Measuring Spatial Accessibility to Hospitals of Acute Myocardial Infarction in Multi Period Scale: A Case Study in Shijingshan District, Beijing, China
Abstract
:1. Introduction
1.1. Study on the AMI Emergency Treatment
1.2. Study on the Hospital Accessibility
1.3. Web Mapping API
2. Materials and Methods
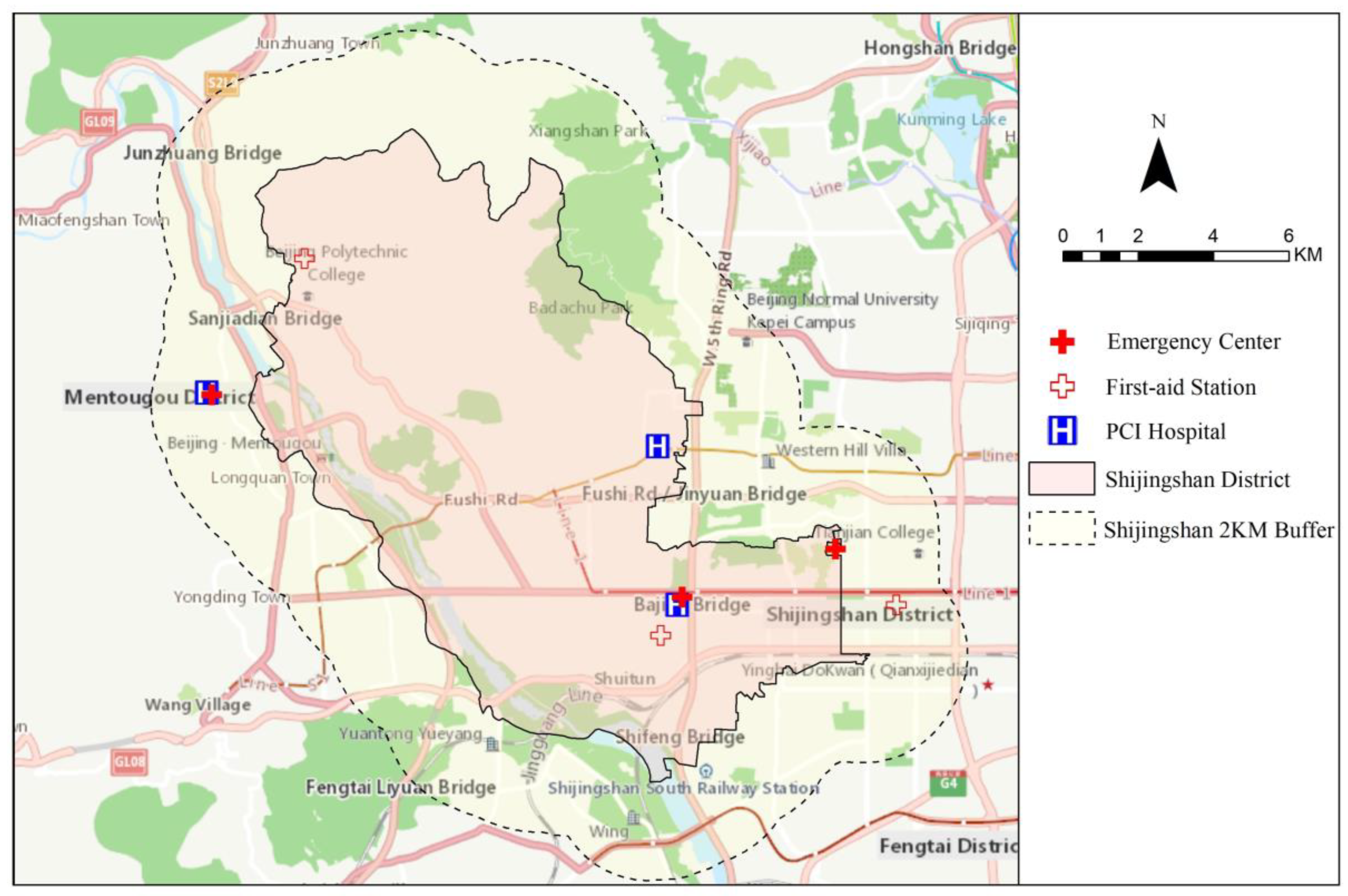
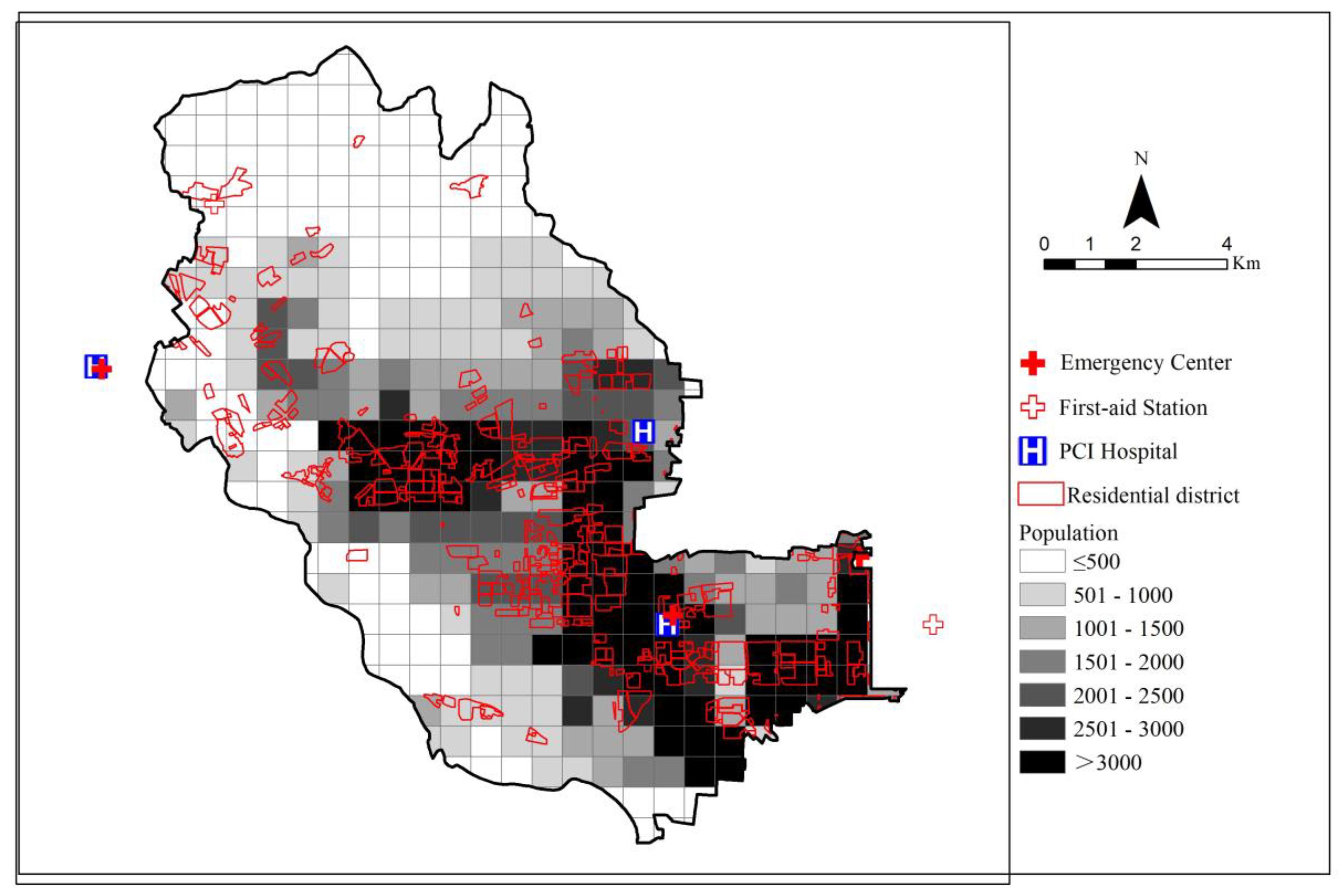
2.1. Overview of the Study Area
2.2. Data
2.2.1. Medical Facility Data
2.2.2. Travel Time Data
2.2.3. Demographic, Residential Area, and Administrative Division Data
2.2.4. Experimental Period
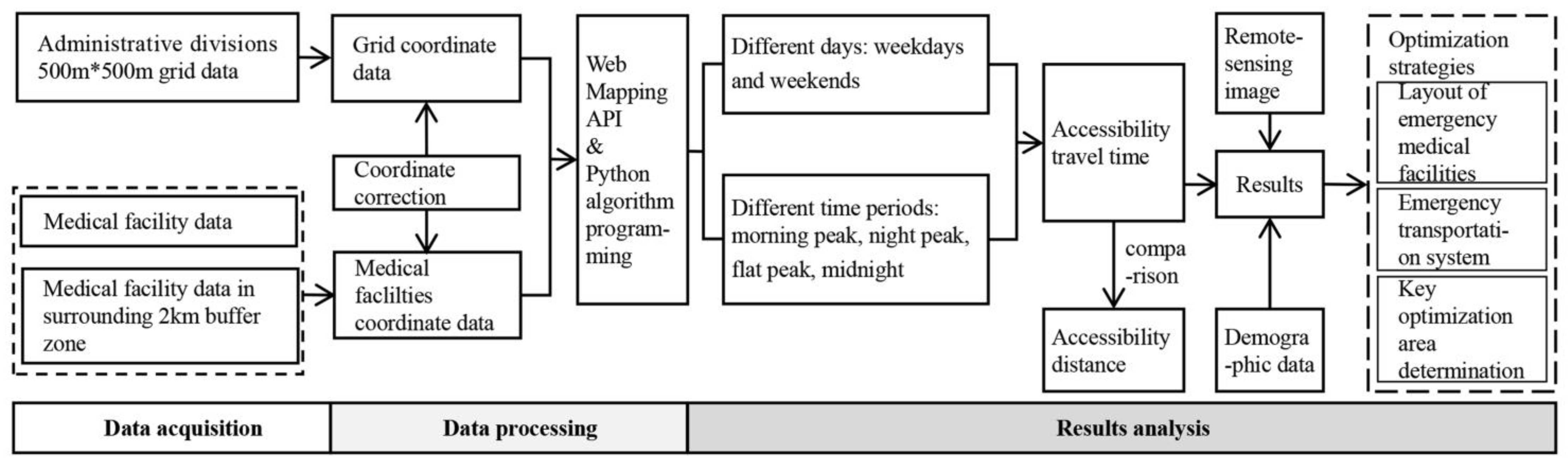
2.3. Method
2.3.1. A Framework for AMI Hospital Accessibility Measurement
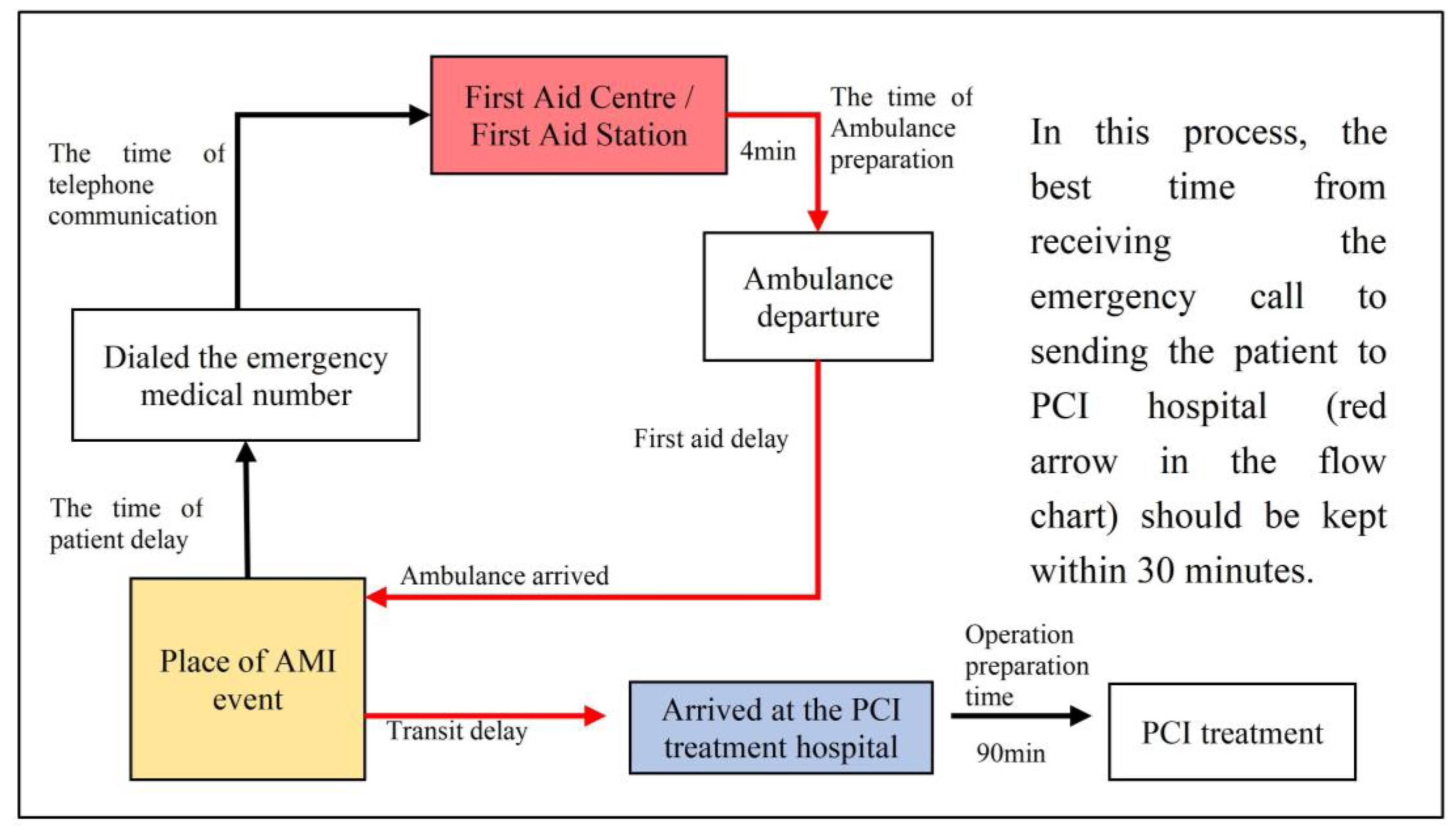
2.3.2. AMI Emergency Treatment Process
2.3.3. Measuring Spatial Accessibility to Hospitals
2.3.4. Propose Optimization Strategies Based on Demographic and Residential Area Data
3. Results
3.1. Analysis of the AMI Hospital Accessibility on Weekdays
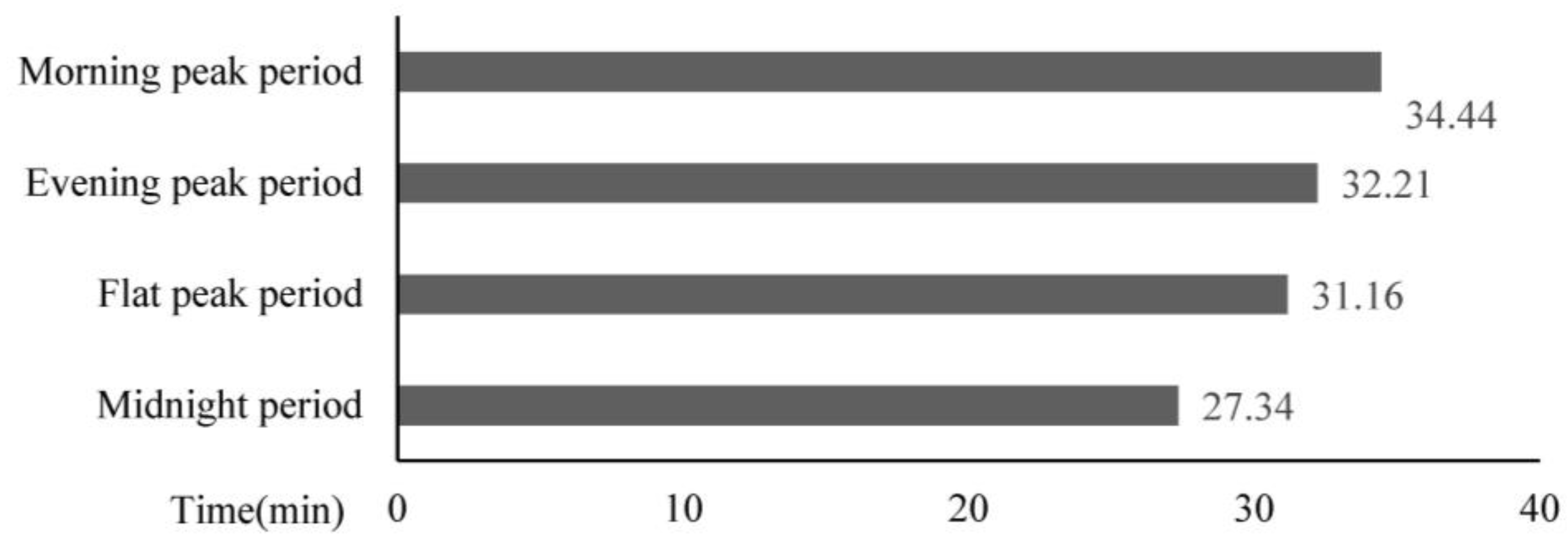
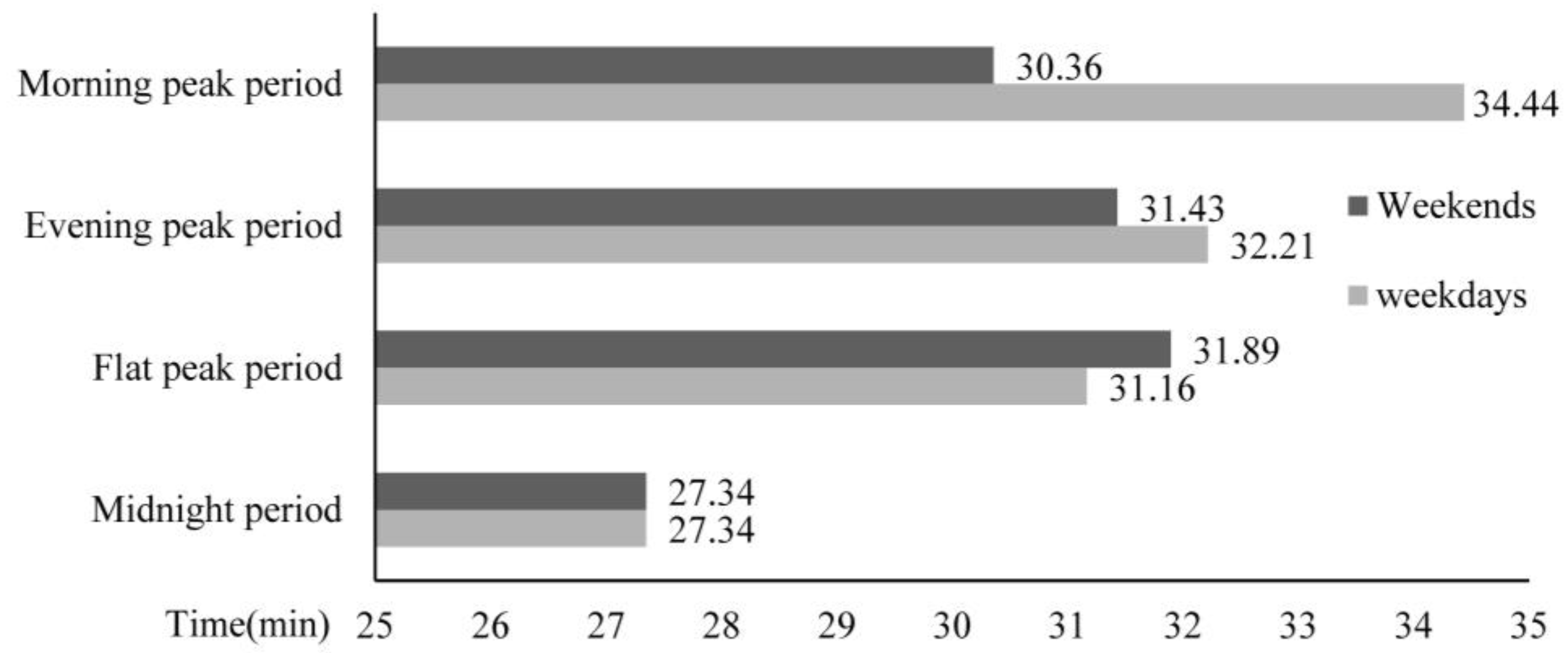
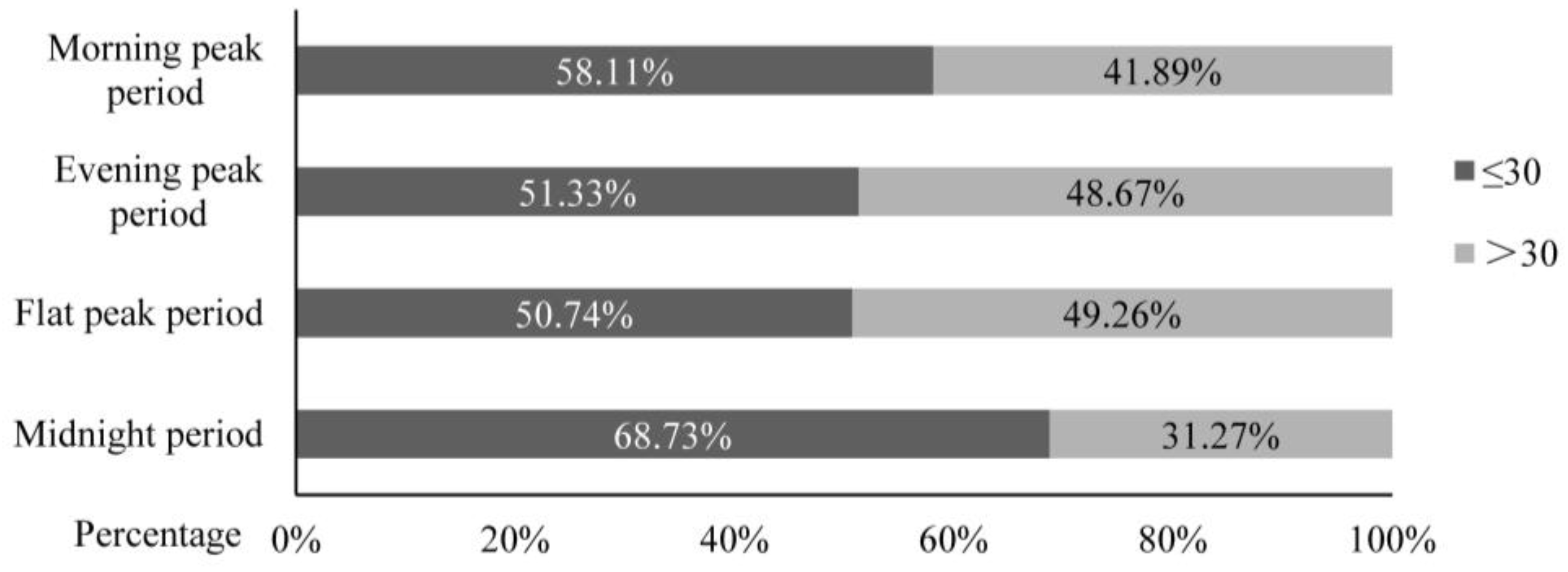
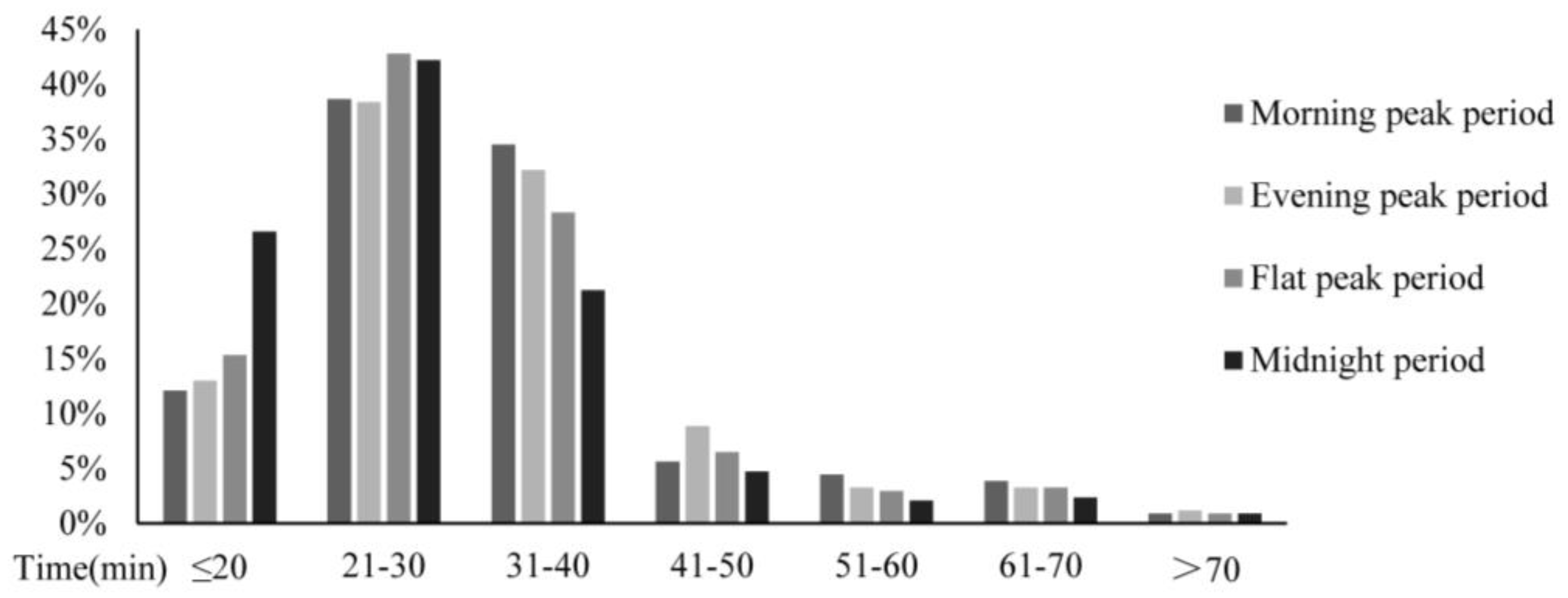
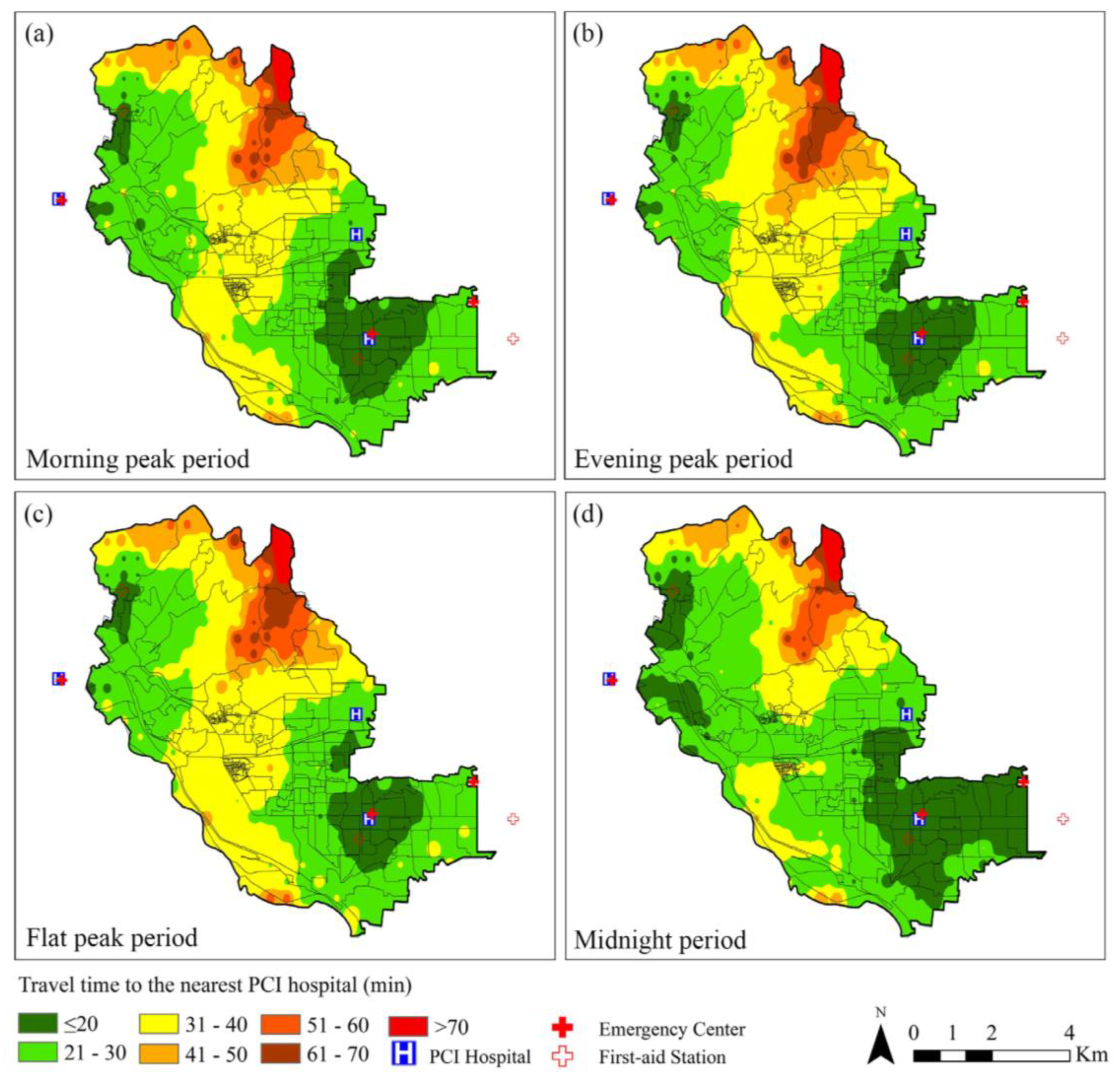
3.1.1. Analysis of AMI Accessibility Travel Time on Weekdays
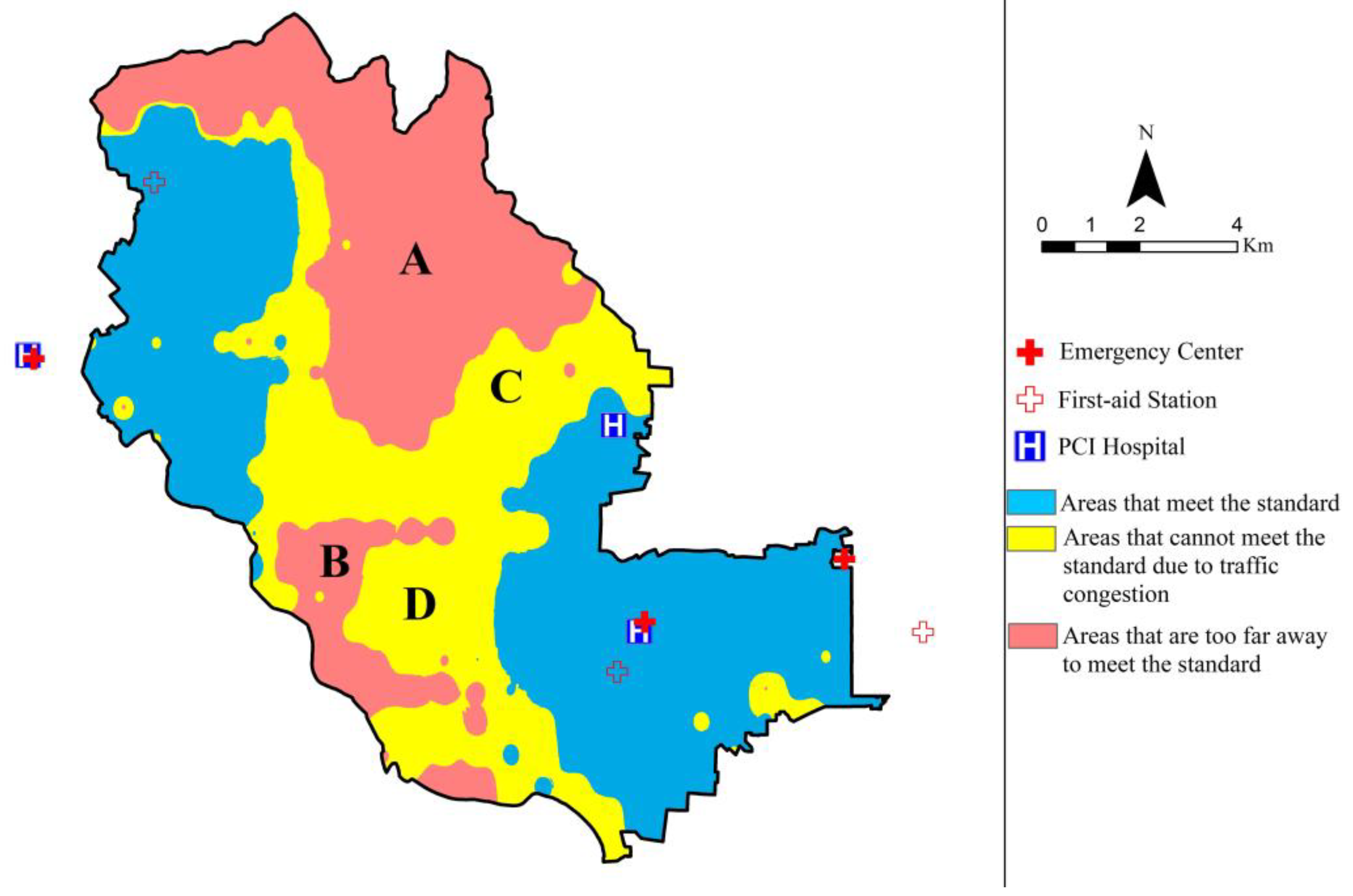
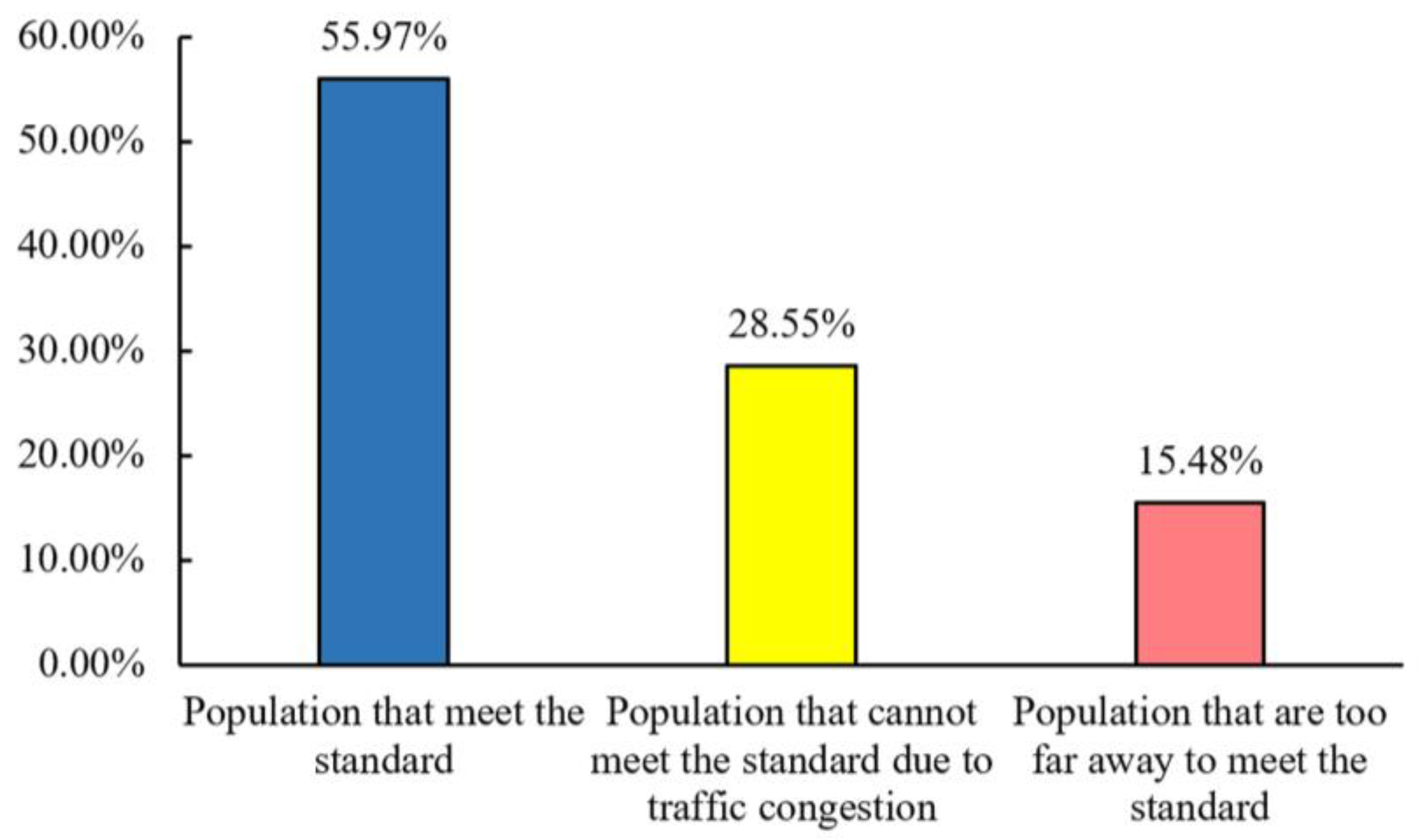
3.1.2. Spatial Pattern Analysis on Weekdays
3.2. Analysis of the AMI Hospital Accessibility on Weekends
3.2.1. Analysis of AMI Accessibility Travel Time on Weekends
3.2.2. Spatial Pattern Analysis on Weekends
3.3. Optimizing Strategies for AMI Hospital Accessibility
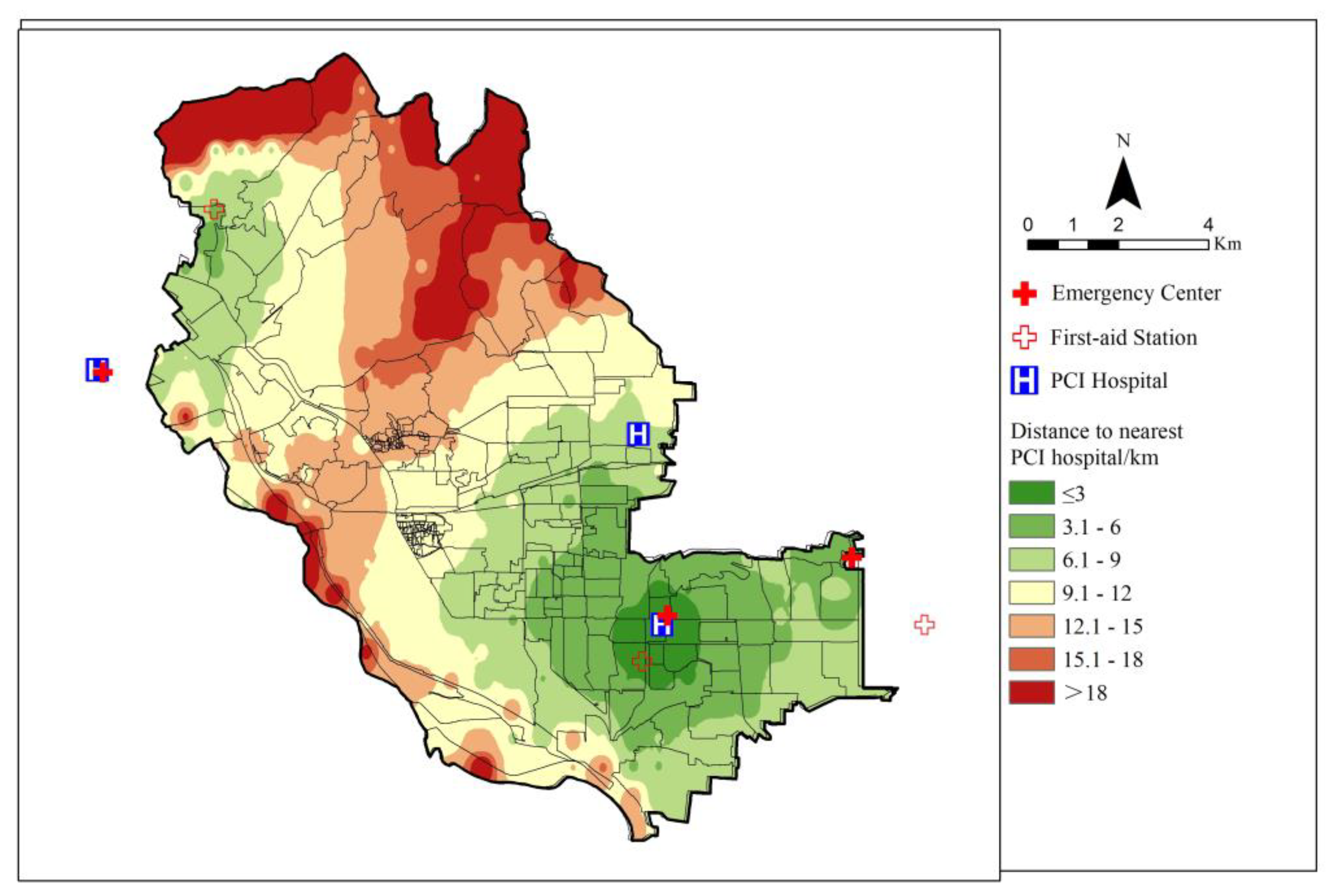
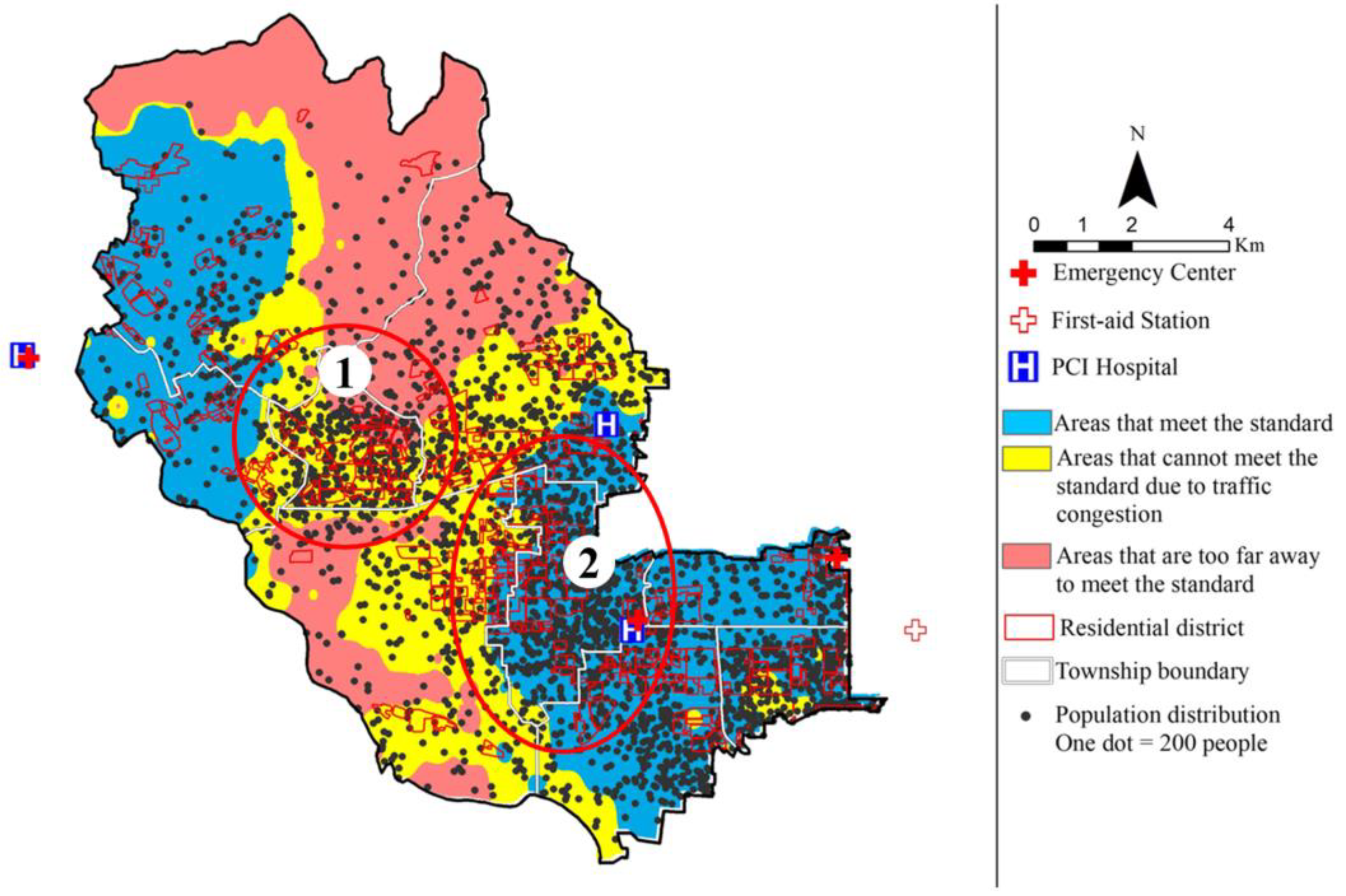
3.3.1. Optimization Strategy for the Layout of Emergency Medical Facilities
3.3.2. Optimization Strategy for the Emergency Transportation System
3.3.3. Key Optimization Area Determination Based on Demographic and Residential Area Data
4. Discussion
4.1. Influencing Factors of AMI Hospital Accessibility
4.2. Temporal and Spatial Distribution Differences of AMI Hospital Accessibility
4.3. Comparison of Analytical Methods with Existing Research Methods
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Center for Cardiovascular Diseases. Available online: https://www.nccd.org.cn/News/Information/Index/1089 (accessed on 29 November 2021).
- Boersma, E.; Mercado, N.; Poldermans, D.; Gardien, M.; Vos, J.; Simoons, M.L. Acute myocardial infarction. Lancet 2003, 361, 847–858. [Google Scholar] [CrossRef]
