Evaluation of the Effectiveness of Staphylococcus Phages in a Skincare Serum against Staphylococcus spp.
Abstract
1. Introduction
2. Materials and Methods
2.1. Bacterial Strains Used and Culture Condition
2.2. Isolation and Purification of Staphylococcus Phages
2.3. Host Range Determination
2.4. Transmission Electron Microscopy of Selected Staphylococcus Phage
2.5. Efficiency of Plating of Selected Staphylococcus Phage
2.6. Lytic Ability of Staphylococcus Phage
2.7. Lytic Activity of Selected Staphylococcus Phage in the Presence of Cosmetic Preservative
2.8. Formulation of Skincare Serum Containing Selected Staphylococcus Phage
2.9. Survivability of Staphylococcus Phage in Skincare Serum
2.10. Statistical Analysis
3. Results
3.1. Isolation of Staphylococcus Phages
3.2. Host Range Determination of Staphylococcus Phages
3.3. Transmission Electron Microscopy of Selected Staphylococcus Phage
3.4. Efficiency of Plating of Selected Staphylococcus Phage
3.5. Lytic Ability of Staphylococcus Phage A1
3.6. Survivability of Staphylococcus Phage in the Presence of Cosmetic Preservative
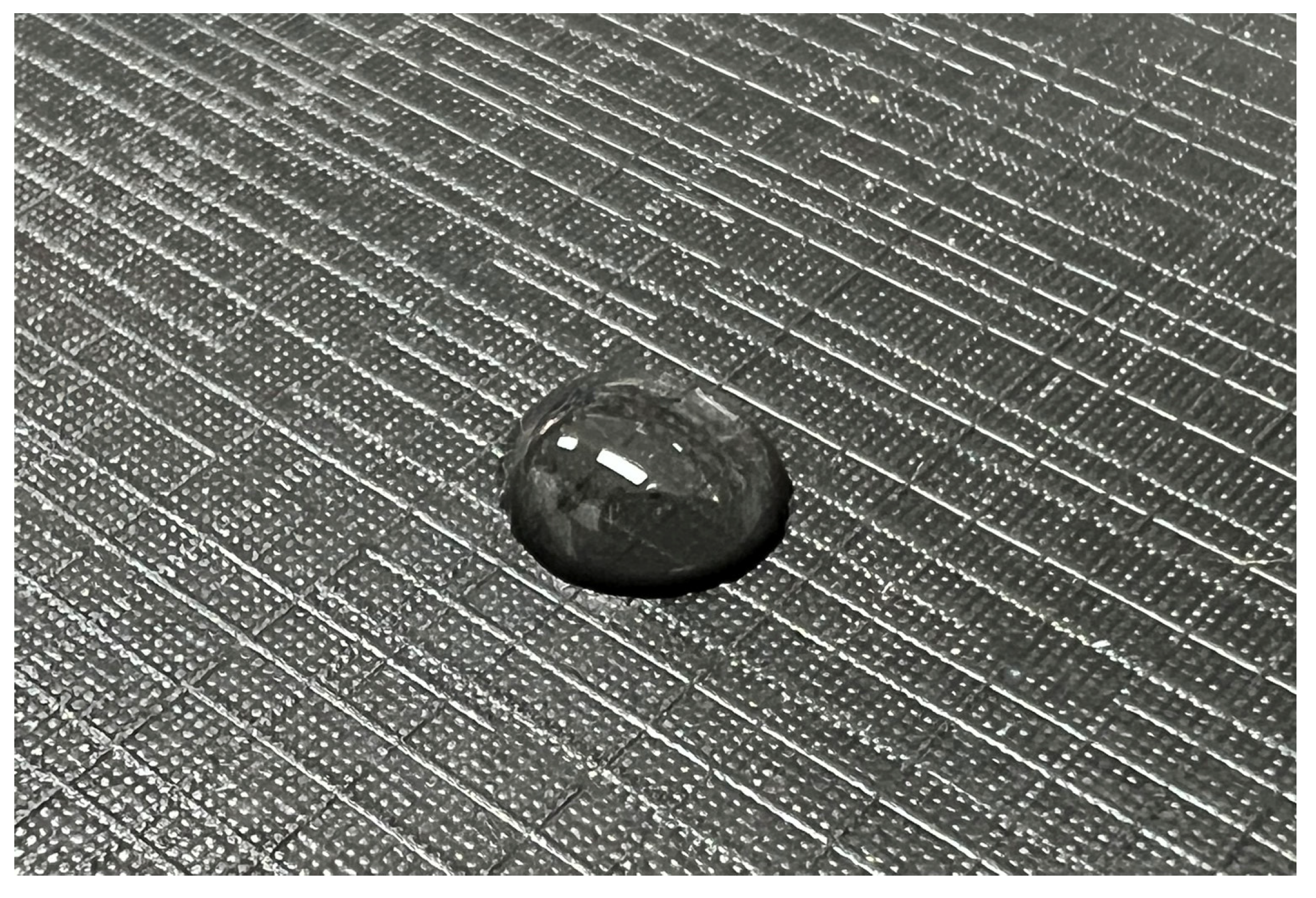
3.7. Formulation of Skincare Serum Containing Staphylococcus Phage
3.8. Survivability of Staphylococcus Phage in Skincare Serum
4. Discussion
4.1. Sources and Lytic Ability of Staphylococcus Phages
4.2. Cosmetic Formulation Containing Potential Phages Targeting Skin Diseases Caused by Staphylococcus spp.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Götz, F.; Bannerman, T.; Schleifer, K.H. The Genera Staphylococcus and Macrococcus. In The Prokaryotes; Dworkin, M., Falkow, S., Rosenberg, E., Schleifer, K.H., Stackebrandt, E., Eds.; Springer: New York, NY, USA, 2006; pp. 5–75. [Google Scholar]
- Del Giudice, P. Skin infections caused by Staphylococcus aureus. Acta Derm. Venereol. 2020, 100, 208–215. [Google Scholar] [CrossRef] [PubMed]
- Miró, E.M.; Sánchez, N.P. Cutaneous manifestations of infectious diseases. In Atlas of Dermatology in Internal Medicine; Sánchez, N., Ed.; Springer: New York, NY, USA, 2012; pp. 77–119. [Google Scholar]
- New Study Reveals How MRSA Infection Can Permanently Harm Immune Function. Available online: https://hms.harvard.edu/news/lasting-effects (accessed on 3 September 2023).
- Linz, M.S.; Mattappallil, A.; Finkel, D.; Parker, D. Clinical impact of Staphylococcus aureus skin and soft tissue infections. Antibiotics 2023, 12, 557. [Google Scholar] [CrossRef] [PubMed]
- Tayel, A.A.; Shaban, S.M.; Moussa, S.H.; Elguindy, N.M.; Diab, A.M.; Mazrou, K.E.; Ghanem, R.A.; El-Sabbagh, S.M. Bioactivity and application of plant seeds’ extracts to fight resistant strains of Staphylococcus aureus. Ann. Agric. Sci. 2018, 63, 47–53. [Google Scholar] [CrossRef]
