Tissue Ablation Using Irreversible Electrolytic Electroporation with Reduced Voltage
Abstract
1. Introduction
2. Materials and Methods
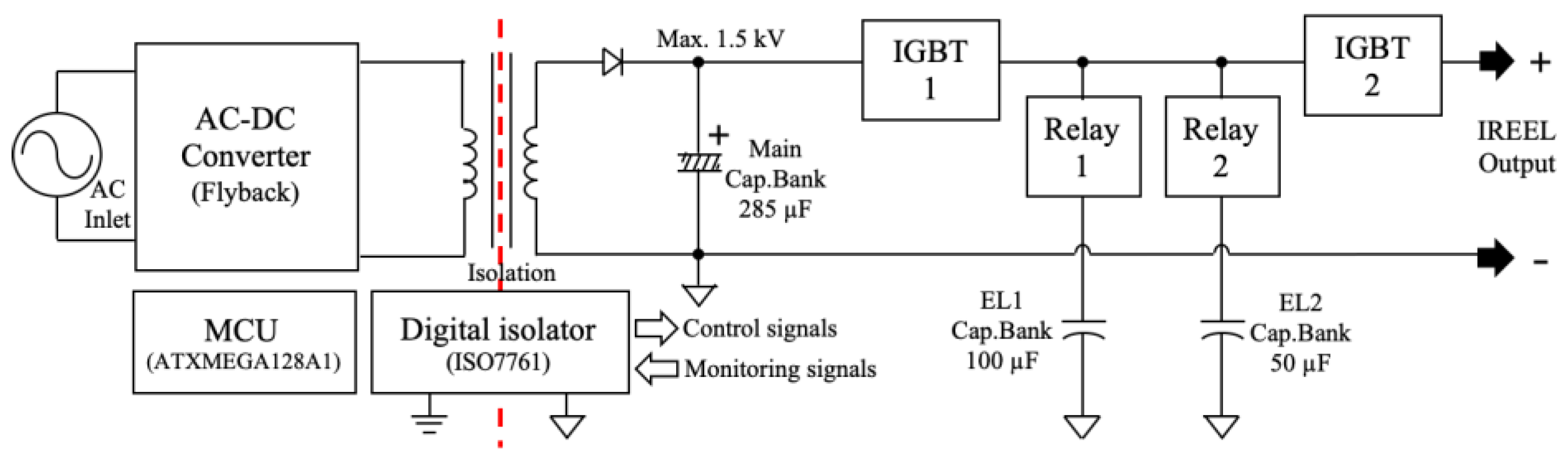
2.1. Development of the IREEL
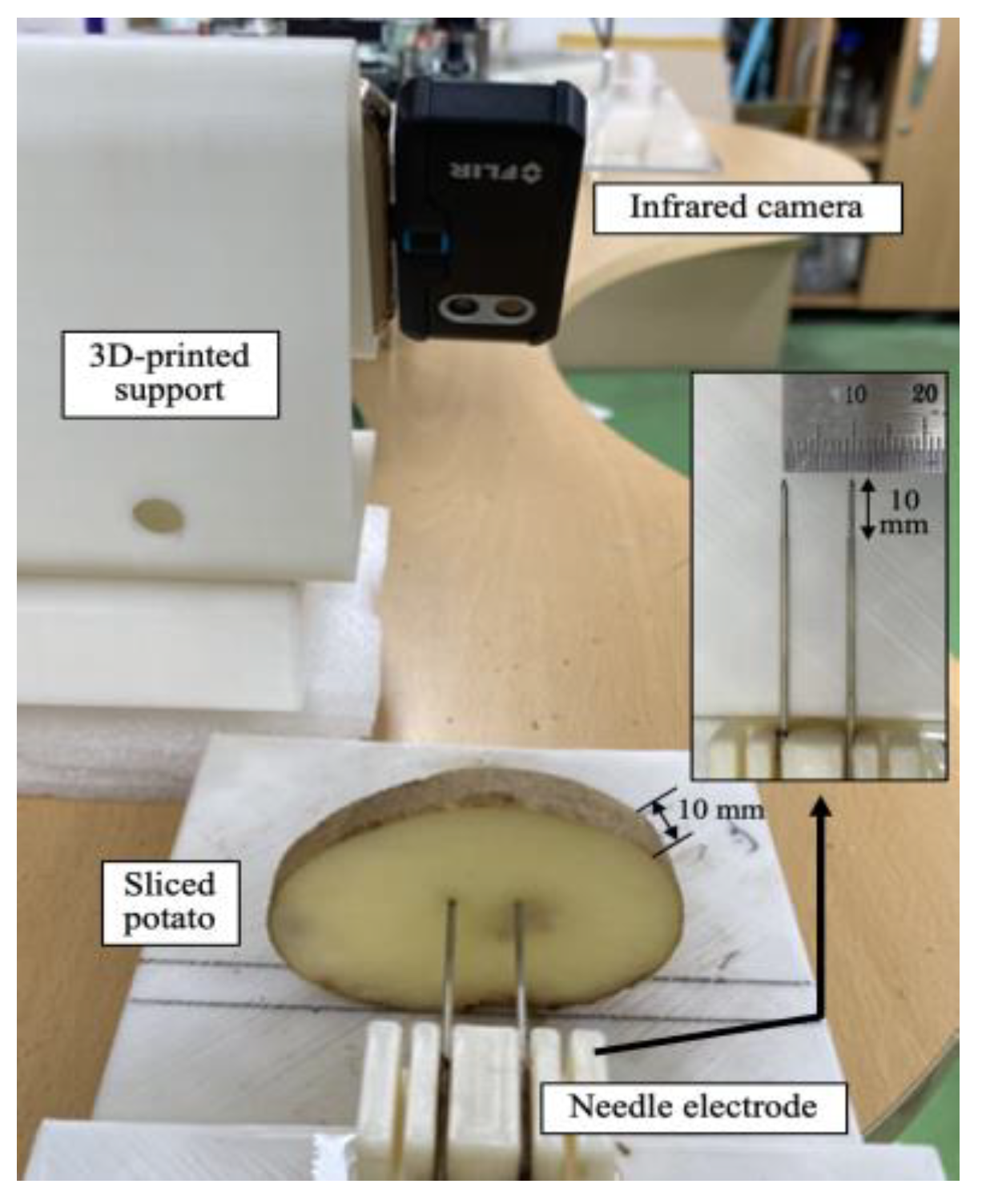
2.2. TTC Test on a Potato as a Tissue Phantom
2.3. Quantification of the Biological Changes
2.4. Statistical Analysis
3. Results
3.1. Output Waveforms of the IREEL
3.2. Changes in the Ablation Areas with PTT
3.3. Changes in pH with the PTT
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Lanka, P.; Francis, K.J.; Kruit, H.; Farina, A.; Cubeddu, R.; Sekar, S.K.V.; Manohar, S.; Pifferi, A. Optical signatures of radiofrequency ablation in biological tissues. Sci. Rep. 2021, 11, 6579. [Google Scholar] [CrossRef] [PubMed]
- Yao, R.; Hu, J.; Zhao, W.; Cheng, Y.; Feng, C. A review of high-intensity focused ultrasound as a novel and non-invasive interventional radiology technique. J. Interv. Med. 2022, 5, 127–132. [Google Scholar] [CrossRef] [PubMed]
- Bastos, D.C.A.; Fuentes, D.T.; Traylor, J.; Weinberg, J.; Kumar, V.A.; Stafford, J.; Li, J.; Rao, G.; Prabhu, S.S. The use of laser interstitial thermal therapy in the treatment of brain metastases: A literature review. Int. J. Hyperth. 2022, 37, 53–60. [Google Scholar] [CrossRef]
- Kwak, K.; Yu, B.; Lewandowski, R.J.; Kim, D.H. Recent progress in cryoablation cancer therapy and nanoparticles mediated cryoablation. Theranostics 2022, 12, 2175–2204. [Google Scholar] [CrossRef]
- Liang, L.; Cool, D.; Kakani, N.; Wang, G.; Ding, H.; Fenster, A. Automatic radiofrequency ablation planning for liver tumors with multiple constraints based on set covering. IEEE Trans. Med. Imaging 2020, 39, 1459–1471. [Google Scholar] [CrossRef]
- Pezzilli, R.; Ricci, C.; Serra, S.; Casadei, R.; Monari, F.; D’Ambra, M.; Corinaldesi, R.; Minni, F. The problems of radiofrequency ablation as an approach for advanced unresectable ductal pancreatic carcinoma. Cancers 2010, 2, 1419–1431. [Google Scholar] [CrossRef]
- Hu, K.; Lian, Y.; Wang, J.; Li, W.; Yao, Z.; Liu, B.; Ren, J. Continuous, large-volume hydrodissection to protect delicate structures around the thyroid throughout the radiofrequency ablation procedure. J. Int. Med. Res. 2020, 48, 300060520937526. [Google Scholar]