- Ding, S.; Chen, B. Rationality Assessment of the Spatial Distributions of Urban Medical Facility. J. Geo-Inf. Sci. 2017, 19, 185–196. [Google Scholar] [CrossRef]
- GBD 2016 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1260–1344. [Google Scholar] [CrossRef] [Green Version]
- Giuseppe, D.L.; Harry, S.; Jan, P.O.; Elliott, M.A. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: Every minute of delay counts. Circulation 2004, 109, 1223–1225. [Google Scholar] [CrossRef] [Green Version]
- ESC Scientific Document Group. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar] [CrossRef]
- Elliott, M.A. Bypassing the emergency department to improve the process of care for ST-elevation myocardial infarction: Necessary but not sufficient. Circulation 2013, 128, 322–324. [Google Scholar] [CrossRef] [Green Version]
- Shen, Y.-C.; Hsia, R.Y. Association Between Emergency Department Closure and Treatment, Access, and Health Outcomes Among Patients With Acute Myocardial Infarction. Circulation 2016, 134, 1595–1597. [Google Scholar] [CrossRef] [Green Version]
- Trifan, A.L.; Dragomir, L.; Anghele, M.; Elkan, E.M.; Munteanu, S.; Moscu, C.; Stoian, V.-I.; Telehuz, A.; Zlati, M.L.; Lungu, M.; et al. Assessment of Transportation by Air for Patients with Acute ST-Elevation Myocardial Infarction from Non-PCI Centers. Healthcare 2021, 9, 299. [Google Scholar] [CrossRef]
- Hansen, W.G. How accessibility shapes land-use. J. Am. Ins. Planners 1959, 25, 73–76. [Google Scholar] [CrossRef]
- Geurs, K.T.; Wee, B.V. Accessibility evaluation of land-use and transport strategies: Review and research directions. J. Transp. Geogr. 2004, 12, 127–140. [Google Scholar] [CrossRef]
- Wang, F. Measurement, Optimization, and Impact of Health Care Accessibility: A Methodological Review. Ann. Am. Assoc. Geogr. 2012, 102, 1104–1112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dalvi, M.Q.; Martin, K.M. The measurement of accessibility: Some preliminary results. Transportation 1976, 5, 17–42. [Google Scholar] [CrossRef]
- Zhengna, S.; Wen, C.; Qianjin, C.; Lei, Z. Measurement of Spatial Accessibility to Health Care Facilities and Defining Health Professional Shortage Areas Based on Improved Potential Model—A Case Study of Rudong County in Jiangsu Province. Sci.Geogr. Sin. 2010, 30, 213–219. [Google Scholar] [CrossRef]
- Penchansky, R.; Thomas, J.W. The concept of access: Definition and relationship to consumer satisfaction. Med. Care 1981, 19, 127–140. [Google Scholar] [CrossRef] [PubMed]
