2. Case Report
The patient received all the necessary information, and informed consent was obtained before any procedures were conducted.
A 39-year-old female Caucasian patient with a weight of 41 kg and a height of 158 cm with juvenile DM who had been on corticosteroid treatment for 28 years first presented to our practice in July 2023, dissatisfied with her undereye bags. Several plastic surgery services rejected her case due to the complexity of her preexisting conditions. Her past medical history included DM, long-term glucocorticoid treatment, type 2 diabetes with insulin therapy, high blood pressure, hypercholesterolemia, and chronic blepharoconjunctivitis. Her DM was managed with oral methylprednisolone, usually 8 mg per day, that she had been taking for the vast majority of her life. The dose was increased to 12 mg per day on two separate occasions more than ten years ago (at that time) for a few days due to disease flare-ups. Also, 2.5 years before her presentation, a trial of Azathioprine was initiated, but it was interrupted after a few months due to poor tolerance. An attempt was made to reduce the dose of methylprednisolone by half one month before the surgery, but after 4 days, the patient manifested joint and muscle pain with reduced mobility. The usual dose of methylprednisolone was reintroduced and maintained throughout the surgical treatments.
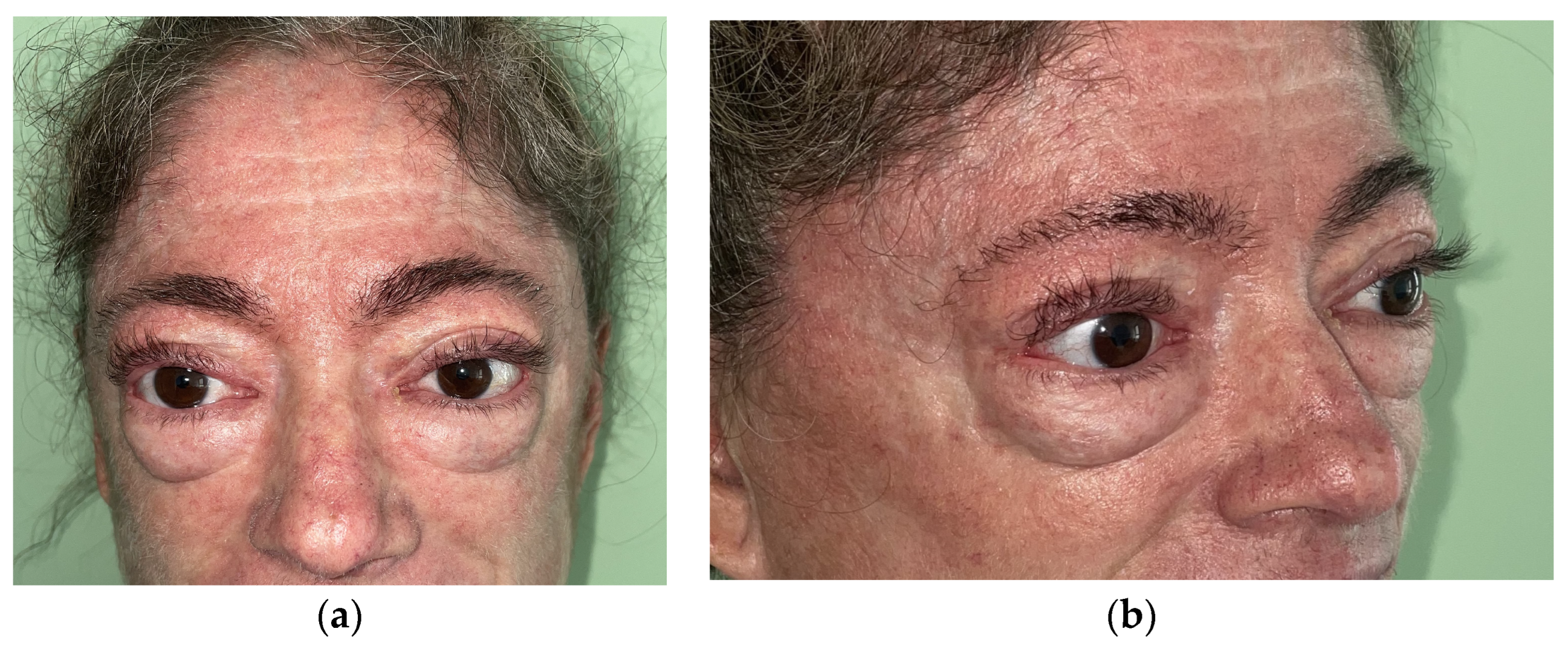
A clinical examination revealed the facial manifestation of her condition, including a facial maculo-papular erythematous rash, marked xerosis, indurated skin, and scalp involvement with erythematous plaques but also exophthalmia, facial asymmetry, and lagophthalmos (
Figure 1). She also presented with poikiloderma of the neck and upper chest.
