Endothelial Progenitor Cell Response to Acute Multicomponent Exercise Sessions with Different Durations
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Demographics and Clinical Data
2.3. EPCs and CECs Quantification by Flow Cytometry
2.4. Exercise Sessions
2.5. Statistical Analysis
3. Results
3.1. Participant Characteristics
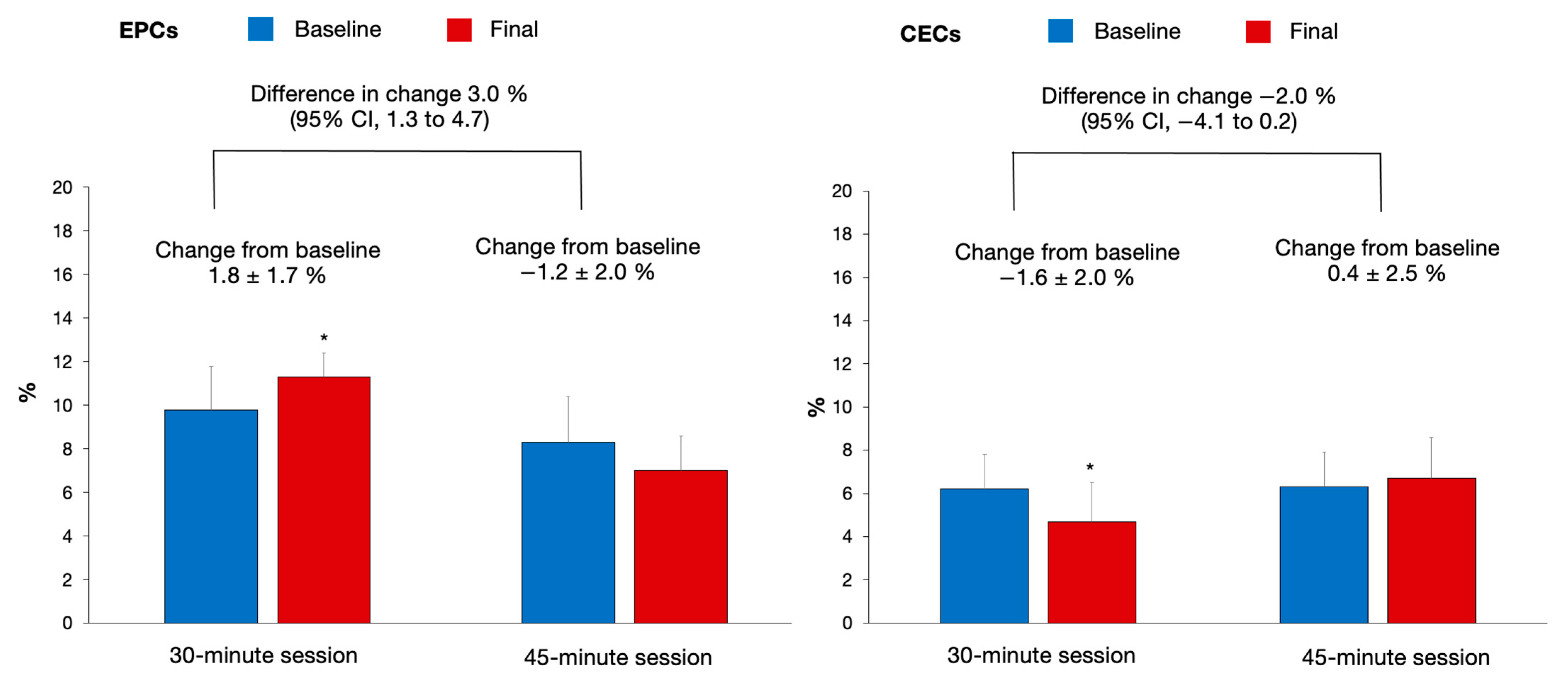
3.2. Effects on EPCs and CECs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jia, G.; Aroor, A.R.; Jia, C.; Sowers, J.R. Endothelial cell senescence in aging-related vascular dysfunction. Biochim. Biophys. Acta Mol. Basis Dis. 2019, 1865, 1802–1809. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.J.; Wu, Z.Y.; Nie, X.W.; Bian, J.S. Role of Endothelial Dysfunction in Cardiovascular Diseases: The Link Between Inflammation and Hydrogen Sulfide. Front. Pharmacol. 2019, 10, 1568. [Google Scholar] [CrossRef] [PubMed]
- Park, K.-H.; Park, W.J. Endothelial Dysfunction: Clinical Implications in Cardiovascular Disease and Therapeutic Approaches. J. Korean Med. Sci. 2015, 30, 1213–1225. [Google Scholar] [CrossRef] [PubMed]
- Giannitsi, S.; Bougiakli, M.; Bechlioulis, A.; Naka, K. Endothelial dysfunction and heart failure: A review of the existing bibliography with emphasis on flow mediated dilation. JRSM Cardiovasc. Dis. 2019, 8, 2048004019843047. [Google Scholar] [CrossRef]
- Asahara, T.; Murohara, T.; Sullivan, A.; Silver, M.; van der Zee, R.; Li, T.; Witzenbichler, B.; Schatteman, G.; Isner, J.M. Isolation of putative progenitor endothelial cells for angiogenesis. Science 1997, 275, 964–967. [Google Scholar] [CrossRef]
- Yoder, M.C. Human endothelial progenitor cells. Cold Spring Harb. Perspect. Med. 2012, 2, a006692. [Google Scholar] [CrossRef]
- Wang, J.S.; Lee, M.Y.; Lien, H.Y.; Weng, T.P. Hypoxic exercise training improves cardiac/muscular hemodynamics and is associated with modulated circulating progenitor cells in sedentary men. Int. J. Cardiol. 2014, 170, 315–323. [Google Scholar] [CrossRef]
- Guo, Y.; Ledesma, R.A.; Peng, R.; Liu, Q.; Xu, D. The Beneficial Effects of Cardiac Rehabilitation on the Function and Levels of Endothelial Progenitor Cells. Heart Lung Circ. 2017, 26, 10–17. [Google Scholar] [CrossRef][Green Version]
- Rosenzweig, A. Endothelial progenitor cells. N. Engl. J. Med. 2003, 348, 581–582. [Google Scholar] [CrossRef]
- Koutroumpi, M.; Dimopoulos, S.; Psarra, K.; Kyprianou, T.; Nanas, S. Circulating endothelial and progenitor cells: Evidence from acute and long-term exercise effects. World J. Cardiol. 2012, 4, 312–326. [Google Scholar] [CrossRef]
- Zhang, M.; Malik, A.B.; Rehman, J. Endothelial progenitor cells and vascular repair. Curr. Opin. Hematol. 2014, 21, 224–228. [Google Scholar] [CrossRef] [PubMed]
- Ross, M.D. Endothelial Regenerative Capacity and Aging: Influence of Diet, Exercise and Obesity. Curr. Cardiol. Rev. 2018, 14, 233–244. [Google Scholar] [CrossRef] [PubMed]
- Mudyanadzo, T.A. Endothelial Progenitor Cells and Cardiovascular Correlates. Cureus 2018, 10, e3342. [Google Scholar] [CrossRef] [PubMed]