- Gary, H. A Literature Review of the Use of GIS-Based Measures of Access to Health Care Services. Health Serv. Outcome 2004, 5, 119–139. [Google Scholar] [CrossRef]
- Khan, A.A. An integrated approach to measuring potential spatial access to health care services. Socio Econ. Plan. Sci. 1992, 26, 275–287. [Google Scholar] [CrossRef]
- Dewulf, B.; Neutens, T.; De Weerdt, Y.; Van De Weghe, N. Accessibility to primary health care in Belgium: An evaluation of policies awarding financial assistance in shortage areas. BMC Fam. Pract. 2013, 14, 122. [Google Scholar] [CrossRef] [Green Version]
- Lovett, A.; Sunnenberg, G.; Haynes, R. Using GIS to assess accessibility to primary health care services. Public Health Pract. Opp. Pit. 2004, 2, 187–204. [Google Scholar]
- Hare, T.S.; Barcus, H. Geographical accessibility and Kentucky’s heart-related hospital services. Appl. Geogr. 2007, 27, 181–205. [Google Scholar] [CrossRef]
- Ting, H.-W.; Chien, T.-Y.; Lai, K.R.; Pan, R.-H.; Wu, K.-H.; Chen, J.-M.; Chan, C.-L. Differences in Spontaneous Intracerebral Hemorrhage Cases between Urban and Rural Regions of Taiwan: Big Data Analytics of Government Open Data. Int. J. Environ. Res. Public Health 2017, 14, 1548. [Google Scholar] [CrossRef] [Green Version]
- Wang, Z.; Nie, K. Measuring Spatial Patterns of Health Care Facilities and Their Relationships with Hypertension Inpatients in a Network-Constrained Urban System. Int. J. Environ. Res. Public Health 2019, 16, 3204. [Google Scholar] [CrossRef] [Green Version]
- Abu Bakar, M.A.; Samat, N.; Yaacob, N.S. Spatial accessibility to health care services among children with cerebral palsy in Johor, Peninsular Malaysia. Geospat. Health 2021, 16, 987. [Google Scholar] [CrossRef] [PubMed]
- Benevenuto, R.G.; Azevedo, I.C.C.; Caulfield, B. Assessing the spatial burden in health care accessibility of low-income families in rural Northeast Brazil. J. Transp. Health 2019, 14, 100595. [Google Scholar] [CrossRef]
- Siegel, M.; Koller, D.; Vogt, V.; Sundmacher, L. Developing a composite index of spatial accessibility across different health care sectors: A German example. Health Policy 2016, 120, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Lechowski, Ł.; Jasion, A. Spatial Accessibility of Primary Health Care in Rural Areas in Poland. Int. J. Environ. Res. Public Health 2021, 18, 9282. [Google Scholar] [CrossRef]
- Hundt, G.L.; Alzaroo, S.; Hasna, F.; Alsmeiran, M. The provision of accessible, acceptable health care in rural remote areas and the right to health: Bedouin in the North East region of Jordan. Soc. Sci. Med. 2012, 74, 36–43. [Google Scholar] [CrossRef]
