Long-Term Impacts of Diurnal Temperature Range on Mortality and Cardiovascular Disease: A Nationwide Prospective Cohort Study
Abstract
:1. Introduction
2. Methods
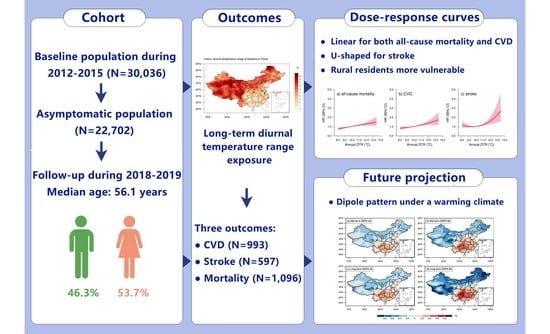
2.1. Study Population and Follow-Up
2.2. Outcome Ascertainment
2.3. DTR Exposure Assessment
2.4. Future Projection
2.5. Covariate Measurement
2.6. Statistical Analysis
3. Results
3.1. Baseline Characteristics of Study Participants
3.2. Long-Term Impacts of DTR Exposure on Health Outcomes
3.3. Subgroup Analysis and Effect Modification
3.4. Future Projection of DTR in China
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Murray, C.J.L.; Aravkin, A.Y.; Zheng, P.; Abbafati, C.; Abbas, K.M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abdelalim, A.; Abdollahi, M.; Abdollahpour, I.; et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the global burden of disease study 2019. Lancet 2020, 396, 1223–1249. [Google Scholar] [CrossRef] [PubMed]
- Joseph, P.; Leong, D.; McKee, M.; Anand, S.S.; Schwalm, J.D.; Teo, K.; Mente, A.; Yusuf, S. Reducing the global burden of cardiovascular disease, part 1: The epidemiology and risk factors. Circ. Res. 2017, 121, 677–694. [Google Scholar] [CrossRef] [PubMed]
- Braganza, K.; Karoly, D.J.; Arblaster, J.M. Diurnal temperature range as an index of global climate change during the twentieth century. Geophys. Res. Lett. 2004, 31, 405–407. [Google Scholar] [CrossRef]
- Hansen, J.; Sato, M.; Ruedy, R. Long-term changes of the diurnal temperature cycle: Implications about mechanisms of global climate change. Atmos. Res. 1995, 37, 175–209. [Google Scholar] [CrossRef]
- Kan, H.; London, S.J.; Chen, H.; Song, G.; Chen, G.; Jiang, L.; Zhao, N.; Zhang, Y.; Chen, B. Diurnal temperature range and daily mortality in Shanghai, China. Env. Res. 2007, 103, 424–431. [Google Scholar] [CrossRef]
- Yang, J.; Zhou, M.; Li, M.; Yin, P.; Wang, B.; Pilot, E.; Liu, Y.; van der Hoek, W.; van Asten, L.; Krafft, T.; et al. Diurnal temperature range in relation to death from stroke in China. Env. Res. 2018, 164, 669–675. [Google Scholar] [CrossRef]
- Zhang, Y.; Peng, M.; Wang, L.; Yu, C. Association of diurnal temperature range with daily mortality in England and Wales: A nationwide time-series study. Sci. Total Env. 2018, 619, 291–300. [Google Scholar] [CrossRef]
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: Update from the GBD 2019 study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef]
- Du, X.; Patel, A.; Anderson, C.; Dong, J.; Ma, C. Epidemiology of cardiovascular disease in China and opportunities for improvement: JACC international. J. Am. Coll. Cardiol. 2019, 73, 3135–3147. [Google Scholar] [CrossRef]
- Zhao, D.; Liu, J.; Wang, M.; Zhang, X.; Zhou, M. Epidemiology of cardiovascular disease in China: Current features and implications. Nat. Rev. Cardiol. 2019, 16, 203–212. [Google Scholar] [CrossRef]