- Akinduti, P.A.; Emoh-Robinson, V.; Obamoh-Triumphant, H.F.; Obafemi, Y.D.; Banjo, T.T. Antibacterial activities of plant leaf extracts against multi-antibiotic resistant Staphylococcus aureus associated with skin and soft tissue infections. BMC Complement. Med. Ther. 2022, 22, 47. [Google Scholar] [CrossRef]
- Gonelimali, F.D.; Lin, J.; Miao, W.; Xuan, J.; Charles, F.; Chen, M.; Hatab, S.R. Antimicrobial properties and mechanism of action of some plant extracts against food pathogens and spoilage microorganisms. Front. Microbiol. 2018, 9, 1639. [Google Scholar] [CrossRef]
- Xiao, S.; Cui, P.; Shi, W.; Zhang, Y. Identification of essential oils with activity against stationary phase Staphylococcus aureus. BMC Complement. Med. Ther. 2020, 20, 99. [Google Scholar] [CrossRef]
- Bona, E.; Massa, N.; Novello, G.; Pavan, M.; Rocchetti, A.; Berta, G.; Gamalero, E. Essential oil antibacterial activity against methicillin-resistant and-susceptible Staphylococcus aureus strains. Microbiol. Res. 2019, 10, 8331. [Google Scholar] [CrossRef]
- Uzair, B.; Niaz, N.; Bano, A.; Khan, A.B.; Zafar, N.; Iqbal, M.; Tahira, R.; Fasim, F. Essential oils showing in vitro anti MRSA and synergistic activity with penicillin group of antibiotics. Pak. J. Pharm. Sci. 2017, 30, 1997–2002. [Google Scholar]
- Adamczak, A.; Ożarowski, M.; Karpiński, T.M. Antibacterial activity of some flavonoids and organic acids widely distributed in plants. J. Clin. Med. 2019, 9, 109. [Google Scholar] [CrossRef]
- Zhu, C.; Zhao, Y.; Zhao, X.; Liu, S.; Xia, X.; Zhang, S.; Wang, Y.; Zhang, H.; Xu, Y.; Chen, S.; et al. The antimicrobial peptide MPX can kill Staphylococcus aureus, reduce biofilm formation, and effectively treat bacterial skin infections in mice. Front. Vet. Sci. 2022, 9, 819921. [Google Scholar] [CrossRef]
- Shang, L.; Li, J.; Song, C.; Nina, Z.; Li, Q.; Chou, S.; Wang, Z.; Shan, A. Hybrid antimicrobial peptide targeting Staphylococcus aureus and displaying anti-infective activity in a murine model. Front. Microbiol. 2020, 11, 1767. [Google Scholar] [CrossRef] [PubMed]
- Mantle, D.; Gok, M.A.; Lennard, T.W. Adverse and beneficial effects of plant extracts on skin and skin disorders. Advers. Drug React. Toxicol. Rev. 2001, 20, 89–103. [Google Scholar]
- Clokie, M.R.; Millard, A.D.; Letarov, A.V.; Heaphy, S. Phages in nature. Bacteriophage 2011, 1, 31–45. [Google Scholar] [CrossRef] [PubMed]
- Uyttebroek, S.; Chen, B.; Onsea, J.; Ruythooren, F.; Debaveye, Y.; Devolder, D.; Spriet, I.; Depypere, M.; Wagemans, J.; Lavigne, R.; et al. Safety and efficacy of phage therapy in difficult-to-treat infections: A systematic review. Lancet Infect. Dis 2022, 22, E208–E220. [Google Scholar] [CrossRef]
- Ly-Chatain, M.H. The factors affecting effectiveness of treatment in phages therapy. Front. Microbiol. 2014, 5, 51. [Google Scholar] [CrossRef]
