Receptor Ligands as Helping Hands to L-DOPA in the Treatment of Parkinson’s Disease
Abstract
1. Introduction
2. Serotonin Receptors
2.1. 5-HT1ARs
2.2. 5-HT1BRs
2.3. 5-HT2ARs
2.4. 5-HT3Rs
2.5. 5-HT4Rs
3. Glutamate Receptors
3.1. iGluRs
3.1.1. NMDA Receptors
3.1.2. AMPA Receptors
3.2. mGluRs
3.2.1. mGlu2/3Rs
3.2.2. mGlu4Rs
3.2.3. mGlu5Rs
3.2.4. mGlu7Rs and mGlu8Rs
4. Noradrenergic Receptors
4.1. α2-Ars
4.2. β-ARs
5. Adenosine Receptors
5.1. A1 Receptors
5.2. A2A Receptors
5.3. A1/A2A Receptors
6. Histamine Receptors
6.1. H2 Receptors
6.2. H3 Receptors
6.3. H4 Receptors
7. Cholinergic Receptors
7.1. Muscarinic Receptors
7.2. Nicotinic Agonists
8. GABA Receptors
9. Neurokinin Receptors
10. Opioid Receptors
11. Sigma-1 (σ1) Receptors
12. Conclusions
- -
- the causes of such a pathology are mostly unknown;
- -
- the dopaminergic system and other receptors, as well as several enzymatic targets not discussed in this review, mutually affect each other and are deeply altered over the course of the disease (Figure 19);
- -
- the same drug used in PD therapy or for the treatment of co-morbidities may aggravate the progression of different disease symptoms;
- -
- the symptoms are individual and fluctuating during the day;
- -
- frequently divergent results come from the experimental models used in the evaluation of drug candidates.
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Compound | PubChem CID (Reaxys ID) |
| 5’Cl5’d-(±)-ENBA | 15599147 |
| 8-OH-DPAT | 1220 |
| ABT-089 | 178052 |
| ABT-107 | 11151363 |
| ABT-126 | 24987875 |
| ABT-894 | 10131048 |
| ADX88178 | 46836872 |
| Amantadine | 2130 |
| AMN082 | 11698390 |
| ANR 94 | 11805896 |
| Apomorphine | 6005 |
| AQW051 | 50914822 |
| Aripiprazole | 60795 |
| AZD1446 | 24795080 |
| Befiradol | 9865384 |
| Benzatropine | 1201549 |
| Biperiden | 2381 |
| BMY-14802 | 108046 |
| Bromocriptine | 31101 |
| Buspirone | 2477 |
| Cabergoline | 54746 |
| Caffeine | 2519 |
| CJ-1639 | 53475319 |
| Clozapine | 135398737 |
| CP94253 | 4029677 |
| Cyprodine | 24758534 |
| D-512 | (26962985) |
| D-636 | (33944059) |
| D-653 | (33944076) |
| D-656 | (33944078) |
| DCPG | 16062593 |
| DDMPA-8 | (33958274) |
| DETQ | 117720272 |
| Dextromethorphan | 5360696 |
| Dicyclomine | 3042 |
| Dihydroergocriptine | 114948 |
| Dipraglurant | 44557636 |
| Dizocilpine | 180081 |
| DPI-289 | (12841869) |
| Eltoprazine | 65853 |
| F13714 | (8361393) |
| F15599 | 11741361 |
| Famotidine | 5702160 |
| Fenobam | 135659063 |
| Fipamezole | 213041 |
| Foliglurax | 135565465 |
| Idazoxan | 54459 |
| Ifenprodil | 3689 |
| Istradefylline | 5311037 |
| JNJ7777120 | 4908365 |
| Ketamine | 3821 |
| L-745,870 | 5311200 |
| Lactomorphin | Not Available |
| Lanepitant | 3086681 |
| Lisuride | 28864 |
| LSP1-2111 | 46898088 |
| Lu AF21934 | 66553157 |
| LY379268 | 10197984 |
| Mavoglurant | 9926832 |
| Mecamylamine | 4032 |
| Memantine | 4054 |
| Mianserin | 4184 |
| Mirtazapine | 4205 |
| Mosapride | 119584 |
| MPEP | 3025961 |
| MSX-3 | 10256041 |
| MTEP | 9794218 |
| N-acetyl-L-tryptophan | 700653 |
| Nalbuphine | 5311304 |
| Naloxone | 5284596 |
| Naltrindole | 5497186 |
| Nicotine | 89594 |
| Nizatidine | 3033637 |
| Ondansetron | 4595 |
| Perampanel | 9924495 |
| Pergolide | 47811 |
| Pimavanserin | 10071196 |
| Piribedil | 4850 |
| Pitolisant | 9948102 |
| Pramipexole | 119570 |
| Preladenant | 10117987 |
| Pridopidine | 9795739 |
| Propranolol | 4946 |
| Prucalopride | 3052762 |
| Pruvanserin | 6433122 |
| Quetiapine | 5002 |
| Radiprodil | 10200813 |
| Ropinirole | 5095 |
| Rotigotine | 59227 |
| SAGE-217 | 86294073 |
| Salbutamol | 2083 |
| Sarizotan | 6918388 |
| SK609 | 6486733 |
| SLV-308 | 6918524 |
| SNC-80 | 123924 |
| ST1535 | 9860294 |
| ST3932 | (20692973) |
| ST4206 | 46912314 |
| Talampanel | 164509 |
| Tandospirone | 91273 |
| Tapentadol | 9838022 |
| Tavapadon | 86764100 |
| Telenzepine | 5387 |
| Tezampanel | 127894 |
| Thioperamide | 3035905 |
| Topiramate | 5284627 |
| Tozadenant | 11618368 |
| Traxoprodil | 219101 |
| Trihexyphenidyl | 5572 |
| U50,488 | 3036289 |
| V81444 | 44537963 |
| Vipadenant | 21874557 |
| VU0364770 | 836002 |
| VU0467154 | 73774630 |
| VU0476406 | (23873237) |
| VU6004461 | (29581513) |
| Zolpidem | 5732 |
References
- Apostolova, I.; Taleb, D.S.; Lipp, A.; Galazky, I.; Kupitz, D.; Lange, C.; Makowski, M.R.; Brenner, W.; Amthauer, H.; Plotkin, M.; et al. Utility of Follow-up Dopamine Transporter Spect with 123i-Fp-Cit in the Diagnostic Workup of Patients with Clinically Uncertain Parkinsonian Syndrome. Clin. Nucl. Med. 2017, 42, 589–594. [Google Scholar] [CrossRef]
- Nido, G.S.; Dolle, C.; Flones, I.; Tuppen, H.A.; Alves, G.; Tysnes, O.B.; Haugarvoll, K.; Tzoulis, C. Ultradeep Mapping of Neuronal Mitochondrial Deletions in Parkinson’s Disease. Neurobiol. Aging 2018, 63, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Agosti, V.; Vitale, C.; Avella, D.; Rucco, R.; Santangelo, G.; Sorrentino, P.; Varriale, P.; Sorrentino, G. Effects of Global Postural Reeducation on Gait Kinematics in Parkinsonian Patients: A Pilot Randomized Three-Dimensional Motion Analysis Study. Neurol. Sci. 2016, 37, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Falaki, A.; Huang, X.; Lewis, M.M.; Latash, M.L. Dopaminergic Modulation of Multi-Muscle Synergies in Postural Tasks Performed by Patients with Parkinson’s Disease. J. Electromyogr. Kinesiol. 2017, 33, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Kataoka, H.; Okada, Y.; Kiriyama, T.; Kita, Y.; Nakamura, J.; Morioka, S.; Shomoto, K.; Ueno, S. Can Postural Instability Respond to Galvanic Vestibular Stimulation in Patients with Parkinson’s Disease? J. Mov. Disord. 2016, 9, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Ozinga, S.J.; Koop, M.M.; Linder, S.M.; Machado, A.G.; Dey, T.; Alberts, J.L. Three-Dimensional Evaluation of Postural Stability in Parkinson’s Disease with Mobile Technology. NeuroRehabilitation 2017, 41, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Picconi, B.; Hernandez, L.F.; Obeso, J.A.; Calabresi, P. Motor Complications in Parkinson’s Disease: Striatal Molecular and Electrophysiological Mechanisms of Dyskinesias. Mov. Disord. 2018, 33, 867–876. [Google Scholar] [CrossRef]
- Silva, K.G.; De Freitas, T.B.; Dona, F.; Gananca, F.F.; Ferraz, H.B.; Torriani-Pasin, C.; Pompeu, J.E. Effects of Virtual Rehabilitation Versus Conventional Physical Therapy on Postural Control, Gait, and Cognition of Patients with Parkinson’s Disease: Study Protocol for a Randomized Controlled Feasibility Trial. Pilot Feasibility Stud. 2017, 3, 68. [Google Scholar] [CrossRef]
- Wilczyński, J.; Habik, N. The Effect of L-Dopa on Postural Stability in Parkinson’s Disease Patients. Appl. Sci. 2019, 9, 409. [Google Scholar] [CrossRef]
- Steib, S.; Klamroth, S.; Gassner, H.; Pasluosta, C.; Eskofier, B.; Winkler, J.; Klucken, J.; Pfeifer, K. Perturbation During Treadmill Training Improves Dynamic Balance and Gait in Parkinson’s Disease: A Single-Blind Randomized Controlled Pilot Trial. Neurorehabil. Neural Repair 2017, 31, 758–768. [Google Scholar] [CrossRef]
- Wilczynski, J.; Pedrycz, A.; Mucha, D.; Ambrozy, T.; Mucha, D. Body Posture, Postural Stability, and Metabolic Age in Patients with Parkinson’s Disease. BioMed Res. Int. 2017, 2017, 3975417. [Google Scholar] [CrossRef]
- Bryant, M.S.; Hou, J.G.; Collins, R.L.; Protas, E.J. Contribution of Axial Motor Impairment to Physical Inactivity in Parkinson Disease. Am. J. Phys. Med. Rehabil. 2016, 95, 348–354. [Google Scholar] [CrossRef]
- Caetano, M.J.D.; Lord, S.R.; Allen, N.E.; Brodie, M.A.; Song, J.; Paul, S.S.; Canning, C.G.; Menant, J.C. Stepping Reaction Time and Gait Adaptability Are Significantly Impaired in People with Parkinson’s Disease: Implications for Fall Risk. Parkinsonism Relat. Disord. 2018, 47, 32–38. [Google Scholar] [CrossRef]
- Beuter, A.; Hernandez, R.; Rigal, R.; Modolo, J.; Blanchet, P.J. Postural Sway and Effect of Levodopa in Early Parkinson’s Disease. Can. J. Neurol. Sci. 2008, 35, 65–68. [Google Scholar] [CrossRef]
- Bonnet, C.T.; Delval, A.; Szaffarczyk, S.; Defebvre, L. Levodopa Has Primarily Negative Influences on Postural Control in Patients with Parkinson’s Disease. Behav. Brain Res. 2017, 331, 67–75. [Google Scholar] [CrossRef]
- Mercuri, N.B.; Bernardi, G. The ‘Magic’ of L-Dopa: Why Is It the Gold Standard Parkinson’s Disease Therapy? Trends Pharmacol. Sci. 2005, 26, 341–344. [Google Scholar] [CrossRef]
- Olanow, C.W.; Agid, Y.; Mizuno, Y.; Albanese, A.; Bonucelli, U.; Damier, P.; De Yebenes, J.; Gershanik, O.; Guttman, M.; Grandas, F.; et al. Levodopa in the Treatment of Parkinson’s Disease: Current Controversies. Mov. Disord. 2004, 19, 997–1005. [Google Scholar] [CrossRef]
- Poewe, W.; Antonini, A.; Zijlmans, J.C.; Burkhard, P.R.; Vingerhoets, F. Levodopa in the Treatment of Parkinson’s Disease: An Old Drug Still Going Strong. Clin. Interv. Aging 2010, 5, 229–238. [Google Scholar]
- Smith, E.S.; Hardy, G.A.; Schallert, T.; Lee, H.J. The Impact of L-Dopa on Attentional Impairments in a Rat Model of Parkinson’s Disease. Neuroscience 2016, 337, 295–305. [Google Scholar] [CrossRef]
- Cossu, G.; Ricchi, V.; Pilleri, M.; Mancini, F.; Murgia, D.; Ricchieri, G.; Mereu, A.; Melis, M.; Antonini, A. Levodopa-Carbidopa Intrajejunal Gel in Advanced Parkinson Disease with “on” Freezing of Gait. Neurol. Sci. 2015, 36, 1683–1686. [Google Scholar] [CrossRef]
- Standaert, D.G.; Rodriguez, R.L.; Slevin, J.T.; Lobatz, M.; Eaton, S.; Chatamra, K.; Facheris, M.F.; Hall, C.; Sail, K.; Jalundhwala, Y.J.; et al. Effect of Levodopa-Carbidopa Intestinal Gel on Non-Motor Symptoms in Patients with Advanced Parkinson’s Disease. Mov. Disord. Clin. Pract. 2017, 4, 829–837. [Google Scholar] [CrossRef]
- Zibetti, M.; Merola, A.; Artusi, C.A.; Rizzi, L.; Angrisano, S.; Reggio, D.; De Angelis, C.; Rizzone, M.; Lopiano, L. Levodopa/Carbidopa Intestinal Gel Infusion in Advanced Parkinson’s Disease: A 7-Year Experience. Eur. J. Neurol. 2014, 21, 312–318. [Google Scholar] [CrossRef]
- Kocer, B.; Guven, H.; Comoglu, S.S. Homocysteine Levels in Parkinson’s Disease: Is Entacapone Effective? BioMed Res. Int. 2016, 2016, 7563705. [Google Scholar] [CrossRef]
- Scott, L.J. Opicapone: A Review in Parkinson’s Disease. Drugs 2016, 76, 1293–1300. [Google Scholar] [CrossRef]
- Ferreira, J.J.; Katzenschlager, R.; Bloem, B.R.; Bonuccelli, U.; Burn, D.; Deuschl, G.; Dietrichs, E.; Fabbrini, G.; Friedman, A.; Kanovsky, P.; et al. Summary of the Recommendations of the EFNS/MDS-ES Review on Therapeutic Management of Parkinson’s Disease. Eur. J. Neurol. 2013, 20, 5–15. [Google Scholar] [CrossRef]
- Cenci, M.A. Molecular Mechanisms of L-Dopa-Induced Dyskinesia. In Handbook of Behavioral Neuroscience; Steiner, H., Tseng, K.Y., Eds.; Elsevier: Amsterdam, The Netherlands, 2016; Vol. 24, pp. 857–871. [Google Scholar]
- Cerri, S.; Siani, F.; Blandini, F. Investigational Drugs in Phase I and Phase II for Levodopa-Induced Dyskinesias. Expert Opin. Investig. Drugs 2017, 26, 777–791. [Google Scholar] [CrossRef]
- Curtze, C.; Nutt, J.G.; Carlson-Kuhta, P.; Mancini, M.; Horak, F.B. Levodopa Is a Double-Edged Sword for Balance and Gait in People with Parkinson’s Disease. Mov. Disord. 2015, 30, 1361–1370. [Google Scholar] [CrossRef]
- Hechtner, M.C.; Vogt, T.; Zöllner, Y.; Schröder, S.; Sauer, J.B.; Binder, H.; Singer, S.; Mikolajczyk, R. Quality of Life in Parkinson’s Disease Patients with Motor Fluctuations and Dyskinesias in Five European Countries. Parkinsonism Relat. Disord. 2014, 20, 969–974. [Google Scholar] [CrossRef]
- Perez-Lloret, S.; Negre-Pages, L.; Damier, P.; Delval, A.; Derkinderen, P.; Destee, A.; Meissner, W.G.; Tison, F.; Rascol, O. L-DOPA-Induced Dyskinesias, Motor Fluctuations and Health-Related Quality of Life: The Copark Survey. Eur. J. Neurol. 2017, 24, 1532–1538. [Google Scholar] [CrossRef]
- Dragasevic-Miskovic, N.; Petrovic, I.; Stankovic, I.; Kostic, V.S. Chemical Management of Levodopa-Induced Dyskinesia in Parkinson’s Disease Patients. Expert Opin. Pharmacother. 2019, 20, 219–230. [Google Scholar] [CrossRef]
- Oertel, W.; Schulz, J.B. Current and Experimental Treatments of Parkinson Disease: A Guide for Neuroscientists. J. Neurochem. 2016, 139 (Suppl. 1), 325–337. [Google Scholar] [CrossRef]
- Dong, J.; Cui, Y.; Li, S.; Le, W. Current Pharmaceutical Treatments and Alternative Therapies of Parkinson’s Disease. Curr. Neuropharmacol. 2016, 14, 339–355. [Google Scholar] [CrossRef]
- Moore, T.J.; Glenmullen, J.; Mattison, D.R. Reports of Pathological Gambling, Hypersexuality, and Compulsive Shopping Associated with Dopamine Receptor Agonist Drugsimpulse Control Disorders and Dopamine Agonistsimpulse Control Disorders and Dopamine Agonists. JAMA Intern. Med. 2014, 174, 1930–1933. [Google Scholar] [CrossRef] [PubMed]
- Connolly, B.S.; Lang, A.E. Pharmacological Treatment of Parkinson Disease: A Review. JAMA 2014, 311, 1670–1683. [Google Scholar] [CrossRef] [PubMed]
- Noyes, K.; Dick, A.W.; Holloway, R.G. Pramipexole and Levodopa in Early Parkinson’s Disease. Pharmacoeconomics 2005, 23, 1257–1270. [Google Scholar] [CrossRef]
- Thanvi, B.; Lo, N.; Robinson, T. Levodopa-Induced Dyskinesia in Parkinson’s Disease: Clinical Features, Pathogenesis, Prevention and Treatment. Postgrad. Med. J. 2007, 83, 384–388. [Google Scholar] [CrossRef] [PubMed]
- Espay, A.J.; Morgante, F.; Merola, A.; Fasano, A.; Marsili, L.; Fox, S.H.; Bezard, E.; Picconi, B.; Calabresi, P.; Lang, A.E. Levodopa-Induced Dyskinesia in Parkinson Disease: Current and Evolving Concepts. Ann. Neurol. 2018, 84, 797–811. [Google Scholar] [CrossRef] [PubMed]
- Sohur, U.S.; Gray, D.L.; Duvvuri, S.; Zhang, Y.; Thayer, K.; Feng, G. Phase 1 Parkinson’s Disease Studies Show the Dopamine D1/D5 Agonist PF-06649751 Is Safe and Well Tolerated. Neurol. Ther. 2018, 7, 307–319. [Google Scholar] [CrossRef] [PubMed]
- Guigoni, C.; Aubert, I.; Li, Q.; Gurevich, V.V.; Benovic, J.L.; Ferry, S.; Mach, U.; Stark, H.; Leriche, L.; Håkansson, K.; et al. Pathogenesis of Levodopa-Induced Dyskinesia: Focus on D1 and D3 Dopamine Receptors. Parkinsonism Relat. Disord. 2005, 11, S25–S29. [Google Scholar] [CrossRef]
- Svensson, K.A.; Heinz, B.A.; Schaus, J.M.; Beck, J.P.; Hao, J.; Krushinski, J.H.; Reinhard, M.R.; Cohen, M.P.; Hellman, S.L.; Getman, B.G.; et al. An Allosteric Potentiator of the Dopamine D1 Receptor Increases Locomotor Activity in Human D1 Knock-in Mice without Causing Stereotypy or Tachyphylaxis. J. Pharmacol. Exp. Ther. 2017, 360, 117–128. [Google Scholar] [CrossRef]
- Bruns, R.F.; Mitchell, S.N.; Wafford, K.A.; Harper, A.J.; Shanks, E.A.; Carter, G.; O’Neill, M.J.; Murray, T.K.; Eastwood, B.J.; Schaus, J.M.; et al. Preclinical Profile of a Dopamine D1 Potentiator Suggests Therapeutic Utility in Neurological and Psychiatric Disorders. Neuropharmacology 2018, 128, 351–365. [Google Scholar] [CrossRef]
- Meltzer, H.Y.; Rajagopal, L.; Matrisciano, F.; Hao, J.; Svensson, K.A.; Huang, M. The Allosteric Dopamine D1 Receptor Potentiator, Detq, Ameliorates Subchronic Phencyclidine-Induced Object Recognition Memory Deficits and Enhances Cortical Acetylcholine Efflux in Male Humanized D1 Receptor Knock-in Mice. Behav. Brain Res. 2019, 361, 139–150. [Google Scholar] [CrossRef]
- Fiorentini, C.; Busi, C.; Gorruso, E.; Gotti, C.; Spano, P.; Missale, C. Reciprocal Regulation of Dopamine D1 and D3 Receptor Function and Trafficking by Heterodimerization. Mol. Pharmacol. 2008, 74, 59–69. [Google Scholar] [CrossRef]
- Marcellino, D.; Ferré, S.; Casadó, V.; Cortés, A.; Le Foll, B.; Mazzola, C.; Drago, F.; Saur, O.; Stark, H.; Soriano, A.; et al. Identification of Dopamine D1–D3 Receptor Heteromers. Indications for a Role of Synergistic D1-D3 Receptor Interactions in the Striatum. J. Biol. Chem. 2008, 283, 26016–26025. [Google Scholar] [CrossRef]
- Solis, O.; Garcia-Montes, J.R.; Gonzalez-Granillo, A.; Xu, M.; Moratalla, R. Dopamine D3 Receptor Modulates L-Dopa-Induced Dyskinesia by Targeting D1 Receptor-Mediated Striatal Signaling. Cereb. Cortex 2017, 27, 435–446. [Google Scholar] [CrossRef]
- Fiorentini, C.; Savoia, P.; Bono, F.; Tallarico, P.; Missale, C. The D3 Dopamine Receptor: From Structural Interactions to Function. Eur. Neuropsychopharmacol. 2015, 25, 1462–1469. [Google Scholar] [CrossRef]
- Solis, O.; Moratalla, R. Dopamine Receptors: Homomeric and Heteromeric Complexes in L-DOPA-Induced Dyskinesia. J. Neural Transm. 2018, 125, 1187–1194. [Google Scholar] [CrossRef]
- Bézard, E.; Ferry, S.; Mach, U.; Stark, H.; Leriche, L.; Boraud, T.; Gross, C.; Sokoloff, P. Attenuation of Levodopa-Induced Dyskinesia by Normalizing Dopamine D3 Receptor Function. Nat. Med. 2003, 9, 762–767. [Google Scholar] [CrossRef]
