Intervention in Neuropsychiatric Disorders by Suppressing Inflammatory and Oxidative Stress Signal and Exploration of In Silico Studies for Potential Lead Compounds from Holigarna caustica (Dennst.) Oken leaves
Abstract
1. Introduction
2. Materials and Methods
2.1. Drugs, Chemicals, and Equipment
2.2. Plant Collection, Identification, and Preparation of Methanol Extract (MEHC)
2.3. In Vivo Neuropharmacological Activity
2.3.1. Experimental Animals and Ethical Statements
2.3.2. Acute Oral Toxicity Test
2.3.3. Experimental Design (Drugs and Treatments)
2.3.4. Anxiolytic Activity
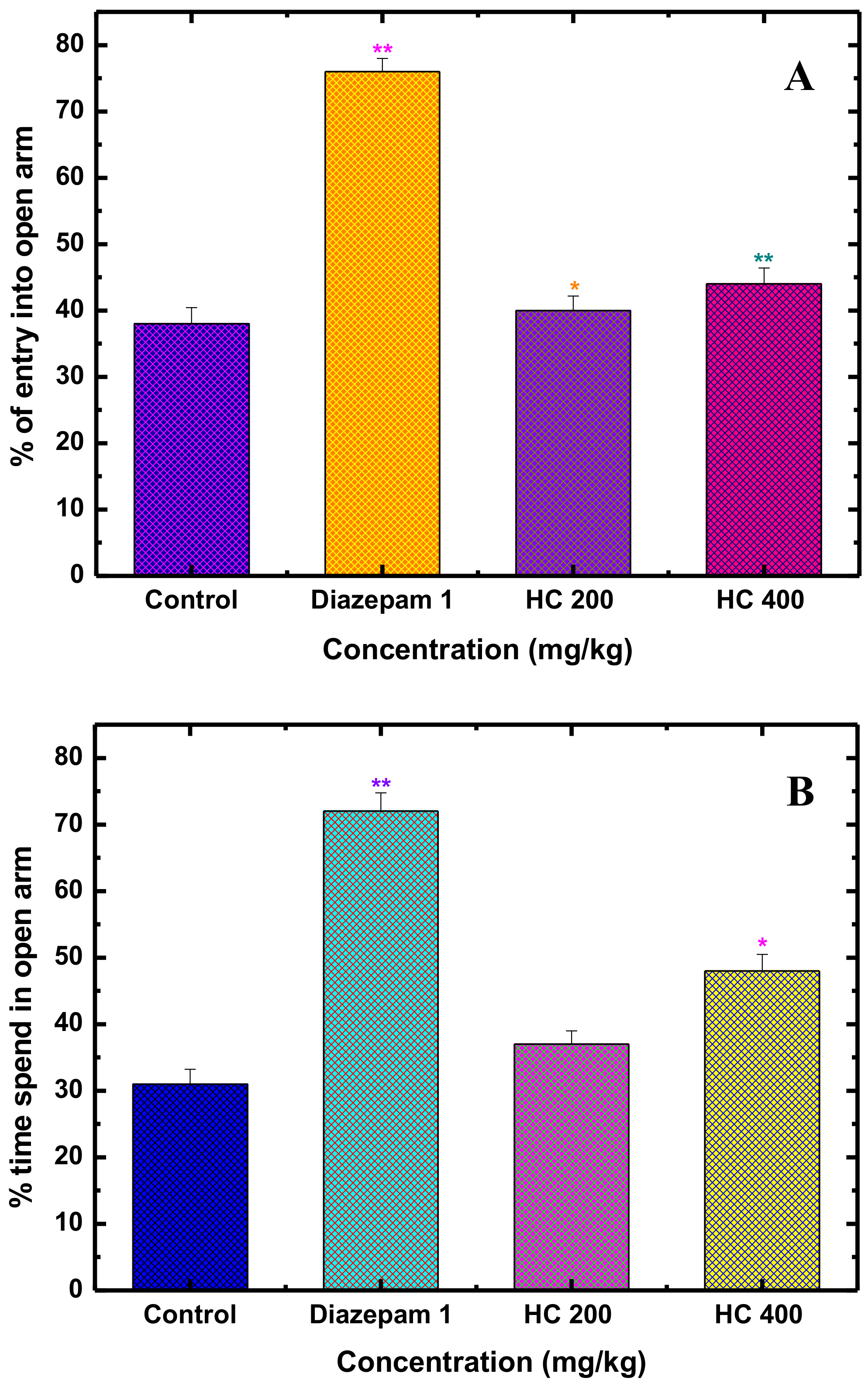
Elevated Plus Maze Test in Mice (EPM)
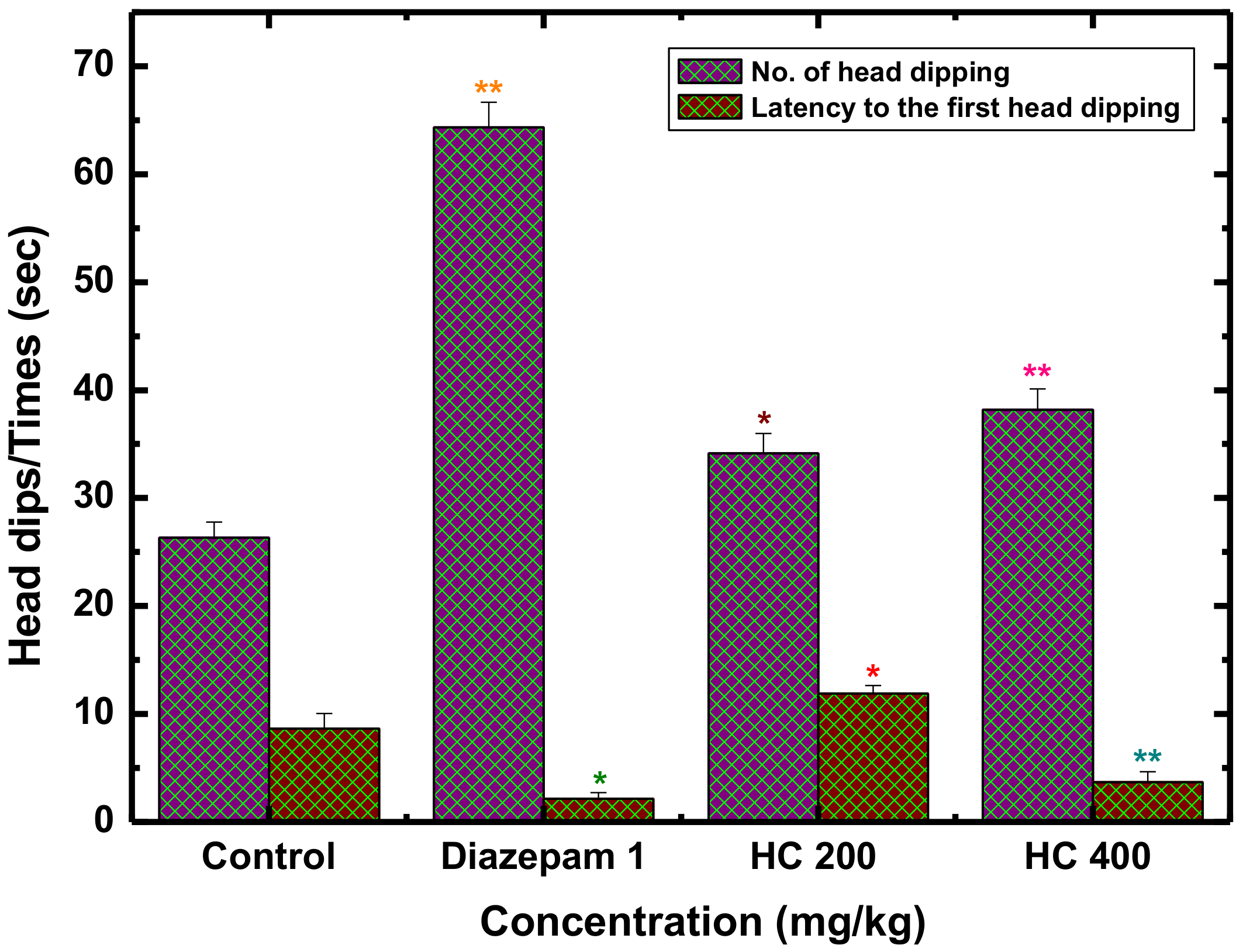
Hole-Board Test for Exploratory Behavior in Mice (HBT)
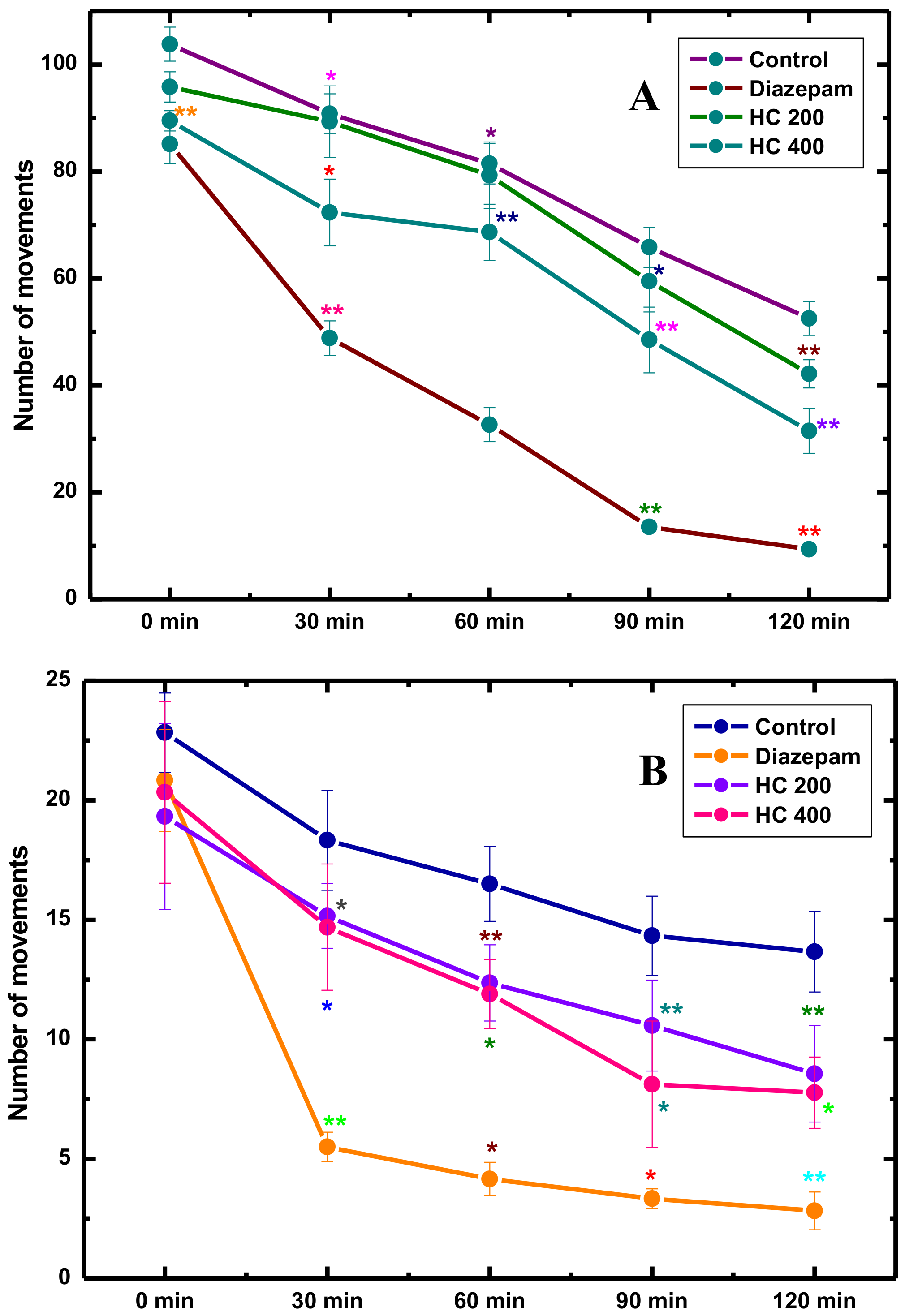
2.3.5. Locomotor and Exploration Activity
Open Field Test (OFT)
Hole-Cross Test (HCT)
