IoT-Based Wearable and Smart Health Device Solutions for Capnography: Analysis and Perspectives
Abstract
1. Introduction
- -
- By reviewing the literature and previous surveys on the topic, there is a related effort by researchers to test and validate health devices audited by innovative technologies, especially flexible ones. However, these studies have gaps regarding relevant points that this survey addresses, as indicated in Table 1 and discussed throughout the document;
- -
- Background study regarding capnography and mechanical ventilation monitoring systems;
- -
- Review of the main contributions pointed out by the research community on the topic;
- -
- Analysis and discussion of the main features and functions of innovative technologies applied to healthcare;
- -
- A comprehensive review of the performance and feasibility of smart and wearable solutions, emphasizing the importance and contributions of Internet of Things (IoT)-based solutions for capnography;
- -
- A performance comparison table of several IoT-based wearable and smart health solutions, highlighting contributions, limitations, performance, and feasibility;
- -
- Analysis and perspectives concerning relevant open issues and future perspectives within the area.
2. Capnography
2.1. Backgroud
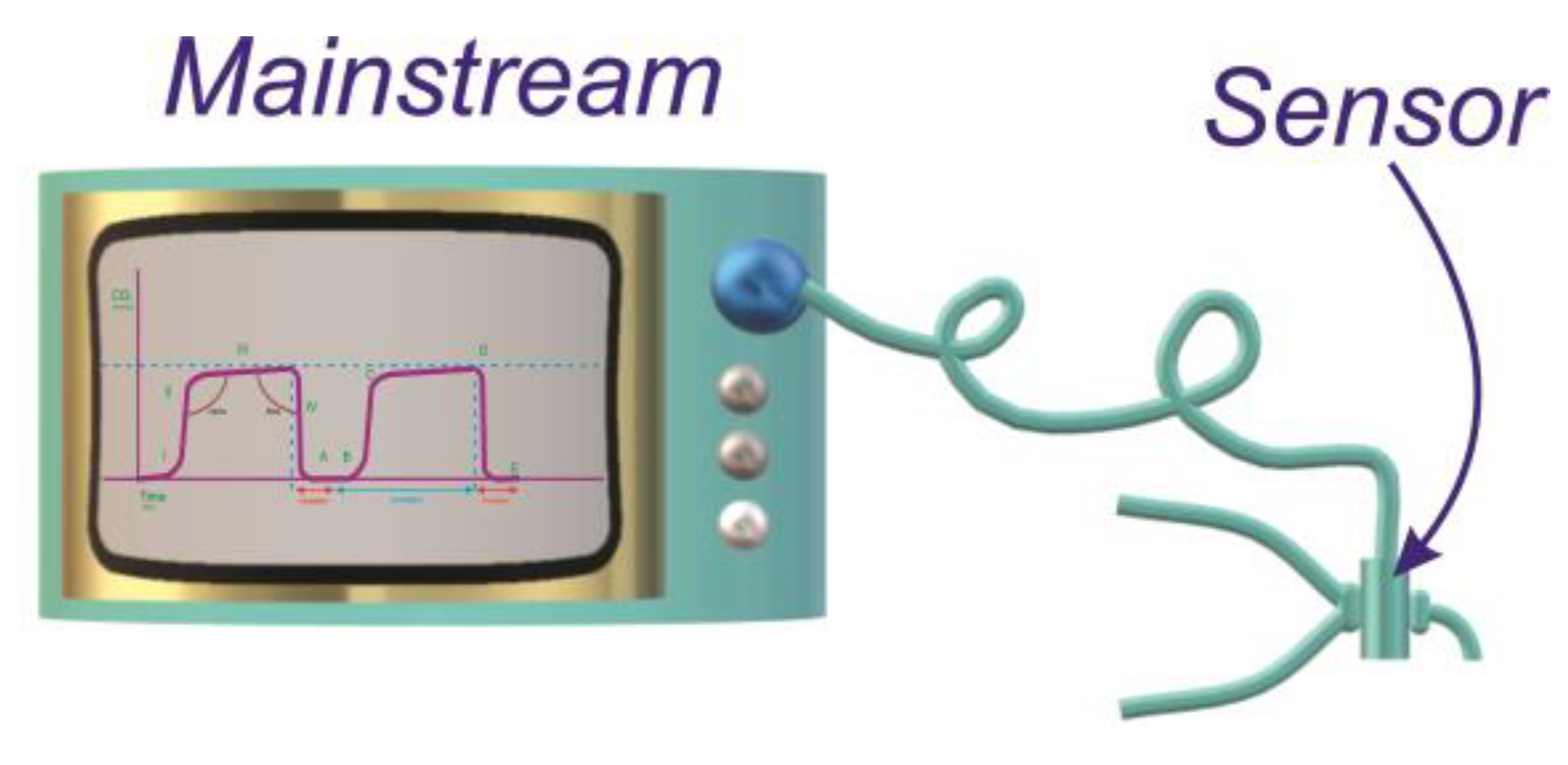
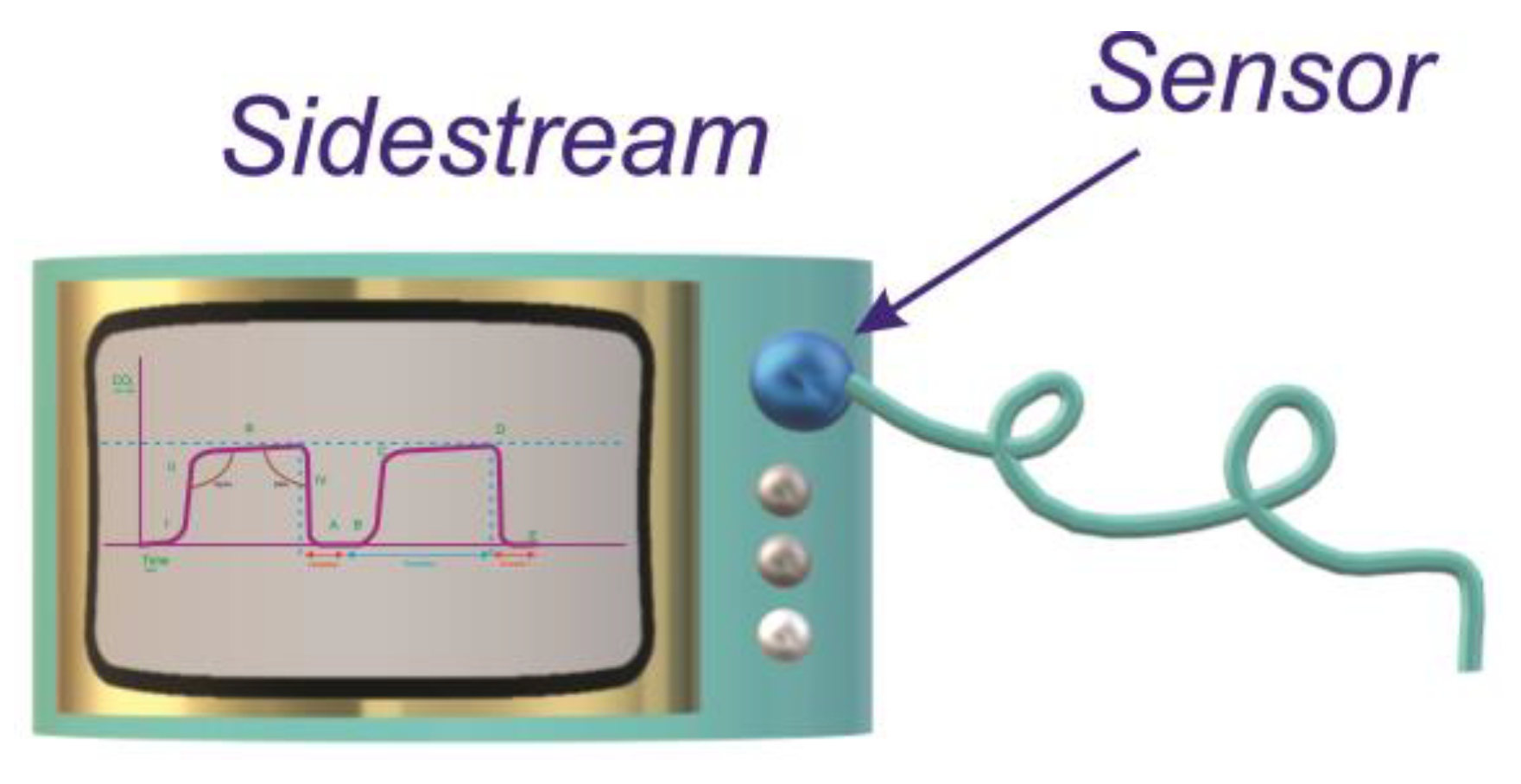
2.2. Types of Capnographs
3. Monitoring System for Mechanical Ventilation
3.1. Emergency Ventilators
- Invasive: in cases where the device is triggered to the patient via an endotracheal tube or tracheostomy
- Non-invasive: in cases where the device is connected to the patient via masks
3.2. Use of Capnography in Mechanical Ventilation Support
4. Innovative Solutions Applied to Health Care
IoT-Based Wearable Smart Health Device Solutions for Capnography
| Reference and Year | Title | IoT in General | IoHT | Contributions |
|---|---|---|---|---|
| [162], (2022) | Cloud-Assisted IoT System for Epidemic Disease Detection and Spread Monitoring | ✓ | The researchers discussed wearable technology, network architecture, wireless and wearable sensors, and the Internet of Things, and developed a prototype that uses a mobile application; the authors highlighted that this model, when compared to other technologies, demonstrated real-time monitoring, robustness, and effectiveness. | |
| [164], (2020) | Real Time Pacemaker Patient Monitoring System Based on Internet of Things | ✓ | The approach of these authors provides a discussion of the Internet of Things related to the remote monitoring system. They proposed a new electrocardiogram (ECG) monitoring method for use in pacemaker patients. This model applies IoT techniques, operates in real time with remote access, and has the ability to send and present data that is displayed on a particular website (www.thinger.io) through the Wi-Fi protocol. | |
| [165], (2021) | Research and development of an IoT-based remote asthma patient monitoring system | ✓ | The researchers addressed and discussed the disease asthma, remote patient monitoring (RPM), and technological applications such as the MAX30100 pulse oximeter and heart rate sensor, precision non-contact thermometer GY-906 MLX90614, humidity and temperature sensor DHT11, MQ-135 gas sensor, AD8232 ECG sensor, Android studio, Java, and programming languages. In their research they implemented a monitoring system that allows physicians to monitor asthmatic patients from a remote area. The authors even developed the back-end using Django—open-source web architecture based on Python, and the front-end through a website application, hypertext mark-up language (HTML), cascading style sheets (CSS), Javascript, and jQuery. | |
| [166], (2020) | Resilient Respiration Rate Monitoring with Real-time Bimodal CSI Data | - | - | The authors’ discussion covers monitoring, wireless fidelity sensors, data preprocessing, biomedical monitoring, fading channels, and orthogonal frequency division multiplexing—OFDM. They presented a monitoring system called ResBeat, based on 5 GHz Wi-Fi techniques to exploit bimodal channel state (CSI) information, including amplitude and phase difference, for real-time, long-term, contactless respiratory rate monitoring. Although the authors did not use IoT, the device demonstrated effectiveness and efficiency, as it was extensively tested in three different environments, compared to two alternative methods, and was considered to have superior performance and feasibility. |
| [167], (2021) | Design and validation of a handheld capnography device for cardiopulmonary assessment based on the Arduino platform | - | - | The research addresses the pertinent issues of capnography, discusses the technologies of infrared CO2 sensors, and discusses Arduino-specific algorithms for reading CO2 in breathing. They developed a portable monitoring system for use in hospital and home environments. |
| [168], (2021) | Sensors for daily life: a review | - | - | The researchers contributed a detailed review of types of modern sensors that are used in everyday life, discussing associated nomenclature and measurements for sensors, in addition to the numerous applications of the technology of these devices. Their study considers a relationship with the health area that attends to a variety of cases, including the elderly, athletes, and patients at risk. |
| [169], (2019) | Unsupervised Detection of Apnea Using Commodity RFID Tags With a Recurrent Variational Autoencoder | ✓ | The authors’ approach considers a discussion about the impact of the Internet of Things applied to health, particularly in the vital signs monitoring system, to assist patients with respiratory diseases. They implemented the AutoTag system, applying an unsupervised recurrent variational-autoencoder-based method for estimating respiratory rate and detecting abnormal respiration with commercially available RFID tags. | |
| [170], (2018) | Recurrent Variational Autoencoder for Unsupervised Apnea Detection with RFID Tags | - | - | The researchers addressed the application of the Internet of Things in healthcare and discussed RFID technologies, frequency-hopping with real-time calibration for RFID systems. They also analyzed the importance of monitoring continuous breathing in cases of apnea. To answer these questions, they suggested a new method of respiratory rate monitoring system called “Auto Tag” with the function of a recurrent variational autoencoder for detection of apnea and respiration. |
| [171], (2019) | Prototype of On-Board Platform for Measuring Vital Signs Using IoT | ✓ | The research discusses embedded technology e-Health platform techniques based on the IoT, artificial neural networks, Arduino UNO R3, embedded platforms, and the application of various sensors, such as the AMS 5915 blood pressure sensor, AD8232 electrocardiogram sensor, breathing apparatus MAX30100, and IR body temperature sensor MLX90614. They developed an experimental wearable device indicated for general-purpose use. | |