- Jault, P.; Leclerc, T.; Jennes, S.; Pirnay, J.P.; Que, Y.A.; Resch, G.; Rousseau, A.F.; Ravat, F.; Carsin, H.; Floch, R.L.; et al. Efficacy and tolerability of a cocktail of bacteriophages to treat burn wounds infected by Pseudomonas aeruginosa (PhagoBurn): A randomised, controlled, double-blind phase 1/2 trial. Lancet Infect. Dis. 2019, 19, 35–45. [Google Scholar] [CrossRef]
- Wang, C.; Nie, T.; Lin, F.; Connerton, I.F.; Lu, Z.; Zhou, S.; Hang, H. Resistance mechanisms adopted by a Salmonella Typhimurium mutant against bacteriophage. Virus Res. 2019, 273, 197759. [Google Scholar] [CrossRef]
- Kolenda, C.; Medina, M.; Bonhomme, M.; Laumay, F.; Roussel-Gaillard, T.; Martins-Simoes, P.; Tristan, A.; Pirot, F.; Ferry, T.; Laurent, F.; et al. Phage Therapy against Staphylococcus aureus: Selection and optimization of production protocols of novel broad-spectrum Silviavirus phages. Pharmaceutics 2022, 14, 1885. [Google Scholar] [CrossRef]
- Jiang, Y.; Xu, Q.; Jiang, L.; Zheng, R. Isolation and characterization of a lytic Staphylococcus aureus phage WV against Staphylococcus aureus biofilm. Intervirology 2021, 64, 169–177. [Google Scholar] [CrossRef]
- Kaźmierczak, N.; Grygorcewicz, B.; Roszak, M.; Bochentyn, B.; Piechowicz, L. Comparative assessment of bacteriophage and antibiotic activity against multidrug-resistant Staphylococcus aureus biofilms. Int. J. Mol. Sci. 2022, 23, 1274. [Google Scholar] [CrossRef]
- Abo-elmaaty, S.; El Dougdoug, N.K.; Hazaa, M.M. Improved antibacterial efficacy of bacteriophage-cosmetic formulation for treatment of Staphylococcus aureus in vitro. Ann. Agric. Sci. 2016, 61, 201–206. [Google Scholar] [CrossRef][Green Version]
- Pelyuntha, W.; Ngasaman, R.; Yingkajorn, M.; Chukiatsiri, K.; Benjakul, S.; Vongkamjan, K. Isolation and characterization of potential Salmonella phages targeting multidrug-resistant and major serovars of Salmonella derived from broiler production chain in Thailand. Front. Microbiol. 2021, 12, 662461. [Google Scholar] [CrossRef] [PubMed]
- Pelyuntha, W.; Sanguankiat, A.; Kovitvadhi, A.; Vongkamjan, K. Broad lytic spectrum of novel Salmonella phages on ciprofloxacin-resistant Salmonella contaminated in the broiler production chain. Vet. World 2022, 15, 2039–2045. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.G.; Jun, J.W.; Giri, S.S.; Yun, S.; Kim, H.J.; Chi, C.; Kim, S.W.; Park, S.C. Complete genome sequence of Staphylococcus aureus bacteriophage pSa-3. Genome Announc. 2017, 5, e00182-17. [Google Scholar] [CrossRef] [PubMed]
- Göller, P.C.; Elsener, T.; Lorgé, D.; Radulovic, N.; Bernardi, V.; Naumann, A.; Amri, N.; Khatchatourova, E.; Coutinho, F.H.; Loessner, M.J.; et al. Multi-species host range of staphylococcal phages isolated from wastewater. Nat. Commun. 2021, 12, 6965. [Google Scholar] [CrossRef] [PubMed]
