Abstract
Objective: The objective of this study was to analyze the prevalence and key sociodemographic and lifestyle determinants of metabolic syndrome (MetS) and the hypertriglyceridemic waist (HTGW) phenotype in a large occupational cohort. Background: Metabolic syndrome (MetS) and the hypertriglyceridemic waist (HTGW) phenotype, defined as the simultaneous presence of elevated waist circumference and high triglyceride levels, are major predictors of cardiometabolic morbidity and mortality. Despite their clinical relevance, data on their distribution and determinants in large occupational populations remain limited. Methods: A cross-sectional analysis was conducted on 139,634 employed adults (56,352 women and 83,282 men) across Spain, based on standardized clinical evaluations and validated questionnaires assessing physical activity, diet, smoking, alcohol consumption, education, and occupational class. Logistic regression models were used to estimate associations with MetS and HTGW. A longitudinal subsample of 40,431 individuals was followed over a 10-year period (2009–2019) to assess trends in metabolic risk phenotypes. Results: Male sex, older age, lower educational attainment, and unhealthy lifestyle behaviors were associated with a higher prevalence of both MetS and the HTGW phenotype. Physical inactivity, low adherence to the Mediterranean diet, and alcohol consumption were significantly associated with increased risk. The HTGW phenotype proved useful in identifying high-risk individuals, with a steadily increasing prevalence over time. Conclusions: Sociodemographic disparities and modifiable lifestyle factors significantly influence the prevalence and progression of MetS and HTGW in the Spanish workforce. Preventive strategies should emphasize early workplace screening, promotion of healthy behaviors, and reduction in educational and socioeconomic inequalities to mitigate cardiometabolic risk.
1. Introduction
Metabolic syndrome (MetS) represents a constellation of interrelated cardiometabolic risk factors—including central obesity, hypertension, dyslipidemia, and impaired glucose metabolism—that collectively elevate the risk of cardiovascular disease (CVD), type 2 diabetes mellitus (T2DM), and all-cause mortality [1]. The global prevalence of MetS has been steadily increasing, with current estimates indicating that approximately 25% of the adult population is affected [2]. In Spain, the prevalence of MetS varies depending on the diagnostic criteria applied, with studies reporting rates ranging from 24% to 37% [3,4].
The etiology of MetS is multifactorial, encompassing both genetic predispositions and modifiable lifestyle factors such as diet, physical activity, smoking, and alcohol consumption [5]. Socioeconomic status (SES) and educational attainment have also been identified as significant determinants, influencing health-related behaviors and access to healthcare resources [6]. Lower SES and educational levels are consistently associated with a higher prevalence of MetS, likely due to limited health literacy and reduced engagement in preventive health practices [7].
Dietary patterns, particularly adherence to the Mediterranean diet, have been inversely associated with MetS. This dietary pattern, characterized by high consumption of fruits, vegetables, whole grains, legumes, nuts, and olive oil, along with moderate intake of fish and poultry, has demonstrated protective effects against MetS and its components [8]. In contrast, diets high in ultra-processed foods and saturated fats have been linked to an increased risk of MetS [9].
Physical inactivity is another critical modifiable risk factor. Sedentary behavior contributes to obesity, insulin resistance, and dyslipidemia—all key components of MetS [10]. Regular physical activity has been shown to improve metabolic parameters and reduce the incidence of MetS [11].
The hypertriglyceridemic waist (HTGW) phenotype, defined by increased waist circumference and elevated triglyceride levels, has emerged as a practical and cost-effective clinical marker for identifying individuals at high risk for MetS and CVD [12]. This phenotype is particularly prevalent among individuals with poor dietary habits and sedentary lifestyles [13].
Despite a growing body of literature on MetS, large-scale studies investigating the interplay between sociodemographic factors, lifestyle behaviors, and educational attainment within the Spanish working population remain scarce. Understanding these associations is essential for developing targeted public health strategies aimed at reducing the burden of MetS and its complications.
This study aims to address this gap by analyzing data from over 139,000 Spanish workers to explore the relationships between sociodemographic characteristics, lifestyle behaviors, educational attainment, and the prevalence of MetS and the HTGW phenotype. By identifying key determinants, this research seeks to inform the design of effective prevention strategies tailored to high-risk occupational groups.
We hypothesize that lower educational level, unhealthy behaviors, and lower occupational class are significantly associated with increased prevalence of MetS and HTGW in the Spanish working population. The objective is to assess the prevalence and determinants of MetS and HTGW among Spanish workers, with a particular focus on sociodemographic and lifestyle factors. Understanding these associations may support the development of workplace-based preventive interventions and inform national public health policies aimed at mitigating cardiometabolic risk in vulnerable subgroups.
2. Methods
2.1. Study Design and Participant Selection
The investigation followed a two-stage methodological framework. In the first phase, a cross-sectional descriptive analysis was conducted involving 139,634 employees (56,352 women and 83,282 men) from various autonomous communities in Spain, including the Balearic Islands, Andalusia, Canary Islands, Valencian Community, Catalonia, Madrid, Castilla-La Mancha, Castilla y León, and the Basque Country. Participants represented a broad range of employment sectors, particularly hospitality, commerce, healthcare, public administration, transportation, industry, and cleaning services. Data were collected during routine occupational health assessments conducted by medical units affiliated with the participating companies. The data collection period extended from December 2020 to December 2021.
The second phase comprised a retrospective longitudinal analysis of a subsample of 40,431 individuals (24,229 men and 16,202 women) selected from the original cohort, for whom complete data were available. This phase spanned a ten-year period, from 2009 to 2019.
All anthropometric, clinical, and biochemical data were obtained by trained healthcare professionals employed by the collaborating institutions. Prior to data collection, standardized protocols were implemented to ensure methodological consistency and to minimize inter-observer variability.
2.2. Inclusion Criteria
Participants were eligible for inclusion if they met the following criteria:
- Aged between 18 and 69 years, representing the working-age population.
- Actively employed by one of the participating companies and not on medical leave at the time of data collection.
- Availability of complete data required for the calculation of cardiovascular risk metrics.
- Provision of informed consent for the use of anonymized data for epidemiological research.
- For inclusion in the longitudinal analysis: availability of complete records from both 2009 and 2019, with no major changes in sociodemographic or lifestyle characteristics over the study period.
A flowchart summarizing the recruitment and selection process is provided in Figure 1.
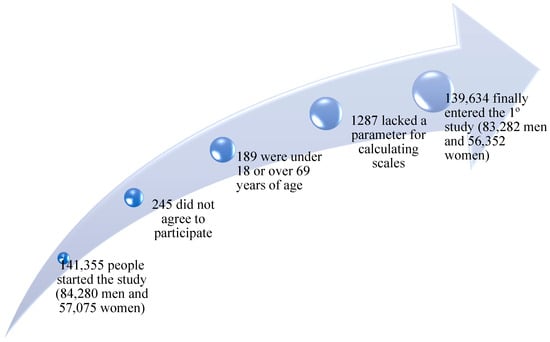
Figure 1.
Flowchart of participants.
2.3. Measurement and Data Collection Procedures
Measurements were conducted by trained professionals following harmonized protocols to ensure accuracy and reproducibility. These procedures included the assessment of body composition, blood pressure, and laboratory biomarkers.
Body weight and height were recorded using a calibrated SECA 700 scale. Waist circumference was measured with a SECA tape, following standard anthropometric procedures: the tape was positioned horizontally at the midpoint between the last palpable rib and the iliac crest, with participants standing upright and relaxed.
Blood pressure was measured using an automatic OMRON M3 device. Readings were taken in a seated position after a minimum of 10 min of rest. Three readings were obtained at one-minute intervals, and the average value was used for analysis [14].