| [176], (2018) | An Intelligent Real Time IoT Based System (IRTBS) for Monitoring ICU Patient | ✓ | The authors addressed relevant issues of the Internet of Things, (IoT) such as high technicalization, robustness, and accuracy, in addition to studying sensors and intercommunicating devices. The researchers proposed an IoT-based monitoring system with remote access, fast communication between the health team, proactive and fast treatment, error reduction and time savings. |
5. Analysis, Discussion, and Open Issues
Open Issues
- Application of modern and flexible sensors in capnography. Modern and flexible sensors can considerably reduce the cost of the capnograph in terms of development and production because they are abundantly found in the market and considered robust devices by the literature.
- Application of the IoT Blynk platform in capnography. The IoT Blynk platform provides the ability to integrate and develop devices with remote and real-time management. It can offer to healthcare professionals a continuous and fast monitoring system, since it has a robust, dynamic, effective, and efficient architecture.
- 3D prototyping technologies to develop capnographs. The use of 3D technology has been an excellent alternative in device development, primarily “emergency” devices. These devices were widely used in the most serious period of the COVID-19 pandemic due to their low cost and fast production process. The use of 3D technology can involve lightweight and comfortable materials, offering remarkable functions and features, such as safety, ease of use, adjustability, and flexibility.
- Development of a flexible and intelligent monitoring system. This can promote evolution in mechanical ventilation support and revolutionize healthcare systems worldwide, making service stations in intensive care units much more dynamic and safer. Furthermore, it may impact e-Health applications and help in other contexts of pandemic crises in the future.
6. Lessons Learned
7. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mobilio, M.; Kato, T.; Kudo, H.; Micucci, D. Ambient Assisted Living for an Ageing Society: A Technological Overview. AI* AAL 2016, 1803, 43–58. [Google Scholar]
- Kotfis, K.; Williams Roberson, S.; Wilson, J.E.; Dabrowski, W.; Pun, B.T.; Ely, E. COVID-19: ICU delirium management during SARS-CoV-2 pandemic. Crit. Care 2020, 24, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Andrews, L.J.; Benken, S.T. COVID-19: ICU delirium management during SARS-CoV-2 pandemic—Pharmacological considerations. Crit. Care 2020, 24, 1–2. [Google Scholar] [CrossRef]
- Mirvakili, S.M.; Sim, D.; Langer, R. Inverse Pneumatic Artificial Muscles for Application in Low-Cost Ventilators. Adv. Intell. Syst. 2021, 3, 2000200. [Google Scholar] [CrossRef]
- Mirvakili, S.M.; Sim, D.; Langer, R. Reverse Pneumatic Artificial Muscles for Application in Low-Cost Artificial Respirators. Biorxiv 2020. [Google Scholar] [CrossRef]
- Wang, Y.; Kung, L.; Byrd, T.A. Big data analytics: Understanding its capabilities and potential benefits for healthcare organizations. Technol. Forecast. Soc. Change 2018, 126, 3–13. [Google Scholar] [CrossRef]
- Nasajpour, M.; Pouriyeh, S.; Parizi, R.M.; Dorodchi, M.; Valero, M.; Arabnia, H.R. Internet of Things for current COVID-19 and future pandemics: An exploratory study. J. Healthc. Inform. Res. 2020, 4, 325–364. [Google Scholar] [CrossRef]
- Islam, M.M.; Rahaman, A.; Islam, M.R. Development of smart healthcare monitoring system in IoT environment. SN Comput. Sci. 2020, 1, 185. [Google Scholar] [CrossRef] [PubMed]
- Chaari, M.Z.; Al-Rahimi, R.; Aljaberi, A. Real-Time Monitoring of Indoor Healthcare Tracking Using the Internet of Things Based IBeacon. In International Conference on Remote Engineering and Virtual Instrumentation; Springer: Cham, Switzerland, 2021; pp. 332–342. [Google Scholar]
- Khan, Z.H.; Siddique, A.; Lee, C.W. Robotics utilization for healthcare digitization in global COVID-19 management. Int. J. Environ. Res. Public Health 2020, 17, 3819. [Google Scholar] [CrossRef]
- Belfiore, M.P.; Urraro, F.; Grassi, R.; Giacobbe, G.; Patelli, G.; Cappabianca, S.; Reginelli, A. Artificial intelligence to codify lung CT in Covid-19 patients. La Radiol. Med. 2020, 125, 500–504. [Google Scholar] [CrossRef]
- Biermann, S.; Magi, A.; Sachse, P.; Hoffmann, M.; Wedrich, K.; Müller, L.; Koppert, R.; Ortlepp, T.; Baldauf, J. Advanced broadband MEMS infrared emitter based on high-temperature-resistant nanostructured surfaces and packaging solutions for harsh environments. Terahertz RF Millim. Submillimeter-Wave Technol. Appl. XIII SPIE 2020, 11279, 31–45. [Google Scholar] [CrossRef]
- Jing, Y.; Yuhua, C.; Yupeng, Y.; Xiaofei, L.; Zuwei, Z.; Ming, X.; Dengpan, W.; Jiangdong, M.; Yong, M.; Yuzhe, Z. Design and optimization of an integrated MEMS gas chamber with high transmissivity. Digit. Commun. Netw. 2021, 7, 82–91. [Google Scholar] [CrossRef]
- Mandel, J.C.; Kreda, D.A.; Mandl, K.D.; Kohane, I.S.; Ramoni, R.B. SMART on FHIR: A standards-based, interoperable apps platform for electronic health records. J. Am. Med. Inform. Assoc. 2016, 23, 899–908. [Google Scholar] [CrossRef]
- Ozer, T.; Agir, I.; Henry, C.S. Rapid prototyping of ion-selective electrodes using a low-cost 3D printed internet-of-things (IoT) controlled robot. Talanta 2022, 247, 123544. [Google Scholar] [CrossRef] [PubMed]
- Firouzi, F.; Farahani, B.; Daneshmand, M.; Grise, K.; Song, J.; Saracco, R.; Wang, L.L.; Lo, K.; Angelov, P.; Soares, E.; et al. Harnessing the power of smart and connected health to tackle COVID-19: Iot, ai, robotics, and blockchain for a better world. IEEE Internet Things J. 2021, 8, 12826–12846. [Google Scholar] [CrossRef]
- Austin, P.N.; Branson, R.D. Using anesthesia machines as critical care ventilators during the COVID-19 pandemic. Respir. Care 2021, 66, 1184–1195. [Google Scholar] [CrossRef]
- Vahidi, H.; Taleai, M.; Yan, W.; Shaw, R. Digital citizen science for responding to COVID-19 crisis: Experiences from Iran. Int. J. Environ. Res. Public Health 2021, 18, 9666. [Google Scholar] [CrossRef]
- Guvener, O.; Eyidogan, A.; Oto, C.; Huri, P.Y. Novel additive manufacturing applications for communicable disease prevention and control: Focus on recent COVID-19 pandemic. Emergent Mater. 2021, 4, 351–361. [Google Scholar] [CrossRef] [PubMed]
- Guvener, O.; Eyidogan, A.; Oto, C.; Huri, P.Y. Robotics, smart wearable technologies, and autonomous intelligent systems for healthcare during the COVID-19 pandemic: An analysis of the state of the art and future vision. Adv. Intell. Syst. 2020, 2, 2000071. [Google Scholar]
- Henkel, A.P.; Čaić, M.; Blaurock, M.; Okan, M. Robotic transformative service research: Deploying social robots for consumer well-being during COVID-19 and beyond. J. Serv. Manag. 2020, 31, 1131–1148. [Google Scholar] [CrossRef]
