Wearable Augmented Reality Application for Shoulder Rehabilitation
Abstract
1. Introduction
2. Materials and Methods
2.1. Rationale
2.2. Selection of the Head-Mounted Display
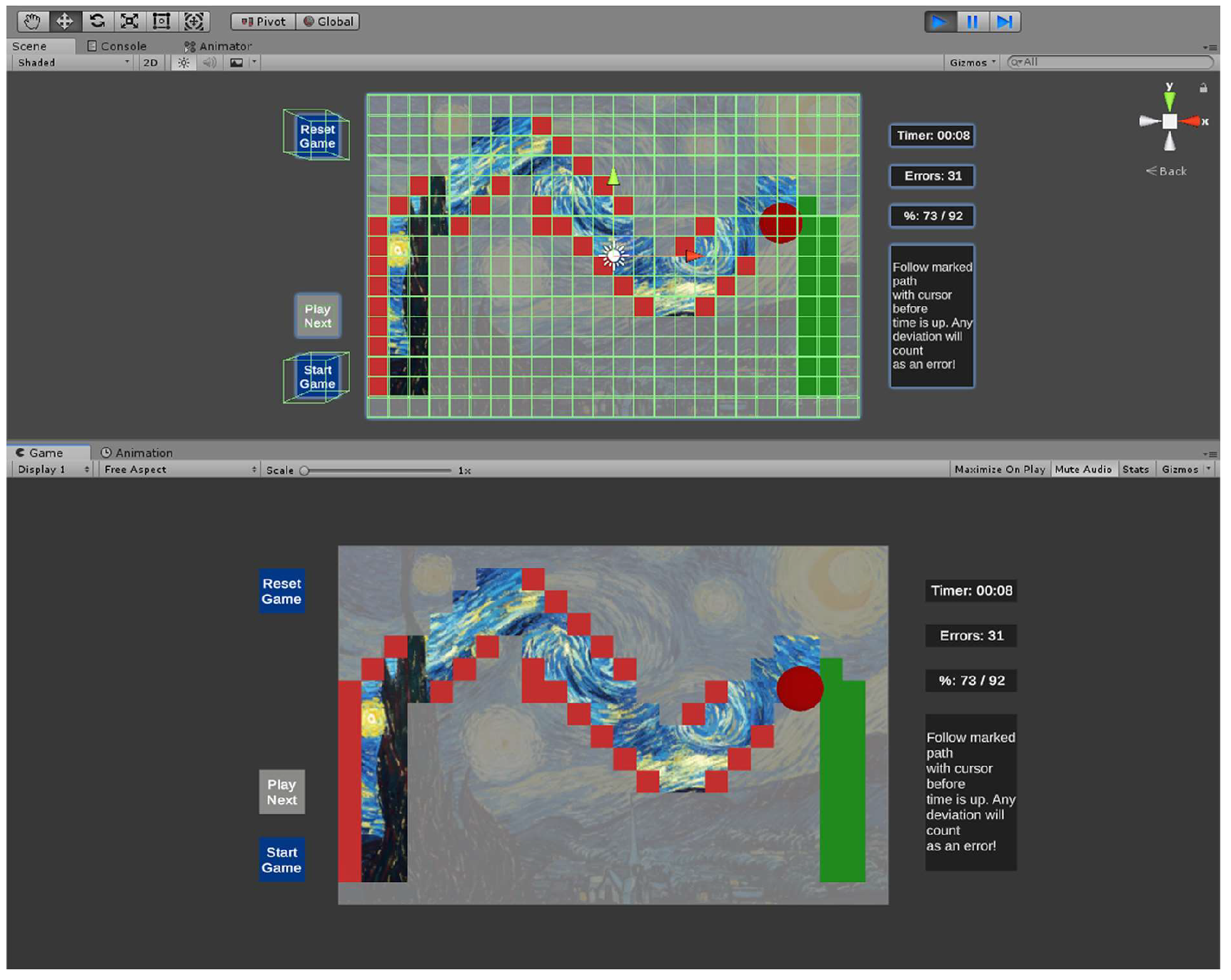
