Comparison of the Modified TyG Indices and Other Parameters to Predict Non-Alcoholic Fatty Liver Disease in Youth
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Anthropometric Measurements
2.3. Laboratory Analyses
2.4. Ultrasonographic Analyses
2.5. Statistical Analyses
3. Results
3.1. Characteristics and Parameters of the Participants According to the NAFLD Grade
3.2. ORs of the Parameters for Predicting NAFLD
3.3. Cut-Off Values and AUC of the Parameters for Predicting NAFLD
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Song, K.; Park, G.; Lee, H.S.; Lee, M.; Lee, H.I.; Ahn, J.; Lee, E.; Choi, H.S.; Suh, J.; Kwon, A. Trends in prediabetes and non-alcoholic fatty liver disease associated with abdominal obesity among korean children and adolescents: Based on the korea national health and nutrition examination survey between 2009 and 2018. Biomedicines 2022, 10, 584. [Google Scholar] [CrossRef] [PubMed]
- Song, K.; Park, G.; Lee, H.S.; Lee, M.; Lee, H.I.; Choi, H.S.; Suh, J.; Kwon, A.; Kim, H.S.; Chae, H.W. Comparison of the triglyceride glucose index and modified triglyceride glucose indices to predict nonalcoholic fatty liver disease in youths. J. Pediatr. 2022, 242, 79–85.e71. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.R.; Kim, H.R.; Kim, M.J.; Ko, J.S.; Seo, J.K. Noninvasive parameters and hepatic fibrosis scores in children with nonalcoholic fatty liver disease. World J. Gastroenterol. 2012, 18, 1525–1530. [Google Scholar] [CrossRef] [PubMed]
- Welsh, J.A.; Karpen, S.; Vos, M.B. Increasing prevalence of nonalcoholic fatty liver disease among united states adolescents, 1988–1994 to 2007–2010. J. Pediatr. 2013, 162, 496–500.e491. [Google Scholar] [CrossRef]
- Vos, M.B.; Abrams, S.H.; Barlow, S.E.; Caprio, S.; Daniels, S.R.; Kohli, R.; Mouzaki, M.; Sathya, P.; Schwimmer, J.B.; Sundaram, S.S.; et al. Naspghan clinical practice guideline for the diagnosis and treatment of nonalcoholic fatty liver disease in children: Recommendations from the expert committee on nafld (econ) and the north american society of pediatric gastroenterology, hepatology and nutrition (naspghan). J. Pediatr. Gastroenterol. Nutr. 2017, 64, 319–334. [Google Scholar] [PubMed]
- Lee, J.H.; Kim, D.; Kim, H.J.; Lee, C.H.; Yang, J.I.; Kim, W.; Kim, Y.J.; Yoon, J.H.; Cho, S.H.; Sung, M.W.; et al. Hepatic steatosis index: A simple screening tool reflecting nonalcoholic fatty liver disease. Dig. Liver Dis. 2010, 42, 503–508. [Google Scholar] [CrossRef] [PubMed]