- Brock, R.M.; Beitel-White, N.; Davalos, R.V.; Allen, I.C. Starting a fire without flame: The induction of cell death and inflammation in electroporation-based tumor ablation strategies. Front. Oncol. 2020, 10, 1235. [Google Scholar] [CrossRef] [PubMed]
- Batista Napotnik, T.B.; Polajžer, T.; Miklavčič, D. Cell death due to electroporation—A review. Bioelectrochemistry 2021, 141, 107871. [Google Scholar] [CrossRef]
- Thomson, K.R.; Kavnoudias, H.; Neal, R.E. Introduction to irreversible electroporation—Principles and techniques. Tech. Vasc. Interv. Radiol. 2015, 18, 128–134. [Google Scholar] [CrossRef]
- Liu, L.; Zhang, J.; Teng, T.; Yang, Y.; Zhang, W.; Wu, W.; Li, G.; Zheng, X. Electroporation of SUMO-His-Cre protein triggers a specific recombinase-mediated cassette exchange in HEK 293T cells. Protein Expr. Purif. 2022, 198, 106128. [Google Scholar] [CrossRef] [PubMed]
- Potočnik, T.; Miklavčič, D.; Lebar, A.M. Gene transfer by electroporation with high frequency bipolar pulses in vitro. Bioelectrochemistry 2021, 140, 107803. [Google Scholar] [CrossRef]
- Yarmush, M.L.; Golberg, A.; Serša, G.; Kotnik, T.; Miklavčič, D. Electroporation-based technologies for medicine: Principles; applications; and challenges. Annu. Rev. Biomed. Eng. 2014, 16, 295–320. [Google Scholar] [CrossRef] [PubMed]
- Rubinsky, B. Irreversible Electroporation in Medicine. Technol. Cancer Res. Treat. 2007, 6, 255–260. [Google Scholar] [CrossRef] [PubMed]
- Guo, F.; Qian, K.; Zhang, L.; Liu, X.; Peng, H. Multiphysics modelling of electroporation under uni-or bipolar nanosecond pulse sequences. Bioelectrochemistry 2021, 141, 107878. [Google Scholar] [CrossRef]
- Marino, M.; Luján, E.; Mocskos, E.; Marshall, G. OpenEP: An open-source simulator for electroporation-based tumor treatments. Sci. Rep. 2021, 11, 1423. [Google Scholar] [CrossRef]
- Sano, M.B.; Fesmire, C.C.; DeWitt, M.R.; Xing, L. Burst and continuous high frequency irreversible electroporation protocols evaluated in a 3D tumor model. Phys. Med. Biol. 2018, 63, 135022. [Google Scholar] [CrossRef]
- Markelc, B.; Čemažar, M.; Serša, G. Effects of Reversible and Irreversible Electroporation on Endothelial Cells and Tissue Blood Flow. In Handbook of Electroporation, 1st ed.; Miklavcic, D., Ed.; Springer: New York, NY, USA, 2017; pp. 607–620. [Google Scholar]
