Measurement of Oxidative Stress Index in 102 Patients with Peyronie’s Disease
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Purpose of This Study
- •
- The assessment of the OS index in PD patients and in the subjects of the control group;
- •
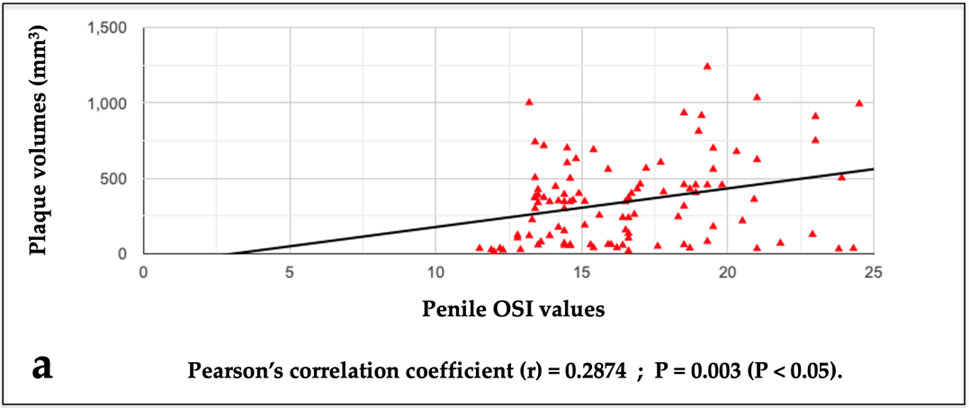
- The investigation of a potential relationship between the penile OSI values and the penile plaque volumes;
- •
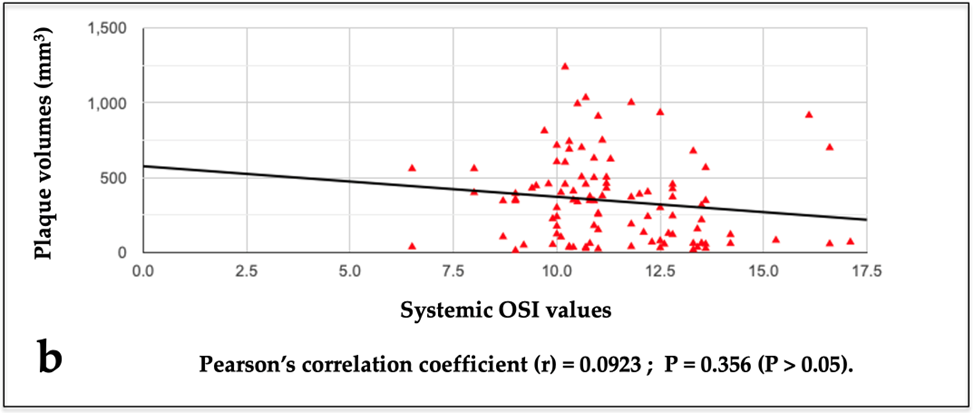
- The investigation of a potential relationship between systemic OSI values (obtained from blood samples from a peripheral vein) and plaque volumes;
- •
- The investigation of a potential relationship between systemic OSI values and penile OSI values;