2.3.6. Antidepressant Activity
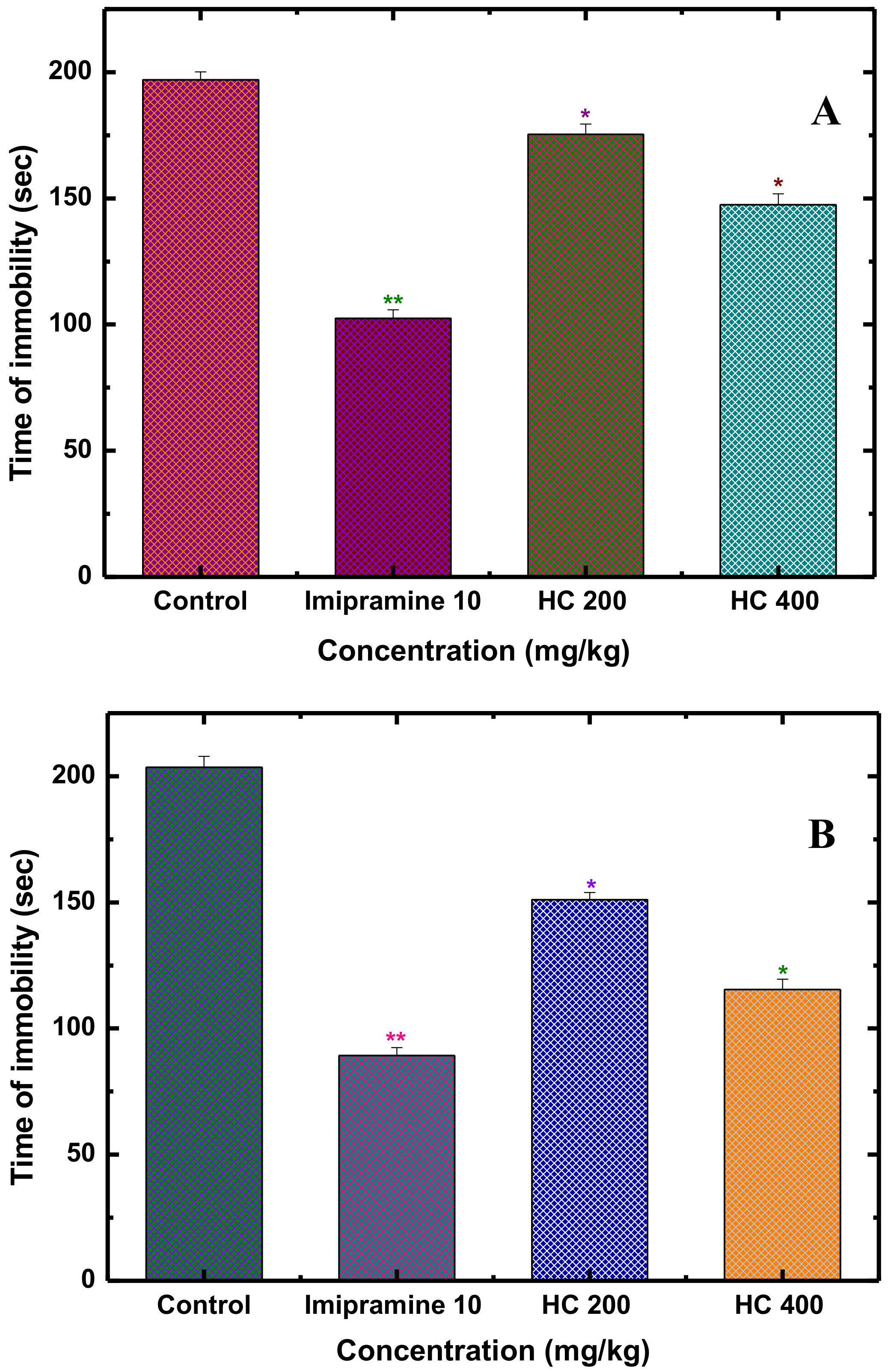
Forced Swim Test (FST)
Tail Suspension Test (TST)
2.4. Anti-Inflammatory Activity of MEHC in Histamine-Induced Paw Edema Test in Mice
2.5. In Vitro Antioxidant Activity
2.5.1. 1,1-Diphenyl-2-picrylhydrazyl Radical (DPPH) Radical Scavenging Activity
2.5.2. H2O2 Scavenging Activity
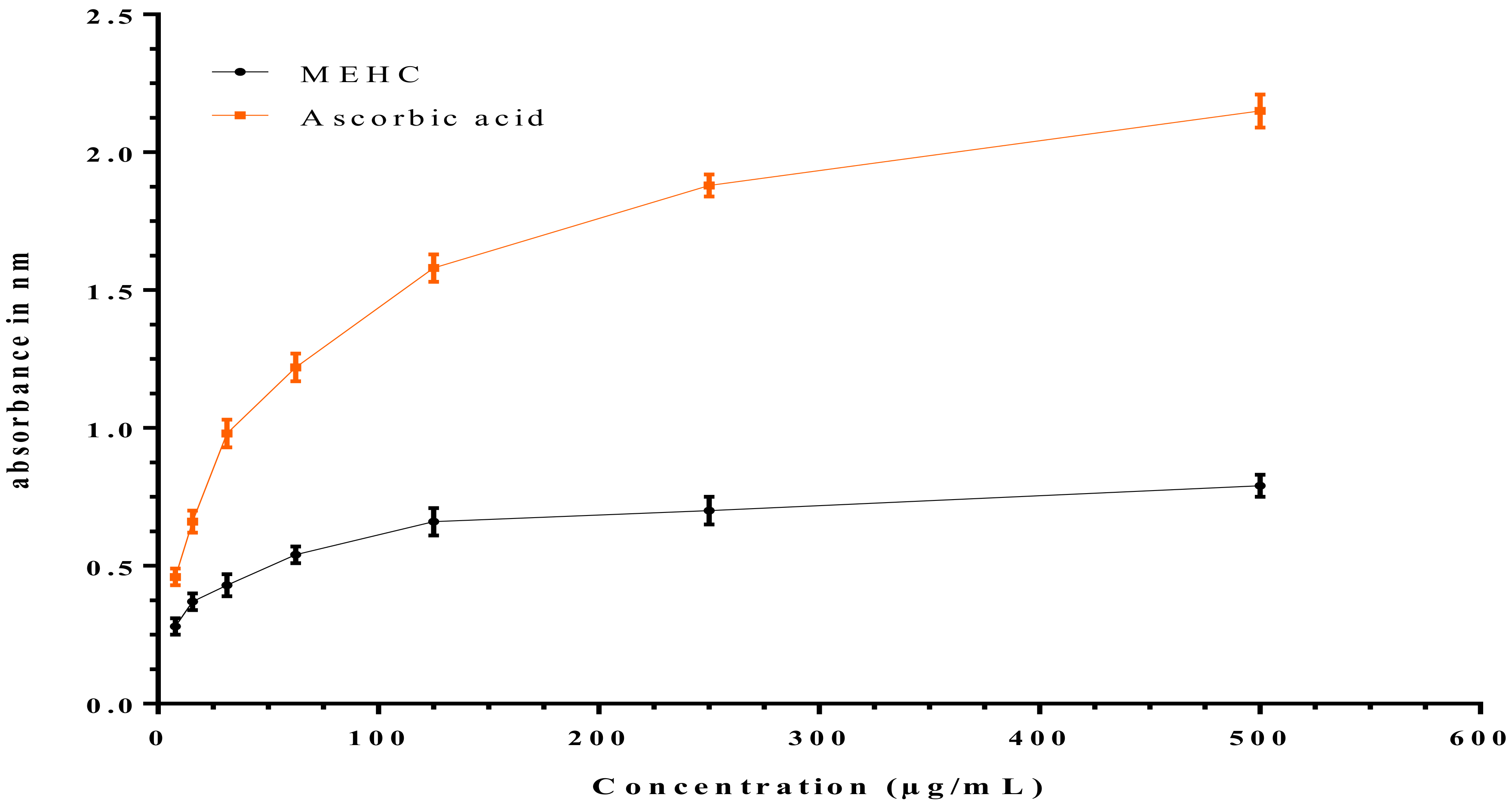
2.5.3. Ferric Reducing Power Assay (FRPA)
2.6. Quantitative Phytochemical Analysis
2.6.1. Determination of Total Antioxidant Capacity (TAC)
2.6.2. Determination of Total Phenolic Content (TPC)
2.6.3. Determination of Total Flavonoid Content
2.6.4. Determination of Total Flavonol Content
2.6.5. Determination of Total Proanthocyanidin Content
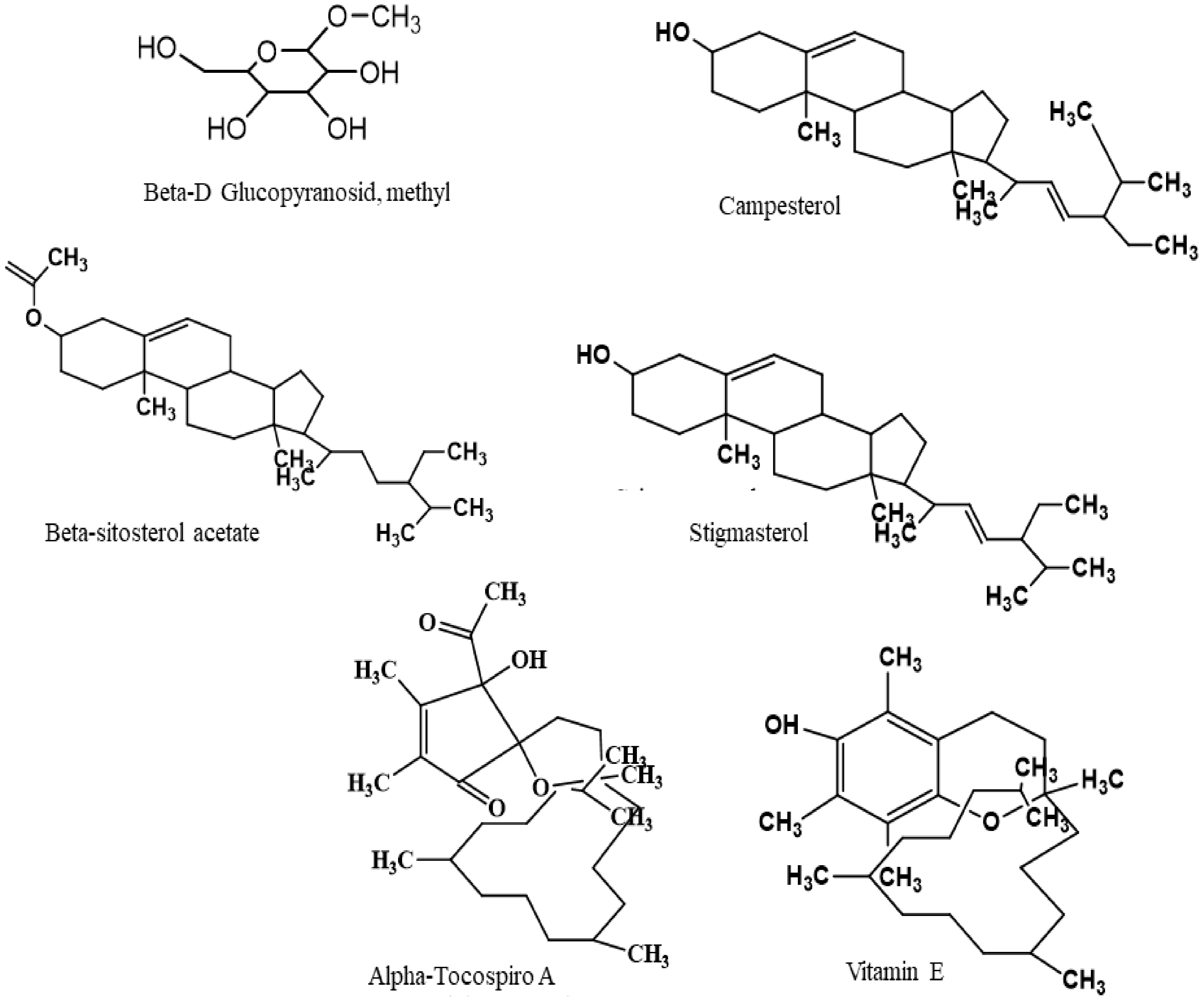
2.7. Chemical Compounds Studied in this Article
2.8. In Silico Studies
2.8.1. Molecular Docking Analysis: Ligand Preparation