- Sano, M.B.; Fan, R.E.; Cheng, K.; Saenz, Y.; Sonn, G.A.; Hwang, G.L.; Xing, L. Reduction of muscle contractions during irreversible electroporation therapy using high-frequency bursts of alternating polarity pulses: A laboratory investigation in an ex vivo swine model. J. Vasc. Interv. Radiol. 2018, 29, 893–898. [Google Scholar] [CrossRef]
- Cvetkoska, A.; Maček-Lebar, A.; Trdina, P.; Miklavčič, D.; Reberšek, M. Muscle contractions and pain sensation accompanying high-frequency electroporation pulses. Sci. Rep. 2022, 12, 8019. [Google Scholar] [CrossRef]
- Aras, K.K.; Efimov, I.R. Irreversible electroporation: Proceed with caution. Heart Rhythm. 2018, 15, 1880–1881. [Google Scholar] [CrossRef]
- Fusco, R.; Di Bernardo, E.D.; D’Alessio, V.; Salati, S.; Cadossi, M. Reduction of muscle contraction and pain in electroporation-based treatments: An overview. World J. Clin. Oncol. 2021, 12, 367–381. [Google Scholar] [CrossRef] [PubMed]
- Kalra, N.; Gupta, P.; Gorsi, U.; Bhujade, H.; Chaluvashetty, S.B.; Duseja, A. Irreversible electroporation for unresectable hepatocellular carcinoma: Initial experience. Cardiovasc. Interv. Radiol. 2019, 42, 584–590. [Google Scholar] [CrossRef]
- Siddiqui, I.A.; Kirks, R.C.; Latouche, E.L.; DeWitt, M.R.; Swet, J.H.; Baker, E.H.; Vrochides, D.; Iannitti, D.A.; Davalos, R.V.; McKillop, I.H. High-frequency irreversible electroporation: Safety and efficacy of next-generation irreversible electroporation adjacent to critical hepatic structures. Surg. Innov. 2017, 24, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Wardhana, G.; Raman, N.M.; Abayazid, M.; Fütterer, J.J. Investigating the effect of electrode orientation on irreversible electroporation with experiment and simulation. Int. J. Comput. Assist. Radiol. Surg. 2022, 17, 1399–1407. [Google Scholar] [CrossRef] [PubMed]
- van den Bos, W.; de Bruin, D.M.; Jurhill, R.R.; Savci-Heijink, C.D.; Muller, B.G.; Varkarakis, I.M.; Skolarikos, A.; Zondervan, P.J.; Laguna-Pes, M.P.; Wijkstra, H.; et al. The correlation between the electrode configuration and histopathology of irreversible electroporation ablations in prostate cancer patients. World J. Urol. 2016, 34, 657–664. [Google Scholar] [CrossRef] [PubMed]