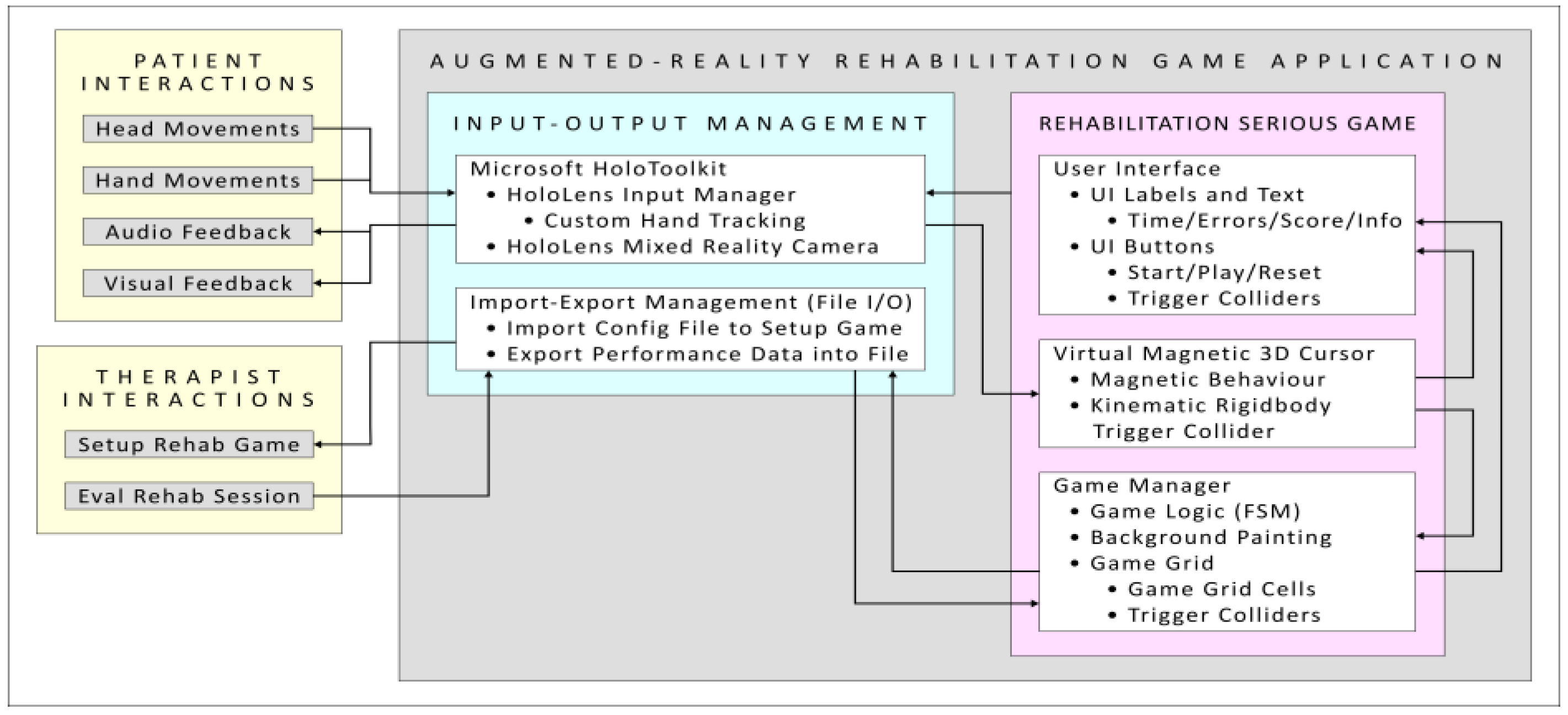
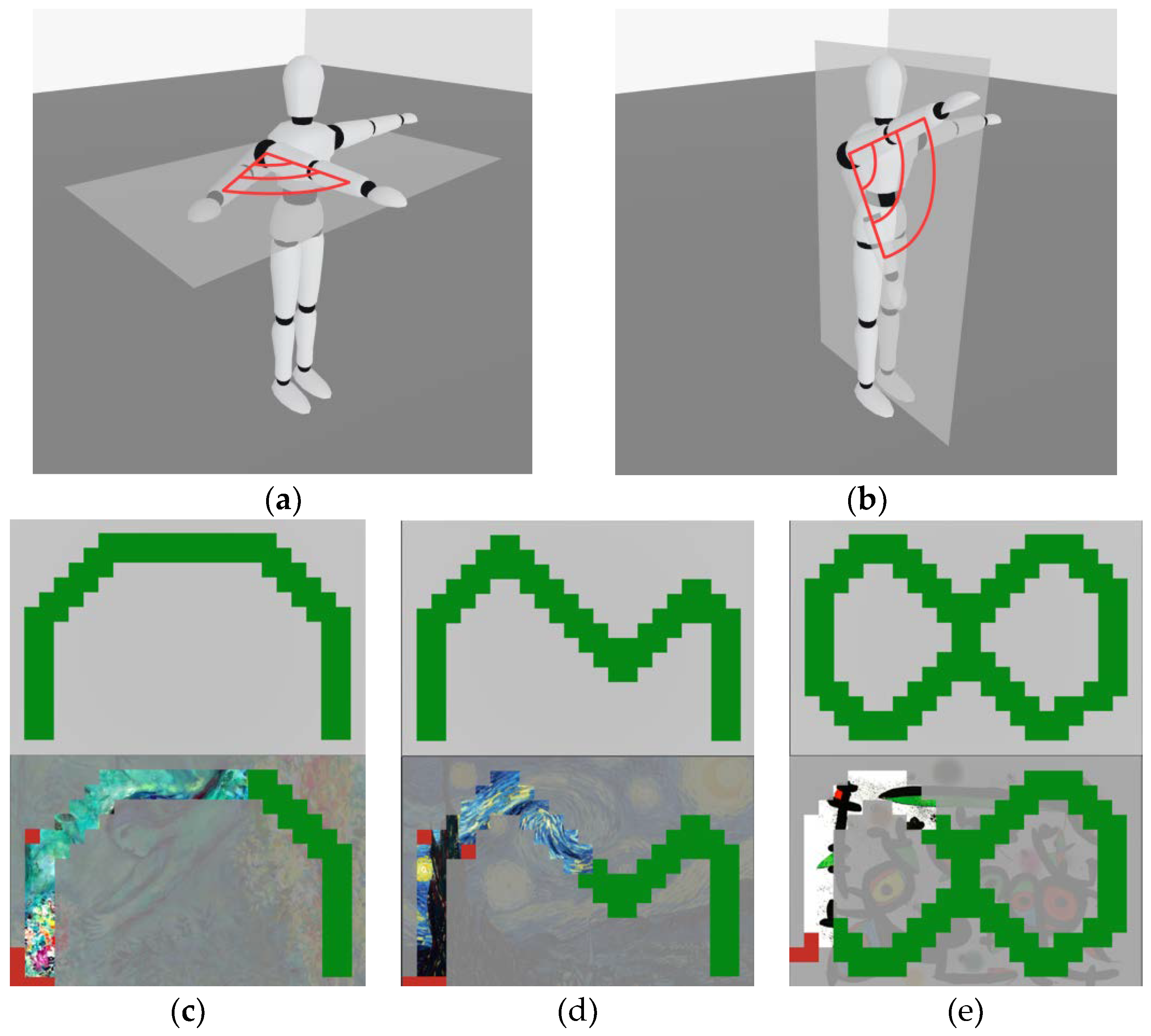
2.3. Design of the AR Rehabilitation Serious Game
2.4. Design of the AR Rehabilitation Serious Game