2.8.2. Molecular Docking Analysis: Enzyme/Receptor Preparation
2.8.3. Molecular Docking Analysis: Glide Standard Precision Docking
2.8.4. In Silico Study: Determination of Pharmacokinetic Parameters by SwissADME
2.8.5. In Silico Study: Toxicological Properties Prediction by AdmetSAR
2.8.6. In Silico Study: Prediction of Activity Spectra for Substances (PASS) Study by PASS Online
2.9. Statistical Analysis
3. Results and Discussion
3.1. Anxiolytic Activity
3.2. Locomotor and Exploration Activity
3.3. Antidepressant Activity
3.4. Histamine-Induced Paw Edema (Anti-Inflammatory Test)
3.5. In Vitro Antioxidant Activity
3.6. Quantitative Phytochemical Analysis
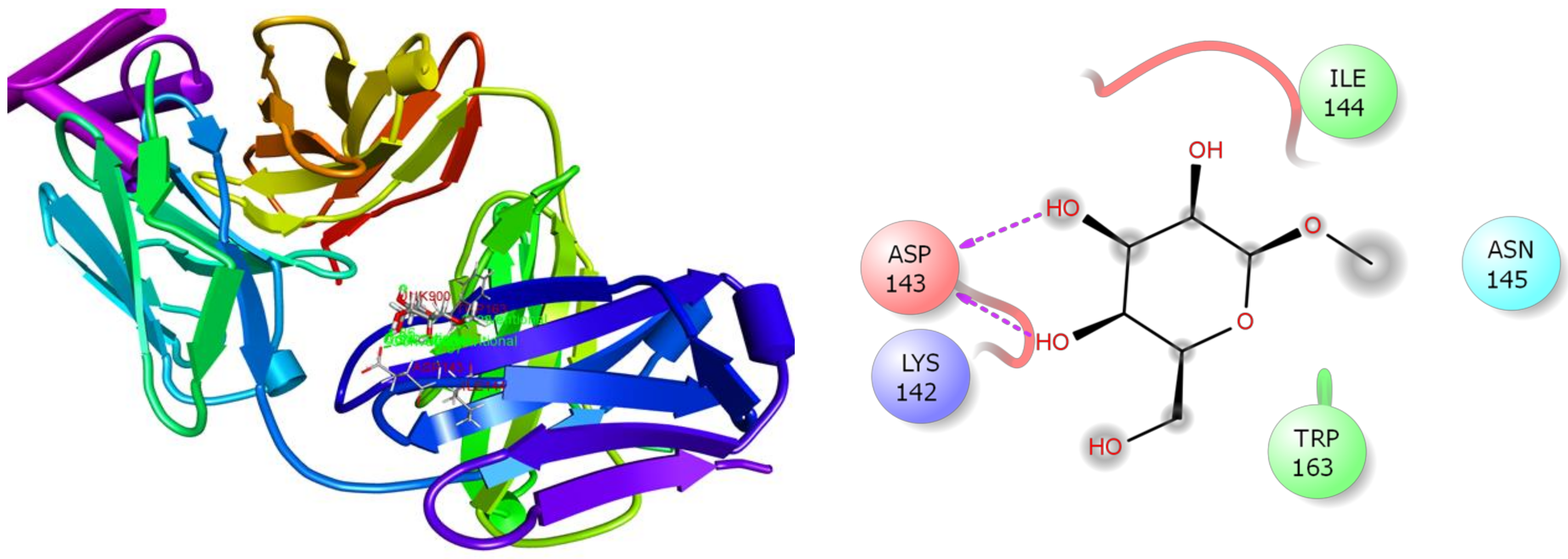
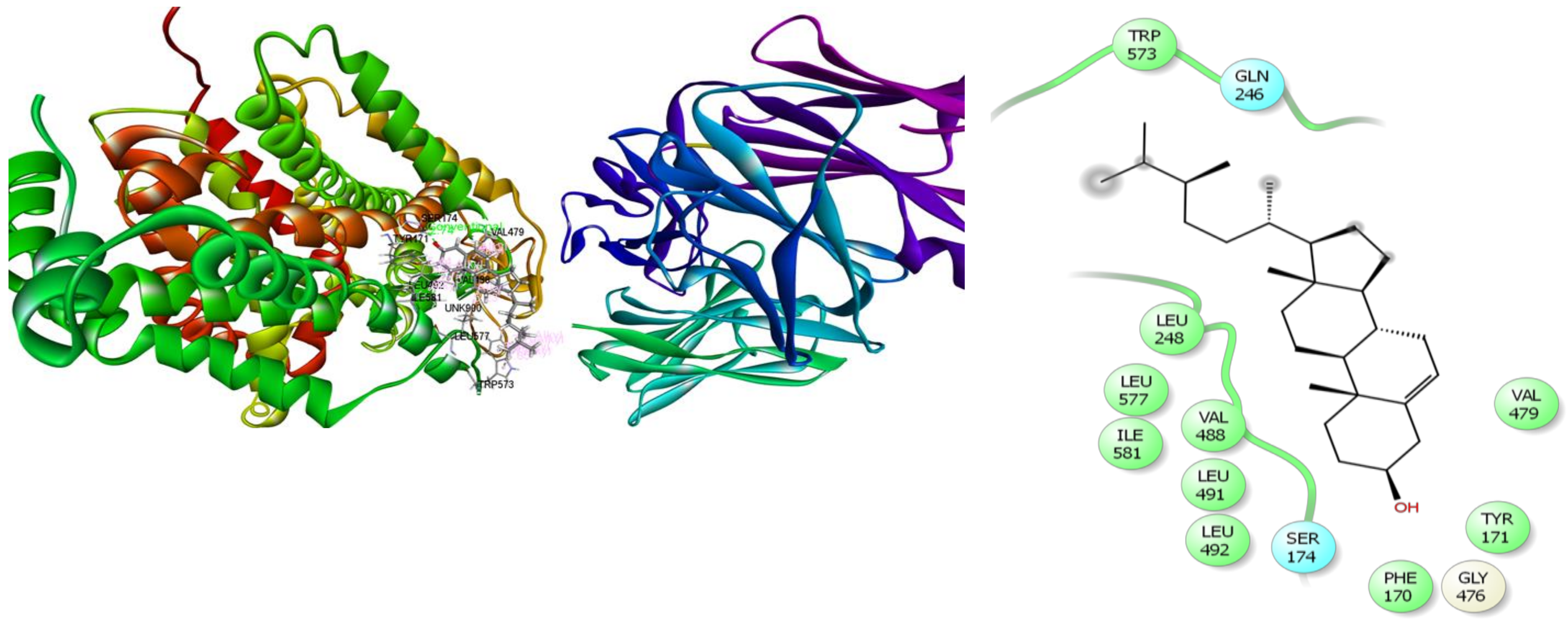
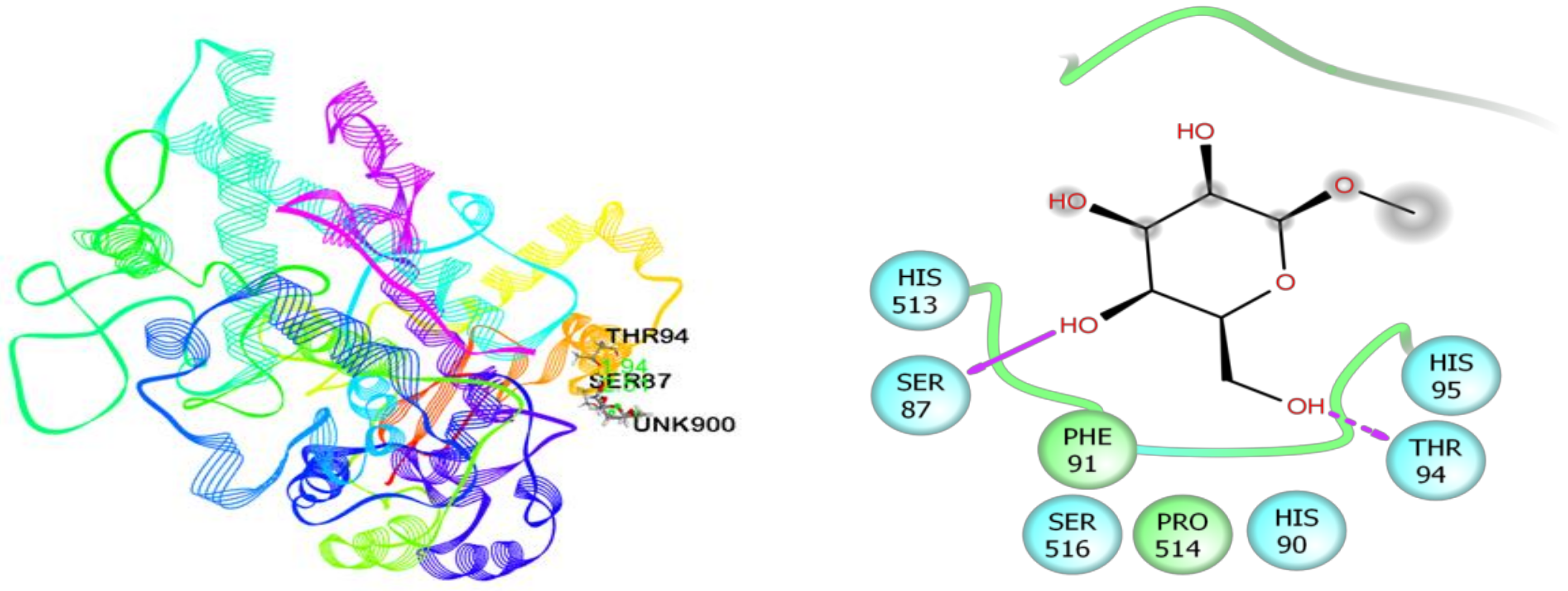
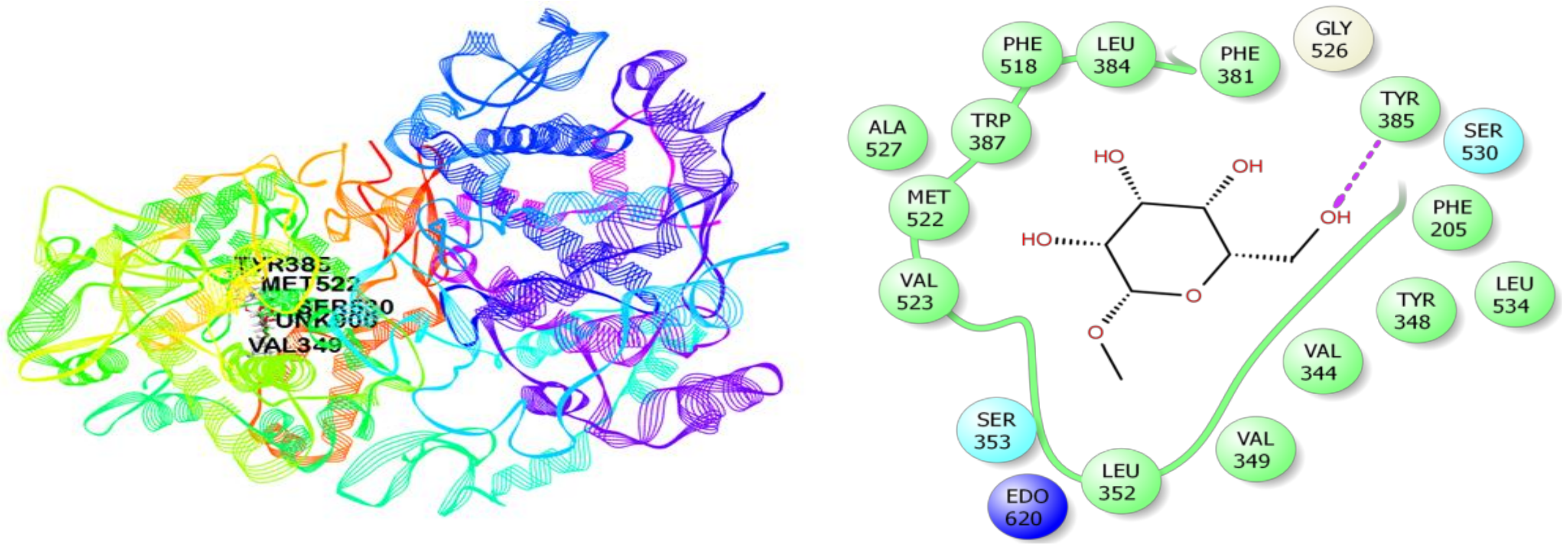
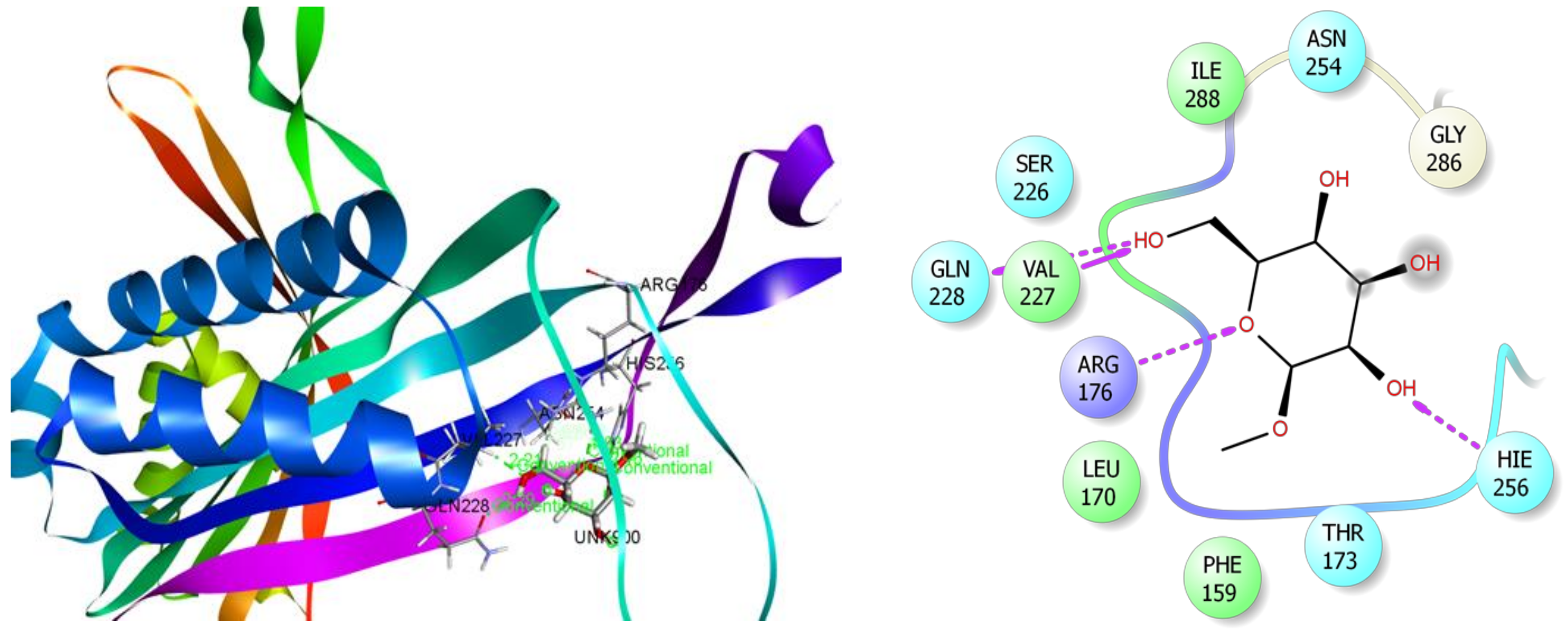
3.7. In Silico Studies
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| MEHC refers to methanol extract of Holigarna caustica leaves | |
| p.o.: | per oral; |
| i.p.: | Intraperitoneal; |
| ANOVA: | Analysis of variance; |
| BW: | body weight; |
| SEM: | standard error of mean; |
| SPSS: | statistical package for social science. |
| ADME/T: | Absorption, Distribution, Metabolism, Excretion, and Toxicity; |
| PASS: | Prediction of Activity Spectra for Substances. |
References
- Depressive Disorders - Psychiatric Disorders - MSD Manual Professional Edition. Available online: https://www.msdmanuals.com/professional/psychiatric-disorders/mood-disorders/depressive-disorders (accessed on 20 December 2019).
- Global Burden of Disease Study 2017 (GBD 2017) Data Resources | GHDx. Available online: http://ghdx.healthdata.org/gbd-2017 (accessed on 20 December 2019).