- Alsamhi, S.H.; Lee, B. Blockchain for Multi-Robot Collaboration to Combat COVID-19 and Future Pandemics. arXiv 2020, arXiv:2010.02137. [Google Scholar]
- Zemmar, A.; Lozano, A.M.; Nelson, B.J. The rise of robots in surgical environments during COVID-19. Nat. Mach. Intell. 2020, 2, 566–572. [Google Scholar] [CrossRef]
- Shen, Y.; Guo, D.; Long, F.; Mateos, L.A.; Ding, H.; Xiu, Z.; Hellman, R.B.; King, A.; Chen, S.; Zhang, C.; et al. Robots under COVID-19 pandemic: A comprehensive survey. IEEE Access 2020, 9, 1590–1615. [Google Scholar] [CrossRef]
- Boussen, S.; Cordier, P.-Y.; Malet, A.; Simeone, P.; Cataldi, S.; Vaisse, C.; Roche, X.; Castelli, A.; Assal, M.; Pepin, G.; et al. Triage and monitoring of COVID-19 patients in intensive care using unsupervised machine learning. Comput. Biol. Med. 2022, 142, 105192. [Google Scholar] [CrossRef] [PubMed]
- Martellucci, C.A.; Flacco, M.E.; Martellucci, M.; Violante, F.S.; Manzoli, L. Inhaled CO2 concentration while wearing face masks: A pilot study using capnography. Environ. Health Insights 2022, 16, 11786302221123573. [Google Scholar]
- Dost, B.; Kömürcü, Ö.; Bilgin, S.; Dökmeci, H.; Terzi, O.; Barış, S. Investigating the Effects of Protective Face Masks on the Respiratory Parameters of Children in the Postanesthesia Care Unit During the COVID-19 Pandemic. J. PeriAnesthesia Nurs. 2022, 37, 94–99. [Google Scholar] [CrossRef]
- Ogura, T.; Ishiwatari, H.; Fujimori, N.; Iwasaki, E.; Ishikawa, K.; Satoh, T.; Kaneko, J.; Sato, J.; Oono, T.; Matsumoto, K.; et al. Propensity score matching analysis for adverse events of EUS-guided biliary drainage in advanced elderly patients (PEACE study). Ther. Adv. Gastroenterol. 2022, 15, 17562848221092612. [Google Scholar] [CrossRef]
- Li, J.; Cheng, X.; Tian, X.; Zhao, H.; Li, L. Compact carbon dioxide sensor using tunable diode laser absorption spectroscopy for capnographic monitoring. Spectrosc. Lett. 2022, 55, 183–191. [Google Scholar] [CrossRef]
- Fouzas, S.; Kentgens, A.-C.; Lagiou, O.; Frauchiger, B.S.; Wyler, F.; Theodorakopoulos, I.; Yammine, S.; Latzin, P. Novel volumetric capnography indices measure ventilation inhomogeneity in cystic fibrosis. ERJ Open Res. 2022, 8, 00440–2021. [Google Scholar] [CrossRef]
- Baucas, M.J.; Spachos, P.; Gregori, S. Internet-of-Things Devices and Assistive Technologies for Health Care: Applications, Challenges, and Opportunities. IEEE Signal Process. Mag. 2021, 38, 65–77. [Google Scholar] [CrossRef]
- Merry, A.F.; Cooper, J.B.; Soyannwo, O.; Wilson, I.H.; Eichhorn, J.H. An iterative process of global quality improvement: The International Standards for a Safe Practice of Anesthesia 2010. Can. J. Anesth./J. Can. D’anesthésie 2010, 57, 1021–1026. [Google Scholar] [CrossRef] [PubMed]
- Rahmani, A.M.; Gia, T.N.; Negash, B.; Anzanpour, A.; Azimi, I.; Jiang, M.; Liljeberg, P. Exploiting smart e-Health gateways at the edge of healthcare Internet-of-Things: A fog computing approach. Future Gener. Comput. Syst. 2018, 78, 641–658. [Google Scholar] [CrossRef]
- Raj, P.; Chatterjee, J.M.; Kumar, A.; Balamurugan, B. (Eds.) Internet of Things Use Cases for the Healthcare Industry; Springer: Berlin/Heidelberg, Germany, 2020. [Google Scholar]
- Charulatha, A.R.; Sujatha, R. Smart healthcare use cases and applications. In Internet of Things Use Cases for the Healthcare Industry; Springer: Cham, Sweitzerland, 2020; pp. 185–203. [Google Scholar]
- Shakshuki, E.M.; Reid, M.; Sheltami, T.R. An adaptive user interface in healthcare. Procedia Comput. Sci. 2015, 56, 49–58. [Google Scholar] [CrossRef]
- Alnanih, R.; Ormandjieva, O. Mapping hci principles to design quality of mobile user interfaces in healthcare applications. Procedia Comput. Sci. 2016, 94, 75–82. [Google Scholar] [CrossRef]
- Singh, R.P.; Javaid, M.; Haleem, A.; Suman, R. Internet of things (IoT) applications to fight against COVID-19 pandemic. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 521–524. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Ali, Y.; Nazir, S.; Niazi, M. ISA evaluation framework for security of internet of health things system using AHP-TOPSIS methods. IEEE Access 2020, 8, 152316–152332. [Google Scholar] [CrossRef]
- Turcu, C.; Turcu, C. Improving the Quality of Healthcare through Internet of Things. arXiv 2019. [Google Scholar] [CrossRef]
- Kaur, H.; Atif, M.; Chauhan, R. An internet of healthcare things (IoHT)-based healthcare monitoring system. In Advances in Intelligent Computing and Communication; Springer: Singapore, 2020; pp. 475–482. [Google Scholar]
- Ning, L.; Ali, Y.; Ke, H.; Nazir, S.; Huanli, Z. A hybrid MCDM approach of selecting lightweight cryptographic cipher based on ISO and NIST lightweight cryptography security requirements for internet of health things. IEEE Access 2020, 8, 220165–220187. [Google Scholar] [CrossRef]
- Klugman, C.M.; Dunn, L.B.; Schwartz, J.; Cohen, I.G. The Ethics of Smart Pills and Self-Acting Devices: Autonomy, Truth-Telling, and Trust at the Dawn of Digital Medicine. Am. J. Bioeth. 2018, 18, 38–47. [Google Scholar] [CrossRef]
- Stawarz, K.; Cox, A.L.; Blandford, A. Don’t forget your pill! Designing effective medication reminder apps that support users’ daily routines. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, Toronto, ON, Canada, 26 April–1 May 2014; pp. 2269–2278. [Google Scholar]
- Tongaonkar, A.; Dai, S.; Nucci, A.; Song, D. Understanding mobile app usage patterns using in-app advertisements. In International Conference on Passive and Active Network Measurement; Springer: Berlin/Heidelberg, Germany, 2013; pp. 63–72. [Google Scholar]
- Krieger, W.H. Medical apps: Public and academic perspectives. Perspect. Biol. Med. 2013, 56, 259–273. [Google Scholar] [CrossRef]
- Mondol, A.S.; Emi, I.A.; Stankovic, J.A. MedRem: An interactive medication reminder and tracking system on wrist devices. In Proceedings of the 2016 IEEE Wireless Health (WH), Bethesda, MD, USA, 25–27 October 2016; pp. 1–8. [Google Scholar] [CrossRef]
- Lo Presti, D.; Carnevale, A.; D’Abbraccio, J.; Massari, L.; Massaroni, C.; Sabbadini, R.; Zaltieri, M.; Di Tocco, J.; Bravi, M.; Miccinilli, S.; et al. A multi-parametric wearable system to monitor neck movements and respiratory frequency of computer workers. Sensors 2020, 20, 536. [Google Scholar] [CrossRef]
- Al-Halhouli, A.A.; Al-Ghussain, L.; El Bouri, S.; Habash, F.; Liu, H.; Zheng, D. Clinical evaluation of stretchable and wearable inkjet-printed strain gauge sensor for respiratory rate monitoring at different body postures. Appl. Sci. 2020, 10, 480. [Google Scholar] [CrossRef]
- Lamberti, J.P. Respiratory monitoring in general care units. Respir. Care 2020, 65, 870–881. [Google Scholar] [CrossRef] [PubMed]
- Mandzukovska, H.; Sofijanova, A.; Naunova-Timovska, S.; Voinovska, T.; Kimovska-Hristov, M.; Jordanovska, O. High Frequency Oscillatory Ventilation in Infants: The Clinical Practice in N. Macedonia. Maced. J. Anaesth. 2021. Available online: https://repository.ukim.mk/handle/20.500.12188/15374 (accessed on 2 February 2023).