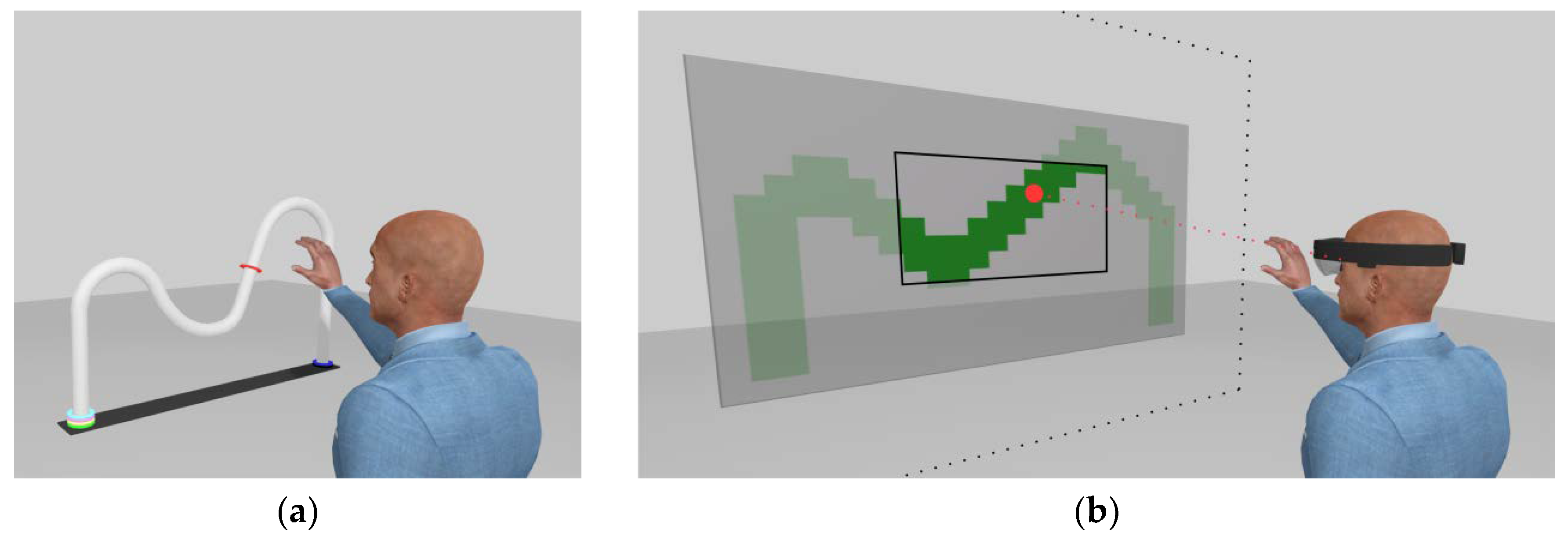
2.5. Hand Tracking and Virtual Cursor Control
- Derive the 3D vector, , starting from the Mixed Reality Camera 3D position and ending at the 3D position of the tracked hand.