- Payer, D.E.; Guttman, M.; Kish, S.J.; Tong, J.; Adams, J.R.; Rusjan, P.; Houle, S.; Furukawa, Y.; Wilson, A.A.; Boileau, I. D3 Dopamine Receptor-Preferring [11C]PHNO PET Imaging in Parkinson Patients with Dyskinesia. Neurology 2016, 86, 224–230. [Google Scholar] [CrossRef]
- Ghosh, B.; Antonio, T.; Zhen, J.; Kharkar, P.; Reith, M.E.A.; Dutta, A.K. Development of (S)-N6-(2-(4-(Isoquinolin-1-yl)Piperazin-1-yl)Ethyl)-N6-Propyl-4,5,6,7-Tetrahydrobenzo[d]-Thiazole-2,6-Diamine and Its Analogue as a D3 Receptor Preferring Agonist: Potent in Vivo Activity in Parkinson’s Disease Animal Models. J. Med. Chem. 2010, 53, 1023–1037. [Google Scholar] [CrossRef]
- Hiller, C.; Kling, R.C.; Heinemann, F.W.; Meyer, K.; Hübner, H.; Gmeiner, P. Functionally Selective Dopamine D2/D3 Receptor Agonists Comprising an Enyne Moiety. J. Med. Chem. 2013, 56, 5130–5141. [Google Scholar] [CrossRef]
- Tschammer, N.; Elsner, J.; Goetz, A.; Ehrlich, K.; Schuster, S.; Ruberg, M.; Kühhorn, J.; Thompson, D.; Whistler, J.; Hübner, H.; et al. Highly Potent 5-Aminotetrahydropyrazolopyridines: Enantioselective Dopamine D3 Receptor Binding, Functional Selectivity, and Analysis of Receptor−Ligand Interactions. J. Med. Chem. 2011, 54, 2477–2491. [Google Scholar] [CrossRef]
- Zhang, H.; Tong, R.; Bai, L.; Shi, J.; Ouyang, L. Emerging Targets and New Small Molecule Therapies in Parkinson’s Disease Treatment. Bioorg. Med. Chem. 2016, 24, 1419–1430. [Google Scholar] [CrossRef]
- Zhao, Y.; Lu, X.; Yang, C.-y.; Huang, Z.; Fu, W.; Hou, T.; Zhang, J. Computational Modeling toward Understanding Agonist Binding on Dopamine 3. J. Chem. Inf. Model. 2010, 50, 1633–1643. [Google Scholar] [CrossRef] [PubMed]
- Gil-Mast, S.; Kortagere, S.; Kota, K.; Kuzhikandathil, E.V. An Amino Acid Residue in the Second Extracellular Loop Determines the Agonist-Dependent Tolerance Property of the Human D3 Dopamine Receptor. ACS Chem. Neurosci. 2013, 4, 940–951. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kortagere, S.; Kuzhikandahil, E.V. Novel D3 Dopamine Receptor Agonists to Treat Dyskinesia in Parkinson’s Disease. U.S. Patent WO2012021629 e, 16 February 2012. [Google Scholar]
- Westrich, L.; Gil-Mast, S.; Kortagere, S.; Kuzhikandathil, E.V. Development of Tolerance in D3 Dopamine Receptor Signaling Is Accompanied by Distinct Changes in Receptor Conformation. Biochem. Pharmacol. 2010, 79, 897–907. [Google Scholar] [CrossRef] [PubMed]
- Cote, S.R.; Kuzhikandathil, E.V. In vitro and In vivo Characterization of the Agonist-Dependent D3 Dopamine Receptor Tolerance Property. Neuropharmacology 2014, 79, 359–367. [Google Scholar] [CrossRef]
- Xu, W.; Wang, X.; Tocker, A.M.; Huang, P.; Reith, M.E.; Liu-Chen, L.Y.; Smith, A.B., 3rd; Kortagere, S. Functional Characterization of a Novel Series of Biased Signaling Dopamine D3 Receptor Agonists. ACS Chem. Neurosci. 2017, 8, 486–500. [Google Scholar] [CrossRef] [PubMed]
- Simms, S.L.; Huettner, D.P.; Kortagere, S. In Vivo Characterization of a Novel Dopamine D3 Receptor Agonist to Treat Motor Symptoms of Parkinson’s Disease. Neuropharmacology 2016, 100, 106–115. [Google Scholar] [CrossRef]
- Chen, J.; Collins, G.T.; Levant, B.; Woods, J.; Deschamps, J.R.; Wang, S. Cj-1639: A Potent and Highly Selective Dopamine D3 Receptor Full Agonist. ACS Med. Chem. Lett. 2011, 2, 620–625. [Google Scholar] [CrossRef]
- Das, B.; Modi, G.; Dutta, A. Dopamine D3 Agonists in the Treatment of Parkinson’s Disease. Curr. Top. Med. Chem. 2015, 15, 908–926. [Google Scholar] [CrossRef]
- Lindenbach, D.; Das, B.; Conti, M.M.; Meadows, S.M.; Dutta, A.K.; Bishop, C. D-512, a Novel Dopamine D2/3 Receptor Agonist, Demonstrates Greater Anti-Parkinsonian Efficacy Than Ropinirole in Parkinsonian Rats. Br. J. Pharmacol. 2017, 174, 3058–3071. [Google Scholar] [CrossRef]
- Santra, S.; Xu, L.; Shah, M.; Johnson, M.; Dutta, A. D-512 and D-440 as Novel Multifunctional Dopamine Agonists: Characterization of Neuroprotection Properties and Evaluation of in Vivo Efficacy in a Parkinson’s Disease Animal Model. ACS Chem. Neurosci. 2013, 4, 1382–1392. [Google Scholar] [CrossRef]
- Elmabruk, A.; Das, B.; Yedlapudi, D.; Xu, L.; Antonio, T.; Reith, M.E.A.; Dutta, A.K. Design, Synthesis, and Pharmacological Characterization of Carbazole Based Dopamine Agonists as Potential Symptomatic and Neuroprotective Therapeutic Agents for Parkinson’s Disease. ACS Chem. Neurosci. 2019, 10, 396–411. [Google Scholar] [CrossRef]
- Glennon, J.C.; Van Scharrenburg, G.; Ronken, E.; Hesselink, M.B.; Reinders, J.H.; Van Der Neut, M.; Long, S.K.; Feenstra, R.W.; McCreary, A.C. In Vitro Characterization of SLV308 (7-[4-Methyl-1-Piperazinyl]-2(3h)-Benzoxazolone, Monohydrochloride): A Novel Partial Dopamine D2 and D3 Receptor Agonist and Serotonin 5-HT1A Receptor Agonist. Synapse 2006, 60, 599–608. [Google Scholar] [CrossRef]
- Del Bello, F.; Ambrosini, D.; Bonifazi, A.; Newman, A.H.; Keck, T.M.; Giannella, M.; Giorgioni, G.; Piergentili, A.; Cappellacci, L.; Cilia, A.; et al. Multitarget 1,4-Dioxane Compounds Combining Favorable D2-Like and 5-HT1A Receptor Interactions with Potential for the Treatment of Parkinson’s Disease or Schizophrenia. ACS Chem. Neurosci. 2019. [Google Scholar] [CrossRef]
- DeLong, M.R. Primate Models of Movement Disorders of Basal Ganglia Origin. Trends Neurosci. 1990, 13, 281–285. [Google Scholar] [CrossRef]
- Huot, P.; Johnston, T.H.; Koprich, J.B.; Fox, S.H.; Brotchie, J.M. The Pharmacology of L-DOPA-Induced Dyskinesia in Parkinson’s Disease. Pharmacol. Rev. 2013, 65, 171–222. [Google Scholar] [CrossRef]
- Del Bello, F.; Bonifazi, A.; Giorgioni, G.; Cifani, C.; Micioni Di Bonaventura, M.V.; Petrelli, R.; Piergentili, A.; Fontana, S.; Mammoli, V.; Yano, H.; et al. 1-[3-(4-Butylpiperidin-1-yl)Propyl]-1,2,3,4-Tetrahydroquinolin-2-One (77-LH-28-1) as a Model for the Rational Design of a Novel Class of Brain Penetrant Ligands with High Affinity and Selectivity for Dopamine D4 Receptor. J. Med. Chem. 2018, 61, 3712–3725. [Google Scholar] [CrossRef]
- DeLong, M.R.; Wichmann, T. Circuits and Circuit Disorders of the Basal Ganglia. Arch. Neurol. 2007, 64, 20–24. [Google Scholar] [CrossRef]
- Lindsley, C.W.; Hopkins, C.R. Return of D4 Dopamine Receptor Antagonists in Drug Discovery. J. Med. Chem. 2017, 60, 7233–7243. [Google Scholar] [CrossRef]
- Wichmann, T.; DeLong, M.R. Functional Neuroanatomy of the Basal Ganglia in Parkinson’s Disease. Adv. Neurol. 2003, 91, 9–18. [Google Scholar]
- Huot, P.; Johnston, T.H.; Koprich, J.B.; Aman, A.; Fox, S.H.; Brotchie, J.M. L-745,870 Reduces L-DOPA-Induced Dyskinesia in the 1-Methyl-4-Phenyl-1,2,3,6-Tetrahydropyridine-Lesioned Macaque Model of Parkinson’s Disease. J. Pharmacol. Exp. Ther. 2012, 342, 576–585. [Google Scholar] [CrossRef]
- Huot, P.; Johnston, T.H.; Koprich, J.B.; Espinosa, M.C.; Reyes, M.G.; Fox, S.H.; Brotchie, J.M. L-745,870 Reduces the Expression of Abnormal Involuntary Movements in the 6-OHDA-Lesioned Rat. Behav. Pharmacol. 2015, 26, 101–108. [Google Scholar] [CrossRef]
- Witt, J.O.; McCollum, A.L.; Hurtado, M.A.; Huseman, E.D.; Jeffries, D.E.; Temple, K.J.; Plumley, H.C.; Blobaum, A.L.; Lindsley, C.W.; Hopkins, C.R. Synthesis and Characterization of a Series of Chiral Alkoxymethyl Morpholine Analogs as Dopamine Receptor 4 (D4R) Antagonists. Bioorg. Med. Chem. Lett. 2016, 26, 2481–2488. [Google Scholar] [CrossRef]
- Sebastianutto, I.; Maslava, N.; Hopkins, C.R.; Cenci, M.A. Validation of an Improved Scale for Rating L-Dopa-Induced Dyskinesia in the Mouse and Effects of Specific Dopamine Receptor Antagonists. Neurobiol. Dis. 2016, 96, 156–170. [Google Scholar] [CrossRef]
- Lanza, K.; Bishop, C. Serotonergic Targets for the Treatment of L-DOPA-Induced Dyskinesia. J. Neural Transm. 2018, 125, 1203–1216. [Google Scholar] [CrossRef]
- Carta, M.; Tronci, E. Serotonin System Implication in L-Dopa-Induced Dyskinesia: From Animal Models to Clinical Investigations. Front. Neurol. 2014, 5, 78. [Google Scholar] [CrossRef]
- Carta, M.; Carlsson, T.; Kirik, D.; Bjorklund, A. Dopamine Released from 5-HT Terminals Is the Cause of L-DOPA-Induced Dyskinesia in Parkinsonian Rats. Brain 2007, 130, 1819–1833. [Google Scholar] [CrossRef]
- Nicholson, S.L.; Brotchie, J.M. 5-Hydroxytryptamine (5-HT, Serotonin) and Parkinson’s Disease—Opportunities for Novel Therapeutics to Reduce the Problems of Levodopa Therapy. Eur. J. Neurol. 2002, 9 (Suppl. 3), 1–6. [Google Scholar] [CrossRef]
- Dupre, K.B.; Ostock, C.Y.; Eskow Jaunarajs, K.L.; Button, T.; Savage, L.M.; Wolf, W.; Bishop, C. Local Modulation of Striatal Glutamate Efflux by Serotonin 1A Receptor Stimulation in Dyskinetic, Hemiparkinsonian Rats. Exp. Neurol. 2011, 229, 288–299. [Google Scholar] [CrossRef]
- Dupre, K.B.; Ostock, C.Y.; George, J.A.; Eskow Jaunarajs, K.L.; Hueston, C.M.; Bishop, C. Effects of 5-HT1A Receptor Stimulation on D1 Receptor Agonist-Induced Striatonigral Activity and Dyskinesia in Hemiparkinsonian Rats. ACS Chem. Neurosci. 2013, 4, 747–760. [Google Scholar] [CrossRef]
- Iravani, M.M.; Tayarani-Binazir, K.; Chu, W.B.; Jackson, M.J.; Jenner, P. In 1-Methyl-4-Phenyl-1,2,3,6-Tetrahydropyridine-Treated Primates, the Selective 5-Hydroxytryptamine 1a Agonist (R)-(+)-8-Ohdpat Inhibits Levodopa-Induced Dyskinesia but Only with\ Increased Motor Disability. J. Pharmacol. Exp. Ther. 2006, 319, 1225–1234. [Google Scholar] [CrossRef]
- Bartoszyk, G.D.; Van Amsterdam, C.; Greiner, H.E.; Rautenberg, W.; Russ, H.; Seyfried, C.A. Sarizotan, a Serotonin 5-HT1A Receptor Agonist and Dopamine Receptor Ligand. 1. Neurochemical Profile. J. Neural Transm. 2004, 111, 113–126. [Google Scholar] [CrossRef]
- Bibbiani, F.; Oh, J.D.; Chase, T.N. Serotonin 5-HT1A Agonist Improves Motor Complications in Rodent and Primate Parkinsonian Models. Neurology 2001, 57, 1829–1834. [Google Scholar] [CrossRef]
- Goetz, C.G.; Damier, P.; Hicking, C.; Laska, E.; Muller, T.; Olanow, C.W.; Rascol, O.; Russ, H. Sarizotan as a Treatment for Dyskinesias in Parkinson’s Disease: A Double-Blind Placebo-Controlled Trial. Mov. Disord. 2007, 22, 179–186. [Google Scholar] [CrossRef]
- Goetz, C.G.; Laska, E.; Hicking, C.; Damier, P.; Müller, T.; Nutt, J.; Warren Olanow, C.; Rascol, O.; Russ, H. Placebo Influences on Dyskinesia in Parkinson’s Disease. Mov. Disord. 2008, 23, 700–707. [Google Scholar] [CrossRef]
- Kannari, K.; Kurahashi, K.; Tomiyama, M.; Maeda, T.; Arai, A.; Baba, M.; Suda, T.; Matsunaga, M. Tandospirone Citrate, a Selective 5-HT1A Agonist, Alleviates L-DOPA-Induced Dyskinesia in Patients with Parkinson’s Disease. No to shinkei = Brain and nerve 2002, 54, 133–137. [Google Scholar]
- Ludwig, C.L.; Weinberger, D.R.; Bruno, G.; Gillespie, M.; Bakker, K.; LeWitt, P.A.; Chase, T.N. Buspirone, Parkinson’s Disease, and the Locus Ceruleus. Clin. Neuropharmacol. 1986, 9, 373–378. [Google Scholar] [CrossRef]
- Politis, M.; Wu, K.; Loane, C.; Brooks, D.J.; Kiferle, L.; Turkheimer, F.E.; Bain, P.; Molloy, S.; Piccini, P. Serotonergic Mechanisms Responsible for Levodopa-Induced Dyskinesias in Parkinson’s Disease Patients. J. Clin. Invest. 2014, 124, 1340–1349. [Google Scholar] [CrossRef]
- Bezard, E.; Tronci, E.; Pioli, E.Y.; Li, Q.; Porras, G.; Bjorklund, A.; Carta, M. Study of the Antidyskinetic Effect of Eltoprazine in Animal Models of Levodopa-Induced Dyskinesia. Mov. Disord. 2013, 28, 1088–1096. [Google Scholar] [CrossRef]
- Schipper, J.; Tulp, M.T.M.; Sijbesma, H. Neurochemical Profile of Eltoprazine. Drug Metabol. Drug Interact. 1990, 8, 85–114. [Google Scholar] [CrossRef]
- Tronci, E.; Fidalgo, C.; Stancampiano, R.; Carta, M. Effect of Selective and Non-Selective Serotonin Receptor Activation on L-DOPA-Induced Therapeutic Efficacy and Dyskinesia in Parkinsonian Rats. Behav. Brain Res. 2015, 292, 300–304. [Google Scholar] [CrossRef]
- Svenningsson, P.; Rosenblad, C.; Af Edholm Arvidsson, K.; Wictorin, K.; Keywood, C.; Shankar, B.; Lowe, D.A.; Bjorklund, A.; Widner, H. Eltoprazine Counteracts L-Dopa-Induced Dyskinesias in Parkinson’s Disease: A Dose-Finding Study. Brain 2015, 138, 963–973. [Google Scholar] [CrossRef]
- Ko, W.K.D.; Li, Q.; Cheng, L.Y.; Morelli, M.; Carta, M.; Bezard, E. A Preclinical Study on the Combined Effects of Repeated Eltoprazine and Preladenant Treatment for Alleviating L-DOPA-Induced Dyskinesia in Parkinson’s Disease. Eur. J. Pharmacol. 2017, 813, 10–16. [Google Scholar] [CrossRef]
- Pinna, A.; Ko, W.K.; Costa, G.; Tronci, E.; Fidalgo, C.; Simola, N.; Li, Q.; Tabrizi, M.A.; Bezard, E.; Carta, M.; et al. Antidyskinetic Effect of A2A and 5HT1A/1B Receptor Ligands in Two Animal Models of Parkinson’s Disease. Mov. Disord. 2016, 31, 501–511. [Google Scholar] [CrossRef]
- Huot, P.; Johnston, T.H.; Fox, S.H.; Newman-Tancredi, A.; Brotchie, J.M. The Highly-Selective 5-HT(1A) Agonist F15599 Reduces L-DOPA-Induced Dyskinesia without Compromising Anti-Parkinsonian Benefits in the MPTP-Lesioned Macaque. Neuropharmacology 2015, 97, 306–311. [Google Scholar] [CrossRef]
- Iderberg, H.; McCreary, A.C.; Varney, M.A.; Cenci, M.A.; Newman-Tancredi, A. Activity of Serotonin 5-HT(1A) Receptor ’Biased Agonists’ in Rat Models of Parkinson’s Disease and L-DOPA-Induced Dyskinesia. Neuropharmacology 2015, 93, 52–67. [Google Scholar] [CrossRef]
- Iderberg, H.; McCreary, A.C.; Varney, M.A.; Kleven, M.S.; Koek, W.; Bardin, L.; Depoortere, R.; Cenci, M.A.; Newman-Tancredi, A. NLX-112, a Novel 5-HT1A Receptor Agonist for the Treatment of L-DOPA-Induced Dyskinesia: Behavioral and Neurochemical Profile in Rat. Exp. Neurol. 2015, 271, 335–350. [Google Scholar] [CrossRef]
- Chilmonczyk, Z.; Bojarski, A.J.; Pilc, A.; Sylte, I. Functional Selectivity and Antidepressant Activity of Serotonin 1A Receptor Ligands. Int. J. Mol. Sci. 2015, 16, 18474–18506. [Google Scholar] [CrossRef]
- Llado-Pelfort, L.; Assie, M.B.; Newman-Tancredi, A.; Artigas, F.; Celada, P. Preferential in Vivo Action of F15599, a Novel 5-HT(1A) Receptor Agonist, at Postsynaptic 5-HT(1A) Receptors. Br. J. Pharmacol. 2010, 160, 1929–1940. [Google Scholar] [CrossRef] [PubMed]
- Newman-Tancredi, A.; Martel, J.C.; Assie, M.B.; Buritova, J.; Lauressergues, E.; Cosi, C.; Heusler, P.; Bruins Slot, L.; Colpaert, F.C.; Vacher, B.; et al. Signal Transduction and Functional Selectivity of F15599, a Preferential Post-Synaptic 5-HT1A Receptor Agonist. Br. J. Pharmacol. 2009, 156, 338–353. [Google Scholar] [CrossRef] [PubMed]
- Newman-Tancredi, A.; Varney, M.A.; McCreary, A.C. Effects of the Serotonin 5-HT1A Receptor Biased Agonists, F13714 and F15599, on Striatal Neurotransmitter Levels Following L-DOPA Administration in Hemi-Parkinsonian Rats. Neurochem. Res. 2018, 43, 1035–1046. [Google Scholar] [CrossRef] [PubMed]
- Eskow Jaunarajs, K.L.; Dupre, K.B.; Steiniger, A.; Klioueva, A.; Moore, A.; Kelly, C.; Bishop, C. Serotonin 1B Receptor Stimulation Reduces D1 Receptor Agonist-Induced Dyskinesia. Neuroreport 2009, 20, 1265–1269. [Google Scholar] [CrossRef]
- Iderberg, H.; Rylander, D.; Bimpisidis, Z.; Cenci, M.A. Modulating mGluR5 and 5-HT1A/1B Receptors to Treat L-Dopa-Induced Dyskinesia: Effects of Combined Treatment and Possible Mechanisms of Action. Exp. Neurol. 2013, 250, 116–124. [Google Scholar] [CrossRef]
- Roberts, C. ACP-103, a 5-HT2A Receptor Inverse Agonist. Curr. Opin. Investig. Drugs 2006, 7, 653–660. [Google Scholar] [PubMed]
- Vanover, K.E.; Betz, A.J.; Weber, S.M.; Bibbiani, F.; Kielaite, A.; Weiner, D.M.; Davis, R.E.; Chase, T.N.; Salamone, J.D. A 5-HT2A Receptor Inverse Agonist, ACP-103, Reduces Tremor in a Rat Model and Levodopa-Induced Dyskinesias in a Monkey Model. Pharmacol. Biochem. Behav. 2008, 90, 540–544. [Google Scholar] [CrossRef]
- Stahl, S.M. Mechanism of Action of Pimavanserin in Parkinson’s Disease Psychosis: Targeting Serotonin 5HT2A and 5HT2C Receptors. CNS Spectr. 2016, 21, 271–275. [Google Scholar] [CrossRef]
- Cummings, J.; Isaacson, S.; Mills, R.; Williams, H.; Chi-Burris, K.; Corbett, A.; Dhall, R.; Ballard, C. Pimavanserin for Patients with Parkinson’s Disease Psychosis: A Randomised, Placebo-Controlled Phase 3 Trial. Lancet 2014, 383, 533–540. [Google Scholar] [CrossRef]
- Hamadjida, A.; Nuara, S.G.; Bedard, D.; Gaudette, F.; Beaudry, F.; Gourdon, J.C.; Huot, P. The Highly Selective 5-HT2A Antagonist EMD-281,014 Reduces Dyskinesia and Psychosis in the L-Dopa-Treated Parkinsonian Marmoset. Neuropharmacology 2018, 139, 61–67. [Google Scholar] [CrossRef]
- Frouni, I.; Kwan, C.; Bedard, D.; Belliveau, S.; Bourgeois-Cayer, E.; Gaudette, F.; Beaudry, F.; Hamadjida, A.; Huot, P. Effect of the Selective 5-HT2A Receptor Antagonist EMD-281,014 on L-DOPA-Induced Abnormal Involuntary Movements in the 6-OHDA-Lesioned Rat. Exp. Brain Res. 2019, 237, 29–36. [Google Scholar] [CrossRef]