- Martins, I.P.M.; Nakato, A.M.; Hembecker, P.K.; Ioshii, S.O.; Nohama, P. Correlation of End-Tidal Carbon Dioxide with Arterial Carbon Dioxide in Mechanically Ventilated Neonates: A Scoping Review. Global Pediatric Health 2021, 8, 2333794X211016790. [Google Scholar] [CrossRef]
- Jacobs, F.; Scheerhoorn, J.; Mestrom, E.; van der Stam, J.; Bouwman, R.A.; Nienhuijs, S. Reliability of heart rate and respiration rate measurements with a wireless accelerometer in postbariatric recovery. PLoS ONE 2021, 16, e0247903. [Google Scholar] [CrossRef]
- Rodrigues, M.J.; Postolache, O.; Cercas, F. Physiological and Behavior Monitoring Systems for Smart Healthcare Environments: A Review. Sensors 2020, 20, 2186. [Google Scholar] [CrossRef]
- Abdulmalek, S.; Nasir, A.; Jabbar, W.A.; Almuhaya, M.A.M.; Bairagi, A.K.; Khan, A.-M.; Kee, S.-H. IoT-Based Healthcare-Monitoring System towards Improving Quality of Life: A Review. Healthcare 2022, 10, 1993. [Google Scholar] [CrossRef]
- Elhoseny, M.; Thilakarathne, N.N.; Alghamdi, M.I.; Mahendran, R.K.; Gardezi, A.A.; Weerasinghe, H.; Welhenge, A. Security and Privacy Issues in Medical Internet of Things: Overview, Countermeasures, Challenges and Future Directions. Sustainability 2021, 13, 11645. [Google Scholar] [CrossRef]
- Kashyap, V.; Kumar, A.; Kumar, A.; Hu, Y.-C. A Systematic Survey on Fog and IoT Driven Healthcare: Open Challenges and Research Issues. Electronics 2022, 11, 2668. [Google Scholar] [CrossRef]
- Junaid, S.B.; Imam, A.A.; Abdulkarim, M.; Surakat, Y.A.; Balogun, A.O.; Kumar, G.; Shuaibu, A.N.; Garba, A.; Sahalu, Y.; Mohammed, A.; et al. Recent Advances in Artificial Intelligence and Wearable Sensors in Healthcare Delivery. Appl. Sci. 2022, 12, 10271. [Google Scholar] [CrossRef]
- Stavropoulos, T.G.; Papastergiou, A.; Mpaltadoros, L.; Nikolopoulos, S.; Kompatsiaris, I. IoT Wearable Sensors and Devices in Elderly Care: A Literature Review. Sensors 2020, 20, 2826. [Google Scholar] [CrossRef] [PubMed]
- He, T.; Lee, C. Evolving Flexible Sensors, Wearable and Implantable Technologies Towards BodyNET for Advanced Healthcare and Reinforced Life Quality. IEEE Open J. Circuits Syst. 2021, 2, 702–720. [Google Scholar] [CrossRef]
- Chang, Y.; Zuo, J.; Zhang, H.; Duan, X. State-of-the-art and recent developments in micro/nanoscale pressure sensors for smart wearable devices and health monitoring systems. Nanotechnol. Precis. Eng. 2019, 3, 43–52. [Google Scholar] [CrossRef]
- Thomas, A.; McGrath, B. Patient safety inci-dents associated with airway devices in critical care: A review of reports to the uk national patient safetyagency. Anaesthesia 2009, 64, 358–365. [Google Scholar] [CrossRef]
- Kannan, S.; Manji, M. Survey of use of end-tidalcarbon dioxide for confirming tracheal tube placement in intensive care units in the uk. Anaesthesia 2003, 58, 476–479. [Google Scholar] [CrossRef]
- Georgiou, A.P.; Gouldson, S.; Amphlett, A.M. The use of capnography and the availability of air-way equipment on intensive care units in the uk andthe republic of ireland. Anaesthesia 2010, 65, 462–467. [Google Scholar] [CrossRef]
- Lamperti, M.; Biasucci, D.G.; Disma, N.; Pittiruti, M.; Breschan, C.; Vailati, D.; Subert, M.; Traškaite, V.; Macas, A.; Estebe, J.P.; et al. European Society of Anaesthesiology guidelines on peri-operative use of ultrasound-guided for vascular access (PERSEUS vascular access). Eur. J. Anaesthesiol. 2020, 37, 344–376. [Google Scholar] [CrossRef] [PubMed]
- Honardar, M.R.; Posner, K.L.; Domino, K.B. Delayed detection of esophageal intubation in anesthesia malpractice claims: Brief report of a case series. Anesth. Analg. 2017, 125, 1948. [Google Scholar] [CrossRef]
- Pinto, A.L.R. Relatório de Estágio no Serviço de Anestesiologia e no Serviço de Cuidados Intensivos. Available online: file:///C:/Users/MDPI/Downloads/302922577.pdf (accessed on 2 February 2023).
- Bodenham Chair, A.; Babu, S.; Bennett, J.; Binks, R.; Fee, P.; Fox, B.; Johnston, A.J.; Klein, A.A.; Langton, J.A.; Mclure, H.; et al. Association of Anaesthetists of Great Britain and Ireland: Safe vascular access. Anaesthesia 2016, 71, 573–585. [Google Scholar] [CrossRef]
- Huang, C.H.; Wei, K.H. Applications of capnography in airway management outside the operating room. Signa Vitae 2021, 17, 18–24. [Google Scholar]
- Gelb, A.W.; Morriss, W.W.; Johnson, W.; Merry, A.F. World Health Organization-World Federation of Societies of Anaesthesiologists (WHO-WFSA) international standards for a safe practice of anesthesia. Can. J. Anesth./J. Can. D’anesthésie 2018, 65, 698–708. [Google Scholar] [CrossRef] [PubMed]
- McQueen, K.; Coonan, T.; Ottaway, A.; Hendel, S.; Bagutifils, P.R.; Froese, A.; Neighbor, R.; Perndt, H. The bare minimum: The reality of global anaesthesia and patient safety. World J. Surg. 2015, 39, 2153–2160. [Google Scholar] [CrossRef]
- Korsós, A.; Peták, F.; Südy, R.; Schranc, Á.; Fodor, G.H.; Babik, B. Use of capnography to verify emergency ventilator sharing in the COVID-19 era. Respir. Physiol. Neurobiol. 2021, 285, 103611. [Google Scholar] [CrossRef]
- Russotto, V.; Cook, T.M. Capnography use in the critical care setting: Why do clinicians fail to implement this safety measure? Br. J. Anaesth. 2021, 127, 661–664. [Google Scholar] [CrossRef]
- Goonasekera, C.; Smith, E.-J. The Basics of Intra-Operative Neurophysiological Monitoring for the Clinician: A Practical Guide; Cambridge Scholars Publishing: Newcastle Upon Tyne, UK, 2021; ISBN 9781527570436. [Google Scholar]
- Pandit, J.J.; Eriksson, L.I. Reversing neuromuscular blockade: Not just the diaphragm, but carotid body function too. Anesthesiology 2019, 131, 453–455. [Google Scholar] [CrossRef]
- Cascella, M.; Bimonte, S.; Amruthraj, N.J. Awareness during emergence from anesthesia: Features and future research directions. World J. Clin. Cases 2020, 8, 245. [Google Scholar] [CrossRef] [PubMed]
- Chung, F.; Wong, J.; Mestek, M.L.; Niebel, K.H.; Lichtenthal, P. Characterization of respiratory compromise and the potential clinical utility of capnography in the post-anesthesia care unit: A blinded observational trial. J. Clin. Monit. Comput. 2019, 34, 541–551. [Google Scholar] [CrossRef] [PubMed]
- Khanna, A.K.; Bergese, S.D.; Jungquist, C.R.; Morimatsu, H.; Uezono, S.; Lee, S.; Ti, L.K.; Urman, R.D.; McIntyre, R., Jr.; Tornero, C.; et al. Prediction of opioid-induced respiratory depression on inpatient wards using continuous capnography and oximetry: An international prospective, observational trial. Anesth. Analg. 2020, 131, 1012. [Google Scholar] [CrossRef]
- Ahrens, T. The most important vital signs are not being measured. Aust. Crit. Care 2008, 21, 3–5. [Google Scholar] [CrossRef]
- Saleh, H.; Younis, E.M.G.; Sahal, R.; Ali, A.A. Predicting Systolic Blood Pressure in Real-Time Using Streaming Data and Deep Learning. Mob. Netw. Appl. 2020, 26, 326–335. [Google Scholar] [CrossRef]
- Elliott, M.; Coventry, A. Critical Care: The Oight Vital Signs of Patient Monitoring. Br. J. Nurs. 2012, 21, 621–625. [Google Scholar] [CrossRef] [PubMed]
- Musumeci, M.M.; Martinez, B.P.; Nogueira, I.C.; Alcanfor, T. Re-cursos fisioterapêuticos utilizados em unidades deterapia intensiva para avaliação e tratamento das disfunções respiratórias de pacientes com COVID-19. Assobrafir Ciência 2020, 11 (Suppl. S1), 73–86. [Google Scholar] [CrossRef]
- Semmelmann, A.; Loop, T. Anesthesia for interventional pulmonology. Curr. Opin. Anaesthesiol. 2021, 35, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Demirel, I.; Altun, A.Y.; Bolat, E.; Kilinc, M.; Deniz, A.; Aksu, A.; Bestas, A. Effect of patient state index monitoring on the recovery characteristics in morbidly obese patients: Comparison of inhalation anesthesia and total intravenous anesthesia. J. PeriAnesthesia Nurs. 2021, 36, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Brennan, L.; Oduro-Dominah, L.; Oduro-Dominah, L. Neonatal anaesthesia. In Neonatal Intensive Care Nursing; Routledge: London, UK, 2019; pp. 517–550. [Google Scholar]
- Bhende, M.S. End-tidal carbon dioxide monitoring in pediatrics: Concepts and technology. J. Postgrad. Med. 2002, 47, 153. [Google Scholar]
- Bhende, M.S.; Lacovey, D.C. End tidal carbon dioxide monitoring in pediatrics-clinical applications. Prehospital Emerg. Care 2001, 5, 208–213. [Google Scholar] [CrossRef]
- Wollner, E.; Nourian, M.M.; Booth, W.; Conover, S.; Law, T.; Lilaonitkul, M.; Gelb, A.W.; Lipnick, M.S. The impactof capnography on patient safety in high and low-income settings: A scoping review. Br. J. Ofanaesthesia 2020, 125, e88–e103. [Google Scholar] [CrossRef]
- Weiniger, C.F.; Akdagli, S.; Turvall, E.; Deutsch, L.; Carvalho, B. Prospective observational investigation of capnography and pulse oximetry monitoring after cesarean delivery with intrathecal morphine. Obstet. Anesth. Dig. 2019, 128, 513–522. [Google Scholar]
- Jungquist, C.R.; Chandola, V.; Spulecki, C.; Nguyen, K.V.; Crescenzi, P.; Tekeste, D.; Sayapaneni, P.R. Identifying Patients Experiencing Opioid-Induced Respiratory Depression During Recovery from Anesthesia: The Application of Electronic Monitoring Devices. Worldviews Evid. -Based Nurs. 2019, 16, 186–194. [Google Scholar] [CrossRef]
- Dobson, G.; Chow, L.; Flexman, A.; Hurdle, H.; Kurrek, M.; Laflamme, C.; Perrault, M.A.; Sparrow, K.; Stacey, S.; Swart, P.; et al. Guidelines to the practice of anesthesia–revised edition 2019. Can. J. Anesth./J. Can. D’anesthésie 2019, 66, 75–108. [Google Scholar] [CrossRef] [PubMed]
- Lipnick, M.S.; Mavoungou, P.; Gelb, A.W. The global capnography gap: A call to action. Anaesthesia 2019, 74, 147–150. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.Y.; Lee, D.; Ryu, H.; Han, J.H.; Ko, J.; Tyler, J.W. Capnography-guided endotracheal intubation as an alternative to existing intubation methods in rabbits. J. Am. Assoc. Lab. Anim. Sci. 2019, 58, 240–245. [Google Scholar] [CrossRef]
- Kodali, B.S. A Comprehensive Educational Website. Capnography. Available online: https://www.capnography.com/about-this-site/about-the-author (accessed on 26 February 2023).
