The Paediatric Glaucoma Diagnostic Ability of Optical Coherence Tomography: A Comparison of Macular Segmentation and Peripapillary Retinal Nerve Fibre Layer Thickness
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Glaucoma Diagnosis and Related Parameters
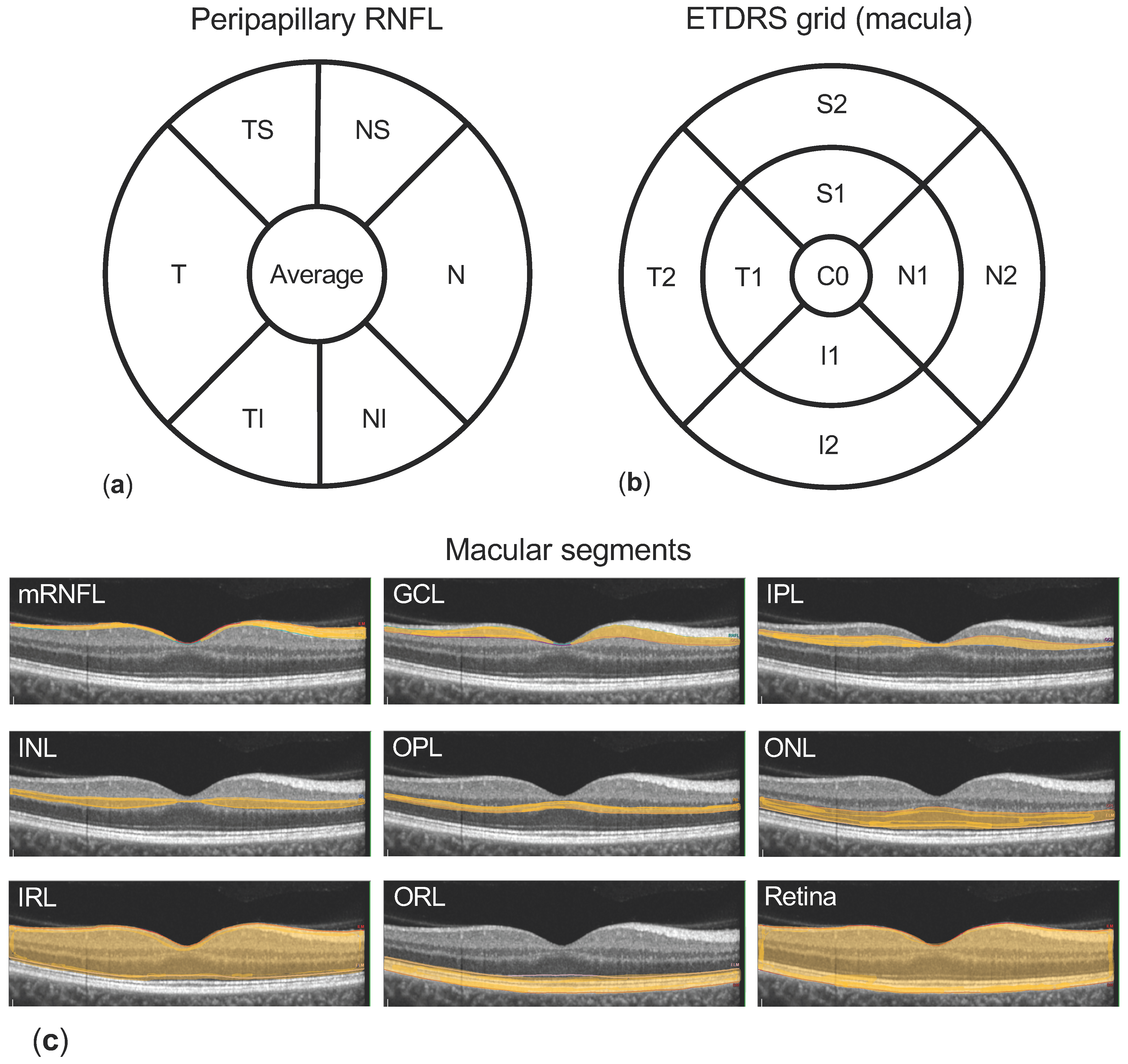
2.3. OCT Measurements
2.4. Statistical Analysis
3. Results
3.1. Patients’ Characteristics
3.2. Comparison of Macular Layer Thickness in Glaucoma Patients and Healthy Individuals
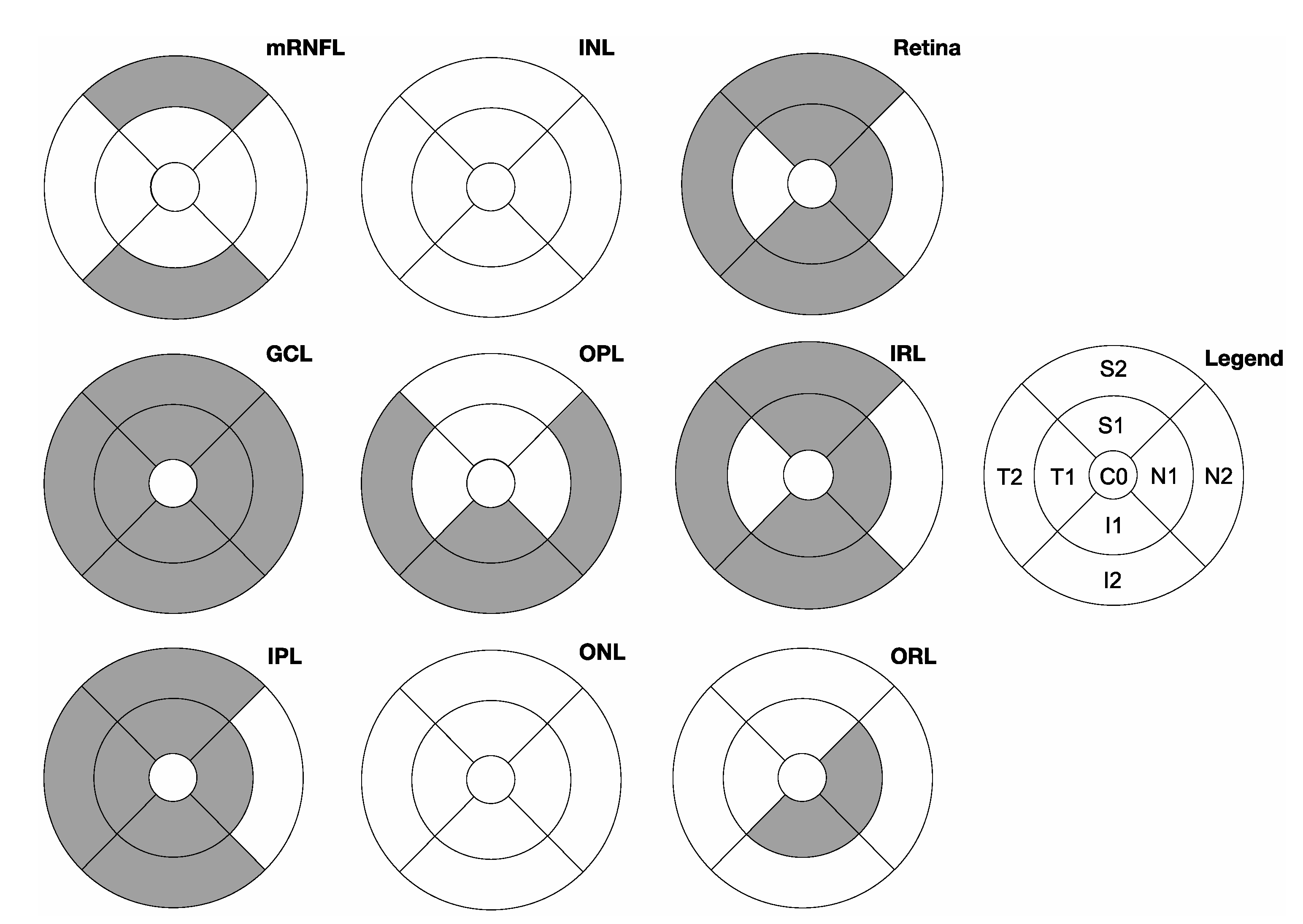
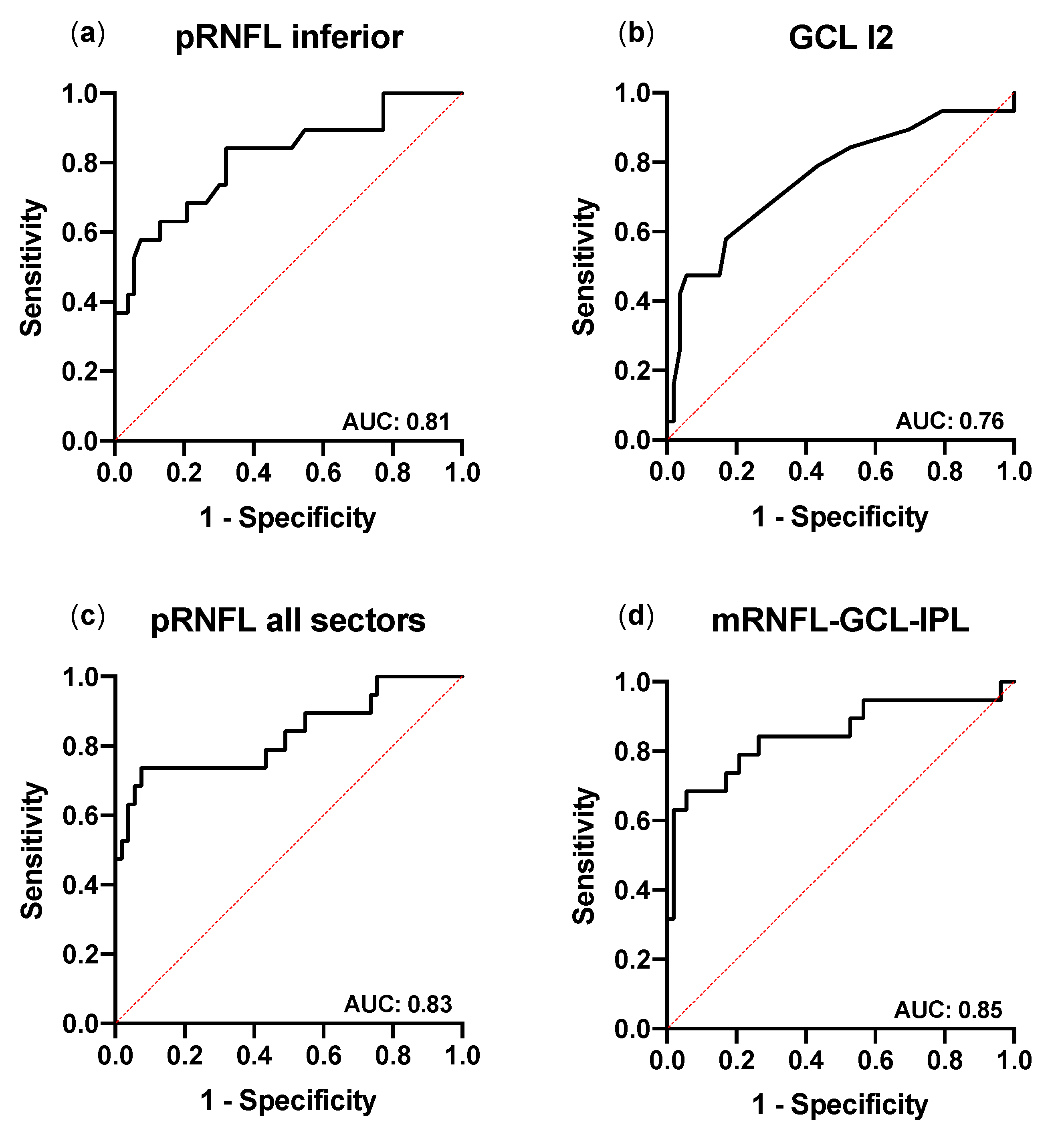
3.3. Glaucoma Discriminative Ability of pRNFL and Macular Thickness Measurements
4. Discussion
- The thickness of both pRNFL and selected macular segments is reduced in glaucoma patients;
- The reduced thickness of the pRNFL and of macular segments correlate positively with the presence of glaucoma;
- The thickness of the pRNFL and of macular segments shows a high discriminative ability in paediatric glaucoma.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hoguet, A.; Grajewski, A.; Hodapp, E.; Chang, T.C.P. A retrospective survey of childhood glaucoma prevalence according to Childhood Glaucoma Research Network classification. Indian J. Ophthalmol. 2016, 64, 118–123. [Google Scholar] [CrossRef]
- Gilbert, C.; Rahi, J.; Quinn, G. Visual impairment and blindness in children. In The Epidemiology of Eye Disease; Johnson, G., Minassian, D., Weale, R., West, S., Eds.; Edward Arnold Ltd.: London, UK, 2003; pp. 260–286. [Google Scholar]
- Thau, A.; Lloyd, M.; Freedman, S.; Beck, A.; Grajewski, A.; Levin, A.V. New classification system for pediatric glaucoma: Implications for clinical care and a research registry. Curr. Opin. Ophthalmol. 2018, 29, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Gospe, S.M.; Bhatti, M.T.; El-Dairi, M.A. Emerging Applications of Optical Coherence Tomography in Pediatric Optic Neuropathies. Semin. Pediatr. Neurol. 2017, 24, 135–142. [Google Scholar] [CrossRef]