- Lundblad, M.; Andersson, M.; Winkler, C.; Kirik, D.; Wierup, N.; Cenci, M.A. Pharmacological Validation of Behavioural Measures of Akinesia and Dyskinesia in a Rat Model of Parkinson’s Disease. Eur. J. Neurosci. 2002, 15, 120–132. [Google Scholar] [CrossRef]
- Visanji, N.P.; Gomez-Ramirez, J.; Johnston, T.H.; Pires, D.; Voon, V.; Brotchie, J.M.; Fox, S.H. Pharmacological Characterization of Psychosis-Like Behavior in the MPTP-Lesioned Nonhuman Primate Model of Parkinson’s Disease. Mov. Disord. 2006, 21, 1879–1891. [Google Scholar] [CrossRef]
- Durif, F.; Debilly, B.; Galitzky, M.; Morand, D.; Viallet, F.; Borg, M.; Thobois, S.; Broussolle, E.; Rascol, O. Clozapine Improves Dyskinesias in Parkinson Disease. Neurology 2004, 62, 381–388. [Google Scholar] [CrossRef]
- Morgante, L.; Epifanio, A.; Spina, E.; Zappia, M.; Di Rosa, A.E.; Marconi, R.; Basile, G.; Di Raimondo, G.; La Spina, P.; Quattrone, A. Quetiapine and Clozapine in Parkinsonian Patients with Dopaminergic Psychosis. Clin. Neuropharmacol. 2004, 27, 153–156. [Google Scholar] [CrossRef]
- DeVane, C.L.; Nemeroff, C.B. Clinical Pharmacokinetics of Quetiapine: An Atypical Antipsychotic. Clin. Pharmacokinet. 2001, 40, 509–522. [Google Scholar] [CrossRef]
- Gefvert, O.; Bergstrom, M.; Langstrom, B.; Lundberg, T.; Lindstrom, L.; Yates, R. Time Course of Central Nervous Dopamine-D2 and 5-HT2 Receptor Blockade and Plasma Drug Concentrations after Discontinuation of Quetiapine (Seroquel) in Patients with Schizophrenia. Psychopharmacology 1998, 135, 119–126. [Google Scholar] [CrossRef]
- Oh, J.D.; Bibbiani, F.; Chase, T.N. Quetiapine Attenuates Levodopa-Induced Motor Complications in Rodent and Primate Parkinsonian Models. Exp. Neurol. 2002, 177, 557–564. [Google Scholar] [CrossRef]
- Katzenschlager, R.; Manson, A.J.; Evans, A.; Watt, H.; Lees, A.J. Low Dose Quetiapine for Drug Induced Dyskinesias in Parkinson’s Disease: A Double Blind Cross over Study. J. Neurol. Neurosurg. Psychiatry 2004, 75, 295–297. [Google Scholar]
- Grunder, G.; Kungel, M.; Ebrecht, M.; Gorocs, T.; Modell, S. Aripiprazole: Pharmacodynamics of a Dopamine Partial Agonist for the Treatment of Schizophrenia. Pharmacopsychiatry 2006, 39 (Suppl. 1), S21–25. [Google Scholar] [CrossRef]
- Friedman, J.H.; Berman, R.M.; Goetz, C.G.; Factor, S.A.; Ondo, W.G.; Wojcieszek, J.; Carson, W.H.; Marcus, R.N. Open-Label Flexible-Dose Pilot Study to Evaluate the Safety and Tolerability of Aripiprazole in Patients with Psychosis Associated with Parkinson’s Disease. Mov. Disord. 2006, 21, 2078–2081. [Google Scholar] [CrossRef] [PubMed]
- Meco, G.; Stirpe, P.; Edito, F.; Purcaro, C.; Valente, M.; Bernardi, S.; Vanacore, N. Aripiprazole in L-Dopa-Induced Dyskinesias: A One-Year Open-Label Pilot Study. J. Neural Transm. 2009, 116, 881–884. [Google Scholar] [CrossRef] [PubMed]
- Anttila, S.A.K.; Leinonen, E.V.J. A Review of the Pharmacological and Clinical Profile of Mirtazapine. CNS Drug Rev 2001, 7, 249–264. [Google Scholar] [CrossRef] [PubMed]
- Hamadjida, A.; Nuara, S.G.; Gourdon, J.C.; Huot, P. The Effect of Mianserin on the Severity of Psychosis and Dyskinesia in the Parkinsonian Marmoset. Prog. Neuropsychopharmacol. Biol. Psychiatry 2018, 81, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Hamadjida, A.; Nuara, S.G.; Veyres, N.; Frouni, I.; Kwan, C.; Sid-Otmane, L.; Harraka, M.J.; Gourdon, J.C.; Huot, P. The Effect of Mirtazapine on Dopaminergic Psychosis and Dyskinesia in the Parkinsonian Marmoset. Psychopharmacology 2017, 234, 905–911. [Google Scholar] [CrossRef]
- Meco, G.; Fabrizio, E.; Di Rezze, S.; Alessandri, A.; Pratesi, L. Mirtazapine in L-Dopa-Induced Dyskinesias. Clin. Neuropharmacol. 2003, 26, 179–181. [Google Scholar] [CrossRef]
- Aboulghasemi, N.; Hadipour Jahromy, M.; Ghasemi, A. Anti-Dyskinetic Efficacy of 5-Ht3 Receptor Antagonist in the Hemi-Parkinsonian Rat Model. IBRO Rep. 2019, 6, 40–44. [Google Scholar] [CrossRef]
- Asai, H.; Udaka, F.; Hirano, M.; Minami, T.; Oda, M.; Kubori, T.; Nishinaka, K.; Kameyama, M.; Ueno, S. Increased Gastric Motility During 5-HT4 Agonist Therapy Reduces Response Fluctuations in Parkinson’s Disease. Parkinsonism Relat. Disord. 2005, 11, 499–502. [Google Scholar] [CrossRef]
- Mendez-David, I.; David, D.J.; Darcet, F.; Wu, M.V.; Kerdine-Romer, S.; Gardier, A.M.; Hen, R. Rapid Anxiolytic Effects of a 5-HT(4) Receptor Agonist Are Mediated by a Neurogenesis-Independent Mechanism. Neuropsychopharmacology 2014, 39, 1366–1378. [Google Scholar] [CrossRef]
- Navailles, S.; Di Giovanni, G.; De Deurwaerdere, P. The 5-HT4 Agonist Prucalopride Stimulates L-DOPA-Induced Dopamine Release in Restricted Brain Regions of the Hemiparkinsonian Rat in Vivo. CNS Neurosci. Ther. 2015, 21, 745–747. [Google Scholar] [CrossRef]
- Liu, Y.; Liu, Z.; Li, F.; Kong, F. Therapeutic Effect of Mosapride Citrate on Gastrointestinal Tract Function Disorder of Patients with Parkinson’s Syndrome. J. Jilin Univ. Med. Ed. 2017, 43, 125–129. [Google Scholar]
- Sgambato-Faure, V.; Cenci, M.A. Glutamatergic Mechanisms in the Dyskinesias Induced by Pharmacological Dopamine Replacement and Deep Brain Stimulation for the Treatment of Parkinson’s Disease. Prog. Neurobiol. 2012, 96, 69–86. [Google Scholar] [CrossRef]
- Chase, T.N.; Oh, J.D.; Konitsiotis, S. Antiparkinsonian and Antidyskinetic Activity of Drugs Targeting Central Glutamatergic Mechanisms. J. Neurol. 2000, 247 (Suppl. 2), II36–42. [Google Scholar] [CrossRef]
- Cenci, M.A.; Ohlin, K.E.; Odin, P. Current Options and Future Possibilities for the Treatment of Dyskinesia and Motor Fluctuations in Parkinson’s Disease. CNS Neurol. Disord. Drug Targets 2011, 10, 670–684. [Google Scholar] [CrossRef]
- Rascol, O.; Fox, S.; Gasparini, F.; Kenney, C.; Di Paolo, T.; Gomez-Mancilla, B. Use of Metabotropic Glutamate 5-Receptor Antagonists for Treatment of Levodopa-Induced Dyskinesias. Parkinsonism Relat. Disord. 2014, 20, 947–956. [Google Scholar] [CrossRef]
- Mellone, M.; Stanic, J.; Hernandez, L.F.; Iglesias, E.; Zianni, E.; Longhi, A.; Prigent, A.; Picconi, B.; Calabresi, P.; Hirsch, E.C.; et al. NMDA Receptor Glun2a/Glun2b Subunit Ratio as Synaptic Trait of Levodopa-Induced Dyskinesias: From Experimental Models to Patients. Front. Cell. Neurosci. 2015, 9, 245. [Google Scholar] [CrossRef]
- Paille, V.; Picconi, B.; Bagetta, V.; Ghiglieri, V.; Sgobio, C.; Di Filippo, M.; Viscomi, M.T.; Giampa, C.; Fusco, F.R.; Gardoni, F.; et al. Distinct Levels of Dopamine Denervation Differentially Alter Striatal Synaptic Plasticity and NMDA Receptor Subunit Composition. J. Neurosci. 2010, 30, 14182–14193. [Google Scholar] [CrossRef]
- Calon, F.; Morissette, M.; Ghribi, O.; Goulet, M.; Grondin, R.; Blanchet, P.J.; Bedard, P.J.; Di Paolo, T. Alteration of Glutamate Receptors in the Striatum of Dyskinetic 1-Methyl-4-Phenyl-1,2,3,6-Tetrahydropyridine-Treated Monkeys Following Dopamine Agonist Treatment. Prog. Neuropsychopharmacol. Biol. Psychiatry 2002, 26, 127–138. [Google Scholar] [CrossRef]
- Calon, F.; Rajput, A.H.; Hornykiewicz, O.; Bédard, P.J.; Di Paolo, T. Levodopa-Induced Motor Complications Are Associated with Alterations of Glutamate Receptors in Parkinson’s Disease. Neurobiol. Dis. 2003, 14, 404–416. [Google Scholar] [CrossRef]
- Chase, T.N.; Oh, J.D. Striatal Dopamine- and Glutamate-Mediated Dysregulation in Experimental Parkinsonism. Trends Neurosci. 2000, 23, S86–S91. [Google Scholar] [CrossRef]
- Hadj Tahar, A.; Gregoire, L.; Darre, A.; Belanger, N.; Meltzer, L.; Bedard, P.J. Effect of a Selective Glutamate Antagonist on L-Dopa-Induced Dyskinesias in Drug-Naive Parkinsonian Monkeys. Neurobiol. Dis. 2004, 15, 171–176. [Google Scholar] [CrossRef]
- Morissette, M.; Dridi, M.; Calon, F.; Tahar, A.H.; Meltzer, L.T.; Bédard, P.J.; Di Paolo, T. Prevention of Dyskinesia by an NMDA Receptor Antagonist in MPTP Monkeys: Effect on Adenosine A2A Receptors. Synapse 2006, 60, 239–250. [Google Scholar] [CrossRef]
- Nash, J.E.; Fox, S.H.; Henry, B.; Hill, M.P.; Peggs, D.; McGuire, S.; Maneuf, Y.; Hille, C.; Brotchie, J.M.; Crossman, A.R. Antiparkinsonian Actions of Ifenprodil in the MPTP-Lesioned Marmoset Model of Parkinson’s Disease. Exp. Neurol. 2000, 165, 136–142. [Google Scholar] [CrossRef]
- Nash, J.E.; Ravenscroft, P.; McGuire, S.; Crossman, A.R.; Menniti, F.S.; Brotchie, J.M. The NR2B-Selective NMDA Receptor Antagonist CP-101,606 Exacerbates L-DOPA-Induced Dyskinesia and Provides Mild Potentiation of Anti-Parkinsonian Effects of L-DOPA in the MPTP-Lesioned Marmoset Model of Parkinson’s Disease. Exp. Neurol. 2004, 188, 471–479. [Google Scholar] [CrossRef]
- Nutt, J.G.; Gunzler, S.A.; Kirchhoff, T.; Hogarth, P.; Weaver, J.L.; Krams, M.; Jamerson, B.; Menniti, F.S.; Landen, J.W. Effects of a NR2B Selective NMDA Glutamate Antagonist, CP-101,606, on Dyskinesia and Parkinsonism. Mov. Disord. 2008, 23, 1860–1866. [Google Scholar] [CrossRef]
- Igarashi, M.; Habata, T.; Akita, H.; Noda, K.; Ogata, M.; Saji, M. The NR2B Antagonist, Ifenprodil, Corrects the L-Dopa-Induced Deficit of Bilateral Movement and Reduces C-Fos Expression in the Subthalamic Nucleus of Hemiparkinsonian Rats. Neurosci. Res. 2015, 96, 45–53. [Google Scholar] [CrossRef]
- Rylander, D.; Recchia, A.; Mela, F.; Dekundy, A.; Danysz, W.; Cenci, M.A. Pharmacological Modulation of Glutamate Transmission in a Rat Model of L-DOPA-Induced Dyskinesia: Effects on Motor Behavior and Striatal Nuclear Signaling. J. Pharmacol. Exp. Ther. 2009, 330, 227–235. [Google Scholar] [CrossRef]
- Wessell, R.H.; Ahmed, S.M.; Menniti, F.S.; Dunbar, G.L.; Chase, T.N.; Oh, J.D. NR2B Selective NMDA Receptor Antagonist CP-101,606 Prevents Levodopa-Induced Motor Response Alterations in Hemi-Parkinsonian Rats. Neuropharmacology 2004, 47, 184–194. [Google Scholar] [CrossRef]
- Michel, A.; Downey, P.; Van Damme, X.; De Wolf, C.; Schwarting, R.; Scheller, D. Behavioural Assessment of the A2a/NR2B Combination in the Unilateral 6-OHDA-Lesioned Rat Model: A New Method to Examine the Therapeutic Potential of Non-Dopaminergic Drugs. PLoS ONE 2015, 10, e0135949. [Google Scholar] [CrossRef]
- Michel, A.; Nicolas, J.-M.; Rose, S.; Jackson, M.; Colman, P.; Briône, W.; Sciberras, D.; Muglia, P.; Scheller, D.K.; Citron, M.; et al. Antiparkinsonian Effects of the "Radiprodil and Tozadenant" Combination in MPTP-Treated Marmosets. PLoS ONE 2017, 12, e0182887. [Google Scholar] [CrossRef]
- Snow, B.J.; Macdonald, L.; McAuley, D.; Wallis, W. The Effect of Amantadine on Levodopa-Induced Dyskinesias in Parkinson’s Disease: A Double-Blind, Placebo-Controlled Study. Clin. Neuropharmacol. 2000, 23, 82–85. [Google Scholar] [CrossRef] [PubMed]
- Wolf, E.; Seppi, K.; Katzenschlager, R.; Hochschorner, G.; Ransmayr, G.; Schwingenschuh, P.; Ott, E.; Kloiber, I.; Haubenberger, D.; Auff, E.; et al. Long-Term Antidyskinetic Efficacy of Amantadine in Parkinson’s Disease. Mov. Disord. 2010, 25, 1357–1363. [Google Scholar] [CrossRef]
- Sawada, H.; Oeda, T.; Kuno, S.; Nomoto, M.; Yamamoto, K.; Yamamoto, M.; Hisanaga, K.; Kawamura, T. Amantadine for Dyskinesias in Parkinson’s Disease: A Randomized Controlled Trial. PLoS ONE 2010, 5, e15298. [Google Scholar] [CrossRef] [PubMed]
- Perez-Lloret, S.; Rascol, O. Efficacy and Safety of Amantadine for the Treatment of L-DOPA-Induced Dyskinesia. J. Neural Transm. 2018, 125, 1237–1250. [Google Scholar] [CrossRef] [PubMed]
- Da Silva-Junior, F.P.; Braga-Neto, P.; Sueli Monte, F.; de Bruin, V.M. Amantadine Reduces the Duration of Levodopa-Induced Dyskinesia: A Randomized, Double-Blind, Placebo-Controlled Study. Parkinsonism Relat. Disord. 2005, 11, 449–452. [Google Scholar] [CrossRef] [PubMed]
- Ory-Magne, F.; Corvol, J.C.; Azulay, J.P.; Bonnet, A.M.; Brefel-Courbon, C.; Damier, P.; Dellapina, E.; Destee, A.; Durif, F.; Galitzky, M.; et al. Withdrawing Amantadine in Dyskinetic Patients with Parkinson Disease: The Amandysk Trial. Neurology 2014, 82, 300–307. [Google Scholar] [CrossRef]
- Thomas, A.; Iacono, D.; Luciano, A.L.; Armellino, K.; Di Iorio, A.; Onofrj, M. Duration of Amantadine Benefit on Dyskinesia of Severe Parkinson’s Disease. J. Neurol. Neurosurg. Psychiatry 2004, 75, 141–143. [Google Scholar] [PubMed]
- Bortolanza, M.; Bariotto-Dos-Santos, K.D.; Dos-Santos-Pereira, M.; da-Silva, C.A.; Del-Bel, E. Antidyskinetic Effect of 7-Nitroindazole and Sodium Nitroprusside Associated with Amantadine in a Rat Model of Parkinson’s Disease. Neurotox. Res. 2016, 30, 88–100. [Google Scholar] [CrossRef]
- Merello, M.; Nouzeilles, M.I.; Cammarota, A.; Leiguarda, R. Effect of Memantine (NMDA Antagonist) on Parkinson’s Disease: A Double-Blind Crossover Randomized Study. Clin. Neuropharmacol. 1999, 22, 273–276. [Google Scholar]
- Moreau, C.; Delval, A.; Tiffreau, V.; Defebvre, L.; Dujardin, K.; Duhamel, A.; Petyt, G.; Hossein-Foucher, C.; Blum, D.; Sablonniere, B.; et al. Memantine for Axial Signs in Parkinson’s Disease: A Randomised, Double-Blind, Placebo-Controlled Pilot Study. J. Neurol. Neurosurg. Psychiatry 2013, 84, 552–555. [Google Scholar] [CrossRef]
- Wictorin, K.; Widner, H. Memantine and Reduced Time with Dyskinesia in Parkinson’s Disease. Acta Neurol. Scand. 2016, 133, 355–360. [Google Scholar] [CrossRef] [PubMed]
- Paquette, M.A.; Anderson, A.M.; Lewis, J.R.; Meshul, C.K.; Johnson, S.W.; Paul Berger, S. MK-801 Inhibits L-DOPA-Induced Abnormal Involuntary Movements Only at Doses That Worsen Parkinsonism. Neuropharmacology 2010, 58, 1002–1008. [Google Scholar] [CrossRef] [PubMed]
- Flores, A.J.; Bartlett, M.J.; Root, B.K.; Parent, K.L.; Heien, M.L.; Porreca, F.; Polt, R.; Sherman, S.J.; Falk, T. The Combination of the Opioid Glycopeptide MMP-2200 and a NMDA Receptor Antagonist Reduced L-Dopa-Induced Dyskinesia and MMP-2200 by Itself Reduced Dopamine Receptor 2-Like Agonist-Induced Dyskinesia. Neuropharmacology 2018, 141, 260–271. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, M.J.; Joseph, R.M.; LePoidevin, L.M.; Parent, K.L.; Laude, N.D.; Lazarus, L.B.; Heien, M.L.; Estevez, M.; Sherman, S.J.; Falk, T. Long-Term Effect of Sub-Anesthetic Ketamine in Reducing L-DOPA-Induced Dyskinesias in a Preclinical Model. Neurosci. Lett. 2016, 612, 121–125. [Google Scholar] [CrossRef] [PubMed]
- Sherman, S.J.; Estevez, M.; Magill, A.B.; Falk, T. Case Reports Showing a Long-Term Effect of Subanesthetic Ketamine Infusion in Reducing L-Dopa-Induced Dyskinesias. Case Rep. Neurol. 2016, 8, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Santini, E.; Sgambato-Faure, V.; Li, Q.; Savasta, M.; Dovero, S.; Fisone, G.; Bezard, E. Distinct Changes in cAMP and Extracellular Signal-Regulated Protein Kinase Signalling in L-DOPA-Induced Dyskinesia. PLoS ONE 2010, 5, e12322. [Google Scholar] [CrossRef] [PubMed]
- Santini, E.; Valjent, E.; Usiello, A.; Carta, M.; Borgkvist, A.; Girault, J.A.; Herve, D.; Greengard, P.; Fisone, G. Critical Involvement of cAMP/DARPP-32 and Extracellular Signal-Regulated Protein Kinase Signaling in L-DOPA-Induced Dyskinesia. J. Neurosci. 2007, 27, 6995–7005. [Google Scholar] [CrossRef]
- Ba, M.; Kong, M.; Yang, H.; Ma, G.; Lu, G.; Chen, S.; Liu, Z. Changes in Subcellular Distribution and Phosphorylation of GluR1 in Lesioned Striatum of 6-Hydroxydopamine-Lesioned and L-Dopa-Treated Rats. Neurochem. Res. 2006, 31, 1337–1347. [Google Scholar] [CrossRef]
- Errico, F.; Bonito-Oliva, A.; Bagetta, V.; Vitucci, D.; Romano, R.; Zianni, E.; Napolitano, F.; Marinucci, S.; Di Luca, M.; Calabresi, P.; et al. Higher Free D-Aspartate and N-Methyl-D-Aspartate Levels Prevent Striatal Depotentiation and Anticipate L-DOPA-Induced Dyskinesia. Exp. Neurol. 2011, 232, 240–250. [Google Scholar] [CrossRef]
- Bibbiani, F.; Oh, J.D.; Kielaite, A.; Collins, M.A.; Smith, C.; Chase, T.N. Combined Blockade of AMPA and NMDA Glutamate Receptors Reduces Levodopa-Induced Motor Complications in Animal Models of PD. Exp. Neurol. 2005, 196, 422–429. [Google Scholar] [CrossRef]
- Kobylecki, C.; Cenci, M.A.; Crossman, A.R.; Ravenscroft, P. Calcium-Permeable AMPA Receptors Are Involved in the Induction and Expression of L-Dopa-Induced Dyskinesia in Parkinson’s Disease. J. Neurochem. 2010, 114, 499–511. [Google Scholar] [CrossRef]
- Konitsiotis, S.; Blanchet, P.J.; Verhagen, L.; Lamers, E.; Chase, T.N. AMPA Receptor Blockade Improves Levodopa-Induced Dyskinesia in MPTP Monkeys. Neurology 2000, 54, 1589–1595. [Google Scholar] [CrossRef]
- Vijayakumar, D.; Jankovic, J. Drug-Induced Dyskinesia, Part 1: Treatment of Levodopa-Induced Dyskinesia. Drugs 2016, 76, 759–777. [Google Scholar] [CrossRef]
- White, H.S.; Brown, S.D.; Woodhead, J.H.; Skeen, G.A.; Wolf, H.H. Topiramate Modulates GABA-Evoked Currents in Murine Cortical Neurons by a Nonbenzodiazepine Mechanism. Epilepsia 2000, 41 (Suppl. 1), S17–20. [Google Scholar] [CrossRef]