- Vižintin, A.; Vidmar, J.; Ščančar, J.; Miklavčič, D. Effect of interphase and interpulse delay in high-frequency irreversible electroporation pulses on cell survival; membrane permeabilization and electrode material release. Bioelectrochemistry 2020, 134, 107523. [Google Scholar] [CrossRef]
- Arena, C.B.; Sano, M.B.; Rossmeisl, J.H.; Caldwell, J.L.; Garcia, P.A.; Rylander, M.N.; Davalos, R.V. High-frequency irreversible electroporation (H-FIRE) for non-thermal ablation without muscle contraction. Biomed. Eng. OnLine 2011, 10, 102. [Google Scholar] [CrossRef] [PubMed]
- Yao, C.; Lv, Y.; Zhao, Y.; Dong, S.; Liu, H.; Ma, J. Synergistic combinations of short high-voltage pulses and long low-voltage pulses enhance irreversible electroporation efficacy. Sci. Rep. 2017, 7, 15123. [Google Scholar] [CrossRef]
- Lv, Y.; Yao, C.; Rubinsky, B. A 2-D cell layer study on synergistic combinations of high-voltage and low-voltage irreversible electroporation pulses. IEEE Trans. Biomed. Eng. 2020, 67, 957–965. [Google Scholar] [CrossRef]
- Fesmire, C.C.; Petrella, R.A.; Kaufman, J.D.; Topasna, N.; Sano, M.B. Irreversible electroporation is a thermally mediated ablation modality for pulses on the order of one microsecond. Bioelectrochemistry 2020, 135, 107544. [Google Scholar] [CrossRef]
- Fesmire, C.C.; Petrella, R.A.; Fogle, C.A.; Gerber, D.A.; Xing, L.; Sano, M.B. Temperature dependence of high frequency irreversible electroporation evaluated in a 3D tumor model. Ann. Biomed. Eng. 2020, 48, 2233–2246. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; Chan, S.S.Y.; Aksic, N.; Bajalovic, N.; Loke, D.K. Ultralong-time recovery and low-voltage electroporation for biological cell monitoring enabled by a microsized multipulse framework. ACS Omega 2021, 6, 35325–35333. [Google Scholar] [CrossRef] [PubMed]
- Kurata, K.; Yoshimatsu, S.; Takamatsu, H. Low-voltage irreversible electroporation using a comb-shaped contact electrode. IEEE Trans. Biomed. Eng. 2020, 67, 420–427. [Google Scholar] [CrossRef] [PubMed]
