Abstract
It has been consistently demonstrated that circulating lipids and particularly low-density lipoprotein cholesterol (LDL-C) play a significant role in the development of coronary artery disease (CAD). Several trials have been focused on the reduction of LDL-C values in order to interfere with atherothrombotic progression. Importantly, for patients who experience acute coronary syndrome (ACS), there is a 20% likelihood of cardiovascular (CV) event recurrence within the two years following the index event. Moreover, the mortality within five years remains considerable, ranging between 19 and 22%. According to the latest guidelines, one of the main goals to achieve in ACS is an early improvement of the lipid profile. The evidence-based lipid pharmacological strategy after ACS has recently been enhanced. Although novel lipid-lowering drugs have different targets, the result is always the overexpression of LDL receptors (LDL-R), increased uptake of LDL-C, and lower LDL-C plasmatic levels. Statins, ezetimibe, and PCSK9 inhibitors have been shown to be safe and effective in the post-ACS setting, providing a consistent decrease in ischemic event recurrence. However, these drugs remain largely underprescribed, and the consistent discrepancy between real-world data and guideline recommendations in terms of achieved LDL-C levels represents a leading issue in secondary prevention. Although the cost-effectiveness of these new therapeutic advancements has been clearly demonstrated, many concerns about the cost of some newer agents continue to limit their use, affecting the outcome of patients who experienced ACS. In spite of the fact that according to the current recommendations, a stepwise lipid-lowering approach should be adopted, several more recent data suggest a "strike early and strike strong" strategy, based on the immediate use of statins and, eventually, a dual lipid-lowering therapy, reducing as much as possible the changes in lipid-lowering drugs after ACS. This review aims to discuss the possible lipid-lowering strategies in post-ACS and to identify those patients who might benefit most from more powerful treatments and up-to-date management.
1. Introduction
Coronary artery disease (CAD) is still a leading cause of global mortality, in spite of interventional and pharmacological strategy improvements [1].
Acute coronary syndrome (ACS) represents one of the most severe clinical presentations of coronary artery disease (CAD) [2].
In the last decades, ACS management has been considerably improved, leading to a significant reduction in in-hospital mortality, from 30% to 3–8% [3].
Remarkably, at five years, the mortality rate has been estimated to be 19–22% [4,5].
Moreover, in the 24 months following an ACS event, the survivors have a 30% likelihood of experiencing a second event [6].
The recurrence of ischemic cardiovascular (CV) events and, consequently, the need for new revascularizations has been shown to be associated with higher mortality in the long run [7,8,9,10].
Nowadays, it has been well-recognized that dyslipidemia is the main cause of atherosclerosis development. Therefore, it should be adequately treated in order to achieve a significant reduction in CV risk, especially in patients who experienced ACS. Indeed, a lower rate of CV events and mortality has been shown to be associated with effective lipid management in this group of patients [5].
In the latest years, lipid-lowering strategies have been noticeably improved. Because of this, physicians may have several options to treat this subset of patients.
An early lipid-lowering pharmacological approach at hospital discharge combined with short-term follow-up has been recently proposed in order to reduce adverse events in post-ACS patients [11].
Nonetheless, post-ACS management remains suboptimal, particularly in terms of lipid therapeutic target achievement.
This review aims to promote an understanding of the main therapeutic options, with a special focus on those recently introduced in clinical practice, for lipid management in patients who experienced ACS.
2. Lipid-Lowering Therapy (LLT)
Dyslipidemia is a metabolic disorder determined by the concurrence of genetic conditions and unhealthy lifestyles [12].
A close relationship between the incidence of atherosclerosis and serum cholesterol levels has been well recognized [13], and increased values of low-density lipoprotein cholesterol (LDL-C) are the primary cause of the development and progression of atherosclerosis [14].
Indeed inflammation, LDL-C, platelet activation, and endothelial dysfunction have been considered the leading atherogenic factors [15,16]. Remarkably, it has been shown that LDL-C and circulating monocyte levels are linked, confirming the correlation between lipids, inflammatory status, and CAD progression [17,18].
Furthermore, it has been established that intensive lipid-lowering therapy (LLT) may improve plaque phenotype, contributing to plaque stabilization [19,20].
Moreover, it has been claimed that an intensive LLT is correlated with better outcomes in those patients who experienced ACS [21,22].
Consequently, the reduction [21,23] of circulating LDL-C is one of the most relevant goals to achieve for CVD prevention. This goal is achievable thanks to several effective pharmacological interventions currently available [24]. Table 1 summarizes the action of LLT.

Table 1.
Main lipid-lowering drugs.
2.1. Statins
Statin therapy has been shown to decrease all-cause mortality and 5-year incidence of major adverse cardiovascular events (MACE) by 12% and 21%, respectively, per mmol/L LDL-C reduced (roughly equivalent to 39 mg/dL) [37]. A 20% reduction of CV adverse events rate has been reported using statins compared with placebo and high-intensity statins compared with low-intensity statins for each LDL 1.0-mmol/L reduction [23].
Nowadays, statins are considered the first-line pharmacological therapy in order to manage dyslipidemia and reduce CV risk [38]. Some statins derive from fungal fermentation, such as lovastatin, pravastatin, and simvastatin [39], others from synthetic processes (atorvastatin, rosuvastatin) [39].
It has been shown that statins competitively inhibit the activity of 3-hydroxy-3-methyl-glutaryl-coenzyme A reductase (HMGR), which converts 3-hydroxy-3-methyl-glutaryl-coenzyme A (HMG-CoA) into mevalonic acid, a cholesterol precursor [40].
This phase is an early rate-limiting step in cholesterol biosynthesis. The binding of statins with HMG-CoA reductase is reversible [41].
As a result of statin activity, a non-linear dose-dependent LDL-C reduction occurs.
Considering the fact that mevalonate, derived from HMGR, is also the precursor of many other nonsteroidal isoprenoid compounds, such as farnesyl pyrophosphate (FPP) and geranylgeranyl pyrophosphate (FPD), statins also affect the Ras-related small GTPase signaling pathway (Ras and Rho) [42].
Some of the statins’ pleiotropic effects are ascribed to the inhibition of these intracellular isoprenoid-dependent proteins [43]. Indeed, several cardioprotective effects of statins observed during chronic use have been thought to be not directly linked to cholesterol levels [44,45,46].
Anti-inflammatory activity has also been postulated [47]. A potent modulating effect on endothelial cell nitric oxide synthase (eNOS) resulting in the upregulation of eNOS enzyme and a decrease in nitric oxide (NO) production [47], as well as a reduction in cytokine C-reactive protein (CRP) levels, has been reported [31,48,49,50].
A large number of experimental and clinical studies investigated the potential additional effects of statins, postulating an improvement in endothelial function and vascular tone, plaque stabilization effects and anti-thrombotic activity, and reduction in oxidative stress [47].
An incremental lowering of LDL-C values, which has been shown in patients receiving intensive statin therapy compared with those treated with moderate-dose statins, results in a lower rate of nonfatal CV events [21,30,51,52,53]. Good tolerance has been generally reported in patients treated with statins, but 20% of intolerant patients reported statin intolerance syndrome with adverse effects on muscles, varying from myalgia to myopathy, myositis, and rhabdomyolysis [54,55]. Statin-induced intolerance may cause therapy interruption [56,57].
A rise in the risk of adverse CV outcomes has been reported in patients discontinuing statin therapy [58,59]. A genetic predisposition has been hypothesized to be involved in the development of statin-induced muscle failure [60].
However, safety issues associated with intensive statin therapy and the evidence of residual risk of recurrent CV events [61] have led to the introduction of additional non-statin therapies in clinical practice [62].
2.2. Ezetimibe
Ezetimibe joins a new drug class of selective cholesterol absorption inhibitors that block the internalization of cholesterol into enterocytes at the level of the brush border of the small intestine [63].
The ezetimibe-mediated inhibition of the Niemann–Pick C1-like 1 (NPC1L1) polytopic transmembrane protein results in reduced intestinal cholesterol absorption [64].
A 10–14% and 23–24% LDL-C plasma level reduction has been observed in patients treated with ezetimibe alone or in addition to statins, respectively [65,66]. Ezetimibe combined with a low dose of statins may represent a suitable option in case of symptoms of intolerance in patients treated with full doses of statins [65]. More recent studies have shown great results with ezetimibe and bempedoic acid co-therapy, with a 38% mean difference in LDL cholesterol level reduction compared to the placebo [67].
In the IMPROVE-IT trial, in high-risk patients post ACS, the combination strategy of ezetimibe 10 mg and simvastatin 40 mg proved to be superior to simvastatin 40 mg alone in lowering the recurrence of CV events, irrespective of baseline LDL-C levels [68]. An incremental beneficial effect of ezetimibe added to statin has been observed in patients with DM and in those without DM but at high risk of recurrent CV events [69].
2.3. Bempedoic Acid
Bempedoic acid has recently entered the pharmacological armamentarium for dyslipidemia treatment [70].
After its conversion to the active metabolite by acyl-CoA synthetase 1 (ACSVL1), exclusively expressed in liver cells, bempedoic acid lowers cholesterol synthesis by inhibiting adenosine triphosphate (ATP) citrate lyase, which, in the enzymatic cascade that leads to cholesterol synthesis, acts upstream of HMGCR.
Similarly to statins, reduced hepatic cholesterol synthesis induced by bempedoic acid leads to the upregulation of LDL-R expression and, consequently, reduction in LDL-C levels [71]. The reason why fewer muscular adverse effects have been associated with this therapy is that bempedoic acid is a prodrug selectively activated in the hepatic tissue. In skeletal muscle, the prodrug can not be activated due to the absence of ACSVL1, explaining the reduction in adverse muscle effects mentioned above. Moreover, ATP citrate lyase downregulation and AMP-activated protein kinase (AMPK) upregulation improves glucose metabolism regulation [60] and reduces the inflammatory pathway and cytokine production [72]
The safety and efficacy of the long-term use of bempedoic acid have been investigated in several clinical trials, including Cholesterol Lowering via BEmpedoic Acid, an ACL-inhibiting Regimen (CLEAR) Tranquility [67], CLEAR Serenity [73], CLEAR Wisdom [73], and CLEAR Harmony [74,75]. At a daily dose of 180 mg, an LDL-C reduction from 17.4 to 28.5% was obtained [76].
Recently, in a trial that included 13,970 patients, 69.9% with a previous CV event with statin intolerance, the incidence of primary endpoint events (death from CV causes, nonfatal myocardial infarction, nonfatal stroke, or coronary revascularization) was 13% lower in the treated group. The incidences of gout and cholelithiasis were higher with bempedoic acid than with placebo (3.1% vs. 2.1% and 2.2% vs. 1.2%, respectively), as were the incidences of small increases in serum creatinine, uric acid, and hepatic enzyme levels [77].
2.4. PCSK9 Inhibitors
Proprotein convertase subtilisin-like kexin type 9 (PCSK9) is a serine protease mainly expressed in the liver that targets LDL-Rs, promoting their lysosomal degradation and decreasing circulating LDL-C clearance [78]. PCSK9 monoclonal antibodies (mAbs) selectively bind to extracellular PCSK9, preventing LDL-R degradation and lowering plasma LDL-C levels. Two fully human mAbs, Alirocumab and Evolocumab, have been approved by FDA and EMA [79].