- Silverdale, M.A.; Nicholson, S.L.; Crossman, A.R.; Brotchie, J.M. Topiramate Reduces Levodopa-Induced Dyskinesia in the MPTP-Lesioned Marmoset Model of Parkinson’s Disease. Mov. Disord. 2005, 20, 403–409. [Google Scholar] [CrossRef]
- Kobylecki, C.; Hill, M.P.; Crossman, A.R.; Ravenscroft, P. Synergistic Antidyskinetic Effects of Topiramate and Amantadine in Animal Models of Parkinson’s Disease. Mov. Disord. 2011, 26, 2354–2363. [Google Scholar] [CrossRef]
- Kobylecki, C.; Burn, D.J.; Kass-Iliyya, L.; Kellett, M.W.; Crossman, A.R.; Silverdale, M.A. Randomized Clinical Trial of Topiramate for Levodopa-Induced Dyskinesia in Parkinson’s Disease. Parkinsonism Relat. Disord. 2014, 20, 452–455. [Google Scholar] [CrossRef]
- Eggert, K.; Squillacote, D.; Barone, P.; Dodel, R.; Katzenschlager, R.; Emre, M.; Lees, A.J.; Rascol, O.; Poewe, W.; Tolosa, E.; et al. Safety and Efficacy of Perampanel in Advanced Parkinson’s Disease: A Randomized, Placebo-Controlled Study. Mov. Disord. 2010, 25, 896–905. [Google Scholar] [CrossRef]
- Lees, A.; Fahn, S.; Eggert, K.M.; Jankovic, J.; Lang, A.; Micheli, F.; Maral Mouradian, M.; Oertel, W.H.; Olanow, C.W.; Poewe, W.; et al. Perampanel, an AMPA Antagonist, Found to Have No Benefit in Reducing “Off” Time in Parkinson’s Disease. Mov. Disord. 2012, 27, 284–288. [Google Scholar] [CrossRef]
- Rascol, O.; Barone, P.; Behari, M.; Emre, M.; Giladi, N.; Olanow, C.W.; Ruzicka, E.; Bibbiani, F.; Squillacote, D.; Patten, A.; et al. Perampanel in Parkinson Disease Fluctuations: A Double-Blind Randomized Trial with Placebo and Entacapone. Clin. Neuropharmacol. 2012, 35, 15–20. [Google Scholar] [CrossRef]
- Marin, C.; Jimenez, A.; Bonastre, M.; Vila, M.; Agid, Y.; Hirsch, E.C.; Tolosa, E. Ly293558, an AMPA Glutamate Receptor Antagonist, Prevents and Reverses Levodopa-Induced Motor Alterations in Parkinsonian Rats. Synapse 2001, 42, 40–47. [Google Scholar] [CrossRef]
- Litim, N.; Morissette, M.; Di Paolo, T. Metabotropic Glutamate Receptors as Therapeutic Targets in Parkinson’s Disease: An Update from the Last 5 Years of Research. Neuropharmacology 2017, 115, 166–179. [Google Scholar] [CrossRef]
- Sebastianutto, I.; Cenci, M.A. mGlu Receptors in the Treatment of Parkinson’s Disease and L-DOPA-Induced Dyskinesia. Curr. Opin. Pharm. 2018, 38, 81–89. [Google Scholar] [CrossRef]
- Murray, T.K.; Messenger, M.J.; Ward, M.A.; Woodhouse, S.; Osborne, D.J.; Duty, S.; O’Neill, M.J. Evaluation of the mGluR2/3 Agonist LY379268 in Rodent Models of Parkinson’s Disease. Pharmacol. Biochem. Behav. 2002, 73, 455–466. [Google Scholar] [CrossRef]
- Amalric, M.; Lopez, S.; Goudet, C.; Fisone, G.; Battaglia, G.; Nicoletti, F.; Pin, J.P.; Acher, F.C. Group III and Subtype 4 Metabotropic Glutamate Receptor Agonists: Discovery and Pathophysiological Applications in Parkinson’s Disease. Neuropharmacology 2013, 66, 53–64. [Google Scholar] [CrossRef]
- Le Poul, E.; Bolea, C.; Girard, F.; Poli, S.; Charvin, D.; Campo, B.; Bortoli, J.; Bessif, A.; Luo, B.; Koser, A.J.; et al. A Potent and Selective Metabotropic Glutamate Receptor 4 Positive Allosteric Modulator Improves Movement in Rodent Models of Parkinson’s Disease. J. Pharmacol. Exp. Ther. 2012, 343, 167–177. [Google Scholar] [CrossRef]
- Bennouar, K.E.; Uberti, M.A.; Melon, C.; Bacolod, M.D.; Jimenez, H.N.; Cajina, M.; Kerkerian-Le Goff, L.; Doller, D.; Gubellini, P. Synergy between L-DOPA and a Novel Positive Allosteric Modulator of Metabotropic Glutamate Receptor 4: Implications for Parkinson’s Disease Treatment and Dyskinesia. Neuropharmacology 2013, 66, 158–169. [Google Scholar] [CrossRef]
- Lopez, S.; Bonito-Oliva, A.; Pallottino, S.; Acher, F.; Fisone, G. Activation of Metabotropic Glutamate 4 Receptors Decreases L-DOPA-Induced Dyskinesia in a Mouse Model of Parkinson’s Disease. J. Parkinsons Dis. 2011, 1, 339–346. [Google Scholar]
- Iderberg, H.; Maslava, N.; Thompson, A.D.; Bubser, M.; Niswender, C.M.; Hopkins, C.R.; Lindsley, C.W.; Conn, P.J.; Jones, C.K.; Cenci, M.A. Pharmacological Stimulation of Metabotropic Glutamate Receptor Type 4 in a Rat Model of Parkinson’s Disease and L-DOPA-Induced Dyskinesia: Comparison between a Positive Allosteric Modulator and an Orthosteric Agonist. Neuropharmacology 2015, 95, 121–129. [Google Scholar] [CrossRef]
- Charvin, D.; Pomel, V.; Ortiz, M.; Frauli, M.; Scheffler, S.; Steinberg, E.; Baron, L.; Deshons, L.; Rudigier, R.; Thiarc, D.; et al. Discovery, Structure-Activity Relationship, and Antiparkinsonian Effect of a Potent and Brain-Penetrant Chemical Series of Positive Allosteric Modulators of Metabotropic Glutamate Receptor 4. J. Med. Chem. 2017, 60, 8515–8537. [Google Scholar] [CrossRef]
- Charvin, D.; Di Paolo, T.; Bezard, E.; Gregoire, L.; Takano, A.; Duvey, G.; Pioli, E.; Halldin, C.; Medori, R.; Conquet, F. An Mglu4-Positive Allosteric Modulator Alleviates Parkinsonism in Primates. Mov. Disord. 2018, 33, 1619–1631. [Google Scholar] [CrossRef] [PubMed]
- Marin, C.; Bonastre, M.; Aguilar, E.; Jimenez, A. The Metabotropic Glutamate Receptor Antagonist 2-Methyl-6-(Phenylethynyl) Pyridine Decreases Striatal VGlut2 Expression in Association with an Attenuation of L-DOPA-Induced Dyskinesias. Synapse 2011, 65, 1080–1086. [Google Scholar] [CrossRef] [PubMed]
- Mela, F.; Marti, M.; Dekundy, A.; Danysz, W.; Morari, M.; Cenci, M.A. Antagonism of Metabotropic Glutamate Receptor Type 5 Attenuates L-Dopa-Induced Dyskinesia and Its Molecular and Neurochemical Correlates in a Rat Model of Parkinson’s Disease. J. Neurochem. 2007, 101, 483–497. [Google Scholar] [CrossRef]
- Morin, N.; Gregoire, L.; Gomez-Mancilla, B.; Gasparini, F.; Di Paolo, T. Effect of the Metabotropic Glutamate Receptor Type 5 Antagonists MPEP and MTEP in Parkinsonian Monkeys. Neuropharmacology 2010, 58, 981–986. [Google Scholar] [CrossRef] [PubMed]
- Morin, N.; Morissette, M.; Gregoire, L.; Gomez-Mancilla, B.; Gasparini, F.; Di Paolo, T. Chronic Treatment with MPEP, an mGlu5 Receptor Antagonist, Normalizes Basal Ganglia Glutamate Neurotransmission in L-DOPA-Treated Parkinsonian Monkeys. Neuropharmacology 2013, 73, 216–231. [Google Scholar] [CrossRef] [PubMed]
- Rylander, D.; Iderberg, H.; Li, Q.; Dekundy, A.; Zhang, J.; Li, H.; Baishen, R.; Danysz, W.; Bezard, E.; Cenci, M.A. A mGluR5 Antagonist under Clinical Development Improves L-DOPA-Induced Dyskinesia in Parkinsonian Rats and Monkeys. Neurobiol. Dis. 2010, 39, 352–361. [Google Scholar] [CrossRef]
- Ko, W.K.; Pioli, E.; Li, Q.; McGuire, S.; Dufour, A.; Sherer, T.B.; Bezard, E.; Facheris, M.F. Combined Fenobam and Amantadine Treatment Promotes Robust Antidyskinetic Effects in the 1-Methyl-4-Phenyl-1,2,3,6-Tetrahydropyridine (MPTP)-Lesioned Primate Model of Parkinson’s Disease. Mov. Disord. 2014, 29, 772–779. [Google Scholar] [CrossRef]
- Fuzzati-Armentero, M.T.; Cerri, S.; Levandis, G.; Ambrosi, G.; Montepeloso, E.; Antoninetti, G.; Blandini, F.; Baqi, Y.; Muller, C.E.; Volpini, R.; et al. Dual Target Strategy: Combining Distinct Non-Dopaminergic Treatments Reduces Neuronal Cell Loss and Synergistically Modulates L-DOPA-Induced Rotational Behavior in a Rodent Model of Parkinson’s Disease. J. Neurochem. 2015, 134, 740–747. [Google Scholar] [CrossRef]
- Berg, D.; Godau, J.; Trenkwalder, C.; Eggert, K.; Csoti, I.; Storch, A.; Huber, H.; Morelli-Canelo, M.; Stamelou, M.; Ries, V.; et al. AFQ056 Treatment of Levodopa-Induced Dyskinesias: Results of 2 Randomized Controlled Trials. Mov. Disord. 2011, 26, 1243–1250. [Google Scholar] [CrossRef]
- Stocchi, F.; Rascol, O.; Destee, A.; Hattori, N.; Hauser, R.A.; Lang, A.E.; Poewe, W.; Stacy, M.; Tolosa, E.; Gao, H.; et al. AFQ056 in Parkinson Patients with Levodopa-Induced Dyskinesia: 13-Week, Randomized, Dose-Finding Study. Mov. Disord. 2013, 28, 1838–1846. [Google Scholar] [CrossRef]
- Trenkwalder, C.; Stocchi, F.; Poewe, W.; Dronamraju, N.; Kenney, C.; Shah, A.; von Raison, F.; Graf, A. Mavoglurant in Parkinson’s Patients with L-Dopa-Induced Dyskinesias: Two Randomized Phase 2 Studies. Mov. Disord. 2016, 31, 1054–1058. [Google Scholar] [CrossRef]
- Kumar, R.; Hauser, R.A.; Mostillo, J.; Dronamraju, N.; Graf, A.; Merschhemke, M.; Kenney, C. Mavoglurant (AFQ056) in Combination with Increased Levodopa Dosages in Parkinson’s Disease Patients. Int. J. Neurosci. 2016, 126, 20–24. [Google Scholar] [CrossRef]
- Tison, F.; Keywood, C.; Wakefield, M.; Durif, F.; Corvol, J.C.; Eggert, K.; Lew, M.; Isaacson, S.; Bezard, E.; Poli, S.M.; et al. A Phase 2a Trial of the Novel mGluR5-Negative Allosteric Modulator Dipraglurant for Levodopa-Induced Dyskinesia in Parkinson’s Disease. Mov. Disord. 2016, 31, 1373–1380. [Google Scholar] [CrossRef] [PubMed]
- Mitsukawa, K.; Yamamoto, R.; Ofner, S.; Nozulak, J.; Pescott, O.; Lukic, S.; Stoehr, N.; Mombereau, C.; Kuhn, R.; McAllister, K.H.; et al. A Selective Metabotropic Glutamate Receptor 7 Agonist: Activation of Receptor Signaling Via an Allosteric Site Modulates Stress Parameters in Vivo. Proc. Natl. Acad. Sci. USA 2005, 102, 18712–18717. [Google Scholar] [CrossRef] [PubMed]
- Broadstock, M.; Austin, P.J.; Betts, M.J.; Duty, S. Antiparkinsonian Potential of Targeting Group III Metabotropic Glutamate Receptor Subtypes in the Rodent Substantia Nigra Pars Reticulata. Br. J. Pharmacol. 2012, 165, 1034–1045. [Google Scholar] [CrossRef] [PubMed]
- Konieczny, J.; Lenda, T. Contribution of the mGluR7 Receptor to Antiparkinsonian-Like Effects in Rats: A Behavioral Study with the Selective Agonist AMN082. Pharmacol. Rep. 2013, 65, 1194–1203. [Google Scholar] [CrossRef]
- Johnson, K.A.; Jones, C.K.; Tantawy, M.N.; Bubser, M.; Marvanova, M.; Ansari, M.S.; Baldwin, R.M.; Conn, P.J.; Niswender, C.M. The Metabotropic Glutamate Receptor 8 Agonist (S)-3,4-DCPG Reverses Motor Deficits in Prolonged but Not Acute Models of Parkinson’s Disease. Neuropharmacology 2013, 66, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Foote, S.L.; Bloom, F.E.; Aston-Jones, G. Nucleus Locus Ceruleus: New Evidence of Anatomical and Physiological Specificity. Physiol. Rev. 1983, 63, 844–914. [Google Scholar] [CrossRef] [PubMed]
- Zarow, C.; Lyness, S.A.; Mortimer, J.A.; Chui, H.C. Neuronal Loss Is Greater in the Locus Coeruleus Than Nucleus Basalis and Substantia Nigra in Alzheimer and Parkinson Diseases. Arch. Neurol. 2003, 60, 337–341. [Google Scholar] [CrossRef] [PubMed]
- Fornai, F.; di Poggio, A.B.; Pellegrini, A.; Ruggieri, S.; Paparelli, A. Noradrenaline in Parkinson’s Disease: From Disease Progression to Current Therapeutics. Curr. Med. Chem. 2007, 14, 2330–2334. [Google Scholar] [CrossRef] [PubMed]
- McMillan, P.J.; White, S.S.; Franklin, A.; Greenup, J.L.; Leverenz, J.B.; Raskind, M.A.; Szot, P. Differential Response of the Central Noradrenergic Nervous System to the Loss of Locus Coeruleus Neurons in Parkinson’s Disease and Alzheimer’s Disease. Brain Res. 2011, 1373, 240–252. [Google Scholar] [CrossRef]
- Mavridis, M.; Degryse, A.D.; Lategan, A.J.; Marien, M.R.; Colpaert, F.C. Effects of Locus Coeruleus Lesions on Parkinsonian Signs, Striatal Dopamine and Substantia Nigra Cell Loss after 1-Methyl-4-Phenyl-1,2,3,6-Tetrahydropyridine in Monkeys: A Possible Role for the Locus Coeruleus in the Progression of Parkinson’s Disease. Neuroscience 1991, 41, 507–523. [Google Scholar] [CrossRef]
- Rommelfanger, K.S.; Edwards, G.L.; Freeman, K.G.; Liles, L.C.; Miller, G.W.; Weinshenker, D. Norepinephrine Loss Produces More Profound Motor Deficits Than MPTP Treatment in Mice. Proc. Natl. Acad. Sci. USA 2007, 104, 13804–13809. [Google Scholar] [CrossRef]
- Savola, J.M.; Hill, M.; Engstrom, M.; Merivuori, H.; Wurster, S.; McGuire, S.G.; Fox, S.H.; Crossman, A.R.; Brotchie, J.M. Fipamezole (JP-1730) Is a Potent Alpha2 Adrenergic Receptor Antagonist That Reduces Levodopa-Induced Dyskinesia in the MPTP-Lesioned Primate Model of Parkinson’s Disease. Mov. Disord. 2003, 18, 872–883. [Google Scholar] [CrossRef]
- Barnum, C.J.; Bhide, N.; Lindenbach, D.; Surrena, M.A.; Goldenberg, A.A.; Tignor, S.; Klioueva, A.; Walters, H.; Bishop, C. Effects of Noradrenergic Denervation on L-DOPA-Induced Dyskinesia and Its Treatment by A- and B-Adrenergic Receptor Antagonists in Hemiparkinsonian Rats. Pharmacol. Biochem. Behav. 2012, 100, 607–615. [Google Scholar] [CrossRef]
- Rascol, O.; Arnulf, I.; Peyro-Saint Paul, H.; Brefel-Courbon, C.; Vidailhet, M.; Thalamas, C.; Bonnet, A.M.; Descombes, S.; Bejjani, B.; Fabre, N.; et al. Idazoxan, an Alpha-2 Antagonist, and L-DOPA-Induced Dyskinesias in Patients with Parkinson’s Disease. Mov. Disord. 2001, 16, 708–713. [Google Scholar] [CrossRef]
- Johnston, T.H.; Fox, S.H.; Piggott, M.J.; Savola, J.M.; Brotchie, J.M. The Alpha(2) Adrenergic Antagonist Fipamezole Improves Quality of Levodopa Action in Parkinsonian Primates. Mov. Disord. 2010, 25, 2084–2093. [Google Scholar] [CrossRef]
- Dimitrova, T.; Bara-Jimenez, W.; Savola, J.; Encarnacion, E.; Mouradian, M.; Chase, T. Alpha-2 Adrenergic Antagonist Effects in Parkinson’s Disease; Neurology, 2011; Lippincott Williams & Wilkins 530 Walnut St: Philadelphia, PA, USA; p. A540.
- Lewitt, P.A.; Hauser, R.A.; Lu, M.; Nicholas, A.P.; Weiner, W.; Coppard, N.; Leinonen, M.; Savola, J.M. Randomized Clinical Trial of Fipamezole for Dyskinesia in Parkinson Disease (Fjord Study). Neurology 2012, 79, 163–169. [Google Scholar] [CrossRef]
- Rainbow, T.C.; Parsons, B.; Wolfe, B.B. Quantitative Autoradiography of Beta 1- and Beta 2-Adrenergic Receptors in Rat Brain. Proc. Natl. Acad. Sci. USA 1984, 81, 1585–1589. [Google Scholar] [CrossRef]
- Waeber, C.; Rigo, M.; Chinaglia, G.; Probst, A.; Palacios, J.M. Beta-Adrenergic Receptor Subtypes in the Basal Ganglia of Patients with Huntington’s Chorea and Parkinson’s Disease. Synapse 1991, 8, 270–280. [Google Scholar] [CrossRef]
- Bhide, N.; Lindenbach, D.; Barnum, C.J.; George, J.A.; Surrena, M.A.; Bishop, C. Effects of the Beta-Adrenergic Receptor Antagonist Propranolol on Dyskinesia and L-DOPA-Induced Striatal Da Efflux in the Hemi-Parkinsonian Rat. J. Neurochem. 2015, 134, 222–232. [Google Scholar] [CrossRef]
- Pagano, G.; Tan, E.E.; Haider, J.M.; Bautista, A.; Tagliati, M. Constipation Is Reduced by Beta-Blockers and Increased by Dopaminergic Medications in Parkinson’s Disease. Parkinsonism Relat. Disord. 2015, 21, 120–125. [Google Scholar] [CrossRef]
- Julius, A.; Longfellow, K. Movement Disorders: A Brief Guide in Medication Management. Med. Clin. N. Am. 2016, 100, 733–761. [Google Scholar] [CrossRef]
- Magistrelli, L.; Comi, C. Beta2-Adrenoceptor Agonists in Parkinson’s Disease and Other Synucleinopathies. J. Neuroimmune Pharmacol. 2019. [Google Scholar] [CrossRef]
- Latini, S.; Pedata, F. Adenosine in the Central Nervous System: Release Mechanisms and Extracellular Concentrations. J. Neurochem. 2001, 79, 463–484. [Google Scholar] [CrossRef]
- Ferré, S. Adenosine-Dopamine Interactions in the Ventral Striatum. Implications for the Treatment of Schizophrenia. Psychopharmacology 1997, 133, 107–120. [Google Scholar]
- Ferré, S.; Popoli, P.; Giménez-Llort, L.; Rimondini, R.; Müller, C.E.; Strömberg, I.; Ögren, S.O.; Fuxe, K. Adenosine/Dopamine Interaction: Implications for the Treatment of Parkinson’s Disease. Parkinsonism Relat. Disord. 2001, 7, 235–241. [Google Scholar] [CrossRef]
- Fastbom, J.; Pazos, A.; Palacios, J.M. The Distribution of Adenosine A1 Receptors and 5’-Nucleotidase in the Brain of Some Commonly Used Experimental Animals. Neuroscience 1987, 22, 813–826. [Google Scholar] [CrossRef]
- Mango, D.; Bonito-Oliva, A.; Ledonne, A.; Cappellacci, L.; Petrelli, R.; Nistico, R.; Berretta, N.; Fisone, G.; Mercuri, N.B. Adenosine A1 Receptor Stimulation Reduces D1 Receptor-Mediated Gabaergic Transmission from Striato-Nigral Terminals and Attenuates L-Dopa-Induced Dyskinesia in Dopamine-Denervated Mice. Exp. Neurol. 2014, 261, 733–743. [Google Scholar] [CrossRef]
- Ferre, S.; Quiroz, C.; Woods, A.S.; Cunha, R.; Popoli, P.; Ciruela, F.; Lluis, C.; Franco, R.; Azdad, K.; Schiffmann, S.N. An Update on Adenosine A2A-Dopamine D2 Receptor Interactions: Implications for the Function of G Protein-Coupled Receptors. Curr. Pharm. Des. 2008, 14, 1468–1474. [Google Scholar] [CrossRef]
- Pollack, A.E.; Fink, J.S. Adenosine Antagonists Potentiate D2 Dopamine-Dependent Activation of Fos in the Striatopallidal Pathway. Neuroscience 1995, 68, 721–728. [Google Scholar] [CrossRef]
- Zheng, J.; Zhang, X.; Zhen, X. Development of Adenosine A2A Receptor Antagonists for the Treatment of Parkinson’s Disease: A Recent Update and Challenge. ACS Chem. Neurosci. 2019, 10, 783–791. [Google Scholar] [CrossRef]
- Approval for Manufacturing and Marketing of Nouriast Tablets 20 Mg, a Novel Antiparkinsonian Agent, Kyowa Hakko Kirin Co Ltd Press Release. 25 March 2019. Available online: https://www.kyowa-kirin.com/news_releases/2013/e20130325_04.html (accessed on 9 April 2019).
