Novel Biomarkers and Advanced Cardiac Imaging in Aortic Stenosis: Old and New
Abstract
1. Introduction. Current State of Knowledge
2. Pathophysiology of Cardiac Dysfunction in Aortic Stenosis
2.1. Left Ventricular Response to Aortic Stenosis
2.2. Left Atrial Response to Aortic Stenosis
3. Echocardiographic Assessment of the Left Ventricle and Left Atrium in Aortic Stenosis
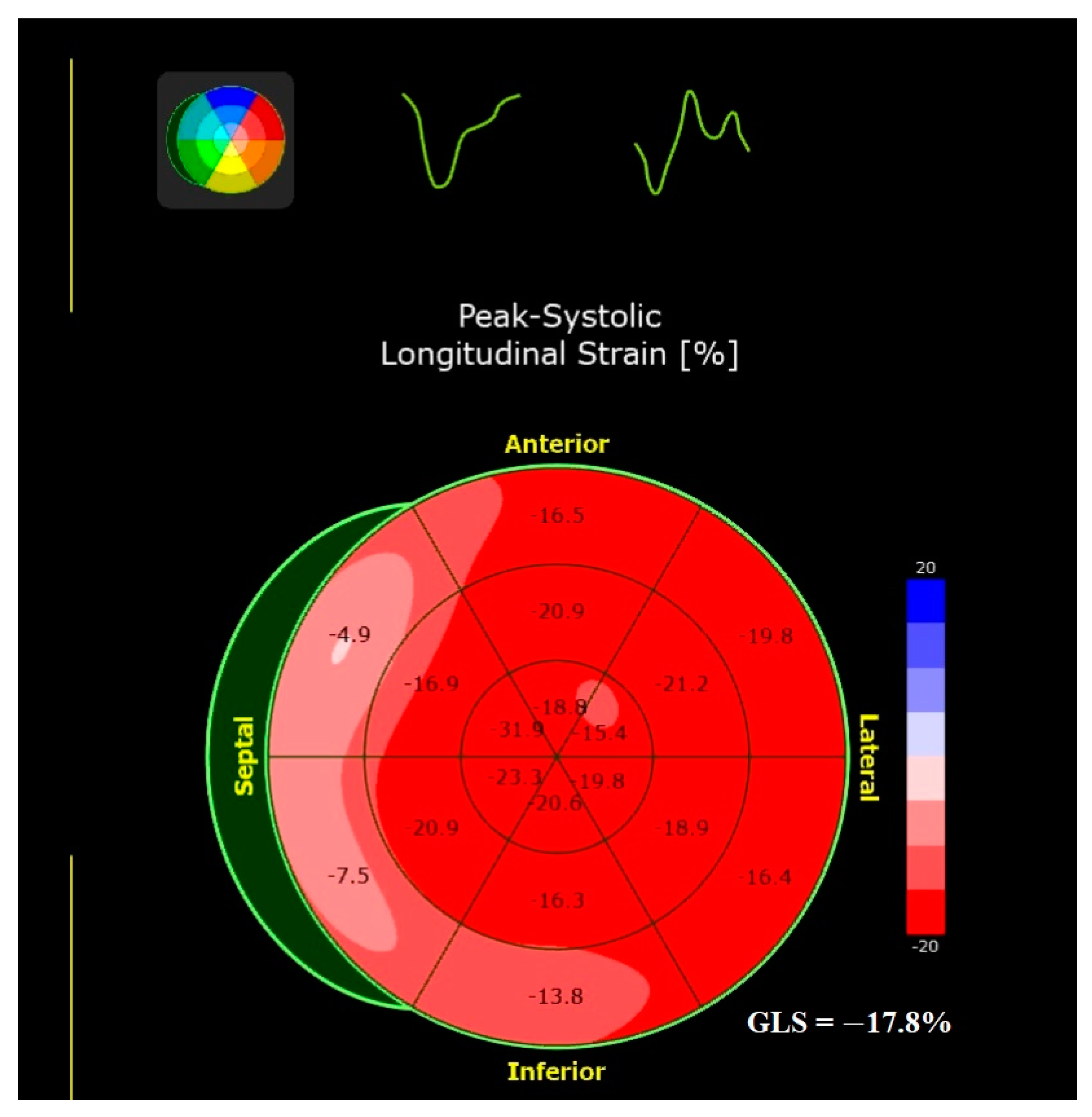
3.1. Left Ventricular Remodeling and Function
3.2. Left Atrial Remodeling and Function
4. Cardiac Magnetic Resonance in Aortic Stenosis
5. Molecular Biomarkers
5.1. Galectin-3
5.2. sST2
5.3. Micro-RNAs
5.4. Growth Differentiation Factor-15 (GDF-15)
5.5. Collagen Turnover Biomarkers, Matrix Metalloproteinases (MMPs), and Tissue Inhibitors of MMPs
5.6. Brain Natriuretic Peptide, N-Terminal-Pro-Brain Natriuretic Peptide, and Troponin
5.7. Other Biomarkers
| Biomarker | Authors | Year | Reference | Biomarker | Authors | Year | Reference |
|---|---|---|---|---|---|---|---|
| Gal-3 | Arangalage et al. | 2016 | [65] | MMPs | Liu et al. | 2004 | [115] |
| Zhou et al. | 2016 | [73] | Fielitz et al. | 2004 | [108] | ||
| Bobrowska et al. | 2017 | [66] | Bjørnstad et al. | 2008 | [113] | ||
| Agoston-Coldea et al. | 2018 | [67] | Givvimani et al. | 2010 | [114] | ||
| White et al. | 2021 | [72] | Zhou et al. | 2020 | [116] | ||
| Baran et al. | 2022 | [71] | Bäz et al. | 2020 | [112] | ||
| Ramos et al. | 2023 | [74] | Park et al. | 2014 | [109] | ||
| Lurins et al. | 2019 | [110] | |||||
| sST2 | Lancellotti et al. | 2015 | [78] | Foussier et al. | 2021 | [106] | |
| Lindman et al. | 2015 | [84] | |||||
| Fabiani et al. | 2017 | [81] | TIMP | Fielitz et al. | 2004 | [108] | |
| Sobczak et al. | 2017 | [82] | Liu et al. | 2004 | [115] | ||
| Boxhammer et al. | 2022 | [80] | Givvimani et al. | 2010 | [114] | ||
| Arrieta et al. | 2023 | [79] | Park et al. | 2014 | [109] | ||
| Bäz et al. | 2020 | [112] | |||||
| NT-proBNP | Bergler-Klein et al. | 2004 | [122] | Foussier et al. | 2021 | [106] | |
| Weber et al. | 2006 | [126] | |||||
| Lindman et al. | 2015 | [84] | |||||
| Sobczak et al. | 2017 | [82] | Collagen turnover biomarkers | Du et al. | 2012 | [105] | |
| Agoston-Coldea et al. | 2018 | [67] | Kupari et al. | 2013 | [104] | ||
| Gumauskienė et al. | 2018 | [101] | Foussier et al. | 2021 | [106] | ||
| Ito et al. | 2020 | [127] | Zhang et al. | 2022 | [103] | ||
| Zhang et al. | 2020 | [120] | |||||
| White et al. | 2021 | [72] | miRNAs | Villar et al. | 2013 | [96] | |
| Tan et al. | 2022 | [137] | García et al. | 2013 | [92] | ||
| Perry et al. | 2022 | [134] | Røsjø et al. | 2014 | [91] | ||
| Bernard et al. | 2023 | [125] | Derda et al. | 2015 | [90] | ||
| Ramos et al. | 2023 | [74] | Fabiani et al. | 2016 | [94] | ||
| García et al. | 2020 | [89] | |||||
| BNP | Bergler-Klein et al. | 2004 | [122] | ||||
| Lancellotti et al. | 2015 | [78] | |||||
| Nakatsuma et al. | 2019 | [123] | |||||
| hs-TnT | Ferrer-Sistach et al. | 2019 | [131] | GDF-15 | Lindman et al. | 2015 | [84] |
| Barbieri et al. | 2019 | [128] | Gumauskienė et al. | 2018 | [101] | ||
| Holmgren et al. | 2020 | [132] | Fabiani et al. | 2020 | [100] | ||
| White et al. | 2021 | [72] | Hofmanis et al. | 2021 | [98] | ||
| Baran et al. | 2022 | [71] | Basmadjian et al. | 2023 | [99] | ||
| Tan et al. | 2022 | [137] | |||||
| Perry et al. | 2022 | [134] | |||||
| Hadziselimovic et al. | 2023 | [130] |
6. Conclusions and Future Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- Chatterjee, A.; Kazui, T.; Acharya, D. Growing prevalence of aortic stenosis—Question of age or better recognition? Int. J. Cardiol. 2023, 388, 131155. [Google Scholar] [CrossRef] [PubMed]
- Santangelo, G.; Bursi, F.; Faggiano, A.; Moscardelli, S.; Simeoli, P.S.; Guazzi, M.; Lorusso, R.; Carugo, S.; Faggiano, P. The Global Burden of Valvular Heart Disease: From Clinical Epidemiology to Management. J. Clin. Med. 2023, 12, 2178. [Google Scholar] [CrossRef] [PubMed]
- Pibarot, P.; Clavel, M.A. Live longer and better without aortic valve stenosis. Lancet Healthy Longev. 2022, 3, e573–e574. [Google Scholar] [CrossRef] [PubMed]
- Strange, G.A.; Stewart, S.; Curzen, N.; Ray, S.; Kendall, S.; Braidley, P.; Pearce, K.; Pessotto, R.; Playford, D.; Gray, H.H. Uncovering the treatable burden of severe aortic stenosis in the UK. Open Heart 2022, 9, e001783. [Google Scholar] [CrossRef] [PubMed]
- Stewart, S.; Afoakwah, C.; Chan, Y.K.; Strom, J.B.; Playford, D.; Strange, G.A. Counting the cost of premature mortality with progressively worse aortic stenosis in Australia: A clinical cohort study. Lancet Healthy Longev. 2022, 3, e599–e606. [Google Scholar] [CrossRef] [PubMed]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. ESC/EACTS Scientific Document Group. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2022, 43, 561–632. [Google Scholar] [CrossRef] [PubMed]
- Otto, C.M.; Nishimura, R.A.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P., 3rd; Gentile, F.; Jneid, H.; Krieger, E.V.; Mack, M.; McLeod, C.; et al. 2020 ACC/AHA Guideline for the Management of Patients with Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2021, 143, e35–e71. [Google Scholar] [CrossRef] [PubMed]
- Gerber, I.L.; Stewart, R.A.; Legget, M.E.; West, T.M.; French, R.L.; Sutton, T.M.; Yandle, T.G.; French, J.K.; Richards, A.M.; White, H.D. Increased plasma natriuretic peptide levels reflect symptom onset in aortic stenosis. Circulation 2003, 107, 1884–1890. [Google Scholar] [CrossRef] [PubMed]
- Dahl, J.S.; Christensen, N.L.; Videbæk, L.; Poulsen, M.K.; Carter-Storch, R.; Hey, T.M.; Pellikka, P.A.; Steffensen, F.H.; Møller, J.E. Left ventricular diastolic function is associated with symptom status in severe aortic valve stenosis. Circ. Cardiovasc. Imaging 2014, 7, 142–148. [Google Scholar] [CrossRef]