- Aragona, C.O.; Imbalzano, E.; Mamone, F.; Cairo, V.; Lo Gullo, A.; D’Ascola, A.; Sardo, M.A.; Scuruchi, M.; Basile, G.; Saitta, A.; et al. Endothelial Progenitor Cells for Diagnosis and Prognosis in Cardiovascular Disease. Stem Cells Int. 2016, 2016, 8043792. [Google Scholar] [CrossRef] [PubMed]
- Chong, A.Y.; Blann, A.D.; Patel, J.; Freestone, B.; Hughes, E.; Lip, G.Y. Endothelial dysfunction and damage in congestive heart failure: Relation of flow-mediated dilation to circulating endothelial cells, plasma indexes of endothelial damage, and brain natriuretic peptide. Circulation 2004, 110, 1794–1798. [Google Scholar] [CrossRef]
- Lee, K.W.; Lip, G.Y.; Tayebjee, M.; Foster, W.; Blann, A.D. Circulating endothelial cells, von Willebrand factor, interleukin-6, and prognosis in patients with acute coronary syndromes. Blood 2005, 105, 526–532. [Google Scholar] [CrossRef]
- Farinacci, M.; Krahn, T.; Dinh, W.; Volk, H.-D.; Düngen, H.-D.; Wagner, J.; Konen, T.; von Ahsen, O. Circulating endothelial cells as biomarker for cardiovascular diseases. Res. Pract. Thromb. Haemost. 2018, 3, 49–58. [Google Scholar] [CrossRef]
- Pelliccia, A.; Sharma, S.; Gati, S.; Bäck, M.; Börjesson, M.; Caselli, S.; Collet, J.P.; Corrado, D.; Drezner, J.A.; Halle, M.; et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur. Heart J. 2021, 42, 17–96. [Google Scholar] [CrossRef]
- World Health Organization. Global Recommendations on Physical Activity for Health; World Health Organization: Geneva, Switzerland, 2010; pp. 3–58. [Google Scholar]
- Pedralli, M.L.; Marschner, R.A.; Kollet, D.P.; Neto, S.G.; Eibel, B.; Tanaka, H.; Lehnen, A.M. Different exercise training modalities produce similar endothelial function improvements in individuals with prehypertension or hypertension: A randomized clinical trial. Sci. Rep. 2020, 10, 7628. [Google Scholar] [CrossRef]
- Santos-Parker, J.R.; LaRocca, T.J.; Seals, D.R. Aerobic exercise and other healthy lifestyle factors that influence vascular aging. Adv. Physiol. Educ. 2014, 38, 296–307. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Lopes, J.; Teixeira, M.; Cavalcante, S.; Gouveia, M.; Duarte, A.; Ferreira, M.; Simões, M.I.; Conceição, M.; Ribeiro, I.P.; Gonçalves, A.C.; et al. Reduced Levels of Circulating Endothelial Cells and Endothelial Progenitor Cells in Patients with Heart Failure with Reduced Ejection Fraction. Arch. Med. Res. 2022, 22, S0188–S4409. [Google Scholar] [CrossRef] [PubMed]
- Samman Tahhan, A.; Hammadah, M.; Sandesara, P.B.; Hayek, S.S.; Kalogeropoulos, A.P.; Alkhoder, A.; Mohamed Kelli, H.; Topel, M.; Ghasemzadeh, N.; Chivukula, K.; et al. Progenitor Cells and Clinical Outcomes in Patients With Heart Failure. Circ. Heart Fail. 2017, 10, e004106. [Google Scholar] [CrossRef] [PubMed]
- Chiang, C.H.; Huang, P.H.; Leu, H.B.; Hsu, C.Y.; Wang, K.F.; Chen, J.W.; Lin, S.J. Decreased circulating endothelial progenitor cell levels in patients with heart failure with preserved ejection fraction. Cardiology 2013, 126, 191–201. [Google Scholar] [CrossRef] [PubMed]
