Retatrutide—A Game Changer in Obesity Pharmacotherapy
Abstract
1. Introduction
2. Materials and Methods
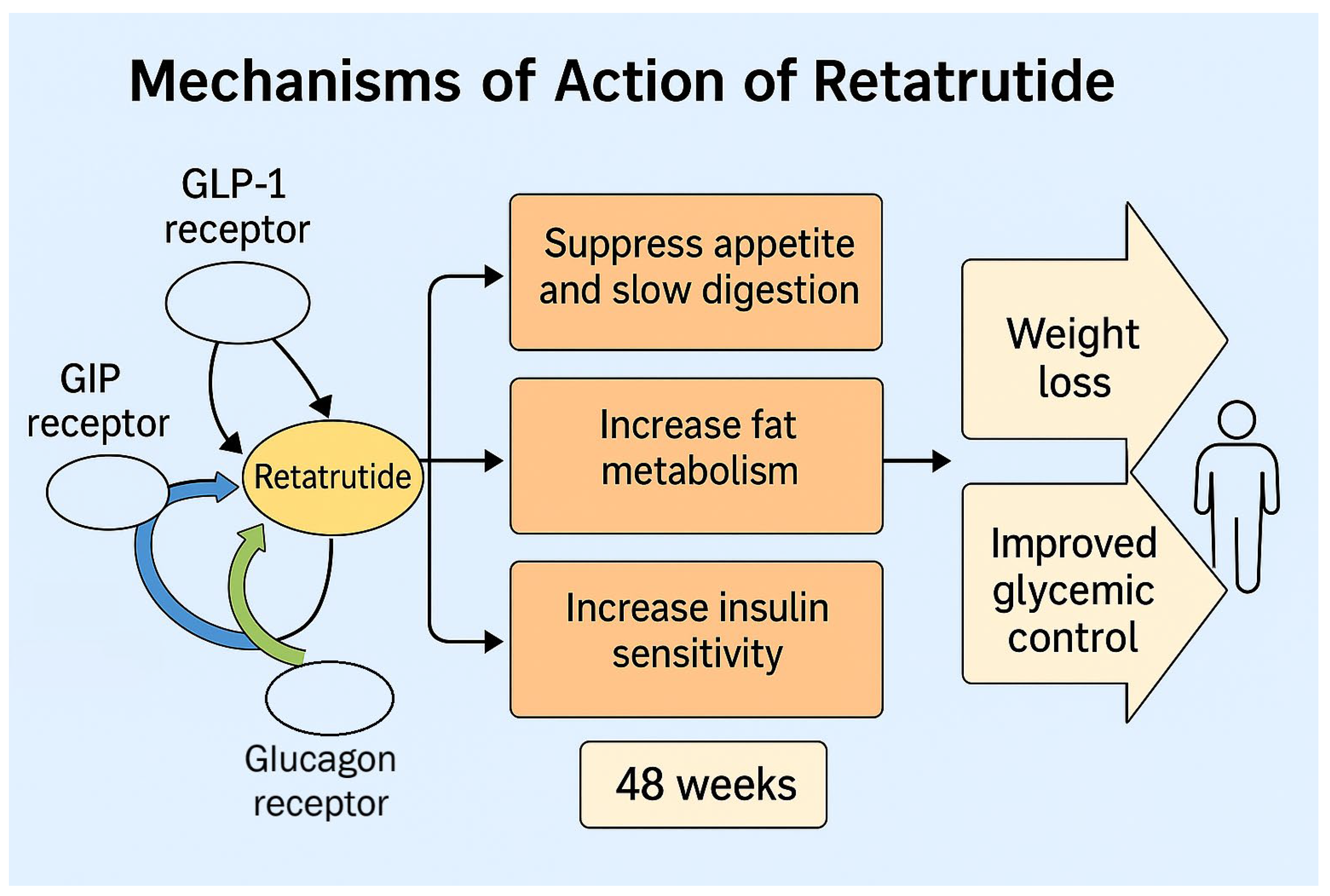
3. Targeted Molecules
3.1. Glucagon-like Peptide (GLP-1)
3.2. Glucose-Dependent Insulinotropic Polypeptide (GIP)
3.3. Glucagon
4. General Aspects of Retatrutide
Molecular Structure—Pharmacology
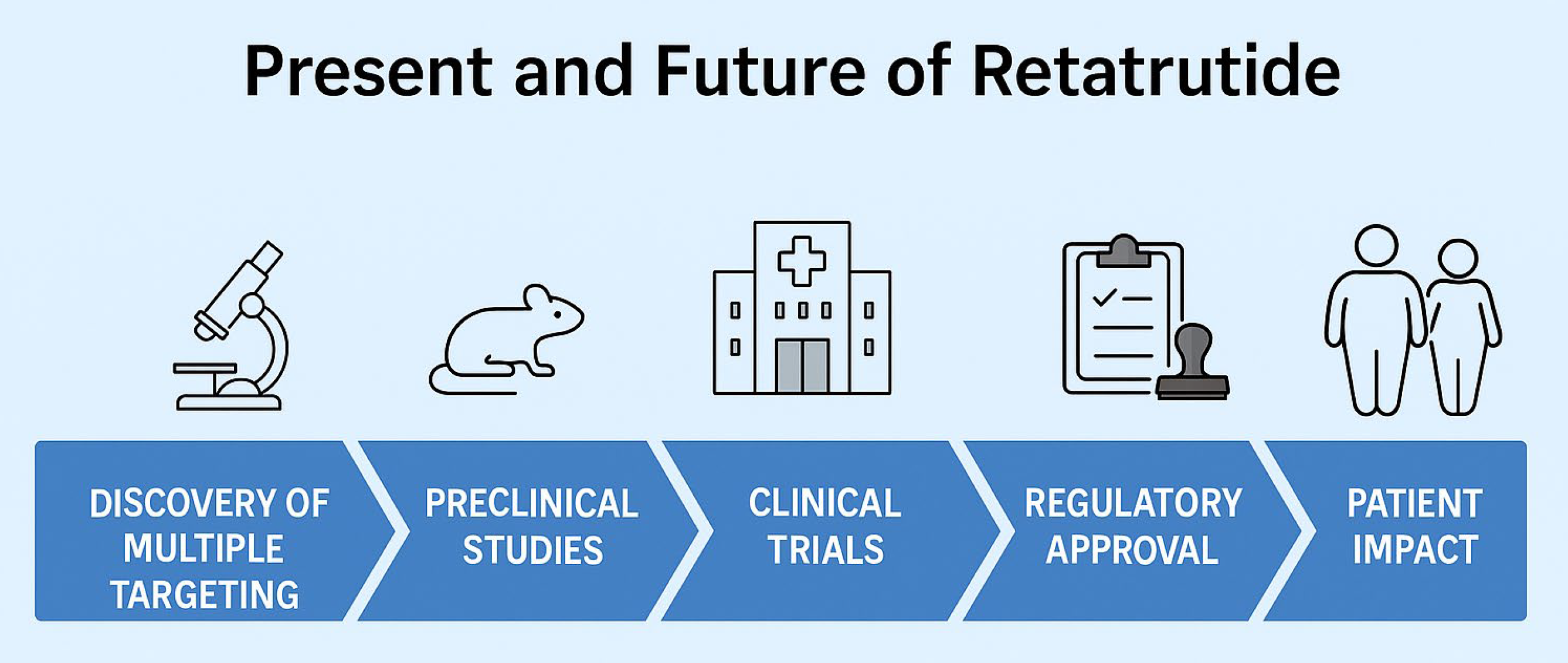
5. Insights from Animal Studies
6. Insights from Human Studies
6.1. Phase I Trials
6.2. Phase II Trials
7. The Future—Phase III Trials
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, Regional, and National Prevalence of Overweight and Obesity in Children and Adults during 1980–2013: A Systematic Analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef] [PubMed]
- Haslam, D.W.; James, W.P.T. Obesity. Lancet 2005, 366, 1197–1209. [Google Scholar] [CrossRef]
- Peeters, A.; Barendregt, J.J.; Willekens, F.; Mackenbach, J.P.; Mamun, A.A.; Bonneux, L. Obesity in Adulthood and Its Consequences for Life Expectancy: A Life-Table Analysis. Ann. Intern. Med. 2003, 138, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Kelly, T.; Yang, W.; Chen, C.-S.; Reynolds, K.; He, J. Global Burden of Obesity in 2005 and Projections to 2030. Int. J. Obes. 2008, 32, 1431–1437. [Google Scholar] [CrossRef]
- Nauck, M.A.; Wefers, J.; Meier, J.J. Treatment of Type 2 Diabetes: Challenges, Hopes, and Anticipated Successes. Lancet Diabetes Endocrinol. 2021, 9, 525–544. [Google Scholar] [CrossRef]
- Holt, R.I.G.; Cockram, C.S.; Ma, R.C.W.; Luk, A.O.Y. Diabetes and Infection: Review of the Epidemiology, Mechanisms and Principles of Treatment. Diabetologia 2024, 67, 1168–1180. [Google Scholar] [CrossRef]
- Younossi, Z.M.; Golabi, P.; Price, J.K.; Owrangi, S.; Gundu-Rao, N.; Satchi, R.; Paik, J.M. The Global Epidemiology of Nonalcoholic Fatty Liver Disease and Nonalcoholic Steatohepatitis Among Patients With Type 2 Diabetes. Clin. Gastroenterol. Hepatol. 2024, 22, 1999–2010.e8. [Google Scholar] [CrossRef]
- Li, T.; Zhao, J.; Cao, H.; Han, X.; Lu, Y.; Jiang, F.; Li, X.; Sun, J.; Zhou, S.; Sun, Z.; et al. Dietary Patterns in the Progression of Metabolic Dysfunction-Associated Fatty Liver Disease to Advanced Liver Disease: A Prospective Cohort Study. Am. J. Clin. Nutr. 2024, 120, 518–527. [Google Scholar] [CrossRef]