- Lancellotti, P.; Moonen, M.; Magne, J.; O’Connor, K.; Cosyns, B.; Attena, E.; Donal, E.; Pierard, L. Prognostic effect of long-axis left ventricular dysfunction and B-type natriuretic peptide levels in asymptomatic aortic stenosis. Am. J. Cardiol. 2010, 105, 383–388. [Google Scholar] [CrossRef]
- Lancellotti, P.; Donal, E.; Magne, J.; Moonen, M.; O’Connor, K.; Daubert, J.C.; Pierard, L.A. Risk stratification in asymptomatic moderate to severe aortic stenosis: The importance of the valvular, arterial and ventricular interplay. Heart 2010, 96, 1364–1371. [Google Scholar] [CrossRef] [PubMed]
- Cameli, M.; Mandoli, G.E.; Mondillo, S. Left atrium: The last bulwark before overt heart failure. Heart Fail. Rev. 2017, 22, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Treibel, T.A.; Kozor, R.; Schofield, R.; Benedetti, G.; Fontana, M.; Bhuva, A.N.; Sheikh, A.; López, B.; González, A.; Manisty, C.; et al. Reverse Myocardial Remodeling Following Valve Replacement in Patients with Aortic Stenosis. J. Am. Coll. Cardiol. 2018, 71, 860–871. [Google Scholar] [CrossRef] [PubMed]
- Treibel, T.A.; López, B.; González, A.; Menacho, K.; Schofield, R.S.; Ravassa, S.; Fontana, M.; White, S.K.; DiSalvo, C.; Roberts, N.; et al. Reappraising myocardial fibrosis in severe aortic stenosis: An invasive and non-invasive study in 133 patients. Eur. Heart J. 2018, 39, 699–709. [Google Scholar] [CrossRef] [PubMed]
- Aziminia, N.; Nitsche, C.; Mravljak, R.; Bennett, J.; Thornton, G.D.; Treibel, T.A. Heart failure and excess mortality after aortic valve replacement in aortic stenosis. Expert Rev. Cardiovasc. Ther. 2023, 21, 193–210. [Google Scholar] [CrossRef] [PubMed]
- Stein, E.J.; Fearon, W.F.; Elmariah, S.; Kim, J.B.; Kapadia, S.; Kumbhani, D.J.; Gillam, L.; Whisenant, B.; Quader, N.; Zajarias, A.; et al. Left Ventricular Hypertrophy and Biomarkers of Cardiac Damage and Stress in Aortic Stenosis. J. Am. Heart Assoc. 2022, 11, e023466. [Google Scholar] [CrossRef] [PubMed]
- Galiuto, L.; Lotrionte, M.; Crea, F.; Anselmi, A.; Biondi-Zoccai, G.G.; De Giorgio, F.; Baldi, A.; Baldi, F.; Possati, G.; Gaudino, M.; et al. Impaired coronary and myocardial flow in severe aortic stenosis is associated with increased apoptosis: A transthoracic Doppler and myocardial contrast echocardiography study. Heart 2006, 92, 208–212. [Google Scholar] [CrossRef] [PubMed]
- Garcia, D.; Camici, P.G.; Durand, L.G.; Rajappan, K.; Gaillard, E.; Rimoldi, O.E.; Pibarot, P. Impairment of coronary flow reserve in aortic stenosis. J. Appl. Physiol. 2009, 106, 113–121. [Google Scholar] [CrossRef]
- Kampaktsis, P.N.; Kokkinidis, D.G.; Wong, S.C.; Vavuranakis, M.; Skubas, N.J.; Devereux, R.B. The role and clinical implications of diastolic dysfunction in aortic stenosis. Heart 2017, 103, 1481–1487. [Google Scholar] [CrossRef]
- Klein, A.; Ramchand, J.; Nagueh, S. Aortic Stenosis and Diastolic Dysfunction. J. Am. Coll. Cardiol. 2020, 76, 2952–2955. [Google Scholar] [CrossRef]
- Spilias, N.; Martyn, T.; Denby, K.J.; Harb, S.C.; Popovic, Z.B.; Kapadia, S.R. Left Ventricular Systolic Dysfunction in Aortic Stenosis: Pathophysiology, Diagnosis, Management, and Future Directions. Struct. Heart 2022, 6, 100089. [Google Scholar] [CrossRef] [PubMed]
- Stassen, J.; Ewe, S.H.; Butcher, S.C.; Amanullah, M.R.; Mertens, B.J.; Hirasawa, K.; Singh, G.K.; Sin, K.Y.; Ding, Z.P.; Pio, S.M.; et al. Prognostic implications of left ventricular diastolic dysfunction in moderate aortic stenosis. Heart 2022, 108, 1401–1407. [Google Scholar] [CrossRef] [PubMed]
- Fragogiannis, N.G. Cardiac fibrosis. Cardiovasc. Res. 2021, 117, 1450–1488. [Google Scholar] [CrossRef] [PubMed]
- Heymans, S.; Schroen, B.; Vermeersch, P.; Milting, H.; Gao, F.; Kassner, A.; Gillijns, H.; Herijgers, P.; Flameng, W.; Carmeliet, P.; et al. Increased cardiac expression of tissue inhibitor of metalloproteinase-1 and tissue inhibitor of metalloproteinase-2 is related to cardiac fibrosis and dysfunction in the chronic pressure-overloaded human heart. Circulation 2005, 112, 1136–1144. [Google Scholar] [CrossRef]
- Fielitz, J.; Hein, S.; Mitrovic, V.; Pregla, R.; Zurbrügg, H.R.; Warnecke, C.; Schaper, J.; Fleck, E.; Regitz-Zagrosek, V. Activation of the cardiac renin-angiotensin system and increased myocardial collagen expression in human aortic valve disease. J. Am. Coll. Cardiol. 2001, 37, 1443–1449. [Google Scholar] [CrossRef] [PubMed]
- Castrichini, M.; Vitrella, G.; De Luca, A.; Altinier, A.; Korcova, R.; Pagura, L.; Radesich, C.; Sinagra, G. Clinical impact of myocardial fibrosis in severe aortic stenosis. Eur. Heart J. Suppl. 2021, 23, E147–E150. [Google Scholar] [CrossRef] [PubMed]
- Brilla, C.G.; Maisch, B. Regulation of the structural remodelling of the myocardium: From hypertrophy to heart failure. Eur. Heart J. 1994, 15, 45–52. [Google Scholar] [CrossRef]
- Schellings, M.W.; Pinto, Y.M.; Heymans, S. Matricellular proteins in the heart: Possible role during stress and remodeling. Cardiovasc. Res. 2004, 64, 24–31. [Google Scholar] [CrossRef]
- Frangogiannis, N.G. Matricellular proteins in cardiac adaptation and disease. Physiol. Rev. 2012, 92, 635–688. [Google Scholar] [CrossRef]
- Sun, M.; Chen, M.; Dawood, F.; Zurawska, U.; Li, J.Y.; Parker, T.; Kassiri, Z.; Kirshenbaum, L.A.; Arnold, M.; Khokha, R.; et al. Tumor necrosis factor-alpha mediates cardiac remodeling and ventricular dysfunction after pressure overload state. Circulation 2007, 115, 1398–1407. [Google Scholar] [CrossRef]
- Salvador, A.M.; Nevers, T.; Velázquez, F.; Aronovitz, M.; Wang, B.; Abadía Molina, A.; Jaffe, I.Z.; Karas, R.H.; Blanton, R.M.; Alcaide, P. Intercellular Adhesion Molecule 1 Regulates Left Ventricular Leukocyte Infiltration, Cardiac Remodeling, and Function in Pressure Overload-Induced Heart Failure. J. Am. Heart Assoc. 2016, 5, e003126. [Google Scholar] [CrossRef] [PubMed]