- Williams, E.; Dassios, T.; Greenough, A.; Greenough, A. Carbon dioxide monitoring in the newborn infant. Pediatr. Pulmonol. 2021, 56, 3148–3156. [Google Scholar] [CrossRef] [PubMed]
- Cereceda-Sánchez, F.J.; Molina-Mula, J. Systematic review of capnography with mask ventilation during cardiopulmonary resuscitation maneuvers. J. Clin. Med. 2019, 8, 358. [Google Scholar] [CrossRef] [PubMed]
- Baba, Y.; Takatori, F.; Inoue, M.; Matsubara, I. A Novel Mainstream Capnometer System for Non-invasive Positive Pressure Ventilation. In Proceedings of the 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Montreal, QC, Canada, 20–24 July 2020; pp. 4446–4449. [Google Scholar] [CrossRef]
- Aoyagi, T.; Kabumoto, K.; Takatori, F.; Inoue, M. A Novel Nasal Cannula Type Mainstream Capnometer System Capable of Oxygen Administration. In Proceedings of the 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Montreal, QC, Canada, 20–24 July 2020; pp. 4450–4453. [Google Scholar] [CrossRef]
- Williams, E.; Dassios, T.; Greenough, A. GREENOUGH, Anne. Assessment of sidestream end-tidal capnography in ventilated infants on the neonatal unit. Pediatr. Pulmonol. 2020, 55, 1468–1473. [Google Scholar] [CrossRef] [PubMed]
- Pons, T.L.; Flexas, J.; von Caemmerer, S.; Evans, J.R.; Genty, B.; Ribas-Carbo, M.; Brugnoli, E. Estimating mesophyll conductance to CO2: Methodology, potential errors, and recommendations. J. Exp. Bot. 2009, 60, 2217–2234. [Google Scholar] [CrossRef]
- Boon, G.J.A.M.; Ende-Verhaar, Y.M.; Bavalia, R.; El Bouazzaoui, L.H.; Delcroix, M.; Dzikowska-Diduch, O.; Huisman, M.V.; Kurnicka, K.; A Mairuhu, A.T.; Middeldorp, S.; et al. Non-invasive early exclusion of chronic thromboembolic pulmonary hypertension after acute pulmonary embolism: The InShape II study. Thorax 2021, 76, 1002–1009. [Google Scholar] [CrossRef]
- Güntner, A.T.; Abegg, S.; Königstein, K.; Gerber, P.A.; Schmidt-Trucksäss, A.; Pratsinis, S.E. Breath sensors for health monitoring. ACS Sens. 2019, 4, 268–280. [Google Scholar] [CrossRef]
- Çardaközü, T.; Arslan, Z.İ.; Cesur, S.; Aksu, B. Comparison of hemodynamic response to tracheal intubation with two different videolaryngoscopes: A randomized clinical trial. Braz. J. Anesthesiol. 2021; in press. [Google Scholar] [CrossRef]
- Cui, Y.; Wang, Y.; Cao, R.; Li, G.; Deng, L.; Li, J. The low fresh gas flow anesthesia and hypothermia in neonates undergoing digestive surgeries: A retrospective before-after study. BMC Anesthesiol. 2020, 20, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Duyu, M.; Bektas, A.D.; Karakaya, Z.; Bahar, M.; Gunalp, A.; Caglar, Y.M.; Yersel, M.N.; Bozkurt, O. Comparing the novel microstream and the traditional mainstream method of end-tidal CO2 monitoring with respect to PaCO2 as gold standard in intubated critically ill children. Sci. Rep. 2020, 10, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Gallant, S.L. Evaluating the Impact of End-Tidal Carbon Dioxide Monitoring in Emergency Department Sepsis Patients. Ph.D. Thesis, Rutgers University-School of Nursing-RBHS, New Brunswick, NJ, USA, 2019. [Google Scholar]
- Hoff, I.E.; Høiseth, L.; Kirkebøen, K.A.; Landsverk, S.A. Volumetric and end-tidal capnography for the detection of cardiac output changes in mechanically ventilated patients early after open heart surgery. Crit. Care Res. Pract. 2019, 2019, 6393649. [Google Scholar]
- Krauss, B.; Falk, J.; Ladde, J. Carbon Dioxide Monitoring (Capnography). UpToDate. 2016. Available online: http://www.uptodate.com/contents/carbon-dioxide-monitoring-capnography (accessed on 26 February 2023).
- Uzunosmanoğlu, H.; Emektar, E.; Dağar, S.; Çorbacıoğlu, K.; Çevik, Y. Predictive value of capnography for severity of acute gastroenteritis in the emergency department. Am. J. Emerg. Med. 2020, 38, 1159–1162. [Google Scholar] [CrossRef] [PubMed]
- Baez, E. Use of Capnography during Resuscitation of Patients in Intensive Care Units. Ph.D. Thesis, Grand Canyon University, Phoenix, AZ, USA, 2021. [Google Scholar]
- Lee, Y.L.; Hwang, K.Y.; Yew, W.S.; Ng, S.Y. An abnormal capnography trace due to air embolism in the lateral position. BMJ Case Rep. CP 2019, 12, e231316. [Google Scholar] [CrossRef]
- Askar, H.; Misch, J.; Chen, Z.; Chadha, S.; Wang, H.-L. Capnography monitoring in procedural intravenous sedation: A systematic review and meta-analysis. Clin. Oral Investig. 2020, 24, 3761–3770. [Google Scholar] [CrossRef]
- Theissen, A.; Piriou, V.; Fuz, F.; Autran, M.; Albaladejo, P.; Trouiller, P. Serious adverse events and deaths linked to poor ventilator use: A report of four closed claims. Anaesth. Crit. Care Pain Med. 2019, 38, 143–145. [Google Scholar] [CrossRef]
- Jaffe, M.B.; Eisenkraft, J.B.; Orr, J. Respiratory Gas Monitoring. In Anesthesia Equipment, 3rd ed.; Saunders, W.B., Ed.; Wiley: Chichester, UK, 2021; pp. 195–217. ISBN 9780323672795. [Google Scholar] [CrossRef]
- Andreolio, C.; Piva, J.P.; Bruno, F.; da Rocha, T.S.; Garcia, P.C. Airway resistance and respiratory compliance in children with acute viral bronchiolitis requiring mechanical ventilation support. Indian J. Crit. Care Med. 2021, 25, 88–93. [Google Scholar] [CrossRef]
- Frat, J.P.; Ricard, J.D.; Quenot, J.P.; Pichon, N.; Demoule, A.; Forel, J.M.; Mira, J.P.; Coudroy, R.; Berquier, G.; Voisin, B.; et al. Non-invasive ventilation versus high-flow nasal cannula oxygen therapy with apnoeic oxygenation for preoxygenation before intubation of patients with acute hypoxaemic respiratory failure: A randomised, multicentre, open-label trial. Lancet Respir. Med. 2019, 7, 303–312. [Google Scholar] [CrossRef]
- Li, X.; Huang, Q.; Wu, D. Distributed large-scale co-simulation for IoT-aided smart grid control. IEEE Access 2017, 5, 19951–19960. [Google Scholar] [CrossRef]
- Rodrigues, J.J.P.C.; Sendra, S.; de la Torre, I. e-Health Systems—Theory, Advances and Technical Applications, 1st ed.; Elsevier: Amsterdam, The Netherlands, 2016; p. 296. [Google Scholar]
- Wright, B.J. Lung-protective ventilation strategies and adjunctive treatments for the emergency medicine patient with acute respiratory failure. Emerg. Med. Clin. 2014, 32, 871–887. [Google Scholar] [CrossRef] [PubMed]
- Melo, A.S.; de Almeida, R.M.S.; de Oliveira, C.D. A mecânica da ventilação mecânica. Rev. Médica Minas Gerais 2014, 24, 43–48. [Google Scholar]
- Yim, K.; Ko, H.; Yang, M.L.; Li, T.; Ip, S.; Tsui, J. A paradigm shift in the provision of improved critical care in the emergency department. Hong Kong Med. J. 2018, 293–297. [Google Scholar] [CrossRef] [PubMed]
- Fichtner, F.; Mörer, O.; Laudi, S.; Weber-Carstens, S.; Nothacker, M.; Kaisers, U. Mechanical ventilation and extracorporeal membrane oxygenation in acute respiratory insufficiency. Dtsch. Ärzteblatt Int. 2018, 115, 840. [Google Scholar] [CrossRef] [PubMed]
- Melo, E.M.; Teixeira, C.S.; de Oliveira, R.T.; de Almeida, D.T.; de Freitas, J.E.G.L.; Frota, N.M.; Studart, R.M.B. Cuidados de enfermagem ao utente sob ventilação mecânica internado em unidade de terapia intensiva. Rev. De Enferm. Ref. 2014, 4, 55–63. [Google Scholar]
- Khairuddin, A.; Azir, K.F.K.; Kan, P.E. Limitations and future of electrocardiography devices: A review and the perspective from the Internet of Things. In Proceedings of the 2017 International Conference on Research and Innovation in Information Systems (ICRIIS), Langkawi, Malaysia, 16–17 July 2017; pp. 1–7. [Google Scholar]
- Sivieri, E.M.; Eichenwald, E.C.; Rub, D.M.; Abbasi, S. An in-line high frequency flow interrupter applied to nasal CPAP: Improved carbon dioxide clearance in a premature infant lung model. Pediatr. Pulmonol. 2019, 54, 1974–1981. [Google Scholar] [CrossRef] [PubMed]
- Kreit, J.W. Volume capnography in the intensive care unit: Physiological principles, measurements, and calculations. Ann. Am. Thorac. Soc. 2019, 16, 291–300. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Haleem, A.; Deshmukh, S.G.; Javaid, M. Exploring the impact of COVID-19 pandemic on medical supply chain disruption. J. Ind. Integr. Manag. 2021, 6, 235–255. [Google Scholar] [CrossRef]
- Darwish, A.; Hassanien, A.E.; Elhoseny, M.; Sangaiah, A.K.; Muhammad, K. The impact of the hybrid platform of internet of things and cloud computing on healthcare systems: Opportunities, challenges, and open problems. J. Ambient Intell. Humaniz. Comput. 2019, 10, 4151–4166. [Google Scholar] [CrossRef]
- Bhuiyan, M.N.; Rahman, M.M.; Billah, M.M.; Saha, D. Internet of things (IoT): A review of its enabling technologies in healthcare applications, standards protocols, security, and market opportunities. IEEE Internet Things J. 2021, 8, 10474–10498. [Google Scholar] [CrossRef]
- MIT Emergency Ventilator|Design Toolbox. MIT Emergency Ventilator. Available online: https://emergency-vent.mit.edu/ (accessed on 19 April 2021).