- Hao, G.; Wang, X.; Chen, Z.; Zhang, L.; Zhang, Y.; Wei, B.; Zheng, C.; Kang, Y.; Jiang, L.; Zhu, Z.; et al. Prevalence of heart failure and left ventricular dysfunction in China: The China hypertension survey, 2012–2015. Eur. J. Heart Fail. 2019, 21, 1329–1337. [Google Scholar] [CrossRef]
- Wang, Z.; Chen, Z.; Zhang, L.; Wang, X.; Hao, G.; Zhang, Z.; Shao, L.; Tian, Y.; Dong, Y.; Zheng, C.; et al. Status of hypertension in China. Circulation 2018, 137, 2344–2356. [Google Scholar] [CrossRef]
- Kang, Y.; Tang, H.; Zhang, L.; Wang, S.; Wang, X.; Chen, Z.; Zheng, C.; Yang, Y.; Wang, Z.; Huang, G.; et al. Long-term temperature variability and the incidence of cardiovascular diseases: A large, representative cohort study in China. Env. Pollut. 2021, 278, 116831. [Google Scholar] [CrossRef] [PubMed]
- WHO (World Health Organization). International Statistical Classification of Diseases and Related Health Problems, 10th Revision. Available online: http://apps.who.int/classifications/icd10/browse/2016/en (accessed on 10 January 2020).
- Cao, X.; Tang, H.; Zheng, C.; Kang, Y.; Zhang, L.; Wang, X.; Chen, Z.; Yang, Y.; Zhou, H.; Chen, L.; et al. Association of heating fuel types with mortality and cardiovascular events among non-smokers in China. Env. Pollut. 2021, 291, 118207. [Google Scholar] [CrossRef] [PubMed]
- Tang, H.; Zheng, C.; Cao, X.; Wang, S.; Zhang, L.; Wang, X.; Chen, Z.; Song, Y.; Chen, C.; Tian, Y.; et al. Blue sky as a protective factor for cardiovascular disease. Front. Public Health 2022, 10, 1016853. [Google Scholar] [CrossRef] [PubMed]
- Szentimrey, T. Multiple Analysis of Series for Homogenization (MASH). In Proceeding Second Seminar for Homogenization of Surface Climatological Data; WCDMP-41; WMO: Budapest, Hungary, 1999; Volume 41, pp. 27–46. [Google Scholar]
- Thrasher, B.; Wang, W.; Michaelis, A.; Melton, F.; Lee, T.J.; Nemani, R. NASA global daily downscaled projections, CMIP6. Sci. Data 2022, 9, 262. [Google Scholar] [CrossRef]
- Wood, A.W.; Leung, L.R.; Sridhar, V.; Lettenmaier, D.P. Hydrologic implications of dynamical and statistical approaches to downscaling climate model outputs. Clim. Change 2004, 62, 189–216. [Google Scholar] [CrossRef]
- Kong, L.; Tang, X.; Zhu, J.; Wang, Z.; Li, J.; Wu, H.; Wu, Q.; Chen, H.; Zhu, L.; Wang, W.; et al. A 6-year-long (2013–2018) high-resolution air quality reanalysis dataset in China based on the assimilation of surface observations from CNEMC. Earth Syst. Sci. Data 2021, 13, 529–570. [Google Scholar] [CrossRef]
- Zheng, C.; Tang, H.; Wang, X.; Chen, Z.; Zhang, L.; Kang, Y.; Yang, Y.; Chen, L.; Zhou, H.; Cai, J.; et al. Left ventricular diastolic dysfunction and cardiovascular disease in different ambient air pollution conditions: A prospective cohort study. Sci. Total Env. 2022, 831, 154872. [Google Scholar] [CrossRef]