- Pinto, A.; Köptcke, L.S.; David, R.; Kuper, H. A National Accessibility Audit of Primary Health Care Facilities in Brazil—Are People with Disabilities Being Denied Their Right to Health? Int. J. Environ. Res. Public Health 2021, 18, 2953. [Google Scholar] [CrossRef]
- Cheng, M.; Tao, L.; Huang, Y.L.a. Measuring Spatial Accessibility of Urban Medical Facilities: A Case Study in Changning District of Shanghai in China. Int. J. Environ. Res. Public Health 2021, 18, 9598. [Google Scholar] [CrossRef]
- Gao, F.; Jaffrelot, M.; Deguen, S. Measuring hospital spatial accessibility using the enhanced two-step floating catchment area method to assess the impact of spatial accessibility to hospital and non-hospital care on the length of hospital stay. BMC Health Serv. Res. 2021, 21, 1078. [Google Scholar] [CrossRef]
- Wang, X.; Yang, H.; Duan, Z.; Pan, J. Spatial accessibility of primary health care in China: A case study in Sichuan Province. Soc. Sci. Med. 2018, 209, 14–24. [Google Scholar] [CrossRef]
- Zhang, J.; Han, P.; Sun, Y.; Zhao, J.; Yang, L. Assessing Spatial Accessibility to Primary Health Care Services in Beijing, China. Int. J. Environ. Res. Public Health 2021, 18, 13182. [Google Scholar] [CrossRef] [PubMed]
- Kotavaara, O.; Nivala, A.; Lankila, T.; Huotari, T.; Delmelle, E.; Antikainen, H. Geographical accessibility to primary health care in Finland–Grid-based multimodal assessment. Appl. Geogr. 2021, 136, 102583. [Google Scholar] [CrossRef]
- Chen, W.; Cheng, L.; Chen, X.; Chen, J.; Cao, M. Measuring accessibility to health care services for older bus passengers: A finer spatial resolution. J. Transp. Geogr. 2021, 93, 103068. [Google Scholar] [CrossRef]
- Caviglia, M.; Dell’Aringa, M.; Putoto, G.; Buson, R.; Pini, S.; Youkee, D.; Jambai, A.; Vandy, M.J.; Rosi, P.; Hubloue, I.; et al. Improving Access to Healthcare in Sierra Leone: The Role of the Newly Developed National Emergency Medical Service. Int. J. Environ. Res. Public Health 2021, 18, 9546. [Google Scholar] [CrossRef] [PubMed]
- Langford, M.; Higgs, G.; Fry, R. Multi-modal two-step floating catchment area analysis of primary health care accessibility. Health Place 2016, 38, 70–81. [Google Scholar] [CrossRef] [PubMed]
- Andersen, R. A behavioral model of families’ use of health services. J. Hum. Resour. 1968, 7, 125. [Google Scholar]