- Whittard, E.; Redfern, J.; Xia, G.; Millard, A.; Ragupathy, R.; Malic, S.; Enright, M.C. Phenotypic and genotypic characterization of novel polyvalent bacteriophages with potent in vitro activity against an international collection of genetically diverse Staphylococcus aureus. Front. Cell. Infect. Microbiol. 2021, 11, 698909. [Google Scholar] [CrossRef]
- Sofy, A.R.; Abd El Haliem, N.F.; Refaey, E.E.; Hmed, A.A. Polyvalent phage CoNShP-3 as a natural antimicrobial agent showing lytic and antibiofilm activities against antibiotic-resistant coagulase-negative staphylococci strains. Foods 2020, 9, 673. [Google Scholar] [CrossRef]
- Liu, S.; Hon, K.; Bouras, G.S.; Psaltis, A.J.; Shearwin, K.; Wormald, P.J.; Vreugde, S. APTC-C-SA01: A novel bacteriophage cocktail targeting Staphylococcus aureus and MRSA biofilms. Int. J. Mol. Sci. 2022, 23, 6116. [Google Scholar] [CrossRef]
- Shimamori, Y.; Mitsunaka, S.; Yamashita, H.; Suzuki, T.; Kitao, T.; Kubori, T.; Nagai, H.; Takeda, S.; Ando, H. Staphylococcal phage in combination with Staphylococcus epidermidis as a potential treatment for Staphylococcus aureus-associated atopic dermatitis and suppressor of phage-resistant mutants. Viruses 2020, 13, 7. [Google Scholar] [CrossRef]
- Kozajda, A.; Jeżak, K. Occupational exposure to Staphylococcus aureus in the wastewater treatment plants environment. Med. Pr. 2020, 71, 265–278. [Google Scholar] [CrossRef]
- Amirsoleimani, A.; Brion, G.M.; Diene, S.M.; François, P.; Richard, E.M. Prevalence and characterization of Staphylococcus aureus in wastewater treatment plants by whole genomic sequencing. Water Res. 2019, 158, 193–202. [Google Scholar] [CrossRef] [PubMed]
- Hyman, P. Phages for phage therapy: Isolation, characterization, and host range breadth. Pharmaceuticals 2019, 12, 35. [Google Scholar] [CrossRef] [PubMed]
- Aghaee, B.L.; Mirzaei, M.K.; Alikhani, M.Y.; Mojtahedi, A. Sewage and sewage-contaminated environments are the most prominent sources to isolate phages against Pseudomonas aeruginosa. BMC Microbiol. 2021, 21, 132. [Google Scholar] [CrossRef]
- Landemaine, L.; Da Costa, G.; Fissier, E.; Francis, C.; Morand, S.; Verbeke, J.; Michel, M.L.; Briandet, R.; Sokol, H.; Gueniche, A.; et al. Staphylococcus epidermidis isolates from atopic or healthy skin have opposite effect on skin cells: Potential implication of the AHR pathway modulation. Front. Immunol. 2023, 14, 1098160. [Google Scholar]
- Štrancar, V.; Marušić, M.; Tušar, J.; Praček, N.; Kolenc, M.; Šuster, K.; Horvat, S.; Janež, N.; Peterka, M. Isolation and in vitro characterization of novel S. epidermidis phages for therapeutic applications. Front. Cell. Infect. Microbiol. 2023, 13, 607. [Google Scholar] [CrossRef] [PubMed]
- Duc, H.M.; Son, H.M.; Honjoh, K.I.; Miyamoto, T. Isolation and application of bacteriophages to reduce Salmonella contamination in raw chicken meat. LWT 2018, 91, 353–360. [Google Scholar] [CrossRef]
