.org/10.3390/ijgi14090362
APA StyleDeng, S., Zhu, S., Chen, X., Liang, J., & Zheng, R. (2025). A Multi-Scale Geographically Weighted Regression Approach to Understanding Community-Built Environment Determinants of Cardiovascular Disease: Evidence from Nanning, China. ISPRS International Journal of Geo-Information, 14(9), 362. https://doi.org/10.3390/ijgi14090362