- •
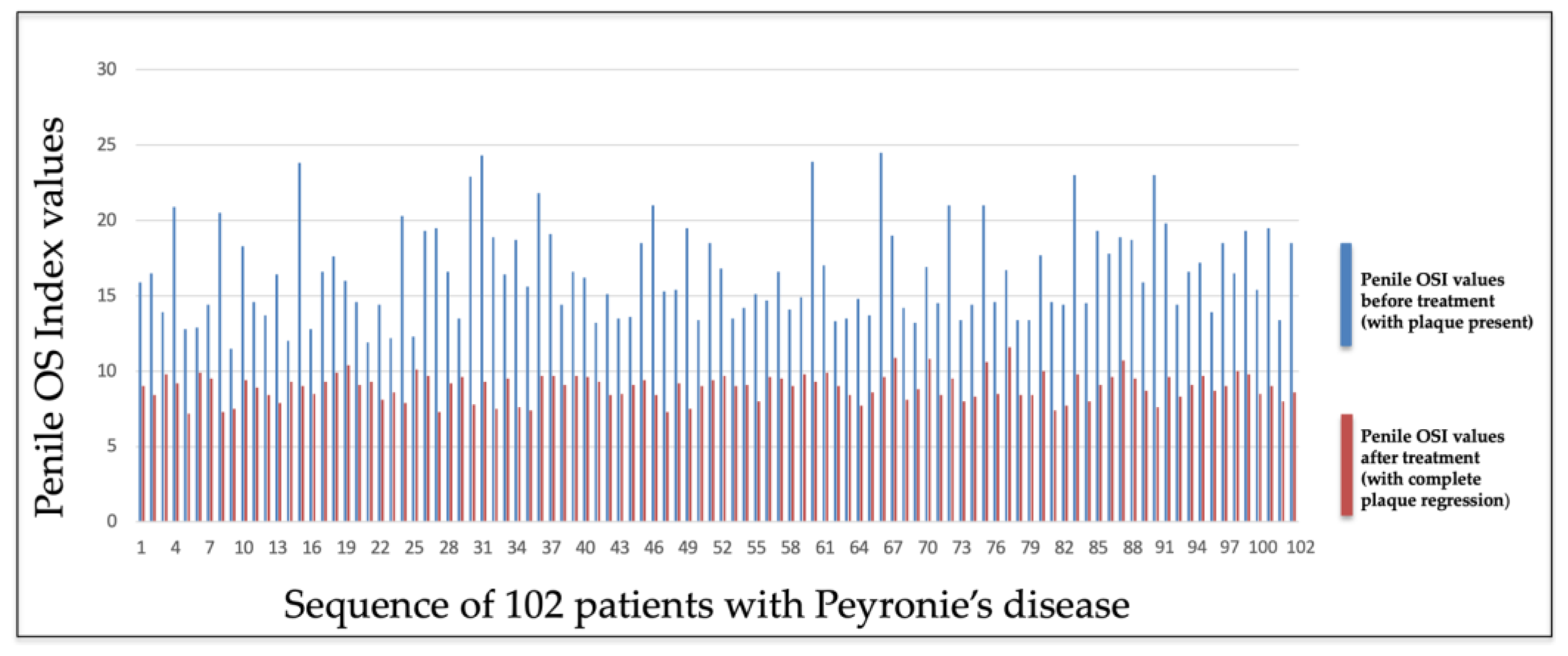
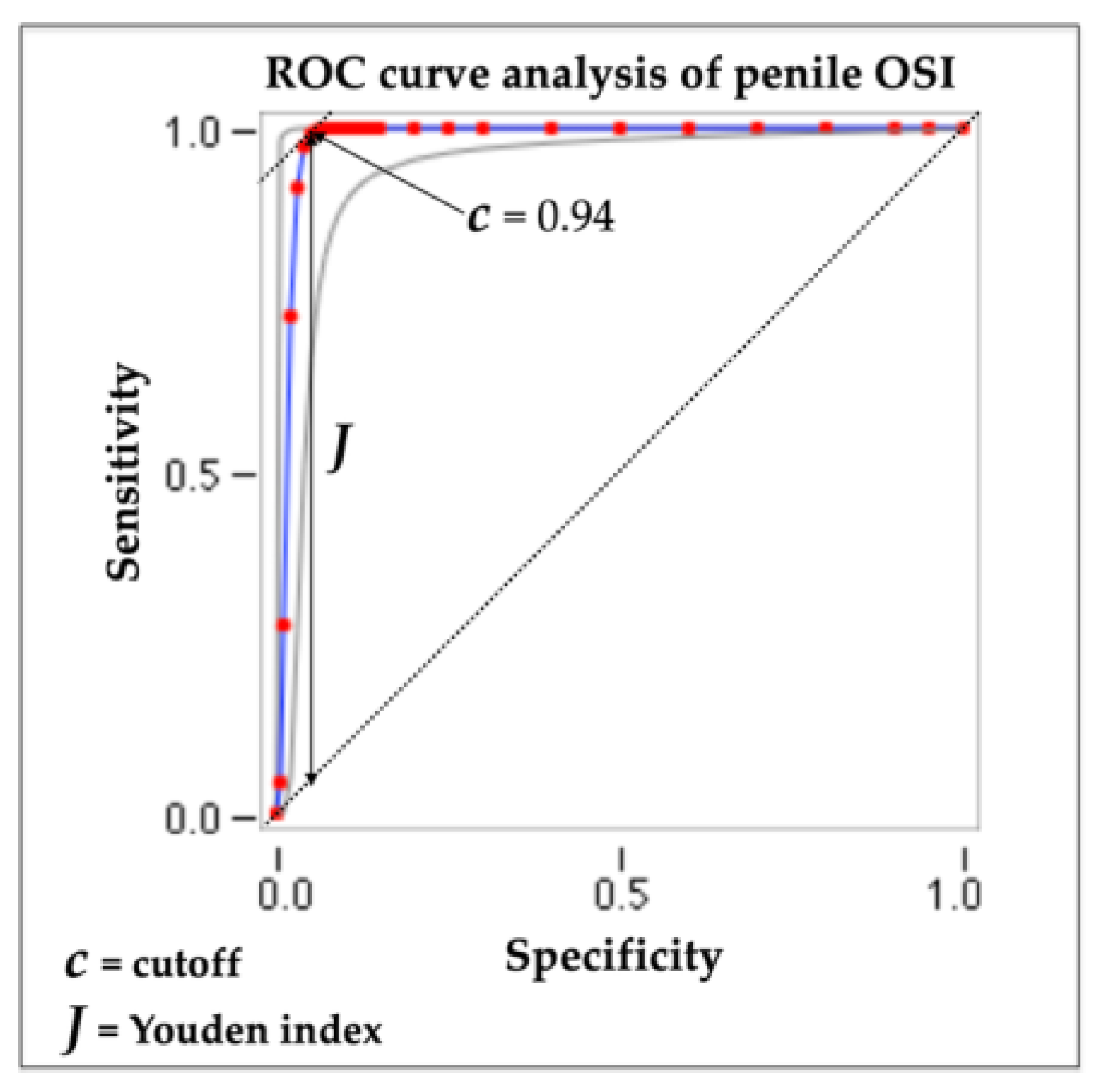
- The identification of normal penile OSI values indicative of disease area regression (PD plaque);
- •
- The investigation of a potential correlation between penile OSI values and chronic pathological conditions;
- •
- The investigation of a potential correlation between systemic OSI values and chronic pathological conditions in progress;
- •
- The investigation of a potential correlation between penile OSI values and an anxious–depressive state;
- •
- The investigation of a potential correlation between systemic OSI values and an anxious–depressive state.