- Pelyuntha, W.; Vongkamjan, K. Combined effects of Salmonella phage cocktail and organic acid for controlling Salmonella Enteritidis in chicken meat. Food Control 2022, 133, 108653. [Google Scholar] [CrossRef]
- Guo, Z.; Lin, H.; Ji, X.; Yan, G.; Lei, L.; Han, W.; Gu, J.; Huang, J. Therapeutic applications of lytic phages in human medicine. Microb. Pathog. 2020, 142, 104048. [Google Scholar] [CrossRef]
- Feng, T.; Leptihn, S.; Dong, K.; Loh, B.; Zhang, Y.; Stefan, M.I.; Li, M.; Guo, X.; Cui, Z. JD419, a Staphylococcus aureus phage with a unique morphology and broad host range. Front. Microbiol. 2021, 12, 602902. [Google Scholar] [CrossRef]
- Gutiérrez, D.; Vandenheuvel, D.; Martínez, B.; Rodríguez, A.; Lavigne, R.; García, P. Two phages, phiIPLA-RODI and phiIPLA-C1C, lyse mono-and dual-species staphylococcal biofilms. Appl. Environ. Microbiol. 2015, 81, 3336–3348. [Google Scholar] [CrossRef]
- Viral Skin Defense: Phage Therapy, a Commentary. Available online: https://www.cosmeticsandtoiletries.com/research/tech-transfer/article/21835917/biocogent-llc-viral-skin-defense-phage-therapy-a-commentary (accessed on 19 June 2023).
- Castillo, D.E.; Nanda, S.; Keri, J.E. Propionibacterium (Cutibacterium) acnes bacteriophage therapy in acne: Current evidence and future perspectives. Dermatol. Ther. 2019, 9, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Farfán, J.; Gonzalez, J.M.; Vives, M. The immunomodulatory potential of phage therapy to treat acne: A review on bacterial lysis and immunomodulation. PeerJ 2022, 10, e13553. [Google Scholar] [CrossRef] [PubMed]
- Jończyk-Matysiak, E.; Weber-Dąbrowska, B.; Żaczek, M.; Międzybrodzki, R.; Letkiewicz, S.; Łusiak-Szelchowska, M.; Górski, A. Prospects of phage application in the treatment of acne caused by Propionibacterium acnes. Front. Microbiol. 2017, 8, 164. [Google Scholar] [CrossRef]
- Barr, J.J.; Youle, M.; Rohwer, F. Innate and acquired bacteriophage-mediated immunity. Bacteriophage 2013, 3, e25857. [Google Scholar] [CrossRef] [PubMed]
- Roach, D.R.; Leung, C.Y.; Henry, M.; Morello, E.; Singh, D.; Di Santo, J.P.; Weitz, J.S.; Debarbieux, L. Synergy between the host immune system and bacteriophage is essential for successful phage therapy against an acute respiratory pathogen. Cell Host Microbe 2017, 22, 38–47. [Google Scholar] [CrossRef]
- Górski, A.; Międzybrodzki, R.; Borysowski, J.; Dąbrowska, K.; Wierzbicki, P.; Ohams, M.; Korczak-Kowalska, G.; Olszowska-Zaremba, N.; Łusiak-Szelachowska, M.; Kłak, M.; et al. Phage as a modulator of immune responses: Practical implications for phage therapy. Adv Virus Res. 2012, 83, 41–71. [Google Scholar]
- Ross, A.; Ward, S.; Hyman, P. More is better: Selecting for broad host range bacteriophages. Front. Microbiol. 2016, 7, 1352. [Google Scholar] [CrossRef]
- Stability Testing of Cosmetics. Available online: https://www.makingcosmetics.com/Stability-Testing-of-Cosmetics_ep_59.html (accessed on 11 November 2023).