- Langenegger, S.J.; Funk, J.; Töteberg-Harms, M. Reproducibility of Retinal Nerve Fiber Layer Thickness Measurements Using the Eye Tracker and the Retest Function of Spectralis SD-OCT in Glaucomatous and Healthy Control Eyes. Investig. Opthalmology Vis. Sci. 2011, 52, 3338. [Google Scholar] [CrossRef][Green Version]
- Xu, L.; Freedman, S.F.; Silverstein, E.; Muir, K.; El-Dairi, M. Longitudinal reproducibility of spectral domain optical coherence tomography in children with physiologic cupping and stable glaucoma. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2019. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.; Swanson, E.; Lin, C.; Schuman, J.; Stinson, W.; Chang, W.; Hee, M.; Flotte, T.; Gregory, K.; Puliafito, C.; et al. Optical coherence tomography. Science 1991, 254, 1178–1181. [Google Scholar] [CrossRef]
- Ghasia, F.F.; Freedman, S.F.; Rajani, A.; Holgado, S.; Asrani, S.; El-Dairi, M. Optical coherence tomography in paediatric glaucoma: Time domain versus spectral domain. Br. J. Ophthalmol. 2013, 97, 837–842. [Google Scholar] [CrossRef]
- Zhang, Q.; Qi, Y.; Chen, L.; Shi, X.; Bai, Y.; Huang, L.; Yu, W.; Jiang, Y.; Zhao, M.; Li, X. The relationship between anti-vascular endothelial growth factor and fibrosis in proliferative retinopathy: Clinical and laboratory evidence. Br. J. Ophthalmol. 2016, 100, 1443–1450. [Google Scholar] [CrossRef][Green Version]
- Chauhan, B.C.; Nicolela, M.T.; Artes, P.H. Incidence and rates of visual field progression after longitudinally measured optic disc change in glaucoma. Ophthalmology 2009, 116, 2110–2118. [Google Scholar] [CrossRef] [PubMed]
- El-Dairi, M.A.; Holgado, S.; Asrani, S.G.; Enyedi, L.B.; Freedman, S.F. Correlation between optical coherence tomography and glaucomatous optic nerve head damage in children. Br. J. Ophthalmol. 2009, 93, 1325–1330. [Google Scholar] [CrossRef]