2.2.1. Inclusion and Exclusion Criteria
2.2.2. Data Collection
2.2.3. Sample Collection
2.2.4. Plasma Collection
2.2.5. d-ROMs and PAT Measurements
2.2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stuntz, M.; Perlaky, A.; des Vignes, F.; Kyriakides, T.; Glass, D. The prevalence of Peyronie’s disease in the United States: A population-based study. PLoS ONE 2016, 11, e0150157. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, U.; Sommer, F.; Klotz, T.; Braun, M.; Reifenrath, B.; Engelmann, U. The prevalence of Peyronie’s disease: Results of a large survey. BJU Int. 2001, 88, 727–730. [Google Scholar] [CrossRef] [PubMed]
- DiBenedetti, D.B.; Nguyen, D.; Zografos, L.; Ziemiecki, R.; Zhou, X. A Population-based study of peyronie’s disease: Prevalence and treatment patterns in the United States. Adv. Urol. 2011, 2011, 282503. [Google Scholar] [CrossRef] [PubMed]
- La Pera, G.; Pescatori, E.S.; Calabrese, M.; Boffini, A.; Colombo, F.; Andriani, E.; Natali, A.; Vaggi, L.; Catuogno, C.; Giustini, M.; et al. Peyronie’s disease: Prevalence and association with cigarette smoking. A multicenter population-based study in men aged 50–69 years. Eur. Urol. 2001, 40, 525–530. [Google Scholar] [CrossRef] [PubMed]
- Bias, W.B.; Nyberg, L.M., Jr.; Hochberg, M.C.; Walsh, P.C.; Opitz, J.M. Peyronie’s disease: A newly recognized autosomal-dominant trait. Am. J. Med. Genet. 1982, 12, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Herati, A.S.; Pastuszak, A.W. The Genetic Basis of Peyronie’s Disease: A Review. Sex Med. Rev. 2016, 4, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Weidner, W.; Schroeder-Printzen, I.; Weiske, W.-H.; Vosshenrich, R. Sexual dysfunction in Peyronie’s disease: An analysis of 222 patients without previous local plaque therapy. J. Urol. 1997, 157, 325–328. [Google Scholar] [CrossRef] [PubMed]
- Hellstrom, W.J.; Bivalacqua, T.J. Peyronie’s disease: Etiology, medical, and surgical therapy. J. Androl. 2000, 21, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Pryor, J.P.; Ralph, D.J. Clinical presentations of Peyronie’s disease. Int. J. Impot. Res. 2002, 14, 414–417. [Google Scholar] [CrossRef] [PubMed]
- Nelson, C.J.; Diblasio, C.; Kendirci, M.; Hellstrom, W.; Guhring, P.; Mulhall, J.P. The chronology of depression and distress in men with Peyronie’s disease. J. Sex. Med. 2008, 5, 1985–1990. [Google Scholar] [CrossRef] [PubMed]
- Devine, C.J., Jr.; Somers, K.D.; Ladaga, L.E. Peyronie’s disease: Pathophysiology. Prog. Clin. Biol. Res. 1991, 370, 355–358. [Google Scholar] [PubMed]
- Jarow, J.P.; Lowe, F.C. Penile trauma: An etiologic factor in Peyronie’s disease and erectile dysfunction. J. Urol. 1997, 158, 1388–1390. [Google Scholar] [CrossRef] [PubMed]
- Somers, K.D.; Dawson, D.M. Fibrin deposition in Peyronie’s disease plaque. J. Urol. 1997, 157, 311–315. [Google Scholar] [CrossRef] [PubMed]
- Devine, C.J., Jr.; Somers, K.D.; Jordan, G.H.; Schlossberg, S.M. Proposal: Trauma as a cause of Peyronie’s lesion. J. Urol. 1997, 157, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Bilgutay, A.N.; Pastuszak, A.W. Peyronie’s disease: What’s around the bend? Indian J. Urol. 2016, 32, 6–14. [Google Scholar] [PubMed]
- Moreland, R.B.; Nehra, A. Pathophysiology of Peyronie’s disease. Int. J. Impot. Res. 2002, 14, 406–410. [Google Scholar] [CrossRef] [PubMed]
- Paulis, G.; Brancato, T. Inflammatory mechanisms and oxidative stress in Peyronie’s disease: Therapeutic “rationale” and related emerging treatment strategies. Inflamm. Allergy Drug Targets 2012, 11, 48–57. [Google Scholar] [CrossRef] [PubMed]
- El-Sakka, A.I.; Salabas, E.; Dinçer, M.; Kadioglu, A. The pathophysiology of Peyronie’s disease. Arab. J. Urol. 2013, 11, 272–277. [Google Scholar] [CrossRef] [PubMed]
- Paulis, G.; Romano, G.; Paulis, L.; Barletta, D. Recent Pathophysiological Aspects of Peyronie’s Disease: Role of Free Radicals, Rationale, and Therapeutic Implications for Antioxidant Treatment-Literature Review. Adv. Urol. 2017, 2017, 4653512. [Google Scholar] [CrossRef] [PubMed]