| Bacterial Isolate | Code Name | Source of Origin |
|---|---|---|
| S. aureus (n = 5) | ATCC25923 | Laboratory collection |
| SA1 | Human skin (acne) | |
| SA2 | Human skin (acne) | |
| SA3 | Human skin (acne) | |
| SA4 | Human skin (acne) | |
| MRSA (n = 4) | SA3503 | Purulent wound |
| SA5809 | Purulent wound | |
| SA1362 | Purulent wound | |
| SA2031 | Purulent wound | |
| S. capitis (n = 2) | SC1 | Human skin (acne) |
| SC2 | Human skin (acne) | |
| S. epidermidis (n = 2) | PC6 | Human skin (acne) |
| SE-F1 | Human skin (acne) |
| Staphylococcus Phage | Host of Isolation | Source of Origin 1 | Plaque Morphotype |
|---|---|---|---|
| A1 | SC1 | W1 | 1.3 mm |
| A2 | SA3 | S1 | 0.6 mm |
| A3 | ATCC25923 | W2 | 0.6 mm |
| A4 | SA2 | W3 | 0.5 mm |
| A5 | SA5809 | W5 | 0.4 mm |
| A6 | SA5809 | W6 | 0.4 mm |
| A7 | SA1362 | W3 | 0.5 mm |
| A8 | SA2031 | S1 | 0.6 mm |
| A9 | SA1 | W6 | 0.5 mm |
| A10 | SC1 | W6 | 0.4 mm |
| A11 | SA3 | W7 | 0.5 mm |
| A12 | SC2 | W4 | 0.5 mm |
| A13 | SC2 | W5 | 0.4 mm |
| A14 | SA4 | W7 | 0.4 mm |
| A15 | SA4 | W1 | 0.4 mm |
| A16 | SA4 | W8 | 0.4 mm |
| A17 | SA4 | W3 | 0.6 mm |
| Tested Isolates | Staphylococcus Phages 1 | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A1 | A2 | A3 | A4 | A5 | A6 | A7 | A8 | A9 | A10 | A11 | A12 | A13 | A14 | A15 | A16 | A17 | |
| ATCC25923 | + | − | + | − | − | − | − | − | − | − | − | − | − | − | − | − | − |
| SA1 | + | + | − | − | − | − | − | − | + | − | − | − | − | − | − | − | − |
| SA2 | + | − | − | + | − | − | − | − | − | − | − | − | − | − | − | − | − |
| SA3 | + | + | − | − | − | − | − | − | − | − | + | − | − | − | − | − | − |
| SA4 | − | − | − | − | − | − | − | − | − | − | − | − | − | + | + | + | + |
| SA3503 | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − |
| SA5809 | − | − | − | − | + | + | − | − | − | − | − | − | − | − | − | − | − |
| SA1362 | − | − | − | − | − | − | + | − | − | − | − | − | − | − | − | − | − |
| SA2031 | + | − | − | − | − | − | − | + | − | − | − | − | − | − | − | − | − |
| SC1 | + | − | − | − | − | − | − | − | − | + | − | − | − | − | − | − | − |
| SC2 | + | + | − | − | − | − | − | − | − | − | − | + | + | − | − | − | − |
| PC6 | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − |
| SE-F1 | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − |
| %Total lysis | 53.8 | 23.1 | 7.7 | 7.7 | 7.7 | 7.7 | 7.7 | 7.7 | 7.7 | 7.7 | 7.7 | 7.7 | 7.7 | 7.7 | 7.7 | 7.7 | 7.7 |
| Profile Code | B1 | N1 | N2 | N3 | N4 | N4 | N5 | N6 | N7 | N8 | N9 | N10 | N10 | N11 | N11 | N11 | N11 |
| Staphylococcus spp. | EOP Value 1 | Category 2 |
|---|---|---|
| ATCC25923 | 0.81 ± 0.07 | High |
| SA1 | 0.23 ± 0.09 | Medium |
| SA2 | 0.71 ± 0.16 | High |
| SA3 | 0.44 ± 0.05 | Medium |