- Hess, D.B.; Asrani, S.G.; Bhide, M.G.; Enyedi, L.B.; Stinnett, S.S.; Freedman, S.F. Macular and retinal nerve fiber layer analysis of normal and glaucomatous eyes in children using optical coherence tomography. Am. J. Ophthalmol. 2005, 139, 509–517. [Google Scholar] [CrossRef]
- Zareii, R.; Soleimani, M.; Moghimi, S.; Eslami, Y.; Fakhraie, G.; Amini, H. Relationship between GDx VCC and Stratus OCT in juvenile glaucoma. Eye 2009, 23, 2182–2186. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Curcio, C.A.; Allen, K.A. Topography of ganglion cells in human retina. J. Comp. Neurol. 1990, 300, 5–25. [Google Scholar] [CrossRef] [PubMed]
- Oddone, F.; Lucenteforte, E.; Michelessi, M.; Rizzo, S.; Donati, S.; Parravano, M.; Virgili, G. Macular versus Retinal Nerve Fiber Layer Parameters for Diagnosing Manifest Glaucoma: A Systematic Review of Diagnostic Accuracy Studies. Ophthalmology 2016, 123, 939–949. [Google Scholar] [CrossRef] [PubMed]
- Gama, R.; Santos, J.C.; Costa, R.S.; da Costa, D.C.; Eirô, N. Optical coherence tomography analysis of the inner retinal layers in children. Can. J. Ophthalmol. 2018, 53, 614–620. [Google Scholar] [CrossRef]
- Sung, K.R.; Wollstein, G.; Kim, N.R.; Na, J.H.; Nevins, J.E.; Kim, C.Y.; Schuman, J.S. Macular assessment using optical coherence tomography for glaucoma diagnosis. Br. J. Ophthalmol. 2012, 96, 1452–1455. [Google Scholar] [CrossRef] [PubMed]
- Pazos, M.; Dyrda, A.A.; Biarnés, M.; Gómez, A.; Martín, C.; Mora, C.; Fatti, G.; Antón, A. Diagnostic Accuracy of Spectralis SD OCT Automated Macular Layers Segmentation to Discriminate Normal from Early Glaucomatous Eyes. Ophthalmology 2017, 124, 1218–1228. [Google Scholar] [CrossRef] [PubMed]
- Unterlauft, J.D.; Rehak, M.; Böhm, M.R.R.; Rauscher, F.G. Analyzing the impact of glaucoma on the macular architecture using spectral-domain optical coherence tomography. PLoS ONE 2018, 13, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.R.; Lee, E.S.; Seong, G.J.; Kim, J.H.; An, H.G.; Kim, C.Y. Structure–Function Relationship and Diagnostic Value of Macular Ganglion Cell Complex Measurement Using Fourier-Domain OCT in Glaucoma. Investig. Opthalmology Vis. Sci. 2010, 51, 4646. [Google Scholar] [CrossRef] [PubMed]