Venous blood samples were collected after at least 12 h of fasting. Laboratory evaluations included plasma glucose, total cholesterol, and triglyceride concentrations, all assessed using enzymatic methods on automated analyzers. HDL-C was measured after precipitation with dextran sulfate–magnesium chloride. LDL-C levels were calculated using the Friedewald equation: LDL = Total cholesterol − HDL − (Triglycerides/5). All biochemical parameters are reported in mg/dL [15].
2.4. Definitions of Metabolic Syndrome
2.4.1. NCEP ATP III (National Cholesterol Education Program Adult Treatment Panel III)
MetS is diagnosed when at least three of the following criteria are met:
- Waist circumference > 102 cm in men or >88 cm in women;
- Triglycerides ≥ 150 mg/dL or specific treatment for hypertriglyceridemia;
- Blood pressure ≥ 130/85 mmHg;
- HDL cholesterol < 40 mg/dL in men or <50 mg/dL in women, or specific treatment;
- Fasting glucose > 110 mg/dL or specific treatment for hyperglycemia.
2.4.2. International Diabetes Federation (IDF)
MetS is diagnosed when central obesity is present—defined as a waist circumference > 80 cm in women and >94 cm in men—along with at least two of the following criteria:
- Triglycerides ≥ 150 mg/dL or specific treatment for hypertriglyceridemia;
- Systolic blood pressure ≥ 130 mmHg or diastolic ≥ 85 mmHg, or previous diagnosis of hypertension under treatment;
- HDL cholesterol < 40 mg/dL in men or <50 mg/dL in women, or specific treatment for this lipid abnormality;
- Fasting glucose > 100 mg/dL or previous diagnosis of type 2 diabetes.
2.4.3. Joint Interim Statement (JIS)
MetS is diagnosed when at least three of the following criteria are met:
- Waist circumference > 94 cm in men and > 80 cm in women;
- Triglycerides ≥ 150 mg/dL or specific treatment for hypertriglyceridemia;
- Systolic blood pressure ≥ 130 mmHg or diastolic ≥ 85 mmHg, or previous diagnosis of hypertension under treatment;
- HDL cholesterol < 40 mg/dL in men or <50 mg/dL in women, or specific treatment;
- Fasting glucose > 110 mg/dL or previous diagnosis of type 2 diabetes [16].
As part of the metabolic risk assessment, the hypertriglyceridemic waist (HTGW) phenotype was evaluated based on the concurrent presence of elevated waist circumference and high fasting triglyceride levels. Specifically, individuals were classified as having this phenotype if they exhibited a waist circumference ≥ 102 cm in men or ≥ 88 cm in women, together with fasting triglycerides ≥ 150 mg/dL. This criterion has been validated as a surrogate marker for visceral adiposity and is associated with increased cardiometabolic risk, including insulin resistance and atherogenic dyslipidemia [17]. Identifying this phenotype in occupational cohorts provides a practical and accessible approach to early risk stratification using routine clinical data.
2.5. Lifestyle and Sociodemographic Variables
Participants were classified as current smokers if they had smoked at least one cigarette per day (or an equivalent amount of tobacco) in the past month or had quit within the previous year [18].
Diet quality was assessed using the 14-item Mediterranean Diet Adherence Screener (MEDAS), originally developed for the PREDIMED study. Each item scores either 0 or 1, and a total score of ≥9 indicates high adherence to the Mediterranean diet, which is associated with cardiovascular health benefits [19].
Physical activity was evaluated using the International Physical Activity Questionnaire (IPAQ), which captures activity in three domains—occupational, commuting, and leisure—as well as sedentary behavior over the preceding seven days. Activities are categorized as vigorous, moderate, or walking, and results are expressed in MET-minutes/week, a standard metric in public health research [20].
Alcohol consumption was measured in standard alcohol units (SAUs), with one unit equivalent to 10 g of pure ethanol, based on national guidelines. Excessive intake was defined as ≥14 SAUs per week for women and ≥21 SAUs per week for men [21].
Occupational social class was classified according to the 2011 National Classification of Occupations (CNO-11) and criteria established by the Spanish Society of Epidemiology [22]:
- Class I: University-educated professionals and senior executives;
- Class II: Skilled self-employed workers and intermediate-level positions;
- Class III: Manual laborers and unskilled workers.
Educational attainment was categorized into three levels: primary, secondary, and tertiary (university-level) education.
2.6. Statistical Methods
Descriptive statistics were used to characterize the study population at baseline. Continuous variables are presented as means and standard deviations (SDs), and group differences were assessed using independent-samples t-tests. Categorical variables are presented as percentages, and comparisons were made using chi-square tests.
Multinomial logistic regression models were used to examine the associations between sociodemographic and behavioral factors and the presence of MetS (according to both NCEP ATP III and IDF definitions) and the HTGW phenotype in the cross-sectional dataset. Covariates included age group, sex, educational level, occupational class, smoking status, physical activity, alcohol consumption, and adherence to the Mediterranean diet. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated for all models.
In addition to the cross-sectional analysis, a retrospective longitudinal analysis was performed on a subsample of 40,431 individuals with complete data from both 2009 and 2019. For this phase, paired comparisons were conducted to evaluate changes in the prevalence of MetS and HTGW over the 10-year period. The percentage change between baseline (PRE) and follow-up (POST) values was calculated using the following formula:
[(POST − PRE)/PRE] × 100
Statistical significance for within-group comparisons was assessed using McNemar’s test for categorical variables. All statistical analyses were conducted using IBM SPSS Statistics version 29.0 (IBM Corp., Armonk, NY, USA). A p-value < 0.05 was considered statistically significant for all tests.
3. Results
Table 1 and Table 2 provide a detailed sex-stratified overview of anthropometric, biochemical, blood pressure, educational, and lifestyle characteristics among 139,634 Spanish workers. Statistically significant sex differences were observed across nearly all variables (p < 0.001), with men exhibiting higher average values for weight, blood pressure, total and LDL cholesterol, triglycerides, and glucose, while women showed higher levels of HDL cholesterol.

Table 1.
Characteristics of population.
Table 1.
Characteristics of population.
| Men n = 83,282 | Women n = 56,352 | ||
|---|---|---|---|
| Mean (SD) | Mean (SD) | p-Value | |
| Age (years) | 41.4 (10.7) | 40.1 (10.4) | <0.001 |
| Height (cm) | 173.8 (7.1) | 161.2 (6.5) | <0.001 |
| Weight (kg) | 83.2 (14.6) | 66.3 (13.9) | <0.001 |
| Systolic blood pressure (mmHg) | 126.2 (15.9) | 115.6 (15.7) | <0.001 |
| Diastolic blood pressure (mmHg) | 76.6 (10.9) | 71.1 (10.7) | <0.001 |
| Total cholesterol (mg/dL) | 199.6 (38.6) | 194.6 (36.9) | <0.001 |
| HDL cholesterol (mg/dL) | 50.0 (7.7) | 54.7 (9.2) | <0.001 |
| LDL cholesterol (mg/dL) | 122.6 (37.4) | 121.5 (37.1) | <0.001 |
| Triglycerides (mg/dL) | 133.8 (95.6) | 90.8 (49.7) | <0.001 |
| Glucose (mg/dL) | 93.0 (25.4) | 86.8 (18.1) | <0.001 |
| % | % | p-value | |
| < 30 years | 15.1 | 18.0 | <0.001 |
| 30–39 years | 29.6 | 31.0 | |
| 40–49 years | 30.2 | 30.3 | |
| 50–59 years | 20.9 | 17.7 | |
| 60–69 years | 4.2 | 3.0 | |
| Social class I | 7.5 | 13.6 | <0.001 |
| Social class II | 23.8 | 32.1 | |
| Social class III | 68.7 | 54.1 | |
| Elementary school | 66.4 | 48.1 | <0.001 |
| High school | 26.9 | 40.0 | |
| University | 6.7 | 11.9 | |
| Non-smokers | 66.8 | 67.9 | <0.001 |
| Smokers | 33.2 | 32.1 | |
| Non-physical activity | 62.4 | 51.4 | <0.001 |
| Yes physical activity | 37.6 | 48.6 | |
| Non-Mediterranean diet | 65.8 | 52.8 | <0.001 |
| Yes Mediterranean diet | 34.2 | 47.2 | |
| Non-alcohol consumption | 67.3 | 84.4 | <0.001 |
| Yes alcohol consumption | 32.7 | 15.6 |
LDL—low density lipoprotein-cholesterol. HDL-c—high density lipoprotein-cholesterol. SD—standard deviation.