- von Loeffelholz, C.; Roth, J.; Coldewey, S.; Birkenfeld, A. The Role of Physical Activity in Nonalcoholic and Metabolic Dysfunction Associated Fatty Liver Disease. Biomedicines 2021, 9, 1853. [Google Scholar] [CrossRef]
- Ryan, M.C.; Itsiopoulos, C.; Thodis, T.; Ward, G.; Trost, N.; Hofferberth, S.; O’Dea, K.; Desmond, P.V.; Johnson, N.A.; Wilson, A.M. The Mediterranean Diet Improves Hepatic Steatosis and Insulin Sensitivity in Individuals with Non-Alcoholic Fatty Liver Disease. J. Hepatol. 2013, 59, 138–143. [Google Scholar] [CrossRef]
- Gelli, C.; Tarocchi, M.; Abenavoli, L.; Di Renzo, L.; Galli, A.; De Lorenzo, A. Effect of a Counseling-Supported Treatment with the Mediterranean Diet and Physical Activity on the Severity of the Non-Alcoholic Fatty Liver Disease. World J. Gastroenterol. 2017, 23, 3150. [Google Scholar] [CrossRef] [PubMed]
- Drucker, D.J.; Nauck, M.A. The Incretin System: Glucagon-like Peptide-1 Receptor Agonists and Dipeptidyl Peptidase-4 Inhibitors in Type 2 Diabetes. Lancet 2006, 368, 1696–1705. [Google Scholar] [CrossRef]
- Drucker, D.J.; Holst, J.J. The Expanding Incretin Universe: From Basic Biology to Clinical Translation. Diabetologia 2023, 66, 1765–1779. [Google Scholar] [CrossRef]
- Drucker, D.J. Prevention of Cardiorenal Complications in People with Type 2 Diabetes and Obesity. Cell Metab. 2024, 36, 338–353. [Google Scholar] [CrossRef]
- Ussher, J.R.; Drucker, D.J. Glucagon-like Peptide 1 Receptor Agonists: Cardiovascular Benefits and Mechanisms of Action. Nat. Rev. Cardiol. 2023, 20, 463–474. [Google Scholar] [CrossRef]
- Karagiannis, T.; Malandris, K.; Avgerinos, I.; Stamati, A.; Kakotrichi, P.; Liakos, A.; Vasilakou, D.; Kakaletsis, N.; Tsapas, A.; Bekiari, E. Subcutaneously Administered Tirzepatide vs Semaglutide for Adults with Type 2 Diabetes: A Systematic Review and Network Meta-Analysis of Randomised Controlled Trials. Diabetologia 2024, 67, 1206–1222. [Google Scholar] [CrossRef]
- Le Roux, C.; Mondoh, A. Treatment of Obesity with Medications Binding the Glucagon-like Peptide 1 Receptor: What Is the Current State of Play? Expert. Opin. Pharmacother. 2024, 25, 131–138. [Google Scholar] [CrossRef]
- Kappe, C.; Tracy, L.M.; Patrone, C.; Iverfeldt, K.; Sjöholm, Å. GLP-1 Secretion by Microglial Cells and Decreased CNS Expression in Obesity. J. Neuroinflamm. 2012, 9, 766. [Google Scholar] [CrossRef]