- Long, M.T.; Gandhi, S.; Loomba, R. Advances in non-invasive biomarkers for the diagnosis and monitoring of non-alcoholic fatty liver disease. Metabolism 2020, 111S, 154259. [Google Scholar] [CrossRef]
- Monelli, F.; Venturelli, F.; Bonilauri, L.; Manicardi, E.; Manicardi, V.; Rossi, P.G.; Massari, M.; Ligabue, G.; Riva, N.; Schianchi, S. Systematic review of existing guidelines for nafld assessment. Hepatoma Res. 2021, 7, 25. [Google Scholar] [CrossRef]
- Wada, T.; Zeniya, M. Background of the fib-4 index in japanese non-alcoholic fatty liver disease. Intern. Med. 2015, 54, 127–132. [Google Scholar] [CrossRef][Green Version]
- Rigamonti, A.E.; Bondesan, A.; Rondinelli, E.; Cella, S.G.; Sartorio, A. The role of aspartate transaminase to platelet ratio index (apri) for the prediction of non-alcoholic fatty liver disease (nafld) in severely obese children and adolescents. Metabolites 2022, 12, 155. [Google Scholar] [CrossRef]
- Ismaiel, A.; Leucuta, D.C.; Popa, S.L.; Fagoonee, S.; Pellicano, R.; Abenavoli, L.; Dumitrascu, D.L. Noninvasive biomarkers in predicting nonalcoholic steatohepatitis and assessing liver fibrosis: Systematic review and meta-analysis. Panminerva Med. 2021, 63, 508–518. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.B.; Kim, M.K.; Kang, S.; Park, K.; Kim, J.H.; Baik, S.J.; Nam, J.S.; Ahn, C.W.; Park, J.S. Triglyceride glucose index is superior to the homeostasis model assessment of insulin resistance for predicting nonalcoholic fatty liver disease in korean adults. Endocrinol. Metab. 2019, 34, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Kitae, A.; Hashimoto, Y.; Hamaguchi, M.; Obora, A.; Kojima, T.; Fukui, M. The triglyceride and glucose index is a predictor of incident nonalcoholic fatty liver disease: A population-based cohort study. Can. J. Gastroenterol. Hepatol. 2019, 2019, 5121574. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Cho, Y.K.; Kim, E.H.; Lee, M.J.; Jung, C.H.; Park, J.Y.; Kim, H.K.; Lee, W.J. Triglyceride glucose-waist circumference is superior to the homeostasis model assessment of insulin resistance in identifying nonalcoholic fatty liver disease in healthy subjects. J. Clin. Med. 2021, 11, 41. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Dai, L.; Zhong, Y.; Xie, G. Usefulness of the triglyceride glucose-body mass index in evaluating nonalcoholic fatty liver disease: Insights from a general population. Lipids Health Dis. 2021, 20, 77. [Google Scholar] [CrossRef]