Table 2.
Physical characteristics and metabolic indicators of Spanish workers.
Table 2.
Physical characteristics and metabolic indicators of Spanish workers.
| Men n = 83,282 | Women n = 56,352 | ||
|---|---|---|---|
| Variables | Mean (SD) | Mean (SD) | p-Value |
| Age (years) | 41.4 (10.7) | 40.1 (10.4) | <0.001 |
| Height (cm) | 173.8 (7.1) | 161.2 (6.5) | <0.001 |
| Weight (kg) | 83.2 (14.6) | 66.3 (13.9) | <0.001 |
| Systolic blood pressure (mmHg) | 126.2 (15.9) | 115.6 (15.7) | <0.001 |
| Diastolic blood pressure (mmHg) | 76.6 (10.9) | 71.1 (10.7) | <0.001 |
| Total cholesterol (mg/dL) | 199.6 (38.6) | 194.6 (36.9) | <0.001 |
| HDL-cholesterol (mg/dL) | 50.0 (7.7) | 54.7 (9.2) | <0.001 |
| LDL-cholesterol (mg/dL) | 122.6 (37.4) | 121.5 (37.1) | <0.001 |
| Triglycerides (mg/dL) | 133.8 (95.6) | 90.8 (49.7) | <0.001 |
| Glucose (mg/dL) | 93.0 (25.4) | 86.8 (18.1) | <0.001 |
HDL—high density lipoprotein. LDL—low density lipoprotein. SD—standard deviation.
Lifestyle-related variables also revealed notable differences: women were more likely to report healthier behaviors, including greater adherence to the Mediterranean diet, higher levels of physical activity, and lower alcohol consumption.
These patterns highlight the importance of sex-disaggregated analysis in research on metabolic and cardiovascular risk, as well as the critical role of social class and educational attainment in shaping health-related behaviors.
Table 3 reveals substantial age- and sex-related gradients in the prevalence of metabolic syndrome (MS) using both ATPIII and IDF definitions. Table 3 presents also substantial age- and sex-related gradients in the prevalence of metabolic syndrome (MetS), based on both ATP III and IDF criteria, as well as the hypertriglyceridemic waist (HTGW) phenotype. Prevalence increases progressively with age in both sexes but remains consistently higher in men across all age groups and socioeconomic strata. For example, the prevalence of MetS-IDF peaks at 35.9% among men aged 60–69, compared to just 14.8% among women in the same age category.

Table 3.
Prevalence of metabolic syndrome according to NCEP ATP III and IDF criteria, and hypertriglyceridemic waist phenotype (HTGW), with 95% confidence intervals, among Spanish Workers based on sociodemographic, educational, and lifestyle characteristics.
Table 3.
Prevalence of metabolic syndrome according to NCEP ATP III and IDF criteria, and hypertriglyceridemic waist phenotype (HTGW), with 95% confidence intervals, among Spanish Workers based on sociodemographic, educational, and lifestyle characteristics.
| MS NCEP ATPIII | MS IDF | HTGW | ||
|---|---|---|---|---|
| Variables Men | n | % (95% CI) | % (95% CI) | % (95% CI) |
| <30 years | 12,558 | 3.4 (3.1–3.7) | 5.0 (4.6–5.4) | 4.7 (4.3–5.1) |
| 30–39 years | 24,648 | 8.8 (8.4–9.2) | 11.8 (11.4–12.2) | 10.8 (10.4–11.2) |
| 40–49 years | 25,178 | 18.7 (18.2–19.2) | 23.2 (22.7–23.7) | 18.0 (17.5–18.5) |
| 50–59 years | 17,370 | 29.5 (28.8–30.2) | 32.7 (32.0–33.4) | 19.0 (18.4–19.6) |
| 60–69 years | 3528 | 44.9 (43.3–46.5) | 35.9 (34.3–37.5) | 20.1 (18.8–21.4) |
| Social class I | 6234 | 13.6 (12.8–14.4) | 17.1 (16.2–18.0) | 10.0 (9.3–10.7) |
| Social class II | 19,856 | 17.0 (16.4–17.6) | 19.0 (18.4–19.6) | 14.4 (13.9–14.9) |
| Social class III | 57,192 | 17.3 (17.0–17.6) | 22.2 (21.8–22.6) | 15.5 (15.1–15.9) |
| Elementary school | 55,306 | 20.9 (20.6–21.2) | 22.8 (22.5–23.1) | 14.3 (14.0–14.6) |
| High school | 22,408 | 15.4 (15.0–15.8) | 18.5 (18.1–18.9) | 15.5 (15.1–15.9) |
| University | 5568 | 14.5 (13.7–15.3) | 18.0 (17.1–18.9) | 10.3 (9.6–11.0) |
| Non-smokers | 55,618 | 15.8 (15.5–16.1) | 19.4 (19.1–19.7) | 14.2 (13.9–14.5) |
| Smokers | 27,664 | 19.0 (18.5–19.5) | 19.7 (19.2–20.2) | 14.6 (14.2–15.0) |
| Non-physical activity | 51,984 | 26.4 (26.0–26.8) | 30.6 (30.2–31.0) | 23.0 (22.6–23.4) |
| Yes physical activity | 31,298 | 0.9 (0.7–1.1) | 1.4 (1.2–1.6) | 2.3 (2.0–2.6) |
| Non-Mediterranean diet | 54,792 | 25.0 (24.6–25.4) | 28.9 (28.5–29.3) | 21.8 (21.4–22.2) |
| Yes Mediterranean diet | 28,490 | 1.2 (1.0–1.4) | 1.7 (1.5–1.9) | 3.4 (3.1–3.7) |
| Non-alcohol consumption | 56,022 | 7.6 (7.3–7.9) | 8.8 (8.5–9.1) | 6.1 (5.8–6.4) |
| Yes alcohol consumption | 27,260 | 35.8 (35.1–36.5) | 41.8 (41.1–42.5) | 31.3 (30.6–32.0) |
| Variables Women | n | % (95% CI) | % (95% CI) | % (95% CI) |
| <30 years | 10,110 | 1.4 (1.2–1.6) | 1.2 (1.0–1.4) | 0.9 (0.7–1.1) |
| 30–39 years | 17,460 | 3.4 (3.1–3.7) | 3.0 (2.7–3.3) | 1.6 (1.4–1.8) |
| 40–49 years | 17,094 | 8.3 (7.9–8.7) | 6.5 (6.1–6.9) | 2.9 (2.6–3.2) |
| 50–59 years | 9984 | 18.5 (17.7–19.3) | 12.0 (11.4–12.6) | 5.5 (5.1–5.9) |
| 60–69 years | 1704 | 29.0 (26.8–31.2) | 14.8 (13.1–16.5) | 6.1 (5.0–7.2) |
| Social class I | 7632 | 3.3 (2.9–3.7) | 2.7 (2.3–3.1) | 1.3 (1.0–1.6) |
| Social class II | 18,112 | 7.7 (7.3–8.1) | 6.1 (5.7–6.5) | 2.7 (2.4–3.0) |
| Social class III | 30,608 | 9.3 (9.0–9.6) | 6.8 (6.5–7.1) | 3.1 (2.9–3.3) |
| Elementary school | 27,086 | 9.6 (9.3–9.9) | 6.5 (6.2–6.8) | 3.2 (3.0–3.4) |
| High school | 22,574 | 7.3 (7.0–7.6) | 5.6 (5.3–5.9) | 2.8 (2.6–3.0) |
| University | 6692 | 3.4 (3.0–3.8) | 2.8 (2.4–3.2) | 1.0 (0.8–1.2) |
| Non-smokers | 38,252 | 7.1 (6.8–7.4) | 4.9 (4.6–5.2) | 2.7 (2.5–2.9) |
| Smokers | 18,100 | 8.4 (7.9–8.9) | 6.0 (5.6–6.4) | 2.8 (2.5–3.1) |
| Non-physical activity | 28,962 | 15.2 (14.7–15.7) | 11.1 (10.6–11.6) | 5.3 (5.0–5.6) |
| Yes physical activity | 27,390 | 0.3 (0.2–0.4) | 0.7 (0.5–0.9) | 0.5 (0.3–0.7) |
| Non-Mediterranean diet | 29,764 | 14.4 (13.9–14.9) | 10.7 (10.2–11.2) | 5.2 (4.9–5.5) |
| Yes Mediterranean diet | 26,588 | 0.4 (0.3–0.5) | 1.2 (1.0–1.4) | 0.9 (0.7–1.1) |
| Non-alcohol consumption | 47,536 | 2.6 (2.4–2.8) | 1.9 (1.7–2.1) | 1.1 (0.9–1.3) |
| Yes alcohol consumption | 8816 | 16.8 (16.0–17.6) | 16.6 (15.8–17.4) | 11.9 (11.2–12.6) |
MS—metabolic syndrome. NCEP ATPIII—National Cholesterol Education Program Adult Treatment. Panel III. IDF—International Diabetes Federation. HTGW—hypertriglyceridemic waist.