- Bivalacqua, T.J.; Champion, H.C.; Hellstrom, W.J. Implications of nitric oxide synthase isoforms in the pathophysiology of Peyronie’s disease. Int. J. Impot. Res. 2002, 14, 345–352. [Google Scholar] [CrossRef] [PubMed]
- Sikka, S.C.; Hellstrom, W.J. Role of oxidative stress and antioxidants in Peyronie’s disease. Int. J. Impot. Res. 2002, 14, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Cadavid, N.F.; Magee, T.R.; Ferrini, M.; Qian, A.; Vernet, D.; Rajfer, J. Gene expression in Peyronie’s disease. Int. J. Impot. Res. 2002, 14, 361–374. [Google Scholar] [CrossRef] [PubMed]
- Davila, H.H.; Magee, T.R.; Vernet, D.; Rajfer, J.; Gonzalez-Cadavid, N.F. Gene transfer of inducible nitric oxide synthase complementary DNA regresses the fibrotic plaque in an animal model of Peyronie’s disease. Biol. Reprod. 2004, 71, 1568–1577. [Google Scholar] [CrossRef] [PubMed]
- Paulis, G.; De Giorgio, G.; Paulis, L. Role of Oxidative Stress in Peyronie’s Disease: Biochemical Evidence and Experiences of Treatment with Antioxidants. Int. J. Mol. Sci. 2022, 23, 15969. [Google Scholar] [CrossRef] [PubMed]
- Levine, L.; Rybak, J.; Corder, C.; Farrel, M.R. Peyronie’s disease plaque calcification--prevalence, time to identification, and development of a new grading classification. J. Sex. Med. 2013, 10, 3121–3128. [Google Scholar] [CrossRef] [PubMed]
- Paulis, G.; Paulis, A. Calcification in Peyronie’s disease: Its role and clinical influence on the various symptoms and signs of the disease, including psychological impact. Our study of 551 patients. Arch. Ital. Urol. Androl. 2023, 95, 11549. [Google Scholar] [CrossRef] [PubMed]
- Mulhall, J.P.; Schiff, J.; Guhring, P. An analysis of the natural history of Peyronie’s disease. J. Urol. 2006, 175, 2115–2118. [Google Scholar] [CrossRef] [PubMed]
- Garaffa, G.; Trost, L.W.; Serefoglu, E.C.; Ralph, D.; Hellstrom, W.J.G. Understanding the course of Peyronie’s disease. Int. J. Clin. Pract. 2013, 67, 781–788. [Google Scholar] [CrossRef] [PubMed]
- Paulis, G.; Cavallini, G. Clinical evaluation of natural history of Peyronie’s disease: Our experience, old myths and new certainties. Inflamm. Allergy Drug Targets 2013, 12, 341–348. [Google Scholar] [CrossRef] [PubMed]
- Jalkut, M.; Gonzalez-Cadavid, N.; Rajfer, J. Peyronie’s disease: A review. Rev. Urol. 2003, 5, 142–148. [Google Scholar] [PubMed]
- Levine, L.A.; Larsen, S. Wein, A.J., Kavoussi, L.R., Partin, A.W., Peters, C.A., Eds.; Diagnosis and management of Peyronie disease. In Campbell-Walsh Urology, 11th ed.; Elsevier Saunders: Philadelphia, PA, USA, 2015; pp. 722–748. [Google Scholar]
- Brimley, S.C.; Yafi, F.A.; Greenberg, J.; Hellstrom, W.J.; Nguyen, H.M.T.; Hatzichristodoulou, G. Review of management options for active-phase Peyronie’s disease. Sex. Med. Rev. 2019, 7, 329–337. [Google Scholar] [CrossRef] [PubMed]
- Capoccia, E.; Levine, L.A. Contemporary review of Peyronie’s disease treatment. Curr. Urol. Rep. 2018, 19, 51. [Google Scholar] [CrossRef] [PubMed]
- Gur, S.; Limin, M.; Hellstrom, W.J. Current status and new developments in Peyronie’s disease: Medical, minimally invasive and surgical treatment options. Expert Opin. Pharmacother. 2011, 12, 931–944. [Google Scholar] [CrossRef] [PubMed]
- Tsambarlis, P.; Levine, L.A. Nonsurgical management of Peyronie’s disease. Nat. Rev. Urol. 2019, 16, 172–186. [Google Scholar] [CrossRef] [PubMed]
- Tan, R.B.W.; Sangkum, P.; Mitchell, G.C.; Hellstrom, W.J.G. Update on medical management of Peyronie’s disease. Curr. Urol. Rep. 2014, 15, 415. [Google Scholar] [CrossRef] [PubMed]