- Christou, A.; Ntagios, M.; Hart, A.; Dahiya, R. GlasVent—The Rapidly Deployable Emergency Ventilator. Glob. Chall. 2020, 4, 2000046. [Google Scholar] [CrossRef]
- DeBoer, B.; Barari, A.; Nonoyama, M.; Dubrowski, A.; Zaccagnini, M.; Hosseini, A. Preliminary Design and Development of a Mechanical Ventilator Using Industrial Automation Components for Rapid Deployment During the COVID-19 Pandemic. Cureus 2021, 13. [Google Scholar] [CrossRef] [PubMed]
- Fiorineschi, L.; Frillici, F.S.; Rotini, F. Challenging COVID-19 with Creativity: Supporting Design Space Exploration for Emergency Ventilators. Appl. Sci. 2020, 10, 4955. [Google Scholar] [CrossRef]
- Tang, S.; Shelden, D.R.; Eastman, C.M.; Pishdad-Bozorgi, P.; Gao, X. A review of building information modeling (BIM) and the internet of things (IoT) devices integration: Present status and future trends. Autom. Constr. 2019, 101, 127–139. [Google Scholar] [CrossRef]
- Ronen, M.; Weissbrod, R.; Overdyk, F.J.; Ajizian, S. Smart respiratory monitoring: Clinical development and validation of the IPI™(Integrated Pulmonary Index) algorithm. J. Clin. Monit. Comput. 2017, 31, 435–442. [Google Scholar] [CrossRef]
- Rahaman, A.; Islam, M.; Islam, R.; Sadi, M.S.; Nooruddin, S. Developing IoT Based Smart Health Monitoring Systems: A Review. Rev. D’intelligence Artif. 2019, 33, 435–440. [Google Scholar]
- Dias, D.; Paulo Silva Cunha, J. Wearable health devices—Vital sign monitoring, systems and technologies. Sensors 2018, 18, 2414. [Google Scholar] [CrossRef]
- Selby, S.T.; Abramo, T.; Hobart-Porter, N. An update on end-tidal CO2 monitoring. Pediatr. Emerg. Care 2018, 34, 888–892. [Google Scholar] [CrossRef]
- Aminiahidashti, H.; Shafiee, S.; Kiasari, A.Z.; Sazgar, M. Applications of end-tidal carbon dioxide (ETCO2) monitoring in emergency department; a narrative review. Emergency 2018, 6, e5. [Google Scholar] [PubMed]
- Suriñach Ayats, B. Evaluating the Use of End-Tidal Carbon Dioxine in a Sepsis Code Patient as A Goalfor the Early Resuscitation Treatment in the Emergency Department. 2017. Available online: https://dugi-doc.udg.edu/handle/10256/14285 (accessed on 2 February 2023).
- Duckworth, L.P.; Rommie, L. How to read and interpret end-tidal capnography waveforms. JEMS 2017, 42, 1. [Google Scholar]
- Zamani, M.; Esfahani, M.N.; Joumaa, I.; Heydari, F. Accuracy of real-time intratracheal bedside ultrasonography and waveform capnography for confirmation of intubation in multiple trauma patients. Adv. Biomed. Res. 2018, 7, 95. [Google Scholar]
- Sandroni, C.; De Santis, P.; D’Arrigo, S. Capnography during cardiac arrest. Resuscitation 2018, 132, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Teng, W.-N.; Ting, C.-K.; Wang, Y.-T.; Hou, M.-C.; Tsou, M.-Y.; Chiang, H.; Lin, C.-L. Oral capnography is more effective than nasal capnography during sedative upper gastrointestinal endoscopy. J. Clin. Monit. Comput. 2017, 32, 321–326. [Google Scholar] [CrossRef] [PubMed]
- DiCorpo, J.E.; Schwester, D.; Dudley, L.S.; Merlin, M.A. Wave Asa Window. Using waveform capnogra-phy to achieve a bigger physiologi-cal patient picture. JEMS 2015, 40, 32–35. [Google Scholar]
- Pereira, D.A.; Sobrinho, W.S.; Sarmento, W.E.; de Souza, D.T.; Machado, H.C.L.; de Lima, S.M.F.; Fernandes, W.E.S. Efeitos Da Ventilação Mecânica Invasiva Nos Pacientes Com Traumatismo Cranioencefálico Na Unidade De Terapia Intensiva: Uma Revisão Da Literatura. Revista Uniabeu 2018, 11, 352–362. [Google Scholar]
- Mosing, M.; Senior, J.M. Maintenance of equine anaesthesia over the last 50 years: Controlled inhalation of volatile anaesthetics and pulmonary ventilation. Equine Vet. J. 2018, 50, 282–291. [Google Scholar] [CrossRef]
- Hines, R.L.; Jones, S.B. (Eds.) Stoelting’s Anesthesia and Co-Existing Disease E-Book; Elsevier Health Sciences: Amsterdam, The Netherlands, 2021. [Google Scholar]
- Schenck, E.J.; Hoffman, K.; Goyal, P.; Choi, J.; Torres, L.; Rajwani, K.; Tam, C.W.; Ivascu, N.; Martinez, F.J.; Berlin, D.A. Respiratory mechanics and gas exchange in COVID-19–associated respiratory failure. Ann. Am. Thorac. Soc. 2020, 17, 1158–1161. [Google Scholar] [CrossRef]
- Cheung, J.C.H.; Ho, L.T.; Cheng, J.V.; Cham, E.Y.K.; Lam, K.N. Staff safety during emergency airway management for COVID-19 in Hong Kong. Lancet Respir. Med. 2020, 8, e19. [Google Scholar] [CrossRef]
- Fong, S.; Li, E.; Violato, E.; Reid, A.; Gu, Y. Impact of aerosol box on intubation during COVID-19: A simulation study of normal and difficult airways. Can. J. Anesth./J. Can. D’anesthésie 2021, 68, 496–504. [Google Scholar] [CrossRef]
- MacLeod, S.; Tkatch, R.; Kraemer, S.; Fellows, A.; McGinn, M.; Schaeffer, J.; Yeh, C. COVID-19 Era social isolation among older adults. Geriatrics 2021, 6, 52. [Google Scholar] [CrossRef] [PubMed]
- Rackley, C.R. Monitoring during mechanical ventilation. Respir. Care 2020, 65, 832–846. [Google Scholar] [CrossRef]
- Kremeier, P.; Böhm, S.H.; Tusman, G. Clinical use of volumetric capnography in mechanically ventilated patients. J. Clin. Monit. Comput. 2020, 34, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Montrief, T.; Ramzy, M.; Long, B.; Gottlieb, M.; Hercz, D. COVID-19 Respiratory Support in the Emergency Department Setting. Am. J. Emerg. Med. 2020, 38, 2160–2168. [Google Scholar] [CrossRef] [PubMed]
- Mansour, M.; Elmekawy, F.A.; Diab, H.S. Role of capnography in detecting hypercapnic events during weaning from mechanical ventilation. Egypt. J. Chest Dis. Tuberc. 2021, 70, 81. [Google Scholar]
- Brill, S.E.; Wedzicha, J.A. Oxygen therapy in acute exacerbations of chronic obstructive pulmonary disease. Int. J. Chronic Obstr. Pulm. Dis. 2014, 9, 1241. [Google Scholar]
- Akhila, V.; Vasavi, Y.; Nissie, K.; Rao, P.V. An IoT based patient monitoring system using arduino uno. Int. Res. J. Eng. Technol. 2020, 7, 3170–3174. [Google Scholar]
- Paktil, R. IoT Based Patient Monitoring System Using Arduino. Int. Res. J. Eng. Technol. 2020, 7, 6469–6471. [Google Scholar]
- Singla, S. AI and IoT in Healthcare. In Internet of Things Use Cases for the Healthcare Industry; Raj, P., Chatterjee, J., Kumar, A., Balamurugan, B., Eds.; Springer: Cham, Switzerland, 2020. [Google Scholar] [CrossRef]
- Hariharan, U.; Rajkumar, K.; Akilan, T.; Jeyavel, J. Smart Wearable Devices for Remote Patient Monitoring in Healthcare 4.0. In Internet of Medical Things; Springer: Cham, Switzerland, 2021; pp. 117–135. [Google Scholar]
- Saha, H.N.; Roy, R.; Chakraborty, S. Cloud-Assisted IoT System for Epidemic Disease Detection and Spread Monitoring. Smart Healthc. Syst. Des. Secur. Priv. Asp. 2022, 87–114. [Google Scholar] [CrossRef]
- Dharani, J.M.; Divya, C.; Fathima, R.F.F.; Mizriya, A.R. Iot based advanced universal patient health (uph) observation system using raspberry pi 3b. Int. J. Eng. Tech. Res. 2018, 8, 264843. [Google Scholar]
- Abdul-Jabbar, H.M.; Abed, J.K. Real Time Pacemaker Patient Monitoring System Based on Internet of Things. In IOP Conference Series: Materials Science and Engineering; IOP Publishing: Bristol, UK, 2020; p. 012093. [Google Scholar]
- Anan, S.R.; Hossain, M.; Milky, M.; Khan, M.M.; Masud, M.; Aljahdali, S. Research and development of an iot-based remote asthma patient monitoring system. J. Healthc. Eng. 2021, 2021, 2192913. [Google Scholar] [CrossRef]
- Wang, X.; Yang, C.; Mao, S. Resilient Respiration Rate Monitoring with Realtime Bimodal CSI Data. IEEE Sens. J. 2020, 20, 10187–10198. [Google Scholar] [CrossRef]
- Singh, O.P.; El-Badawy, I.M.; Malarvili, M.B. Design and validation of a handheld capnography device for cardiopulmonary assessment based on the Arduino platform. J. Innov. Opt. Health Sci. 2021, 14, 2150015. [Google Scholar] [CrossRef]
- Javaid, M.; Haleem, A.; Rab, S.; Singh, R.P.; Suman, R. Sensors for daily life: A review. Sens. Int. 2021, 2, 100121. [Google Scholar] [CrossRef]
- CYang, C.; Wang, X.; Mao, S. Unsupervised Detection of Apnea Using Commodity RFID Tags With a Recurrent Variational Autoencoder. IEEE Access 2019, 7, 67526–67538. [Google Scholar] [CrossRef]
- Yang, C.; Wang, X.; Mao, S. AutoTag: Recurrent Variational Autoencoder for Unsupervised Apnea Detection with RFID Tags. In Proceedings of the 2018 IEEE Global Communications Conference (GLOBECOM), Abu Dhabi, United Arab, 9–13 December 2018; pp. 1–7. [Google Scholar] [CrossRef]