- Sviklāne, L.; Olmane, E.; Dzērve, Z.; Kupčs, K.; Pīrāgs, V.; Sokolovska, J. Fatty liver index and hepatic steatosis index for prediction of non-alcoholic fatty liver disease in type 1 diabetes. J. Gastroenterol. Hepatol. 2018, 33, 270–276. [Google Scholar] [CrossRef]
- Kim, J.H.; Yun, S.; Hwang, S.S.; Shim, J.O.; Chae, H.W.; Lee, Y.J.; Lee, J.H.; Kim, S.C.; Lim, D.; Yang, S.W.; et al. The 2017 korean national growth charts for children and adolescents: Development, improvement, and prospects. Korean J. Pediatr. 2018, 61, 135–149. [Google Scholar] [CrossRef]
- Moon, J.S.; Lee, S.Y.; Nam, C.M.; Choi, J.-M.; Choe, B.-K.; Seo, J.-W.; Oh, K.; Jang, M.-J.; Hwang, S.-S.; Yoo, M.H. 2007 korean national growth charts: Review of developmental process and an outlook. Clin. Exp. Pediatrics 2008, 51, 1–25. [Google Scholar] [CrossRef]
- Roberts, W.C. The friedewald-levy-fredrickson formula for calculating low-density lipoprotein cholesterol, the basis for lipid-lowering therapy. Am. J. Cardiol. 1988, 62, 345–346. [Google Scholar] [CrossRef]
- Cui, Y.; Blumenthal, R.S.; Flaws, J.A.; Whiteman, M.K.; Langenberg, P.; Bachorik, P.S.; Bush, T.L. Non-high-density lipoprotein cholesterol level as a predictor of cardiovascular disease mortality. Arch. Intern. Med. 2001, 161, 1413–1419. [Google Scholar] [CrossRef]
- Song, K.; Park, G.; Lee, H.S.; Choi, Y.; Oh, J.S.; Choi, H.S.; Suh, J.; Kwon, A.; Kim, H.S.; Chae, H.W. Prediction of insulin resistance by modified triglyceride glucose indices in youth. Life 2021, 11, 286. [Google Scholar] [CrossRef] [PubMed]
- Loaeza-del-Castillo, A.; Paz-Pineda, F.; Oviedo-Cárdenas, E.; Sánchez-Avila, F.; Vargas-Vorácková, F. Ast to platelet ratio index (apri) for the noninvasive evaluation of liver fibrosis. Ann. Hepatol. 2008, 7, 350–357. [Google Scholar] [CrossRef]
- Vallet-Pichard, A.; Mallet, V.; Nalpas, B.; Verkarre, V.; Nalpas, A.; Dhalluin-Venier, V.; Fontaine, H.; Pol, S. Fib-4: An inexpensive and accurate marker of fibrosis in hcv infection. Comparison with liver biopsy and fibrotest. Hepatology 2007, 46, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Saadeh, S.; Younossi, Z.M.; Remer, E.M.; Gramlich, T.; Ong, J.P.; Hurley, M.; Mullen, K.D.; Cooper, J.N.; Sheridan, M.J. The utility of radiological imaging in nonalcoholic fatty liver disease. Gastroenterology 2002, 123, 745–750. [Google Scholar] [CrossRef] [PubMed]