- World Health Organization. Depression and other common mental disorders: Global health estimates; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Möller, H.-J.; Bandelow, B.; Volz, H.-P.; Barnikol, U.B.; Seifritz, E.; Kasper, S. The relevance of ‘mixed anxiety and depression’as a diagnostic category in clinical practice. Eur. Arch. Psychiatry Clin. Neurosci. 2016, 266, 725–736. [Google Scholar] [CrossRef] [PubMed]
- Kara, S.; Yazici, K.M.; Güleç, C.; Ünsal, I. Mixed anxiety–depressive disorder and major depressive disorder: Comparison of the severity of illness and biological variables. Psychiatry Res. 2000, 94, 59–66. [Google Scholar] [CrossRef]
- Berton, O.; Nestler, E.J. New approaches to antidepressant drug discovery: Beyond monoamines. Nat. Rev. Neurosci. 2006, 7, 137. [Google Scholar] [CrossRef] [PubMed]
- Han, C.; Pae, C.-U. Pain and depression: A neurobiological perspective of their relationship. Psychiatry Investig. 2015, 12, 1. [Google Scholar] [CrossRef]
- Marks, D.M.; Shah, M.J.; Patkar, A.A.; Masand, P.S.; Park, G.-Y.; Pae, C.-U. Serotonin-norepinephrine reuptake inhibitors for pain control: Premise and promise. Curr. Neuropharmacol. 2009, 7, 331–336. [Google Scholar] [CrossRef]
- Hassan, W.; Eduardo Barroso Silva, C.; Mohammadzai, I.U.; Batista Teixeira da Rocha, J.; Landeira-Fernandez, J. Association of oxidative stress to the genesis of anxiety: Implications for possible therapeutic interventions. Curr. Neuropharmacol. 2014, 12, 120–139. [Google Scholar] [CrossRef]
- Beckhauser, T.F.; Francis-Oliveira, J.; De Pasquale, R. Reactive oxygen species: Physiological and physiopathological effects on synaptic plasticity: Supplementary issue: Brain plasticity and repair. J. Exp. Neurosci. 2016, 10, JEN-S39887. [Google Scholar] [CrossRef]
- Bakunina, N.; Pariante, C.M.; Zunszain, P.A. Immune mechanisms linked to depression via oxidative stress and neuroprogression. Immunology 2015, 144, 365–373. [Google Scholar] [CrossRef]
- Penn, E.; Tracy, D.K. The drugs don’t work? Antidepressants and the current and future pharmacological management of depression. Ther. Adv. Psychopharmacol. 2012, 2, 179–188. [Google Scholar] [CrossRef]
- Wang, S.-M.; Han, C.; Bahk, W.-M.; Lee, S.-J.; Patkar, A.A.; Masand, P.S.; Pae, C.-U. Addressing the side effects of contemporary antidepressant drugs: A comprehensive review. Chonnam Med. J. 2018, 54, 101–112. [Google Scholar] [CrossRef]
- Cox, P.A.; Balick, M.J. The ethnobotanical approach to drug discovery. Sci. Am. 1994, 270, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Balunas, M.J.; Kinghorn, A.D. Drug discovery from medicinal plants. Life Sci. 2005, 78, 431–441. [Google Scholar] [CrossRef] [PubMed]
- Dutra, R.C.; Campos, M.M.; Santos, A.R.S.; Calixto, J.B. Medicinal plants in Brazil: Pharmacological studies, drug discovery, challenges and perspectives. Pharmacol. Res. 2016, 112, 4–29. [Google Scholar] [CrossRef] [PubMed]
- Quattrocchi, U. CRC World Dictionary of Medicinal and Poisonous Plants: Common Names, Scientific Names, Eponyms, Synonyms, and Etymology (5 Volume Set); CRC press: Boca Raton, FL, USA, 2012; ISBN 142008044X. [Google Scholar]
- Adnan, M.; Nazim Uddin Chy, M.; Mostafa Kamal, A.T.M.; Barlow, J.W.; Faruque, M.O.; Yang, X.; Uddin, S.B. Evaluation of anti-nociceptive and anti-inflammatory activities of the methanol extract of Holigarna caustica (Dennst.) Oken leaves. J. Ethnopharmacol. 2019, 236. [Google Scholar] [CrossRef]
- Nih, O.D.; Oer, O. Guide Laboratory Animals For The Care And Use OF Eighth Edition Committee for the Update of the Guide for the Care and Use of Laboratory Animals Institute for Laboratory Animal Research Division on Earth and Life Studies; National Academics Press: Washington, DC, USA, 2011; ISBN 9780309154000. [Google Scholar]
- Pellow, S.; File, S.E. Anxiolytic and anxiogenic drug effects on exploratory activity in an elevated plus-maze: A novel test of anxiety in the rat. Pharmacol. Biochem. Behav. 1986, 24, 525–529. [Google Scholar] [CrossRef]
- Sonavane, G.S.; Sarveiya, V.P.; Kasture, V.S.; Kasture, S.B. Anxiogenic activity of Myristica fragrans seeds. Pharmacol. Biochem. Behav. 2002, 71, 239–244. [Google Scholar] [CrossRef]
- Gupta, B.D.; Dandiya, P.C.; Gupta, M.L. A psycho-pharmacological analysis of behaviour in rats. Jpn. J. Pharmacol. 1971, 21, 293–298. [Google Scholar] [CrossRef]
- Takagi, K.; WATANABE, M.; SAITO, H. Studies of the spontaneous movement of animals by the hole cross test; effect of 2-dimethyl-aminoethanol and its acyl esters on the central nervous system. Jpn. J. Pharmacol. 1971, 21, 797–810. [Google Scholar] [CrossRef]
- Porsolt, R.D.; Bertin, A.; Jalfre, M. Behavioral despair in mice: A primary screening test for antidepressants. Arch. Int. Pharmacodyn. thérapie 1977, 229, 327–336. [Google Scholar]
- Steru, L.; Chermat, R.; Thierry, B.; Simon, P. The tail suspension test: A new method for screening antidepressants in mice. Psychopharmacology (Berl). 1985, 85, 367–370. [Google Scholar] [CrossRef]
- Adnan, M.; Chy, N.U.; Mostafa Kamal, A.T.M.; Azad, M.O.K.; Paul, A.; Uddin, S.B.; Barlow, J.W.; Faruque, M.O.; Park, C.H.; Cho, D.H. Investigation of the Biological Activities and Characterization of Bioactive Constituents of Ophiorrhiza rugosa var. prostrata (D. Don) & Mondal Leaves through In Vivo, In Vitro, and In Silico Approaches. Molecules 2019, 24, 1367. [Google Scholar]
- Braca, A.; De Tommasi, N.; Di Bari, L.; Pizza, C.; Politi, M.; Morelli, I. Antioxidant principles from bauhinia t arapotensis. J. Nat. Prod. 2001, 64, 892–895. [Google Scholar] [CrossRef] [PubMed]
- Adnan, M.; Chy, M.N.U.; Rudra, S.; Tahamina, A.; Das, R.; Tanim, M.A.H.; Siddique, T.I.; Hoque, A.; Tasnim, S.M.; Paul, A. Evaluation of Bonamia semidigyna (Roxb.) for antioxidant, antibacterial, anthelmintic and cytotoxic properties with the involvement of polyphenols. Orient. Pharm. Exp. Med. 2019, 19, 187–199. [Google Scholar] [CrossRef]
- Ruch, R.J.; Cheng, S.; Klaunig, J.E. Prevention of cytotoxicity and inhibition of intercellular communication by antioxidant catechins isolated from Chinese green tea. Carcinogenesis 1989, 10, 1003–1008. [Google Scholar] [CrossRef] [PubMed]
- Oyaizu, M. Studies on products of browning reaction. Japanese J. Nutr. Diet. 1986, 44, 307–315. [Google Scholar] [CrossRef]
- Garratt, D.C. The quantitative analysis of drugs; Springer Science & Business Media: Berlin, Germany, 2012; ISBN 1461333806. [Google Scholar]
- Harborne, A.J. Phytochemical methods a guide to modern techniques of plant analysis; Springer Science & Business Media: Berlin, Germany, 1998; ISBN 0412572702. [Google Scholar]
- Aiyegoro, O.A.; Okoh, A.I. Preliminary phytochemical screening and in vitro antioxidant activities of the aqueous extract of Helichrysum longifolium DC. BMC Complement. Altern. Med. 2010, 10, 21. [Google Scholar] [CrossRef] [PubMed]
- Kumaran, A.; Karunakaran, R.J. In vitro antioxidant activities of methanol extracts of five Phyllanthus species from India. LWT-Food Sci. Technol. 2007, 40, 344–352. [Google Scholar] [CrossRef]
- Oyedemi, S.O.; Bradley, G.; Afolayan, A.J. In-vitro and-vivo antioxidant activities of aqueous extract of Strychnos henningsii Gilg. African J. Pharm. Pharmacol. 2010, 4, 70–78. [Google Scholar]
- Berman, H.M.; Battistuz, T.; Bhat, T.N.; Bluhm, W.F.; Bourne, P.E.; Burkhardt, K.; Feng, Z.; Gilliland, G.L.; Iype, L.; Jain, S. The protein data bank Acta Crystallogr. D Biol. Crystallogr 2002, 58, 899–907. [Google Scholar] [CrossRef] [PubMed]
- Lenaeus, M.J.; Burdette, D.; Wagner, T.; Focia, P.J.; Gross, A. Structures of KcsA in complex with symmetrical quaternary ammonium compounds reveal a hydrophobic binding site. Biochemistry 2014, 53, 5365–5373. [Google Scholar] [CrossRef]
- Coleman, J.A.; Green, E.M.; Gouaux, E. X-ray structures and mechanism of the human serotonin transporter. Nature 2016, 532, 334. [Google Scholar] [CrossRef] [PubMed]
- Harman, C.A.; Turman, M.V.; Kozak, K.R.; Marnett, L.J.; Smith, W.L.; Garavito, R.M. Structural basis of enantioselective inhibition of cyclooxygenase-1 by S-α-substituted indomethacin ethanolamides. J. Biol. Chem. 2007, 282, 28096–28105. [Google Scholar] [CrossRef] [PubMed]
- Vecchio, A.J.; Simmons, D.M.; Malkowski, M.G. Structural basis of fatty acid substrate binding to cyclooxygenase-2. J. Biol. Chem. 2010, 285, 22152–22163. [Google Scholar] [CrossRef] [PubMed]
- Retailleau, P.; Colloc’h, N.; Vivarès, D.; Bonnete, F.; Castro, B.; El Hajji, M.; Mornon, J.-P.; Monard, G.; Prangé, T. Complexed and ligand-free high-resolution structures of urate oxidase (Uox) from Aspergillus flavus: A reassignment of the active-site binding mode. Acta Crystallogr. Sect. D Biol. Crystallogr. 2004, 60, 453–462. [Google Scholar] [CrossRef] [PubMed]
- Friesner, R.A.; Banks, J.L.; Murphy, R.B.; Halgren, T.A.; Klicic, J.J.; Mainz, D.T.; Repasky, M.P.; Knoll, E.H.; Shelley, M.; Perry, J.K. Glide: A new approach for rapid, accurate docking and scoring. 1. Method and assessment of docking accuracy. J. Med. Chem. 2004, 47, 1739–1749. [Google Scholar] [CrossRef] [PubMed]
- Chy, M.N.U.; Adnan, M.; Rauniyar, A.K.; Amin, M.M.; Majumder, M.; Islam, M.S.; Afrin, S.; Farhana, K.; Nesa, F.; Sany, M.A. Evaluation of anti-nociceptive and anti-inflammatory activities of Piper sylvaticum (Roxb.) stem by experimental and computational approaches. Orient. Pharm. Exp. Med. 2019, 1–15. [Google Scholar] [CrossRef]
- admetSAR. Available online: http://lmmd.ecust.edu.cn/admetsar2/ (accessed on 31 March 2020).