Unhealthy lifestyle behaviors—particularly alcohol consumption and physical inactivity—are strongly associated with higher prevalence rates of MetS and HTGW, especially among men. In contrast, individuals reporting adherence to the Mediterranean diet exhibit substantially lower prevalence across all metabolic phenotypes.
Table 4 presents the adjusted odds ratios (ORs) for the presence of MetS-ATPIII, MetS-IDF, and the hypertriglyceridemic waist (HTGW) phenotype across a range of sociodemographic and lifestyle factors. Male sex, older age, lower educational attainment, lower occupational class, smoking, physical inactivity, low adherence to the Mediterranean diet, and alcohol consumption all emerged as significant and independent risk factors for all three outcomes.

Table 4.
Adjusted prevalence estimates with 95% confidence intervals derived from logistic regression models based on sociodemographic, educational, and lifestyle characteristics in Spanish workers.
Table 4.
Adjusted prevalence estimates with 95% confidence intervals derived from logistic regression models based on sociodemographic, educational, and lifestyle characteristics in Spanish workers.
| MS NCEP ATPIII | MS IDF | HTGW | |
|---|---|---|---|
| Variables | OR (95% CI) | OR (95% CI) | OR (95% CI) |
| Women | 1 | 1 | 1 |
| Men | 1.61 (1.54–1.67) | 3.05 (2.92–3.19) | 4.25 (4.01–4.50) |
| <30 years | 1 | 1 | 1 |
| 30–39 years | 1.87 (1.75–1.99) | 1.14 (1.09–1.24) | 1.23 (1.16–1.30) |
| 40–49 years | 2.70 (2.51–2.90) | 1.22 (1.17–1.28) | 1.77 (1.56–1.97) |
| 50–59 years | 4.38 (4.05–4.72) | 1.86 (1.72–2.01) | 2.23 (1.88–2.59) |
| 60–69 years | 7.90 (7.09–8.70) | 3.17 (2.86–3.49) | 3.42 (2.60–4.23) |
| Social class I | 1 | 1 | 1 |
| Social class II | 1.21 (1.15–1.27) | 1.19 (1.15–1.23) | 1.19 (1.13–1.25) |
| Social class III | 1.93 (1.74–2.13) | 1.63 (1.49–1.77) | 1.88 (1.61–2.15) |
| University | 1 | 1 | 1 |
| High school | 1.25 (1.18–1.32) | 1.23 (1.18–1.28) | 1.14 (1.09–1.19) |
| Elementary school | 2.05 (1.80–2.30) | 1.59 (1.50–1.69) | 2.15 (1.88–2.42) |
| Non-smokers | 1 | 1 | 1 |
| Smokers | 1.23 (1.18–1.29) | 1.25 (1.18–1.32) | 1.19 (1.14–1.25) |
| Yes physical activity | 1 | 1 | 1 |
| Non-physical activity | 10.50 (9.07–11.94) | 9.92 (8.61–11.23) | 12.33 (10.12–12.53) |
| Yes Mediterranean diet | 1 | 1 | 1 |
| Non-Mediterranean diet | 2.18 (1.91–2.46) | 2.07 (1.81–2.34) | 7.35 (6.03–8.67) |
| Non-alcohol consumption | 1 | 1 | 1 |
| Yes alcohol consumption | 4.53(4.35–4.72) | 4.52 (4.34–4.71) | 4.31 (4.12–4.51) |
MS Metabolic syndrome. NCEP ATPIII National Cholesterol Education Program Adult Treatment. Panel III. IDF International Diabetes Federation. HTGW Hypertriglyceridemic waist.
Notably, the associations were particularly strong for physical inactivity (e.g., OR = 10.50 for MetS-ATPIII) and poor adherence to the Mediterranean diet (e.g., OR = 7.35 for HTGW), highlighting the critical role of modifiable lifestyle behaviors in cardiometabolic risk.
Table 5 summarizes the findings of the retrospective longitudinal analysis conducted on a subsample of 40,431 Spanish workers over a 10-year period (2009–2019). The table reports changes in the prevalence of metabolic syndrome (MetS) based on both NCEP-ATPIII and IDF criteria, as well as the hypertriglyceridemic waist (HTGW) phenotype, disaggregated by sex and stratified by age, occupational class, educational level, smoking status, physical activity, dietary habits, and alcohol consumption.

Table 5.
Prevalence of metabolic syndrome according to NCEP ATP III and IDF criteria, and hypertriglyceridemic waist phenotype (HTGW), before and after the study period, with absolute differences, stratified by sex and sociodemographic, educational, and lifestyle characteristics.
Table 5.