Statin treatment increases circulating PCSK9 serum levels; consequently, the greatest effect of these mAbs has been observed when used in combination with statins [80]. A reduction in LDL-C plasma levels has been shown, of up to 65% for alirocumab and 80% for evolocumab, following an injection every 2 or 4 weeks [81].
PCSK9 mAbs were associated with a 20% lower risk of myocardial infarction, a 22% lower risk of ischemic stroke, and a 17% lower risk of coronary revascularization [82]. Their use was associated with a favorable safety profile without increasing risk of neurocognitive adverse events, liver enzyme elevations, rhabdomyolysis, or new-onset diabetes mellitus. According to the GLAGOV data [83], both molecules have been shown to favor morphological stabilization and reduction of carotid plaques [20,84,85,86,87], delaying ASCVD progression.
2.5. Inclisiran
Small interfering RNA (siRNA) molecules now represent the next generation of drugs designed to antagonize PCSK9. Inclisiran is an siRNA specific for PCSK9 that prevents the translation of PCSK9 messenger RNA, leading to decreased concentrations of the protein and lower concentrations of LDL cholesterol.
Inclisiran blocks the expression of a specific gene by selectively silencing the translation of PCSK9 messenger RNA (mRNA) [88], leading to a long-lasting reduction in LDL-C even up to 12 months [89,90]. It was thought that the reason why inclisiran has such long-term efficacy is that the silencing complex remained active even after mRNA degradation, resulting in a considerable and long-lasting reduction in plasma LDL-C levels [89]. Consequently, inclisiran has been considered an attractive therapeutic option, particularly for non-adherent patients [91]. What the impact of inclisiran on reducing lipoproteins and MACE is, has been largely investigated in the ORION/VICTORION studies [90,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106], which evidenced a decrease in LDL-C over 1 year of 29.5–38.7% and 29.9–46.4% after a single dose and after two doses, respectively (p < 0.001). Moreover, Lp(a) has been shown to significantly decrease.
3. Historical Randomized Controlled Trials with Statin and Ezetimibe
Statins are the first drugs with a marked and sustained effect on the reduction of LDL-C that have been extensively studied in several clinical trials. Statin trials have played a pivotal role in demonstrating the effects of lipid-lowering therapies (LLT) in reducing CV risk in both primary and secondary prevention. These trials have consistently shown that statin therapy reduces the risk of major CV events by approximately 20–50% among different populations at high CV risk. Different trials focused on the early initiation of statin therapy in patients with ACS [107]. Indeed, starting treatment early after ACS allows for the potential benefits of statins to be maximized. During this acute phase, aggressive lipid-lowering therapy can have a substantial impact on reducing plaque instability, inflammation, and subsequent CV events. The Pravastatin in Acute Coronary Treatment (PACT) trial and the Fluvastatin On Risk Diminishing After Acute myocardial infarction (FLORIDA) trial both showed that moderate-intensity statin treatment did not significantly reduce the early incidence of major CV events [29,108]. The Myocardial Ischemia Reduction with Aggressive Cholesterol Lowering (MIRACL) trial demonstrated that early initiation of high-dose atorvastatin in patients with unstable angina or non-ST-segment elevation myocardial infarction resulted in a reduction in MACE. Patients in the atorvastatin group had a 16% reduction in the risk of the primary endpoint, which included death from any cause, non-fatal myocardial infarction, cardiac arrest, or recurrent symptomatic myocardial ischemia requiring emergency rehospitalization [31]. The Aggrastat to Zocor (A to Z) trial compared early intensive statin therapy with simvastatin followed by a switch to high-dose atorvastatin versus standard-dose simvastatin in patients with ACS [30]. The trial found that the early intensive therapy group had a lower incidence of MACE compared to the standard therapy group. At 30 days, the early intensive therapy group had a 16% reduction in the composite endpoint of death from any cause, non-fatal myocardial infarction, readmission for ACS, or stroke. However, there was no significant difference between the two groups in the primary endpoint of death from CV causes, non-fatal myocardial infarction, or resuscitated cardiac arrest. The Pravastatin or Atorvastatin Evaluation and Infection Therapy-Thrombolysis In Myocardial Infarction 22 (PROVE-IT TIMI 22) trial compared the effectiveness of high-dose atorvastatin versus standard-dose pravastatin in reducing CV events among patients with recent ACS [21]. The event rate was 26.3% in the atorvastatin group and 32.7% in the pravastatin group, representing a relative risk reduction of 16% in favor of high-dose atorvastatin. These data provided evidence that high-intensity statin treatment after ACS improves patient outcomes and reduces the burden of CV disorders. The rationale for the benefit of a more intensive lipid-lowering therapy has been reinforced by the Treating to New Targets (TNT) study, which demonstrated that intensive lipid-lowering therapy with atorvastatin 80 mg resulted in a significant reduction in MACE compared to moderate therapy with atorvastatin 10 mg in patients with stable CAD [51].
In addition to statins, the IMPROVE-IT trial investigated the role of ezetimibe, a cholesterol absorption inhibitor, in further reducing CV risk [36]. The trial enrolled over 18,000 patients with recent ACS and showed that adding ezetimibe led to a 6.4% reduction in the composite endpoint of CV death, major coronary event, or non-fatal stroke compared to statin therapy alone. Despite the relatively modest effect on the outcome, the IMPROVE-IT trial provided important evidence supporting the LDL-C hypothesis and highlighted the incremental benefit of combining other therapies with statins in reducing MACE in patients with recent ACS (Table 2).

Table 2.
Landmark statin trials in secondary prevention after Acute Coronary Syndromes.
4. Evidence on PCSK9 Inhibitors in Post-ACS
In post-acute ACS, and more generally in patients with high and very high CV risk, LDL-C reduction is the foundation of secondary prevention management. Randomized clinical trials have demonstrated that, after an ACS event, early treatment with a high-efficacy statin, such as atorvastatin 80 mg, leads to an early clinical benefit in terms of MACE reduction. Due to the non-negligible rate of ACS patients who do not achieve LDL-C level targets with the use of statin therapy alone, further therapeutic options should be implemented. PCSK9 has been found to be a therapeutic target to reduce LDL-C levels effectively and powerfully. Over the last decades, basic and clinical research have led to the development of two monoclonal antibodies, alirocumab and evolocumab, which are able to lower LDL-C levels and improve prognosis. In addition to high-intensity statin treatment, PCSK9 antibodies have been shown to reduce LDL-C by up to 75% compared to placebo. In the randomized controlled trial ODYSSEY outcome, alirocumab was tested in patients treated with high-intensity statins and a recent ACS (1–12 months) [109]. Patients treated with alirocumab had a lower incidence of the primary endpoint, which was a composite of MACE, including death from CAD, nonfatal acute myocardial infarction (AMI), ischemic stroke, or unstable angina requiring hospitalization. In addition, alirocumab, on top of optimal lipid-lowering treatment, was associated with reduced mortality among patients with more than a three-year follow-up [90]. In this study, patients with greater LDL-C levels at baseline (>100 mg/dL) had the greater benefit in terms of mortality reduction. Alirocumab also reduced lipoprotein (a) levels by 5.0 mg/dL, and Lp(a) reduction predicted lower MACE incidence [110].
In a prespecified analysis of the Further Cardiovascular Outcomes Research With PCSK9 Inhibition in Subjects With Elevated Risk (FOURIER) trial that examined data from 5711 patients with a recent myocardial infarction (<12 months), evolocumab reduced the incidence of the primary endpoint (a composite of CV death, AMI, stroke, coronary revascularization, or hospitalization for unstable angina) and key secondary endpoint (a composite of CV death, AMI, or stroke) by 19% and 25%, respectively [111]. Due to the higher incidence of events among patients with a recent myocardial infarction, in these patients, the event risk reduction at three-year follow-up was greater compared to those who had a myocardial infarction > 12 months before randomization. These results confirm that earlier achievement of lower LDL-C levels confers a greater clinical benefit. The Evolocumab for Early Reduction of LDL Cholesterol Levels in Patients With Acute Coronary Syndromes (EVOPACS) study investigated lipid-lowering treatment with evolocumab 420 mg started during hospitalization for ACS. In this study, patients were randomized to receive evolocumab or placebo in addition to atorvastatin 40 mg. Evolocumab was administered during the index hospitalization, but the interval times from ACS symptoms’ presentation and the first dose of drug administration were not reported. Mean LDL-C levels at enrollment were 136 ± 38 mg/dL. Evolocumab was found to be well tolerated and to lead to a significant LDL-C reduction (mean percentage changes vs. placebo −40.7%; 95% confidence interval (CI) −45.2 to −36.2%; p < 0.001) with >95% of treated patients that achieved recommended LDL-C target levels at week 8 after ACS [33]. The Evolocumab in Acute Coronary Syndrome (EVACS) study [112] is a randomized controlled trial that tested evolocumab 420 mg vs. placebo, on top of high-intensity statins, in patients with non-ST-segment elevation myocardial infarction ( NSTEMI). In this study, evolocumab was administered within 24 hours of presentation. At hospital discharge, the percentage of patients treated with evolocumab that achieved LDL-C levels recommended by 2019 European Society of Cardiology guidelines (<55 mg/dL) was higher than that of patients in the placebo group (65.4% vs. 23.8%, respectively; p < 0.01).
The randomized, sham-controlled, double-blind EPIC-STEMI trial evaluated the change in LDL-C when alirocumab was used in patients with ST-segment elevation myocardial infarction (STEMI) treated with primary percutaneous coronary intervention (PCI). Alirocumab 150 mg administered before primary PCI, at 2 weeks and at 4 weeks led to a 72.9% reduction in LDL-C level at 6 weeks as compared to a 48.1% reduction in the sham-control group (p < 0.001) [34].
A further small placebo-controlled, double-blind study randomized 20 patients 1:1 to receive alirocumab 150 mg or placebo within 24 hours of NSTEMI presentation. At 14 days from treatment administration, in the group managed with alirocumab, a significant reduction in LDL-C level (−64 mg/dL, −96 to −47 mg/dL) was found as compared with the placebo group (+1 mg/dL, −25 to +16 mg/dL) [35].
Overall, available evidence on the use of anti-PCSK9 monoclonal antibodies in the ACS setting consistently shows a powerful and early effect of these drugs in terms of LDL-C reduction and better prognosis (Table 3), without relevant safety issues. These findings support the use of anti-PCSK9 monoclonal antibodies in the early phase of ACS.

Table 3.
Main clinical studies that have assessed the PCSK9 inhibitors in the post-ACS setting.
In more recent years, pharmacological research has led to the development of PCSK9 inhibitors that act by interfering with PCSK9 hepatic synthesis. Inclisiran, a small interfering RNA agent, is a drug in a more advanced phase of development. When tested in patients with ASCVD, inclisiran has been found to reduce LDL-C levels by up to 53% [102]. However, no evidence on the specific setting of ACS or on clinical outcomes is currently available.
The VICTORION-INCEPTION trial is currently ongoing. This is a phase IIIb, randomized, open-label study aimed at assessing inclisiran effectiveness when administered on top of usual care in patients within 5 weeks from an ACS and with LDL-C levels ≥ 70 mg/dL, despite statin treatment [113].