Given her significant medical history, the patient was subjected to preoperative assessments by rheumatologists, cardiologists, ophthalmologists, and anesthesiologist. Imaging studies including MRI and local soft tissue ultrasound examinations were also conducted to differentiate lymphedema from herniated fat pads. The assessors concluded that the herniated fat pads were responsible for her appearance.
The surgical procedure was performed under general anesthesia. A lower blepharoplasty was carried out through an infraciliary skin incision, with preservation of 1 cm of the orbicularis muscle. Then, the dissection was continued under the muscle, with skin–muscle flap elevation down to the orbital margin. The orbitomalar ligament was divided, and the preperiosteal dissection was continued for about 1 cm. The septum was incised at the arcus marginalis, and the orbital fat pads were exposed (
Figure 2). A part of the herniated fat from the central, medial, and lateral fat pads was removed, followed by repositioning the excess from the central and medial fat pads over the infraorbital rim to blend the junction between the cheek and eyelid. The exposure was difficult due to the loss of skin elasticity, requiring meticulous dissection to access the retro septal fat pads. Additionally, the lateral orbital SMAS flap was advanced cranially and fixed to the lateral orbital margin in order to achieve midfacial elevation and lid support. No tarsoligamentous laxity was encountered. No skin was removed, except for the lateral dog ear correction, requiring an approximately 1 mm wide skin excision at the lateral side of the incision.