- Tokuda, K.; Kai, H.; Kuwahara, F.; Yasukawa, H.; Tahara, N.; Kudo, H.; Takemiya, K.; Koga, M.; Yamamoto, T.; Imaizumi, T. Pressure-independent effects of angiotensin II on hypertensive myocardial fibrosis. Hypertension 2004, 43, 499–503. [Google Scholar] [CrossRef] [PubMed]
- Maltes, S.; Abecasis, J.; Pinto, D.G.; Santos, R.R.; Oliveira, L.; Mendes, G.S.; Guerreiro, S.; Lima, T.; Freitas, P.; Ferreira, A.; et al. Histology-verified myocardial fibrosis and quantification in severe AS patients: Correlation with non-invasive LV myocardial tissue assessment. Eur. Heart J. 2022, 43, ehac544-2996. [Google Scholar] [CrossRef]
- Rosca, M.; Lancellotti, P.; Popescu, B.A.; Piérard, L.A. Left atrial function: Pathophysiology, echocardiographic assessment, and clinical applications. Heart 2011, 97, 1982–1989. [Google Scholar] [CrossRef] [PubMed]
- Kane, G.C.; Karon, B.L.; Mahoney, D.W.; Redfield, M.M.; Roger, V.L.; Burnett, J.C., Jr.; Jacobsen, S.J.; Rodeheffer, R.J. Progression of left ventricular diastolic dysfunction and risk of heart failure. JAMA 2011, 306, 856–863. [Google Scholar] [CrossRef] [PubMed]
- Nagueh, S.F.; Smiseth, O.A.; Appleton, C.P.; Byrd, B.F., 3rd; Dokainish, H.; Edvardsen, T.; Flachskampf, F.A.; Gillebert, T.C.; Klein, A.L.; Lancellotti, P.; et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2016, 29, 277–314. [Google Scholar] [CrossRef] [PubMed]
- Sygitowicz, G.; Maciejak-Jastrzębska, A.; Sitkiewicz, D. A Review of the Molecular Mechanisms Underlying Cardiac Fibrosis and Atrial Fibrillation. J. Clin. Med. 2021, 10, 4430. [Google Scholar] [CrossRef] [PubMed]
- Molnár, A.Á.; Sánta, A.; Pásztor, D.T.; Merkely, B. Atrial Cardiomyopathy in Valvular Heart Disease: From Molecular Biology to Clinical Perspectives. Cells 2023, 12, 1796. [Google Scholar] [CrossRef]
- Zheng, L.; Wang, J.; Zhang, R.; Zhang, Y.; Geng, J.; Cao, L.; Zhao, X.; Geng, J.; Du, X.; Hu, Y.; et al. Angiotensin II Mediates Cardiomyocyte Hypertrophy in Atrial Cardiomyopathy via Epigenetic Transcriptional Regulation. Comput. Math. Methods Med. 2022, 2022, 6312100. [Google Scholar] [CrossRef]
- Fragão-Marques, M.; Miranda, I.; Martins, D.; Barroso, I.; Mendes, C.; Pereira-Neves, A.; Falcão-Pires, I.; Leite-Moreira, A. Atrial matrix remodeling in atrial fibrillation patients with aortic stenosis. BMC Cardiovasc. Disord. 2020, 20, 468. [Google Scholar] [CrossRef]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 28, 1–39.e14. [Google Scholar] [CrossRef] [PubMed]
- Herrmann, S.; Störk, S.; Niemann, M.; Lange, V.; Strotmann, J.M.; Frantz, S.; Beer, M.; Gattenlöhner, S.; Voelker, W.; Ertl, G.; et al. Low-gradient aortic valve stenosis myocardial fibrosis and its influence on function and outcome. J. Am. Coll. Cardiol. 2011, 58, 402–412. [Google Scholar] [CrossRef] [PubMed]
- Magne, J.; Cosyns, B.; Popescu, B.A.; Carstensen, H.G.; Dahl, J.; Desai, M.Y.; Kearney, L.; Lancellotti, P.; Marwick, T.H.; Sato, K.; et al. Distribution and Prognostic Significance of Left Ventricular Global Longitudinal Strain in Asymptomatic Significant Aortic Stenosis: An Individual Participant Data Meta-Analysis. JACC Cardiovasc. Imaging 2019, 12, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Kempny, A.; Diller, G.P.; Kaleschke, G.; Orwat, S.; Funke, A.; Radke, R.; Schmidt, R.; Kerckhoff, G.; Ghezelbash, F.; Rukosujew, A.; et al. Longitudinal left ventricular 2D strain is superior to ejection fraction in predicting myocardial recovery and symptomatic improvement after aortic valve implantation. Int. J. Cardiol. 2013, 167, 2239–2243. [Google Scholar] [CrossRef] [PubMed]
- Lozano Granero, V.C.; Fernández Santos, S.; Fernández-Golfín, C.; Plaza Martín, M.; de la Hera Galarza, J.M.; Faletra, F.F.; Swaans, M.J.; López-Fernández, T.; Mesa, D.; La Canna, G.; et al. Immediate improvement of left ventricular mechanics following transcatheter aortic valve replacement. Cardiol. J. 2018, 25, 487–494. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, K.; Magne, J.; Rosca, M.; Pierard, L.A.; Lancellotti, P. Impact of aortic valve stenosis on left atrial phasic function. Am. J. Cardiol. 2010, 106, 1157–1162. [Google Scholar] [CrossRef] [PubMed]
- Mateescu, A.D.; Călin, A.; Beladan, C.C.; Roşca, M.; Enache, R.; Băicuş, C.; Botezatu, S.; Ginghină, C.; Popescu, B.A. Left Atrial Dysfunction as an Independent Correlate of Heart Failure Symptoms in Patients with Severe Aortic Stenosis and Preserved Left Ventricular Ejection Fraction. J. Am. Soc. Echocardiogr. 2019, 32, 257–266. [Google Scholar] [CrossRef]
- Pernigo, M.; Benfari, G.; Geremia, G.; Noni, M.; Borio, G.; Mazzali, G.; Zamboni, M.; Onorati, F.; Faggian, G.; Vassanelli, C.; et al. Atrial Function as an Independent Predictor of Postoperative Atrial Fibrillation in Patients Undergoing Aortic Valve Surgery for Severe Aortic Stenosis. J. Am. Soc. Echocardiogr. 2017, 30, 956–965.e1. [Google Scholar] [CrossRef]
- O’Connor, K.; Magne, J.; Rosca, M.; Pierard, L.A.; Lancellotti, P. Left atrial function and remodelling in aortic stenosis. Eur. J. Echocardiogr. 2011, 12, 299–305. [Google Scholar] [CrossRef]
- Prioli, A.; Marino, P.; Lanzoni, L.; Zardini, P. Increasing degrees of left ventricular filling impairment modulate left atrial function in humans. Am. J. Cardiol. 1998, 82, 756–761. [Google Scholar] [CrossRef]
- Kuppahally, S.S.; Akoum, N.; Burgon, N.S.; Badger, T.J.; Kholmovski, E.G.; Vijayakumar, S.; Rao, S.N.; Blauer, J.; Fish, E.N.; Dibella, E.V.; et al. Left atrial strain and strain rate in patients with paroxysmal and persistent atrial fibrillation: Relationship to left atrial structural remodeling detected by delayed-enhancement MRI. Circ. Cardiovasc. Imaging 2010, 3, 231–239. [Google Scholar] [CrossRef]