5. Current Guideline Recommendations
Patients who present with ACS are at increased risk of experiencing recurrent CV events, especially within the first year after hospital discharge. LDL-C has been shown to be a causal factor for the development of atherosclerosis, and a strong relationship between pharmacologic LDL-C lowering and a reduction in CV events post-ACS has been shown. According to the ESC/EAS guidelines [25], it has been recommended to initiate a high-intensity statin up to the highest tolerated dose in all statin-naive ACS patients with no contraindication; a 50% LDL-C reduction from baseline value and an LDL-C goal of <1.4 mmol/L (<55 mg/dL) is recommended. In those with recurrent events within 2 years, a goal of <1.0 mmol/L (<40 mg/dL) for LDL-C should be considered.
LDL-C levels tend to decrease during the first 24 h after ACS, and the lower value can be measured 7 days after the event (a mean reduction in LDL-C of 10% approximately); therefore, a lipid profile should be assessed as soon as possible after admission for ACS. LLT should be initiated as soon as possible. The latest ESC/EAS guidelines [25] still recommend a stepwise approach. Lipid levels should be re-evaluated 4–6 weeks after ACS, and if the LDL-C goal is not achieved, a combination with ezetimibe is recommended.
Statins are generally well tolerated; indeed, myopathy and muscle symptoms are not frequently reported. Among patients in whom statins cannot be prescribed due to intolerance or adverse effects, it has been suggested to start with PCSK9 inhibitors in combination with ezetimibe. PCSK9 inhibitors also lower triglycerides, raise HDL-C and apolipoprotein A-I, and lower lipoprotein(a). In patients presenting with ACS already on a high-intensity statin and/or ezetimibe, it should be advisable to prescribe PCSK9 inhibitors before discharge.
The 2018 AHA/ACC Guidelines recommended intensifying the approach to LDL-C reduction in secondary prevention even though their target is different from ours (≤70 mg/dL) [114].
The following ESC guidelines on CVD prevention and NSTEMI [26,115] have not changed the treatment target for LDL-C, confirming the step-by-step approach, also in secondary prevention (Table 4).

Table 4.
International Guidelines Overview.
6. Real-World Data
Many observational studies have been designed to examine the level of hypolipidemic drug treatment in patients with CAD, namely post-acute coronary syndromes (ACS) in the real world, as well as to provide contemporary data on the implementation of guideline recommendations for LLT across different settings and populations, e.g., how this impacts LDL-C goal achievement.
The main studies assessing these items were the European Action on Secondary Prevention through Intervention to Reduce Events (EUROASPIRE) I, II, III, IV, and V studies [116,117,118,119,120], the EU-Wide Cross-Sectional Observational Study of Lipid-Modifying Therapy Use in Secondary and Primary Care (DA VINCI) [121], the DYSIS-China [122], the DYSIS II Study [123], the TARGET study [124], The Hyperlipidaemia Therapy in tERtiary Cardiological cEnTer (TERCET) Registry [125], The Acute Coronary Syndrome Management (ACOSYM) registry [126], the ACS patient pathway project [127], and the HYDRA-ACS registry [128].
In the first EUROASPIRE, only 33% of the patients received LLT [116]. The use of LLT was relatively higher (60.9%) in EUROASPIRE II [117]; however, the most frequently used doses of LLT agents were much lower than the doses of proven effect used in clinical trials [117]. The use of statins was 78% in the EUROASPIRE III [118], with wide variations between countries.
Of patients at high and very high CV risk from the Cegedim Longitudinal Practice Database in Germany from 2011 to 2013, only 35% received current statin treatment [129]. In the Greek TARGET study, at the end of the follow-up, 87.7% of patients remained on statin treatment [124].
EUROASPIRE V [130] highlighted that the percentage of CAD adults receiving statins at ìLDL goal in ACS patients has not been achieved [27,36,131].
There are several factors that impact LDL-C goal achievement after ACS discharge. By and large, they may be differentiated as those related to the patient, those related to physicians, and those related to the socio-sanitary system (Figure 1). High-intensity statins combined with ezetimibe have been shown to improve adherence, so this combination should be preferred at discharge [132,133]. The monthly and yearly administration of PCSK9 antibodies and siRNA, respectively, have been related to improved adherence and prognosis.
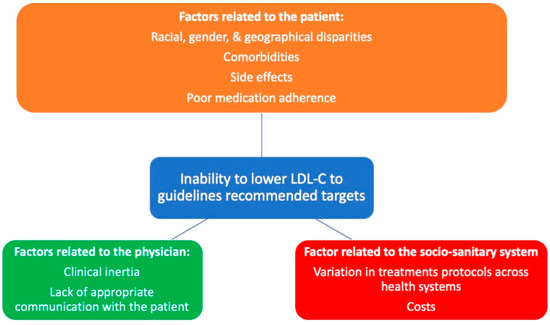
Figure 1.
Factors affecting LDL-C goal achievement.
Nonadherence has been estimated at 59.2% after 1 year [134]. Medication adherence largely influences life-long risk [135], and an increase in CV risk of 5% has been described for 10% of LLT nonadherence [136].
LDL-C control seems better in men than in women [120,123,137,138]. Baseline LDL-C level is obviously negatively associated with goal achievement rate [137]. Regarding common comorbidities, patients with obesity [123], concomitant coronary heart disease (CHD), and peripheral arterial disease (PAD) or diabetes were least likely to reach their target LDL-C goals [139]. However, discordant data about diabetic patients and those with chronic kidney disease (CKD) have been reported [120,123,138]. Better adherence is obviously associated with an improved goal achievement rate [137]. Additionally, patients who quit smoking have a better LDL-goal achievement rate than smokers [123,137], and more patients with recent ACS achieved the LDL-C target (33.8%) compared to chronic CHD patients (21.2%) [122]; this may be a proxy of self-empowerment in facing the postinfarction period. Statin side effects (real or perceived) and intolerance, with consequent treatment withdrawn, may obviously also play a role in the gap between LDL goal and LDL value achieved in clinical practice.
Clinical inertia by the physician (both in starting and reinforcing treatments) appears to be a fundamental factor, too. LDL-C control, in fact, is better in those on a high-intensity LLT compared to those on low- or moderate-intensity LLT [120,123,126,140,141], as well as in those prescribed statin and ezetimibe combinations than in those prescribed intensive statin monotherapy [137,142]. Goal attainment for secondary prevention was 45% for patients on statins only, 53% for those receiving combination therapy with ezetimibe, and 67% for those receiving combination therapy with PCSK9 inhibitors, respectively [121]. Stating a target in discharge documentation was associated with significant improvements in lipid testing and patients achieving LDL-C targets [143].
The role of the sociosanitary system is clear, not only due to variations in protocols and practices across health systems, e.g., with regulatory obstacles (consequent to the high cost of new-generation agents), but also in the availability of cardio-rehabilitation. Patients that have participated in cardiac rehabilitation programs after a CV event, in fact, show the best levels of LDL-C target achievement [144]. In addition, different reimbursement politics may partly explain some geographical variations in undertreatment.
7. Future Perspectives
As previously emphasized, there is a gap between guideline recommendations and current clinical practice. In the real world, a low proportion of patients reach the recommended targets, underlying the need for new therapeutic strategies. Recent studies have demonstrated the safety and efficacy of an early and significant reduction in LDL-C levels in patients with ACS. In an ideal post-ACS scenario, we would need 12 weeks for patients to receive optimal LLT if the stepwise approach suggested by the guidelines is implemented. However, the first 100 days correspond to the most vulnerable phase after an ACS.
A fast-track strategy has been recently proposed for post-ACS patients [11] and those who experienced an AMI within the last 12 months or had multiple previous CV events [145].
Recently, a panel of Italian cardiologists on the use of a mini-Dolphy technique has reported a broad consensus on the early systematic use of combination therapies in post-ACS patients [146]
In-hospital initiation of PCSK9 inhibitors enables achieving LDL-C goals in the majority of patients in the most vulnerable phase.
Musumeci et al. [147] proposed a triple-therapy approach (high-intensity statins, ezetimibe, and PCSK9 inhibitors) immediately after discharge, in those patients who recently experienced an ACS and were considered to be at prohibitive risk due to their clinical, angiographic, and lipidic features, in order to achieve an early and significant LDL-C reduction. This strategy, according to previous data [135,145], is based on the risk profile of patients and takes into account several factors such as multiple CV events, multiple ASCVD localizations, and multivessel CAD. Additionally, a tailored and early approach recently proposed by De Luca et al. [11] suggests the intensive use of LLT and drug refund requirements, also highlighting the importance of short-term follow-up.
Notably, it has been suggested to take into account the expected reduction value for the single drug used.
According to this statement [11], statin-naive patients in the post-ACS period should start high-intensity statin therapy during hospitalization in order to obtain a 50% reduction in LDL-C, adding also ezetimibe [146,148].
Conversely, in those patients previously treated with statins, the type and dose of statin should be considered, and the use of a more-intensive LLT should be evaluated. For intolerant patients, ezetimibe and PCSK9 inhibitor use are advisable [11]
Notably, it is the patients with baseline LDL-C values higher than 100 mg/dL that are expected to benefit from an early combined LLT approach the most. This is due to the fact that these patients are unlikely to lower LDL by more than 55 mg/dL using only high-intensity statins; hence, in this context, a double or triple LLT approach should be reasonable. And now, the “strike early and strong approach” is considered to be the most advisable one [27].
8. Conclusions
In conclusion, gaps between clinical guidelines and clinical practice for lipid management persist across Europe. Too many CAD patients with dyslipidemia are still inadequately treated, and LDL-C control is suboptimal; the available LLT armamentarium, including combination therapy, remains largely underused in high- and very-high-risk patients, leading to suboptimal management of residual risk.
There is a strong need for novel strategies to intensify lipid-modifying management and improve long-term LDL-C control after ACS. More-effective strategies for the management of dyslipidemia are needed in order to minimize the discrepancy between real-world clinical practice and current guideline recommendations.