- Lynch, J.W.; Kaplan, G.A.; Cohen, R.D.; Tuomilehto, J.; Salonen, J.T. Do cardiovascular risk factors explain the relation between socioeconomic status, risk of all-cause mortality, cardiovascular mortality, and acute myocardial infarction? Am. J. Epidemiol. 1996, 13, 934–942. [Google Scholar] [CrossRef] [Green Version]
- Elfassy, T.; Swift, S.L.; Glymour, M.M.; Calonico, S.; Jacobs, D.R.; Mayeda, E.R.; Kershaw, K.N.; Kiefe, C.; Hazzouri, A.Z.A. Associations of income volatility with incident cardiovascular disease and all-cause mortality in a US cohort. Circulation 2019, 139, 850–859. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.; Tang, H.; Jiang, L.; Wang, S.; Wang, X.; Chen, Z.; Zhang, L.; Zheng, C.; Wang, Z.; Huang, G.; et al. Air temperature variability and high-sensitivity C reactive protein in a general population of China. Sci. Total. Env. 2020, 749, 141588. [Google Scholar] [CrossRef] [PubMed]
- Zanobetti, A.; O’Neill, M.S.; Gronlund, C.J.; Schwartz, J.D. Summer temperature variability and long-term survival among elderly people with chronic disease. Proc. Natl. Acad. Sci. USA 2012, 109, 6608–6613. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, J.; Yan, Z.W.; Feng, J.M. Exaggerated effect of urbanization in the diurnal temperature range via “observation minus reanalysis” and the physical causes. J. Geophys. Res. Atmos. 2018, 123, 7223–7237. [Google Scholar] [CrossRef]
- Halonen, J.I.; Zanobetti, A.; Sparrow, D.; Vokonas, P.S.; Schwartz, J. Associations between outdoor temperature and markers of inflammation: A cohort study. Env. Healthy 2010, 9, 42. [Google Scholar] [CrossRef] [Green Version]
- Martinez-Nicolas, A.; Meyer, M.; Hunkler, S.; Madrid, J.A.; Rol, M.A.; Meyer, A.H.; Schötzau, A.; Orgül, S.; Kräuchi, K. Daytime variation in ambient temperature affects skin temperatures and blood pressure: Ambulatory winter/summer comparison in healthy young women. Physiol. Behav. 2015, 149, 203–211. [Google Scholar] [CrossRef]
- Thompson, P.D.; Franklin, B.A.; Balady, G.J.; Blair, S.N.; Corrado, D.; Estes, N.A., III; Fulton, J.E.; Gordon, N.F.; Haskell, W.L.; Link, M.S.; et al. Exercise and acute cardiovascular events placing the risks into perspective: A scientific statement from the American heart association council on nutrition, physical activity, and metabolism and the council on clinical cardiology. Circulation 2007, 115, 2358–2368. [Google Scholar]
- Okamoto-Mizuno, K.; Mizuno, K. Effects of thermal environment on sleep and circadian rhythm. J. Physiol. Anthropol. 2012, 31, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Easterling, D.R.; Horton, B.; Jones, P.D.; Peterson, T.C.; Karl, T.R.; Parker, D.E.; Salinger, M.J.; Razuvayev, V.; Plummer, N.; Jamason, P.; et al. Maximum and minimum temperature trends for the globe. Science 1997, 277, 364–367. [Google Scholar] [CrossRef] [Green Version]