- Kim, S.J.; Choisy, S.C.; Barman, P.; Zhang, H.; Hancox, J.C.; Jones, S.A.; James, A.F. Atrial remodeling and the substrate for atrial fibrillation in rat hearts with elevated afterload. Circ. Arrhythm. Electrophysiol. 2011, 4, 761–769. [Google Scholar] [CrossRef] [PubMed]
- Flett, A.S.; Sado, D.M.; Quarta, G.; Mirabel, M.; Pellerin, D.; Herrey, A.S.; Hausenloy, D.J.; Ariti, C.; Yap, J.; Kolvekar, S.; et al. Diffuse myocardial fibrosis in severe aortic stenosis: An equilibrium contrast cardiovascular magnetic resonance study. Eur. Heart J. Cardiovasc. Imaging 2012, 13, 819–826. [Google Scholar] [CrossRef] [PubMed]
- Everett, R.J.; Tastet, L.; Clavel, M.A.; Chin, C.W.L.; Capoulade, R.; Vassiliou, V.S.; Kwiecinski, J.; Gomez, M.; van Beek, E.J.R.; White, A.C.; et al. Progression of Hypertrophy and Myocardial Fibrosis in Aortic Stenosis: A Multicenter Cardiac Magnetic Resonance Study. Circ. Cardiovasc. Imaging 2018, 11, e007451. [Google Scholar] [CrossRef] [PubMed]
- Musa, T.A.; Treibel, T.A.; Vassiliou, V.S.; Captur, G.; Singh, A.; Chin, C.; Dobson, L.E.; Pica, S.; Loudon, M.; Malley, T.; et al. Myocardial Scar and Mortality in Severe Aortic Stenosis. Circulation 2018, 138, 1935–1947. [Google Scholar] [CrossRef] [PubMed]
- Bing, R.; Everett, R.J.; Tuck, C.; Semple, S.; Lewis, S.; Harkess, R.; Mills, N.L.; Treibel, T.A.; Prasad, S.; Greenwood, J. P et al. Rationale and design of the randomized, controlled Early Valve Replacement Guided by Biomarkers of Left Ventricular Decompensation in Asymptomatic Patients with Severe Aortic Stenosis (EVOLVED) trial. Am. Heart J. 2019, 212, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Park, J.B.; Yoon, Y.E.; Park, E.A.; Kim, H.K.; Lee, W.; Kim, Y.J.; Cho, G.Y.; Sohn, D.W.; Greiser, A.; et al. Noncontrast Myocardial T1 Mapping by Cardiac Magnetic Resonance Predicts Outcome in Patients with Aortic Stenosis. JACC Cardiovasc. Imaging 2018, 11, 974–983. [Google Scholar] [CrossRef]
- Cavalcante, J.L.; Rijal, S.; Abdelkarim, I.; Althouse, A.D.; Sharbaugh, M.S.; Fridman, Y.; Soman, P.; Forman, D.E.; Schindler, J.T.; Gleason, T.G.; et al. Cardiac amyloidosis is prevalent in older patients with aortic stenosis and carries worse prognosis. J. Cardiovasc. Magn. Reson. 2017, 19, 98. [Google Scholar] [CrossRef] [PubMed]
- Nangia-Makker, P.; Hogan, V.; Balan, V.; Raz, A. Chimeric galectin-3 and collagens: Biomarkers and potential therapeutic targets in fibroproliferative diseases. J. Biol. Chem. 2022, 298, 102622. [Google Scholar] [CrossRef]
- Sharma, U.C.; Pokharel, S.; van Brakel, T.J.; van Berlo, J.H.; Cleutjens, J.P.; Schroen, B.; André, S.; Crijns, H.J.; Gabius, H.J.; Maessen, J.; et al. Galectin-3 marks activated macrophages in failure-prone hypertrophied hearts and contributes to cardiac dysfunction. Circulation 2004, 110, 3121–3128. [Google Scholar] [CrossRef]
- Song, X.; Qian, X.; Shen, M.; Jiang, R.; Wagner, M.B.; Ding, G.; Chen, G.; Shen, B. Protein kinase C promotes cardiac fibrosis and heart failure by modulating galectin-3 expression. Biochim. Biophys. Acta 2015, 1853, 513–521. [Google Scholar] [CrossRef] [PubMed]
- Ibarrola, J.; Arrieta, V.; Sádaba, R.; Martinez-Martinez, E.; Garcia-Peña, A.; Alvarez, V.; Fernández-Celis, A.; Gainza, A.; Santamaría, E.; Fernández-Irigoyen, J.; et al. Galectin-3 down-regulates antioxidant peroxiredoxin-4 in human cardiac fibroblasts: A new pathway to induce cardiac damage. Clin. Sci. 2018, 132, 1471–1485. [Google Scholar] [CrossRef] [PubMed]
- Frunza, O.; Russo, I.; Saxena, A.; Shinde, A.V.; Humeres, C.; Hanif, W.; Rai, V.; Su, Y.; Frangogiannis, N.G. Myocardial Galectin-3 Expression Is Associated with Remodeling of the Pressure-Overloaded Heart and May Delay the Hypertrophic Response without Affecting Survival, Dysfunction, and Cardiac Fibrosis. Am. J. Pathol. 2016, 186, 1114–1127. [Google Scholar] [CrossRef]
- Arrieta, V.; Martinez-Martinez, E.; Ibarrola, J.; Alvarez, V.; Sádaba, R.; Garcia-Peña, A.; Fernández-Celis, A.; Cachofeiro, V.; Rossignol, P.; López-Andrés, N. A role for galectin-3 in the development of early molecular alterations in short-term aortic stenosis. Clin. Sci. 2017, 131, 935–949. [Google Scholar] [CrossRef]
- Arangalage, D.; Nguyen, V.; Robert, T.; Melissopoulou, M.; Mathieu, T.; Estellat, C.; Codogno, I.; Huart, V.; Duval, X.; Cimadevilla, C.; et al. Determinants and prognostic value of Galectin-3 in patients with aortic valve stenosis. Heart 2016, 102, 862–868. [Google Scholar] [CrossRef]
- Bobrowska, B.; Wieczorek-Surdacka, E.; Kruszelnicka, O.; Chyrchel, B.; Surdacki, A.; Dudek, D. Clinical Correlates and Prognostic Value of Plasma Galectin-3 Levels in Degenerative Aortic Stenosis: A Single-Center Prospective Study of Patients Referred for Invasive Treatment. Int. J. Mol. Sci. 2017, 18, 947. [Google Scholar] [CrossRef] [PubMed]
- Agoston-Coldea, L.; Bheecarry, K.; Petra, C.; Strambu, L.; Ober, C.; Revnic, R.; Lupu, S.; Mocan, T.; Fodor, D. The value of global longitudinal strain and galectin-3 for predicting cardiovascular events in patients with severe aortic stenosis. Med. Ultrason 2018, 20, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Z.; Cai, K.; Xu, C.; Zhan, Q.; Xu, X.; Xu, D.; Zeng, Q. Prognostic Value of Serum Galectin-3 in Chronic Heart Failure: A Meta-Analysis. Front. Cardiovasc. Med. 2022, 9, 783707. [Google Scholar] [CrossRef]
- Chen, Y.S.; Gi, W.T.; Liao, T.Y.; Lee, M.T.; Lee, S.H.; Hsu, W.T.; Chang, S.S.; Lee, C.C. Using the galectin-3 test to predict mortality in heart failure patients: A systematic review and meta-analysis. Biomark. Med. 2016, 10, 329–342. [Google Scholar] [CrossRef]