- Ekor, M. The growing use of herbal medicines: Issues relating to adverse reactions and challenges in monitoring safety. Front. Pharmacol. 2014, 4, 177. [Google Scholar] [CrossRef]
- Nissen, N. Practitioners of Western herbal medicine and their practice in the UK: Beginning to sketch the profession. Complement. Ther. Clin. Pract. 2010, 16, 181–186. [Google Scholar] [CrossRef]
- Sarwar, R.; Farooq, U.; Naz, S.; Khan, A.; Bukhari, S.M.; Khan, H.; Karim, N.; Khan, I.; Ahmed, A.; Al-Harrasi, A. Isolation and Characterization of Two New Secondary Metabolites From Quercus incana and Their Antidepressant-and Anxiolytic-Like Potential. Front. Pharmacol. 2018, 9, 298. [Google Scholar] [CrossRef]
- Singh, Y.N.; Singh, N.N. Therapeutic potential of kava in the treatment of anxiety disorders. CNS Drugs 2002, 16, 731–743. [Google Scholar] [CrossRef]
- Benson, S.; Downey, L.A.; Stough, C.; Wetherell, M.; Zangara, A.; Scholey, A. An acute, double-blind, placebo-controlled cross-over study of 320 mg and 640 mg doses of Bacopa monnieri (CDRI 08) on multitasking stress reactivity and mood. Phyther. Res. 2014, 28, 551–559. [Google Scholar] [CrossRef]
- Ngan, A.; Conduit, R. A double-blind, placebo-controlled investigation of the effects of Passiflora incarnata (Passionflower) herbal tea on subjective sleep quality. Phyther. Res. 2011, 25, 1153–1159. [Google Scholar] [CrossRef] [PubMed]
- Amsterdam, J.D.; Yao, Y.; Mao, J.J.; Soeller, I.; Rockwell, K.; Shults, J. Randomized, double-blind, placebo-controlled trial of Cimicifuga racemosa (black cohosh) in women with anxiety disorder due to menopause. J. Clin. Psychopharmacol. 2009, 29, 478. [Google Scholar] [CrossRef] [PubMed]
- Agha-Hosseini, M.; Kashani, L.; Aleyaseen, A.; Ghoreishi, A.; Rahmanpour, H.; Zarrinara, A.R.; Akhondzadeh, S. Crocus sativus L.(saffron) in the treatment of premenstrual syndrome: A double-blind, randomised and placebo-controlled trial. BJOG An Int. J. Obstet. Gynaecol. 2008, 115, 515–519. [Google Scholar] [CrossRef] [PubMed]
- Fajemiroye, J.O.; da Silva, D.M.; de Oliveira, D.R.; Costa, E.A. Treatment of anxiety and depression: Medicinal plants in retrospect. Fundam. Clin. Pharmacol. 2016, 30, 198–215. [Google Scholar] [CrossRef]
- Williamson, E.M.; Okpako, D.T.; Evans, F.J. Pharmacological methods in phytotherapy research: Volume 1: Selection, preparation and pharmacological evaluation of plant material; John Wiley & Sons Ltd.: Hoboken, NJ, USA, 1996; ISBN 0471942170. [Google Scholar]
- Cryan, J.F.; Sweeney, F.F. The age of anxiety: Role of animal models of anxiolytic action in drug discovery. Br. J. Pharmacol. 2011, 164, 1129–1161. [Google Scholar] [CrossRef]
- Fuchs, E.; Flügge, G. Experimental animal models for the simulation of depression and anxiety. Dialogues Clin. Neurosci. 2006, 8, 323. [Google Scholar]
- Lister, R.G. The use of a plus-maze to measure anxiety in the mouse. Psychopharmacology (Berl). 1987, 92, 180–185. [Google Scholar] [CrossRef]
- Adnan, M.; Chy, M.; Uddin, N.; Kamal, A.T.M.; Chowdhury, M.; Islam, M.; Hossain, M.; Tareq, A.M.; Bhuiyan, M.; Hossain, I. Unveiling Pharmacological Responses and Potential Targets Insights of Identified Bioactive Constituents of Cuscuta reflexa Roxb. Leaves through In Vivo and In Silico Approaches. Pharmaceuticals 2020, 13, 50. [Google Scholar] [CrossRef]
- Thoeringer, C.K.; Erhardt, A.; Sillaber, I.; Mueller, M.B.; Ohl, F.; Holsboer, F.; Keck, M.E. Long-term anxiolytic and antidepressant-like behavioural effects of tiagabine, a selective GABA transporter-1 (GAT-1) inhibitor, coincide with a decrease in HPA system activity in C57BL/6 mice. J. Psychopharmacol. 2010, 24, 733–743. [Google Scholar] [CrossRef]
- Sillaber, I.; Panhuysen, M.; Henniger, M.S.H.; Ohl, F.; Kühne, C.; Pütz, B.; Pohl, T.; Deussing, J.M.; Paez-Pereda, M.; Holsboer, F. Profiling of behavioral changes and hippocampal gene expression in mice chronically treated with the SSRI paroxetine. Psychopharmacology (Berl). 2008, 200, 557–572. [Google Scholar] [CrossRef] [PubMed]
- Adnan, M.; Chy, M.; Uddin, N.; Kama, A.T.M.; Azad, M.; Kalam, O.; Chowdhury, K.A.A.; Kabir, M.S.H.; Gupta, S.D.; Chowdhury, M. Comparative Study of Piper sylvaticum Roxb. Leaves and Stems for Anxiolytic and Antioxidant Properties Through in vivo, in vitro, and in silico Approaches. Biomedicines 2020, 8, 68. [Google Scholar] [CrossRef] [PubMed]
- Prut, L.; Belzung, C. The open field as a paradigm to measure the effects of drugs on anxiety-like behaviors: A review. Eur. J. Pharmacol. 2003, 463, 3–33. [Google Scholar] [CrossRef]
- Mandelli, M.; Tognoni, G.; Garattini, S. Clinical pharmacokinetics of diazepam. Clin. Pharmacokinet. 1978, 3, 72–91. [Google Scholar] [CrossRef]
- Sarris, J.; Teschke, R.; Stough, C.; Scholey, A.; Schweitzer, I. Re-introduction of kava (Piper methysticum) to the EU: Is there a way forward? Planta Med. 2011, 77, 107–110. [Google Scholar] [CrossRef] [PubMed]
- Mennini, T.; Caccia, S.; Garattini, S. Mechanism of action of anxiolytic drugs. In Progress in Drug Research/Fortschritte der Arzneimittelforschung/Progrès des recherches pharmaceutiques; Springer: Berlin, Germany, 1987; pp. 315–347. [Google Scholar]
- Baldwin, D.S.; Polkinghorn, C. Evidence-based pharmacotherapy of generalized anxiety disorder. Int. J. Neuropsychopharmacol. 2005, 8, 293–302. [Google Scholar] [CrossRef] [PubMed]
- Sarris, J.; Panossian, A.; Schweitzer, I.; Stough, C.; Scholey, A. Herbal medicine for depression, anxiety and insomnia: A review of psychopharmacology and clinical evidence. Eur. Neuropsychopharmacol. 2011, 21, 841–860. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Gu, J.; Wang, X.; Xie, K.; Luan, Q.; Wan, N.; Zhang, Q.; Jiang, H.; Liu, D. Antidepressant-like activity of resveratrol treatment in the forced swim test and tail suspension test in mice: The HPA axis, BDNF expression and phosphorylation of ERK. Pharmacol. Biochem. Behav. 2013, 112, 104–110. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Liu, C.; Wang, Y.; Wang, P.; Li, Y.; Li, B. Herbal medicine for anxiety, depression and insomnia. Curr. Neuropharmacol. 2015, 13, 481–493. [Google Scholar] [CrossRef]
- Tallman, J.F.; Cassella, J.; Kehne, J.; Corpora, N. Mechanism of action of anxiolytics; 2002. [Google Scholar]
- Nestler, E.J.; Barrot, M.; DiLeone, R.J.; Eisch, A.J.; Gold, S.J.; Monteggia, L.M. Neurobiology of depression. Neuron 2002, 34, 13–25. [Google Scholar] [CrossRef]
- Arborelius, L.; Owens, M.J.; Plotsky, P.M.; Nemeroff, C.B. The role of corticotropin-releasing factor in depression and anxiety disorders. J. Endocrinol. 1999, 160, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Kandere-Grzybowska, K.; Gheorghe, D.; Priller, J.; Esposito, P.; Huang, M.; Gerard, N.; Theoharides, T.C. Stress-induced dura vascular permeability does not develop in mast cell-deficient and neurokinin-1 receptor knockout mice. Brain Res. 2003, 980, 213–220. [Google Scholar] [CrossRef]
- Shelukhina, I.; Mikhailov, N.; Abushik, P.; Nurullin, L.; Nikolsky, E.E.; Giniatullin, R. Cholinergic nociceptive mechanisms in rat meninges and trigeminal ganglia: Potential implications for migraine pain. Front. Neurol. 2017, 8, 163. [Google Scholar] [CrossRef] [PubMed]
- Teuscher, C.; Subramanian, M.; Noubade, R.; Gao, J.F.; Offner, H.; Zachary, J.F.; Blankenhorn, E.P. Central histamine H3 receptor signaling negatively regulates susceptibility to autoimmune inflammatory disease of the CNS. Proc. Natl. Acad. Sci. 2007, 104, 10146–10151. [Google Scholar] [CrossRef]
- Maydych, V. The Interplay Between Stress, Inflammation, and Emotional Attention: Relevance for Depression. Front. Neurosci. 2019, 13. [Google Scholar] [CrossRef]
- Toyota, H.; Dugovic, C.; Koehl, M.; Laposky, A.D.; Ngo, K.; Wu, Y.; Lee, D.H.; Yanai, K.; Sakurai, E.; Watanabe, T. Behavioral characterization of mice lacking histamine H3 receptors. Mol. Pharmacol. 2002, 62, 389–397. [Google Scholar] [CrossRef]