Prevalence of metabolic syndrome according to NCEP ATP III and IDF criteria, and hypertriglyceridemic waist phenotype (HTGW), before and after the study period, with absolute differences, stratified by sex and sociodemographic, educational, and lifestyle characteristics.
| MS NCEP ATPIII | MS IDF | HTGW | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| PRE | POST | PRE | POST | PRE | POST | |||||
| Variables Men | n | % | % | Difference (%) | % | % | Difference (%) | % | % | Difference (%) |
| <30 years | 3645 | 3.3 | 3.5 | 4.8 | 4.6 | 4.8 | 5.1 | 4.5 | 4.6 | 2.8 |
| 30–39 years | 6933 | 8.2 | 9.0 | 9.8 | 11.0 | 12.1 | 9.6 | 10.0 | 10.7 | 6.9 |
| 40–49 years | 7013 | 15.8 | 17.6 | 11.3 | 20.7 | 22.9 | 10.8 | 16.1 | 17.8 | 10.8 |
| 50–59 years | 4952 | 22.9 | 27.8 | 21.2 | 26.6 | 31.9 | 20.1 | 16.3 | 19.2 | 17.8 |
| Social class I | 1760 | 7.8 | 8.5 | 8.5 | 9.7 | 10.2 | 5.2 | 5.5 | 5.8 | 5.6 |
| Social class II | 5368 | 11.8 | 13.2 | 11.8 | 15.4 | 16.8 | 8.8 | 9.7 | 10.6 | 9.5 |
| Social class III | 15,415 | 14.9 | 17.4 | 16.9 | 22.7 | 25.9 | 13.9 | 16.8 | 19.9 | 18.2 |
| Elementary school | 14,914 | 14.5 | 17.0 | 17.0 | 21.8 | 24.8 | 14.0 | 16.5 | 19.5 | 18.0 |
| High school | 6053 | 11.6 | 13.0 | 12.0 | 16.3 | 17.7 | 8.7 | 10.2 | 11.2 | 9.6 |
| University | 1576 | 7.6 | 8.2 | 8.3 | 10.0 | 10.5 | 5.3 | 5.7 | 6.0 | 5.7 |
| Non-smokers | 15,122 | 11.6 | 12.5 | 8.0 | 13.9 | 14.8 | 6.2 | 9.4 | 10.1 | 7.5 |
| Smokers | 7421 | 16.9 | 19.8 | 17.2 | 20.7 | 23.8 | 14.8 | 17.7 | 19.9 | 12.4 |
| Yes physical activity | 8535 | 4.4 | 4.6 | 5.0 | 6.3 | 6.5 | 3.3 | 4.9 | 5.1 | 3.3 |
| Non-physical activity | 14,008 | 27.1 | 31.9 | 17.9 | 22.4 | 25.9 | 15.5 | 20.1 | 23.4 | 16.2 |
| Yes Mediterranean diet | 7767 | 6.1 | 6.5 | 5.7 | 7.6 | 7.9 | 3.9 | 6.6 | 6.9 | 3.9 |
| Non-Mediterranean diet | 14,776 | 25.7 | 29.8 | 16.1 | 18.3 | 20.9 | 14.1 | 16.3 | 18.8 | 15.1 |
| Non-alcohol consumption | 15,107 | 8.4 | 8.8 | 4.5 | 9.5 | 10.2 | 6.9 | 9.6 | 10.3 | 6.8 |
| Yes alcohol consumption | 7436 | 18.3 | 21.9 | 19.5 | 22.5 | 24.9 | 10.9 | 20.7 | 24.3 | 17.3 |
| Variables Women | n | % | % | Difference (%) | % | % | Difference (%) | % | % | Difference (%) |
| <30 years | 2833 | 1.6 | 1.6 | 2.9 | 1.5 | 1.5 | 3.1 | 0.9 | 0.9 | 1.9 |
| 30–39 years | 4824 | 3.1 | 3.3 | 4.9 | 2.9 | 3.1 | 5.1 | 1.6 | 1.7 | 5.1 |
| 40–49 years | 4636 | 7.5 | 8.2 | 8.8 | 5.9 | 6.4 | 9.0 | 2.8 | 3.0 | 9.0 |
| 50–59 years | 2768 | 15.9 | 17.9 | 12.6 | 10.6 | 11.9 | 12.5 | 5.1 | 5.7 | 11.8 |
| Social class I | 1973 | 5.5 | 5.9 | 6.8 | 4.2 | 4.4 | 4.7 | 1.7 | 1.8 | 4.4 |
| Social class II | 4920 | 7.6 | 8.2 | 8.5 | 5.7 | 6.1 | 7.9 | 2.7 | 2.9 | 6.9 |
| Social class III | 8168 | 14.2 | 15.8 | 11.2 | 9.9 | 11.2 | 13.1 | 5.2 | 5.8 | 12.0 |
| Elementary school | 7289 | 13.4 | 14.9 | 11.0 | 9.6 | 10.8 | 12.8 | 5.1 | 5.7 | 11.8 |
| High school | 6056 | 8.4 | 9.1 | 8.7 | 6.2 | 6.7 | 8.1 | 2.9 | 3.1 | 7.1 |
| University | 1716 | 5.8 | 6.2 | 6.9 | 4.3 | 4.5 | 4.8 | 1.8 | 1.9 | 4.5 |
| Non-smokers | 10,236 | 7.5 | 7.9 | 5.5 | 5.5 | 5.8 | 6.0 | 2.5 | 2.6 | 5.5 |
| Smokers | 4825 | 10.7 | 11.8 | 10.2 | 8.6 | 9.5 | 10.9 | 4.4 | 4.8 | 9.9 |
| Yes physical activity | 7317 | 3.0 | 3.1 | 3.1 | 2.3 | 2.4 | 2.9 | 1.1 | 1.1 | 1.9 |
| Non-physical activity | 7744 | 14.2 | 16.2 | 14 | 12.9 | 14.5 | 12.5 | 5.9 | 6.5 | 10.8 |
| Yes Mediterranean diet | 7029 | 3.8 | 3.9 | 3.9 | 2.8 | 2.9 | 3.5 | 1.6 | 1.6 | 2.5 |
| Non-Mediterranean diet | 8032 | 13.1 | 14.8 | 13.1 | 11.7 | 13.0 | 11.0 | 5.3 | 5.8 | 9.1 |
| Non-alcohol consumption | 12,750 | 6.2 | 6.5 | 5.0 | 4.6 | 4.8 | 5.0 | 2.0 | 2.1 | 4.8 |
| Yes alcohol consumption | 2311 | 12.0 | 13.3 | 10.9 | 8.3 | 9.2 | 10.5 | 4.9 | 5.4 | 10.9 |
MS—metabolic syndrome. NCEP ATPIII—National Cholesterol Education Program Adult Treatment Panel III. IDF—International Diabetes Federation. HTGW—hypertriglyceridemic waist. PRE = year 2009, POST = year 2019. The formula for calculating the difference is [POST − PRE/PRE] as a percentage.
The results reveal a consistent upward trend in the prevalence of all three conditions over the decade, particularly among men, individuals with lower educational attainment, and those engaging in unhealthy behaviors. For example, among men aged 50–59, the prevalence of MetS-IDF increased from 26.6% to 31.9%, while HTGW rose from 16.3% to 19.2%. Among women with only primary education, MetS-IDF prevalence rose from 9.6% to 10.8%, and HTGW from 5.1% to 5.7%. These changes reinforce the patterns observed in the cross-sectional data and suggest a progressive deterioration in cardiometabolic profiles over time.
The most pronounced relative increases were observed among individuals who were physically inactive or who did not adhere to the Mediterranean diet. For instance, HTGW prevalence in physically inactive men rose from 20.1% to 23.4%, while MetS-IDF prevalence among non-adherent men increased from 18.3% to 20.9%. These trends highlight the cumulative adverse impact of unhealthy behaviors on metabolic health and underscore the urgent need for sustained public health interventions.
Overall, Table 5 strengthens the evidence that lifestyle factors and social determinants not only influence current metabolic risk but also shape long-term health trajectories. The longitudinal component of the study adds valuable insight into the progression of cardiometabolic risk and suggests potential reversibility through targeted, behavior-based interventions.
4. Discussion
This large-scale study underscores the critical influence of sociodemographic, lifestyle, and educational variables on the prevalence of metabolic syndrome (MetS) and the hypertriglyceridemic waist (HTGW) phenotype within a representative cohort of Spanish workers. The findings reveal significant disparities by sex, age, educational attainment, and health-related behaviors, consistent with prior research and reinforcing the urgency of targeted interventions.