- Casado, A.; Cerveró, A.; López-de-Eguileta, A.; Fernández, R.; Fonseca, S.; González, J.C.; Pacheco, G.; Gándara, E.; Gordo-Vega, M.Á. Topographic correlation and asymmetry analysis of ganglion cell layer thinning and the retinal nerve fiber layer with localized visual field defects. PLoS ONE 2019, 14, e0222347. [Google Scholar] [CrossRef]
- Silverstein, E.; Freedman, S.; Zéhil, G.-P.P.; Jiramongkolchai, K.; El-Dairi, M. The macula in pediatric glaucoma: Quantifying the inner and outer layers via optical coherence tomography automatic segmentation. J. AAPOS 2016, 20, 332–336. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, S.; Addepalli, U.K.; Rao, H.L.; Garudadri, C.S.; Mandal, A.K. Spectral domain optical coherence tomography in children operated for primary congenital glaucoma. Br. J. Ophthalmol. 2014, 98, 162–165. [Google Scholar] [CrossRef]
- Morales-Fernandez, L.; Jimenez-Santos, M.; Martinez-de-la-Casa, J.M.; Sanchez-Jean, R.; Nieves, M.; Saenz-Frances, F.; Garcia-Saenz, S.; Perucho, L.; Gomez-de-Liaño, R.; Garcia-Feijoo, J. Diagnostic capacity of SD-OCT segmented ganglion cell complex versus retinal nerve fiber layer analysis for congenital glaucoma. Eye 2018, 32, 1338–1344. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.; Chang, T.; Freedman, S. Definition, classification, differential diagnosis. In Childhood Glaucoma; Weinreb, R.N., Grajewski, A., Papadopoulos, M., Grigg, J., Freedman, S., Eds.; Kugler Publications: Amsterdam, The Netherlands, 2013; pp. 3–10. [Google Scholar]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Pilat, A.V.; Shah, S.; Sheth, V.; Purohit, R.; Proudlock, F.A.; Abbott, J.; Gottlob, I. Detection and characterisation of optic nerve and retinal changes in primary congenital glaucoma using hand-held optical coherence tomography. BMJ Open Ophthalmol. 2019, 4, e000194. [Google Scholar] [CrossRef] [PubMed]