- Silva, J.P.; Da Silva, R.F.; De Souza, M.H.S. Protótipo De Plataforma Embarcada Para Medição De Sinais Vitais Utilizando Iot. 2019. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwio-Zjrsbf9AhXJ3GEKHZgMB_YQFnoECA8QAQ&url=https%3A%2F%2Fwww.editorarealize.com.br%2Feditora%2Fanais%2Fconedu%2F2019%2FTRABALHO_EV127_MD1_SA20_ID13796_26092019192528.pdf&usg=AOvVaw1_O-IZPUrg3MyB1rCub5g0 (accessed on 2 February 2023).
- Ahmed, Z.U.; Mortuza, M.G.; Uddin, M.J.; Kabir, H.; Mahiuddin; Hoque, J. Internet of Things based patient health monitoring system using wearable biomedical device. In Proceedings of the 2018 international conference on innovation in engineering and technology (ICIET), Dhaka, Bangladesh, 27–28 December 2018; pp. 1–5. [Google Scholar]
- Dusarlapudi, K.; Raju, K.N.; Narayanam, V.S.K. COVID-19 patient breath monitoring and assessment with MEMS accelerometer-based DAQ-a Machine Learning Approach. Nveo-Nat. Volatiles Essent. Oils J.|NVEO 2021, 1567–1575. [Google Scholar]
- AJara, A.J.; Zamora-Izquierdo, M.A.; Skarmeta, A.F. Interconnection Framework for mHealth and Remote Monitoring Based on the Internet of Things. IEEE J. Sel. Areas Commun. 2013, 31, 47–65. [Google Scholar] [CrossRef]
- Valera, A.J.J.; Zamora, M.A.; Skarmeta, A.F.G. An Architecture Based on Internet of Things to Support Mobility and Security in Medical Environment. In Proceedings of the 2010 7th IEEE Consumer Communications and Networking Conference, Las Vegas, NV, USA, 9–12 January 2010; pp. 1–5. [Google Scholar] [CrossRef]
- Prajapati, B.; Parikh, S.; Patel, J. An Intelligent Real Time IoT Based System (IRTBS) for Monitoring ICU Patient. In Information and Communication Technology for Intelligent Systems (ICTIS 2017)—Volume 2. ICTIS 2017; Smart Innovation, Systems and Technologies; Satapathy, S., Joshi, A., Eds.; Springer: Cham, Switzerland, 2018; Volume 84. [Google Scholar] [CrossRef]
- Naranjo-Hernández, D.; Talaminos-Barroso, A.; Reina-Tosina, J.; Roa, L.M.; Barbarov-Rostan, G.; Cejudo-Ramos, P.; Márquez-Martín, E.; Ortega-Ruiz, F. Smart vest for respiratory rate monitoring of COPD patients based on non-contact capacitive sensing. Sensors 2018, 18, 2144. [Google Scholar] [CrossRef]
- Van Loon, K.; Breteler, M.J.M.; Van Wolfwinkel, L.; Rheineck Leyssius, A.T.; Kossen, S.; Kalkman, C.J.; Van Zaane, B.; Peelen, L.M. Wireless non-invasive continuous respiratory monitoring with FMCW radar: A clinical validation study. J. Clin. Monit. Comput. 2016, 30, 797–805. [Google Scholar] [CrossRef]
- Bae, T.W.; Kwon, K.K.; Kim, K.H. Vital block and vital sign server for ECG and vital sign monitoring in a portable u-vital system. Sensors 2020, 20, 1089. [Google Scholar] [CrossRef]
- Chowdhury, M.; Hopper, R.; Ali, S.; Gardner, J.; Udrea, F. MEMS infrared emitter and detector for capnography applications. Procedia Eng. 2016, 168, 1204–1207. [Google Scholar] [CrossRef]
- 181. Priya, G.; Lawanya Shri, M.; GangaDevi, E.; Chatterjee, J.M. IoT Use Cases and Applications. In Internet of Things Use Cases for the Healthcare Industry; Springer: Cham, Switzerland, 2020; pp. 205–220. [Google Scholar]
- George, U.Z.; Moon, K.S.; Lee, S.Q. Extraction and Analysis of Respiratory Motion Using a Comprehensive Wearable Health Monitoring System. Sensors 2021, 21, 1393. [Google Scholar] [CrossRef]
- Zaveri, K.A.; Amin, M.H.; Amin, M.S.; Patel, M.R. IoT based real time low cost home quarantine patient aid system using blynk app. J. Phys. Conf. Ser. 2021, 2007, 012014. [Google Scholar] [CrossRef]
- Ketu, S.; Mishra, P.K. Internet of Healthcare Things: A contemporary survey. J. Netw. Comput. Appl. 2021, 192, 103179. [Google Scholar] [CrossRef]
- Vijayalakshmi, A.; Jose, D.V. Internet of Things for Ambient-Assisted Living—An Overview. In Internet of Things Use Cases for the Healthcare Industry; Springer: Cham, Switzerland, 2020; pp. 221–239. [Google Scholar]
- Al-Halhouli, A.A.; Albagdady, A.; Alawadi, J.F.; Abeeleh, M.A. Monitoring Symptoms of Infectious Diseases: Perspectives for Printed Wearable Sensors. Micromachines 2021, 12, 620. [Google Scholar] [CrossRef] [PubMed]
- Brickman Raredon, M.S.; Fisher, C.; Heerdt, P.; Deshpande, R.; Nivison, S.; Fajardo, E.; Akhtar, S.; Raredon, T.; Niklason, L. Pressure-Regulated Ventilator Splitting (PReVentS)–A COVID-19 Response Paradigm from Yale University. MedRxiv 2020. [Google Scholar] [CrossRef]
- Ali, S.M.; Mahmood, M.S.; Mahmood, N.S. Design of a Low-Cost Ventilator to Support Breathing for Patients with Respiratory Failure Arising from COVID-19. In IOP Conference Series: Materials Science and Engineering; IOP Publishing: Bristol, UK, 2021; p. 012143. [Google Scholar]
- Li, W.; Chai, Y.; Khan, F.; Jan, S.R.U.; Verma, S.; Menon, V.G.; Li, X. A comprehensive survey on machine learning-based big data analytics for IoT-enabled smart healthcare system. Mob. Netw. Appl. 2021, 26, 234–252. [Google Scholar] [CrossRef]
- Stojanovic, R.; Skraba, A. Simplified open HW/SW pulse oximetry interface for purpose of COVID-19 symptoms detection and monitoring. In Proceedings of the 2021 10th Mediterranean Conference on Embedded Computing (MECO), Budva, Montenegro, 7–10 June 2021; pp. 1–5. [Google Scholar]
- Stephens, T.N.; Joerin, A.; Rauws, M.; Werk, L.N. Feasibility of pediatric obesity and prediabetes treatment support through Tess, the AI behavioral coaching chatbot. Transl. Behav. Med. 2019, 9, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Massaroni, C.; Di Tocco, J.; Bravi, M.; Carnevale, A.; Presti, D.L.; Sabbadini, R.; Miccinilli, S.; Sterzi, S.; Formica, D.; Schena, E. Respiratory monitoring during physical activities with a multi-sensor smart garment and related algorithms. IEEE Sens. J. 2019, 20, 2173–2180. [Google Scholar] [CrossRef]

| Surveys | Abdulmalek et al. [55] | Kashyap et al. [57] | Chang et al. [61] | Rodrigues, Postolache and Cercas [54] | Elhoseny et al. [56] | He and Lee [60] | Junaid et al. [58] | Stavropoulos et al. [59] | This Survey | |
|---|---|---|---|---|---|---|---|---|---|---|
| Relevant Points | ||||||||||
| Year | 2022 | 2022 | 2020 | 2020 | 2021 | 2021 | 2022 | 2020 | 2023 | |
| Designer (Portable) | ✓ | ✓ | ✓ | |||||||
| Easy to use | ✓ | |||||||||
| Safe and comfortable (patient) | ✓ | |||||||||
| Real-time | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Remote Access | ✓ | ✓ | ✓ | |||||||
| Autonomous | ✓ | ✓ | ✓ | |||||||
| Data Security | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Continuous monitoring | ✓ | ✓ | ✓ | ✓ | ||||||
| Robustness | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Reliability | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Energy efficiency | ✓ | ✓ | ||||||||
| Cost and economy | ✓ | ✓ | ||||||||
| Accuracy | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Complexity | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| Scalability | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| Authors with Reference | Title | Contributions | Limitations | Performance | Feasibility |
|---|---|---|---|---|---|
| Dharani et al. (2018) [163] | IoT Based Advanced Universal Patient Health (UPH) Observation System Using Raspberry Pi 3B | The researchers talked about wearable and smart technologies based on the Internet of Things (IoT) standard and integrated cloud solutions. The contribution of the authors adds to the issues related to innovative technologies (Arduino and RaspBerry Pi 3 platforms), modern and flexible sensors, scalable techniques, and the development of the prototype health monitoring system UPHM. | Needs to focus on security and data privacy | Robust, portable, flexible, remote access, real-time, continuous monitoring. | Low-cost, economical, effective, and efficient |
| Ahmed, Zia Uddin et al. (2018) [172] | Internet of Things Based Patient Health Monitoring System Using Wearable Biomedical Device | The researchers proposed an automated, intelligent, digital IoT-based architecture to provide doctors with remote patient health status monitoring support. The relevance of this study consists of an affordable and practical system. | Sensor instability and patient data security | Portable Real-time, continuous remote monitoring | Low energy consumption and cost, economical, effective, and efficient |