- Update the 3D rotation of the “Virtual 3D Magnetic Cursor” to align it with the 3D vector .
- Translate by, t (see magnetic behavior below), the virtual cursor 3D model along the 3D vector .
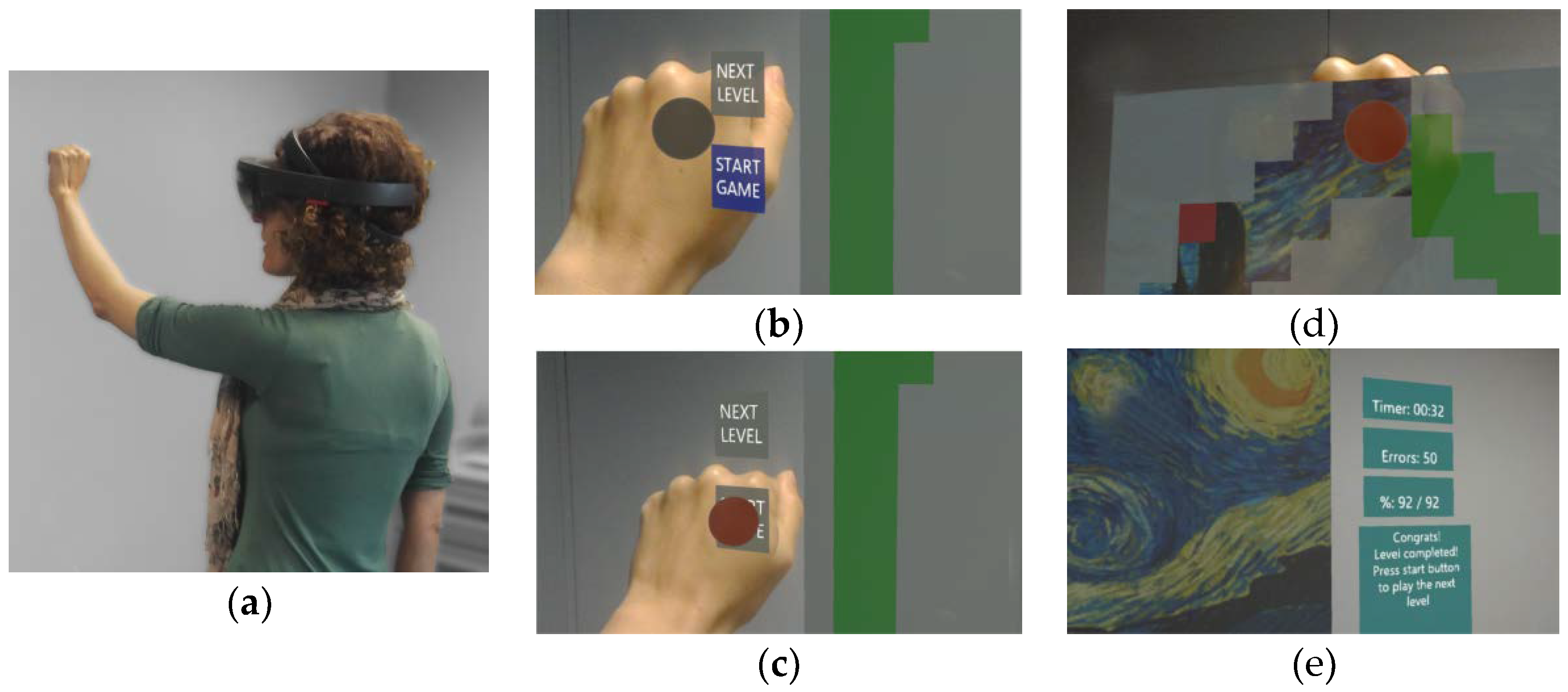
2.6. System Testing: Performance and User Evaluation
- Administration of a “Consent and a Demographic Form” (Table 2), including information about the subject’s previous experience with videogames, AR, and HoloLens.
- Introduction to the AR rehabilitation game app (game goals, UI, and virtual cursor control) with a standardized 8–10 min oral explanation.
- User-specific HoloLens calibration using the Microsoft Calibration app.
- Introduction to the HoloLens 3D tracking (workspace, gestures) using the Microsoft Learn Gestures app.
- Testing of our AR rehab game app until the completion of all nine shoulder ROM rehabilitation exercises.
- Administration of a “Likert Questionnaire” to collect the subject evaluation on the engagement and ergonomics of our AR rehab game app.