Low-grade chronic inflammation has been identified as a central mechanism in the pathophysiology of MetS and its association with hypertriglyceridemia [23]. Visceral obesity and insulin resistance contribute to a pro-inflammatory state in which hypertrophied adipocytes and infiltrating immune cells secrete cytokines such as TNF-α, IL-6, and MCP-1. These mediators impair insulin signaling and promote lipolysis, increasing the flux of free fatty acids to the liver and stimulating hepatic triglyceride synthesis and very-low-density lipoprotein (VLDL) production. These triglyceride-rich lipoproteins exacerbate dyslipidemia and sustain systemic inflammation [24].
Additionally, hypertriglyceridemia has been positively associated with elevated levels of high-sensitivity C-reactive protein (hsCRP), functioning as both a marker and an amplifier of the inflammatory state in MetS. This relationship supports its role in the development of atherosclerosis and type 2 diabetes, emphasizing the need for comprehensive clinical management [25].
The substantially higher prevalence of MetS and HTGW among men aligns with findings from European and global cohorts [26], including data from the European Health Interview Survey and the European Prospective Investigation into Cancer and Nutrition (EPIC) study, both of which linked male sex and older age with increased cardiometabolic risk [27].
This study also highlights strong associations between lower educational attainment and greater odds of both MetS and HTGW, underscoring the persistent impact of social determinants on health. These disparities may be partially mediated by differences in health literacy, healthcare access, and adoption of preventive behaviors [28].
However, it should be noted that data were collected exclusively from an actively employed population, potentially underestimating the true burden of MetS and HTGW relative to the general population. Individuals with severe health conditions or unemployed individuals, who may exhibit higher prevalence rates, were excluded. This selection bias has been acknowledged and addressed in the study’s limitations.
Adherence to the Mediterranean diet emerged as a significant protective factor, consistent with findings from the PREDIMED trials and the SUN cohort, where better diet quality was inversely associated with visceral adiposity and metabolic dysfunction [29,30]. Similarly, regular physical activity was independently associated with reduced odds of MetS and HTGW, underscoring the value of structured workplace wellness programs. A recent meta-analysis confirmed the dose-dependent benefits of physical activity in reducing cardiometabolic risk [31].
Of particular concern, physical inactivity and low adherence to the Mediterranean diet showed the highest odds ratios for all outcomes studied. This pattern reflects the clustering of unhealthy behaviors observed in the Global Burden of Disease (GBD) Study and the UK Biobank [32,33]. Furthermore, alcohol consumption—especially among men—was strongly associated with elevated risk, despite ongoing debate about threshold effects and potential benefits of light-to-moderate intake [34].
A key limitation is the cross-sectional design, which precludes causal inference and raises the possibility of reverse causality. While associations were found between lifestyle factors and MetS, it is plausible that some behaviors (e.g., poor diet or reduced activity) may result from, rather than cause, metabolic conditions. Moreover, self-reported lifestyle data, although collected via validated instruments, are vulnerable to recall and social desirability biases.
Despite these limitations, the HTGW phenotype proved to be a sensitive and practical surrogate marker for visceral adiposity and insulin resistance, as supported by previous occupational studies [35,36]. Its simplicity and reliance on routine clinical measurements enhance its utility in both primary and occupational care.
The consistency and magnitude of associations between lifestyle behaviors and the prevalence of MetS and HTGW reinforce the critical role of modifiable factors in the etiology of these metabolic conditions. Unhealthy behaviors sustained over time appear to have a cumulative impact on metabolic deterioration, significantly increasing cardiometabolic disease risk.
Importantly, the retrospective longitudinal analysis of 40,431 workers adds temporal depth to these findings, demonstrating a progressive worsening of cardiometabolic risk over a 10-year period (2009–2019). Rising prevalence of MetS and HTGW across all subgroups—particularly men, older adults, and individuals with lower educational attainment—mirrors trends observed in other long-term population-based studies, such as the Spanish PREDAPS cohort [37] and the Framingham Offspring Study [38].
The longitudinal data also highlight the impact of persistent unhealthy behaviors. For example, HTGW prevalence in physically inactive men rose from 20.1% to 23.4%, consistent with patterns observed in the AusDiab and D.E.S.I.R. studies, which documented the cumulative effect of sedentary lifestyles on metabolic deterioration [39,40]. Likewise, workers with only primary education experienced the greatest increases in MetS and HTGW, replicating the educational gradient reported in the Whitehall II Study and the EPIC-Norfolk cohort [41,42].
These comparisons strengthen the external validity of our findings and suggest that the deterioration of metabolic health among Spanish workers reflects a broader international trend. Moreover, they reaffirm the relevance of the HTGW phenotype as a simple, early marker for metabolic risk in occupational settings.
From a public health perspective, the data underscore how lifestyle and social determinants shape both current and future metabolic trajectories. While metabolic alterations may follow a progressive course, they may still be reversible with sustained, targeted interventions.
5. Strengths
- Large sample size: With over 139,000 participants and a longitudinal subsample exceeding 40,000, the study offers high statistical power and subgroup granularity.
- Occupational population: Inclusion of actively employed individuals facilitates development of pragmatic, workplace-based health promotion policies.
- Integrated phenotyping: Simultaneous assessment of MetS using both ATP III and IDF criteria, along with HTGW, enhances diagnostic robustness.
- Comprehensive variable set: Inclusion of sociodemographic, clinical, lifestyle, and dietary data enables multidimensional analyses.
- Temporal perspective: The 10-year retrospective follow-up provides insight into trends and trajectories of metabolic risk.
- Validated instruments: The use of validated tools (e.g., MEDAS and IPAQ) ensures reliable assessment of key behavioral variables in both cross-sectional and longitudinal contexts.
6. Limitations
- Healthy worker effect: Restricting the sample to actively employed individuals likely underestimates the true burden of metabolic disorders in the general population [43].
- Cross-sectional design: Limits causal inference and raises concerns about reverse causality (e.g., metabolic conditions leading to poor lifestyle choices). While longitudinal data were included, the retrospective design and lack of intermediate time points limit causal modeling.
- Self-reported lifestyle data: Despite validated instruments, responses may be influenced by recall or social desirability biases, particularly in a working adult population [44].
- Omission of psychosocial variables: Important factors such as stress, sleep patterns, and chronotype were not assessed, although they are increasingly recognized as relevant to metabolic risk [45].
7. Conclusions
In conclusion, this study highlights the substantial prevalence of metabolic syndrome (MetS) and the hypertriglyceridemic waist (HTGW) phenotype among Spanish workers, particularly among men, individuals with lower educational attainment, and those engaging in unhealthy lifestyle behaviors. The strength and consistency of the associations with modifiable risk factors underscore the critical need for preventive strategies tailored to these high-risk groups. Implementing targeted interventions within occupational settings offers a promising avenue to promote healthier behaviors and reduce cardiometabolic risk at the population level.
Future longitudinal research is warranted to elucidate causal mechanisms and rigorously assess the long-term effectiveness of workplace-based preventive interventions.
Author Contributions
Conceptualization, Á.A.L.-G., J.I.R.-M. and J.O.d.H.; data collection and analysis, Á.A.L.-G., J.O.d.H. and C.B.-C.; data curation, Á.A.L.-G. and C.B.-C.; methodology, J.I.R.-M. and Á.A.L.-G.; validation, P.R.-S., C.B.-C. and P.J.T.L.; formal analysis, Á.A.L.-G. and P.R.-S.; investigation, J.O.d.H., P.R.-S., C.B.-C. and P.J.T.L.; draft, J.O.d.H.; revision, J.I.R.-M. and Á.A.L.-G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was carried out in full accordance with the principles of the Declaration of Helsinki (2013) and adhered to applicable ethical standards for human research. Participant confidentiality and anonymity were rigorously maintained throughout the study. Ethical approval was granted by the Research Ethics Committee of the Balearic Islands (CEI-IB) under reference code IB 4383/20, authorized on 23 November 2020. Participant data were anonymized using coded identifiers, accessible only to the principal investigator. All procedures complied with the Spanish Organic Law 3/2018 of 5 December 2018, which protects personal data and digital rights. In accordance with this legislation, participants retained the right to access, rectify, cancel, or object to the processing of their personal information at any time.