- Yiannakoulias, N.; Bland, W.; Svenson, L.W. Estimating the effect of turn penalties and traffic congestion on measuring spatial accessibility to primary health care. Appl. Geogr. 2013, 39, 172–182. [Google Scholar] [CrossRef]
- Rong, P.; Zheng, Z.; Kwan, M.; Qin, Y. Evaluation of the spatial equity of medical facilities based on improved potential model and map service API: A case study in Zhengzhou, China. Appl. Geogr. 2020, 119, 102192. [Google Scholar] [CrossRef]
- Rosenblatt, M. Remarks on some nonparametric estimates of a density function. Ann. Math. Stat. 1956, 27, 832–837. [Google Scholar] [CrossRef]
- Yang, D.H.; Goerge, R.; Mullner, R. Comparing GIS-based methods of measuring spatial accessibility to health services. J. Med. Syst. 2006, 30, 23–32. [Google Scholar] [CrossRef]
- Fan, P.; Xu, L.; Yue, W.; Chen, J. Accessibility of public urban green space in an urban periphery: The case of Shanghai. Landsc. Urban Plan. 2016, 165, 177–192. [Google Scholar] [CrossRef]
- Wang, F.H.; Luo, W. Assessing spatial and non-spatial factors for healthcare access: Towards an integrated approach to defining health professional shortage areas. Health Place 2005, 11, 131–146. [Google Scholar] [CrossRef] [PubMed]
- Luo, W.; Wang, F. Measures of spatial accessibility to health care in a GIS environment: Synthesis and a case study in the chicago region. Environ. Plann. Plann. Des. 2003, 30, 865–884. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xing, L.; Liu, Y.; Wang, B.; Wang, Y.; Liu, H. An environmental justice study on spatial access to parks for youth by using an improved 2SFCA method in Wuhan, China. Cities 2020, 96, 102405. [Google Scholar] [CrossRef]
- Luo, W.; Qi, Y. An enhanced two-step floating catchment area (E2SFCA) method for measuring spatial accessibility to primary care physicians. Health Place 2009, 15, 1100–1107. [Google Scholar] [CrossRef]
- Wan, N.; Zou, B.; Sternberg, T. A three-step floating catchment area method for analyzing spatial access to health services. Int. J. Geogr. Inf. Sci. 2012, 26, 1073–1089. [Google Scholar] [CrossRef]
- Delamater, P.L. Spatial accessibility in suboptimally configured health care systems: A modified two-step floating catchment area (M2SFCA) metric. Health Place 2013, 24, 30–43. [Google Scholar] [CrossRef]
- Luo, W.; Whippo, T. Variable catchment sizes for the two-step floating catchment area (2SFCA) method. Health Place 2012, 18, 789–795. [Google Scholar] [CrossRef]
- Cheng, G.; Zeng, X.; Duan, L.; Lu, X.; Sun, H.; Jiang, T.; Li, Y. Spatial difference analysis for accessibility to high level hospitals based on travel time in Shenzhen, China. Habitat Int. 2016, 53, 485–494. [Google Scholar] [CrossRef] [Green Version]