3. Results
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Riva, G.; Baños, R.M.; Botella, C.; Mantovani, F.; Gaggioli, A. Transforming Experience: The Potential of Augmented Reality and Virtual Reality for Enhancing Personal and Clinical Change. Front. Psychiatry 2016, 7, 164. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, A.G.; Ritter, E.M.; Champion, H.; Higgins, G.; Fried, M.P.; Moses, G.; Smith, C.D.; Satava, R.M. Virtual reality simulation for the operating room—Proficiency-based training as a paradigm shift in surgical skills training. Ann. Surg. 2005, 241, 364–372. [Google Scholar] [CrossRef] [PubMed]
- Carneiro, F.; Tavares, R.; Rodrigues, J.; Abreu, P.; Restivo, M.T. A Gamified Approach for Hand Rehabilitation Device. Int. J. Online Eng. 2018, 14, 179–186. [Google Scholar] [CrossRef]
- Bank, P.J.M.; Cidota, M.A.; Ouwehand, P.W.; Lukosch, S.G. Patient-Tailored Augmented Reality Games for Assessing Upper Extremity Motor Impairments in Parkinson’s Disease and Stroke. J. Med. Syst. 2018, 42, 246. [Google Scholar] [CrossRef]
- Azuma, R.; Baillot, Y.; Behringer, R.; Feiner, S.; Julier, S.; MacIntyre, B. Recent advances in augmented reality. IEEE Comput. Graph. 2001, 21, 34–47. [Google Scholar] [CrossRef]
- Al-Issa, H.; Regenbrecht, H.; Hale, L. Augmented reality applications in rehabilitation to improve physical outcomes. Phys. Ther. Rev. 2012, 17, 16–28. [Google Scholar] [CrossRef]
- Merians, A.S.; Jack, D.; Boian, R.; Tremaine, M.; Burdea, G.C.; Adamovich, S.V.; Recce, M.; Poizner, H. Virtual reality-augmented rehabilitation for patients following stroke. Phys. Ther. 2002, 82, 898–915. [Google Scholar]
- Mitchell, C.; Adebajo, A.; Hay, E.; Carr, A. Shoulder pain: Diagnosis and management in primary care. BMJ (Clin. Res. Ed.) 2005, 331, 1124–1128. [Google Scholar] [CrossRef]
- Linaker, C.H.; Walker-Bone, K. Shoulder disorders and occupation. Best Pract. Res. Clin. Rheumatol. 2015, 29, 405–423. [Google Scholar] [CrossRef]
- Natale, G.; Condino, S.; Soldani, P.; Fornai, F.; Mattioli Belmonte, M.; Gesi, M. Natale et. al.’s response to Stecco’s fascial nomenclature editorial. J. Bodyw. Mov. Ther. 2014, 18, 588–590. [Google Scholar] [CrossRef]
- Natale, G.; Condino, S.; Stecco, A.; Soldani, P.; Belmonte, M.M.; Gesi, M. Is the cervical fascia an anatomical proteus? Surg. Radiol. Anat. 2015, 37, 1119–1127. [Google Scholar] [CrossRef]
- Assis, G.A.D.; Corrêa, A.G.D.; Martins, M.B.R.; Pedrozo, W.G.; Lopes, R.D.D. An augmented reality system for upper-limb post-stroke motor rehabilitation: A feasibility study. Disabil. Rehabilit: Assist. Technol. 2016, 11, 521–528. [Google Scholar] [CrossRef]
- King, M.; Hale, L.; Pekkari, A.; Persson, M.; Gregorsson, M.; Nilsson, M. An affordable, computerised, table-based exercise system for stroke survivors. Disabil. Rehabilit. Assist. Technol. 2010, 5, 288–293. [Google Scholar] [CrossRef]
- Aung, Y.; Al-Jumaily, A. Augmented reality-based RehaBio system for shoulder rehabilitation. J. Mechatron. Autom. 2014, 4, 52–62. [Google Scholar] [CrossRef]
- Da Gama, A.E.F.; Chaves, T.M.; Figueiredo, L.S.; Baltar, A.; Meng, M.; Navab, N.; Teichrieb, V.; Fallavollita, P. MirrARbilitation: A clinically-related gesture recognition interactive tool for an AR rehabilitation system. Comput. Methods Progr. Biomed. 2016, 135, 105–114. [Google Scholar] [CrossRef]
- Gama, A.D.; Chaves, T.; Figueiredo, L.; Teichrieb, V. Poster: Improving motor rehabilitation process through a natural interaction based system using Kinect sensor. In Proceedings of the 2012 IEEE Symposium on 3D User Interfaces (3DUI), Costa Mesa, CA, USA, 4–5 March 2012; pp. 145–146. [Google Scholar]
- Aung, Y.M.; Al-Jumaily, A. Augmented Reality based Illusion System with biofeedback. In Proceedings of the 2nd Middle East Conference on Biomedical Engineering, Doha, Qatar, 17–20 February 2014; pp. 265–268. [Google Scholar]