- Jakubowska, A.; Le Roux, C.W.; Viljoen, A. The Road towards Triple Agonists: Glucagon-Like Peptide 1, Glucose-Dependent Insulinotropic Polypeptide and Glucagon Receptor—An Update. Endocrinol. Metab. 2024, 39, 12–22. [Google Scholar] [CrossRef]
- Drucker, D.J. The Biology of Incretin Hormones. Cell Metab. 2006, 3, 153–165. [Google Scholar] [CrossRef]
- Heppner, K.M.; Kirigiti, M.; Secher, A.; Paulsen, S.J.; Buckingham, R.; Pyke, C.; Knudsen, L.B.; Vrang, N.; Grove, K.L. Expression and Distribution of Glucagon-Like Peptide-1 Receptor MRNA, Protein and Binding in the Male Nonhuman Primate (Macaca Mulatta) Brain. Endocrinology 2015, 156, 255–267. [Google Scholar] [CrossRef] [PubMed]
- Yapici-Eser, H.; Appadurai, V.; Eren, C.Y.; Yazici, D.; Chen, C.-Y.; Öngür, D.; Pizzagalli, D.A.; Werge, T.; Hall, M.-H. Association between GLP-1 Receptor Gene Polymorphisms with Reward Learning, Anhedonia and Depression Diagnosis. Acta Neuropsychiatr. 2020, 32, 218–225. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Cui, M.; Li, G.; Liu, Y.; Xu, Y.; Eftekhar, S.P.; Ala, M. The Pathophysiological Associations Between Obesity, NAFLD, and Atherosclerotic Cardiovascular Diseases. Horm. Metab. Res. 2024, 56, 683–696. [Google Scholar] [CrossRef]
- Müller, T.D.; Finan, B.; Bloom, S.R.; D’Alessio, D.; Drucker, D.J.; Flatt, P.R.; Fritsche, A.; Gribble, F.; Grill, H.J.; Habener, J.F.; et al. Glucagon-like Peptide 1 (GLP-1). Mol. Metab. 2019, 30, 72–130. [Google Scholar] [CrossRef]
- Inagaki, N.; Seino, Y.; Takeda, J.; Yano, H.; Yamada, Y.; Bell, G.I.; Eddy, R.L.; Fukushima, Y.; Byers, M.G.; Shows, T.B.; et al. Gastric Inhibitory Polypeptide: Structure and Chromosomal Localization of the Human Gene. Mol. Endocrinol. 1989, 3, 1014–1021. [Google Scholar] [CrossRef]
- Nicze, M.; Dec, A.; Borówka, M.; Krzyżak, D.; Bołdys, A.; Bułdak, Ł.; Okopień, B. Molecular Mechanisms behind Obesity and Their Potential Exploitation in Current and Future Therapy. Int. J. Mol. Sci. 2024, 25, 8202. [Google Scholar] [CrossRef]
- Müller, T.D.; Clemmensen, C.; Finan, B.; DiMarchi, R.D.; Tschöp, M.H. Anti-Obesity Therapy: From Rainbow Pills to Polyagonists. Pharmacol. Rev. 2018, 70, 712–746. [Google Scholar] [CrossRef]