- Lundblad, M.; Vaudano, E.; Cenci, M.A. Cellular and Behavioural Effects of the Adenosine A2a Receptor Antagonist KW-6002 in a Rat Model of L-Dopa-Induced Dyskinesia. J. Neurochem. 2003, 84, 1398–1410. [Google Scholar] [CrossRef]
- Kanda, T.; Jackson, M.J.; Smith, L.A.; Pearce, R.K.; Nakamura, J.; Kase, H.; Kuwana, Y.; Jenner, P. Adenosine A2A Antagonist: A Novel Antiparkinsonian Agent That Does Not Provoke Dyskinesia in Parkinsonian Monkeys. Ann. Neurol. 1998, 43, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Kanda, T.; Tashiro, T.; Kuwana, Y.; Jenner, P. Adenosine A2A Receptors Modify Motor Function in MPTP-Treated Common Marmosets. Neuroreport 1998, 9, 2857–2860. [Google Scholar] [CrossRef]
- Kanda, T.; Jackson, M.J.; Smith, L.A.; Pearce, R.K.; Nakamura, J.; Kase, H.; Kuwana, Y.; Jenner, P. Combined Use of the Adenosine A(2A) Antagonist KW-6002 with L-DOPA or with Selective D1 or D2 Dopamine Agonists Increases Antiparkinsonian Activity but Not Dyskinesia in MPTP-Treated Monkeys. Exp. Neurol. 2000, 162, 321–327. [Google Scholar] [CrossRef]
- Uchida, S.; Tashiro, T.; Kawai-Uchida, M.; Mori, A.; Jenner, P.; Kanda, T. Adenosine a(2)a-Receptor Antagonist Istradefylline Enhances the Motor Response of L-DOPA without Worsening Dyskinesia in MPTP-Treated Common Marmosets. J. Pharmacol. Sci. 2014, 124, 480–485. [Google Scholar] [CrossRef]
- Bibbiani, F.; Oh, J.D.; Petzer, J.P.; Castagnoli, N., Jr.; Chen, J.F.; Schwarzschild, M.A.; Chase, T.N. A2A Antagonist Prevents Dopamine Agonist-Induced Motor Complications in Animal Models of Parkinson’s Disease. Exp. Neurol. 2003, 184, 285–294. [Google Scholar] [CrossRef]
- Grondin, R.; Bedard, P.J.; Hadj Tahar, A.; Gregoire, L.; Mori, A.; Kase, H. Antiparkinsonian Effect of a New Selective Adenosine A2A Receptor Antagonist in MPTP-Treated Monkeys. Neurology 1999, 52, 1673–1677. [Google Scholar] [CrossRef]
- Ko, W.K.D.; Camus, S.M.; Li, Q.; Yang, J.; McGuire, S.; Pioli, E.Y.; Bezard, E. An Evaluation of Istradefylline Treatment on Parkinsonian Motor and Cognitive Deficits in 1-Methyl-4-Phenyl-1,2,3,6-Tetrahydropyridine (MPTP)-Treated Macaque Models. Neuropharmacology 2016, 110, 48–58. [Google Scholar] [CrossRef]
- Hauser, R.A.; Hubble, J.P.; Truong, D.D. Randomized Trial of the Adenosine A(2A) Receptor Antagonist Istradefylline in Advanced PD. Neurology 2003, 61, 297–303. [Google Scholar] [CrossRef]
- Hauser, R.A.; Shulman, L.M.; Trugman, J.M.; Roberts, J.W.; Mori, A.; Ballerini, R.; Sussman, N.M. Study of Istradefylline in Patients with Parkinson’s Disease on Levodopa with Motor Fluctuations. Mov. Disord. 2008, 23, 2177–2185. [Google Scholar] [CrossRef]
- Stacy, M.; Silver, D.; Mendis, T.; Sutton, J.; Mori, A.; Chaikin, P.; Sussman, N.M. A 12-Week, Placebo-Controlled Study (6002-US-006) of Istradefylline in Parkinson Disease. Neurology 2008, 70, 2233–2240. [Google Scholar] [CrossRef]
- LeWitt, P.A.; Guttman, M.; Tetrud, J.W.; Tuite, P.J.; Mori, A.; Chaikin, P.; Sussman, N.M.; Group, U.S.S. Adenosine A2A Receptor Antagonist Istradefylline (KW-6002) Reduces “Off” Time in Parkinson’s Disease: A Double-Blind, Randomized, Multicenter Clinical Trial (6002-US-005). Ann. Neurol. 2008, 63, 295–302. [Google Scholar] [CrossRef]
- Pourcher, E.; Fernandez, H.H.; Stacy, M.; Mori, A.; Ballerini, R.; Chaikin, P. Istradefylline for Parkinson’s Disease Patients Experiencing Motor Fluctuations: Results of the KW-6002-US-018 Study. Parkinsonism Relat. Disord. 2012, 18, 178–184. [Google Scholar] [CrossRef]
- Zhu, C.; Wang, G.; Li, J.; Chen, L.; Wang, C.; Wang, Y.; Lin, P.; Ran, H. Adenosine A2A Receptor Antagonist Istradefylline 20 Versus 40 Mg/Day as Augmentation for Parkinson’s Disease: A Meta-Analysis. Neurol. Res. 2014, 36, 1028–1034. [Google Scholar] [CrossRef]
- Kondo, T.; Mizuno, Y. A Long-Term Study of Istradefylline Safety and Efficacy in Patients with Parkinson Disease. Clin. Neuropharmacol. 2015, 38, 41–46. [Google Scholar] [CrossRef]
- Takahashi, M.; Fujita, M.; Asai, N.; Saki, M.; Mori, A. Safety and Effectiveness of Istradefylline in Patients with Parkinson’s Disease: Interim Analysis of a Post-Marketing Surveillance Study in Japan. Expert Opin. Pharmacother. 2018, 19, 1635–1642. [Google Scholar] [CrossRef]
- Torti, M.; Vacca, L.; Stocchi, F. Istradefylline for the Treatment of Parkinson’s Disease: Is It a Promising Strategy? Expert Opin. Pharmacother. 2018, 19, 1821–1828. [Google Scholar] [CrossRef]
- Hodgson, R.A.; Bedard, P.J.; Varty, G.B.; Kazdoba, T.M.; Di Paolo, T.; Grzelak, M.E.; Pond, A.J.; Hadjtahar, A.; Belanger, N.; Gregoire, L.; et al. Preladenant, a Selective A(2A) Receptor Antagonist, Is Active in Primate Models of Movement Disorders. Exp. Neurol. 2010, 225, 384–390. [Google Scholar] [CrossRef]
- Hodgson, R.A.; Bertorelli, R.; Varty, G.B.; Lachowicz, J.E.; Forlani, A.; Fredduzzi, S.; Cohen-Williams, M.E.; Higgins, G.A.; Impagnatiello, F.; Nicolussi, E.; et al. Characterization of the Potent and Highly Selective A2A Receptor Antagonists Preladenant and SCH 412348 [7-[2-[4-2,4-Difluorophenyl]-1-Piperazinyl]Ethyl]-2-(2-Furanyl)-7h-Pyrazolo[4,3-E][1,2,4]Triazolo[1,5-C]Pyrimidin-5-Amine] in Rodent Models of Movement Disorders and Depression. J. Pharmacol. Exp. Ther. 2009, 330, 294–303. [Google Scholar]
- Factor, S.A.; Wolski, K.; Togasaki, D.M.; Huyck, S.; Cantillon, M.; Ho, T.W.; Hauser, R.A.; Pourcher, E. Long-Term Safety and Efficacy of Preladenant in Subjects with Fluctuating Parkinson’s Disease. Mov. Disord. 2013, 28, 817–820. [Google Scholar] [CrossRef]
- Hauser, R.A.; Cantillon, M.; Pourcher, E.; Micheli, F.; Mok, V.; Onofrj, M.; Huyck, S.; Wolski, K. Preladenant in Patients with Parkinson’s Disease and Motor Fluctuations: A Phase 2, Double-Blind, Randomised Trial. Lacet. Neurol. 2011, 10, 221–229. [Google Scholar] [CrossRef]
- Hattori, N.; Kikuchi, M.; Adachi, N.; Hewitt, D.; Huyck, S.; Saito, T. Adjunctive Preladenant: A Placebo-Controlled, Dose-Finding Study in Japanese Patients with Parkinson’s Disease. Parkinsonism Relat. Disord. 2016, 32, 73–79. [Google Scholar] [CrossRef]
- Hauser, R.; Stocchi, F.; Rascol, O.; Huyck, S.; Ha, X.; Capece, R.; Wolski, K.; Ho, T.; Sklar, P.; Lines, C.; et al. Phase-3 Clinical Trials of Adjunctive Therapy with Preladenant, an Adenosine 2a Antagonist, in Patients with Parkinson’s Disease (P7.087). Neurology 2014, 82, P7.087. [Google Scholar]
- Hauser, R.A.; Stocchi, F.; Rascol, O.; Huyck, S.B.; Capece, R.; Ho, T.W.; Sklar, P.; Lines, C.; Michelson, D.; Hewitt, D. Preladenant as an Adjunctive Therapy with Levodopa in Parkinson Disease: Two Randomized Clinical Trials and Lessons Learned. JAMA neurol 2015, 72, 1491–1500. [Google Scholar] [CrossRef]
- Black, K.J.; Koller, J.M.; Campbell, M.C.; Gusnard, D.A.; Bandak, S.I. Quantification of Indirect Pathway Inhibition by the Adenosine A2a Antagonist SYN115 in Parkinson Disease. J. Neurosci. 2010, 30, 16284–16292. [Google Scholar] [CrossRef]
- Hauser, R.A.; Olanow, C.W.; Kieburtz, K.D.; Pourcher, E.; Docu-Axelerad, A.; Lew, M.; Kozyolkin, O.; Neale, A.; Resburg, C.; Meya, U.; et al. Tozadenant (SYN115) in Patients with Parkinson’s Disease Who Have Motor Fluctuations on Levodopa: A Phase 2b, Double-Blind, Randomised Trial. Lacet. Neurol. 2014, 13, 767–776. [Google Scholar] [CrossRef]
- Papapetropoulos, S.; Borgohain, R.; Kellet, M.; Giladi, N.; Tomic, D.; Coppell, A. The Adenosine A2A Receptor Antagonist BIIB014 Is Effective in Improving on-Time in Parkinson’s Disease (PD) Patients with Motor Fluctuations. Mov. Disord. 2010, 25, S305. [Google Scholar]
- Pawsey, S.; Donaldson, K.; Warrington, S.; Tranter, E. A Phase I Single and Repeated Dose Pharmacokinetic Study of Oral V81444, a Selective Non-Xanthine Adenosine A2A Receptor Antagonist. J. Neurol. Sci. 2013, 333, e135. [Google Scholar] [CrossRef]
- Núñez, F.; Taura, J.; Camacho, J.; López-Cano, M.; Fernández-Dueñas, V.; Castro, N.; Castro, J.; Ciruela, F. PBF509, an Adenosine A(2A) Receptor Antagonist with Efficacy in Rodent Models of Movement Disorders. Front. Pharmacol. 2018, 9, 1200. [Google Scholar] [CrossRef]
- Tronci, E.; Simola, N.; Borsini, F.; Schintu, N.; Frau, L.; Carminati, P.; Morelli, M. Characterization of the Antiparkinsonian Effects of the New Adenosine A2A Receptor Antagonist ST1535: Acute and Subchronic Studies in Rats. Eur. J. Pharmacol. 2007, 566, 94–102. [Google Scholar] [CrossRef]
- Rose, S.; Ramsay Croft, N.; Jenner, P. The Novel Adenosine A2a Antagonist ST1535 Potentiates the Effects of a Threshold Dose of L-Dopa in Unilaterally 6-OHDA-Lesioned Rats. Brain Res. 2007, 1133, 110–114. [Google Scholar] [CrossRef]
- Rose, S.; Jackson, M.J.; Smith, L.A.; Stockwell, K.; Johnson, L.; Carminati, P.; Jenner, P. The Novel Adenosine A2a Receptor Antagonist ST1535 Potentiates the Effects of a Threshold Dose of L-DOPA in MPTP Treated Common Marmosets. Eur. J. Pharmacol. 2006, 546, 82–87. [Google Scholar] [CrossRef]
- Pinna, A. Adenosine A2A Receptor Antagonists in Parkinson’s Disease: Progress in Clinical Trials from the Newly Approved Istradefylline to Drugs in Early Development and Those Already Discontinued. CNS Drugs 2014, 28, 455–474. [Google Scholar] [CrossRef]
- Bagga, P.; Chugani, A.N.; Patel, A.B. Neuroprotective Effects of Caffeine in MPTP Model of Parkinson’s Disease: A (13)C NMR Study. Neurochem. Int. 2016, 92, 25–34. [Google Scholar] [CrossRef]
- Rivera-Oliver, M.; Diaz-Rios, M. Using Caffeine and Other Adenosine Receptor Antagonists and Agonists as Therapeutic Tools against Neurodegenerative Diseases: A Review. Life Sci. 2014, 101, 1–9. [Google Scholar] [CrossRef]
- Roshan, M.H.; Tambo, A.; Pace, N.P. Potential Role of Caffeine in the Treatment of Parkinson’s Disease. Open Neurol. J. 2016, 10, 42–58. [Google Scholar] [CrossRef]
- Wills, A.-M.A.; Eberly, S.; Tennis, M.; Lang, A.E.; Messing, S.; Togasaki, D.; Tanner, C.M.; Kamp, C.; Chen, J.-F.; Oakes, D.; et al. Caffeine Consumption and Risk of Dyskinesia in Calm-PD. Mov. Disord. 2013, 28, 380–383. [Google Scholar] [CrossRef]
- Postuma, R.B.; Lang, A.E.; Munhoz, R.P.; Charland, K.; Pelletier, A.; Moscovich, M.; Filla, L.; Zanatta, D.; Rios Romenets, S.; Altman, R.; et al. Caffeine for Treatment of Parkinson Disease: A Randomized Controlled Trial. Neurology 2012, 79, 651–658. [Google Scholar] [CrossRef]
- Pilleri, M.; Antonini, A. Therapeutic Strategies to Prevent and Manage Dyskinesias in Parkinson’s Disease. Expert Opin. Drug Saf. 2015, 14, 281–294. [Google Scholar] [CrossRef]
- Lim, S.A.O.; Xia, R.; Ding, Y.; Won, L.; Ray, W.J.; Hitchcock, S.A.; McGehee, D.S.; Kang, U.J. Enhanced Histamine H2 Excitation of Striatal Cholinergic Interneurons in L-DOPA-Induced Dyskinesia. Neurobiol. Dis. 2015, 76, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Johnston, T.H.; van der Meij, A.; Brotchie, J.M.; Fox, S.H. Effect of Histamine H2 Receptor Antagonism on Levodopa-Induced Dyskinesia in the MPTP-Macaque Model of Parkinson’s Disease. Mov. Disord. 2010, 25, 1379–1390. [Google Scholar] [CrossRef]
- Mestre, T.A.; Shah, B.B.; Connolly, B.S.; de Aquino, C.; Al Dhakeel, A.; Walsh, R.; Ghate, T.; Lui, J.P.; Fox, S.H. Famotidine, a Histamine H2 Receptor Antagonist, Does Not Reduce Levodopa-Induced Dyskinesia in Parkinson’s Disease: A Proof-of-Concept Study. Mov. Disord. Clin. Pract. 2014, 1, 219–224. [Google Scholar] [CrossRef]
- Doi, H.; Sakakibara, R.; Sato, M.; Hirai, S.; Masaka, T.; Kishi, M.; Tsuyusaki, Y.; Tateno, A.; Tateno, F.; Takahashi, O.; et al. Nizatidine Ameliorates Gastroparesis in Parkinson’s Disease: A Pilot Study. Mov. Disord. 2014, 29, 562–566. [Google Scholar] [CrossRef] [PubMed]
- Sakakibara, R.; Doi, H.; Sato, M.; Hirai, S.; Masaka, T.; Kishi, M.; Tsuyusaki, Y.; Tateno, A.; Tateno, F.; Aiba, Y.; et al. Nizatidine Ameliorates Slow Transit Constipation in Parkinson’s Disease. J. Am. Geriatr. Soc. 2015, 63, 399–401. [Google Scholar] [CrossRef] [PubMed]
- Ferrada, C.; Ferre, S.; Casado, V.; Cortes, A.; Justinova, Z.; Barnes, C.; Canela, E.I.; Goldberg, S.R.; Leurs, R.; Lluis, C.; et al. Interactions between Histamine H3 and Dopamine D2 Receptors and the Implications for Striatal Function. Neuropharmacology 2008, 55, 190–197. [Google Scholar] [CrossRef]
- Masini, D.; Lopes-Aguiar, C.; Bonito-Oliva, A.; Papadia, D.; Andersson, R.; Fisahn, A.; Fisone, G. The Histamine H3 Receptor Antagonist Thioperamide Rescues Circadian Rhythm and Memory Function in Experimental Parkinsonism. Transl. Psychiatry 2017, 7, e1088. [Google Scholar] [CrossRef]
- Shan, L.; Bossers, K.; Luchetti, S.; Balesar, R.; Lethbridge, N.; Chazot, P.L.; Bao, A.M.; Swaab, D.F. Alterations in the Histaminergic System in the Substantia Nigra and Striatum of Parkinson’s Patients: A Postmortem Study. Neurobiol. Aging 2012, 33, 1488.e1–1488.e13. [Google Scholar] [CrossRef]
- Zhou, P.; Homberg, J.R.; Fang, Q.; Wang, J.; Li, W.; Meng, X.; Shen, J.; Luan, Y.; Liao, P.; Swaab, D.F.; et al. Histamine-4 Receptor Antagonist JNJ7777120 Inhibits Pro-Inflammatory Microglia and Prevents the Progression of Parkinson-Like Pathology and Behaviour in a Rat Model. Brain. Behav. Immun. 2019, 76, 61–73. [Google Scholar] [CrossRef]
- Bordia, T.; Perez, X.A. Cholinergic Control of Striatal Neurons to Modulate L-Dopa-Induced Dyskinesias. Eur. J. Neurosci. 2019, 49, 859–868. [Google Scholar] [CrossRef]
- Conti, M.M.; Chambers, N.; Bishop, C. A New Outlook on Cholinergic Interneurons in Parkinson’s Disease and L-DOPA-Induced Dyskinesia. Neurosci. Biobehav. Rev. 2018, 92, 67–82. [Google Scholar] [CrossRef]
- Perez, X.A.; Bordia, T.; Quik, M. The Striatal Cholinergic System in L-Dopa-Induced Dyskinesias. J. Neural Transm. 2018, 125, 1251–1262. [Google Scholar] [CrossRef]
- Freitas, M.E.; Fox, S.H. Nondopaminergic Treatments for Parkinson’s Disease: Current and Future Prospects. Neurodegener. Dis. Manag. 2016, 6, 249–268. [Google Scholar] [CrossRef]
- Zhang, H.; Bai, L.; He, J.; Zhong, L.; Duan, X.; Ouyang, L.; Zhu, Y.; Wang, T.; Zhang, Y.; Shi, J. Recent Advances in Discovery and Development of Natural Products As source for Anti-Parkinson’s Disease Lead Compounds. Eur. J. Med. Chem. 2017, 141, 257–272. [Google Scholar] [CrossRef]
- Montastruc, J.L.; Llau, M.E.; Rascol, O.; Senard, J.M. Drug-Induced Parkinsonism: A Review. Fund. Clin. Pharmacol. 1994, 8, 293–306. [Google Scholar] [CrossRef]
- Brocks, D.R. Anticholinergic Drugs Used in Parkinson’s Disease: An Overlooked Class of Drugs from a Pharmacokinetic Perspective. J. Pharm. Pharm. Sci. 1999, 2, 39–46. [Google Scholar]
- Fox, S.H.; Katzenschlager, R.; Lim, S.Y.; Ravina, B.; Seppi, K.; Coelho, M.; Poewe, W.; Rascol, O.; Goetz, C.G.; Sampaio, C. The Movement Disorder Society Evidence-Based Medicine Review Update: Treatments for the Motor Symptoms of Parkinson’s Disease. Mov. Disord. 2011, 26 (Suppl. 3), S2–41. [Google Scholar] [CrossRef]
- Ding, Y.; Won, L.; Britt, J.P.; Lim, S.A.; McGehee, D.S.; Kang, U.J. Enhanced Striatal Cholinergic Neuronal Activity Mediates L-DOPA-Induced Dyskinesia in Parkinsonian Mice. Proc. Natl. Acad. Sci. USA 2011, 108, 840–845. [Google Scholar] [CrossRef]
- Ztaou, S.; Lhost, J.; Watabe, I.; Torromino, G.; Amalric, M. Striatal Cholinergic Interneurons Regulate Cognitive and Affective Dysfunction in Partially Dopamine-Depleted Mice. Eur. J. Neurosci. 2018, 48, 2988–3004. [Google Scholar] [CrossRef]
- Kostelnik, A.; Cegan, A.; Pohanka, M. Anti-Parkinson Drug Biperiden Inhibits Enzyme Acetylcholinesterase. BioMed Res. Int. 2017, 2017, 2532764. [Google Scholar] [CrossRef]
- Shen, W.; Plotkin, J.L.; Francardo, V.; Ko, W.K.; Xie, Z.; Li, Q.; Fieblinger, T.; Wess, J.; Neubig, R.R.; Lindsley, C.W.; et al. M4 Muscarinic Receptor Signaling Ameliorates Striatal Plasticity Deficits in Models of L-DOPA-Induced Dyskinesia. Neuron 2015, 88, 762–773. [Google Scholar] [CrossRef]
- Exley, R.; Clements, M.A.; Hartung, H.; McIntosh, J.M.; Franklin, M.; Bermudez, I.; Cragg, S.J. Striatal Dopamine Transmission Is Reduced after Chronic Nicotine with a Decrease in Alpha6-Nicotinic Receptor Control in Nucleus Accumbens. Eur. J. Neurosci. 2013, 38, 3036–3043. [Google Scholar]
- Kosillo, P.; Zhang, Y.-F.; Threlfell, S.; Cragg, S.J. Cortical Control of Striatal Dopamine Transmission Via Striatal Cholinergic Interneurons. Cereb. Cortex 2016, 26, 4160–4169. [Google Scholar] [CrossRef]
- Luo, R.; Janssen, M.J.; Partridge, J.G.; Vicini, S. Direct and GABA-Mediated Indirect Effects of Nicotinic Ach Receptor Agonists on Striatal Neurones. J. Physiol. 2013, 591, 203–217. [Google Scholar] [CrossRef]
- Quik, M.; Zhang, D.; McGregor, M.; Bordia, T. Alpha7 Nicotinic Receptors as Therapeutic Targets for Parkinson’s Disease. Biochem. Pharmacol. 2015, 97, 399–407. [Google Scholar] [CrossRef]
- Brumberg, J.; Küsters, S.; Al-Momani, E.; Marotta, G.; Cosgrove, K.P.; van Dyck, C.H.; Herrmann, K.; Homola, G.A.; Pezzoli, G.; Buck, A.K.; et al. Cholinergic Activity and Levodopa-Induced Dyskinesia: A Multitracer Molecular Imaging Study. Ann. Clin. Transl. Neurol. 2017, 4, 632–639. [Google Scholar] [CrossRef]
- Dajas-Bailador, F.; Wonnacott, S. Nicotinic Acetylcholine Receptors and the Regulation of Neuronal Signalling. Trends Pharmacol. Sci. 2004, 25, 317–324. [Google Scholar] [CrossRef]
- Garcia-Montes, J.R.; Boronat-Garcia, A.; Lopez-Colome, A.M.; Bargas, J.; Guerra-Crespo, M.; Drucker-Colin, R. Is Nicotine Protective against Parkinson’s Disease? An Experimental Analysis. CNS Neurol. Disord. Drug Targets 2012, 11, 897–906. [Google Scholar] [CrossRef]
- Perez, X.A.; Ly, J.; McIntosh, J.M.; Quik, M. Long-Term Nicotine Exposure Depresses Dopamine Release in Nonhuman Primate Nucleus Accumbens. J. Pharmacol. Exp. Ther. 2012, 342, 335–344. [Google Scholar] [CrossRef]
- Perez, X.A.; McIntosh, J.M.; Quik, M. Long-Term Nicotine Treatment Down-Regulates Alpha6beta2* Nicotinic Receptor Expression and Function in Nucleus Accumbens. J. Neurochem. 2013, 127, 762–771. [Google Scholar] [CrossRef]
- Bordia, T.; Campos, C.; McIntosh, J.M.; Quik, M. Nicotinic Receptor-Mediated Reduction in L-DOPA-Induced Dyskinesias May Occur Via Desensitization. J. Pharmacol. Exp. Ther. 2010, 333, 929–938. [Google Scholar] [CrossRef]
- Bordia, T.; Campos, C.; Huang, L.; Quik, M. Continuous and Intermittent Nicotine Treatment Reduces L-3,4-Dihydroxyphenylalanine (L-DOPA)-Induced Dyskinesias in a Rat Model of Parkinson’s Disease. J. Pharmacol. Exp. Ther. 2008, 327, 239–247. [Google Scholar] [CrossRef]
- Bordia, T.; McGregor, M.; McIntosh, J.M.; Drenan, R.M.; Quik, M. Evidence for a Role for α6(∗) Nachrs in L-Dopa-Induced Dyskinesias Using Parkinsonian α6(∗) nAChR Gain-of-Function Mice. Neuroscience 2015, 295, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Bordia, T.; McIntosh, J.M.; Quik, M. The Nicotine-Mediated Decline in L-Dopa-Induced Dyskinesias Is Associated with a Decrease in Striatal Dopamine Release. J. Neurochem. 2013, 125, 291–302. [Google Scholar] [CrossRef] [PubMed]
- Bordia, T.; Zhang, D.; Perez, X.A.; Quik, M. Striatal Cholinergic Interneurons and D2 Receptor-Expressing Gabaergic Medium Spiny Neurons Regulate Tardive Dyskinesia. Exp. Neurol. 2016, 286, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.Z.; Campos, C.; Ly, J.; Ivy Carroll, F.; Quik, M. Nicotinic Receptor Agonists Decrease L-Dopa-Induced Dyskinesias Most Effectively in Partially Lesioned Parkinsonian Rats. Neuropharmacology 2011, 60, 861–868. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.Z.; Grady, S.R.; Quik, M. Nicotine Reduces L-DOPA-Induced Dyskinesias by Acting at Beta2* Nicotinic Receptors. J. Pharmacol. Exp. Ther. 2011, 338, 932–941. [Google Scholar] [CrossRef] [PubMed]
- Quik, M.; Campos, C.; Bordia, T.; Strachan, J.P.; Zhang, J.; McIntosh, J.M.; Letchworth, S.; Jordan, K. Alpha4beta2 Nicotinic Receptors Play a Role in the nAChR-Mediated Decline in L-Dopa-Induced Dyskinesias in Parkinsonian Rats. Neuropharmacology 2013, 71, 191–203. [Google Scholar] [CrossRef]
- Quik, M.; Campos, C.; Grady, S.R. Multiple Cns Nicotinic Receptors Mediate L-Dopa-Induced Dyskinesias: Studies with Parkinsonian Nicotinic Receptor Knockout Mice. Biochem. Pharmacol. 2013, 86, 1153–1162. [Google Scholar] [CrossRef]
- Quik, M.; Mallela, A.; Ly, J.; Zhang, D. Nicotine Reduces Established Levodopa-Induced Dyskinesias in a Monkey Model of Parkinson’s Disease. Mov. Disord. 2013, 28, 1398–1406. [Google Scholar] [CrossRef]
- Quik, M.; Park, K.M.; Hrachova, M.; Mallela, A.; Huang, L.Z.; McIntosh, J.M.; Grady, S.R. Role for Alpha6 Nicotinic Receptors in L-Dopa-Induced Dyskinesias in Parkinsonian Mice. Neuropharmacology 2012, 63, 450–459. [Google Scholar] [CrossRef]
- Quik, M.; Zhang, D.; Perez, X.A.; Bordia, T. Role for the Nicotinic Cholinergic System in Movement Disorders; Therapeutic Implications. Pharmacol. Ther. 2014, 144, 50–59. [Google Scholar] [CrossRef]
- Barreto, G.E.; Iarkov, A.; Moran, V.E. Beneficial Effects of Nicotine, Cotinine and Its Metabolites as Potential Agents for Parkinson’s Disease. Front. Aging Neurosci. 2014, 6, 340. [Google Scholar]
- Quik, M.; Bordia, T.; Zhang, D.; Perez, X.A. Nicotine and Nicotinic Receptor Drugs: Potential for Parkinson’s Disease and Drug-Induced Movement Disorders. Int. Rev. Neurobiol. 2015, 124, 247–271. [Google Scholar]
- Leino, S.; Koski, S.K.; Rannanpää, S.; Salminen, O. Effects of Antidyskinetic Nicotine Treatment on Dopamine Release in Dorsal and Ventral Striatum. Neurosci. Lett. 2018, 672, 40–45. [Google Scholar] [CrossRef]
- Zhang, D.; McGregor, M.; Bordia, T.; Perez, X.A.; McIntosh, J.M.; Decker, M.W.; Quik, M. A7 Nicotinic Receptor Agonists Reduce Levodopa-Induced Dyskinesias with Severe Nigrostriatal Damage. Mov. Disord. 2015, 30, 1901–1911. [Google Scholar] [CrossRef]
- Zhang, D.; McGregor, M.; Decker, M.W.; Quik, M. The Alpha7 Nicotinic Receptor Agonist ABT-107 Decreases L-Dopa-Induced Dyskinesias in Parkinsonian Monkeys. J. Pharmacol. Exp. Ther. 2014, 351, 25–32. [Google Scholar] [CrossRef]
- Di Paolo, T.; Grégoire, L.; Feuerbach, D.; Elbast, W.; Weiss, M.; Gomez-Mancilla, B. AQW051, a Novel and Selective Nicotinic Acetylcholine Receptor α7 Partial Agonist, Reduces L-Dopa-Induced Dyskinesias and Extends the Duration of L-Dopa Effects in Parkinsonian Monkeys. Parkinsonism Relat. Disord. 2014, 20, 1119–1123. [Google Scholar] [CrossRef]
- Trenkwalder, C.; Berg, D.; Rascol, O.; Eggert, K.; Ceballos-Baumann, A.; Corvol, J.-C.; Storch, A.; Zhang, L.; Azulay, J.-P.; Broussolle, E.; et al. A Placebo-Controlled Trial of AQW051 in Patients with Moderate to Severe Levodopa-Induced Dyskinesia. Mov. Disord. 2016, 31, 1049–1054. [Google Scholar] [CrossRef]
- Mather, J.; Burdette, C.; Posener, A. In Potential of Azd1446, a Novel Nicotinic Agonist, for the Treatment of L-DOPA-Induced Dyskinesia in Parkinson’s Disease, Society for Neuroscience Abstr, 2014; p L1.