Author Contributions
Conceptualization, F.L., C.M.R., M.G.A., A.F.A., M.M.G. and F.O.; methodology, G.C., I.D.M., A.P. and C.D.N.; software, C.M.R.; validation, C.M.R.; formal analysis, R.C. and R.R.; investigation, R.C. and R.R.; resources, R.C. and R.R.; data curation, R.C. and R.R.; writing—original draft preparation, F.L., M.G.A., A.F.A., S.A.D.F., C.R., R.C., R.R., A.P., C.D.N. and I.D.M.; writing—review and editing, S.A.D.F., F.L., C.R., M.G. and F.C.; visualization, F.L., M.G.A., C.M.R. and F.C.; supervision, F.L., M.G., M.M.G., F.C. and F.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
We thank Carol Wintheringham for the English editing.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Roth, G.A.; Johnson, C.; Abajobir, A.; Abd-Allah, F.; Abera, S.F.; Abyu, G.; Ahmed, M.; Aksut, B.; Alam, T.; Alam, K.; et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J. Am. Coll. Cardiol. 2017, 70, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Fuster, V.; Kovacic, J.C. Acute coronary syndromes: Pathology, diagnosis, genetics, prevention, and treatment. Circ. Res. 2014, 114, 1847–1851. [Google Scholar] [CrossRef] [PubMed]
- Puymirat, E.; Simon, T.; Cayla, G.; Cottin, Y.; Elbaz, M.; Coste, P.; Lemesle, G.; Motreff, P.; Popovic, B.; Khalife, K.; et al. Acute Myocardial Infarction: Changes in Patient Characteristics, Management, and 6-Month Outcomes Over a Period of 20 Years in the FAST-MI Program (French Registry of Acute ST-Elevation or Non-ST-Elevation Myocardial Infarction) 1995 to 2015. Circulation 2017, 136, 1908–1919. [Google Scholar] [CrossRef] [PubMed]
- Jernberg, T.; Hasvold, P.; Henriksson, M.; Hjelm, H.; Thuresson, M.; Janzon, M. Cardiovascular risk in post-myocardial infarction patients: Nationwide real world data demonstrate the importance of a long-term perspective. Eur. Heart J. 2015, 36, 1163–1170. [Google Scholar] [CrossRef] [PubMed]
- Fox, K.A.; Carruthers, K.F.; Dunbar, D.R.; Graham, C.; Manning, J.R.; De Raedt, H.; Buysschaert, I.; Lambrechts, D.; Van de Werf, F. Underestimated and under-recognized: The late consequences of acute coronary syndrome (GRACE UK-Belgian Study). Eur. Heart J. 2010, 31, 2755–2764. [Google Scholar] [CrossRef]
- Kornowski, R.; Mehran, R.; Dangas, G.; Nikolsky, E.; Assali, A.; Claessen, B.E.; Gersh, B.J.; Wong, S.C.; Witzenbichler, B.; Guagliumi, G.; et al. Prognostic impact of staged versus “one-time” multivessel percutaneous intervention in acute myocardial infarction: Analysis from the HORIZONS-AMI (harmonizing outcomes with revascularization and stents in acute myocardial infarction) trial. J. Am. Coll. Cardiol. 2011, 58, 704–711. [Google Scholar] [CrossRef]
- Palmerini, T.; Della Riva, D.; Biondi-Zoccai, G.; Leon, M.B.; Serruys, P.W.; Smits, P.C.; von Birgelen, C.; Ben-Yehuda, O.; Généreux, P.; Bruno, A.G.; et al. Mortality Following Nonemergent, Uncomplicated Target Lesion Revascularization After Percutaneous Coronary Intervention: An Individual Patient Data Pooled Analysis of 21 Randomized Trials and 32,524 Patients. JACC Cardiovasc. Interv. 2018, 11, 892–902. [Google Scholar] [CrossRef]
- Giustino, G.; Serruys, P.W.; Sabik, J.F., 3rd; Mehran, R.; Maehara, A.; Puskas, J.D.; Simonton, C.A.; Lembo, N.J.; Kandzari, D.E.; Morice, M.C.; et al. Mortality After Repeat Revascularization Following PCI or CABG for Left Main Disease: The EXCEL Trial. JACC Cardiovasc. Interv. 2020, 13, 375–387. [Google Scholar] [CrossRef]
- Parasca, C.A.; Head, S.J.; Milojevic, M.; Mack, M.J.; Serruys, P.W.; Morice, M.C.; Mohr, F.W.; Feldman, T.E.; Colombo, A.; Dawkins, K.D.; et al. Incidence, Characteristics, Predictors, and Outcomes of Repeat Revascularization After Percutaneous Coronary Intervention and Coronary Artery Bypass Grafting: The SYNTAX Trial at 5 Years. JACC Cardiovasc. Interv. 2016, 9, 2493–2507. [Google Scholar] [CrossRef]
- Mehran, R.; Pocock, S.; Nikolsky, E.; Dangas, G.D.; Clayton, T.; Claessen, B.E.; Caixeta, A.; Feit, F.; Manoukian, S.V.; White, H.; et al. Impact of bleeding on mortality after percutaneous coronary intervention results from a patient-level pooled analysis of the REPLACE-2 (randomized evaluation of PCI linking angiomax to reduced clinical events), ACUITY (acute catheterization and urgent intervention triage strategy), and HORIZONS-AMI (harmonizing outcomes with revascularization and stents in acute myocardial infarction) trials. JACC Cardiovasc. Interv. 2011, 4, 654–664. [Google Scholar] [CrossRef]
- De Luca, L.; Riccio, C.; Navazio, A.; Valente, S.; Cipriani, M.; Corda, M.; De Nardo, A.; Francese, G.M.; Napoletano, C.; Tizzani, E.; et al. ANMCO Position paper: Management of hypercholesterolemia in patients with acute coronary syndrome. G. Ital. Cardiol. 2023, 24, 229–240. [Google Scholar] [CrossRef] [PubMed]
- Costanza, M.C.; Cayanis, E.; Ross, B.M.; Flaherty, M.S.; Alvin, G.B.; Das, K.; Morabia, A. Relative contributions of genes, environment, and interactions to blood lipid concentrations in a general adult population. Am. J. Epidemiol. 2005, 161, 714–724. [Google Scholar] [CrossRef] [PubMed]
- Ference, B.A.; Graham, I.; Tokgozoglu, L.; Catapano, A.L. Impact of Lipids on Cardiovascular Health. J. Am. Coll. Cardiol. 2018, 72, 1141–1156. [Google Scholar] [CrossRef]
- Ference, B.A.; Ginsberg, H.N.; Graham, I.; Ray, K.K.; Packard, C.J.; Bruckert, E.; Hegele, R.A.; Krauss, R.M.; Raal, F.J.; Schunkert, H.; et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 2017, 38, 2459–2472. [Google Scholar] [CrossRef]
- Libby, P. Inflammation during the life cycle of the atherosclerotic plaque. Cardiovasc. Res. 2021, 117, 2525–2536. [Google Scholar] [CrossRef] [PubMed]
- Soehnlein, O.; Libby, P. Targeting inflammation in atherosclerosis—From experimental insights to the clinic. Nat. Rev. Drug Discov. 2021, 20, 589–610. [Google Scholar] [CrossRef] [PubMed]
- Bernelot Moens, S.J.; Neele, A.E.; Kroon, J.; van der Valk, F.M.; Van den Bossche, J.; Hoeksema, M.A.; Hoogeveen, R.M.; Schnitzler, J.G.; Baccara-Dinet, M.T.; Manvelian, G.; et al. PCSK9 monoclonal antibodies reverse the pro-inflammatory profile of monocytes in familial hypercholesterolaemia. Eur. Heart J. 2017, 38, 1584–1593. [Google Scholar] [CrossRef] [PubMed]
- Stiekema, L.C.A.; Willemsen, L.; Kaiser, Y.; Prange, K.H.M.; Wareham, N.J.; Boekholdt, S.M.; Kuijk, C.; de Winther, M.P.J.; Voermans, C.; Nahrendorf, M.; et al. Impact of cholesterol on proinflammatory monocyte production by the bone marrow. Eur. Heart J. 2021, 42, 4309–4320. [Google Scholar] [CrossRef]
- Nicholls, S.J.; Kataoka, Y.; Nissen, S.E.; Prati, F.; Windecker, S.; Puri, R.; Hucko, T.; Aradi, D.; Herrman, J.R.; Hermanides, R.S.; et al. Effect of Evolocumab on Coronary Plaque Phenotype and Burden in Statin-Treated Patients Following Myocardial Infarction. JACC Cardiovasc. Imaging 2022, 15, 1308–1321. [Google Scholar] [CrossRef]
- Räber, L.; Ueki, Y.; Otsuka, T.; Losdat, S.; Häner, J.D.; Lonborg, J.; Fahrni, G.; Iglesias, J.F.; van Geuns, R.J.; Ondracek, A.S.; et al. Effect of Alirocumab Added to High-Intensity Statin Therapy on Coronary Atherosclerosis in Patients With Acute Myocardial Infarction: The PACMAN-AMI Randomized Clinical Trial. JAMA 2022, 327, 1771–1781. [Google Scholar] [CrossRef]
- Cannon, C.P.; Braunwald, E.; McCabe, C.H.; Rader, D.J.; Rouleau, J.L.; Belder, R.; Joyal, S.V.; Hill, K.A.; Pfeffer, M.A.; Skene, A.M. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N. Engl. J. Med. 2004, 350, 1495–1504. [Google Scholar] [CrossRef] [PubMed]
- Giugliano, R.P.; Pedersen, T.R.; Park, J.G.; De Ferrari, G.M.; Gaciong, Z.A.; Ceska, R.; Toth, K.; Gouni-Berthold, I.; Lopez-Miranda, J.; Schiele, F.; et al. Clinical efficacy and safety of achieving very low LDL-cholesterol concentrations with the PCSK9 inhibitor evolocumab: A prespecified secondary analysis of the FOURIER trial. Lancet 2017, 390, 1962–1971. [Google Scholar] [CrossRef] [PubMed]
- Baigent, C.; Blackwell, L.; Emberson, J.; Holland, L.E.; Reith, C.; Bhala, N.; Peto, R.; Barnes, E.H.; Keech, A.; Simes, J.; et al. Efficacy and safety of more intensive lowering of LDL cholesterol: A meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 2010, 376, 1670–1681. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, J.L.; Brown, M.S. The LDL receptor. Arterioscler. Thromb. Vasc. Biol. 2009, 29, 431–438. [Google Scholar] [CrossRef] [PubMed]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef]
- Krychtiuk, K.A.; Ahrens, I.; Drexel, H.; Halvorsen, S.; Hassager, C.; Huber, K.; Kurpas, D.; Niessner, A.; Schiele, F.; Semb, A.G.; et al. Acute LDL-C reduction post ACS: Strike early and strike strong: From evidence to clinical practice. A clinical consensus statement of the Association for Acute CardioVascular Care (ACVC), in collaboration with the European Association of Preventive Cardiology (EAPC) and the European Society of Cardiology Working Group on Cardiovascular Pharmacotherapy. Eur. Heart J. Acute Cardiovasc. Care 2022, 11, 939–949. [Google Scholar] [CrossRef]