- Aung, Y.M.; Al-Jumaily, A.; Anam, K. A novel upper limb rehabilitation system with self-driven virtual arm illusion. In Proceedings of the 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Chicago, IL, USA, 26–30 August 2014; pp. 3614–3617. [Google Scholar]
- De Leon, N.I.; Bhatt, S.K.; Al-Jumaily, A. Augmented reality game based multi-usage rehabilitation therapist for stroke patients. Int. J. Smart Sens. Intell. Syst. 2014, 7, 1044–1058. [Google Scholar] [CrossRef]
- Vieira, J.; Sousa, M.; Arsénio, A.M.; Jorge, J. Augmented Reality for Rehabilitation Using Multimodal Feedback. In Proceedings of the 3rd 2015 Workshop on ICTs for improving Patients Rehabilitation Research Techniques, Lisbon, Portugal, 1–2 October 2015; pp. 38–41. [Google Scholar]
- Colomer, C.; Llorens, R.; Noé, E.; Alcañiz, M. Effect of a mixed reality-based intervention on arm, hand, and finger function on chronic stroke. J. Neuroeng. Rehabil. 2016, 13, 45. [Google Scholar] [CrossRef]
- Sousa, M.; Vieira, J.; Medeiros, D.; Arsenio, A.; Jorge, J. SleeveAR: Augmented Reality for Rehabilitation using Realtime Feedback. In Proceedings of the 21st International Conference on Intelligent User Interfaces (Iui’16), Sonoma, CA, USA, 7–10 March 2016; pp. 175–185. [Google Scholar] [CrossRef]
- Mousavi Hondori, H.; Khademi, M.; Dodakian, L.; McKenzie, A.; Lopes, C.V.; Cramer, S.C. Choice of Human–Computer Interaction Mode in Stroke Rehabilitation. Neurorehabilit. Neural Repair 2015, 30, 258–265. [Google Scholar] [CrossRef]
- Viglialoro, R.M.; Condino, S.; Turini, G.; Carbone, M.; Ferrari, V.; Gesi, M. Review of the Augmented Reality Systems for Shoulder Rehabilitation. Information 2019, 10, 154. [Google Scholar] [CrossRef]
- Koulieris, G.-A.; Bui, B.; Banks, M.; Drettakis, G. Accommodation and Comfort in Head-Mounted Displays. ACM Trans. Graph. 2017, 36, 11. [Google Scholar] [CrossRef]
- Hua, H. Enabling Focus Cues in Head-Mounted Displays. Proc. IEEE 2017, 105, 805–824. [Google Scholar] [CrossRef]
- Condino, S.; Carbone, M.; Piazza, R.; Ferrari, M.; Ferrari, V. Perceptual Limits of Optical See-Through Visors for Augmented Reality Guidance of Manual Tasks. IEEE Trans. Biomed. Eng. 2019. [Google Scholar] [CrossRef]
- Karatsidis, A.; Richards, R.E.; Konrath, J.M.; van den Noort, J.C.; Schepers, H.M.; Bellusci, G.; Harlaar, J.; Veltink, P.H. Validation of wearable visual feedback for retraining foot progression angle using inertial sensors and an augmented reality headset. J. Neuroeng. Rehabilit. 2018, 15, 78. [Google Scholar] [CrossRef]
- Mori, S.; Ikeda, S.; Plopski, A.; Sandor, C. BrightView: Increasing Perceived Brightness of Optical See-Through Head-Mounted Displays Through Unnoticeable Incident Light Reduction. In Proceedings of the 2018 IEEE Conference on Virtual Reality and 3D User Interfaces (VR), Reutlingen, Germany, 18–22 March 2018. [Google Scholar] [CrossRef]
- Condino, S.; Turini, G.; Parchi, P.D.; Viglialoro, R.M.; Piolanti, N.; Gesi, M.; Ferrari, M.; Ferrari, V. How to Build a Patient-Specific Hybrid Simulator for Orthopaedic Open Surgery: Benefits and Limits of Mixed-Reality Using the Microsoft HoloLens. J. Healthc. Eng. 2018. [Google Scholar] [CrossRef]
- Bimber, O.; Raskar, R. Spatial Augmented Reality Merging Real and Virtual Worlds; AK Peters/CRC Press: Boca Raton, FL, USA, 2005. [Google Scholar] [CrossRef]
- Alem, L.; Huang, W. Recent Trends of Mobile Collaborative Augmented Reality Systems; Springer: New York, NY, USA, 2011. [Google Scholar]
- Viglialoro, R.M.; Turini, G.; Condino, S.; Ferrari, V.; Gesi, M. Proof of Concept: VR Rehabilitation Game for People with Shoulder Disorders. Lect. Notes Comput. Sci. 2019, 344–350. [Google Scholar] [CrossRef]
- Microsoft. Microsoft Research Blog. Available online: https://www.microsoft.com/en-us/research/blog/ (accessed on 1 July 2019).