The only immediate postoperative problem was persistent and accentuated chemosis at her right eye. The next day following surgery, the patient was discharged and prescribed antibiotic treatment (Augmentin
® (GlaxoSmithKline, Dublin, Ireland) (1 g) twice a day for 7 days), topical dexamethasone and Tobramycin Ophthalmic Solution (Dexatobrom
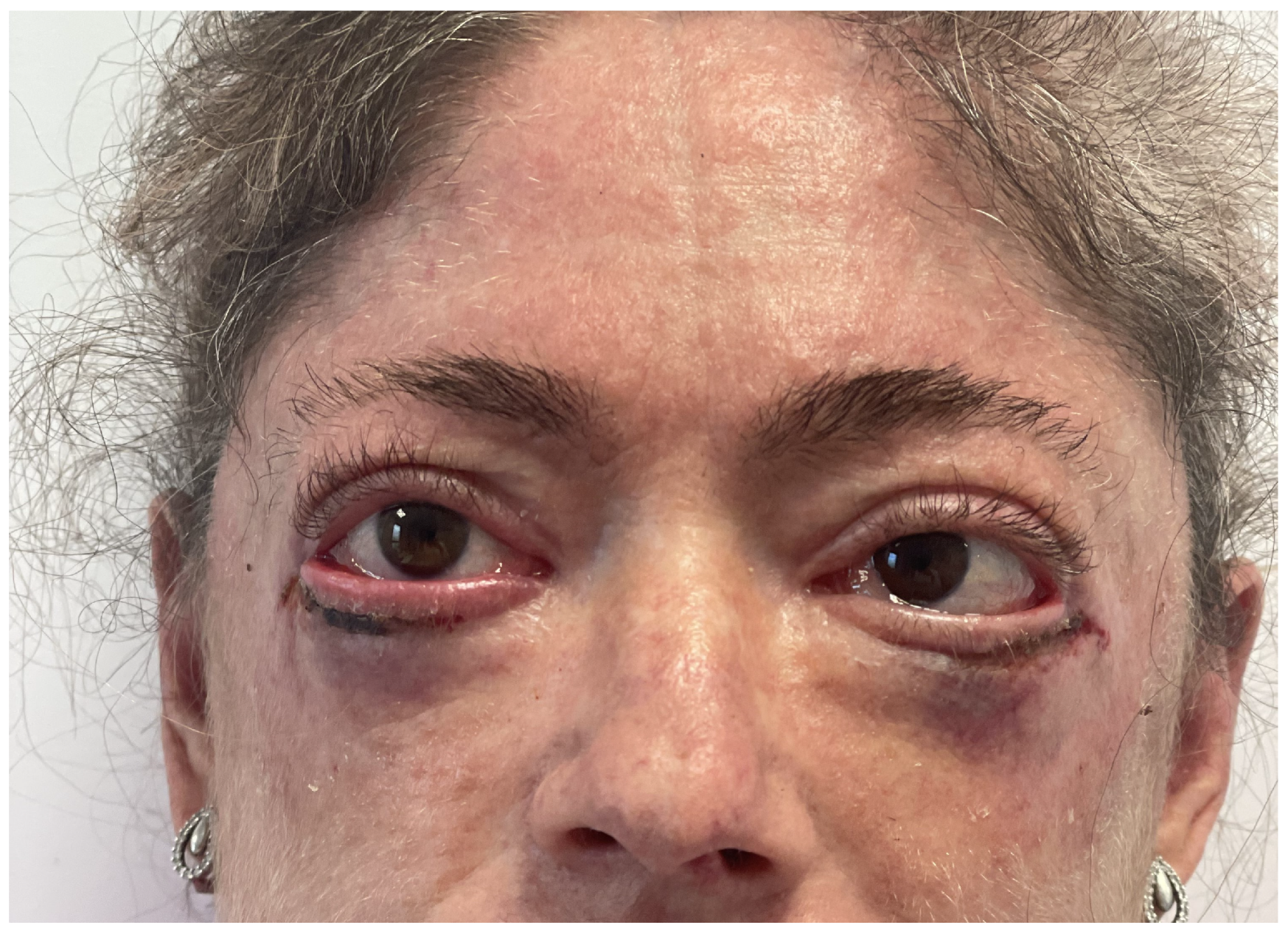
®, (Rompharm, Otopeni, Romania) administration 3 times a day for 7 days, dexpantenol ophthalmic gel administration at night for 7 days, and the application of preservative-free artificial tears for 1 month. No additional pain killers were needed, and the patient continued her chronic treatment including cortisone, as mentioned. At the 1-week follow-up appointment, the stiches were removed; marginal skin necrosis was noted on both sides, with more on the right side (
Figure 3). The wound healed after 12 days of treatment with topical Fucidic acid cream (Fucidin
®, LEO Laboratories Ltd., Dublin, Ireland). No revision surgery was required.
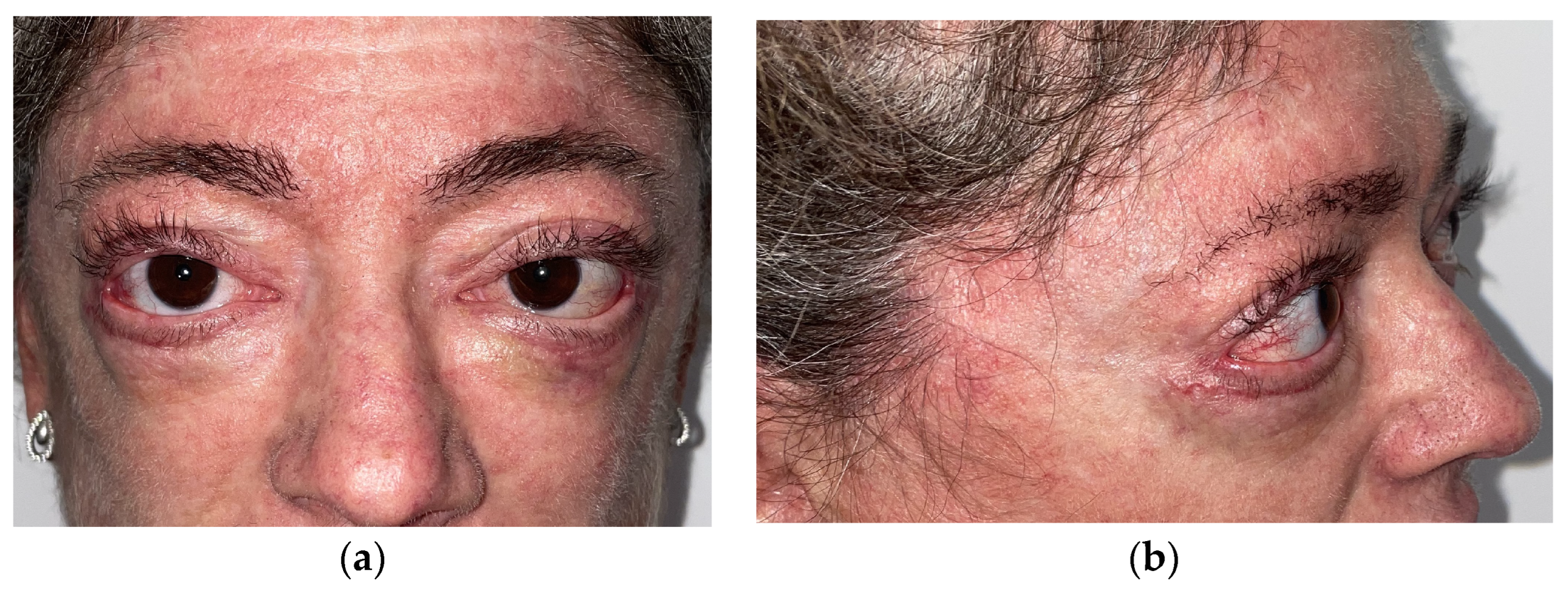
At her 1-month postoperative visit, the wounds were healed, and the conjunctival chemosis settled down. She continued scar management with silicone gel (Stratamed
®, Stratpharma AG, Basel, Switzerland) (
Figure 4).