- Liem, A.; van Boven, A.J.; Withagen, A.P.; Robles de Medina, R.M.; Veeger, N.J.; Tijssen, J.G. Fluvastatin in acute myocardial infarction: Effects on early and late ischemia and events: The FLORIDA trial. Circulation 2000, 102, 2672. [Google Scholar] [CrossRef]
- Thompson, P.L.; Meredith, I.; Amerena, J.; Campbell, T.J.; Sloman, J.G.; Harris, P.J. Effect of pravastatin compared with placebo initiated within 24 hours of onset of acute myocardial infarction or unstable angina: The Pravastatin in Acute Coronary Treatment (PACT) trial. Am. Heart J. 2004, 148, e2. [Google Scholar] [CrossRef]
- de Lemos, J.A.; Blazing, M.A.; Wiviott, S.D.; Lewis, E.F.; Fox, K.A.; White, H.D.; Rouleau, J.L.; Pedersen, T.R.; Gardner, L.H.; Mukherjee, R.; et al. Early intensive vs a delayed conservative simvastatin strategy in patients with acute coronary syndromes: Phase Z of the A to Z trial. JAMA 2004, 292, 1307–1316. [Google Scholar] [CrossRef]
- Schwartz, G.G.; Olsson, A.G.; Ezekowitz, M.D.; Ganz, P.; Oliver, M.F.; Waters, D.; Zeiher, A.; Chaitman, B.R.; Leslie, S.; Stern, T.; et al. Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: The MIRACL study: A randomized controlled trial. JAMA 2001, 285, 1711–1718. [Google Scholar] [CrossRef]
- Nicholls, S.; Lincoff, A.M.; Bays, H.E.; Cho, L.; Grobbee, D.E.; Kastelein, J.J.; Libby, P.; Moriarty, P.M.; Plutzky, J.; Ray, K.K. Rationale and design of the CLEAR-outcomes trial: Evaluating the effect of bempedoic acid on cardiovascular events in patients with statin intolerance. Am. Heart J. 2021, 235, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Koskinas, K.C.; Windecker, S.; Pedrazzini, G.; Mueller, C.; Cook, S.; Matter, C.M.; Muller, O.; Häner, J.; Gencer, B.; Crljenica, C.; et al. Evolocumab for Early Reduction of LDL Cholesterol Levels in Patients With Acute Coronary Syndromes (EVOPACS). J. Am. Coll. Cardiol. 2019, 74, 2452–2462. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.R.; Pare, G.; Lonn, E.M.; Jolly, S.S.; Natarajan, M.K.; Pinilla-Echeverri, N.; Schwalm, J.D.; Sheth, T.N.; Sibbald, M.; Tsang, M.; et al. Effects of routine early treatment with PCSK9 inhibitors in patients undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: A randomised, double-blind, sham-controlled trial. EuroIntervention 2022, 18, e888–e896. [Google Scholar] [CrossRef] [PubMed]
- Trankle, C.R.; Wohlford, G.; Buckley, L.F.; Kadariya, D.; Ravindra, K.; Markley, R.; Park, T.S.; Potere, N.; Van Tassell, B.W.; Abbate, A. Alirocumab in Acute Myocardial Infarction: Results From the Virginia Commonwealth University Alirocumab Response Trial (VCU-AlirocRT). J. Cardiovasc. Pharmacol. 2019, 74, 266–269. [Google Scholar] [CrossRef] [PubMed]
- Cannon, C.P.; Blazing, M.A.; Giugliano, R.P.; McCagg, A.; White, J.A.; Theroux, P.; Darius, H.; Lewis, B.S.; Ophuis, T.O.; Jukema, J.W.; et al. Ezetimibe Added to Statin Therapy after Acute Coronary Syndromes. N. Engl. J. Med. 2015, 372, 2387–2397. [Google Scholar] [CrossRef]
- Baigent, C.; Keech, A.; Kearney, P.M.; Blackwell, L.; Buck, G.; Pollicino, C.; Kirby, A.; Sourjina, T.; Peto, R.; Collins, R.; et al. Efficacy and safety of cholesterol-lowering treatment: Prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005, 366, 1267–1278. [Google Scholar] [CrossRef]
- Lloyd-Jones, D.M.; Morris, P.B.; Ballantyne, C.M.; Birtcher, K.K.; Daly, D.D.; DePalma, S.M.; Minissian, M.B.; Orringer, C.E.; Smith, S.C. 2017 Focused Update of the 2016 ACC Expert Consensus Decision Pathway on the Role of Non-Statin Therapies for LDL-Cholesterol Lowering in the Management of Atherosclerotic Cardiovascular Disease Risk. J. Am. Coll. Cardiol. 2017, 70, 1785–1822. [Google Scholar] [CrossRef]
- Manzoni, M.; Rollini, M. Biosynthesis and biotechnological production of statins by filamentous fungi and application of these cholesterol-lowering drugs. Appl. Microbiol. Biotechnol. 2002, 58, 555–564. [Google Scholar] [CrossRef]
- Trub, A.G.; Wagner, G.R.; Anderson, K.A.; Crown, S.B.; Zhang, G.F.; Thompson, J.W.; Ilkayeva, O.R.; Stevens, R.D.; Grimsrud, P.A.; Kulkarni, R.A.; et al. Statin therapy inhibits fatty acid synthase via dynamic protein modifications. Nat. Commun. 2022, 13, 2542. [Google Scholar] [CrossRef]
- Burnett, J.R.; Barrett, P.H.; Vicini, P.; Miller, D.B.; Telford, D.E.; Kleinstiver, S.J.; Huff, M.W. The HMG-CoA reductase inhibitor atorvastatin increases the fractional clearance rate of postprandial triglyceride-rich lipoproteins in miniature pigs. Arter. Thromb. Vasc. Biol. 1998, 18, 1906–1914. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Arnaud, C.; Veillard, N.R.; Mach, F. Cholesterol-independent effects of statins in inflammation, immunomodulation and atherosclerosis. Curr. Drug Targets Cardiovasc. Haematol. Disord. 2005, 5, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Liao, J.K. Pleiotropic effects of statins—Basic research and clinical perspectives. Circ. J. 2010, 74, 818–826. [Google Scholar] [CrossRef] [PubMed]
- Silverman, M.G.; Ference, B.A.; Im, K.; Wiviott, S.D.; Giugliano, R.P.; Grundy, S.M.; Braunwald, E.; Sabatine, M.S. Association Between Lowering LDL-C and Cardiovascular Risk Reduction Among Different Therapeutic Interventions: A Systematic Review and Meta-analysis. JAMA 2016, 316, 1289–1297. [Google Scholar] [CrossRef]
- Schulz, R. Pleiotropic effects of statins. J. Am. Coll. Cardiol. 2005, 45, 1292–1294. [Google Scholar] [CrossRef][Green Version]
- Buchwald, H.; Varco, R.L.; Matts, J.P.; Long, J.M.; Fitch, L.L.; Campbell, G.S.; Pearce, M.B.; Yellin, A.E.; Edmiston, W.A.; Smink, R.D., Jr.; et al. Effect of partial ileal bypass surgery on mortality and morbidity from coronary heart disease in patients with hypercholesterolemia. Report of the Program on the Surgical Control of the Hyperlipidemias (POSCH). N. Engl. J. Med. 1990, 323, 946–955. [Google Scholar] [CrossRef]
- Lefer, D.J. Statins as potent antiinflammatory drugs. Circulation 2002, 106, 2041–2042. [Google Scholar] [CrossRef]
- Albert, M.A.; Danielson, E.; Rifai, N.; Ridker, P.M. Effect of statin therapy on C-reactive protein levels: The pravastatin inflammation/CRP evaluation (PRINCE): A randomized trial and cohort study. JAMA 2001, 286, 64–70. [Google Scholar] [CrossRef]
- Ridker, P.M.; Rifai, N.; Pfeffer, M.A.; Sacks, F.M.; Moye, L.A.; Goldman, S.; Flaker, G.C.; Braunwald, E. Inflammation, pravastatin, and the risk of coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events (CARE) Investigators. Circulation 1998, 98, 839–844. [Google Scholar] [CrossRef]
- Ridker, P.M.; Danielson, E.; Fonseca, F.A.; Genest, J.; Gotto, A.M., Jr.; Kastelein, J.J.; Koenig, W.; Libby, P.; Lorenzatti, A.J.; MacFadyen, J.G.; et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N. Engl. J. Med. 2008, 359, 2195–2207. [Google Scholar] [CrossRef]
- LaRosa, J.C.; Grundy, S.M.; Waters, D.D.; Shear, C.; Barter, P.; Fruchart, J.C.; Gotto, A.M.; Greten, H.; Kastelein, J.J.; Shepherd, J.; et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N. Engl. J. Med. 2005, 352, 1425–1435. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, T.R.; Faergeman, O.; Kastelein, J.J.; Olsson, A.G.; Tikkanen, M.J.; Holme, I.; Larsen, M.L.; Bendiksen, F.S.; Lindahl, C.; Szarek, M.; et al. High-dose atorvastatin vs usual-dose simvastatin for secondary prevention after myocardial infarction: The IDEAL study: A randomized controlled trial. JAMA 2005, 294, 2437–2445. [Google Scholar] [CrossRef] [PubMed]
- Cannon, C.P.; Steinberg, B.A.; Murphy, S.A.; Mega, J.L.; Braunwald, E. Meta-analysis of cardiovascular outcomes trials comparing intensive versus moderate statin therapy. J. Am. Coll. Cardiol. 2006, 48, 438–445. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Plutzky, J.; Skentzos, S.; Morrison, F.; Mar, P.; Shubina, M.; Turchin, A. Discontinuation of statins in routine care settings: A cohort study. Ann. Intern. Med. 2013, 158, 526–534. [Google Scholar] [CrossRef] [PubMed]
- Mancini, G.B.; Baker, S.; Bergeron, J.; Fitchett, D.; Frohlich, J.; Genest, J.; Gupta, M.; Hegele, R.A.; Ng, D.; Pearson, G.J.; et al. Diagnosis, Prevention, and Management of Statin Adverse Effects and Intolerance: Canadian Consensus Working Group Update (2016). Can. J. Cardiol. 2016, 32, S35–S65. [Google Scholar] [CrossRef]
- Lin, I.; Sung, J.; Sanchez, R.J.; Mallya, U.G.; Friedman, M.; Panaccio, M.; Koren, A.; Neumann, P.; Menzin, J. Patterns of Statin Use in a Real-World Population of Patients at High Cardiovascular Risk. J. Manag. Care Spec. Pharm. 2016, 22, 685–698. [Google Scholar] [CrossRef]
- Cheeley, M.K.; Saseen, J.J.; Agarwala, A.; Ravilla, S.; Ciffone, N.; Jacobson, T.A.; Dixon, D.L.; Maki, K.C. NLA scientific statement on statin intolerance: A new definition and key considerations for ASCVD risk reduction in the statin intolerant patient. J. Clin. Lipidol. 2022, 16, 361–375. [Google Scholar] [CrossRef]