- Zhang, D.; Bordia, T.; McGregor, M.; McIntosh, J.M.; Decker, M.W.; Quik, M. ABT-089 and ABT-894 Reduce Levodopa-Induced Dyskinesias in a Monkey Model of Parkinson’s Disease. Mov. Disord. 2014, 29, 508–517. [Google Scholar] [CrossRef]
- Leino, S.; Koski, S.K.; Hanninen, R.; Tapanainen, T.; Rannanpaa, S.; Salminen, O. Attenuated Dopaminergic Neurodegeneration and Motor Dysfunction in Hemiparkinsonian Mice Lacking the Alpha5 Nicotinic Acetylcholine Receptor Subunit. Neuropharmacology 2018, 138, 371–380. [Google Scholar] [CrossRef]
- O’Gorman Tuura, R.L.; Baumann, C.R.; Baumann-Vogel, H. Beyond Dopamine: GABA, Glutamate, and the Axial Symptoms of Parkinson Disease. Front. Neurol. 2018, 9, 806. [Google Scholar] [CrossRef]
- Błasczyk, J.W. Parkinson’s Disease and Neurodegeneration: GABA-Collapse Hypothesis. Front. Neurosci. 2016, 10, 269. [Google Scholar]
- Assini, R.; Abercrombie, E.D. Zolpidem Ameliorates Motor Impairments in the Unilaterally 6-Hydroxydopamine-Lesioned Rat. Eur. J. Neurosci. 2018, 48, 1896–1905. [Google Scholar] [CrossRef]
- Yang, X.; Zhao, H.; Shi, H.; Wang, X.; Zhang, S.; Zhang, Z.; Zu, J.; Zhang, W.; Shen, X.; Cui, G.; et al. Intranigral Administration of Substance P Receptor Antagonist Attenuated Levodopa-Induced Dyskinesia in a Rat Model of Parkinson’s Disease. Exp. Neurol. 2015, 271, 168–174. [Google Scholar] [CrossRef]
- Thornton, E.; Hassall, M.M.; Corrigan, F.; Vink, R. The Nk1 Receptor Antagonist N-Acetyl-L-Tryptophan Reduces Dyskinesia in a Hemi-Parkinsonian Rodent Model. Parkinsonism Relat. Disord. 2014, 20, 508–513. [Google Scholar] [CrossRef]
- Mabrouk, O.S. Delta Opioid Pharmacology in Parkinson’s Disease. In Delta Opioid Receptor Pharmacology and Therapeutic Applications; Jutkiewicz, E.M., Ed.; Springer International Publishing: Cham, Switzerland, 2018. [Google Scholar] [CrossRef]
- Huang, J.-Z.; Ren, Y.; Xu, Y.; Chen, T.; Xia, T.C.; Li, Z.-R.; Zhao, J.-N.; Hua, F.; Sheng, S.-Y.; Xia, Y. The Delta-Opioid Receptor and Parkinson’s Disease. CNS Neurosci. Ther. 2018, 24, 1089–1099. [Google Scholar] [CrossRef]
- Sgroi, S.; Tonini, R. Opioidergic Modulation of Striatal Circuits, Implications in Parkinson’s Disease and Levodopa Induced Dyskinesia. Front. Neurol. 2018, 9, 524. [Google Scholar] [CrossRef]
- Freo, U.; Furnari, M.; Ori, C. Effects of Tapentadol on Pain, Motor Symptoms and Cognitive Functions in Parkinson’s Disease. J. Pain Res. 2018, 11, 1849–1856. [Google Scholar] [CrossRef]
- Henry, B.; Fox, S.H.; Crossman, A.R.; Brotchie, J.M. Mu- and Delta-Opioid Receptor Antagonists Reduce Levodopa-Induced Dyskinesia in the MPTP-Lesioned Primate Model of Parkinson’s Disease. Exp. Neurol. 2001, 171, 139–146. [Google Scholar] [CrossRef]
- Koprich, J.B.; Fox, S.H.; Johnston, T.H.; Goodman, A.; Le Bourdonnec, B.; Dolle, R.E.; DeHaven, R.N.; DeHaven-Hudkins, D.L.; Little, P.J.; Brotchie, J.M. The Selective Mu-Opioid Receptor Antagonist Adl5510 Reduces Levodopa-Induced Dyskinesia without Affecting Antiparkinsonian Action in MPTP-Lesioned Macaque Model of Parkinson’s Disease. Mov. Disord. 2011, 26, 1225–1233. [Google Scholar] [CrossRef]
- Billet, F.; Costentin, J.; Dourmap, N. Influence of Corticostriatal Δ-Opioid Receptors on Abnormal Involuntary Movements Induced by L-DOPA in Hemiparkinsonian Rats. Exp. Neurol. 2012, 236, 339–350. [Google Scholar] [CrossRef]
- Hudzik, T.J.; Howell, A.; Payza, K.; Cross, A.J. Antiparkinson Potential of Delta-Opioid Receptor Agonists. Eur. J. Pharmacol. 2000, 396, 101–107. [Google Scholar] [CrossRef]
- Nozaki, C.; Le Bourdonnec, B.; Reiss, D.; Windh, R.T.; Little, P.J.; Dolle, R.E.; Kieffer, B.L.; Gaveriaux-Ruff, C. Delta-Opioid Mechanisms for Adl5747 and ADL5859 Effects in Mice: Analgesia, Locomotion, and Receptor Internalization. J. Pharmacol. Exp. Ther. 2012, 342, 799–807. [Google Scholar] [CrossRef]
- Spina, L.; Longoni, R.; Mulas, A.; Chang, K.J.; Di Chiara, G. Dopamine-Dependent Behavioural Stimulation by Non-Peptide Delta Opioids BW373U86 and SNC 80: 1. Locomotion, Rearing and Stereotypies in Intact Rats. Behav. Pharmacol. 1998, 9, 1–8. [Google Scholar]
- Cox, H.; Togasaki, D.M.; Chen, L.; Langston, J.W.; Di Monte, D.A.; Quik, M. The Selective Kappa-Opioid Receptor Agonist U50,488 Reduces L-Dopa-Induced Dyskinesias but Worsens Parkinsonism in MPTP-Treated Primates. Exp. Neurol. 2007, 205, 101–107. [Google Scholar] [CrossRef][Green Version]