- Schuman, J.S.; Hee, M.R.; Arya, A.V.; Pedut-Kloizman, T.; Puliafito, C.A.; Fujimoto, J.G.; Swanson, E.A. Optical coherence tomography: A new tool for glaucoma diagnosis. Curr. Opin. Ophthalmol. 1995, 6, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Perucho-González, L.; Martínez de la Casa, J.M.; Sáenz-Francés, F.; Morales-Fernandez, L.; Méndez-Hernández, C.D.; Sánchez-Jean, R.; García-Feijoó, J. Retinal nerve fiber layer thickness in children with primary congenital glaucoma measured by spectral domain optical coherence tomography. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2019, 23, 94.e1–94.e4. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Dastiridou, A.; Francis, B.A.; Tan, O.; Varma, R.; Greenfield, D.S.; Schuman, J.S.; Huang, D. Comparison of Glaucoma Progression Detection by Optical Coherence Tomography and Visual Field. Am. J. Ophthalmol. 2017, 184, 63–74. [Google Scholar] [CrossRef]
- Kendell, K.R.; Quigley, H.A.; Kerrigan, L.A.; Pease, M.E.; Quigley, E.N. Primary open-angle glaucoma is not associated with photoreceptor loss. Investig. Ophthalmol. Vis. Sci. 1995, 36, 200–205. [Google Scholar]
- Velten, I.M.; Korth, M.; Horn, F.K. The a-wave of the dark adapted electroretinogram in glaucomas: Are photoreceptors affected? Br. J. Ophthalmol. 2001, 85, 397–402. [Google Scholar] [CrossRef] [PubMed]
- Böhm, M.R.R.; Thomasen, H.; Parnitzke, F.; Steuhl, K.P. Clinical, morphological and molecular biological characteristics of the aging eye. Ophthalmologe 2017, 114, 98–107. [Google Scholar] [CrossRef] [PubMed]
- Nouri-Mahdavi, K.; Hoffman, D.; Tannenbaum, D.P.; Law, S.K.; Caprioli, J. Identifying early glaucoma with optical coherence tomography. Am. J. Ophthalmol. 2004, 137, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Michelessi, M.; Lucenteforte, E.; Oddone, F.; Brazzelli, M.; Parravano, M.; Franchi, S.; Ng, S.M.; Virgili, G. Optic Nerve Head and Fibre Layer Imaging for Diagnosing Glaucoma; John Wiley and Sons Ltd.: Hoboken, NJ, USA, 2015; Volume 2015. [Google Scholar]