| Dusarlapudi et al. (2021) [173] | COVID-19 patient breath monitoring and assessment with MEMS accelerometer-based DAQ—a Machine Learning Approach | The authors’ discussion covers the concepts and methods of wearable and smart technologies, the accelerometer device, wireless modules, radio frequency identification (RFID) tools, Arduino, and approaches to the IoT and telemedicine resources. | Updating the system change in the epidemiological profile | Robust Real-time Remote access Continuous monitoring | Efficient and effective solution. |
| Jara, Zamora-Izquierdo and Skarmeta (2013) [174] | Interconnection Framework for mHealth and Remote Monitoring Based on the Internet of Things | The researchers discussed the complex issues related to the personalized health framework with patient data, which can be dynamic and incomplete. Therefore, there are difficulties with mining, analysis, and bias. They contributed an interconnection framework approach to mobile health (mHealth) based on the Internet of Things. They applied the concepts and methods of innovative technologies to develop a continuous monitoring system for vital signs, with remote access, wearable, and with an efficient, safe and scalable sensor. | Needs to focus on security and data privacy | Robust, Flexible Portable, Continuous monitoring, remote access, and real-time. | Low energy consumption and cost, economical, effective, and efficient |
| Prajapati, Parikh and Patel (2018) [176] | Smart Vest for Respiratory Rate Monitoring of COPD Patients Based on Non-Contact Capacitive Sensing | The researchers investigated concepts and applications of capacitive sensing technologies and an e-Health platform based on the Internet of Medical Things (IoMT) to be used in the development of a respiratory rate monitoring system for patients with pulmonary disease (COPD) during the period between respiratory rehabilitation and home exercises with the following functions: non-contact, portable, intelligent, wearable, low-cost and comfortable. | Lack of qualified professionals | Robust Continuous monitoring Real-time, proactive and quick treatment. | Low-cost, economical, effective, and efficient |
| NARANJO-HERNÁNDEZ et al. (2018) [177] | Smart Vest for Respiratory Rate Monitoring of COPD Patients Based on Non-Contact Capacitive Sensing | The researchers investigated concepts and applications of capacitive sensing technologies and an e-Health platform based on the Internet of Medical Things (IoMT) to be used in the development of a respiratory rate monitoring system for patients with Pulmonary Disease (COPD) during the period between respiratory rehabilitation and home exercises with the following functions: non-contact, portable, intelligent, wearable, low cost and comfortable. | Lacks security, interoperability and scalability | Robust Real-time, portable, non-contact, comfortable monitoring. | Low-cost, effective and efficient |
| Loon et al. (2016) [178] | Wireless non-invasive continuous respiratory monitoring with FMCW radar: a clinical validation study | The authors studied the application of “frequency-modulated continuous wave radar” technology to verify its safety in measuring respiratory rate and to present wearable, non-contact, non-invasive monitoring solutions for use by postoperative patients. They developed a reference monitor (pneumotachograph at the time of ventilation and capnography during spontaneous breathing). | Algorithm unavailability and radar inaccuracy FMCW | Robust Portable, non-contact, remote access, real-time, continuous monitoring | Low-cost, economical, effective, and efficient |
| Bae, Kwon, and Kim (2020) [179] | Vital Block and Vital Sign Server for ECG and Vital Sign Monitoring in a Portable u-Vital System | The researchers discussed wearable and smart technologies, addressing the potential of the Internet of Things techniques applied to healthcare. They proposed the ubiquitous Vital (u-Vital) handheld device composed of a system called the vital nlock (VB) with the function of collecting a patient’s electrocardiogram (ECG), blood oxygen saturation (SpO2), non-invasive blood pressure (NiBP), and body temperature (BT) in real time. | Needs to focus on security and privacy of patient data | Robust Portable, real-time processing, data generation and storage. | Effective and efficient solution |
| Chowdhury et al. (2019) [180] | MEMS Infrared Emitter and Detector for Capnography Applications | The approach discussed by the authors shows the importance of a portable, low-cost, more widely used capnography monitoring system, accessible to developing countries, that uses the technologies of a new generation of surface mounted devices (SMD) and micro-electro-mechanical systems (MEMS). | Sensor update | Robust Real-time, portable, non-contact, comfortable monitoring | Low power consumption and cost, effective and efficient. |
| Priya, G. et al. (2020) [181] | IoT Use Cases and Applications | The researchers analyzed concepts and applications of the Internet of Things related to health, health systems, Arduino microcontrollers and machine learning to apply and develop an intelligent prototype. They also disputed numerous case studies on the smart health system. Finally, they presented a wearable and intelligent monitoring system, based on the IoT, which has a great impact on the lives of patients with paralysis and Alzheimer’s. | Sensors with limited capacity | Portable, lightweight, continuous monitoring, real-time, remote access. | Effective and efficient solution |
| George, Moon and Lee (2021) [182] | Extraction and Analysis of Respiratory Motion Using a Comprehensive Wearable Health Monitoring System | The researchers discussed a novel technique for monitoring respiratory functions, such as respiratory rate and tidal volume, with the goal of showing an innovative multisensor approach with application of a new wearable sensor technology with the connection of acoustics and biopotentials and implementation of a lightweight and extensive wearable vital-sign monitoring system. | Need for further research, analysis, and methods. | Robust High level, multisensor, real-time processing. | Effective and efficient solution |
| Zaveri et al. (2021) [183] | IoT based real time low cost home quarantine patient aid system using Blynk app | The researchers discussed IoT, NodeMCU, air quality, oxygen separation level (SpO2), LCD display, heart rate, body temperature sensing, cloud computing, and the Blynk app and proposed a “Home Quarantine Monitoring System” to monitor COVID-19 patients through an application based on IoT-cloud and Blynk. This system uses sensors that collect essential data and sends them to a central server that stores them to be applied whenever there is a need. | Sensor upgrade | Robust Portable, real-time and continuous monitoring High performance (processing, memory and sensors) | Viable model in a crisis scenario, economical, reliable and highly functional |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morais, D.F.T.; Fernandes, G., Jr.; Lima, G.D.; Rodrigues, J.J.P.C. IoT-Based Wearable and Smart Health Device Solutions for Capnography: Analysis and Perspectives. Electronics 2023, 12, 1169. https://doi.org/10.3390/electronics12051169
Morais DFT, Fernandes G Jr., Lima GD, Rodrigues JJPC. IoT-Based Wearable and Smart Health Device Solutions for Capnography: Analysis and Perspectives. Electronics. 2023; 12(5):1169. https://doi.org/10.3390/electronics12051169
Chicago/Turabian StyleMorais, Davisson F. T., Gilberto Fernandes, Jr., Gildário D. Lima, and Joel J. P. C. Rodrigues. 2023. "IoT-Based Wearable and Smart Health Device Solutions for Capnography: Analysis and Perspectives" Electronics 12, no. 5: 1169. https://doi.org/10.3390/electronics12051169
APA StyleMorais, D. F. T., Fernandes, G., Jr., Lima, G. D., & Rodrigues, J. J. P. C. (2023). IoT-Based Wearable and Smart Health Device Solutions for Capnography: Analysis and Perspectives. Electronics, 12(5), 1169. https://doi.org/10.3390/electronics12051169