- Potts, L.F.; Park, E.S.; Woo, J.M.; Dyavar Shetty, B.L.; Singh, A.; Braithwaite, S.P.; Voronkov, M.; Papa, S.M.; Mouradian, M.M. Dual Κ-Agonist/Μ-Antagonist Opioid Receptor Modulation Reduces Levodopa-Induced Dyskinesia and Corrects Dysregulated Striatal Changes in the Nonhuman Primate Model of Parkinson Disease. Ann. Neurol. 2015, 77, 930–941. [Google Scholar] [CrossRef]
- Klintenberg, R.; Svenningsson, P.; Gunne, L.; Andren, P.E. Naloxone Reduces Levodopa-Induced Dyskinesias and Apomorphine-Induced Rotations in Primate Models of Parkinsonism. J. Neural Transm. 2002, 109, 1295–1307. [Google Scholar] [CrossRef]
- Fox, S.; Silverdale, M.; Kellett, M.; Davies, R.; Steiger, M.; Fletcher, N.; Crossman, A.; Brotchie, J. Non-Subtype-Selective Opioid Receptor Antagonism in Treatment of Levodopa-Induced Motor Complications in Parkinson’s Disease. Mov. Disord. 2004, 19, 554–560. [Google Scholar] [CrossRef]
- Gomez-Mancilla, B.; Bedard, P.J. Effect of Nondopaminergic Drugs on L-Dopa-Induced Dyskinesias in MPTP-Treated Monkeys. Clin. Neuropharmacol. 1993, 16, 418–427. [Google Scholar] [CrossRef] [PubMed]
- Johnston, T.H.; Versi, E.; Howson, P.A.; Ravenscroft, P.; Fox, S.H.; Hill, M.P.; Reidenberg, B.E.; Corey, R.; Brotchie, J.M. DPI-289, a Novel Mixed Delta Opioid Agonist / Mu Opioid Antagonist (DAMA), Has L-DOPA-Sparing Potential in Parkinson’s Disease. Neuropharmacology 2018, 131, 116–127. [Google Scholar] [CrossRef] [PubMed]
- Lowery, J.J.; Raymond, T.J.; Giuvelis, D.; Bidlack, J.M.; Polt, R.; Bilsky, E.J. In Vivo Characterization of MMP-2200, a Mixed Delta/Mu Opioid Agonist, in Mice. J. Pharmacol. Exp. Ther. 2011, 336, 767–778. [Google Scholar] [CrossRef] [PubMed]
- Su, T.P.; London, E.D.; Jaffe, J.H. Steroid Binding at Sigma Receptors Suggests a Link between Endocrine, Nervous, and Immune Systems. Science 1988, 240, 219–221. [Google Scholar] [CrossRef] [PubMed]
- Konitsiotis, S. Novel Pharmacological Strategies for Motor Complications in Parkinson’s Disease. Expert Opin. Investig. Drugs 2005, 14, 377–392. [Google Scholar] [CrossRef]
- Mishina, M.; Ishiwata, K.; Ishii, K.; Kitamura, S.; Kimura, Y.; Kawamura, K.; Oda, K.; Sasaki, T.; Sakayori, O.; Hamamoto, M.; et al. Function of Sigma1 Receptors in Parkinson’s Disease. Acta Neurol. Scand. 2005, 112, 103–107. [Google Scholar] [CrossRef]
- Francardo, V.; Bez, F.; Wieloch, T.; Nissbrandt, H.; Ruscher, K.; Cenci, M.A. Pharmacological Stimulation of Sigma-1 Receptors Has Neurorestorative Effects in Experimental Parkinsonism. Brain 2014, 137, 1998–2014. [Google Scholar] [CrossRef]
- Paquette, M.A.; Foley, K.; Brudney, E.G.; Meshul, C.K.; Johnson, S.W.; Berger, S.P. The Sigma-1 Antagonist Bmy-14802 Inhibits L-DOPA-Induced Abnormal Involuntary Movements by a Way-100635-Sensitive Mechanism. Psychopharmacology 2009, 204, 743–754. [Google Scholar] [CrossRef]
- Tsai, S.Y.; Pokrass, M.J.; Klauer, N.R.; De Credico, N.E.; Su, T.P. Sigma-1 Receptor Chaperones in Neurodegenerative and Psychiatric Disorders. Expert Opin. Ther. Targets 2014, 18, 1461–1476. [Google Scholar] [CrossRef]
- Verhagen-Metman, L.; Blanchet, P.J.; van den Munckhof, P.; Del Dotto, P.; Natté, R.; Chase, T.N. A Trial of Dextromethorphan in Parkinsonian Patients with Motor Response Complications. Mov. Disord. 1998, 13, 414–417. [Google Scholar] [CrossRef]
- Fox, S.H.; Metman, L.V.; Nutt, J.G.; Brodsky, M.; Factor, S.A.; Lang, A.E.; Pope, L.E.; Knowles, N.; Siffert, J. Trial of Dextromethorphan/Quinidine to Treat Levodopa-Induced Dyskinesia in Parkinson’s Disease. Mov. Disord. 2017, 32, 893–903. [Google Scholar] [CrossRef]
- Johnston, T.H.; Geva, M.; Steiner, L.; Orbach, A.; Papapetropoulos, S.; Savola, J.M.; Reynolds, I.J.; Ravenscroft, P.; Hill, M.; Fox, S.H.; et al. Pridopidine, a Clinic-Ready Compound, Reduces 3,4-Dihydroxyphenylalanine-Induced Dyskinesia in Parkinsonian Macaques. Mov. Disord. 2018. [Google Scholar] [CrossRef]
- Parkinson, J. An Essay on the Shaking Palsy. 1817. J. Neuropsychiatry. Clin. Neurosci. 2002, 14, 223–236, discussion 222. [Google Scholar] [CrossRef]
- Schaeffer, E.; Pilotto, A.; Berg, D. Pharmacological Strategies for the Management of Levodopa-Induced Dyskinesia in Patients with Parkinson’s Disease. CNS Drugs 2014, 28, 1155–1184. [Google Scholar] [CrossRef]