- Newsome, P.N.; Ambery, P. Incretins (GLP-1 Receptor Agonists and Dual/Triple Agonists) and the Liver. J. Hepatol. 2023, 79, 1557–1565. [Google Scholar] [CrossRef]
- Scott, R.V.; Bloom, S.R. Problem or Solution: The Strange Story of Glucagon. Peptides 2018, 100, 36–41. [Google Scholar] [CrossRef]
- Philippe, J. Insulin Regulation of the Glucagon Gene Is Mediated by an Insulin-Responsive DNA Element. Proc. Natl. Acad. Sci. USA 1991, 88, 7224–7227. [Google Scholar] [CrossRef]
- Brubaker, P.L.; Drucker, D.J. Structure-Function of the Glucagon Receptor Family of G Protein-Coupled Receptors: The Glucagon, GIP, GLP-1, and GLP-2 Receptors. Recept. Channels 2002, 8, 179–188. [Google Scholar] [CrossRef] [PubMed]
- Sutherland, E.W. Studies on the Mechanism of Hormone Action. Science 1972, 177, 401–408. [Google Scholar] [CrossRef] [PubMed]
- Christensen, M.; Bagger, J.I.; Vilsboll, T.; Knop, F.K. The Alpha-Cell as Target for Type 2 Diabetes Therapy. Rev. Diabet. Stud. 2011, 8, 369–381. [Google Scholar] [CrossRef]
- Li, W.; Zhou, Q.; Cong, Z.; Yuan, Q.; Li, W.; Zhao, F.; Xu, H.E.; Zhao, L.H.; Yang, D.; Wang, M.W. Structural Insights into the Triple Agonism at GLP-1R, GIPR and GCGR Manifested by Retatrutide. Cell Discov. 2024, 10, 77. [Google Scholar] [CrossRef]
- Coskun, T.; Urva, S.; Roell, W.C.; Qu, H.; Loghin, C.; Moyers, J.S.; O’Farrell, L.S.; Briere, D.A.; Sloop, K.W.; Thomas, M.K.; et al. LY3437943, a Novel Triple Glucagon, GIP, and GLP-1 Receptor Agonist for Glycemic Control and Weight Loss: From Discovery to Clinical Proof of Concept. Cell Metab. 2022, 34, 1234–1247.e9. [Google Scholar] [CrossRef]
- Ray, A. Retatrutide: A Triple Incretin Receptor Agonist for Obesity Management. Expert. Opin. Investig. Drugs 2023, 32, 1003–1008. [Google Scholar] [CrossRef]
- Rosenstock, J.; Frias, J.; Jastreboff, A.M.; Du, Y.; Lou, J.; Gurbuz, S.; Thomas, M.K.; Hartman, M.L.; Haupt, A.; Milicevic, Z.; et al. Retatrutide, a GIP, GLP-1 and Glucagon Receptor Agonist, for People with Type 2 Diabetes: A Randomised, Double-Blind, Placebo and Active-Controlled, Parallel-Group, Phase 2 Trial Conducted in the USA. Lancet 2023, 402, 529–544. [Google Scholar] [CrossRef]
- Thomsen, R.W.; Mailhac, A.; Løhde, J.B.; Pottegård, A. Real-world Evidence on the Utilization, Clinical and Comparative Effectiveness, and Adverse Effects of Newer GLP-1RA-based Weight-loss Therapies. Diabetes Obes. Metab. 2025, 27, 66–88. [Google Scholar] [CrossRef]