- Molleston, J.P.; Schwimmer, J.B.; Yates, K.P.; Murray, K.F.; Cummings, O.W.; Lavine, J.E.; Brunt, E.M.; Scheimann, A.O.; Unalp-Arida, A. Histological abnormalities in children with nonalcoholic fatty liver disease and normal or mildly elevated alanine aminotransferase levels. J. Pediatr. 2014, 164, 707–713.e703. [Google Scholar] [CrossRef] [PubMed]
- Sugimoto, K.; Moriyasu, F.; Oshiro, H.; Takeuchi, H.; Abe, M.; Yoshimasu, Y.; Kasai, Y.; Sakamaki, K.; Hara, T.; Itoi, T. The role of multiparametric us of the liver for the evaluation of nonalcoholic steatohepatitis. Radiology 2020, 296, 532–540. [Google Scholar] [CrossRef]
- Shannon, A.; Alkhouri, N.; Carter-Kent, C.; Monti, L.; Devito, R.; Lopez, R.; Feldstein, A.E.; Nobili, V. Ultrasonographic quantitative estimation of hepatic steatosis in children with nafld. J. Pediatr. Gastroenterol. Nutr. 2011, 53, 190–195. [Google Scholar] [CrossRef]
- Simental-Mendía, L.E.; Ortega-Pacheco, C.J.; García-Guerrero, E.; Sicsik-Aragón, M.A.; Guerrero-Romero, F.; Martínez-Aguilar, G. The triglycerides and glucose index is strongly associated with hepatic steatosis in children with overweight or obesity. Eur. J. Pediatr. 2021, 180, 1755–1760. [Google Scholar] [CrossRef]
- Kahn, B.B.; Flier, J.S. Obesity and insulin resistance. J. Clin. Investig. 2000, 106, 473–481. [Google Scholar] [CrossRef]
- Tirosh, A.; Shai, I.; Bitzur, R.; Kochba, I.; Tekes-Manova, D.; Israeli, E.; Shochat, T.; Rudich, A. Changes in triglyceride levels over time and risk of type 2 diabetes in young men. Diabetes Care 2008, 31, 2032–2037. [Google Scholar] [CrossRef]
- Zhang, S.; Du, T.; Zhang, J.; Lu, H.; Lin, X.; Xie, J.; Yang, Y.; Yu, X. The triglyceride and glucose index (tyg) is an effective biomarker to identify nonalcoholic fatty liver disease. Lipids Health Dis. 2017, 16, 15. [Google Scholar] [CrossRef] [PubMed]
- Ye, X.; Li, J.; Wang, H.; Wu, J. Pentraxin 3 and the tyg index as two novel markers to diagnose nafld in children. Dis. Markers 2021, 2021, 8833287. [Google Scholar] [CrossRef] [PubMed]
- Styne, D.M.; Arslanian, S.A.; Connor, E.L.; Farooqi, I.S.; Murad, M.H.; Silverstein, J.H.; Yanovski, J.A. Pediatric obesity-assessment, treatment, and prevention: An endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 2017, 102, 709–757. [Google Scholar] [CrossRef] [PubMed]