- Salim, S. Oxidative stress and psychological disorders. Curr. Neuropharmacol. 2014, 12, 140–147. [Google Scholar] [CrossRef]
- Ambade, A.; Mandrekar, P. Oxidative stress and inflammation: Essential partners in alcoholic liver disease. Int. J. Hepatol. 2012, 2012. [Google Scholar] [CrossRef]
- Delattre, J.; Beaudeux, J.-L.; Bonnefont-Rousselot, D. Radicaux libres et stress oxydant(aspects biologiques et pathologiques); Editions Tec & Doc: Paris, France, 2005. [Google Scholar]
- Cardozo-Pelaez, F.; Song, S.; Parthasarathy, A.; Hazzi, C.; Naidu, K.; Sanchez-Ramos, J. Oxidative DNA damage in the aging mouse brain. Mov. Disord. Off. J. Mov. Disord. Soc. 1999, 14, 972–980. [Google Scholar] [CrossRef]
- Rammal, H.; Bouayed, J.; Younos, C.; Soulimani, R. Evidence that oxidative stress is linked to anxiety-related behaviour in mice. Brain. Behav. Immun. 2008, 22, 1156–1159. [Google Scholar] [CrossRef]
- Ridnour, L.A.; Thomas, D.D.; Mancardi, D.; Espey, M.G.; Miranda, K.M.; Paolocci, N.; Feelisch, M.; Fukuto, J.; Wink, D.A. The chemistry of nitrosative stress induced by nitric oxide and reactive nitrogen oxide species. Putting perspective on stressful biological situations. Biol. Chem. 2004, 385, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Bouayed, J.; Bohn, T. Exogenous antioxidants—double-edged swords in cellular redox state: Health beneficial effects at physiologic doses versus deleterious effects at high doses. Oxid. Med. Cell. Longev. 2010, 3, 228–237. [Google Scholar] [CrossRef] [PubMed]
- Kalam Azad, M.O.; Jeong, D.I.; Adnan, M.; Salitxay, T.; Heo, J.W.; Naznin, M.T.; Lim, J.D.; Cho, D.H.; Park, B.J.; Park, C.H. Effect of Different Processing Methods on the Accumulation of the Phenolic Compounds and Antioxidant Profile of Broomcorn Millet (Panicum miliaceum L.) Flour. Foods 2019, 8, 230. [Google Scholar] [CrossRef] [PubMed]
- Adnan, M.; Azad, M.O.K.; Ju, H.S.; Son, J.M.; Park, C.H.; Shin, M.H.; Alle, M.; Cho, D.H. Development of biopolymer-mediated nanocomposites using hot-melt extrusion to enhance the bio-accessibility and antioxidant capacity of kenaf seed flour. Appl. Nanosci. 2019, 1–13. [Google Scholar] [CrossRef]
- Wang, X.; Chen, Y.; Wang, Q.; Sun, L.; Li, G.; Zhang, C.; Huang, J.; Chen, L.; Zhai, H. Support for natural small-molecule phenols as anxiolytics. Molecules 2017, 22, 2138. [Google Scholar] [CrossRef]
- Hritcu, L.; Ionita, R.; Postu, P.A.; Gupta, G.K.; Turkez, H.; Lima, T.C.; Carvalho, C.U.S.; de Sousa, D.P. Antidepressant flavonoids and their relationship with oxidative stress. Oxid. Med. Cell. Longev. 2017, 2017. [Google Scholar] [CrossRef]
- Wagner, H.; Ott, S.; Jurcic, K.; Morton, J.; Neszmelyi, A. Chemistry, 13C-NMR study and pharmacology of two saponins from Colubrina asiatica. Planta Med. 1983, 48, 136–141. [Google Scholar] [CrossRef]
- Awad, R.; Ahmed, F.; Bourbonnais-Spear, N.; Mullally, M.; Ta, C.A.; Tang, A.; Merali, Z.; Maquin, P.; Caal, F.; Cal, V. Ethnopharmacology of Q’eqchi’Maya antiepileptic and anxiolytic plants: Effects on the GABAergic system. J. Ethnopharmacol. 2009, 125, 257–264. [Google Scholar] [CrossRef]
- Smilin, G.B.A.; Abbirami, E.; Sivasudha, T.; Ruckmani, K. Passiflora caerulea L. fruit extract and its metabolites ameliorate epileptic seizure, cognitive deficit and oxidative stress in pilocarpine-induced epileptic mice. Metab. Brain Dis. 2019. [Google Scholar]
- Liu, L.; Cui, Z.-X.; Yang, X.-W.; Xu, W.; Zhang, Y.-B.; Li, F.-J.; Gong, Y.; Liu, N.-F.; Peng, K.-F.; Zhang, P. Simultaneous characterisation of multiple Mahonia fortunei bioactive compounds in rat plasma by UPLC–MS/MS for application in pharmacokinetic studies and anti-inflammatory activity in vitro. J. Pharm. Biomed. Anal. 2019, 113013. [Google Scholar] [CrossRef]
- Ramamurthy, V.; Devi, K.D. PHYTOCHEMICAL PROFILING OF ETHANOLIC LEAVES EXTRACT OF BRASSICA OLERACEA CAPITATA DC. Eur. J. Biomed. 2017, 4, 297–302. [Google Scholar]
- Sabithira, G.; Udayakumar, R. GC-MS analysis of methanolic extracts of leaf and stem of Marsilea minuta (Linn.). J. Complement. Altern. Med. Res. 2017, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Zeb, M.; Khan, S.; Rahman, T.; Sajid, M.; Seloni, S. Isolation and Biological Activity of β-Sitosterol and Stigmasterol from the Roots of Indigofera heterantha. Pharm. Pharmacol. Int. J. 2017, 5, 139. [Google Scholar]
- Bin Sayeed, M.; Karim, S.; Sharmin, T.; Morshed, M. Critical analysis on characterization, systemic effect, and therapeutic potential of beta-sitosterol: A plant-derived orphan phytosterol. Medicines 2016, 3, 29. [Google Scholar] [CrossRef] [PubMed]
- Enema, O.J.; Adesina, S.K.; Umoh, U.F.; Eseyin, O.A. Gas chromatography-mass spectroscopy (GC-MS) studies of fixed oil of leaf of Tetrapleura tetraptera Taub.(Mimosaceae). J. Pharmacogn. Phytochem. 2019, 8, 1237–1241. [Google Scholar]
- Behl Vitamin E and other antioxidants in neuroprotection. Int. J. Vitam. Nutr. Res. 1999, 69, 213–219. [CrossRef] [PubMed]
- Muller, D.P.R. Vitamin E and neurological function. Mol. Nutr. Food Res. 2010, 54, 710–718. [Google Scholar] [CrossRef]
- Godara, P.; Dulara, B.K.; Barwer, N.; Chaudhary, N.S. Comparative GC-MS Analysis of Bioactive Phytochemicals from Different Plant Parts and Callus of Leptadenia reticulata Wight and Arn. Pharmacogn. J. 2019, 11. [Google Scholar] [CrossRef]
- Um, M.Y.; Kim, S.; Jin, Y.; Yoon, M.; Yang, H.; Lee, J.; Jung, J.; Urade, Y.; Huang, Z.; Kwon, S. A novel neurological function of rice bran: A standardized rice bran supplement promotes non-rapid eye movement sleep in mice through histamine H1 receptors. Mol. Nutr. Food Res. 2017, 61, 1700316. [Google Scholar] [CrossRef]
- Sun, J.; Li, X.; Liu, J.; Pan, X.; Zhao, Q. Stigmasterol Exerts Neuro-Protective Effect Against Ischemic/Reperfusion Injury Through Reduction Of Oxidative Stress And Inactivation Of Autophagy. Neuropsychiatr. Dis. Treat. 2019, 15, 2991. [Google Scholar] [CrossRef]
- Zhang, J.X.; Yue, W.B.; Ren, Y.S.; Zhang, C.X. Enhanced role of elaidic acid on acrylamide-induced oxidative stress in epididymis and epididymal sperm that contributed to the impairment of spermatogenesis in mice. Toxicol. Ind. Health 2010, 26, 469–477. [Google Scholar] [CrossRef] [PubMed]
- Shahinozzaman, M.; Taira, N.; Ishii, T.; Halim, M.; Hossain, M.; Tawata, S. Anti-Inflammatory, Anti-Diabetic, and Anti-Alzheimer’s Effects of Prenylated Flavonoids from Okinawa Propolis: An Investigation by Experimental and Computational Studies. Molecules 2018, 23, 2479. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.; Chuaqui, C.E.; Boriack-Sjodin, P.A.; Lee, W.-C.; Pontz, T.; Corbley, M.J.; Cheung, H.-K.; Arduini, R.M.; Mead, J.N.; Newman, M.N. Successful shape-based virtual screening: The discovery of a potent inhibitor of the type I TGFβ receptor kinase (TβRI). Bioorg. Med. Chem. Lett. 2003, 13, 4355–4359. [Google Scholar] [CrossRef] [PubMed]
- Veber, D.F.; Johnson, S.R.; Cheng, H.-Y.; Smith, B.R.; Ward, K.W.; Kopple, K.D. Molecular properties that influence the oral bioavailability of drug candidates. J. Med. Chem. 2002, 45, 2615–2623. [Google Scholar] [CrossRef]
- Lipinski, C.A.; Lombardo, F.; Dominy, B.W.; Feeney, P.J. Experimental and computational approaches to estimate solubility and permeability in drug discovery and development settings. Adv. Drug Deliv. Rev. 1997, 23, 3–25. [Google Scholar] [CrossRef]

| Treatment (mg/kg) | Paw Volume (mm) (% Inhibition) | |||
|---|---|---|---|---|
| 1 h | 2 h | 3 h | 4 h | |
| Control | 0.454 ± 0.010 | 0.392 ± 0.012 | 0.340 ± 0.007 | 0.312 ± 0.008 |
| RSD 10 | 0.350 ± 0.004 *** | 0.290 ± 0.007 *** | 0.264 ± 0.010 *** | 0.248 ± 0.012 *** |
| (42.42) | (60.29) | (66.66) | (78.57) | |
| MEHC 200 | 0.398 ± 0.006 *** | 0.340 ± 0.010 ** | 0.298 ± 0.006 * | 0.288 ± 0.005 |