- Tong, L.S.; Hu, H.T.; Zhang, S.; Yan, S.Q.; Lou, M. Statin withdrawal beyond acute phase affected outcome of thrombolytic stroke patients: An observational retrospective study. Medicine 2015, 94, e779. [Google Scholar] [CrossRef]
- Serban, M.-C.; Colantonio, L.D.; Manthripragada, A.D.; Monda, K.L.; Bittner, V.A.; Banach, M.; Chen, L.; Huang, L.; Dent, R.; Kent, S.T.; et al. Statin Intolerance and Risk of Coronary Heart Events and All-Cause Mortality Following Myocardial Infarction. J. Am. Coll. Cardiol. 2017, 69, 1386–1395. [Google Scholar] [CrossRef]
- Siddiqui, M.K.; Maroteau, C.; Veluchamy, A.; Tornio, A.; Tavendale, R.; Carr, F.; Abelega, N.U.; Carr, D.; Bloch, K.; Hallberg, P.; et al. A common missense variant of LILRB5 is associated with statin intolerance and myalgia. Eur. Heart J. 2017, 38, 3569–3575. [Google Scholar] [CrossRef]
- Preiss, D.; Seshasai, S.R.; Welsh, P.; Murphy, S.A.; Ho, J.E.; Waters, D.D.; DeMicco, D.A.; Barter, P.; Cannon, C.P.; Sabatine, M.S.; et al. Risk of incident diabetes with intensive-dose compared with moderate-dose statin therapy: A meta-analysis. JAMA 2011, 305, 2556–2564. [Google Scholar] [CrossRef]
- Ginsberg, H.N.; Elam, M.B.; Lovato, L.C.; Crouse, J.R., 3rd; Leiter, L.A.; Linz, P.; Friedewald, W.T.; Buse, J.B.; Gerstein, H.C.; Probstfield, J.; et al. Effects of combination lipid therapy in type 2 diabetes mellitus. N. Engl. J. Med. 2010, 362, 1563–1574. [Google Scholar] [CrossRef] [PubMed]
- Nutescu, E.A.; Shapiro, N.L. Ezetimibe: A selective cholesterol absorption inhibitor. Pharmacotherapy 2003, 23, 1463–1474. [Google Scholar] [CrossRef] [PubMed]
- Xie, P.; Jia, L.; Ma, Y.; Ou, J.; Miao, H.; Wang, N.; Guo, F.; Yazdanyar, A.; Jiang, X.C.; Yu, L. Ezetimibe inhibits hepatic Niemann-Pick C1-Like 1 to facilitate macrophage reverse cholesterol transport in mice. Arter. Thromb. Vasc. Biol. 2013, 33, 920–925. [Google Scholar] [CrossRef] [PubMed]
- Pirillo, A.; Catapano, A.L.; Norata, G.D. Niemann-Pick C1-Like 1 (NPC1L1) Inhibition and Cardiovascular Diseases. Curr. Med. Chem. 2016, 23, 983–999. [Google Scholar] [CrossRef]
- Morrone, D.; Weintraub, W.S.; Toth, P.P.; Hanson, M.E.; Lowe, R.S.; Lin, J.; Shah, A.K.; Tershakovec, A.M. Lipid-altering efficacy of ezetimibe plus statin and statin monotherapy and identification of factors associated with treatment response: A pooled analysis of over 21,000 subjects from 27 clinical trials. Atherosclerosis 2012, 223, 251–261. [Google Scholar] [CrossRef]
- Ballantyne, C.M.; Banach, M.; Mancini, G.B.J.; Lepor, N.E.; Hanselman, J.C.; Zhao, X.; Leiter, L.A. Efficacy and safety of bempedoic acid added to ezetimibe in statin-intolerant patients with hypercholesterolemia: A randomized, placebo-controlled study. Atherosclerosis 2018, 277, 195–203. [Google Scholar] [CrossRef]
- Oyama, K.; Giugliano, R.P.; Blazing, M.A.; Park, J.G.; Tershakovec, A.M.; Sabatine, M.S.; Cannon, C.P.; Braunwald, E. Baseline Low-Density Lipoprotein Cholesterol and Clinical Outcomes of Combining Ezetimibe With Statin Therapy in IMPROVE-IT. J. Am. Coll. Cardiol. 2021, 78, 1499–1507. [Google Scholar] [CrossRef]
- Giugliano, R.P.; Cannon, C.P.; Blazing, M.A.; Nicolau, J.C.; Corbalán, R.; Špinar, J.; Park, J.G.; White, J.A.; Bohula, E.A.; Braunwald, E. Benefit of Adding Ezetimibe to Statin Therapy on Cardiovascular Outcomes and Safety in Patients With Versus Without Diabetes Mellitus: Results From IMPROVE-IT (Improved Reduction of Outcomes: Vytorin Efficacy International Trial). Circulation 2018, 137, 1571–1582. [Google Scholar] [CrossRef]
- Colivicchi, F.; Di Fusco, S.A.; Scicchitano, P.; Caldarola, P.; Murrone, A.; Valente, S.; Urbinati, S.; Roncon, L.; Amodeo, V.; Aspromonte, N. Updated clinical evidence and place in therapy of bempedoic acid for hypercholesterolemia: ANMCO position paper. J. Cardiovasc. Med. 2021, 22, 162–171. [Google Scholar] [CrossRef]
- Kosmas, C.E.; Pantou, D.; Sourlas, A.; Papakonstantinou, E.J.; Echavarria Uceta, R.; Guzman, E. New and emerging lipid-modifying drugs to lower LDL cholesterol. Drugs Context 2021, 10, 2021-8-3. [Google Scholar] [CrossRef] [PubMed]
- Filippov, S.; Pinkosky, S.L.; Lister, R.J.; Pawloski, C.; Hanselman, J.C.; Cramer, C.T.; Srivastava, R.A.K.; Hurley, T.R.; Bradshaw, C.D.; Spahr, M.A.; et al. ETC-1002 regulates immune response, leukocyte homing, and adipose tissue inflammation via LKB1-dependent activation of macrophage AMPK. J. Lipid Res. 2013, 54, 2095–2108. [Google Scholar] [CrossRef] [PubMed]
- Laufs, U.; Banach, M.; Mancini, G.B.J.; Gaudet, D.; Bloedon, L.T.; Sterling, L.R.; Kelly, S.; Stroes, E.S.G. Efficacy and Safety of Bempedoic Acid in Patients With Hypercholesterolemia and Statin Intolerance. J. Am. Heart Assoc. 2019, 8, e011662. [Google Scholar] [CrossRef] [PubMed]
- Ray, K.K.; Bays, H.E.; Catapano, A.L.; Lalwani, N.D.; Bloedon, L.T.; Sterling, L.R.; Robinson, P.L.; Ballantyne, C.M. Safety and Efficacy of Bempedoic Acid to Reduce LDL Cholesterol. N. Engl. J. Med. 2019, 380, 1022–1032. [Google Scholar] [CrossRef]
- Ballantyne, C.M.; Banach, M.; Bays, H.E.; Catapano, A.L.; Laufs, U.; Stroes, E.S.G.; Robinson, P.; Lei, L.; Ray, K.K. Long-Term Safety and Efficacy of Bempedoic Acid in Patients With Atherosclerotic Cardiovascular Disease and/or Heterozygous Familial Hypercholesterolemia (from the CLEAR Harmony Open-Label Extension Study). Am. J. Cardiol. 2022, 174, 1–11. [Google Scholar] [CrossRef]
- Sirtori, C.R.; Yamashita, S.; Greco, M.F.; Corsini, A.; Watts, G.F.; Ruscica, M. Recent advances in synthetic pharmacotherapies for dyslipidaemias. Eur. J. Prev. Cardiol. 2020, 27, 1576–1596. [Google Scholar] [CrossRef]
- Nissen, S.E.; Lincoff, A.M.; Brennan, D.; Ray, K.K.; Mason, D.; Kastelein, J.J.P.; Thompson, P.D.; Libby, P.; Cho, L.; Plutzky, J.; et al. Bempedoic Acid and Cardiovascular Outcomes in Statin-Intolerant Patients. N. Engl. J. Med. 2023, 388, 1353–1364. [Google Scholar] [CrossRef]
- Tibolla, G.; Norata, G.D.; Artali, R.; Meneghetti, F.; Catapano, A.L. Proprotein convertase subtilisin/kexin type 9 (PCSK9): From structure-function relation to therapeutic inhibition. Nutr. Metab. Cardiovasc. Dis. 2011, 21, 835–843. [Google Scholar] [CrossRef]
- Ferri, N. Phage display for targeting PCSK9. EBioMedicine 2021, 65, 103267. [Google Scholar] [CrossRef]
- Nozue, T. Lipid Lowering Therapy and Circulating PCSK9 Concentration. J. Atheroscler. Thromb. 2017, 24, 895–907. [Google Scholar] [CrossRef]
- Bergeron, N.; Phan, B.A.; Ding, Y.; Fong, A.; Krauss, R.M. Proprotein convertase subtilisin/kexin type 9 inhibition: A new therapeutic mechanism for reducing cardiovascular disease risk. Circulation 2015, 132, 1648–1666. [Google Scholar] [CrossRef]
- Guedeney, P.; Giustino, G.; Sorrentino, S.; Claessen, B.E.; Camaj, A.; Kalkman, D.N.; Vogel, B.; Sartori, S.; De Rosa, S.; Baber, U.; et al. Efficacy and safety of alirocumab and evolocumab: A systematic review and meta-analysis of randomized controlled trials. Eur. Heart J. 2019, 43, e17–e25. [Google Scholar] [CrossRef]
- Nicholls, S.J.; Puri, R.; Anderson, T.; Ballantyne, C.M.; Cho, L.; Kastelein, J.J.; Koenig, W.; Somaratne, R.; Kassahun, H.; Yang, J.; et al. Effect of Evolocumab on Progression of Coronary Disease in Statin-Treated Patients: The GLAGOV Randomized Clinical Trial. JAMA 2016, 316, 2373–2384. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Lepor, N.E.; Cantón, G.; Contreras, L.; Hippe, D.S.; Isquith, D.A.; Balu, N.; Kedan, I.; Simonini, A.A.; Yuan, C.; et al. Serial magnetic resonance imaging detects a rapid reduction in plaque lipid content under PCSK9 inhibition with alirocumab. Int. J. Cardiovasc. Imaging 2021, 37, 1415–1422. [Google Scholar] [CrossRef] [PubMed]
- Lepor, N.E.; Sun, J.; Canton, G.; Contreras, L.; Hippe, D.S.; Isquith, D.A.; Balu, N.; Kedan, I.; Simonini, A.A.; Yuan, C.; et al. Regression in carotid plaque lipid content and neovasculature with PCSK9 inhibition: A time course study. Atherosclerosis 2021, 327, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Aranzulla, T.C.; Piazza, S.; Ricotti, A.; Musumeci, G.; Gaggiano, A. CARotid plaqUe StabilizatiOn and regression with evolocumab: Rationale and design of the CARUSO study. Catheter. Cardiovasc. Interv. 2021, 98, E115–E121. [Google Scholar] [CrossRef] [PubMed]
- Nicholls, S.J.; Nissen, S.E.; Prati, F.; Windecker, S.; Kataoka, Y.; Puri, R.; Hucko, T.; Kassahun, H.; Liao, J.; Somaratne, R.; et al. Assessing the impact of PCSK9 inhibition on coronary plaque phenotype with optical coherence tomography: Rationale and design of the randomized, placebo-controlled HUYGENS study. Cardiovasc. Diagn. Ther. 2021, 11, 120–129. [Google Scholar] [CrossRef]
- Khvorova, A. Oligonucleotide Therapeutics—A New Class of Cholesterol-Lowering Drugs. N. Engl. J. Med. 2017, 376, 4–7. [Google Scholar] [CrossRef]