- Sheng, G.; Lu, S.; Xie, Q.; Peng, N.; Kuang, M.; Zou, Y. The usefulness of obesity and lipid-related indices to predict the presence of non-alcoholic fatty liver disease. Lipids Health Dis. 2021, 20, 134. [Google Scholar] [CrossRef] [PubMed]
- Sartorio, A.; Del Col, A.; Agosti, F.; Mazzilli, G.; Bellentani, S.; Tiribelli, C.; Bedogni, G. Predictors of non-alcoholic fatty liver disease in obese children. Eur. J. Clin. Nutr. 2007, 61, 877–883. [Google Scholar] [CrossRef] [PubMed]
- Vajro, P.; Lenta, S.; Socha, P.; Dhawan, A.; McKiernan, P.; Baumann, U.; Durmaz, O.; Lacaille, F.; McLin, V.; Nobili, V. Diagnosis of nonalcoholic fatty liver disease in children and adolescents: Position paper of the espghan hepatology committee. J. Pediatr. Gastroenterol. Nutr. 2012, 54, 700–713. [Google Scholar] [CrossRef]
- Ferraioli, G.; Calcaterra, V.; Lissandrin, R.; Guazzotti, M.; Maiocchi, L.; Tinelli, C.; De Silvestri, A.; Regalbuto, C.; Pelizzo, G.; Larizza, D.; et al. Noninvasive assessment of liver steatosis in children: The clinical value of controlled attenuation parameter. BMC Gastroenterol. 2017, 17, 61. [Google Scholar] [CrossRef]
- Shi, M.; Liu, P.; Li, J.; Su, Y.; Zhou, X.; Wu, C.; Chen, X.; Zheng, C. The performance of noninvasive indexes of adults in identification of nonalcoholic fatty liver disease in children. J. Diabetes 2021, 13, 744–753. [Google Scholar] [CrossRef]



| Characteristics | Total (n = 258) | Normal (n = 229) | NAFLD (n = 29) | p |
|---|---|---|---|---|
| Age, years | 18.02 ± 1.41 | 18.00 ± 1.42 | 18.14 ± 1.33 | 0.621 |
| Male, n (%) | 136 (52.71) | 113 (49.34) | 23 (79.31) | 0.002 |
| Height SDS | 0.22 ± 1.08 | 0.19 ± 1.06 | 0.45 ± 1.24 | 0.221 |
| Weight SDS | 0.13 ± 1.4 | −0.11 ± 1.21 | 1.99 ± 1.38 | <0.001 |
| BMI, kg/m2 | 22.03 ± 4.12 | 21.24 ± 3.19 | 28.25 ± 5.27 | <0.001 |
| BMI SDS | 0.01 ± 1.48 | −0.25 ± 1.24 | 2.12 ± 1.56 | <0.001 |
| BMI grade, n (%) Normal | 200 (77.52) | 195 (85.15) | 5 (17.24) | <0.001 |
| Overweight | 27 (10.47) | 21 (9.17) | 6 (20.69) | |
| Obesity | 31 (12.02) | 13 (5.68) | 18 (62.07) | |
| WC, cm | 73.34 ± 10.8 | 71.29 ± 7.29 | 93.8 ± 17.78 | 0.003 |
| Central obesity, n (%) | 10 (9.09) | 5 (5) | 5 (50) | <0.001 |
| WHR | 0.77 ± 0.07 | 0.76 ± 0.06 | 0.87 ± 0.09 | <0.001 |
| WHtR | 0.44 ± 0.06 | 0.43 ± 0.05 | 0.54 ± 0.1 | 0.004 |