Informed Consent Statement
Written informed consent was obtained from all participants involved in the study.
Data Availability Statement
The dataset generated and analyzed during the current study is stored in a secure database managed by ADEMA-Escuela Universitaria, in compliance with data protection regulations. The designated Data Protection Officer is Ángel Arturo López González.
Conflicts of Interest
The authors declare no conflicts of interest related to this study.
References
- Ndumele, C.E.; Neeland, I.J.; Tuttle, K.R.; Chow, S.L.; Mathew, R.O.; Khan, S.S.; Coresh, J.; Baker-Smith, C.M.; Carnethon, M.R.; Després, J.-P.; et al. A Synopsis of the Evidence for the Science and Clinical Management of Cardiovascular-Kidney-Metabolic (CKM) Syndrome: A Scientific Statement From the American Heart Association. Circulation 2023, 148, 1636–1664. [Google Scholar] [CrossRef] [PubMed]
- Saklayen, M.G. The Global Epidemic of the Metabolic Syndrome. Curr. Hypertens. Rep. 2018, 20, 12. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Strauss, M.; Lavie, C.J.; Lippi, G.; Brzęk, A.; Vollenberg, R.; Sanchis-Gomar, F.; Leischik, R. A systematic review of prevalence of metabolic syndrome in occupational groups-Does occupation matter in the global epidemic of metabolic syndrome? Prog. Cardiovasc. Dis. 2022, 75, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Toi, P.L.; Anothaisintawee, T.; Chaikledkaew, U.; Briones, J.R.; Reutrakul, S.; Thakkinstian, A. Preventive Role of Diet Interventions and Dietary Factors in Type 2 Diabetes Mellitus: An Umbrella Review. Nutrients 2020, 12, 2722. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fahed, G.; Aoun, L.; Zerdan, M.B.; Allam, S.; Zerdan, M.B.; Bouferraa, Y.; Assi, H.I. Metabolic Syndrome: Updates on Pathophysiology and Management in 2021. Int. J. Mol. Sci. 2022, 23, 786. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Carrilero, N.; García-Altés, A.; Mendicuti, V.M.; García, B.R. Do governments care about socioeconomic inequalities in health? Narrative review of reports of EU-15 countries. Eur. Policy Anal. 2021, 7, 521–536. [Google Scholar] [CrossRef]
- Fontán-Vela, J.; Ortiz, C.; López-Cuadrado, T.; Téllez-Plaza, M.; García-Esquinas, E.; Galán, I. Alcohol consumption patterns and adherence to the Mediterranean diet in the adult population of Spain. Eur. J. Nutr. 2024, 63, 881–891. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef] [PubMed]
- Moodie, R.; Bennett, E.; Kwong, E.J.L.; Santos, T.M.; Pratiwi, L.; Williams, J.; Baker, P. Ultra-Processed Profits: The Political Economy of Countering the Global Spread of Ultra-Processed Foods-A Synthesis Review on the Market and Political Practices of Transnational Food Corporations and Strategic Public Health Responses. Int. J. Health Policy Manag. 2021, 10, 968–982. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wu, J.; Zhang, H.; Yang, L.; Shao, J.; Chen, D.; Cui, N.; Tang, L.; Fu, Y.; Xue, E.; Lai, C.; et al. Sedentary time and the risk of metabolic syndrome: A systematic review and dose-response meta-analysis. Obes. Rev. 2022, 23, e13510. [Google Scholar] [CrossRef] [PubMed]
- Miranda-Tueros, M.; Ramirez-Peña, J.; Cabanillas-Lazo, M.; Paz-Ibarra, J.L.; Pinedo-Torres, I. Effects of aerobic exercise on components of the metabolic syndrome in older adults with type 2 diabetes mellitus: Systematic review and meta-analysis. Rev. Peru. Med. Exp. Salud Publica 2024, 41, 146–155. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Miñambres, I.; Sánchez-Hernández, J.; Cuixart, G.; Sánchez-Pinto, A.; Sarroca, J.; Pérez, A. Characterization of the hypertriglyceridemic waist phenotype in patients with type2 diabetes mellitus in Spain: An epidemiological study. Rev. Clin. Esp. 2020, 221, 576–581. [Google Scholar] [CrossRef] [PubMed]
- Tárraga Marcos, P.J.; López-González, Á.A.; Rifá, E.M.-A.; Oliveira, H.P.; Sánchez, C.M.; López, P.J.T.; Ramírez-Manent, J.I. The Prevalence of Metabolic Syndrome and Hypertriglyceridemic Waist Based on Sociodemographic Variables and Healthy Habits in Healthcare Workers: A Retrospective Study. Life 2025, 15, 81. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sastre-Alzamora, T.; Tomás-Gil, P.; Paublini, H.; Pallarés, L.; Ramírez-Manent, J.I.; López-González, A.A. Relationship between heart age and insulin resistance risk scales in 139634 Spanish workers. Acad. J. Health Sci. 2024, 39, 16–22. [Google Scholar] [CrossRef]
- Langlois, M.R. The Friedewald formula strikes back. Clin. Chem. Lab. Med. 2025, 63, 1043–1045. [Google Scholar] [CrossRef] [PubMed]
- Jover, A.M.; Ángel, A.; González, L.; Gil, P.T.; Coll, J.L.; Lliteras, P.M.; Ignacio, J.; Manent, R.; López-González, A.A. Hide Association between different cardiometabolic risk scales and metabolic syndrome scales in 418.343 Spanish workers. Acad. J. Health Sci. 2023, 38, 152–157. [Google Scholar] [CrossRef]
- Lu, N.; Cheng, G.; Ma, C.-M.; Liu, X.-L. Hypertriglyceridemic waist phenotype, hypertriglyceridemic waist-to-height ratio phenotype and abnormal glucose metabolism in adolescents. Diabetes Res. Clin. Pract. 2023, 198, 110622. [Google Scholar] [CrossRef] [PubMed]
- Juanola, M.C.A.; López-González, Á.A.; Tomás-Gil, P.; Paublini, H.; López, P.J.T.; Ramírez-Manent, J.I. Influence of tobacco consumption and other variables on the values of different cardiovascular risk factors in 418,343 spanish workers. Acad. J. Health Sci. 2024, 39, 89–95. [Google Scholar] [CrossRef]
- Ahmad, S.; Moorthy, M.V.; Lee, I.M.; Ridker, P.M.; Manson, J.E.; Buring, J.E.; Demler, O.V.; Mora, S. Mediterranean Diet Adherence and Risk of All-Cause Mortality in Women. JAMA Netw. Open. 2024, 7, e2414322. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mestre-Font, M.; Busquets-Cortés, C.; Ramírez-Manent, J.I.; Tomás-Gil, P.; Paublini, H.; López-González, A.A. Influence of sociodemographic variables and healthy habits on the values of overweight and obesity scales in 386,924 Spanish workers. Acad. J. Health Sci. 2024, 39, 27–35. [Google Scholar] [CrossRef]
- de Hevia, J.O.; López-González, Á.A.; Ramírez-Manent, J.I.; Oliveira, H.P.; López, P.J.T.; Riutord-Sbert, P. Relationship between alcohol consumption and other variables with the values of different cardiovascular risk factors in 139634 Spanish workers. Acad. J. Health Sci. 2024, 39, 132–141. [Google Scholar] [CrossRef]
- Domingo-Salvany, A.; Bacigalupe, A.; Carrasco, J.M.; Espelt, A.; Ferrando, J.; Borrell, C.; de Determinantes Sociales de la Sociedad Española de Epidemiología, G. Propuestas de clase social neoweberiana y neomarxista a partir de la Clasificación Nacional de Ocupaciones. Gac. Sanit. 2013, 27, 263–272. (In Spanish) [Google Scholar] [CrossRef] [PubMed]