| (29.29) | (39.70) | (52.38) | (46.42) | |
| MEHC 400 | 0.342 ± 0.005 *** | 0.296 ± 0.005 *** | 0.264 ± 0.010 *** | 0.250 ± 0.010 *** |
| (43.43) | (51.47) | (59.52) | (64.28) | |
| Tested Sample | Phenolic Content (mg GAE/g Dried Extract) | Flavonoid Content (mg QE/g Dried Extract) | Flavonol Content (mg QE/g Dried Extract) | Condensed Tannins Content (mg CAE/g Dried Extract) | Total Antioxidant Capacity (mg AA/g Dried Extract) |
|---|---|---|---|---|---|
| MEHC | 34.76 ± 1.09 | 48.30 ± 1.62 | 38.28 ± 0.04 | 112.91 ± 0.25 | 307.60 ± 0.36 |
| Compounds | Docking Score (kcal/mol) | Glide e Model (kcal/mol) | Glide Energy (kcal/mol) |
|---|---|---|---|
| β-D-Glucopyranoside, methyl | −3.78 | −20.33 | −18.76 |
| Neophytadiene | - | - | - |
| 2-Pentadecanone, 6,10,14-trimethyl | +0.904 | −1.97 | −3.30 |
| Hexadecanoic acid, methyl ester | +3.184 | −5.15 | −10.22 |
| n-Hexadecanoic acid | +2.966 | −13.37 | −17.45 |
| α-Tocospiro A | −1.086 | −19.61 | −20.37 |
| β-Sitosterol acetate | −1.827 | −19.12 | −18.85 |
| Vitamin E | −1.13 | −18.08 | −18.13 |
| Campesterol | - | - | - |
| Stigmasterol | - | - | - |
| Elaidic acid | +2.847 | −12.307 | −16.48 |
| Compounds | Docking Score (kcal/mol) | Glide e Model (kcal/mol) | Glide Energy (kcal/mol) |
|---|---|---|---|
| β-D-Glucopyranoside, methyl | - | - | - |
| Neophytadiene | - | - | - |
| 2-Pentadecanone, 6,10,14-trimethyl | +0.009 | −19.07 | −19.22 |
| Hexadecanoic acid, methyl ester | +2.082 | −14.88 | −17.09 |
| n-Hexadecanoic acid | +2.077 | −14.61 | −17.99 |
| α-Tocospiro A | −2.176 | −13.95 | −14.51 |
| β-Sitosterol acetate | −1.908 | −16.89 | −17.01 |
| Vitamin E | −1.44 | −17.46 | −16.76 |
| Campesterol | −3.199 | −17.20 | −16.38 |
| Stigmasterol | −1.589 | −8.98 | −8.79 |
| Elaidic acid | +2.894 | −7.66 | −11.696 |
| Compounds | COX-1 (PDB: 2OYE) | COX-2 (PDB: 3HS5) | ||||
|---|---|---|---|---|---|---|
| Docking Score (kcal/mol) | Glide e Model (kcal/mol) | Glide Energy (kcal/mol) | Docking Score (kcal/mol) | Glide e Model (kcal/mol) | Glide Energy (kcal/mol) | |
| β-D-Glucopyranoside, methyl | −4.114 | −20.449 | −19.099 | −5.34 | −27.901 | −24.576 |
| Neophytadiene | +1.476 | −11.109 | −13.076 | - | - | - |
| 2-Pentadecanone, 6,10,14-trimethyl | +1.255 | −11.866 | −12.886 | - | - | - |
| Hexadecanoic acid, methyl ester | +3.12 | −9.837 | −12.248 | - | - | - |
| n-Hexadecanoic acid | +3.34 | −9.918 | −12.866 | - | - | - |
| α-Tocospiro A | −1.298 | −12.789 | −12.481 | - | - | - |
| β-Sitosterol acetate | −3.178 | −19.020 | −18.138 | - | - | - |
| Vitamin E | −1.433 | −11.413 | −10.205 | - | - | - |
| Campesterol | −1.488 | −12.445 | −12.152 | - | - | - |
| Stigmasterol | −2.556 | −16.728 | −15.921 | - | - | - |
| Elaidic acid | +2.171 | −12.586 | −15.874 | +0.842 | −0.529 | −2.204 |
| Compounds | Docking Score (kcal/mol) | Glide e Model (kcal/mol) | Glide Energy (kcal/mol) |
|---|---|---|---|
| β-D-Glucopyranoside, methyl | −4.814 | −32.01 | −24.61 |
| Neophytadiene | +2.376 | −10.10 | −12.78 |
| 2-Pentadecanone, 6,10,14-trimethyl | +0.965 | −13.3 | −14.89 |
| Hexadecanoic acid, methyl ester | +3.362 | −9.51 | −13.84 |
| n-Hexadecanoic acid | +2.812 | −16.01 | −20.80 |
| α-Tocospiro A | −2.584 | −31.58 | −28.27 |
| β-Sitosterol acetate | −1.482 | −19.16 | −18.37 |
| Vitamin E | −1.544 | −22.84 | −22.42 |
| Campesterol | −2.968 | −21.60 | −20.87 |
| Stigmasterol | −3.576 | −22.08 | −21.61 |
| Elaidic acid | +1.704 | −18.825 | −22.223 |
| Compound | Lipinski Rules | Lipinski’s Violations | Veber Rules | ||||
|---|---|---|---|---|---|---|---|
| MW | HBA | HBD | Log P | nRB | TPSA | ||
| < 500 | < 10 | < 5 | ≤ 5 | ≤ 1 | ≤ 10 | ≤ 140 | |
| β-D Glucopyranoside, methyl | 194.18 | 6 | 4 | −1.64 | 0 | 2 | 99.38 |
| α-Tocospiro A | 462.70 | 4 | 1 | 6.37 | 1 | 13 | 63.60 |
| β-Sitosterol acetate | 456.74 | 2 | 0 | 7.63 | 1 | 8 | 26.30 |
| Campesterol | 400.68 | 1 | 1 | 6.90 | 1 | 5 | 20.23 |
| Stigmasterol | 412.69 | 1 | 1 | 6.96 | 1 | 5 | 20.23 |
| Vitamin E | 430.71 | 2 | 1 | 8.27 | 1 | 12 | 29.46 |
| Parameters | Compounds | |||||
|---|---|---|---|---|---|---|
| β-D Glucopyranoside, Methyl | α-Tocospiro A | β-Sitosterol Acetate | Campesterol | Stigmasterol | Vitamin E | |
| Ames toxicity | NAT | NAT | NAT | NAT | NAT | NAT |
| Carcinogens | NC | NC | NC | NC | NC | NC |
| Acute oral toxicity | III | III | III | I | I | III |
| Rat Acute Toxicity | 1.1350 | 2.7917 | 2.0248 | 2.8078 | 2.6561 | 2.1598 |
| Compound Name | Biological Properties Predicted by PASS Online | Pa | Pi |
|---|---|---|---|
| β-D Glucopyranoside, methyl | GABA aminotransferase inhibitor | 0.908 | 0.002 |
| Histamine release inhibitor | 0.817 | 0.002 | |
| Free radical scavenger | 0.674 | 0.004 | |
| Lipid peroxidase inhibitor | 0.669 | 0.006 | |
| Antioxidant | 0.667 | 0.004 | |
| α-Tocospiro A | Anti-inflammatory | 0.896 | 0.004 |
| peroxidase inhibitor | 0.734 | 0.009 | |
| Antioxidant | 0.640 | 0.004 | |
| Free radical scavenger | 0.444 | 0.014 | |
| Apoptosis agonist | 0.403 | 0.072 | |
| β-Sitosterol acetate | Prostaglandin-E2 9-reductase inhibitor | 0.946 | 0.003 |
| Oxidoreductase inhibitor | 0.886 | 0.003 | |
| Peroxidase substrate | 0.632 | 0.004 | |
| Anti-inflammatory | 0.575 | 0.037 | |
| TNF expression inhibitor | 0.356 | 0.072 | |
| Campesterol | Wound healing agent | 0.501 | 0.011 |
| Anti-parkinsonian, rigidity relieving | 0.450 | 0.012 | |
| Dementia treatment | 0.745 | 0.031 | |
| Nitric oxide scavenger | 0.353 | 0.004 | |
| Immunomodulator | 0.341 | 0.050 | |
| Stigmasterol | Oxidoreductase inhibitor | 0.933 | 0.001 |
| Antitoxic | 0.755 | 0.004 | |
| Anti-inflammatory | 0.541 | 0.045 | |
| Lipid metabolism regulator | 0.450 | 0.068 | |
| Immunostimulant | 0.360 | 0.061 | |
| Vitamin E | Lipid peroxidase inhibitor | 0.978 | 0.002 |
| Antioxidant | 0.967 | 0.002 | |
| Acute neurologic disorders treatment | 0.935 | 0.004 | |
| Reductant | 0.924 | 0.006 | |
| Anti-inflammatory | 0.830 | 0.005 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adnan, M.; Chy, M.N.U.; Kamal, A.T.M.M.; Chowdhury, K.A.A.; Rahman, M.A.; Reza, A.S.M.A.; Moniruzzaman, M.; Rony, S.R.; Nasrin, M.S.; Azad, M.O.K.; et al. Intervention in Neuropsychiatric Disorders by Suppressing Inflammatory and Oxidative Stress Signal and Exploration of In Silico Studies for Potential Lead Compounds from Holigarna caustica (Dennst.) Oken leaves. Biomolecules 2020, 10, 561. https://doi.org/10.3390/biom10040561
Adnan M, Chy MNU, Kamal ATMM, Chowdhury KAA, Rahman MA, Reza ASMA, Moniruzzaman M, Rony SR, Nasrin MS, Azad MOK, et al. Intervention in Neuropsychiatric Disorders by Suppressing Inflammatory and Oxidative Stress Signal and Exploration of In Silico Studies for Potential Lead Compounds from Holigarna caustica (Dennst.) Oken leaves. Biomolecules. 2020; 10(4):561. https://doi.org/10.3390/biom10040561
Chicago/Turabian StyleAdnan, Md., Md. Nazim Uddin Chy, A.T.M. Mostafa Kamal, Kazi Asfak Ahmed Chowdhury, Md. Atiar Rahman, A. S. M. Ali Reza, Md. Moniruzzaman, Satyajit Roy Rony, Mst. Samima Nasrin, Md. Obyedul Kalam Azad, and et al. 2020. "Intervention in Neuropsychiatric Disorders by Suppressing Inflammatory and Oxidative Stress Signal and Exploration of In Silico Studies for Potential Lead Compounds from Holigarna caustica (Dennst.) Oken leaves" Biomolecules 10, no. 4: 561. https://doi.org/10.3390/biom10040561
APA StyleAdnan, M., Chy, M. N. U., Kamal, A. T. M. M., Chowdhury, K. A. A., Rahman, M. A., Reza, A. S. M. A., Moniruzzaman, M., Rony, S. R., Nasrin, M. S., Azad, M. O. K., Park, C. H., Lim, Y. S., & Cho, D. H. (2020). Intervention in Neuropsychiatric Disorders by Suppressing Inflammatory and Oxidative Stress Signal and Exploration of In Silico Studies for Potential Lead Compounds from Holigarna caustica (Dennst.) Oken leaves. Biomolecules, 10(4), 561. https://doi.org/10.3390/biom10040561