- Sandri, M.; Viehmann, M.; Adams, V.; Rabald, K.; Mangner, N.; Höllriegel, R.; Lurz, P.; Erbs, S.; Linke, A.; Kirsch, K.; et al. Chronic heart failure and aging—Effects of exercise training on endothelial function and mechanisms of endothelial regeneration: Results from the Leipzig Exercise Intervention in Chronic heart failure and Aging (LEICA) study. Eur. J. Prev. Cardiol. 2016, 23, 349–358. [Google Scholar] [CrossRef] [PubMed]
- Van Craenenbroeck, E.M.; Hoymans, V.Y.; Beckers, P.J.; Possemiers, N.M.; Wuyts, K.; Paelinck, B.P.; Vrints, C.J.; Conraads, V.M. Exercise training improves function of circulating angiogenic cells in patients with chronic heart failure. Basic Res. Cardiol. 2010, 105, 665–676. [Google Scholar] [CrossRef]
- Kourek, C.; Alshamari, M.; Mitsiou, G.; Psarra, K.; Delis, D.; Linardatou, V.; Pittaras, T.; Ntalianis, A.; Papadopoulos, C.; Panagopoulou, N.; et al. The acute and long-term effects of a cardiac rehabilitation program on endothelial progenitor cells in chronic heart failure patients: Comparing two different exercise training protocols. Int. J. Cardiol. Heart Vasc. 2021, 32, 100702. [Google Scholar] [CrossRef]
- Whyte, J.J.; Laughlin, M.H. The effects of acute and chronic exercise on the vasculature. Acta Physiol. 2010, 199, 441–450. [Google Scholar] [CrossRef]
- Ribeiro, F.; Ribeiro, I.P.; Gonçalves, A.C.; Alves, A.J.; Melo, E.; Fernandes, R.; Costa, R.; Sarmento-Ribeiro, A.B.; Duarte, J.A.; Carreira, I.M.; et al. Effects of resistance exercise on endothelial progenitor cell mobilization in women. Sci. Rep. 2017, 7, 17880. [Google Scholar] [CrossRef]
- Harris, E.; Rakobowchuk, M.; Birch, K.M. Interval exercise increases angiogenic cell function in postmenopausal women. BMJ Open Sport Exerc. Med. 2017, 3, e000248. [Google Scholar] [CrossRef]
- Krüger, K.; Alack, K.; Ringseis, R.; Mink, L.; Pfeifer, E.; Schinle, M.; Gindler, K.; Kimmelmann, L.; Walscheid, R.; Muders, K.; et al. Apoptosis of T-Cell Subsets after Acute High-Intensity Interval Exercise. Med. Sci. Sports Exerc. 2016, 48, 2021–2029. [Google Scholar] [CrossRef] [PubMed]
- Laufs, U.; Urhausen, A.; Werner, N.; Scharhag, J.; Heitz, A.; Kissner, G.; Böhm, M.; Kindermann, W.; Nickenig, G. Running exercise of different duration and intensity: Effect on endothelial progenitor cells in healthy subjects. Eur. J. Cardiovasc. Prev. Rehabil. 2005, 12, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Schaan, B.D.; Waclawovsky, G.; Umpierre, D.; Figueira, F.R.; de Lima, E.S.; Alegretti, A.P.; Schneider, L.; Matte, U.S.; Rodrigues, T.C. A single session of aerobic or resistance exercise modifies the endothelial progenitor cell levels in healthy subjects, but not in individuals with type 1 diabetes. Diabetol. Metab. Syndr. 2015, 7, A251. [Google Scholar] [CrossRef]
- Krüger, K.; Pilat, C.; Schild, M.; Lindner, N.; Frech, T.; Muders, K.; Mooren, F.C. Progenitor cell mobilization after exercise is related to systemic levels of G-CSF and muscle damage. Scand. J. Med. Sci. Sports 2015, 25, e283–e291. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, Y.; Du, S.; Wang, Q.; Xia, H.; Sun, R. Exercise interventions for improving physical function, daily living activities and quality of life in community-dwelling frail older adults: A systematic review and meta-analysis of randomized controlled trials. Geriatr. Nurs. 2020, 41, 261–273. [Google Scholar] [CrossRef]