- Merćep, I.; Friščić, N.; Strikić, D.; Reiner, Ž. Advantages and Disadvantages of Inclisiran: A Small Interfering Ribonucleic Acid Molecule Targeting PCSK9-A Narrative Review. Cardiovasc. Ther. 2022, 2022, 8129513. [Google Scholar] [CrossRef]
- Ray, K.K.; Stoekenbroek, R.M.; Kallend, D.; Nishikido, T.; Leiter, L.A.; Landmesser, U.; Wright, R.S.; Wijngaard, P.L.; Kastelein, J.J. Effect of 1 or 2 doses of inclisiran on low-density lipoprotein cholesterol levels: One-year follow-up of the ORION-1 randomized clinical trial. JAMA Cardiol. 2019, 4, 1067–1075. [Google Scholar] [CrossRef]
- Di Fusco, S.A.; Maggioni, A.P.; Bernelli, C.; Perone, F.; De Marzo, V.; Conte, E.; Musella, F.; Uccello, G.; De Luca, L.; Gabrielli, D. Inclisiran: A New Pharmacological Approach for Hypercholesterolemia. Rev. Cardiovasc. Med. 2022, 23, 375. [Google Scholar] [CrossRef]
- Hovingh, G.K.; Lepor, N.E.; Kallend, D.; Stoekenbroek, R.M.; Wijngaard, P.L.J.; Raal, F.J. Inclisiran Durably Lowers Low-Density Lipoprotein Cholesterol and Proprotein Convertase Subtilisin/Kexin Type 9 Expression in Homozygous Familial Hypercholesterolemia: The ORION-2 Pilot Study. Circulation 2020, 141, 1829–1831. [Google Scholar] [CrossRef] [PubMed]
- Leiter, L.A.; Teoh, H.; Kallend, D.; Wright, R.S.; Landmesser, U.; Wijngaard, P.L.J.; Kastelein, J.J.P.; Ray, K.K. Inclisiran Lowers LDL-C and PCSK9 Irrespective of Diabetes Status: The ORION-1 Randomized Clinical Trial. Diabetes Care 2019, 42, 173–176. [Google Scholar] [CrossRef] [PubMed]
- Ray, K.K.; Landmesser, U.; Leiter, L.A.; Kallend, D.; Dufour, R.; Karakas, M.; Hall, T.; Troquay, R.P.; Turner, T.; Visseren, F.L.; et al. Inclisiran in Patients at High Cardiovascular Risk with Elevated LDL Cholesterol. N. Engl. J. Med. 2017, 376, 1430–1440. [Google Scholar] [CrossRef] [PubMed]
- Koenig, W.; Ray, K.K.; Landmesser, U.; Leiter, L.A.; Schwartz, G.G.; Wright, R.S.; Conde, L.G.; Han, J.; Raal, F.J. Efficacy and safety of inclisiran in patients with cerebrovascular disease: ORION-9, ORION-10, and ORION-11. Am. J. Prev. Cardiol. 2023, 14, 100503. [Google Scholar] [CrossRef] [PubMed]
- Wright, R.S.; Collins, M.G.; Stoekenbroek, R.M.; Robson, R.; Wijngaard, P.L.; Landmesser, U.; Leiter, L.A.; Kastelein, J.J.; Ray, K.K.; Kallend, D. Effects of renal impairment on the pharmacokinetics, efficacy, and safety of inclisiran: An analysis of the ORION-7 and ORION-1 studies. Mayo Clin. Proc. 2020, 95, 77–89. [Google Scholar] [CrossRef] [PubMed]
- Ray, K.K.; Troquay, R.P.; Visseren, F.L.; Leiter, L.A.; Wright, R.S.; Vikarunnessa, S.; Talloczy, Z.; Zang, X.; Maheux, P.; Lesogor, A. Long-term efficacy and safety of inclisiran in patients with high cardiovascular risk and elevated LDL cholesterol (ORION-3): Results from the 4-year open-label extension of the ORION-1 trial. Lancet Diabetes Endocrinol. 2023, 11, 109–119. [Google Scholar] [CrossRef]
- Stoekenbroek, R.M.; Kallend, D.; Wijngaard, P.L.; Kastelein, J.J. Inclisiran for the treatment of cardiovascular disease: The ORION clinical development program. Future Cardiol. 2018, 14, 433–442. [Google Scholar] [CrossRef]
- Katsiki, N.; Vrablik, M.; Banach, M.; Gouni-Berthold, I. Inclisiran, Low-Density Lipoprotein Cholesterol and Lipoprotein (a). Pharmaceuticals 2023, 16, 577. [Google Scholar] [CrossRef]
- Kallend, D.; Stoekenbroek, R.; He, Y.; Smith, P.F.; Wijngaard, P. Pharmacokinetics and pharmacodynamics of inclisiran, a small interfering RNA therapy, in patients with hepatic impairment. J. Clin. Lipidol. 2022, 16, 208–219. [Google Scholar] [CrossRef]
- U.S. National Library of Medicine. Trial to Assess the Effect of Long Term Dosing of Inclisiran in Subjects With High CV Risk and Elevated LDL-C (ORION-8).
- Ray, K.K.; Wright, R.S.; Kallend, D.; Koenig, W.; Leiter, L.A.; Raal, F.J.; Bisch, J.A.; Richardson, T.; Jaros, M.; Wijngaard, P.L.J.; et al. Two Phase 3 Trials of Inclisiran in Patients with Elevated LDL Cholesterol. N. Engl. J. Med. 2020, 382, 1507–1519. [Google Scholar] [CrossRef] [PubMed]
- Raal, F.J.; Kallend, D.; Ray, K.K.; Turner, T.; Koenig, W.; Wright, R.S.; Wijngaard, P.L.J.; Curcio, D.; Jaros, M.J.; Leiter, L.A.; et al. Inclisiran for the Treatment of Heterozygous Familial Hypercholesterolemia. N. Engl. J. Med. 2020, 382, 1520–1530. [Google Scholar] [CrossRef]
- Samuel, E.; Watford, M.; Egolum, U.O.; Ombengi, D.N.; Ling, H.; Cates, D.W. Inclisiran: A first-in-class siRNA therapy for lowering low-density lipoprotein cholesterol. Ann. Pharmacother. 2023, 57, 317–324. [Google Scholar] [CrossRef] [PubMed]
- van den Bosch, S.E.; Corpeleijn, W.E.; Hutten, B.A.; Wiegman, A. How Genetic Variants in Children with Familial Hypercholesterolemia Not Only Guide Detection, but Also Treatment. Genes 2023, 14, 669. [Google Scholar] [CrossRef]
- Scicchitano, P.; Milo, M.; Mallamaci, R.; De Palo, M.; Caldarola, P.; Massari, F.; Gabrielli, D.; Colivicchi, F.; Ciccone, M.M. Inclisiran in lipid management: A literature overview and future perspectives. Biomed. Pharmacother. 2021, 143, 112227. [Google Scholar] [CrossRef]
- Hulten, E.; Jackson, J.L.; Douglas, K.; George, S.; Villines, T.C. The effect of early, intensive statin therapy on acute coronary syndrome: A meta-analysis of randomized controlled trials. Arch. Intern. Med. 2006, 166, 1814–1821. [Google Scholar] [CrossRef]
- Liem, A.H.; van Boven, A.J.; Veeger, N.J.; Withagen, A.J.; Robles de Medina, R.M.; Tijssen, J.G.; van Veldhuisen, D.J. Effect of fluvastatin on ischaemia following acute myocardial infarction: A randomized trial. Eur. Heart J. 2002, 23, 1931–1937. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, G.G.; Steg, P.G.; Szarek, M.; Bhatt, D.L.; Bittner, V.A.; Diaz, R.; Edelberg, J.M.; Goodman, S.G.; Hanotin, C.; Harrington, R.A.; et al. Alirocumab and Cardiovascular Outcomes after Acute Coronary Syndrome. N. Engl. J. Med. 2018, 379, 2097–2107. [Google Scholar] [CrossRef] [PubMed]
- Bittner, V.A.; Szarek, M.; Aylward, P.E.; Bhatt, D.L.; Diaz, R.; Edelberg, J.M.; Fras, Z.; Goodman, S.G.; Halvorsen, S.; Hanotin, C.; et al. Effect of Alirocumab on Lipoprotein(a) and Cardiovascular Risk After Acute Coronary Syndrome. J. Am. Coll. Cardiol. 2020, 75, 133–144. [Google Scholar] [CrossRef]
- Gencer, B.; Mach, F.; Murphy, S.A.; De Ferrari, G.M.; Huber, K.; Lewis, B.S.; Ferreira, J.; Kurtz, C.E.; Wang, H.; Honarpour, N.; et al. Efficacy of Evolocumab on Cardiovascular Outcomes in Patients With Recent Myocardial Infarction: A Prespecified Secondary Analysis From the FOURIER Trial. JAMA Cardiol. 2020, 5, 952–957. [Google Scholar] [CrossRef]
- Leucker, T.M.; Blaha, M.J.; Jones, S.R.; Vavuranakis, M.A.; Williams, M.S.; Lai, H.; Schindler, T.H.; Latina, J.; Schulman, S.P.; Gerstenblith, G. Effect of Evolocumab on Atherogenic Lipoproteins During the Peri- and Early Postinfarction Period: A Placebo-Controlled, Randomized Trial. Circulation 2020, 142, 419–421. [Google Scholar] [CrossRef]
- Luo, Z.; Huang, Z.; Sun, F.; Guo, F.; Wang, Y.; Kao, S.; Yang, G.; Huang, J.; Li, J.; Zhao, S.; et al. The clinical effects of inclisiran, a first-in-class LDL-C lowering siRNA therapy, on the LDL-C levels in Chinese patients with hypercholesterolemia. J. Clin. Lipidol. 2023, 17, 392–400. [Google Scholar] [CrossRef]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; de Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2019, 73, 3168–3209. [Google Scholar] [CrossRef] [PubMed]
- Collet, J.P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar] [CrossRef] [PubMed]
- Vanuzzo, D.; Pilotto, L.; Ambrosio, G.B.; Pyörälä, K.; Lehto, S.; De Bacquer, D.; De Backer, G.; Wood, D. Potential for cholesterol lowering in secondary prevention of coronary heart disease in europe: Findings from EUROASPIRE study. European Action on Secondary Prevention through Intervention to Reduce Events. Atherosclerosis 2000, 153, 505–517. [Google Scholar] [CrossRef]
- Kotseva, K.; Stagmo, M.; De Bacquer, D.; De Backer, G.; Wood, D. Treatment potential for cholesterol management in patients with coronary heart disease in 15 European countries: Findings from the EUROASPIRE II survey. Atherosclerosis 2008, 197, 710–717. [Google Scholar] [CrossRef]
- Kotseva, K.; Wood, D.; De Backer, G.; De Bacquer, D.; Pyörälä, K.; Keil, U. Euroaspire III: A survey on the lifestyle, risk factors and use of cardioprotective drug therapies in coronary patients from 22 European countries. Eur. J. Cardiovasc. Prev. Rehabil. 2009, 16, 121–137. [Google Scholar] [CrossRef]
- Kotseva, K.; De Bacquer, D.; De Backer, G.; Rydén, L.; Jennings, C.; Gyberg, V.; Abreu, A.; Aguiar, C.; Conde, A.C.; Davletov, K.; et al. Lifestyle and risk factor management in people at high risk of cardiovascular disease. A report from the European Society of Cardiology European Action on Secondary and Primary Prevention by Intervention to Reduce Events (EUROASPIRE) IV cross-sectional survey in 14 European regions. Eur. J. Prev. Cardiol. 2016, 23, 2007–2018. [Google Scholar] [CrossRef]