- Paulis, G.; Brancato, T.; D’ascenzo, R.; De Giorgio, G.; Nupieri, P.; Orsolini, G.; Alvaro, R. Efficacy of vitamin E in the conservative treatment of Peyronie’s disease: Legend or reality? A controlled study of 70 cases. Andrology 2013, 1, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Paulis, G.; Cavallini, G.; De Giorgio, G.; Quattrocchi, S.; Brancato, T.; Alvaro, R. Long-term multimodal therapy (verapamil associated with propolis, blueberry, vitamin E and local diclofenac) on patients with Peyronie’s disease (chronic inflammation of the tunica albuginea). Results of a controlled study. Inflamm. Allergy Drug Targets 2013, 12, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Paulis, G.; Barletta, D.; Turchi, P.; Vitarelli, A.; Dachille, G.; Fabiani, A.; Gennaro, R. Efficacy and safety evaluation of pentoxifylline associated with other antioxidants in medical treatment of Peyronie’s disease: A case-control study. Res. Rep. Urol. 2016, 8, 1–10. [Google Scholar] [PubMed]
- Gennaro, R.; Barletta, D.; Paulis, G. Intralesional hyaluronic acid: An innovative treatment for Peyronie’s disease. Int. Urol. Nephrol. 2015, 47, 1595–1602. [Google Scholar] [CrossRef] [PubMed]
- Zucchi, A.; Costantini, E.; Cai, T.; Cavallini, G.; Liguori, G.; Favilla, V.; De Grande, G.; D’Achille, G.; Silvani, M.; Franco, G.; et al. Intralesional Injection of Hyaluronic Acid in Patients Affected with Peyronie’s Disease: Preliminary Results from a Prospective, Multicenter, Pilot Study. Sex. Med. 2016, 4, e85–e90. [Google Scholar] [CrossRef] [PubMed]
- Kendirci, M.; Hellstrom, W.J. Critical analysis of surgery for Peyronie’s disease. Curr. Opin. Urol. 2004, 6, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Levine, L.A.; Burnett, A.L. Standard operating procedures for Peyronie’s disease. J. Sex. Med. 2013, 10, 230–244. [Google Scholar] [CrossRef] [PubMed]
- Kadioglu, A.; Akman, T.; Sanli, O.; Gurkan, L.; Cakan, M.; Celtik, M. Surgical treatment of Peyronie’s disease: A critical analysis. Eur. Urol. 2006, 50, 235–248. [Google Scholar] [CrossRef] [PubMed]
- Rice, P.G.; Somani, B.K.; Rees, R.W. Twenty Years of Plaque Incision and Grafting for Peyronie’s Disease: A Review of Literature. Sex. Med. 2019, 7, 115–128. [Google Scholar] [CrossRef] [PubMed]
- Ralph, D.; Gonzalez-Cadavid, N.; Mirone, V.; Perovic, S.; Sohn, M.; Usta, M.; Levine, L. The management of Peyronie’s disease: Evidence-based 2010 guidelines. J. Sex. Med. 2010, 7, 2359–2374. [Google Scholar] [CrossRef] [PubMed]
- Hatzimouratidis, K.; Eardley, I.; Giuliano, F.; Hatzichristou, D.; Moncada, I.; Salonia, A.; Vardi, Y.; Wespes, E. EAU guidelines on penile curvature. Eur. Urol. 2012, 62, 543–552. [Google Scholar] [CrossRef] [PubMed]
- Nehra, A.; Alterowitz, R.; Culkin, D.J.; Faraday, M.M.; Hakim, L.S.; Heidelbaugh, J.J.; Khera, M.; Kirkby, E.; McVary, K.T.; Miner, M.M.; et al. Peyronie’s disease: AUA guideline. J. Urol. 2015, 194, 745–753. [Google Scholar] [CrossRef] [PubMed]
- Bella, A.J.; Lee, J.C.; Grober, E.D.; Carrier, S.; Benard, F.; Brock, G.B. Canadian Urological Association guideline for Peyronie’s disease and congenital penile curvature. Can. Urol. Assoc. J. 2018, 12, E197–E209. [Google Scholar] [CrossRef] [PubMed]
- Yesilirmak, N.; Bukan, N.; Kurt, B.; Yuzbasioglu, S.; Zhao, M.; Rodrigues-Braz, D.; Aktas, A.; Behar-Cohen, F.; Bourges, J.-L. Evaluation of Ocular and Systemic Oxidative Stress Markers in Ocular Rosacea Patients. Investig. Opthalmol. Vis. Sci. 2023, 64, 22. [Google Scholar] [CrossRef] [PubMed]
- Dinç, G.; Fentoğlu, Ö.; Doğru, A.; İlhan, I.; Kırzıoğlu, F.Y.; Orhan, H. The evaluation of salivary oxidative stress in patients with familial Mediterranean fever and chronic periodontitis. J. Periodontol. 2018, 89, 1112–1120. [Google Scholar] [CrossRef] [PubMed]
- García-González, A.; Gaxiola-Robles, R.; Zenteno-Savín, T. Oxidative stress in patients with rheumatoid arthritis. Rev. Investig. Clin. 2015, 67, 46–53. [Google Scholar] [CrossRef]
- Singh, S.; Verma, S.K.; Kumar, S.; Ahmad, M.K.; Nischal, A.; Singh, S.K.; Dixit, R.K. Evaluation of Oxidative Stress and Antioxidant Status in Chronic Obstructive Pulmonary Disease. Scand. J. Immunol. 2017, 85, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Paulis, G.; Paulis, A.; De Giorgio, G.; Quattrocchi, S. Measurement of Oxidative Stress Index (OSI) in Penile Corpora Cavernosa and Peripheral Blood of Peyronie’s Disease Patients: A Report of 49 Cases. Metabolites 2024, 14, 55. [Google Scholar] [CrossRef] [PubMed]