- Hammel, N.; Belghith, A.; Weinreb, R.N.; Medeiros, F.A.; Mendoza, N.; Zangwill, L.M. Comparing the Rates of Retinal Nerve Fiber Layer and Ganglion Cell–Inner Plexiform Layer Loss in Healthy Eyes and in Glaucoma Eyes. Am. J. Ophthalmol. 2017, 178, 38–50. [Google Scholar] [CrossRef] [PubMed]
- Shoji, T.; Sato, H.; Ishida, M.; Takeuchi, M.; Chihara, E. Assessment of glaucomatous changes in subjects with high myopia using spectral domain optical coherence tomography. Investig. Ophthalmol. Vis. Sci. 2011, 52, 1098–1102. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Value | p-Value 1 | |
|---|---|---|---|
| Patients | (n) | 72 | |
| Gender | male:female% (n) | 55.6:44.4% (40:32) | |
| Diagnosis | glaucoma:healthy% (n) | 26.4:73.6% (19:53) | |
| Eye | right:left% (n) | 87.5:12.5% (63:9) | |
| Age | mean ± SD (y) | 11.9 ± 3.6 | |
| Glaucoma | 11.2 ± 3.5 | 0.33 | |
| Healthy | 12.2 ± 3.5 | ||
| Range | (y) | 5.5–17.9 | |
| ≤10 years | % (n) | 36.1% (26) | |
| >10 years | % (n) | 63.9% (46) | |
| BCVA | median (CL) (LogMar) | 0.0 (96.0%) | |
| IOP | mean ± SD (mm Hg) | 15.7 ± 4.8 | |
| Glaucoma | 18.7 ± 7.2 | 0.0007 | |
| Healthy | 14.5 ± 2.7 | ||
| ONH horizontal diameter | mean ± SD (mm) | 1.65 ± 0.24 | |
| Glaucoma | 1.55 ± 0.20 | 0.051 | |
| Healthy | 1.68 ± 0.25 | ||
| Linear CDR | median (CL) | 0.6 (96%) | |
| Glaucoma | 0.8 (98%) | 0.030 | |
| Healthy | 0.6 (97%) | ||
| Perimetry (MD) | mean ± SD (dB) | 2.7 ± 4.1 | |
| Glaucoma | 4.3 ± 5.5 | 0.131 | |
| Healthy | 2.4 ± 3.7 | ||
| Follow-up time | mean ± SD (m) | 20.0 ± 14.2 | |
| Diagnosis/Aetiology | n |
|---|---|
| Glaucoma patients | 19 |
| Primary congenital glaucoma (PCG) | 5 (26%) |
| Juvenile primary open angle glaucoma (JOAG) | 7 (37%) |