- Jastreboff, A.M.; Kaplan, L.M.; Frías, J.P.; Wu, Q.; Du, Y.; Gurbuz, S.; Coskun, T.; Haupt, A.; Milicevic, Z.; Hartman, M.L. Triple–Hormone-Receptor Agonist Retatrutide for Obesity—A Phase 2 Trial. N. Engl. J. Med. 2023, 389, 514–526. [Google Scholar] [CrossRef]
- Urva, S.; O’Farrell, L.; Du, Y.; Loh, M.T.; Hemmingway, A.; Qu, H.; Alsina-Fernandez, J.; Haupt, A.; Milicevic, Z.; Coskun, T. The Novel GIP, GLP-1 and Glucagon Receptor Agonist Retatrutide Delays Gastric Emptying. Diabetes Obes. Metab. 2023, 25, 2784–2788. [Google Scholar] [CrossRef]
- Ma, J.; Hu, X.; Zhang, W.; Tao, M.; Wang, M.; Lu, W. Comparison of the Effects of Liraglutide, Tirzepatide, and Retatrutide on Diabetic Kidney Disease in Db/Db Mice. Endocrine 2024, 87, 159–169. [Google Scholar] [CrossRef] [PubMed]
- Jall, S.; Sachs, S.; Clemmensen, C.; Finan, B.; Neff, F.; DiMarchi, R.D.; Tschöp, M.H.; Müller, T.D.; Hofmann, S.M. Monomeric GLP-1/GIP/Glucagon Triagonism Corrects Obesity, Hepatosteatosis, and Dyslipidemia in Female Mice. Mol. Metab. 2017, 6, 440–446. [Google Scholar] [CrossRef] [PubMed]
- Urva, S.; Coskun, T.; Loh, M.T.; Du, Y.; Thomas, M.K.; Gurbuz, S.; Haupt, A.; Benson, C.T.; Hernandez-Illas, M.; D’Alessio, D.A.; et al. LY3437943, a Novel Triple GIP, GLP-1, and Glucagon Receptor Agonist in People with Type 2 Diabetes: A Phase 1b, Multicentre, Double-Blind, Placebo-Controlled, Randomised, Multiple-Ascending Dose Trial. Lancet 2022, 400, 1869–1881. [Google Scholar] [CrossRef] [PubMed]
- Sanyal, A.J.; Kaplan, L.M.; Frias, J.P.; Brouwers, B.; Wu, Q.; Thomas, M.K.; Harris, C.; Schloot, N.C.; Du, Y.; Mather, K.J.; et al. Triple Hormone Receptor Agonist Retatrutide for Metabolic Dysfunction-Associated Steatotic Liver Disease: A Randomized Phase 2a Trial. Nat. Med. 2024, 30, 2037–2048. [Google Scholar] [CrossRef]
- Kokkorakis, M.; Chakhtoura, M.; Rhayem, C.; Al Rifai, J.; Ghezzawi, M.; Valenzuela-Vallejo, L.; Mantzoros, C.S. Emerging Pharmacotherapies for Obesity: A Systematic Review. Pharmacol. Rev. 2025, 77, 100002. [Google Scholar] [CrossRef]
- Conte, C.; Hall, K.D.; Klein, S. Is Weight Loss–Induced Muscle Mass Loss Clinically Relevant? JAMA 2024, 332, 9. [Google Scholar] [CrossRef]