- Serena, B.; Primiterra, M.; Catalani, S.; Finco, A.; Canestrari, F.; Cornelli, U. Performance evaluation of the innovative PAT test, comparison with the common BAP test and influence of interferences on the evaluation of the plasma antioxidant capacity. Clin. Lab. 2013, 59, 1091–1097. [Google Scholar] [PubMed]
- Valtuille, R.A.; Rossi, G.; Gimenez, E. Protective Effect of Autologous Arteriovenous Fistulae Against Oxidative Stress in Hemodialyzed Patients. Cureus 2021, 13, e15398. [Google Scholar] [CrossRef] [PubMed]
- Harma, M.; Harma, M.; Erel, O. Increased oxidative stress in patients with hydatidiform mole. Swiss. Med. Wkly. 2003, 133, 563–566. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, S.; Ozgu-Erdinc, A.S.; Demirtas, C.; Ozturk, G.; Erkaya, S.; Uygur, D. The oxidative stress index increases among patients with hyperemesis gravidarum but not in normal pregnancies. Redox Rep. 2015, 20, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Rodríguez, M.A.; Mendoza-Núñez, V.M. Oxidative Stress Indexes for Diagnosis of Health or Disease in Humans. Oxidative Med. Cell. Longev. 2019, 2019, 4128152. [Google Scholar] [CrossRef] [PubMed]
- The FRAS System. 2023. Available online: https://hedsrl.it/en/fras-5/ (accessed on 31 May 2025).
- Coaccioli, S.; Panaccione, A.; Biondi, R.; Sabatini, C.; Landucci, P.; Del Giorno, R.; Fantera, M.; Mondo, A.M.; Di Cato, L.; Paladini, A.; et al. Evaluation of oxidative stress in rheumatoid and psoriatic arthritis and psoriasis. Clin. Ter. 2009, 160, 467–472. [Google Scholar] [PubMed]
- Karaagac, L.; Koruk, S.T.; Koruk, I.; Aksoy, N. Decreasing oxidative stress in response to treatment in patients with brucellosis: Could it be used to monitor treatment? Int. J. Infect. Dis. 2011, 15, e346–e349. [Google Scholar] [CrossRef] [PubMed]
- Motor, S.; Ozturk, S.; Ozcan, O.; Gurpinar, A.B.; Can, Y.; Yuksel, R.; Yenin, J.Z.; Seraslan, G.; Ozturk, O.H. Evaluation of total antioxidant status, total oxidant status and oxidative stress index in patients with alopecia areata. Int. J. Clin. Exp. Med. 2014, 7, 1089–1093. [Google Scholar] [PubMed]
- Mukhopadhyay, K.; De, S.; Kundu, S.; Ghosh, P.; Chatterjee, S.; Chatterjee, M. Evaluation of levels of oxidative stress as a potential biomarker in patients with rheumatoid arthritis. J. Fam. Med. Prim. Care 2021, 10, 1981–1986. [Google Scholar] [CrossRef] [PubMed]
- Kelâmi, A. Autophotography in evaluation of functional penile disorders. Urology 1983, 21, 628–629. [Google Scholar] [CrossRef] [PubMed]
- Eri, L.M.; Thomassen, H.; Brennhovd, B.; Håheim, L.L. Accuracy and repeatability of prostate volume measurements by transrectal ultrasound. Prostate Cancer Prostatic Dis. 2002, 5, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Chung, B.H. Transrectal ultrasound versus magnetic resonance imaging in the estimation of prostate volume as compared with radical prostatectomy specimens. Urol. Int. 2007, 78, 323–327. [Google Scholar] [CrossRef] [PubMed]
- Rosen, R.C.; Riley, A.; Wagner, G.; Osterloh, I.H.; Kirkpatrick, J.; Mishra, A. The international index of erectile function (IIEF): A multidimensional scale for assessment of erectile dysfunction. Urology 1997, 49, 822–830. [Google Scholar] [CrossRef] [PubMed]
- Kahl, C.; Cleland, J.A. Visual analogue scale, numeric pain rating scale and the McGill pain Questionnaire: An overview of psychometric properties. Phys. Ther. Rev. 2005, 10, 123–128. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Zhu, D.; Pham, Q.M.; Wang, C.; Colonnello, E.; Yannas, D.; Nguyen, B.H.; Zhang, Y.; Jannini, E.A.; Sansone, A. Erectile Dysfunction and Oxidative Stress: A Narrative Review. Int. J. Mol. Sci. 2025, 26, 3073. [Google Scholar] [CrossRef] [PubMed]