- González-Villanueva, L.; Cagnoni, S.; Ascari, L. Design of a wearable sensing system for human motion monitoring in physical rehabilitation. Sensors 2013, 13, 7735–7755. [Google Scholar] [CrossRef]
- Qian, L.; Barthel, A.; Johnson, A.; Osgood, G.; Kazanzides, P.; Navab, N.; Fuerst, B. Comparison of optical see-through head-mounted displays for surgical interventions with object-anchored 2D-display. Int J. CARS 2017, 12, 901–910. [Google Scholar] [CrossRef]
- Microsoft App Quality Criteria. Available online: https://docs.microsoft.com/en-us/windows/mixed-reality/app-quality-criteria (accessed on 1 July 2019).
- Viglialoro, R.; Esposito, N.; Condino, S.; Cutolo, F.; Guadagni, S.; Gesi, M.; Ferrari, M.; Ferrari, V. Augmented Reality to Improve Surgical Simulation. Lessons Learned Towards the Design of a Hybrid Laparoscopic Simulator for Cholecystectomy. IEEE Trans. Biomed. Eng. 2018, 66, 2091–2104. [Google Scholar] [CrossRef]
- Condino, S.; Viglialoro, R.M.; Fani, S.; Bianchi, M.; Morelli, L.; Ferrari, M.; Bicchi, A.; Ferrari, V. Tactile Augmented Reality for Arteries Palpation in Open Surgery Training. Lect. Notes Comput. Sci. 2016, 186–197. [Google Scholar] [CrossRef]
- Viglialoro, R.; Condino, S.; Freschi, C.; Cutolo, F.; Gesi, M.; Ferrari, M.; Ferrari, V. AR visualization of “synthetic Calot’s triangle” for training in cholecystectomy. In Proceedings of the 12th IASTED International Conference on Biomedical Engineering, BioMed, Innsbruck, Austria, 15–17 February 2016. [Google Scholar]
- Zahiri, M.; Nelson, C.A.; Oleynikov, D.; Siu, K.C. Evaluation of Augmented Reality Feedback in Surgical Training Environment. Surg. Innov. 2018, 25, 81–87. [Google Scholar] [CrossRef]
- Yamauchi, Y. Smart Dry Lab: An Augmented Reality (AR) Based Surgical Training Box. Stud. Health Technol. Inform. 2014, 196, 476–478. [Google Scholar]
- Loukas, C.; Lahanas, V.; Georgiou, E. An integrated approach to endoscopic instrument tracking for augmented reality applications in surgical simulation training. Int. J. Med. Robot. Comput. Assist. Surg. MRCAS 2013, 9, 34–51. [Google Scholar] [CrossRef]
- Chytas, D.; Malahias, M.A.; Nikolaou, V.S. Augmented Reality in Orthopedics: Current State and Future Directions. Front. Surg. 2019, 6, 38. [Google Scholar] [CrossRef]
- Salehahmadi, F.; Hajialiasgari, F. Grand Adventure of Augmented Reality in Landscape of Surgery. World J. Plast. Surg. 2019, 8, 135–145. [Google Scholar] [CrossRef]
- Dodd, K.; Brooks, N.P. The Development of Augmented Reality to Enhance Minimally Invasive Surgery. Surg. Technol. Int. 2017, 31, 19–24. [Google Scholar]
- Thomas, D.J. Augmented reality in surgery: The Computer-Aided Medicine revolution. Int. J. Surg. 2016, 36, 25. [Google Scholar] [CrossRef]
- Dunn, J.; Yeo, E.; Moghaddampour, P.; Chau, B.; Humbert, S. The treatment of phantom limb pain: A literature review. NeuroRehabilitation 2017, 40, 595–601. [Google Scholar] [CrossRef]
- Melero, M.; Hou, A.; Cheng, E.; Tayade, A.; Lee, S.C.; Unberath, M.; Navab, N. Upbeat: Augmented Reality-Guided Dancing for Prosthetic Rehabilitation of Upper Limb Amputees. J. Healthc. Eng. 2019, 2019, 2163705. [Google Scholar] [CrossRef]
- Ku, J.; Kim, Y.J.; Cho, S.; Lim, T.; Lee, H.S.; Kang, Y.J. Three-Dimensional Augmented Reality System for Balance and Mobility Rehabilitation in the Elderly: A Randomized Controlled Trial. Cyberpsychol. Behav. Soc. Netw. 2019, 22, 132–141. [Google Scholar] [CrossRef]