| Glucose, mg/dL | 90 ± 7.17 | 89.84 ± 7.07 | 91.28 ± 7.95 | 0.310 |
| AST, IU/L | 20.79 ± 9.38 | 20.25 ± 9.18 | 25.1 ± 9.98 | 0.008 |
| ALT, IU/L | 18.78 ± 16.98 | 16.21 ± 12.02 | 39.07 ± 31.46 | <0.001 |
| TC/HDL-C | 3.17 ± 0.72 | 3.07 ± 0.63 | 3.97 ± 0.88 | <0.001 |
| TG/HDL-C | 1.87 ± 1.76 | 1.68 ± 1.54 | 3.37 ± 2.54 | 0.001 |
| LDL-C/HDL-C | 1.93 ± 0.6 | 1.85 ± 0.55 | 2.56 ± 0.63 | <0.001 |
| Non-HDL-C/HDL-C | 2.17 ± 0.72 | 2.07 ± 0.63 | 2.97 ± 0.88 | <0.001 |
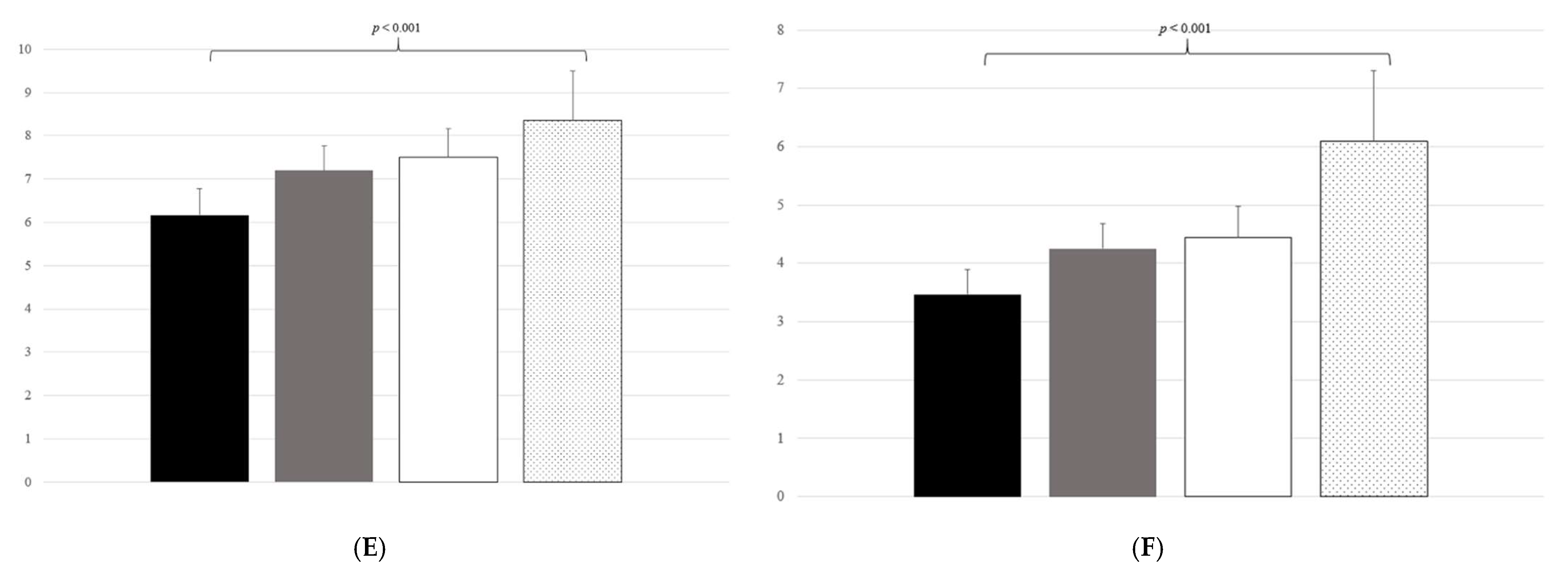
| TyG | 8.22 ± 0.44 | 8.17 ± 0.4 | 8.63 ± 0.54 | <0.001 |
| TyG-BMI | 181.76 ± 39.15 | 173.88 ± 29.45 | 243.96 ± 49.92 | <0.001 |
| TyG-BMI SDS | 0.32 ± 12.5 | −1.97 ± 10.26 | 18.36 ± 13.97 | <0.001 |
| TyG-WC | 603.33 ± 105.26 | 582.8 ± 69.55 | 808.65 ± 171.61 | 0.002 |
| TyG-WHR | 6.34 ± 0.79 | 6.18 ± 0.61 | 7.57 ± 0.89 | <0.001 |
| TyG-WHtR | 3.59 ± 0.59 | 3.48 ± 0.42 | 4.69 ± 0.92 | 0.002 |
| APRI | 0.33 ± 0.15 | 0.32 ± 0.14 | 0.37 ± 0.18 | 0.077 |
| APRI-BMI | 7.16 ± 3.41 | 6.76 ± 2.98 | 10.33 ± 4.76 | <0.001 |
| APRI-BMI SDS | 0.00 ± 0.54 | −0.10 ± 0.46 | 0.74 ± 0.56 | <0.001 |
| APRI-WC | 25.57 ± 10.23 | 25.03 ± 9.63 | 30.95 ± 14.55 | 0.237 |
| APRI-WHR | 0.25 ± 0.11 | 0.24 ± 0.09 | 0.33 ± 0.15 | 0.005 |
| APRI-WHtR | 0.15 ± 0.06 | 0.15 ± 0.06 | 0.18 ± 0.08 | 0.127 |
| FIB-4 | 6.39 ± 5.93 | 5.8 ± 4.98 | 11.1 ± 9.74 | 0.007 |
| HSI | 29.8 ± 6.28 | 28.53 ± 4.65 | 39.89 ± 8.15 | <0.001 |
| NAFLD grade | <0.001 | |||
| Grade 0, n (%) | 227 (87.98) | 227 (100.00) | 0 (0.00) | |
| Grade 1, n (%) | 17 (6.59) | 0 (0.00) | 17 (58.62) | |
| Grade 2, n (%) | 7 (2.71) | 0 (0.00) | 7 (24.13) | |
| Grade 3, n (%) | 7 (2.71) | 0 (0.00) | 7 (24.13) |
| Parameter | Tertile (Range) | OR (95% Cl) | p |
|---|---|---|---|
| TC/HDL-C | |||
| T1 (1.78, 2.80) | Reference | ||
| T2 (2.80, 3.45) | 3.721 (0.750–18.448) | 0.108 | |
| T3 (3.45, 5.80) | 12.724 (2.871–56.388) | <0.001 | |
| TG/HDL-C | |||
| T1 (0.43, 1.21) | Reference | ||
| T2 (1.21, 1.81) | 3.149 (0.618–16.061) | 0.168 | |
| T3 (1.81, 21.14) | 13.566 (3.070–59.951) | <0.001 | |
| LDL-C/HDL-C | |||
| T1 (0.56, 1.62) | Reference | ||
| T2 (1.62, 2.14) | 3.115 (0.610–15.899) | 0.172 | |
| T3 (2.15, 3.82) | 13.715 (3.099–60.701) | <0.001 | |
| Non-HDL-C/HDL-C | |||
| T1 (0.78, 1.80) | Reference | ||
| T2 (1.80, 2.45) | 3.721 (0.750–18.448) | 0.108 | |
| T3 (2.45, 4.80) | 12.724 (2.871–56.388) | <0.001 | |