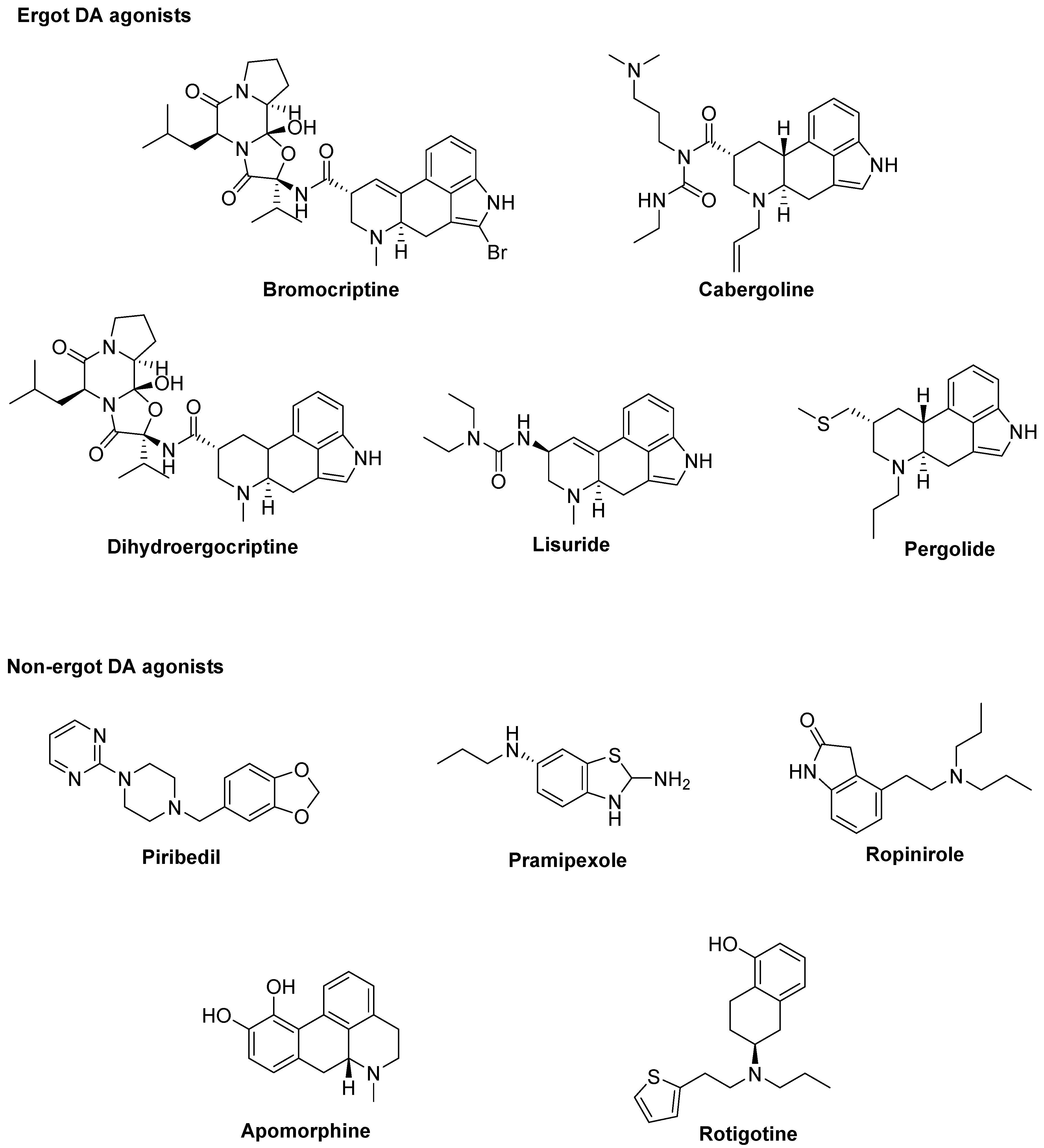
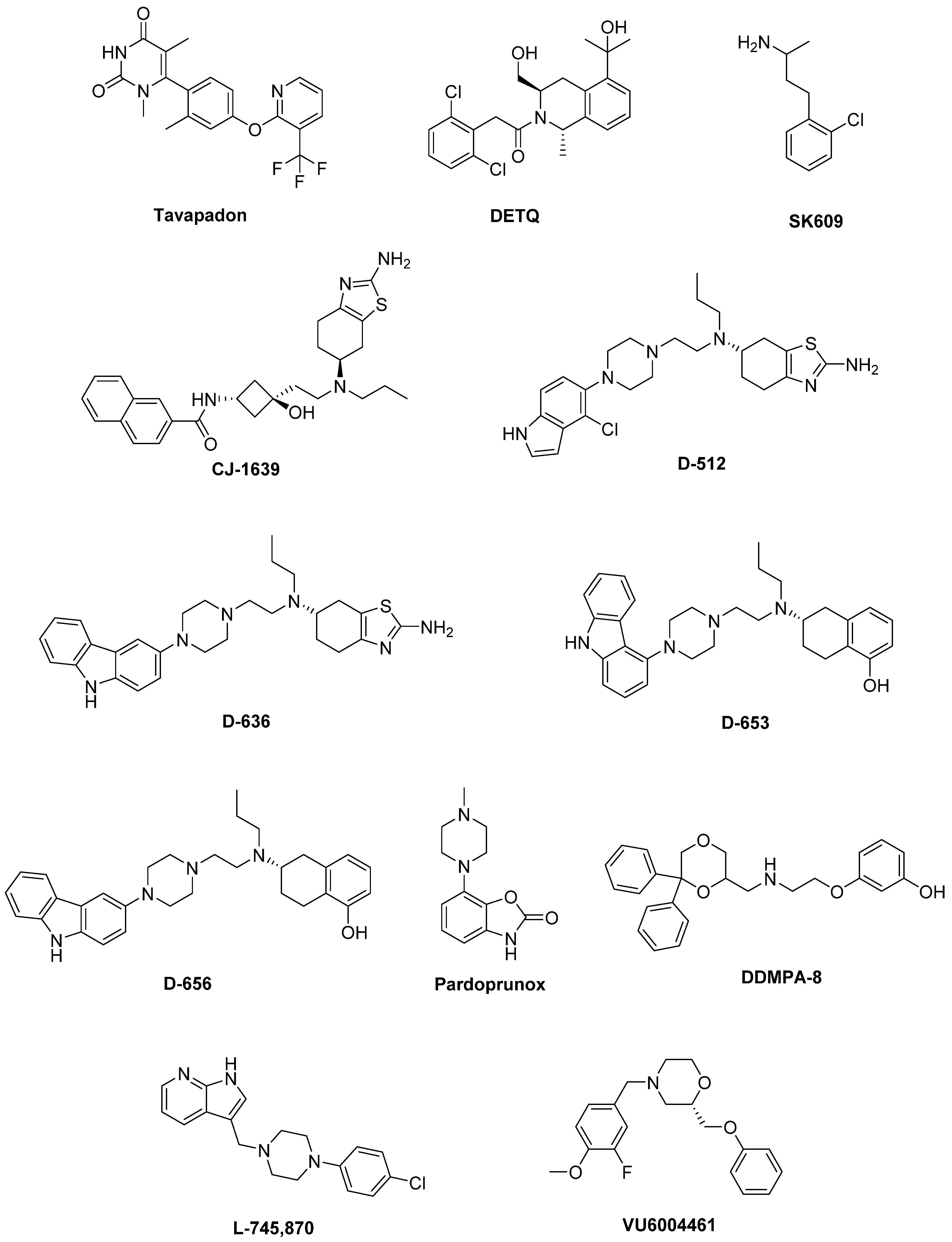
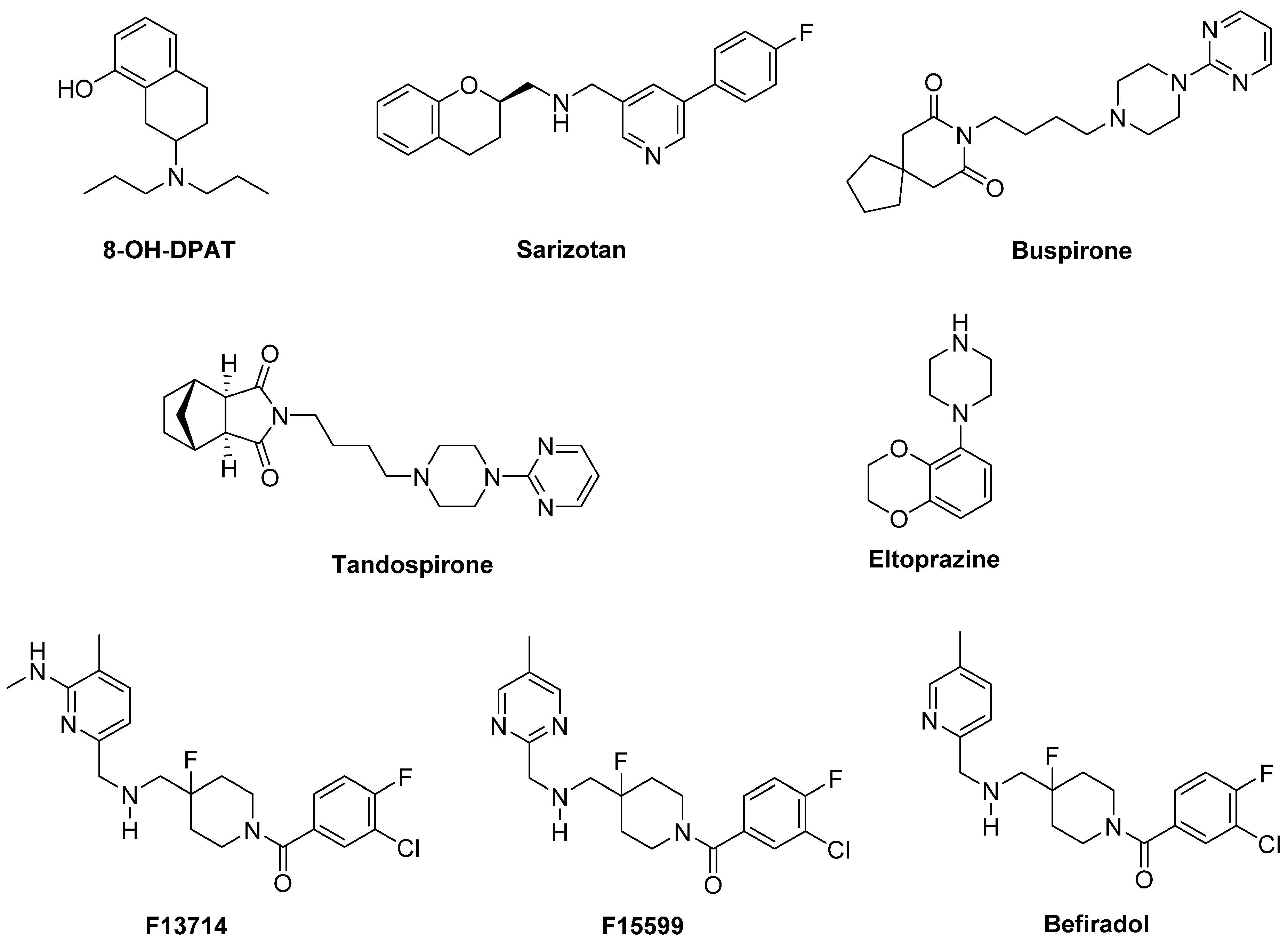
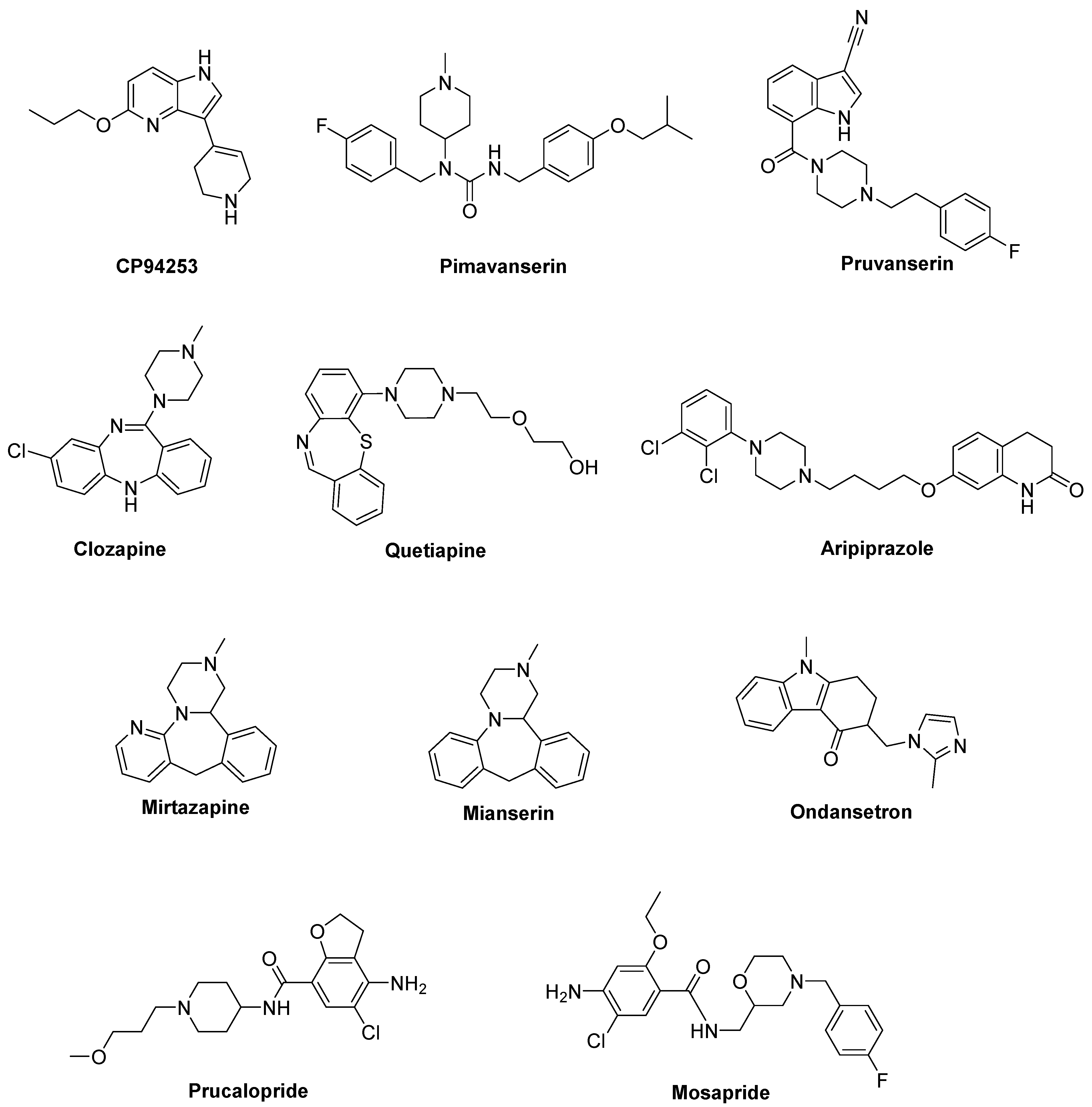

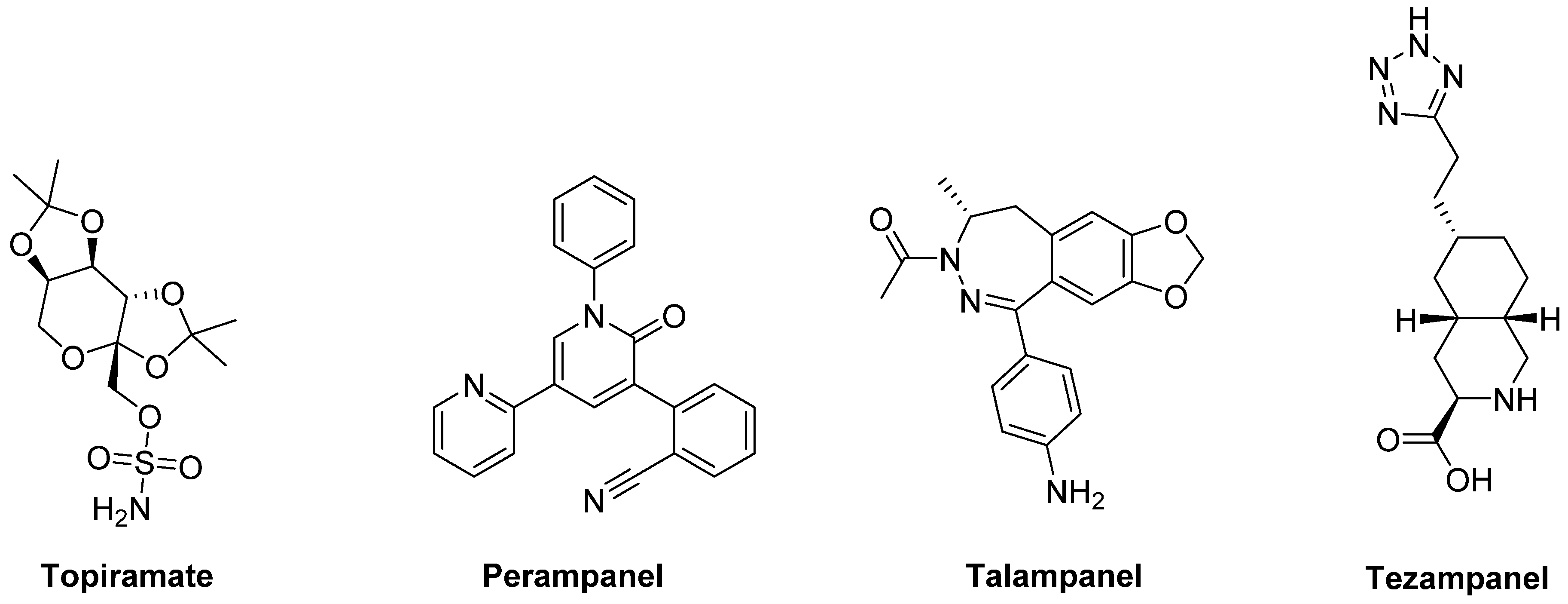


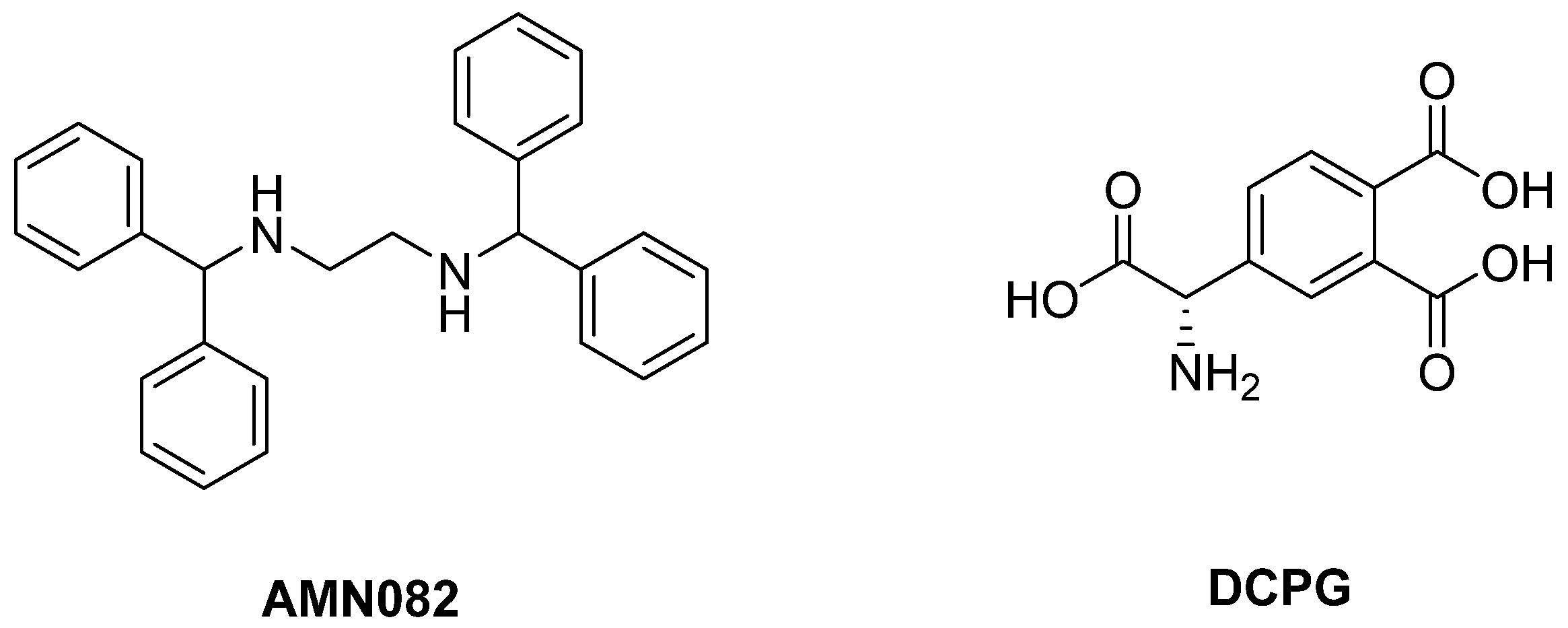
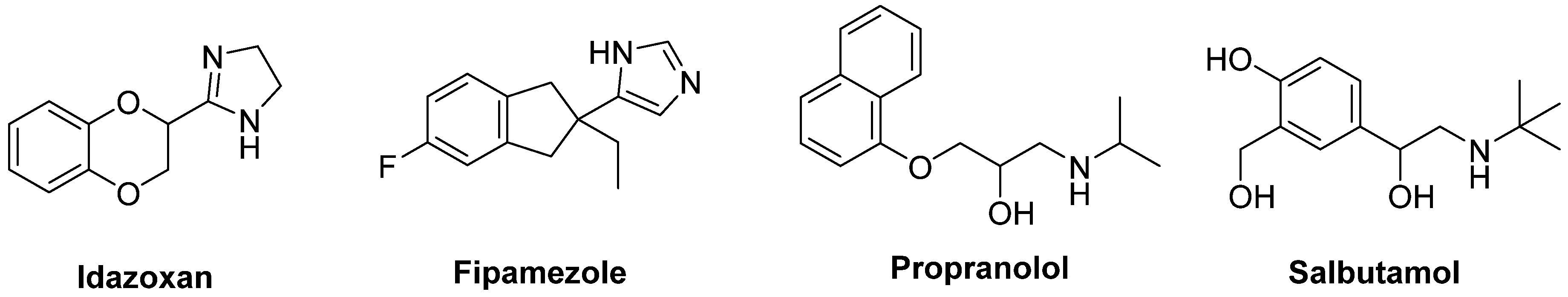
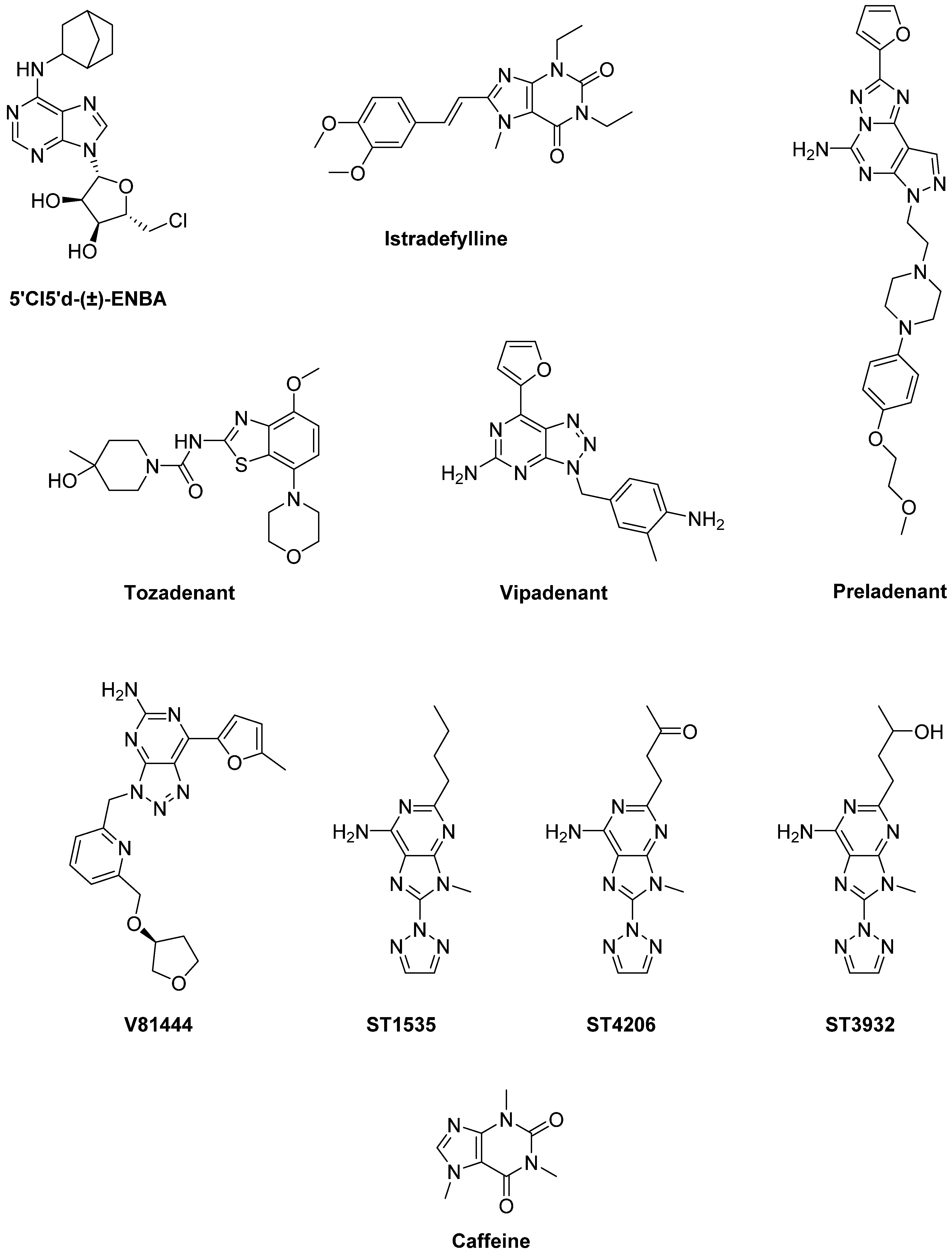

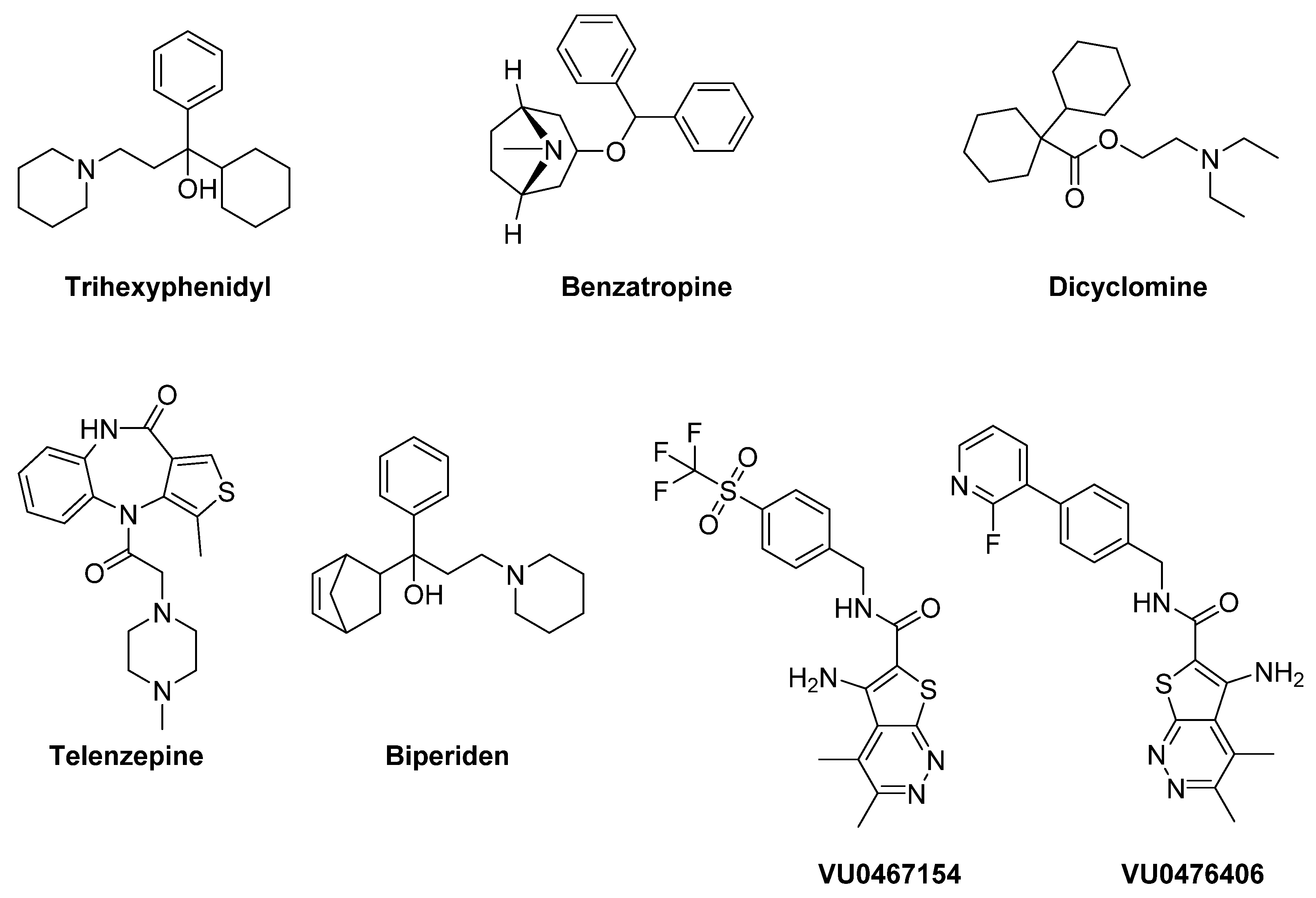
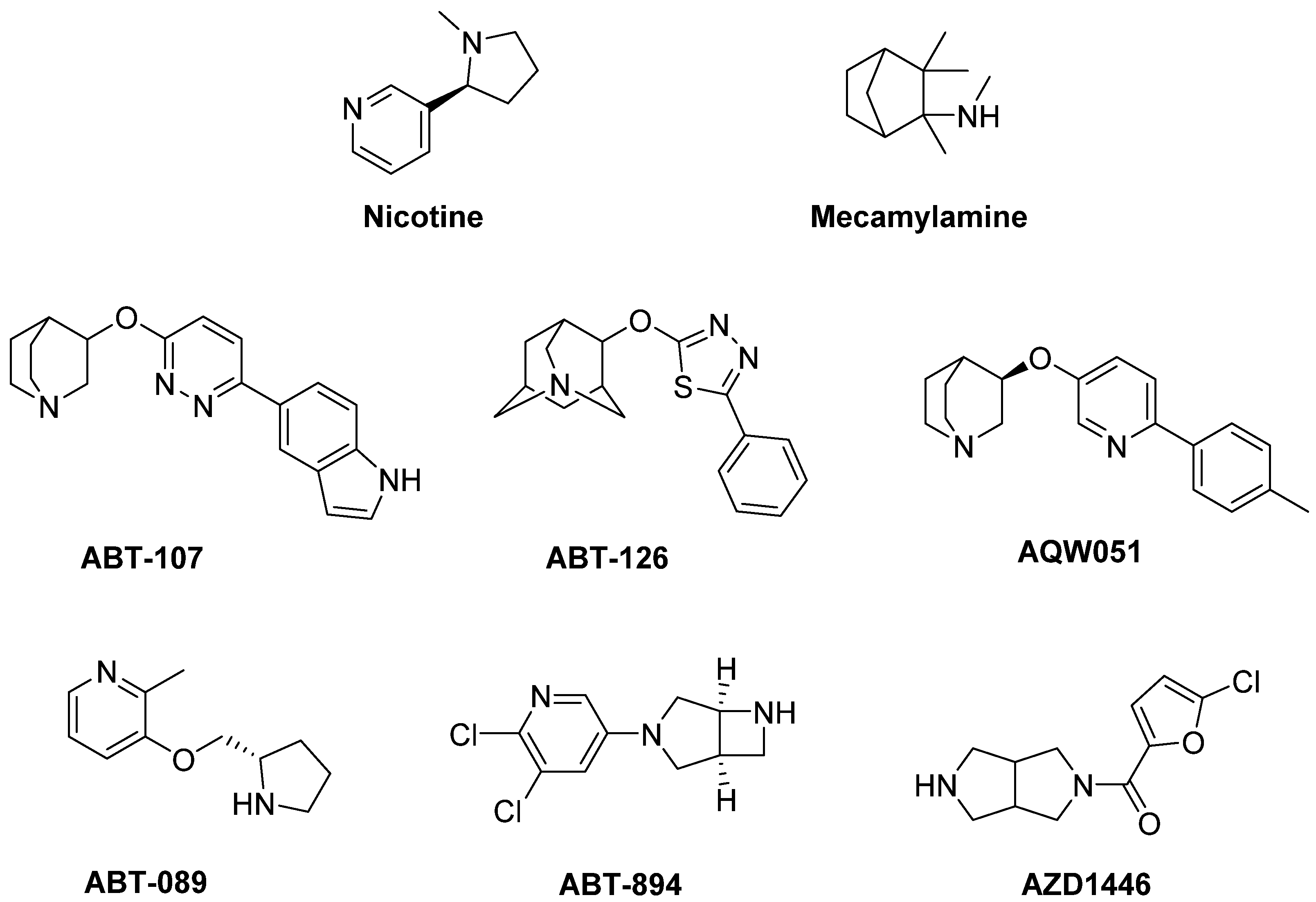
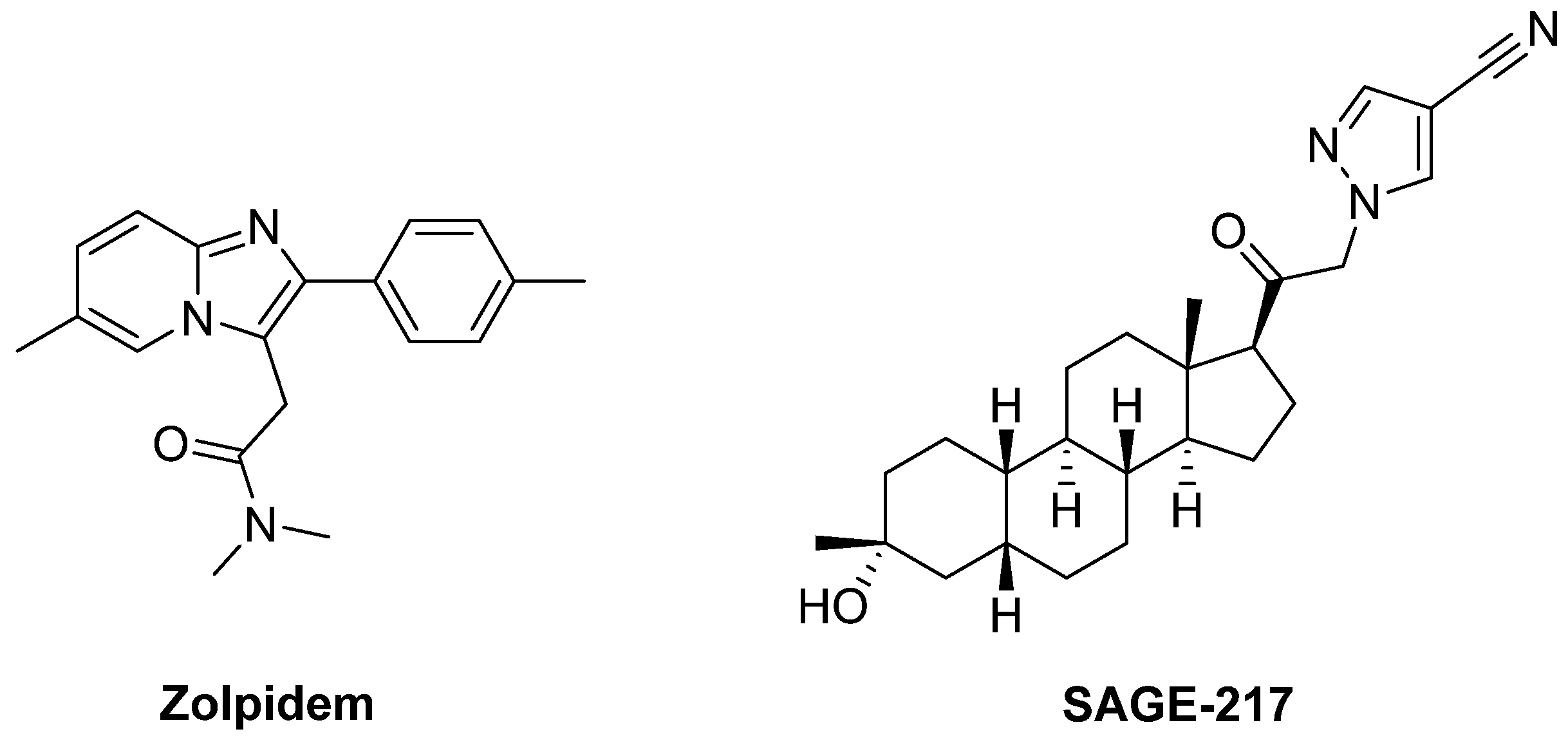
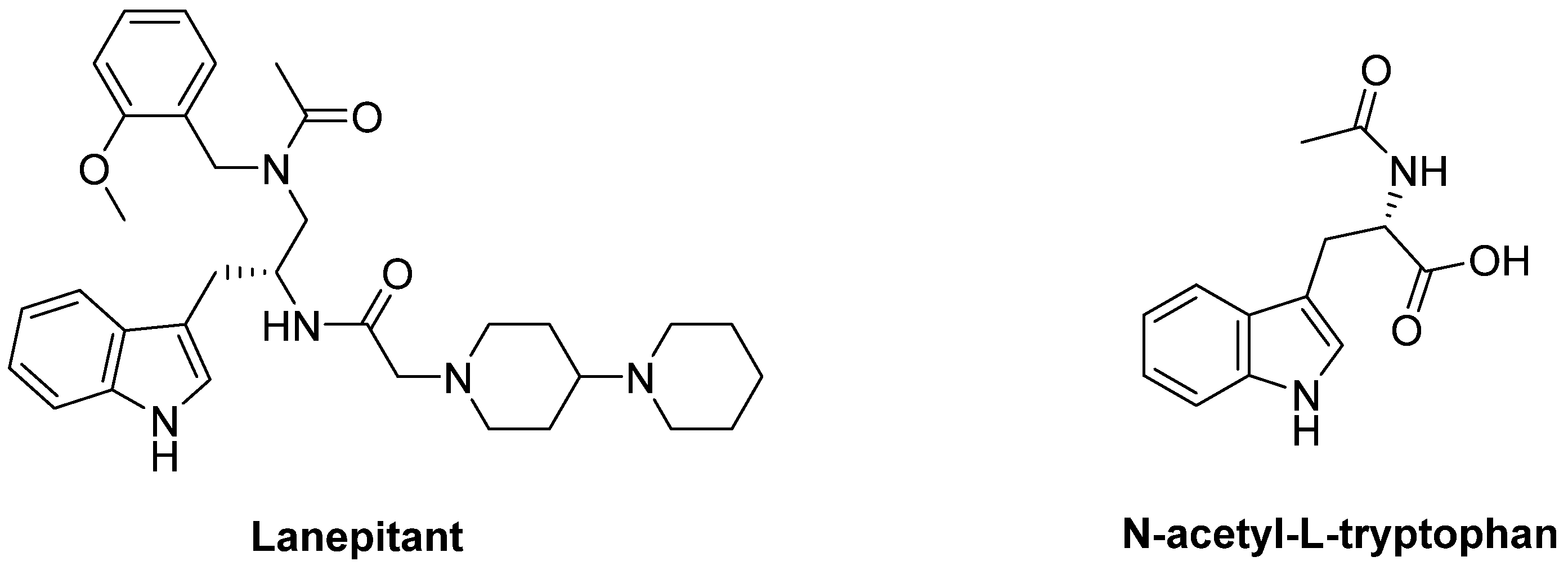
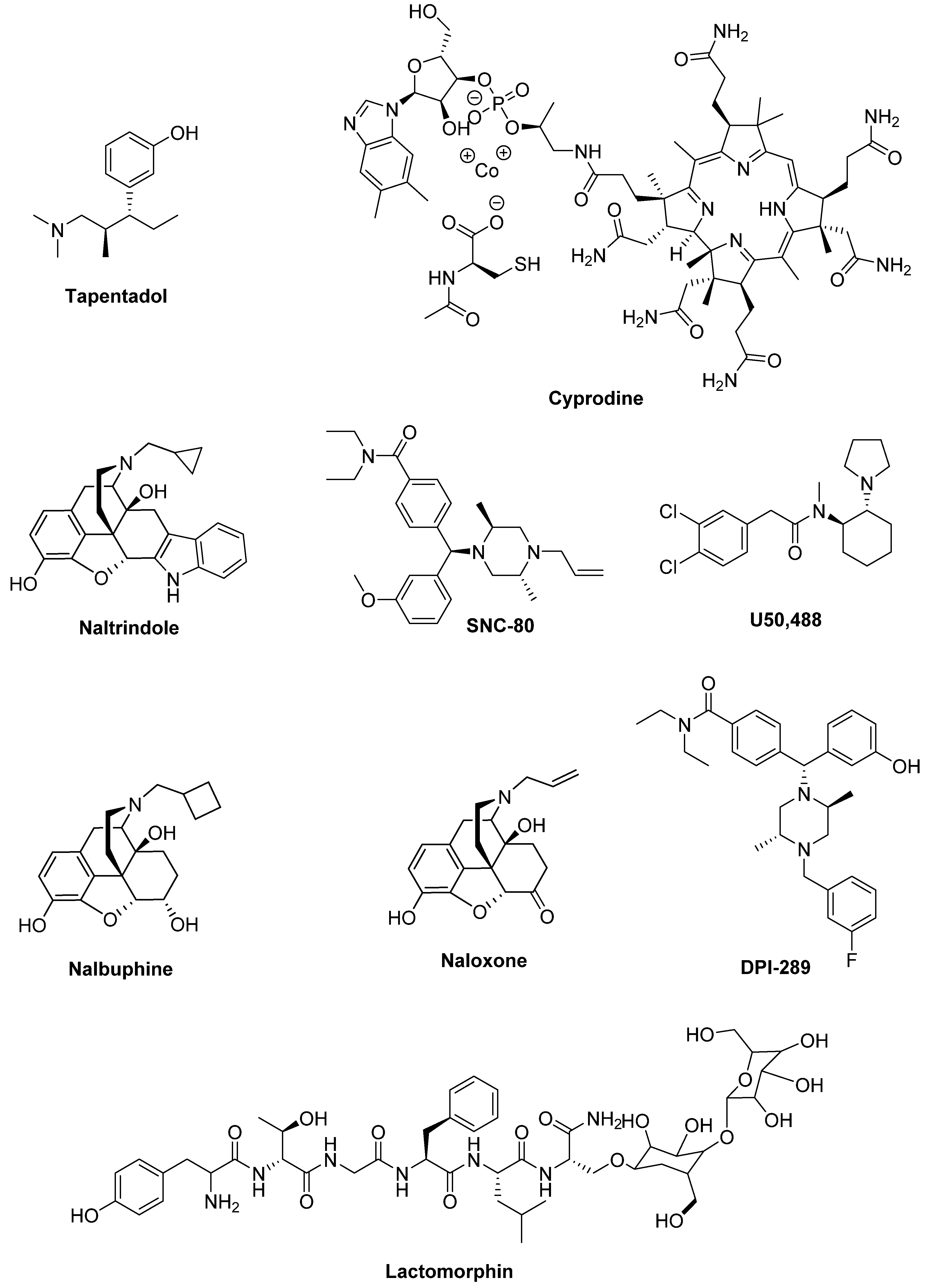

 Physiological activation,
Physiological activation,  pathological alterations in LD-induced dyskinesia (LID),
pathological alterations in LD-induced dyskinesia (LID),  pathological alterations in LID,
pathological alterations in LID,  modulation, ++ increased activation, -- decreased activation. A2A adenosine receptor, α2a and α2ab noradrenergic receptors, AMPA α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid, Cb1 cannabinoid receptor, D1 and D2 dopaminergic receptors, DA dopamine, DA-autoR dopamine autoreceptor, DAT dopamine transporter, GABA γ-aminobutyric acid, Glu glutamate, H3 histamine receptor, LID levodopa-induced dyskinesia, mGluR metabotropic glutamate receptor, NA noradrenaline, nAchR nicotinic acetylcholine receptors, NMDA N-methyl-D-aspartate, OP opioid receptor.
modulation, ++ increased activation, -- decreased activation. A2A adenosine receptor, α2a and α2ab noradrenergic receptors, AMPA α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid, Cb1 cannabinoid receptor, D1 and D2 dopaminergic receptors, DA dopamine, DA-autoR dopamine autoreceptor, DAT dopamine transporter, GABA γ-aminobutyric acid, Glu glutamate, H3 histamine receptor, LID levodopa-induced dyskinesia, mGluR metabotropic glutamate receptor, NA noradrenaline, nAchR nicotinic acetylcholine receptors, NMDA N-methyl-D-aspartate, OP opioid receptor.
 Physiological activation,
Physiological activation,  pathological alterations in LD-induced dyskinesia (LID),
pathological alterations in LD-induced dyskinesia (LID),  pathological alterations in LID,
pathological alterations in LID,  modulation, ++ increased activation, -- decreased activation. A2A adenosine receptor, α2a and α2ab noradrenergic receptors, AMPA α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid, Cb1 cannabinoid receptor, D1 and D2 dopaminergic receptors, DA dopamine, DA-autoR dopamine autoreceptor, DAT dopamine transporter, GABA γ-aminobutyric acid, Glu glutamate, H3 histamine receptor, LID levodopa-induced dyskinesia, mGluR metabotropic glutamate receptor, NA noradrenaline, nAchR nicotinic acetylcholine receptors, NMDA N-methyl-D-aspartate, OP opioid receptor.
modulation, ++ increased activation, -- decreased activation. A2A adenosine receptor, α2a and α2ab noradrenergic receptors, AMPA α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid, Cb1 cannabinoid receptor, D1 and D2 dopaminergic receptors, DA dopamine, DA-autoR dopamine autoreceptor, DAT dopamine transporter, GABA γ-aminobutyric acid, Glu glutamate, H3 histamine receptor, LID levodopa-induced dyskinesia, mGluR metabotropic glutamate receptor, NA noradrenaline, nAchR nicotinic acetylcholine receptors, NMDA N-methyl-D-aspartate, OP opioid receptor.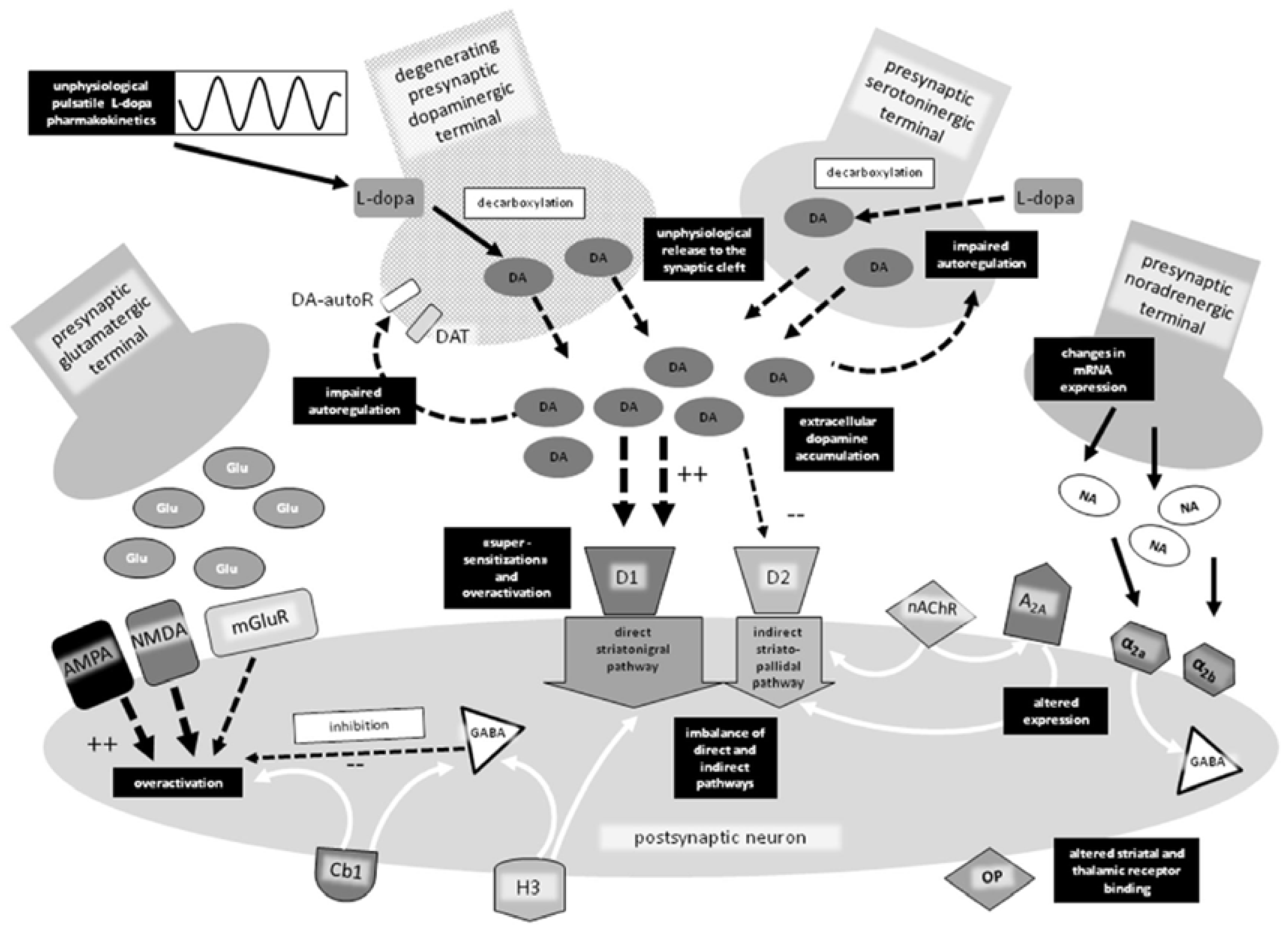
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bello, F.D.; Giannella, M.; Giorgioni, G.; Piergentili, A.; Quaglia, W. Receptor Ligands as Helping Hands to L-DOPA in the Treatment of Parkinson’s Disease. Biomolecules 2019, 9, 142. https://doi.org/10.3390/biom9040142
Bello FD, Giannella M, Giorgioni G, Piergentili A, Quaglia W. Receptor Ligands as Helping Hands to L-DOPA in the Treatment of Parkinson’s Disease. Biomolecules. 2019; 9(4):142. https://doi.org/10.3390/biom9040142
Chicago/Turabian StyleBello, Fabio Del, Mario Giannella, Gianfabio Giorgioni, Alessandro Piergentili, and Wilma Quaglia. 2019. "Receptor Ligands as Helping Hands to L-DOPA in the Treatment of Parkinson’s Disease" Biomolecules 9, no. 4: 142. https://doi.org/10.3390/biom9040142
APA StyleBello, F. D., Giannella, M., Giorgioni, G., Piergentili, A., & Quaglia, W. (2019). Receptor Ligands as Helping Hands to L-DOPA in the Treatment of Parkinson’s Disease. Biomolecules, 9(4), 142. https://doi.org/10.3390/biom9040142