- Sherpa, M.D.; Sonkawade, S.D.; Jonnala, V.; Pokharel, S.; Khazaeli, M.; Yatsynovich, Y.; Kalot, M.A.; Weil, B.R.; Canty, J.M., Jr.; Sharma, U.C. Galectin-3 Is Associated with Cardiac Fibrosis and an Increased Risk of Sudden Death. Cells 2023, 12, 1218. [Google Scholar] [CrossRef]
- Baran, J.; Niewiara, Ł.; Podolec, J.; Siedliński, M.; Józefczuk, E.; Bernacik, A.; Badacz, R.; Przewłocki, T.; Pieniążek, P.; Żmudka, K.; et al. Serum and Vascular Stiffness Biomarkers Associated with the Severity of Degenerative Aortic Valve Stenosis and Cardiovascular Outcomes. J. Cardiovasc. Dev. Dis. 2022, 9, 193. [Google Scholar] [CrossRef] [PubMed]
- White, M.; Baral, R.; Ryding, A.; Tsampasian, V.; Ravindrarajah, T.; Garg, P.; Koskinas, K.C.; Clark, A.; Vassiliou, V.S. Biomarkers Associated with Mortality in Aortic Stenosis: A Systematic Review and Meta-Analysis. Med. Sci. 2021, 9, 29. [Google Scholar] [CrossRef] [PubMed]
- Zhou, K.; Zhou, Y.; Zhao, Y.; Tan, C.; Yuan, Z.; Li, J.; Liao, X.; Gu, L.; Zhou, X. The Relationship between Galectin-3 and Different Patterns of Ventricular Geometry Remodelling in Aortic Valve Stenosis. Heart Lung Circ. 2016, 25, 371–377. [Google Scholar] [CrossRef] [PubMed]
- Ramos, M.; Quezada-Feijoó, M.; Ayala, R.; Manzano, A.; Gómez-Pavón, F.J.; Jaramillo, J.; Herrera, C.; López Vazquez de la Torre, M.; Toro, R. Value of NT-proBNP and Galectin-3 as Biomarkers in the Follow-up of Asymptomatic Elderly Patients with Severe Aortic Stenosis. J. Clin. Med. 2023, 12, 2987. [Google Scholar] [CrossRef] [PubMed]
- Giritharan, S.; Cagampang, F.; Torrens, C.; Salhiyyah, K.; Duggan, S.; Ohri, S. Aortic Stenosis Prognostication in Patients with Type 2 Diabetes: Protocol for Testing and Validation of a Biomarker-Derived Scoring System. JMIR Res. Protoc. 2019, 8, e13186. [Google Scholar] [CrossRef] [PubMed]
- Pusceddu, I.; Dieplinger, B.; Mueller, T. ST2 and the ST2/IL-33 signalling pathway-biochemistry and pathophysiology in animal models and humans. Clin. Chim. Acta 2019, 495, 493–500. [Google Scholar] [CrossRef] [PubMed]
- Matilla, L.; Ibarrola, J.; Arrieta, V.; Garcia-Peña, A.; Martinez-Martinez, E.; Sádaba, R.; Alvarez, V.; Navarro, A.; Fernández-Celis, A.; Gainza, A.; et al. Soluble ST2 promotes oxidative stress and inflammation in cardiac fibroblasts: An in vitro and in vivo study in aortic stenosis. Clin. Sci. 2019, 133, 1537–1548. [Google Scholar] [CrossRef]
- Lancellotti, P.; Dulgheru, R.; Magne, J.; Henri, C.; Servais, L.; Bouznad, N.; Ancion, A.; Martinez, C.; Davin, L.; Le Goff, C.; et al. Elevated Plasma Soluble ST2 Is Associated with Heart Failure Symptoms and Outcome in Aortic Stenosis. PLoS ONE 2015, 10, e0138940. [Google Scholar] [CrossRef]
- Arrieta, V.; Jover, E.; Navarro, A.; Martín-Núñez, E.; Garaikoetxea, M.; Matilla, L.; García-Peña, A.; Fernández-Celis, A.; Gainza, A.; Álvarez, V.; et al. Soluble ST2 levels are related to replacement myocardial fibrosis in severe aortic stenosis. Rev. Esp. Cardiol. 2023, 76, 679–689. [Google Scholar] [CrossRef]
- Boxhammer, E.; Mirna, M.; Bäz, L.; Bacher, N.; Topf, A.; Sipos, B.; Franz, M.; Kretzschmar, D.; Hoppe, U.C.; Lauten, A.; et al. Soluble ST2 as a Potential Biomarker for Risk Assessment of Pulmonary Hypertension in Patients Undergoing TAVR? Life 2022, 12, 389. [Google Scholar] [CrossRef]
- Fabiani, I.; Conte, L.; Pugliese, N.R.; Calogero, E.; Barletta, V.; Di Stefano, R.; Santoni, T.; Scatena, C.; Bortolotti, U.; Naccarato, A.G.; et al. The integrated value of sST2 and global longitudinal strain in the early stratification of patients with severe aortic valve stenosis: A translational imaging approach. Int. J. Cardiovasc. Imaging 2017, 33, 1915–1920. [Google Scholar] [CrossRef] [PubMed]
- Sobczak, S.; Sakowicz, A.; Pietrucha, T.; Lelonek, M. Diagnostic utility of biomarkers of left ventricular stress in patients with aortic stenosis and preserved left ventricular ejection fraction. Kardiochir. Torakochirurgia Pol. 2017, 14, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Mirna, M.; Paar, V.; Gharibeh, S.; Topf, A.; Hoppe, U.C.; Lichtenauer, M. Diverging Concentrations of Soluble Suppression of Tumorigenicity (sST2) Analyzed by two Different Assays—A Limitation for its use in Clinical Practice? Clin. Lab. 2023, 69, 1443–1450. [Google Scholar] [CrossRef] [PubMed]
- Lindman, B.R.; Breyley, J.G.; Schilling, J.D.; Vatterott, A.M.; Zajarias, A.; Maniar, H.S.; Damiano, R.J., Jr.; Moon, M.R.; Lawton, J.S.; Gage, B.F.; et al. Prognostic utility of novel biomarkers of cardiovascular stress in patients with aortic stenosis undergoing valve replacement. Heart 2015, 101, 1382–1388. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Liew, O.W.; Richards, A.M.; Chen, Y.T. Overview of MicroRNAs in Cardiac Hypertrophy, Fibrosis, and Apoptosis. Int. J. Mol. Sci. 2016, 17, 749. [Google Scholar] [CrossRef] [PubMed]
- García, R.; Nistal, J.F.; Merino, D.; Price, N.L.; Fernández-Hernando, C.; Beaumont, J.; González, A.; Hurlé, M.A.; Villar, A.V. p-SMAD2/3 and DICER promote pre-miR-21 processing during pressure overload-associated myocardial remodeling. Biochim. Biophys. Acta 2015, 1852, 1520–1530. [Google Scholar] [CrossRef]
- Adewuyi, J.O.; Patel, R.; Abbasciano, R.; McCann, G.P.; Murphy, G.; Woźniak, M.J.; Singh, A. A systematic review of micro-RNAs in aortic stenosis and cardiac fibrosis. Clin. Transl. Sci. 2022, 15, 1809–1817. [Google Scholar] [CrossRef]
- Verjans, R.; Peters, T.; Beaumont, F.J.; van Leeuwen, R.; van Herwaarden, T.; Verhesen, W.; Munts, C.; Bijnen, M.; Henkens, M.; Diez, J.; et al. MicroRNA-221/222 Family Counteracts Myocardial Fibrosis in Pressure Overload-Induced Heart Failure. Hypertension 2018, 71, 280–288. [Google Scholar] [CrossRef]