| TyG | |||
| T1 (6.94, 8.03) | Reference | ||
| T2 (8.04, 8.38) | 2.049 (0.496–8.473) | 0.322 | |
| T3 (8.39, 10.28) | 8.513 (2.424–29.896) | <0.001 | |
| TyG-BMI | |||
| T1 (111.76, 161.92) | Reference | ||
| T2 (161.99, 191.35) | 3.035 (0.120–76.973) | 0.501 | |
| T3 (191.55, 442.29) | 84.284 (4.964–1431.064) | 0.002 | |
| TyG-BMI SDS | |||
| T1 (−36.73, −5.27) | Reference | ||
| T2 (−5.27, 3.40) | 3.035 (0.120–76.973) | 0.501 | |
| T3 (3.64, 73.23) | 84.284 (4.964–1431.064) | 0.002 | |
| TyG-WC | |||
| T1 (433.82, 563.56) | Reference | ||
| T2 (563.71, 616.19) | 0.974 (0.018–53.130) | 0.990 | |
| T3 (618.63, 1257.24) | 27.869 (1.504–516.395) | 0.026 | |
| TyG-WHR | |||
| T1 (4.81, 5.94) | Reference | ||
| T2 (5.94, 6.57) | 7.271 (0.363–145.773) | 0.195 | |
| T3 (6.61, 10.76) | 73.974 (4.334–1262.656) | 0.003 | |
| TyG-WHtR | |||
| T1 (2.55, 3.32) | Reference | ||
| T2 (3.32, 3.67) | 0.974 (0.018–53.130) | 0.990 | |
| T3 (3.69, 6.95) | 27.869 (1.504–516.395) | 0.026 | |
| APRI | |||
| T1 (0.15, 0.25) | Reference | ||
| T2 (0.26, 0.33) | 1.319 (0.468–3.719) | 0.600 | |
| T3 (0.33, 1.60) | 2.010 (0.760–5.314) | 0.159 | |
| APRI-BMI | |||
| T1 (2.64, 5.46) | Reference | ||
| T2 (5.47, 7.23) | 3.721 (0.750–18.448) | 0.108 | |
| T3 (7.26, 27.63) | 12.724 (2.871–56.388) | <0.001 | |
| APRI-BMI SDS | |||
| T1 (−3.42, −0.20) | Reference | ||
| T2 (−0.19, 0.13) | 3.035 (0.120–76.973) | 0.501 | |
| T3 (0.14, 2.22) | 84.284 (4.964–1431.064) | 0.002 | |
| APRI-WC | |||
| T1 (13.08, 20.35) | Reference | ||
| T2 (20.77, 25.77) | 3.088 (0.306–31.170) | 0.339 | |
| T3 (25.83, 74.34) | 6.774 (0.772–59.418) | 0.084 | |
| APRI-WHR | |||
| T1 (0.10, 0.19) | Reference | ||
| T2 (0.19, 0.26) | 0.789 (0.204–3.054) | 0.732 | |
| T3 (0.26, 0.78) | 4.672 (1.649–13.238) | 0.004 | |
| APRI-WHtR | |||
| T1 (0.08, 0.12) | Reference | ||
| T2 (0.13, 0.15) | 1.500 (0.236–9.552) | 0.668 | |
| T3 (0.15, 0.42) | 2.656 (0.481–14.677) | 0.263 | |
| FIB-4 | |||
| T1 (1.82, 3.76) | Reference | ||
| T2 (3.79, 5.84) | 2.451 (0.612–9.814) | 0.205 | |
| T3 (5.85, 45.91) | 7.846 (2.227–27.645) | 0.001 | |
| HSI | |||
| T1 (17.88, 26.82) | Reference | ||
| T2 (26.90, 30.80) | 5.000 (0.232–107.601) | 0.304 | |
| T3 (30.86, 65.70) | 79.035 (4.650–1343.230) | 0.003 |
| Parameter | Cut-Off | Sensitivity | Specificity | NPV | AUC | 95% CI | p |
|---|---|---|---|---|---|---|---|