- Fang, Z.; Mao, H.; Moser, M.A.J.; Zhang, W.; Qian, Z.; Zhang, B. Irreversible electroporation enhanced by radiofrequency ablation: An in vitro and computational study in a 3D liver tumor model. Ann. Biomed. Eng. 2021, 48, 2126–2138. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Yang, Y.; Ding, L.; Moser, M.A.J.; Zhang, E.M.; Zhang, W. Tumor ablation enhancement by combining radiofrequency ablation and irreversible electroporation: An In Vitro 3D Tumor Study. Ann. Biomed. Eng. 2019, 47, 694–705. [Google Scholar] [CrossRef]
- Klein, N.; Guenther, E.; Mikus, P.; Stehling, M.K.; Rubinsky, B. Single exponential decay waveform; a synergistic combination of electroporation and electrolysis (E2) for tissue ablation. PeerJ 2017, 5, e3190. [Google Scholar] [CrossRef]
- Phillips, M.; Krishnan, H.; Raju, N.; Rubinsky, B. Tissue ablation by a synergistic combination of electroporation and electrolysis delivered by a single pulse. Ann. Biomed. Eng. 2016, 44, 3144–3154. [Google Scholar] [CrossRef]
- Perkons, N.R.; Stein, E.J.; Nwaezeapu, C.; Wildenberg, J.C.; Saleh, K.; Itkin-Ofer, R.; Ackerman, D.; Soulen, M.C.; Hunt, S.J.; Nadolski, G.J.; et al. Electrolytic ablation enables cancer cell targeting through pH modulation. Nat. Commun. 2018, 1, 48. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.; Kim, H.; Park, J.; Kim, K.W.; Sim, S.B.; Chung, J.H. Evaluation of electroporated area using 2, 3, 5-triphenyltetrazolium chloride in a potato model. Sci. Rep. 2021, 11, 20431. [Google Scholar] [CrossRef]
- Hjouj, M.; Rubinsky, B. Magnetic resonance imaging characteristics of nonthermal irreversible electroporation in vegetable tissue. J. Membr. Biol. 2010, 236, 137–146. [Google Scholar] [CrossRef]
- Kang, H.K.; Kim, K.H.; Ahn, J.S.; Kim, H.B.; Yi, J.H.; Kim, H.S. A simple segmentation and quantification method for numerical quantitative analysis of cells and tissues. Technol. Health Care 2020, 28, 401–410. [Google Scholar] [CrossRef]
- Dunki-Jacobs, E.M.; Philip, P.; Martin, R.C.G. Evaluation of thermal injury to liver; pancreas and kidney during irreversible electroporation in an in vivo experimental model. Br. J. Surg. 2014, 101, 1113–1121. [Google Scholar] [CrossRef] [PubMed]
- Novickij, V.; Rembiałkowsk, N.; Szlas, W.; Kulbacka, J. Does the shape of the electric pulse matter in electroporation? Front. Oncol. 2022, 12, 958128. [Google Scholar] [CrossRef] [PubMed]