- García, R.; Salido-Medina, A.B.; Gil, A.; Merino, D.; Gómez, J.; Villar, A.V.; González-Vílchez, F.; Hurlé, M.A.; Nistal, J.F. Sex-Specific Regulation of miR-29b in the Myocardium Under Pressure Overload is Associated with Differential Molecular, Structural and Functional Remodeling Patterns in Mice and Patients with Aortic Stenosis. Cells 2020, 9, 833. [Google Scholar] [CrossRef]
- Derda, A.A.; Thum, S.; Lorenzen, J.M.; Bavendiek, U.; Heineke, J.; Keyser, B.; Stuhrmann, M.; Givens, R.C.; Kennel, P.J.; Schulze, P.C.; et al. Blood-based microRNA signatures differentiate various forms of cardiac hypertrophy. Int. J. Cardiol. 2015, 196, 115–122. [Google Scholar] [CrossRef]
- Røsjø, H.; Dahl, M.B.; Bye, A.; Andreassen, J.; Jørgensen, M.; Wisløff, U.; Christensen, G.; Edvardsen, T.; Omland, T. Prognostic value of circulating microRNA-210 levels in patients with moderate to severe aortic stenosis. PLoS ONE 2014, 9, e91812. [Google Scholar] [CrossRef]
- García, R.; Villar, A.V.; Cobo, M.; Llano, M.; Martín-Durán, R.; Hurlé, M.A.; Nistal, J.F. Circulating levels of miR-133a predict the regression potential of left ventricular hypertrophy after valve replacement surgery in patients with aortic stenosis. J. Am. Heart. Assoc. 2013, 2, e000211. [Google Scholar] [CrossRef]
- Villar, A.V.; García, R.; Merino, D.; Llano, M.; Cobo, M.; Montalvo, C.; Martín-Durán, R.; Hurlé, M.A.; Nistal, J.F. Myocardial and circulating levels of microRNA-21 reflect left ventricular fibrosis in aortic stenosis patients. Int. J. Cardiol. 2013, 167, 2875–2881. [Google Scholar] [CrossRef] [PubMed]
- Fabiani, I.; Scatena, C.; Mazzanti, C.M.; Conte, L.; Pugliese, N.R.; Franceschi, S.; Lessi, F.; Menicagli, M.; De Martino, A.; Pratali, S.; et al. Micro-RNA-21 (biomarker) and global longitudinal strain (functional marker) in detection of myocardial fibrotic burden in severe aortic valve stenosis: A pilot study. J. Transl. Med. 2016, 14, 248. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Iacopo, F.; Lorenzo, C.; Calogero, E.; Matteo, P.; Riccardo, P.N.; Veronica, S.; Valentina, B.; Riccardo, L.; Cristian, S.; Maria, M.C.; et al. Review in Translational Cardiology: MicroRNAs and Myocardial Fibrosis in Aortic Valve Stenosis, a Deep Insight on Left Ventricular Remodeling. J. Cardiovasc. Echogr. 2016, 26, 109–114. [Google Scholar] [PubMed]
- Rochette, L.; Dogon, G.; Zeller, M.; Cottin, Y.; Vergely, C. GDF15 and Cardiac Cells: Current Concepts and New Insights. Int. J. Mol. Sci. 2021, 22, 8889. [Google Scholar] [CrossRef] [PubMed]
- Tretjakovs, P.; Lurins, J.; Svirskis, S.; Gersone, G.; Lurina, D.; Rozenberga, U.; Blumfelds, L.; Bahs, G.; Lejnieks, A.; Mackevics, V. Thioredoxin-1 and Correlations of the Plasma Cytokines Regarding Aortic Valve Stenosis Severity. Biomedicines 2021, 9, 1041. [Google Scholar] [CrossRef] [PubMed]
- Hofmanis, J.; Tretjakovs, P.; Svirskis, S.; Gersone, G.; Hofmane, D.; Rozenberga, U.; Blumfelds, L.; Bahs, G.; Lejnieks, A.; Mackevics, V. Prognostic Utility of Circulating Growth Factors in Aortic Valve Stenosis: A Pilot Study. Medicina 2021, 57, 78. [Google Scholar] [CrossRef] [PubMed]
- Basmadjian, L.; Bouabdallaoui, N.; Simard, F.; O’Meara, E.; Ducharme, A.; Rouleau, J.L.; Racine, N.; White, M.; Sirois, M.G.; Asgar, A.; et al. Growth Differentiation Factor-15 as a Predictor of Functional Capacity, Frailty, and Ventricular Dysfunction in Patients with Aortic Stenosis and Preserved Left Ventricular Ejection Fraction. Am. J. Cardiol. 2023, 186, 11–16. [Google Scholar] [CrossRef]
- Fabiani, I.; Santoni, T.; Angelillis, M.; Petricciuolo, S.; Colli, A.; Pellegrini, G.; Mazzei, D.; Pugliese, N.R.; Petronio, A.S.; De Caterina, R. Growth Differentiation Factor 15 in Severe Aortic Valve Stenosis: Relationship with Left Ventricular Remodeling and Frailty. J. Clin. Med. 2020, 9, 2998. [Google Scholar] [CrossRef]
- Gumauskienė, B.; Krivickienė, A.; Jonkaitienė, R.; Vaškelytė, J.J.; Siudikas, A.; Ereminienė, E. Impact of Left Ventricular Diastolic Dysfunction and Biomarkers on Pulmonary Hypertension in Patients with Severe Aortic Stenosis. Medicina 2018, 54, 63. [Google Scholar] [CrossRef]
- Fragão-Marques, M.; Barroso, I.; Farinha, R.; Miranda, I.M.; Martins, D.; Mancio, J.; Rocha-Neves, J.; Guimarães, J.T.; Leite-Moreira, A.; Falcão-Pires, I. Pericardial NT-Pro-BNP and GDF-15 as Biomarkers of Atrial Fibrillation and Atrial Matrix Remodeling in Aortic Stenosis. Diagnostics 2021, 11, 1422. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Xue, Q.; Zhu, R.; Jiang, Y. Diagnostic Value of PICP and PIIINP in Myocardial Fibrosis: A Systematic Review and Meta-analysis. Clin. Cardiol. 2022; Online ahead of print. [Google Scholar]
- Kupari, M.; Laine, M.; Turto, H.; Lommi, J.; Werkkala, K. Circulating collagen metabolites, myocardial fibrosis and heart failure in aortic valve stenosis. J. Heart Valve Dis. 2013, 22, 166–176. [Google Scholar] [PubMed]
- Du, X.; Wan, Z.; Yu, X.F.; Jia, L.L.; Huang, C.L. Plasma amino-terminal propeptide of procollagen type III is associated with subclinical left ventricular systolic dysfunction in aortic stenosis. Int. J. Cardiol. 2012, 156, 24–27. [Google Scholar] [CrossRef]
- Foussier, C.; Barral, P.A.; Jerosh-Herold, M.; Gariboldi, V.; Rapacchi, S.; Gallon, A.; Bartoli, A.; Bentatou, Z.; Guye, M.; Bernard, M.; et al. Quantification of diffuse myocardial fibrosis using CMR extracellular volume fraction and serum biomarkers of collagen turnover with histologic quantification as standard of reference. Diagn. Interv. Imaging 2021, 102, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Lange, T.; Backhaus, S.; Beuthner, B.E.; Topci, R.; Rigorth, K.R.; Kowallick, J.; Evertz, R.; Schnelle, M.; Ravassa, S.; Díez, J.; et al. Functional and structural reverse myocardial remodeling following transcatheter aortic valve replacement: A prospective cardiovascular magnetic resonance study. J. Cardiovasc. Magn. Reson. 2022, 24, 45. [Google Scholar] [CrossRef] [PubMed]