- García-Hermoso, A.; Ramirez-Vélez, R.; Sáez de Asteasu, M.L.; Martínez-Velilla, N.; Zambom-Ferraresi, F.; Valenzuela, P.L.; Lucia, A.; Izquierdo, M. Safety and Effectiveness of Long-Term Exercise Interventions in Older Adults: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Sports Med. 2020, 50, 1095–1106. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- Hoymans, V.Y.; Van Craenenbroeck, A.H.; Bruyndonckx, L.; van Ierssel, S.H.; Vrints, C.J.; Conraads, V.M.; Van Craenenbroeck, E.M. TransFix® for delayed flow cytometry of endothelial progenitor cells and angiogenic T cells. Microvasc. Res. 2012, 84, 384–386. [Google Scholar] [CrossRef]
- Ahmed, F.W.; Rider, R.; Glanville, M.; Narayanan, K.; Razvi, S.; Weaver, J.U. Metformin improves circulating endothelial cells and endothelial progenitor cells in type 1 diabetes: MERIT study. Cardiovasc. Diabetol. 2016, 15, 116. [Google Scholar] [CrossRef]
- O′Carroll, L.; Wardrop, B.; Murphy, R.P.; Ross, M.D.; Harrison, M. Circulating angiogenic cell response to sprint interval and continuous exercise. Eur. J. Appl. Physiol. 2019, 119, 743–752. [Google Scholar] [CrossRef]
- West, D.J.; Campbell, M.D.; Gonzalez, J.T.; Walker, M.; Stevenson, E.J.; Ahmed, F.W.; Wijaya, S.; Shaw, J.A.; Weaver, J.U. The inflammation, vascular repair and injury responses to exercise in fit males with and without Type 1 diabetes: An observational study. Cardiovasc. Diabetol. 2015, 14, 71. [Google Scholar] [CrossRef] [PubMed]
- Sapp, R.M.; Evans, W.S.; Eagan, L.E.; Chesney, C.A.; Zietowski, E.M.; Prior, S.J.; Ranadive, S.M.; Hagberg, J.M. The effects of moderate and high-intensity exercise on circulating markers of endothelial integrity and activation in young, healthy men. J. Appl. Physiol. 2019, 127, 1245–1256. [Google Scholar] [CrossRef] [PubMed]
- Mutin, M.; Canavy, I.; Blann, A.; Bory, M.; Sampol, J.; Dignat-George, F. Direct evidence of endothelial injury in acute myocardial infarction and unstable angina by demonstration of circulating endothelial cells. Blood 1999, 93, 2951–2958. [Google Scholar] [CrossRef] [PubMed]
- Boos, C.J.; Balakrishnan, B.; Lip, G.Y. The effects of exercise stress testing on soluble E-selectin, von Willebrand factor, and circulating endothelial cells as indices of endothelial damage/dysfunction. Ann. Med. 2008, 40, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Dawson, E.A.; Green, D.J.; Cable, N.T.; Thijssen, D.H. Effects of acute exercise on flow-mediated dilatation in healthy humans. J. Appl. Physiol. 2013, 115, 1589–1598. [Google Scholar] [CrossRef] [PubMed]
- Krüger, K.; Klocke, R.; Kloster, J.; Nikol, S.; Waltenberger, J.; Mooren, F.C. Activity of daily living is associated with circulating CD34+/KDR+ cells and granulocyte colony-stimulating factor levels in patients after myocardial infarction. J. Appl. Physiol. 2014, 116, 532–537. [Google Scholar] [CrossRef]