- Knezevic, E.; Nenic, K.; Milanovic, V.; Knezevic, N.N. The Role of Cortisol in Chronic Stress, Neurodegenerative Diseases, and Psychological Disorders. Cells 2023, 12, 2726. [Google Scholar] [CrossRef] [PubMed]
- Mitsui, Y.; Yamabe, F.; Hori, S.; Uetani, M.; Kobayashi, H.; Nagao, K.; Nakajima, K. Molecular Mechanisms and Risk Factors Related to the Pathogenesis of Peyronie’s Disease. Int. J. Mol. Sci. 2023, 24, 10133. [Google Scholar] [CrossRef] [PubMed]
- Özdemir, E.Ç.; Erciyas, K.; Ünsal, B.; Sezer, U.; Taysi, S.; Araz, M. The Effects of Chronic Periodontitis and Obesity on Total Antioxidant/Oxidant Status and Oxidative Stress Index. Acta Endocrinol. 2022, 18, 294–300. [Google Scholar]
- Paulis, G.; De Giorgio, G. Complete Plaque Regression in Patients with Peyronie’s Disease after Multimodal Treatment with Antioxidants: A Report of 2 Cases. Am. J. Case Rep. 2022, 23, e936146. [Google Scholar] [CrossRef] [PubMed]
- Paulis, G.; De Giorgio, G. Full Regression of Peyronie’s Disease Plaque Following Combined Antioxidant Treatment: A Three-Case Report. Antioxidants 2022, 11, 1661. [Google Scholar] [CrossRef] [PubMed]
- Paulis, G.; De Giorgio, G. Patients with Peyronie’s disease achieve complete plaque regression after multimodal treatment with antioxidants: A case series. J. Med. Case Rep. 2022, 16, 359. [Google Scholar] [CrossRef] [PubMed]
- Paulis, G.; De Giorgio, G. Disappearance of Plaque Following Treatment with Antioxidants in Peyronie’s Disease Patients—A Report of 3 Cases. Clin. Pract. 2022, 12, 1020–1033. [Google Scholar] [CrossRef] [PubMed]
- Paulis, G.; De Giorgio, G.; Paulis, A. Healing of Peyronie’s disease after multimodal antioxidant treatment. A case series. Arch. Ital. Urol. Androl. 2024, 96, 12956. [Google Scholar] [CrossRef] [PubMed]
- Terrier, J.E.; Nelson, C.J. Psychological aspects of Peyronie’s disease. Transl. Androl. Urol. 2016, 5, 290–295. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.F.; Walsh, T.J.; Conti, S.L.; Turek, P.; Lue, T. Risk factors for emotional and relationship problems in Peyronie’s disease. J. Sex. Med. 2008, 5, 2179–2184. [Google Scholar] [CrossRef] [PubMed]
- Nelson, C.J.; Mulhall, J.P. Psychological impact of Peyronie’s disease: A review. J. Sex. Med. 2013, 10, 653–660. [Google Scholar] [CrossRef] [PubMed]
- Cilio, S.; Fallara, G.; Capogrosso, P.; Candela, L.; Belladelli, F.; Pozzi, E.; Corsini, C.; Raffo, M.; Schifano, N.; Boeri, L.; et al. The symptomatic burden of Peyronie’s disease at presentation according to patient age: A critical analysis of the Peyronie’s disease questionnaire (PDQ) domains. Andrology 2023, 11, 501–507. [Google Scholar] [CrossRef] [PubMed]
- Culha, M.G.; Erkan, E.; Cay, T.; Yücetaş, U. The Effect of Platelet-Rich Plasma on Peyronie’s Disease in Rat Model. Urol. Int. 2019, 102, 218–223. [Google Scholar] [CrossRef] [PubMed]
- Bivalacqua, T.J.; Diner, E.K.; Novak, T.E.; Vohra, Y.; Sikka, S.C.; Champion, H.C.; Kadowitz, P.J.; Hellstrom, W.J. A rat model of Peyronie’s disease associated with a decrease in erectile activity and an increase in inducible nitric oxide synthase protein expression. J. Urol. 2000, 163, 1992–1998. [Google Scholar] [CrossRef] [PubMed]
- Sohn, D.W.; Bae, W.J.; Kim, H.S.; Kim, S.W.; Kim, S.W. The anti-inflammatory and antifibrosis effects of anthocyanin extracted from black soybean on a Peyronie disease rat model. Urology 2014, 84, 1112–1116. [Google Scholar] [CrossRef] [PubMed]
| Group of PD Patients (no. 102) Mean Age 49.01 Years (SD ± 11.50) | Control Group (no. 100) Mean Age 49.12 Years (SD ± 11.23) | Statistical Analysis PD Group Versus Control Group (t-Test) p-Value = 0.950 | |||
|---|---|---|---|---|---|
| Demographic characteristics | No. of patients (out of 102) (%) | No. of patients (out of 100) (%) | p-value (chi-square test) | ||
| Race | |||||
| Caucasian | 102 (100%) | 100 (100%) | 1.000 | ||
| Age Range | |||||
| From 20 to 40 years | 25 (24.50%) | 26 (26.0%) | 0.807 | ||