- Lindvall, J.; Svensson, G. The diurnal temperature range in the CMIP5 models. Clim. Dyn. 2015, 44, 405–421. [Google Scholar] [CrossRef]





| Variables | Total (n = 22,702) | Tertiles of DTR (°C) | p Value | ||
|---|---|---|---|---|---|
| 8.04−8.69 (n = 7808) | 8.69−11.11 (n = 7029) | 11.11−13.43 (n = 7865) | |||
| Age, years | 56.1 ± 13.1 | 57.0 ± 13.3 | 55.9 ± 13.2 | 55.5 ± 12.8 | <0.001 |
| Male, n (%) | 10,505 (46.3) | 3612 (46.3) | 3379 (48.1) | 3514 (44.7) | <0.001 |
| Urban, n (%) | 10,130 (44.6) | 1780 (22.8) | 4654 (66.2) | 3696 (47.0) | <0.001 |
| Han ethnicity, n (%) | 20,315 (89.5) | 7299 (93.5) | 6980 (99.3) | 6036 (76.7) | <0.001 |
| Region, n (%) | <0.001 | ||||
| East | 9263 (40.8) | 5086 (65.1) | 1433 (20.4) | 2744 (34.9) | |
| Central | 9460 (41.7) | 1987 (25.4) | 4909 (69.8) | 2564 (32.6) | |
| West | 3979 (17.5) | 735 (9.4) | 687 (9.8) | 2557 (32.5) | |
| Educational to middle school or higher, n (%) | 11,109 (48.9) | 2638 (33.8) | 4026 (57.3) | 4445 (56.5) | <0.001 |
| Smoking, n (%) | <0.001 | ||||
| Current | 5731 (25.2) | 2179 (27.9) | 1686 (24.0) | 1866 (23.7) | |
| Former | 1216 (5.4) | 392 (5.0) | 359 (5.1) | 465 (5.9) | |
| Never | 15,755 (69.4) | 5237 (67.1) | 4984 (70.9) | 5534 (70.4) | |
| Alcohol consumption, n (%) | 6318 (27.8) | 2096 (26.8) | 2074 (29.5) | 2148 (27.3) | <0.001 |
| BMI (kg/m2), n (%) | <0.001 | ||||
| Underweight | 10,213 (45.0) | 4020 (51.5) | 3062 (43.6) | 3131 (39.8) | |
| Normal | 8533 (37.6) | 2733 (35.0) | 2717 (38.7) | 3083 (39.2) | |
| Overweight | 3956 (17.4) | 1055 (13.5) | 1250 (17.8) | 1651 (21.0) | |
| Hypertension, n (%) | 8957 (39.5) | 2997 (38.4) | 2709 (38.5) | 3251 (41.3) | <0.01 |
| Hypercholesterolemia, n (%) | 7724 (34.0) | 2346 (30.0) | 2514 (35.8) | 2864 (36.4) | <0.001 |
| Diabetes mellitus, n (%) | 2286 (10.1) | 714 (9.1) | 661 (9.4) | 911 (11.6) | <0.001 |
| Family history of CVD, n (%) | 2621 (11.5) | 606 (7.8) | 857 (12.2) | 1158 (14.7) | <0.001 |
| CVD medication history, n (%) | 4929 (21.7) | 1560 (20.0) | 1364 (19.4) | 2005 (25.5) | <0.001 |
| PM2.5 (μg/m3) | 61.7 ± 22.5 | 53.3 ± 11.2 | 76.7 ± 24.2 | 56.7 ± 22.9 | <0.001 |
| NO2 (μg/m3) | 29.3 ± 13.3 | 26.7 ± 7.3 | 36.5 ± 14.9 | 24.8 ± 13.7 | <0.001 |
| NDVI | 0.4 ± 0.1 | 0.6 ± 0.1 | 0.4 ± 0.1 | 0.3 ± 0.1 | <0.001 |
| Relative humidity (%) | 66.1 ± 9.6 | 74.9 ± 2.7 | 66.2 ± 8.1 | 57.4 ± 7.1 | <0.001 |
| Ambient temperature (°C) | 12.8 ± 4.8 | 16.9 ± 1.6 | 14.1 ± 2.9 | 7.6 ± 3.6 | <0.001 |
| Outcomes | Per 1 °C Increment | Tertiles of DTR | ptrend | ||
|---|---|---|---|---|---|
| Lowest Tertile | Middle Tertile | Highest Tertile | |||
| All-cause mortality | |||||
| No. of cases | 1096 | 341 | 363 | 392 | / |