- Fielitz, J.; Leuschner, M.; Zurbrügg, H.R.; Hannack, B.; Pregla, R.; Hetzer, R.; Regitz-Zagrosek, V. Regulation of matrix metalloproteinases and their inhibitors in the left ventricular myocardium of patients vwith aortic stenosis. J. Mol. Med. 2004, 82, 809–820. [Google Scholar] [CrossRef] [PubMed]
- Park, J.Y.; Ryu, S.K.; Choi, J.W.; Ho, K.M.; Jun, J.H.; Rha, S.W.; Park, S.M.; Kim, H.J.; Choi, B.G.; Noh, Y.K.; et al. Association of inflammation, myocardial fibrosis and cardiac remodelling in patients with mild aortic stenosis as assessed by biomarkers and echocardiography. Clin. Exp. Pharmacol. Physiol. 2014, 41, 185–191. [Google Scholar] [CrossRef]
- Lurins, J.; Lurina, D.; Svirskis, S.; Nora-Krukle, Z.; Tretjakovs, P.; Mackevics, V.; Lejnieks, A.; Rapisarda, V.; Baylon, V. Impact of several proinflammatory and cell degradation factors in patients with aortic valve stenosis. Exp. Ther. Med. 2019, 17, 2433–2442. [Google Scholar] [CrossRef]
- Polyakova, V.; Hein, S.; Kostin, S.; Ziegelhoeffer, T.; Schaper, J. Matrix metalloproteinases and their tissue inhibitors in pressure-overloaded human myocardium during heart failure progression. J. Am. Coll. Cardiol. 2004, 44, 1609–1618. [Google Scholar] [CrossRef]
- Bäz, L.; Dannberg, G.; Grün, K.; Westphal, J.; Möbius-Winkler, S.; Jung, C.; Pfeil, A.; Schulze, P.C.; Franz, M. Serum Biomarkers of Cardiovascular Remodelling Reflect Extra-Valvular Cardiac Damage in Patients with Severe Aortic Stenosis. Int. J. Mol. Sci. 2020, 21, 4174. [Google Scholar] [CrossRef]
- Bjørnstad, J.L.; Neverdal, N.O.; Vengen, O.A.; Knudsen, C.W.; Husebye, T.; Pepper, J.; Lie, M.; Christensen, G.; Tønnessen, T. Alterations in circulating activin A, GDF-15, TGF-beta3 and MMP-2, -3, and -9 during one year of left ventricular reverse remodelling in patients operated for severe aortic stenosis. Eur. J. Heart Fail. 2008, 10, 1201–1207. [Google Scholar] [CrossRef] [PubMed]
- Givvimani, S.; Tyagi, N.; Sen, U.; Mishra, P.K.; Qipshidze, N.; Munjal, C.; Vacek, J.C.; Abe, O.A.; Tyagi, S.C. MMP-2/TIMP-2/TIMP-4 versus MMP-9/TIMP-3 in transition from compensatory hypertrophy and angiogenesis to decompensatory heart failure. Arch. Physiol. Biochem. 2010, 116, 63–72. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Liu, P.Y.; Tsai, W.C.; Lin, C.C.; Hsu, C.H.; Haung, Y.Y.; Chen, J.H. Invasive measurements of pulse wave velocity correlate with the degree of aortic valve calcification and severity associated with matrix metalloproteinases in elderly patients with aortic valve stenosis. Clin. Sci. 2004, 107, 415–422. [Google Scholar] [CrossRef] [PubMed]
- Zhou, K.; Guo, T.; Xu, Y.; Guo, R. Correlation Between Plasma Matrix Metalloproteinase-28 Levels and Severity of Calcific Aortic Valve Stenosis. Med. Sci. Monit. 2020, 26, e925260. [Google Scholar] [CrossRef] [PubMed]
- Omran, F.; Kyrou, I.; Osman, F.; Lim, V.G.; Randeva, H.S.; Chatha, K. Cardiovascular Biomarkers: Lessons of the Past and Prospects for the Future. Int. J. Mol. Sci. 2022, 23, 5680. [Google Scholar] [CrossRef] [PubMed]
- Cao, Z.; Jia, Y.; Zhu, B. BNP and NT-proBNP as Diagnostic Biomarkers for Cardiac Dysfunction in Both Clinical and Forensic Medicine. Int. J. Mol. Sci. 2019, 20, 1820. [Google Scholar] [CrossRef]
- Gallo, G.; Presta, V.; Volpe, M.; Rubattu, S. Molecular and clinical implications of natriuretic peptides in aortic valve stenosis. J. Mol. Cell. Cardiol. 2019, 129, 266–271. [Google Scholar] [CrossRef]
- Zhang, B.; Xu, H.; Zhang, H.; Liu, Q.; Ye, Y.; Hao, J.; Zhao, Q.; Qi, X.; Liu, S.; Zhang, E.; et al. CHINA-DVD Collaborators. Prognostic Value of N-Terminal Pro-B-Type Natriuretic Peptide in Elderly Patients With Valvular Heart Disease. J. Am. Coll. Cardiol. 2020, 75, 1659–1672. [Google Scholar] [CrossRef]
- Taniguchi, T.; Morimoto, T.; Takeji, Y.; Kato, T.; Kimura, T. CURRENT AS registry Investigators. Contemporary issues in severe aortic stenosis: Review of current and future strategies from the Contemporary Outcomes after Surgery and Medical Treatment in Patients with Severe Aortic Stenosis registry. Heart 2020, 106, 802–809. [Google Scholar] [CrossRef]
- Bergler-Klein, J.; Klaar, U.; Heger, M.; Rosenhek, R.; Mundigler, G.; Gabriel, H.; Binder, T.; Pacher, R.; Maurer, G.; Baumgartner, H. Natriuretic peptides predict symptom-free survival and postoperative outcome in severe aortic stenosis. Circulation 2004, 109, 2302–2308. [Google Scholar] [CrossRef] [PubMed]
- Nakatsuma, K.; Taniguchi, T.; Morimoto, T.; Shiomi, H.; Ando, K.; Kanamori, N.; Murata, K.; Kitai, T.; Kawase, Y.; Izumi, C.; et al. CURRENT AS Registry Investigators. B-type natriuretic peptide in patients with asymptomatic severe aortic stenosis. Heart 2019, 105, 384–390. [Google Scholar] [PubMed]
- Bernard, J.; Tastet, L.; Capoulade, R.; Shen, M.; Clisson, M.; Guzzetti, E.; Larose, É.; Arsenault, M.; Bédard, É.; Côté, N.; et al. Left ventricular asymmetric remodeling and subclinical left ventricular dysfunction in patients with calcific aortic valve stenosis—Results from a subanalysis of the PROGRESSA study. Int. J. Cardiol. 2021, 332, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Bernard, J.; Jean, G.; Bienjonetti-Boudreau, D.; Jacques, F.; Tastet, L.; Salaun, E.; Clavel, M.A. Prognostic utility of N-terminal pro B-type natriuretic peptide ratio in mixed aortic valve disease. Open Heart 2023, 10, e002361. [Google Scholar] [CrossRef] [PubMed]
- Weber, M.; Hausen, M.; Arnold, R.; Nef, H.; Moellman, H.; Berkowitsch, A.; Elsaesser, A.; Brandt, R.; Mitrovic, V.; Hamm, C. Prognostic value of N-terminal pro-B-type natriuretic peptide for conservatively and surgically treated patients with aortic valve stenosis. Heart 2006, 92, 1639–1644. [Google Scholar] [CrossRef] [PubMed]