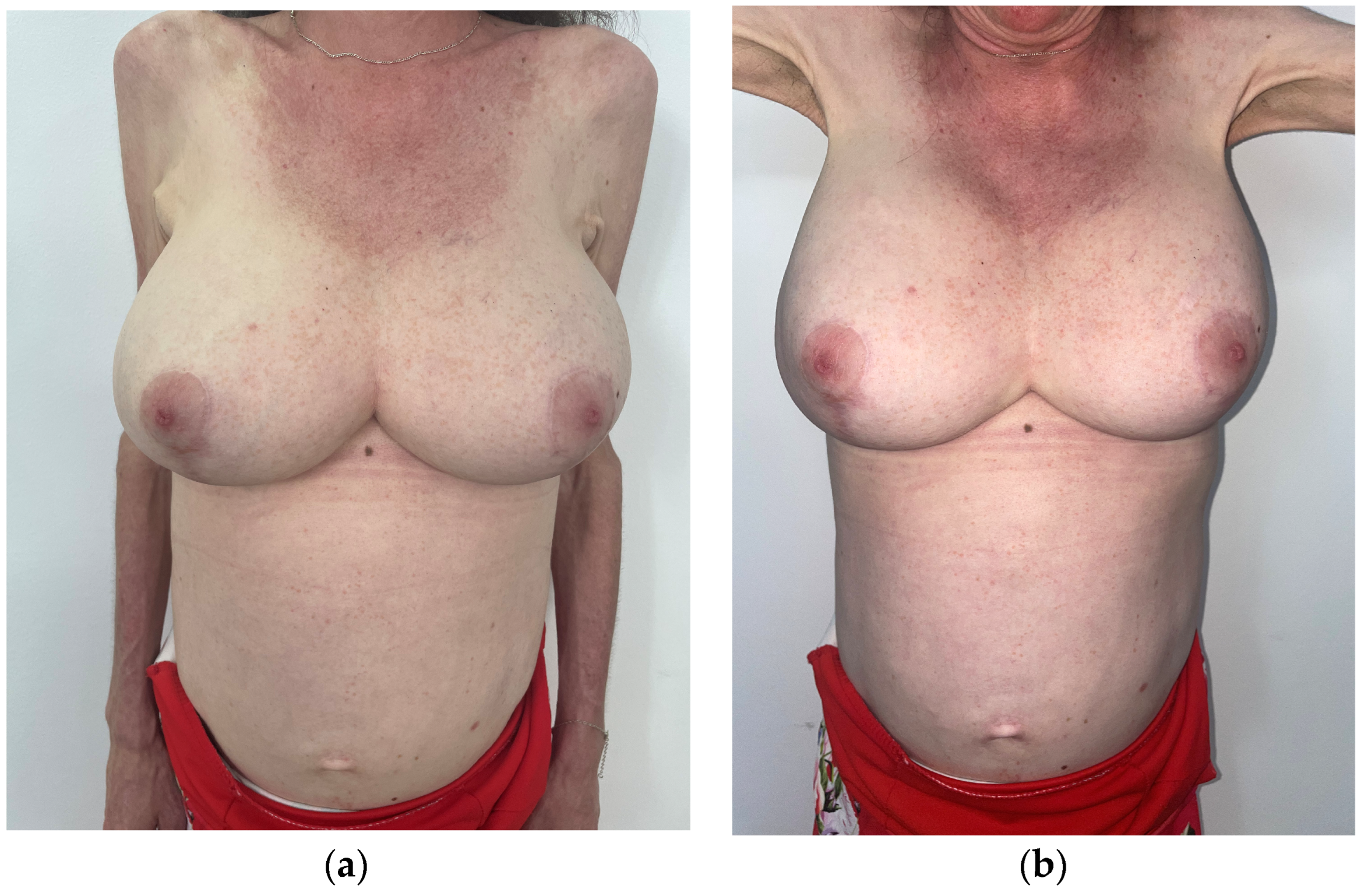
At the same appointment, the patient expressed her desire for breast reduction surgery due to discomfort and physical strain caused by her large breasts
Figure 5.