| Incidence rate † | 10.49 | 10.29 | 10.01 | 11.18 | / |
| Model 1 a | 1.14 (1.09−1.18) | Reference | 1.46 (1.23−1.74) | 1.80 (1.52−2.14) | <0.001 |
| Model 2 b | 1.13 (1.09−1.18) | Reference | 1.46 (1.23−1.74) | 1.77 (1.49−2.10) | <0.001 |
| Model 3 c | 1.14 (1.10−1.19) | Reference | 1.50 (1.25−1.79) | 1.79 (1.51−2.13) | <0.001 |
| Model 4 d | 1.13 (1.08−1.18) | Reference | 1.42 (1.17−1.74) | 1.70 (1.40−2.07) | <0.001 |
| CVD (fatal + nonfatal) | |||||
| No. of cases | 993 | 285 | 328 | 380 | / |
| Incidence rate † | 9.45 | 8.55 | 8.99 | 10.79 | / |
| Model 1 a | 1.13 (1.09−1.18) | Reference | 1.04 (0.86−1.26) | 1.68 (1.42−2.00) | <0.001 |
| Model 2 b | 1.13 (1.08−1.18) | Reference | 1.06 (0.88−1.28) | 1.63 (1.37−1.94) | <0.001 |
| Model 3 c | 1.14 (1.09−1.19) | Reference | 1.09 (0.89−1.32) | 1.66 (1.39−1.98) | <0.001 |
| Model 4 d | 1.12 (1.07−1.18) | Reference | 0.94 (0.75−1.17) | 1.52 (1.24−1.87) | <0.001 |
| Stroke (fatal + nonfatal) | |||||
| No. of cases | 597 | 191 | 192 | 214 | / |
| Incidence rate † | 5.64 | 5.70 | 5.22 | 6.02 | / |
| Model 1 a | 1.11 (1.05−1.17) | Reference | 0.82 (0.64−1.06) | 1.45 (1.16−1.80) | <0.001 |
| Model 2 b | 1.10 (1.04−1.16) | Reference | 0.84 (0.65−1.07) | 1.40 (1.12−1.74) | 0.003 |
| Model 3 c | 1.12 (1.06−1.19) | Reference | 0.86 (0.67−1.12) | 1.42 (1.14−1.77) | 0.001 |
| Model 4 d | 1.09 (1.02−1.16) | Reference | 0.68 (0.51−0.91) | 1.18 (0.91−1.53) | 0.071 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tang, H.; Wang, X.; Kang, Y.; Zheng, C.; Cao, X.; Tian, Y.; Hu, Z.; Zhang, L.; Chen, Z.; Song, Y.; et al. Long-Term Impacts of Diurnal Temperature Range on Mortality and Cardiovascular Disease: A Nationwide Prospective Cohort Study. Metabolites 2022, 12, 1287. https://doi.org/10.3390/metabo12121287
Tang H, Wang X, Kang Y, Zheng C, Cao X, Tian Y, Hu Z, Zhang L, Chen Z, Song Y, et al. Long-Term Impacts of Diurnal Temperature Range on Mortality and Cardiovascular Disease: A Nationwide Prospective Cohort Study. Metabolites. 2022; 12(12):1287. https://doi.org/10.3390/metabo12121287
Chicago/Turabian StyleTang, Haosu, Xin Wang, Yuting Kang, Congyi Zheng, Xue Cao, Yixin Tian, Zhen Hu, Linfeng Zhang, Zuo Chen, Yuxin Song, and et al. 2022. "Long-Term Impacts of Diurnal Temperature Range on Mortality and Cardiovascular Disease: A Nationwide Prospective Cohort Study" Metabolites 12, no. 12: 1287. https://doi.org/10.3390/metabo12121287
APA StyleTang, H., Wang, X., Kang, Y., Zheng, C., Cao, X., Tian, Y., Hu, Z., Zhang, L., Chen, Z., Song, Y., Gu, R., Cai, J., Huang, G., & Wang, Z., on behalf of the China Hypertension Survey Investigators. (2022). Long-Term Impacts of Diurnal Temperature Range on Mortality and Cardiovascular Disease: A Nationwide Prospective Cohort Study. Metabolites, 12(12), 1287. https://doi.org/10.3390/metabo12121287