| Glaucoma associated with non-acquired ocular anomalies (GNAO) | 1 (5%) |
| Glaucoma associated with non-acquired systemic anomalies | 0 (0%) |
| Glaucoma associated with acquired conditions (GAC) | 6 (32%) |
| Glaucoma after cataract (GFC) | 4 (21%) |
| GAC others | 2 (11%) |
| pRNFL Sector Thickness | Glaucoma | Healthy | p-Value 1 | ||
|---|---|---|---|---|---|
| Mean ± SD | 95% CI | Mean ± SD | 95% CI | ||
| Average thickness | 82.8 ± 19.8 | 73.2–92.3 | 98.7 ± 6.93 | 96.8–100.6 | <0.0001 |
| Superior | 98.3 ± 35.1 | 81.4–115.2 | 122 ± 12.9 | 118.2–125.3 | <0.0001 |
| Temporal superior (TS) | 108 ± 38.6 | 89.1–126.3 | 138 ± 15.4 | 133.6–142.1 | <0.0001 |
| Nasal superior (NS) | 88.9 ± 34.3 | 72.4–105.4 | 106 ± 18.5 | 100.6–110.8 | 0.0097 |
| Nasal | 68.0 ± 18.3 | 59.2–76.4 | 75.0 ± 12.5 | 71.5–78.4 | 0.0717 |
| Inferior | 99.4 ± 28.0 | 86.0–112.9 | 128 ± 15.1 | 123.8–132.1 | <0.0001 |
| Nasal inferior (NI) | 87.6 ± 26.9 | 74.7–100.6 | 110 ± 22.5 | 104.2–116.6 | 0.0006 |
| Temporal inferior (TI) | 111 ± 34.9 | 94.4–128.1 | 146 ± 17.3 | 140.8–150.4 | <0.0001 |
| Temporal | 63.8 ± 15.6 | 56.3–71.4 | 70.8 ± 10.7 | 67.9–73.8 | 0.0342 |
| Macular Segment Thickness | Glaucoma | Healthy | p-Value 1 |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Ganglion cell layer (GCL) | |||
| Central (C0) | 20.8 ± 8.6 | 19.4 ± 7.9 | 0.62 |
| Inner superior (S1) | 44.1 ± 11.3 | 52.2 ± 6.2 | 0.0002 |
| Outer superior (S2) | 29.6 ± 5.8 | 33.9 ± 3.5 | 0.0002 |
| Inner nasal (N1) | 45.1 ± 12.9 | 52.9 ± 5.9 | 0.0006 |
| Outer nasal (N2) | 31.2 ± 7.8 | 36.4 ± 4.7 | 0.001 |
| Inner inferior (I1) | 42.8 ± 11.8 | 51.2 ± 7.0 | 0.0004 |
| Outer inferior (I2) | 28.6 ± 5.9 | 33.2 ± 4.2 | 0.0005 |
| Inner temporal (T1) | 40.5 ± 12.4 | 46.8 ± 6.0 | 0.0047 |
| Outer temporal (T2) | 29.3 ± 7.9 | 36.5 ± 4.6 | <0.0001 |
| Inner plexiform layer (IPL) | |||
| Central (C0) | 23.4 ± 7.1 | 23.2 ± 5.3 | 0.93 |
| Inner superior (S1) | 37.0 ± 6.7 | 40.7 ± 4.4 | 0.0089 |
| Outer superior (S2) | 25.2 ± 4.1 | 27.4 ± 3.0 | 0.015 |