- De Backer, G.; Ambrosioni, E.; Borch-Johnsen, K.; Brotons, C.; Cifkova, R.; Dallongeville, J.; Ebrahim, S.; Faergeman, O.; Graham, I.; Mancia, G.; et al. European guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and Other Societies on Cardiovascular Disease Prevention in Clinical Practice. Eur. Heart. J. 2003, 24, 1601–1610. [Google Scholar] [CrossRef] [PubMed]
- Ray, K.K.; Molemans, B.; Schoonen, W.M.; Giovas, P.; Bray, S.; Kiru, G.; Murphy, J.; Banach, M.; De Servi, S.; Gaita, D.; et al. EU-Wide Cross-Sectional Observational Study of Lipid-Modifying Therapy Use in Secondary and Primary Care: The DA VINCI study. Eur. J. Prev. Cardiol. 2021, 28, 1279–1289. [Google Scholar] [CrossRef]
- Zhao, S.; Wang, Y.; Mu, Y.; Yu, B.; Ye, P.; Yan, X.; Li, Z.; Wei, Y.; Ambegaonakr, B.M.; Hu, D. Prevalence of dyslipidaemia in patients treated with lipid-lowering agents in China: Results of the DYSlipidemia International Study (DYSIS). Atherosclerosis 2014, 235, 463–469. [Google Scholar] [CrossRef]
- Gitt, A.K.; Lautsch, D.; Ferrières, J.; De Ferrari, G.M.; Vyas, A.; Baxter, C.A.; Bash, L.D.; Ashton, V.; Horack, M.; Almahmeed, W.; et al. Cholesterol target value attainment and lipid-lowering therapy in patients with stable or acute coronary heart disease: Results from the Dyslipidemia International Study II. Atherosclerosis 2017, 266, 158–166. [Google Scholar] [CrossRef]
- Andrikopoulos, G.; Tzeis, S.; Nikas, N.; Richter, D.; Pipilis, A.; Gotsis, A.; Tsaknakis, T.; Kartalis, A.; Kitsiou, A.; Toli, K.; et al. Short-term outcome and attainment of secondary prevention goals in patients with acute coronary syndrome—Results from the countrywide TARGET study. Int. J. Cardiol. 2013, 168, 922–927. [Google Scholar] [CrossRef] [PubMed]
- Dyrbus, K.; Gasior, M.; Desperak, P.; Nowak, J.; Osadnik, T.; Banach, M. Characteristics of lipid profile and effectiveness of management of dyslipidaemia in patients with acute coronary syndromes—Data from the TERCET registry with 19,287 patients. Pharmacol. Res. 2019, 139, 460–466. [Google Scholar] [CrossRef] [PubMed]
- Navar, A.M.; Matskeplishvili, S.T.; Urina-Triana, M.; Arafah, M.; Chen, J.W.; Sukonthasarn, A.; Corp Dit Genti, V.; Daclin, V.; Peterson, E.D. Prospective evaluation of lipid management following acute coronary syndrome in non-Western countries. Clin. Cardiol. 2021, 44, 955–962. [Google Scholar] [CrossRef] [PubMed]
- Landmesser, U.; Pirillo, A.; Farnier, M.; Jukema, J.W.; Laufs, U.; Mach, F.; Masana, L.; Pedersen, T.R.; Schiele, F.; Steg, G.; et al. Lipid-lowering therapy and low-density lipoprotein cholesterol goal achievement in patients with acute coronary syndromes: The ACS patient pathway project. Atheroscler. Suppl. 2020, 42, e49–e58. [Google Scholar] [CrossRef]
- Gitt, A.K.; Parhofer, K.G.; Laufs, U.; März, W.; Paar, W.D.; Bramlage, P.; Marx, N. Hypercholesterolemia diagnosis, treatment patterns and target achievement in patients with acute coronary syndromes in Germany. Clin. Res. Cardiol. 2023, 112, 299–311. [Google Scholar] [CrossRef]
- März, W.; Dippel, F.W.; Theobald, K.; Gorcyca, K.; Iorga, Ş.R.; Ansell, D. Utilization of lipid-modifying therapy and low-density lipoprotein cholesterol goal attainment in patients at high and very-high cardiovascular risk: Real-world evidence from Germany. Atherosclerosis 2018, 268, 99–107. [Google Scholar] [CrossRef]
- De Backer, G.; Jankowski, P.; Kotseva, K.; Mirrakhimov, E.; Reiner, Ž.; Rydén, L.; Tokgözoğlu, L.; Wood, D.; De Bacquer, D. Management of dyslipidaemia in patients with coronary heart disease: Results from the ESC-EORP EUROASPIRE V survey in 27 countries. Atherosclerosis 2019, 285, 135–146. [Google Scholar] [CrossRef]
- Kotseva, K.; De Backer, G.; De Bacquer, D.; Rydén, L.; Hoes, A.; Grobbee, D.; Maggioni, A.; Marques-Vidal, P.; Jennings, C.; Abreu, A.; et al. Lifestyle and impact on cardiovascular risk factor control in coronary patients across 27 countries: Results from the European Society of Cardiology ESC-EORP EUROASPIRE V registry. Eur. J. Prev. Cardiol. 2019, 26, 824–835. [Google Scholar] [CrossRef]
- Parati, G.; Kjeldsen, S.; Coca, A.; Cushman, W.C.; Wang, J. Adherence to Single-Pill Versus Free-Equivalent Combination Therapy in Hypertension: A Systematic Review and Meta-Analysis. Hypertension 2021, 77, 692–705. [Google Scholar] [CrossRef] [PubMed]
- Katzmann, J.L.; Sorio-Vilela, F.; Dornstauder, E.; Fraas, U.; Smieszek, T.; Zappacosta, S.; Laufs, U. Non-statin lipid-lowering therapy over time in very-high-risk patients: Effectiveness of fixed-dose statin/ezetimibe compared to separate pill combination on LDL-C. Clin. Res. Cardiol. 2022, 111, 243–252. [Google Scholar] [CrossRef]
- Zhang, H.; Plutzky, J.; Turchin, A. Discontinuation of statins in routine care settings. Ann. Intern. Med. 2013, 159, 75–76. [Google Scholar] [CrossRef] [PubMed]
- Ray, K.K.; Reeskamp, L.F.; Laufs, U.; Banach, M.; Mach, F.; Tokgözoğlu, L.S.; Connolly, D.L.; Gerrits, A.J.; Stroes, E.S.G.; Masana, L.; et al. Combination lipid-lowering therapy as first-line strategy in very high-risk patients. Eur. Heart J. 2022, 43, 830–833. [Google Scholar] [CrossRef]
- Kolandaivelu, K.; Leiden, B.B.; O’Gara, P.T.; Bhatt, D.L. Non-adherence to cardiovascular medications. Eur. Heart J. 2014, 35, 3267–3276. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Dong, S.; Shen, P.; Sun, Y.; Lin, H.; Zhai, S. Achievement of low-density lipoprotein cholesterol targets in Chinese patients with atherosclerotic cardiovascular disease after receiving statins and ezetimibe. Front. Cardiovasc. Med. 2022, 9, 988576. [Google Scholar] [CrossRef]
- Hermans, M.P.; Gevaert, S.; Descamps, O.; Missault, L.; Gillot, B.; De Keyzer, D.; Lautsch, D.; Brudi, P.; Ambegaonkar, B.; Vyas, A.; et al. Frequency and predictors of cholesterol target attainment in patients with stable coronary heart disease in Belgium: Results from the Dyslipidemia International Study II (DYSIS II (CHD)). Acta Clin. Belg. 2019, 74, 399–404. [Google Scholar] [CrossRef]
- Mitchell, S.; Roso, S.; Samuel, M.; Pladevall-Vila, M. Unmet need in the hyperlipidaemia population with high risk of cardiovascular disease: A targeted literature review of observational studies. BMC Cardiovasc. Disord. 2016, 16, 74. [Google Scholar] [CrossRef]
- Lee, S.H.; Song, W.H.; Jeong, M.H.; Hur, S.H.; Jeon, D.W.; Jeung, W.; Gitt, A.K.; Horack, M.; Vyas, A.; Lautsch, D.; et al. Dyslipidemia and Rate of Under-Target Low-Density Lipoprotein-Cholesterol in Patients with Coronary Artery Disease in Korea. J. Lipid Atheroscler. 2019, 8, 242–251. [Google Scholar] [CrossRef]
- Liberopoulos, E.; Rallidis, L.; Spanoudi, F.; Xixi, E.; Gitt, A.; Horack, M.; Ashton, V.; Brudi, P.; Lautsch, D.; Ambegaonkar, B.; et al. Attainment of cholesterol target values in Greece: Results from the Dyslipidemia International Study II. Arch. Med. Sci. 2019, 15, 821–831. [Google Scholar] [CrossRef]
- Borrie, A.; Fiennes, E.; Harding, S.A.; Sasse, A. Cholesterol treatment in patients with acute coronary syndromes: Does stating a target improve management? N. Z. Med. J. 2022, 135, 24–31. [Google Scholar] [PubMed]
- Faggiano, P.; Fattirolli, F.; Frisinghelli, A.; Piccioli, L.; Dasseni, N.; Silverii, M.V.; Albricci, L.; D’Ambrosio, G.; Garrì, R.; Esposito, L.; et al. Secondary prevention advices after cardiovascular index event: From drug prescription to risk factors control in real world practice. Monaldi Arch. Chest Dis. 2019, 89. [Google Scholar] [CrossRef] [PubMed]
- De Luca, L.; Riccio, C.; Navazio, A.; Valente, S.; Cipriani, M.; Corda, M.; De Nardo, A.; Francese, G.M.; Napoletano, C.; Tizzani, E.; et al. ANMCO position paper on the management of hypercholesterolaemia in patients with acute coronary syndrome. Eur. Heart J. Suppl. 2023, 25, D312–D322. [Google Scholar] [CrossRef]
- Masiero, G.; Franzone, A.; Silvestri, T.; Castiglioni, B.; Greco, F.; La Manna, A.G.; Limbruno, U.; Longoni, M.; Marchese, A.; Mattesini, A.; et al. PCSK9 inhibitor use in high cardiovascular risk patients: An interventionalist’s overview on efficacy, current recommendations and factual prescription. G. Ital. Cardiol. 2020, 21, 264–270. [Google Scholar] [CrossRef]
- Bilato, C.; Caldarola, P.; Musumeci, G.; Colivicchi, F. Managing lipid risk in acute coronary syndrome patients in the real world: Results from the BEST consensus. G. Ital. Cardiol. 2023, 24, 383–390. [Google Scholar] [CrossRef]
- Musumeci, G.; Annibali, G.; Delnevo, F. Acute coronary syndromes: Hospital management of dyslipidaemia with proprotein convertase subtilisin/kexin 9 inhibitors: Time to act. Eur. Heart J. Suppl. 2023, 25, B114–B118. [Google Scholar] [CrossRef]
- Zuin, M.; Rigatelli, G.; Caldarola, P.; Colivicchi, F.; Roncon, L.; Bilato, C. Real-world efficacy of current lipid-lowering strategies in patients with acute coronary syndrome. Time to change the paradigm for treatment. G. Ital. Cardiol. 2023, 24, 30–40. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).