- Lv, Y.; Yao, C.; Rubinsky, B. A conceivable mechanism responsible for the synergy of high and low voltage irreversible electroporation pulses. Ann. Biomed. Eng. 2019, 47, 1552–1563. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Liu, H.; Bhonsle, S.P.; Wang, Y.; Davalos, R.V.; Yao, C. Ablation outcome of irreversible electroporation on potato monitored by impedance spectrum under multi-electrode system. Biomed. Eng. OnLine 2018, 17, 126. [Google Scholar] [CrossRef]
- López-Alonso, B.; Sarnago, H.; Lucía, O.; Briz, P.; Burdío, J.M. Real-time impedance monitoring during electroporation processes in vegetal tissue using a high-performance generator. Sensors 2020, 20, 3158. [Google Scholar] [CrossRef]





| Voltage (V) | IRE Only | IREEL (PN + PTT) | EL Only | |||
|---|---|---|---|---|---|---|
| PN: 8 | 8 + 400 μs | 8 + 800 μs | 8 + 1600 μs | 8 + 3200 μs | 3200 μs | |
| 500 | 8% (13.41 ± 0.11) | 36% (59.47 ± 5.80) | 59% (96.27 ± 8.98) | 90% (146.71 ± 14.04) | 91% (148.28 ± 20.08) | - |
| 1000 | 14% (22.84 ± 3.34) | 54% (89.19 ± 8.37) | 110% (180.24 ± 21.07) | 144% (235.05 ± 27.49) | 186% (303.12 ± 43.84) | - |
| 1500 | 100% (162.43 ± 27.62) | 104% (169.14 ± 31.74) | 146% (237.45 ± 30.11) | 159% (258.83 ± 36.66) | 209% (339.84 ± 45.91) | 115% (186.64 ± 34.01) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, K.-H.; An, J.; Park, Y.-J.; Park, J.-H.; Kim, H.B.; Yi, J.-H.; Kim, H.-S. Tissue Ablation Using Irreversible Electrolytic Electroporation with Reduced Voltage. Electronics 2023, 12, 2916. https://doi.org/10.3390/electronics12132916
Kim K-H, An J, Park Y-J, Park J-H, Kim HB, Yi J-H, Kim H-S. Tissue Ablation Using Irreversible Electrolytic Electroporation with Reduced Voltage. Electronics. 2023; 12(13):2916. https://doi.org/10.3390/electronics12132916
Chicago/Turabian StyleKim, Ki-Han, Jinsu An, Young-Jin Park, Jung-Hoon Park, Hong Bae Kim, Jeong-Han Yi, and Hyung-Sik Kim. 2023. "Tissue Ablation Using Irreversible Electrolytic Electroporation with Reduced Voltage" Electronics 12, no. 13: 2916. https://doi.org/10.3390/electronics12132916
APA StyleKim, K.-H., An, J., Park, Y.-J., Park, J.-H., Kim, H. B., Yi, J.-H., & Kim, H.-S. (2023). Tissue Ablation Using Irreversible Electrolytic Electroporation with Reduced Voltage. Electronics, 12(13), 2916. https://doi.org/10.3390/electronics12132916