| From 41 to 70 years | 77 (75.49%) | 74 (74.0%) | 0.807 | ||
| Clinical condition associated with PD patients | No. of patients (out of 102) (%) | No. of patients (out of 100) (%) | Statistical analysis Group of PD patients versus Control group p-value (chi-square test) | ||
| Penile curvature | 94 (92.1%) | Average penile curvature Angle (degrees) = 35.07° | 0 | Average penile curvature Angle (degrees) = 0° | <0.0001 |
| Penile pain | 54 (52.9%) | Mean VAS score = 4.4 | 0 | Mean VAS score = 0 | <0.0001 |
| Erectile dysfunction | 40 (39.2%) | Mean IIEF score = 21.1 | 0 | Mean IIEF score = 26.5 | <0.0001 |
| Significant anxiety | 80 (78.4%) | Mean GAD-7 score = 16.4 | 18 (18%) | Mean GAD-7 score = 7.4 | <0.0001 |
| Significant depression | 58 (56.8%) | Mean PHQ-9 score = 15.2 | 6 (6.0%) | Mean PHQ-9 score = 2.6 | <0.0001 |
| Cigarette smoking | 34 (33.3%) | Mean no. of cigarettes per day = 9.2 | 32 (32.0%) | Mean no. of cigarettes per day = 8.9 | 0.891 |
| Clinical Condition Associated with PD Patients | No. of Patients (out of 102) | Correlation with Penile OS Index Values (YES or NO) | Correlation with Systemic OS Index Values (YES or NO) | ||
|---|---|---|---|---|---|
| Penile pain | 54 (52.9%) | Pearson’s correlation coefficient (p = 0.562) | NO | Pearson’s correlation coefficient (p = 0.179) | NO |
| Penile curvature | 94 (92.1%) | Pearson’s correlation coefficient (p = 0.245) | NO | Pearson’s correlation coefficient (p = 0.621) | NO |
| Erectile dysfunction | 40 (39.2%) | Pearson’s correlation coefficient (p = 0.384) | NO | Pearson’s correlation coefficient (p = 0.327) | NO |
| Significant anxiety | 80 (78.4%) | Pearson’s correlation coefficient (p = 0.795) | NO | Pearson’s correlation coefficient (p = 0.926) | NO |
| Significant depression | 58 (56.8%) | Pearson’s correlation coefficient (p = 0.575) | NO | Pearson’s correlation coefficient (p = 0.231) | NO |
| Cigarette smoking | 34 (33.3%) | Pearson’s correlation coefficient (p = 0.927) | NO | Pearson’s correlation coefficient (p = 0.895) | NO |
| PD Patients (no. = 102) Mean (SD±) | Control Group (no. = 100) Mean (SD±) | Statistical Analysis p-Value (t-Test) | |
|---|---|---|---|
| d-ROM values (Carr. U.) | 487.5 (±91.4) | 327.67 (±75.85) | <0.0001 |
| PAT values (Cor. U.) | 3011.77 (±558.06) | 3487.76 (±595.61) | <0.0001 |
| OS Index (OSI) | 16.49 (±3.15) | 9.1 (±1.65) | <0.0001 |
| PHQ-9 Score Range | No. Total Cases (%) | |
|---|---|---|
| No depression | 0 | 4 (3.9) |
| Minimal depression | 1–4 | 6 (5.8) |
| Mild depression | 5–9 | 34 (33.3) |
| Moderate depression | 10–14 | 32 (31.3) |
| Moderately severe depression | 15–19 | 22 (21.5) |
| Severe depression | 20–27 | 4 (3.9) |
| Significantdepression | 10–27 | 58 (56.8) |
| TOTAL | 102 (100) | |
| GAD-7 Score Range | No. Total Cases (%) | |
| No anxiety | 0 | 0 |
| Minimal or mild anxiety | 1–9 | 22 (21.5) |
| Moderate anxiety | 10–14 | 40 (39.2) |
| Severe anxiety | 15–21 | 40 (39.2) |
| Significant anxiety | 10–21 | 80 (78.4) |
| TOTAL | 102 (100) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paulis, G.; Paulis, A.; De Giorgio, G.; Quattrocchi, S. Measurement of Oxidative Stress Index in 102 Patients with Peyronie’s Disease. Metabolites 2025, 15, 503. https://doi.org/10.3390/metabo15080503
Paulis G, Paulis A, De Giorgio G, Quattrocchi S. Measurement of Oxidative Stress Index in 102 Patients with Peyronie’s Disease. Metabolites. 2025; 15(8):503. https://doi.org/10.3390/metabo15080503
Chicago/Turabian StylePaulis, Gianni, Andrea Paulis, Giovanni De Giorgio, and Salvatore Quattrocchi. 2025. "Measurement of Oxidative Stress Index in 102 Patients with Peyronie’s Disease" Metabolites 15, no. 8: 503. https://doi.org/10.3390/metabo15080503
APA StylePaulis, G., Paulis, A., De Giorgio, G., & Quattrocchi, S. (2025). Measurement of Oxidative Stress Index in 102 Patients with Peyronie’s Disease. Metabolites, 15(8), 503. https://doi.org/10.3390/metabo15080503