- Liu, Z.; Yang, H.; Xiong, W.; Chen, G. Spatial accessibilities of medical services at county level based on optimized two-step floating catchment area method. Sci. Geogr. Sin. 2017, 5, 91–100. [Google Scholar] [CrossRef]
- Ye, C.; Hu, L.; Li, M. Urban green space accessibility changes in a high-density city: A case study of Macau from 2010 to 2015. J. Transp. Geogr. 2018, 66, 106–115. [Google Scholar] [CrossRef]
- Zhang, F.; Li, D.; Sherry, A.; Zhang, J. Assessing spatial disparities of accessibility to community-based service resources for Chinese older adults based on travel behavior: A city-wide study of nanjing, China. Habitat Int. 2019, 88, 101984. [Google Scholar] [CrossRef]
- Wu, H.-C.; Tseng, M.-H. Evaluating disparities in elderly community care resources: Using a geographic accessibility and inequality index. Int. J. Environ. Res. Public Health 2018, 15, 1353. [Google Scholar] [CrossRef] [Green Version]
- Xiao, Y.; Chen, X.; Li, Q.; Jia, P.; Li, L.; Chen, Z. Towards healthy China 2030: Modeling health care accessibility with patient referral. Soc. Sci. Med. 2021, 276, 113834. [Google Scholar] [CrossRef] [PubMed]
- Niu, Q.; Wang, Y.; Xia, Y.; Wu, H.; Tang, X. Detailed Assessment of the Spatial Distribution of Urban Parks According to Day and Travel Mode Based on Web Mapping API: A Case Study of Main Parks in Wuhan. Int. J. Environ. Res. Public Health 2018, 15, 1725. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, Y.; Li, Y.; Huang, Y.; Geng, E. Analysis of classification methods and activity characteristics of urban population based on social media data. J. Geo-Inf. Sci. 2017, 19, 1238–1244. [Google Scholar] [CrossRef]
- Wang, F.; Xu, Y. Estimating OD travel time matrix by Google Maps API: Implementation, advantages, and implications. Geogr. Inf. Sci. 2011, 17, 199–209. [Google Scholar] [CrossRef]
- Xu, M.; Xin, J.; Su, S.; Weng, M.; Cai, Z. Social inequalities of park accessibility in Shenzhen, China: The role of park quality, transport modes, and hierarchical socioeconomic characteristics. J. Transp. Geogr. 2017, 62, 38–50. [Google Scholar] [CrossRef]
- Zheng, Z.; Shen, W.; Li, Y.; Qin, Y.; Wang, L. Spatial equity of park green space using KD2SFCA and web map API: A case study of zhengzhou, China. Appl. Geogr. 2020, 123, 102310. [Google Scholar] [CrossRef]