Given the patient’s history of juvenile DM, we postponed the breast reduction surgery for 3 months to ensure optimal management of her condition. During this period, the patient underwent ultrasound and mammography examinations of her breasts to assess their composition and identify any abnormalities, revealing BI-RADS 2 with calcifications in both breasts.
The patient experienced symptoms of macromastia, including back and neck pain and shoulder grooves. Clinical examination revealed ptotic, hypertrophic breasts and significant symmastia. Her breasts were tender, heavy, and hard, with significant calcification tissue, areolar hypertrophy, and asymmetry. The decision to delay the breast reduction surgery was made to prioritize the patient’s overall health and minimize potential risks associated with her underlying condition. The presence of tender, heavy, and calcified breast tissue raised concerns about the surgical approach and postoperative outcome.
We were dealing with a 158 cm high patient weighing 41 kg. The sternal-notch-to-nipple (SNN) distance was measured on both sides: 26 cm on the right side and 28 cm on the left side. The nipple-to-inframammary fold was 14 cm on the right side and 13 cm on the left side.
Three months after her lower blepharoplasty, we performed a wise-pattern breast reduction under general anesthesia on a supero-medial pedicle. The size of the areolas was reduced to 38 mm. The pedicle was maintained at a width of 10 cm, allowing for relatively easy rotation and repositioning of the nipple–areola complex to 19 cm from the sternal notch. A total of 700 g of breast tissue was excised on each side. The tissue samples were sent for histopathological examination: no malignant tissue was present. Due to calcinosis, it was not possible to perform lateral breast liposuction as initially planned. The adipose tissue was notably resistant, making it difficult to pass the cannula through it, leading to the cancellation of this part of the procedure. Aspiration drains were used on each side and removed before discharge. Despite the previously mentioned difficulties, the surgery resulted in a favorable outcome, with the nipple–areola complex displaying a healthy pink color at the end of the surgery and over the next few days.
The patient was discharged two days after surgery and prescribed antibiotic treatment (Augmentin® (1 g) two times a day for seven days) and her chronic treatment. We also recommended that she wear a medical compression bra for 6 weeks.
The first follow up was at 2 weeks after the surgery, when minimal signs of skin distress were noticed at the junction of the inverted T on her left breast. At her one-month follow-up, she presented with a 2/1.5 cm. area of skin necrosis in this region. This was debrided (
Figure 6), and topical sulfadiazine ointment was used initially; after that, Atrauman Ag
® dressing (Hartmann, Hamburg, Germany) was applied till the patch healed completely 4 months later (
Figure 7). The right breast healed uneventfully. A silicone-gel-based ointment (Stratamed
®, Stratpharma AG, Basel, Switzerland) was applied two times a day for 3 months for scar management.
At 9 months post-lower blepharoplasty, a marked improvement was noted in the appearance of the patient’s lower eyelids. The amelioration of these aesthetic concerns not only improved the patient’s self-confidence but also alleviated any discomfort associated with her condition
Figure 8.
Also, breast reduction surgery provided her with relief from physical discomfort and improved her body image (
Figure 9).
3. Discussion
When considering surgery for a patient with DM, it is crucial to approach it with caution and thoroughly consider the patient’s overall health and treatment history. DM is a rare inflammatory disease that affects muscles and skin, and individuals with this condition may face unique challenges when undergoing surgical procedures.
First, prolonged systemic cortisone treatment, commonly used to manage dermatomyositis, can impact the body’s ability to heal after surgery. Corticosteroids can weaken the immune system, increase the risk of infection, slow wound healing, and affect the overall recovery process. It is important for both the patient and the corresponding medical team to be aware of these potential complications and take the necessary precautions.