- Locatelli, J.C.; Costa, J.G.; Haynes, A.; Naylor, L.H.; Fegan, P.G.; Yeap, B.B.; Green, D.J. Incretin-Based Weight Loss Pharmacotherapy: Can Resistance Exercise Optimize Changes in Body Composition? Diabetes Care 2024, 47, 1718–1730. [Google Scholar] [CrossRef]
- Mechanick, J.I.; Butsch, W.S.; Christensen, S.M.; Hamdy, O.; Li, Z.; Prado, C.M.; Heymsfield, S.B. Strategies for Minimizing Muscle Loss during Use of Incretin-mimetic Drugs for Treatment of Obesity. Obes. Rev. 2025, 26. [Google Scholar] [CrossRef]
- Prado, C.M.; Phillips, S.M.; Gonzalez, M.C.; Heymsfield, S.B. Muscle Matters: The Effects of Medically Induced Weight Loss on Skeletal Muscle. Lancet Diabetes Endocrinol. 2024, 12, 785–787. [Google Scholar] [CrossRef]
- Grossman, D.C.; Bibbins-Domingo, K.; Curry, S.J.; Barry, M.J.; Davidson, K.W.; Doubeni, C.A.; Epling, J.W.; Kemper, A.R.; Krist, A.H.; Kurth, A.E.; et al. Screening for Obesity in Children and Adolescents. JAMA 2017, 317, 2417. [Google Scholar] [CrossRef]
| Type of Study | Year | Studies |
|---|---|---|
| Animal Study (mice) | 2017 | Jall et al. |
| Animal Study (mice) | 2023 | Urva et al. |
| Animal Study (mice) | 2024 | Ma et al. |
| Phase I Clinical Study | 2022 | Coskun et al. |
| Phase I Clinical Study | 2022 | Urva et al. |
| Phase II Clinical Study | 2023 | Jastreboff et al. |
| Phase II Clinical Study | 2023 | Rosenstock et al. |
| Phase II Clinical Study | 2024 | Sanyal et al. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Katsi, V.; Koutsopoulos, G.; Fragoulis, C.; Dimitriadis, K.; Tsioufis, K. Retatrutide—A Game Changer in Obesity Pharmacotherapy. Biomolecules 2025, 15, 796. https://doi.org/10.3390/biom15060796
Katsi V, Koutsopoulos G, Fragoulis C, Dimitriadis K, Tsioufis K. Retatrutide—A Game Changer in Obesity Pharmacotherapy. Biomolecules. 2025; 15(6):796. https://doi.org/10.3390/biom15060796
Chicago/Turabian StyleKatsi, Vasiliki, Georgios Koutsopoulos, Christos Fragoulis, Kyriakos Dimitriadis, and Konstantinos Tsioufis. 2025. "Retatrutide—A Game Changer in Obesity Pharmacotherapy" Biomolecules 15, no. 6: 796. https://doi.org/10.3390/biom15060796
APA StyleKatsi, V., Koutsopoulos, G., Fragoulis, C., Dimitriadis, K., & Tsioufis, K. (2025). Retatrutide—A Game Changer in Obesity Pharmacotherapy. Biomolecules, 15(6), 796. https://doi.org/10.3390/biom15060796