- Xia, N.; Cheng, L.; Chen, S.; Wei, X.; Zong, W.; Li, M. Accessibility based on Gravity-Radiation model and Google Maps API: A case study in Australia. J. Transp. Geogr. 2018, 72, 178–190. [Google Scholar] [CrossRef]
- Zhou, X.; Kim, J. Social disparities in tree canopy and park accessibility: A case study of six cities in Illinois using GIS and remote sensing. Urban For. Urban Green. 2013, 12, 88–97. [Google Scholar] [CrossRef]
- Zheng, Z.; Xia, H.; Ambinakudige, S.; Qin, Y.; Li, Y.; Xie, Z.; Zhang, L.; Gu, H. Spatial Accessibility to Hospitals Based on Web Mapping API: An Empirical Study in Kaifeng, China. Sustainability 2019, 11, 1160. [Google Scholar] [CrossRef] [Green Version]
- Beijing Municipal Bureau Statistics. Available online: http://tjj.beijing.gov.cn/tjsj_31433/ (accessed on 29 November 2021).
- AutoNavi. Available online: https://report.amap.com/download_city.do (accessed on 29 November 2021).
- Beijing Transport Institute. Available online: https://www.bjtrc.org.cn/List/index/cid/7.html (accessed on 2 February 2022).
- Bondarenko, M.; Kerr, D.; Sorichetta, A.; Tatem, A.J. Census/Projection-Disaggregated Gridded Population Datasets for 189 Countries in 2020 Using Built-Settlement Growth Model (BSGM) Outputs; WorldPop. University of Southampton: Southampton, UK, 2020. [Google Scholar] [CrossRef]
- The People’s Government of Beijing Municipality. Available online: http://www.beijing.gov.cn/gongkai/shuju/sjjd/202105/t20210519_2392886.html (accessed on 2 February 2022).
- Beijing City Lab. Available online: https://www.beijingcitylab.com/ (accessed on 2 February 2022).
- Beijing Platform for Common Geospatial Information Services. Available online: https://beijing.tianditu.gov.cn/ (accessed on 2 February 2022).
- Xiao, H.; Zhang, H.; Wang, D.; Shen, C.; Naghavi, M. Impact of smoke-free legislation on acute myocardial infarction and stroke mortality: Tianjin, China, 2007–2015. Tob. Control 2019, 29, 54477. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jia, E.Z.; Xu, Z.X.; Cai, H.Z.; Guo, C.Y.; Li, L.; Zhu, T.B.; Wang, L.S.; Cao, K.J.; Ma, W.Z.; Yang, Z.J. Time distribution of the onset of chest pain in subjects with acute ST-Elevation myocardial infarction: An Eight-Year, Single-Center study in china. PLoS ONE 2012, 7, 32478. [Google Scholar] [CrossRef]
- Hopstock, L.A.; Wilsgaard, T.; Njolstad, I.; Mannsverk, J.; Mathiesen, E.B.; Lochen, M.L.; Bonaa, K.H. Seasonal variation in incidence of acute myocardial infarction in a sub-Arctic population: The Troms Study 1974–2004. Eur. J. Cardiov. Prev. Rehabil. 2011, 18, 320–325. [Google Scholar] [CrossRef]