Corticosteroids can impair the body’s natural wound-healing processes by suppressing the inflammatory response, reducing collagen deposition, and impairing angiogenesis [
3]. This can lead to delayed wound healing, an increased risk of infection, and poor aesthetic outcomes, particularly in the context of elective aesthetic procedures. Patients with dermatomyositis may also have underlying muscle weakness and atrophy, which can further complicate recovery from surgical procedures. In addition to the effects of corticosteroids, dermatomyositis itself can negatively impact wound healing [
4,
5]. The chronic inflammation and autoimmune dysregulation associated with this condition can disrupt normal wound-healing pathways [
3].
Additionally, when a patient with DM expresses interest in purely aesthetic procedures, such as a lower blepharoplasty or more extensive plastic surgery such as breast reduction, it is essential for the medical team to have open and honest discussions about the potential risks and benefits. These conversations should consider the patient’s specific health status, including any ongoing symptoms related to their DM, as well as their overall physical and emotional wellbeing.
While high-dose, short-term corticosteroid use may not significantly impact wound healing, chronic, long-term steroid therapy has been associated with a 2–5-fold-increased risk of wound complications [
3].
In our case, healing problems were encountered in both surgeries, with minimal complications in the lower blepharoplasty and more significant ones in the breast reduction surgery.
We chose to use an infraciliary skin incision rather than a transconjunctival approach in the lower blepharoplasty due to the high risk of complications of the latter. Our decision was influenced by the potential greater difficulty of managing conjunctival complications, which could also affect vision, compared to skin complications. Additionally, we considered the patient’s history of chronic blepharoconjunctivitis.
Another aspect of the lower blepharoplasty that should be discussed in this case is the longevity of its effects. A patient’s satisfaction at the 9-month follow-up is a positive indicator of a procedure’s effectiveness within this time frame, but stability is hard to predict. Since there are no long-term follow-up images available in the existing medical literature [
6], it is difficult for us to anticipate the patient’s current status due to the progression of her condition and to determine how long these results will persist.
Breast reduction surgery or reduction mammoplasty is considered the gold-standard treatment for symptomatic hypermastia or hypertrophic breasts [
7].
In breast reduction surgery, the choice of pedicle position is crucial for ensuring optimal blood supply to the nipple–areola complex (NAC). There are several options for the pedicle position, including superomedial, inferior, superior, medial, and lateral pedicles. Each option has its own advantages and involves unique considerations, but the superomedial pedicle is often preferred for its ability to provide good blood supply to the NAC and reduce the chances of NAC necrosis [
8,
9,
10], and these are the reasons why we chose to perform a wise-pattern breast reduction on a superior medial pedicle.
However, it is important to note that while the superomedial pedicle offers significant advantages in terms of blood supply, it can also present challenges at the inset. The rotation of the superomedial pedicle can be technically demanding due to its position. This difficulty was encountered in our case too, not only due to the position of the pedicle but also its width (10 cm) and the fact that our DM patient presented fibrous breast tissue with calcinosis.
In breast reduction surgery, the reported complication rate varies. In a large study conducted at multiple centers, where 16,812 cases of breast reduction were included, Simpson et al. found an overall complication rate of 6.2% [
11]. In wise-pattern breast reduction technique, the complication rate at the T-junction ranges between 3 and 34% [
12], and it has been observed that there is a higher risk of complications when more than 800 g of tissue is removed from a single breast [
13]. In one study, chronic steroids users were 2.22 times more likely to develop wound complications and 1.67 times more likely to develop surgical complications than non-users [
14]. In her left breast, our patient developed T-junction necrosis with wound dehiscence, but it healed by itself 4 months later after just one debridement and the application of topical wound dressings. No other complications were encountered.
In conclusion, our case report sheds light on a crucial yet underexplored area within the field of aesthetic surgery by focusing on patients undergoing prolonged and high-dose systemic cortisol therapy, like our DM patient. Our case report has revealed valuable insights into the potential challenges associated with aesthetic surgeries for individuals undergoing prolonged systemic cortisone therapy. Our findings offer valuable perspective to health care professionals involved in the care of these patients by highlighting the implications of cortisone use for surgical outcome complications and postoperative care.
Furthermore, our case report serves as a catalyst for further investigation and discussion regarding the optimization of aesthetic surgical procedures for individuals with a history of prolonged systemic cortisone therapy. The long-term impact of cortisone use on surgical outcomes, patient satisfaction, and safety warrants ongoing attention and research within the medical community.