- Ito, S.; Miranda, W.R.; Jaffe, A.S.; Oh, J.K. Prognostic Value of N-Terminal Pro-form B-Type Natriuretic Peptide in Patients with Moderate Aortic Stenosis. Am. J. Cardiol. 2020, 125, 1566–1570. [Google Scholar] [CrossRef] [PubMed]
- Barbieri, F.; Senoner, T.; Adukauskaite, A.; Dobner, S.; Holfeld, J.; Semsroth, S.; Lambert, T.; Zweiker, D.; Theurl, T.; Rainer, P.P.; et al. Long-Term Prognostic Value of High-Sensitivity Troponin T Added to N-Terminal Pro Brain Natriuretic Peptide Plasma Levels Before Valve Replacement for Severe Aortic Stenosis. Am. J. Cardiol. 2019, 124, 1932–1939. [Google Scholar] [CrossRef]
- Auensen, A.; Hussain, A.I.; Falk, R.S.; Walle-Hansen, M.M.; Bye, J.; Pettersen, K.I.; Aukrust, P.; Ueland, T.; Gullestad, L.L. Associations of brain-natriuretic peptide, high-sensitive troponin T, and high-sensitive C-reactive protein with outcomes in severe aortic stenosis. PLoS ONE 2017, 12, e0179304. [Google Scholar] [CrossRef]
- Hadziselimovic, E.; Greve, A.M.; Sajadieh, A.; Olsen, M.H.; Kesäniemi, Y.A.; Nienaber, C.A.; Ray, S.G.; Rossebø, A.B.; Wachtell, K.; Nielsen, O.W. Association of high-sensitivity troponin T with outcomes in asymptomatic non-severe aortic stenosis: A post-hoc substudy of the SEAS trial. EClinicalMedicine 2023, 58, 101875. [Google Scholar] [CrossRef]
- Ferrer-Sistach, E.; Lupón, J.; Cediel, G.; Teis, A.; Gual, F.; Serrano, S.; Vallejo, N.; Juncà, G.; López-Ayerbe, J.; Bayés-Genís, A. High-sensitivity troponin T in asymptomatic severe aortic stenosis. Biomarkers 2019, 24, 334–340. [Google Scholar] [CrossRef]
- Holmgren, A.; Ljungberg, J.; Hultdin, J.; Johansson, B.; Bergdahl, I.A.; Näslund, U.; Söderberg, S. Troponin T but not C reactive protein is associated with future surgery for aortic stenosis: A population-based nested case-referent study. Open Heart 2020, 7, e001325. [Google Scholar] [CrossRef] [PubMed]
- Drăgan, A.; Sinescu, I. The Role of the Cardiac Biomarkers in the Renal Cell Carcinoma Multidisciplinary Management. Diagnostics 2023, 13, 1912. [Google Scholar] [CrossRef] [PubMed]
- Perry, A.S.; Stein, E.J.; Biersmith, M.; Fearon, W.F.; Elmariah, S.; Kim, J.B.; Clark, D.E.; Patel, J.N.; Gonzales, H.; Baker, M.; et al. Global Longitudinal Strain and Biomarkers of Cardiac Damage and Stress as Predictors of Outcomes After Transcatheter Aortic Valve Implantation. J. Am. Heart Assoc. 2022, 11, e026529. [Google Scholar] [CrossRef] [PubMed]
- Fragão-Marques, M.; Vitorino, R.; Barroso, I.; Falcão-Pires, I.; Leite-Moreira, A.; Trindade, F. Pericardial Fluid Annexin A1 Is a Marker of Atrial Fibrillation in Aortic Stenosis: A Proteomics Analysis. J. Pers. Med. 2022, 12, 264. [Google Scholar] [CrossRef] [PubMed]
- Hu, P.; Chen, H.; Wang, L.H.; Jiang, J.B.; Li, J.M.; Tang, M.Y.; Guo, Y.C.; Zhu, Q.F.; Pu, Z.X.; Lin, X.P.; et al. Elevated N-terminal pro C-type natriuretic peptide is associated with mortality in patients undergoing transcatheter aortic valve replacement. BMC Cardiovasc. Disord. 2022, 22, 164. [Google Scholar] [CrossRef]
- Tan, E.S.J.; Oon, Y.Y.; Chan, S.P.; Liew, O.W.; Chong, J.P.C.; Tay, E.; Soo, W.M.; Yip, J.W.L.; Gong, L.; Lunaria, J.B.; et al. Novel predictive role for mid-regional proadrenomedullin in moderate to severe aortic stenosis. Heart 2022, 108, 1319–1327. [Google Scholar] [CrossRef]
- Abdelaziz Mohamed, I.; Gadeau, A.P.; Hasan, A.; Abdulrahman, N.; Mraiche, F. Osteopontin: A Promising Therapeutic Target in Cardiac Fibrosis. Cells 2019, 8, 1558. [Google Scholar] [CrossRef]
- Lutz, M.; von Ingersleben, N.; Lambers, M.; Rosenberg, M.; Freitag-Wolf, S.; Dempfle, A.; Lutter, G.; Frank, J.; Bramlage, P.; Frey, N.; et al. Osteopontin predicts clinical outcome in patients after treatment of severe aortic stenosis with transcatheter aortic valve implantation (TAVI). Open Heart 2017, 4, e000633. [Google Scholar] [CrossRef]
- Weber, A.; Büttner, A.; Rellecke, P.; Petrov, G.; Albert, A.; Sixt, S.U.; Lichtenberg, A.; Akhyari, P. Osteopontin as novel biomarker for reversibility of pressure overload induced left ventricular hypertrophy. Biomark. Med. 2020, 14, 513–523. [Google Scholar] [CrossRef]
- Villar, A.V.; Cobo, M.; Llano, M.; Montalvo, C.; González-Vílchez, F.; Martín-Durán, R.; Hurlé, M.A.; Nistal, J.F. Plasma levels of transforming growth factor-beta1 reflect left ventricular remodeling in aortic stenosis. PLoS ONE 2009, 4, e8476. [Google Scholar] [CrossRef]
- Ramchand, J.; Patel, S.K.; Kearney, L.G.; Matalanis, G.; Farouque, O.; Srivastava, P.M.; Burrell, L.M. Plasma ACE2 Activity Predicts Mortality in Aortic Stenosis and Is Associated With Severe Myocardial Fibrosis. JACC Cardiovasc. Imaging. 2020, 13, 655–664. [Google Scholar] [CrossRef]
- Yalta, K.; Palabiyik, O.; Gurdogan, M.; Gurlertop, Y. Serum copeptin might improve risk stratification and management of aortic valve stenosis: A review of pathophysiological insights and practical implications. Ther. Adv. Cardiovasc. Dis. 2019, 13, 1753944719826420. [Google Scholar] [CrossRef]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Drăgan, A.; Mateescu, A.D. Novel Biomarkers and Advanced Cardiac Imaging in Aortic Stenosis: Old and New. Biomolecules 2023, 13, 1661. https://doi.org/10.3390/biom13111661
Drăgan A, Mateescu AD. Novel Biomarkers and Advanced Cardiac Imaging in Aortic Stenosis: Old and New. Biomolecules. 2023; 13(11):1661. https://doi.org/10.3390/biom13111661
Chicago/Turabian StyleDrăgan, Anca, and Anca Doina Mateescu. 2023. "Novel Biomarkers and Advanced Cardiac Imaging in Aortic Stenosis: Old and New" Biomolecules 13, no. 11: 1661. https://doi.org/10.3390/biom13111661
APA StyleDrăgan, A., & Mateescu, A. D. (2023). Novel Biomarkers and Advanced Cardiac Imaging in Aortic Stenosis: Old and New. Biomolecules, 13(11), 1661. https://doi.org/10.3390/biom13111661