- Manfredini, R.; Boari, B.; Smolensky, M.H.; Salmi, R.; Gallerani, M.; Guerzoni, F.; Guerra, V.; Malagoni, A.M.; Manfredini, F. Seasonal Variation in Onset of Myocardial Infarction—a 7-year single-center study in Italy. Chronobiol. Int. 2005, 22, 1121–1135. [Google Scholar] [CrossRef]
- Marchant, B.; Ranjadayalan, K.; Stevenson, R.; Wilkinson, P.; Timmis, A.D. Circadian and seasonal factors in the pathogenesis of acute myocardial infarction: The influence of environmental temperature. Heart 1993, 69, 385–387. [Google Scholar] [CrossRef]
- Marshall, R.J.; Robert, S.; Paul, B. An analysis of the seasonal variation of coronary heart disease and respiratory disease mortality in new zealand. Int. J. Epidemiol. 1988, 17, 325–331. [Google Scholar] [CrossRef] [Green Version]
- Mcelroy, J.A.; Remington, P.L.; Trentham-Dietz, A.; Robert, S.A.; Newcomb, P.A. Geocoding addresses from a large population-based study: Lessons learned. Epidemiology 2003, 14, 399–407. [Google Scholar] [CrossRef]
- Watson, D.F.; Philip, G.M. A refinement of inverse distance weighted interpolation. Geoprocessing 1985, 2, 315–327. [Google Scholar]
- Philip, G.M.; Watson, D.F. A Precise method for determining countoured surfaces. APPEA J. 1982, 22, 205–212. [Google Scholar] [CrossRef]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Su, Y.; Wang, J.; Wang, J.; Wang, G. Measuring Spatial Accessibility to Hospitals of Acute Myocardial Infarction in Multi Period Scale: A Case Study in Shijingshan District, Beijing, China. ISPRS Int. J. Geo-Inf. 2022, 11, 137. https://doi.org/10.3390/ijgi11020137
Su Y, Wang J, Wang J, Wang G. Measuring Spatial Accessibility to Hospitals of Acute Myocardial Infarction in Multi Period Scale: A Case Study in Shijingshan District, Beijing, China. ISPRS International Journal of Geo-Information. 2022; 11(2):137. https://doi.org/10.3390/ijgi11020137
Chicago/Turabian StyleSu, Yuwei, Jingyong Wang, Jiangping Wang, and Guoen Wang. 2022. "Measuring Spatial Accessibility to Hospitals of Acute Myocardial Infarction in Multi Period Scale: A Case Study in Shijingshan District, Beijing, China" ISPRS International Journal of Geo-Information 11, no. 2: 137. https://doi.org/10.3390/ijgi11020137
APA StyleSu, Y., Wang, J., Wang, J., & Wang, G. (2022). Measuring Spatial Accessibility to Hospitals of Acute Myocardial Infarction in Multi Period Scale: A Case Study in Shijingshan District, Beijing, China. ISPRS International Journal of Geo-Information, 11(2), 137. https://doi.org/10.3390/ijgi11020137