| SA4 | <0.001 | Inefficient |
| SA3503 | <0.001 | Inefficient |
| SA5809 | <0.001 | Inefficient |
| SA1362 | <0.001 | Inefficient |
| SA2031 | 0.47 ± 0.02 | Medium |
| SC1 | 1.00 * | High |
| SC2 | 1.60 ± 0.21 | High |
| PC6 | <0.001 | Inefficient |
| SE-F1 | <0.001 | Inefficient |
| Strains | Time (h) | Bacterial Count (log CFU/mL) 1 | ||
|---|---|---|---|---|
| Control | MOI 104 | MOI 105 | ||
| S. aureus ATCC25923 | 0 | 4.1 ± 0.7 a | 4.3 ± 0.3 a | 4.2 ± 0.2 a |
| 6 | 6.7 ± 0.8 b | 2.3 ± 0.2 c* | 0.0 ± 0.0 b* | |
| 12 | 7.2 ± 0.7 c | 1.0 ± 0.3 d* | 0.0 ± 0.0 b* | |
| 18 | 8.2 ± 0.4 d | 2.4 ± 0.6 c* | 0.0 ± 0.0 b* | |
| 24 | 8.5 ± 0.3 d | 3.4 ± 0.2 b* | 0.0 ± 0.0 b* | |
| S. capitis SC1 | 0 | 4.3 ± 0.5 a | 4.1 ± 0.3 a | 4.4 ± 0.5 a |
| 6 | 7.3 ± 0.2 b | 0.0 ± 0.0 b* | 0.0 ± 0.0 b* | |
| 12 | 7.9 ± 0.4 bc | 0.0 ± 0.0 b* | 0.0 ± 0.0 b* | |
| 18 | 8.2 ± 0.3 c | 0.0 ± 0.0 b* | 0.0 ± 0.0 b* | |
| 24 | 8.7 ± 0.3 d | 0.0 ± 0.0 b* | 0.0 ± 0.0 b* | |
| S. epidermidis PC6 | 0 | 4.3 ± 0.2 a | 4.2 ± 0.1 a | 4.0 ± 0.5 a |
| 6 | 6.4 ± 0.2 b | 6.1 ± 0.3 b | 6.2 ± 0.2 b | |
| 12 | 7.3 ± 0.4 c | 7.4 ± 0.1 c | 7.0 ± 0.4 c | |
| 18 | 7.9 ± 01 d | 8.0 ± 0.3 c | 7.8 ± 0.3 d | |
| 24 | 8.5 ± 0.3 e | 8.7 ± 0.6 d | 8.2 ± 0.2 d | |
| Solidant DHM Concentration (% v/v) | Phage Titers (log PFU/mL) 1 | % Survivability 1 |
|---|---|---|
| 0.0 (DI control) | 7.0 ± 0.2 | - |
| 0.10 | 7.0 ± 0.1 | 100.0 ± 0.0 |
| 0.125 | 7.0 ± 0.1 | 99.7 ± 0.2 |
| 0.25 | 0.0 ± 0.0 | 0.0 ± 0.0 |
| 0.50 | 0.0 ± 0.0 | 0.0 ± 0.0 |
| 1.00 | 0.0 ± 0.0 | 0.0 ± 0.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pelyuntha, W.; Yingkajorn, M.; Narkpao, T.; Saeaui, S.; Promkuljan, K.; Vongkamjan, K. Evaluation of the Effectiveness of Staphylococcus Phages in a Skincare Serum against Staphylococcus spp. Cosmetics 2023, 10, 156. https://doi.org/10.3390/cosmetics10060156
Pelyuntha W, Yingkajorn M, Narkpao T, Saeaui S, Promkuljan K, Vongkamjan K. Evaluation of the Effectiveness of Staphylococcus Phages in a Skincare Serum against Staphylococcus spp. Cosmetics. 2023; 10(6):156. https://doi.org/10.3390/cosmetics10060156
Chicago/Turabian StylePelyuntha, Wattana, Mingkwan Yingkajorn, Thamonwan Narkpao, Supanida Saeaui, Khemapsorn Promkuljan, and Kitiya Vongkamjan. 2023. "Evaluation of the Effectiveness of Staphylococcus Phages in a Skincare Serum against Staphylococcus spp." Cosmetics 10, no. 6: 156. https://doi.org/10.3390/cosmetics10060156
APA StylePelyuntha, W., Yingkajorn, M., Narkpao, T., Saeaui, S., Promkuljan, K., & Vongkamjan, K. (2023). Evaluation of the Effectiveness of Staphylococcus Phages in a Skincare Serum against Staphylococcus spp. Cosmetics, 10(6), 156. https://doi.org/10.3390/cosmetics10060156