| TyG | 8.466 | 65.517 | 80.349 | 94.845 | 0.761 | (0.658–0.864) | <0.001 |
| TyG-BMI | 201.617 | 89.655 | 87.773 | 98.529 | 0.941 | (0.908–0.974) | <0.001 |
| TyG-BMI SDS | 3.809 | 96.552 | 76.419 | 99.432 | 0.924 | (0.887–0.960) | <0.001 |
| TyG-WC | 682.997 | 100.000 | 93.000 | 100 | 0.972 | (0.943–1.000) | <0.001 |
| TyG-WHR | 6.708 | 89.286 | 79.717 | 98.256 | 0.923 | (0.877–0.970) | <0.001 |
| TyG-WHtR | 3.955 | 90.000 | 89.000 | 98.889 | 0.947 | (0.896–0.998) | <0.001 |
| APRI | 0.458 | 24.138 | 90.393 | 90.393 | 0.575 | (0.456–0.693) | 0.217 |
| APRI-BMI | 7.923 | 65.517 | 76.856 | 94.624 | 0.773 | (0.685–0.86) | <0.001 |
| APRI-BMI SDS | 0.283 | 89.655 | 85.153 | 98.485 | 0.926 | (0.89–0.962) | <0.001 |
| APRI-WC | 23.756 | 80.000 | 55.000 | 96.491 | 0.684 | (0.53–0.838) | 0.019 |
| APRI-WHR | 0.275 | 64.286 | 77.830 | 94.286 | 0.708 | (0.601–0.815) | <0.001 |
| APRI-WHtR | 0.143 | 80.000 | 57.000 | 96.610 | 0.662 | (0.495–0.829) | 0.057 |
| FIB-4 | 5.201 | 75.862 | 63.319 | 95.395 | 0.737 | (0.635–0.838) | <0.001 |
| HSI | 31.680 | 93.103 | 82.969 | 98.958 | 0.929 | (0.889–0.968) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, K.; Lee, H.W.; Choi, H.S.; Park, G.; Lee, H.S.; Kim, S.J.; Lee, M.; Suh, J.; Kwon, A.; Kim, H.-S.; et al. Comparison of the Modified TyG Indices and Other Parameters to Predict Non-Alcoholic Fatty Liver Disease in Youth. Biology 2022, 11, 685. https://doi.org/10.3390/biology11050685
Song K, Lee HW, Choi HS, Park G, Lee HS, Kim SJ, Lee M, Suh J, Kwon A, Kim H-S, et al. Comparison of the Modified TyG Indices and Other Parameters to Predict Non-Alcoholic Fatty Liver Disease in Youth. Biology. 2022; 11(5):685. https://doi.org/10.3390/biology11050685
Chicago/Turabian StyleSong, Kyungchul, Hae Won Lee, Han Saem Choi, Goeun Park, Hye Sun Lee, Su Jin Kim, Myeongseob Lee, Junghwan Suh, Ahreum Kwon, Ho-Seong Kim, and et al. 2022. "Comparison of the Modified TyG Indices and Other Parameters to Predict Non-Alcoholic Fatty Liver Disease in Youth" Biology 11, no. 5: 685. https://doi.org/10.3390/biology11050685
APA StyleSong, K., Lee, H. W., Choi, H. S., Park, G., Lee, H. S., Kim, S. J., Lee, M., Suh, J., Kwon, A., Kim, H.-S., & Chae, H. W. (2022). Comparison of the Modified TyG Indices and Other Parameters to Predict Non-Alcoholic Fatty Liver Disease in Youth. Biology, 11(5), 685. https://doi.org/10.3390/biology11050685