- Basaran, E.; Aktas, G. Waist-to-height ratio as a novel marker of metabolic syndrome in patients with type 2 diabetes mellitus. Explor. Endocr. Metab. Dis. 2025, 2, 101421. [Google Scholar] [CrossRef]
- Kojta, I.; Chacińska, M.; Błachnio-Zabielska, A. Obesity, Bioactive Lipids, and Adipose Tissue Inflammation in Insulin Resistance. Nutrients 2020, 12, 1305. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Peng, X.; Wu, H. Inflammatory Links Between Hypertriglyceridemia and Atherogenesis. Curr. Atheroscler Rep. 2022, 24, 297–306. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nsabimana, P.; Sombié, O.O.; Pauwels, N.S.; Boynito, W.G.; Tariku, E.Z.; Vasanthakaalam, H.; De Henauw, S.; Abbeddou, S. Association between urbanization and metabolic syndrome in low- and middle-income countries: A systematic review and meta-analysis. Nutr. Metab. Cardiovasc. Dis. 2024, 34, 235–250. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, D.; Luben, R.; Hayat, S.; Talarico, R.; Allen, N.E.; Kuźma, E.; Littlejohns, T.J. Role of age and exposure duration in the association between metabolic syndrome and risk of incident dementia: A prospective cohort study. Lancet Healthy Longev. 2024, 5, 100652. [Google Scholar] [CrossRef] [PubMed]
- Stringhini, S.; Carmeli, C.; Jokela, M.; Avendaño, M.; McCrory, C.; d’Errico, A.; Bochud, M.; Barros, H.; Costa, G.; Chadeau-Hyam, M.; et al. Socioeconomic status, non-communicable disease risk factors, and walking speed in older adults: Multi-cohort population based study. BMJ. 2018, 360, k1046. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Leone, A.; De Amicis, R.; Battezzati, A.; Bertoli, S. Adherence to the Mediterranean Diet and Risk of Metabolically Unhealthy Obesity in Women: A Cross-Sectional Study. Front. Nutr. 2022, 9, 858206. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fabiani, R.; Naldini, G.; Chiavarini, M. Dietary Patterns and Metabolic Syndrome in Adult Subjects: A Systematic Review and Meta-Analysis. Nutrients 2019, 11, 2056. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Garcia, L.; Pearce, M.; Abbas, A.; Mok, A.; Strain, T.; Ali, S.; Crippa, A.; Dempsey, P.C.; Golubic, R.; Kelly, P.; et al. Non-occupational physical activity and risk of cardiovascular disease, cancer and mortality outcomes: A dose-response meta-analysis of large prospective studies. Br. J. Sports Med. 2023, 57, 979–989. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cubas-Basterrechea, G.; Elío, I.; Alonso, G.; Otero, L.; Gutiérrez-Bardeci, L.; Puente, J.; Muñoz-Cacho, P. Adherence to the Mediterranean Diet Is Inversely Associated with the Prevalence of Metabolic Syndrome in Older People from the North of Spain. Nutrients 2022, 14, 4536. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- GBD 2021 Nervous System Disorders Collaborators. Global, regional, and national burden of disorders affecting the nervous system, 1990-2021: A systematic analysis for the Global Burden of Disease Study 2021. Lancet Neurol. 2024, 23, 344–381, Erratum in Lancet Neurol. 2024, 23, e11. https://doi.org/10.1016/S1474-4422(24)00231-X. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chen, H.; Feng, J.; Chen, L.; Huang, J.; Zhang, P.; Chen, C.; Lu, L.; Tang, C. Acupoint stimulation for alcohol use disorder: A systematic review and meta-analysis. Medicine 2023, 102, e32614. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tian, Y.-M.; Ma, N.; Jia, X.-J.; Lu, Q. The “hyper-triglyceridemic waist phenotype” is a reliable marker for prediction of accumulation of abdominal visceral fat in Chinese adults. Eat. Weight. Disord. 2020, 25, 719–726. [Google Scholar] [CrossRef] [PubMed]
- de Cuevillas, B.; Alvarez-Alvarez, I.; Riezu-Boj, J.I.; Navas-Carretero, S.; Martinez, J.A. The hypertriglyceridemic-waist phenotype as a valuable and integrative mirror of metabolic syndrome traits. Sci. Rep. 2021, 11, 21859. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Guallar-Castillón, P.; Pérez, R.F.; López García, E.; León-Muñoz, L.M.; Aguilera, M.T.; Graciani, A.; Gutiérrez-Fisac, J.L.; Banegas, J.R.; Rodríguez-Artalejo, F. Magnitude and management of metabolic syndrome in Spain in 2008-2010: The ENRICA study. Rev. Esp. Cardiol. (Engl. Ed.) 2014, 67, 367–373. [Google Scholar] [CrossRef] [PubMed]
- Masenga, S.K.; Kabwe, L.S.; Chakulya, M.; Kirabo, A. Mechanisms of Oxidative Stress in Metabolic Syndrome. Int. J. Mol. Sci. 2023, 24, 7898. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Balkau, B.; Charles, M.A.; Drivsholm, T.; Borch-Johnsen, K.; Wareham, N.; Yudkin, J.S.; Morris, R.; Zavaroni, I.; van Dam, R.; Feskins, E.; et al. Frequency of the WHO metabolic syndrome in European cohorts, and an alternative definition of an insulin resistance syndrome. Diabetes Metab. 2002, 28, 364–376. [Google Scholar] [PubMed]
- Corbi-Cobo-Losey, M.J.; Martinez-Gonzalez, M.Á.; Gribble, A.K.; Fernandez-Montero, A.; Navarro, A.M.; Domínguez, L.J.; Bes-Rastrollo, M.; Toledo, E. Coffee Consumption and the Risk of Metabolic Syndrome in the ‘Seguimiento Universidad de Navarra’ Project. Antioxidants 2023, 12, 686. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lan, L.; Lang, X.; McKee, M.; Tse, L.A.; Rangarajan, S.; Qiang, D.; Liu, Z.; Wang, B.; Liu, Z.; Yan, M.; et al. Association of sitting time with cardiovascular events among manual and non-manual workers: A prospective cohort study (PURE-China). BMC Public Health 2025, 25, 750. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Karagöz, A.; Onat, A.; Aydın, M.; Can, G.; Şimşek, B.; Yüksel, M. Distinction of hypertriglyceridemic waist phenotype from simple abdominal obesity: Interaction with sex hormone-binding globulin levels to confer high coronary risk. Postgrad Med. 2017, 129, 288–295. [Google Scholar] [CrossRef] [PubMed]
- Möhner, M. An approach to adjust standardized mortality ratios for competing cause of death in cohort studies. Int. Arch. Occup. Environ. Health 2016, 89, 593–598. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Prince, S.A.; Adamo, K.B.; Hamel, M.E.; Hardt, J.; Gorber, S.C.; Tremblay, M. A comparison of direct versus self-report measures for assessing physical activity in adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2008, 5, 56. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hu, J.; Zhu, X.; Yuan, D.; Ji, D.; Guo, H.; Li, Y.; He, Z.; Bai, H.; Zhu, Q.; Shen, C.; et al. Association of sleep duration and sleep quality with the risk of metabolic syndrome in adults: A systematic review and meta-analysis. Endokrynol. Pol. 2022, 73, 968–987. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).