- Volaklis, K.A.; Tokmakidis, S.P.; Halle, M. Acute and chronic effects of exercise on circulating endothelial progenitor cells in healthy and diseased patients. Clin. Res. Cardiol. 2013, 102, 249–257. [Google Scholar] [CrossRef]
- Thijssen, D.H.; Dawson, E.A.; Black, M.A.; Hopman, M.T.; Cable, N.T.; Green, D.J. Brachial artery blood flow responses to different modalities of lower limb exercise. Med. Sci. Sports Exerc. 2009, 41, 1072–1079. [Google Scholar] [CrossRef]
- Thijssen, D.H.; Dawson, E.A.; Tinken, T.M.; Cable, N.T.; Green, D.J. Retrograde flow and shear rate acutely impair endothelial function in humans. Hypertension 2009, 53, 986–992. [Google Scholar] [CrossRef]
- Sabatier, F.; Camoin-Jau, L.; Anfosso, F.; Sampol, J.; Dignat-George, F. Circulating endothelial cells, microparticles and progenitors: Key players towards the definition of vascular competence. J. Cell. Mol. Med. 2009, 13, 454–471. [Google Scholar] [CrossRef]
| Age (years) | 67.1 ± 8.6 |
| Sex (Male/Female) | 3/7 |
| Weight (kg) | 65.9 ± 12.4 |
| Height (cm) | 158.8 ± 8.8 |
| Systolic blood pressure (mmHg) | 129.6 ± 19.4 |
| Diastolic blood pressure (mmHg) | 77.7 ± 11.4 |
| Heart rate (bpm) | 69.4 ± 7.6 |
| Waist circumference (cm) | 93.0 ± 13.2 |
| Body mass index (kg/m2) | 26.0 ± 3.3 |
| Cardiovascular risk factors (n, %) | |
| Obesity class I | 2 (20) |
| Overweight | 4 (40) |
| Hypertension | 3 (30) |
| Type 2 Diabetes mellitus | 2 (20) |
| Dyslipidemia | 5 (50) |
| Current smoker | 1 (10) |
| Medication (n, %) | |
| Statins | 3 (30) |
| Diuretics | 1 (10) |
| Angiotensin II receptor blockers | 1 (10) |
| Anticoagulants | 1 (10) |
| Calcium channel blockers | 1 (10) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cavalcante, S.; Teixeira, M.; Duarte, A.; Ferreira, M.; Simões, M.I.; Conceição, M.; Costa, M.; Ribeiro, I.P.; Gonçalves, A.C.; Oliveira, J.; et al. Endothelial Progenitor Cell Response to Acute Multicomponent Exercise Sessions with Different Durations. Biology 2022, 11, 572. https://doi.org/10.3390/biology11040572
Cavalcante S, Teixeira M, Duarte A, Ferreira M, Simões MI, Conceição M, Costa M, Ribeiro IP, Gonçalves AC, Oliveira J, et al. Endothelial Progenitor Cell Response to Acute Multicomponent Exercise Sessions with Different Durations. Biology. 2022; 11(4):572. https://doi.org/10.3390/biology11040572
Chicago/Turabian StyleCavalcante, Suiane, Manuel Teixeira, Ana Duarte, Miriam Ferreira, Maria I. Simões, Maria Conceição, Mariana Costa, Ilda P. Ribeiro, Ana Cristina Gonçalves, José Oliveira, and et al. 2022. "Endothelial Progenitor Cell Response to Acute Multicomponent Exercise Sessions with Different Durations" Biology 11, no. 4: 572. https://doi.org/10.3390/biology11040572
APA StyleCavalcante, S., Teixeira, M., Duarte, A., Ferreira, M., Simões, M. I., Conceição, M., Costa, M., Ribeiro, I. P., Gonçalves, A. C., Oliveira, J., & Ribeiro, F. (2022). Endothelial Progenitor Cell Response to Acute Multicomponent Exercise Sessions with Different Durations. Biology, 11(4), 572. https://doi.org/10.3390/biology11040572