- Correa-Agudelo, E.; Ferrin, C.; Velez, P.; Gomez, J.D. Computer Imagery and Neurological Rehabilitation: On the Use of Augmented Reality in Sensorimotor Training to Step Up Naturally Occurring Cortical Reorganization in Patients Following Stroke. Stud. Health Technol. Inform. 2016, 220, 71–76. [Google Scholar]
- Luo, X.; Kline, T.; Fischer, H.; Stubblefield, K.; Kenyon, R.; Kamper, D. Integration of augmented reality and assistive devices for post-stroke hand opening rehabilitation. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Shanghai, China, 17–18 January 2006; Volume 7, pp. 6855–6858. [Google Scholar] [CrossRef]

| Virtual Trajectory | Shoulder Movements | ||||||
|---|---|---|---|---|---|---|---|
| % Visible with HoloLens | Width [m] | Height [m] | Horizontal Flexion * | Vertical Flexion ** | |||
| ROM [°] | % of ROM Target | ROM [°] | % of ROM Target | Number of Grid Cells | |||
| 100% | 1.1 | 0.6 | 29 | 47% | 17 | 33% | 66 |
| 67% | 1.7 | 0.9 | 40 | 66% | 24 | 47% | 153 |
| 50% | 2.2 | 1.2 | 48 | 78% | 31 | 61% | 264 |
| 44% | 2.5 | 1.4 | 51 | 84% | 35 | 69% | 350 |
| 40% | 2.8 | 1.5 | 54 | 89% | 37 | 72% | 420 |
| 38% | 3.0 | 1.7 | 56 | 92% | 40 | 79% | 510 |
| 33% | 3.3 | 1.8 | 59 | 96% | 42 | 82% | 594 |
| Number of Subjects | |
|---|---|
| Physiotherapists (yes, no) | 5, 20 |
| Gender (male, female, non-binary) | 14, 11, 0 |
| Age (min, max, mean, standard deviation) | 23, 52, 32, 7.4 |
| Handedness (left, right, ambidextrous) | 2, 23, 0 |
| Vision (10/10 naked eyes, corrected to 10/10 with lenses) | 17, 8 |
| Experience with Video games (none, limited, familiar, experienced) * | 5, 4, 8, 8 |
| Experience with AR (none, limited, familiar, experienced) * | 8, 9, 6, 6 |
| Experience with HoloLens (none, limited, familiar, experienced) * | 16, 6, 1, 2 |
| Item | Median (25°~75°) | p-Value (All) | |||||
|---|---|---|---|---|---|---|---|
| Ph | N-Ph | All | VG | AR | HL | ||
| Engagement |
| 4 (4–4) | 5 (4–5) | 4 (4–5) | 0.618 | 0.175 | 0.439 |
| 4 (3–4) | 4 (3–4.25) | 4 (3–4) | 0.243 | 0.723 | 0.730 | |
| 4 (3–4) | 4 (3–5) | 4 (3–5) | 0.748 | 0.380 | 0.301 | |
| 4 (4–4) | 5 (4–5) | 4 (4–5) | 0.414 | 0.246 | 0.337 | |
| 4 (4–5) | 4 (4–5) | 4 (4–5) | 0.330 | 0.466 | 0.447 | |
| Ergonomics |
| 4 (3–4) | 4 (4–5) | 4 (4–4) | 0.643 | 0.324 | 0.997 |
| 4 (3–4) | 4 (4–5) | 4 (4–5) | 0.445 | 0.270 | 0.612 | |
| 3 (3–4) | 3.5 (2.75–4) | 3 (3–4) | 0.522 | 0.436 | 0.218 | |
| 3 (2–4) | 4 (4–5) | 4 (3–5) | 0.647 | 0.740 | 0.407 | |
| 4 (4–4) | 4 (4–5) | 4 (4–5) | 0.070 | 0.727 | 0.837 | |
| 4 (3–4) | 5 (4–5) | 5 (4–5) | 0.253 | 0.169 | 0.283 | |
| 4 (3–4) | 4 (3–4) | 4 (3–4) | 0.555 | 0.760 | 0.586 | |
| 3 (2–3) | 5 (3.75–5) | 4 (3–5) | 0.018 | 0.353 | 0.140 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Condino, S.; Turini, G.; Viglialoro, R.; Gesi, M.; Ferrari, V. Wearable Augmented Reality Application for Shoulder Rehabilitation. Electronics 2019, 8, 1178. https://doi.org/10.3390/electronics8101178
Condino S, Turini G, Viglialoro R, Gesi M, Ferrari V. Wearable Augmented Reality Application for Shoulder Rehabilitation. Electronics. 2019; 8(10):1178. https://doi.org/10.3390/electronics8101178
Chicago/Turabian StyleCondino, Sara, Giuseppe Turini, Rosanna Viglialoro, Marco Gesi, and Vincenzo Ferrari. 2019. "Wearable Augmented Reality Application for Shoulder Rehabilitation" Electronics 8, no. 10: 1178. https://doi.org/10.3390/electronics8101178
APA StyleCondino, S., Turini, G., Viglialoro, R., Gesi, M., & Ferrari, V. (2019). Wearable Augmented Reality Application for Shoulder Rehabilitation. Electronics, 8(10), 1178. https://doi.org/10.3390/electronics8101178