| Inner nasal (N1) | 40.3 ± 6.1 | 42.3 ± 2.9 | 0.061 |
| Outer nasal (N2) | 26.1 ± 4.7 | 27.9 ± 3.3 | 0.079 |
| Inner inferior (I1) | 35.5 ± 8.4 | 40.1 ± 4.7 | 0.0046 |
| Outer inferior (I2) | 24.2 ± 4.3 | 26.4 ± 3.4 | 0.024 |
| Inner temporal (T1) | 36.9 ± 8.7 | 40.1 ± 4.1 | 0.040 |
| Outer temporal (T2) | 28.3 ± 5.7 | 31.7 ± 3.1 | 0.0019 |
| Retina | |||
| Central (C0) | 287.1 ± 31.5 | 281.3 ± 28.9 | 0.47 |
| Inner superior (S1) | 331.2 ± 25.9 | 343.3 ± 14.7 | 0.015 |
| Outer superior (S2) | 289.0 ± 21.1 | 301.4 ± 15.2 | 0.0078 |
| Inner nasal (N1) | 338.5 ± 20.1 | 346.5 ± 13.9 | 0.065 |
| Outer nasal (N2) | 305.6 ± 29.9 | 316.5 ± 17.1 | 0.060 |
| Inner inferior (I1) | 323.3 ± 26.8 | 339.5 ± 21.5 | 0.010 |
| Outer inferior (I2) | 277.6 ± 21.6 | 293.7 ± 18.2 | 0.0024 |
| Inner temporal (T1) | 318.4 ± 25.2 | 327.5 ± 13.8 | 0.057 |
| Outer temporal (T2) | 274.9 ± 18.0 | 288.2 ± 16.3 | 0.0041 |
| Sector/Subfield | Coefficient | 95% CI | OR | R2 | p-Value 1 | AUC | 95% CI |
|---|---|---|---|---|---|---|---|
| Peripapillary retinal nerve fibre layer (pRNFL) | |||||||
| Multivariate logistic regression | |||||||
| All sectors | 0.39 | <0.0001 | 0.83 | 0.71–0.96 | |||
| Univariate logistic regression | |||||||
| Superior | −0.12 | −0.20–−0.057 | 0.89 | 0.30 | 0.0011 | 0.75 | 0.60–0.90 |
| Temporal superior (TS) | −0.046 | −0.080–−0.020 | 0.96 | 0.21 | 0.0021 | 0.67 | 0.51–0.83 |
| Nasal superior (NS) | −0.047 | −0.080–−0.023 | 0.95 | 0.26 | 0.0010 | 0.72 | 0.57–0.88 |
| Nasal | −0.029 | −0.055–−0.0066 | 0.97 | 0.11 | 0.0169 | 0.61 | 0.44–0.78 |
| Inferior | −0.035 | −0.076–0.0025 | 0.97 | 0.054 | 0.077 | 0.63 | 0.47–0.79 |
| Nasal inferior (NI) | −0.076 | −0.13–−0.039 | 0.93 | 0.33 | 0.0005 | 0.81 | 0.69–0.93 |
| Temporal superior (TI) | −0.042 | −0.071–−0.017 | 0.96 | 0.18 | 0.0023 | 0.73 | 0.59–0.88 |
| Temporal | −0.067 | −0.11–−0.034 | 0.94 | 0.33 | 0.0007 | 0.81 | 0.69–0.93 |
| Superior | −0.053 | −0.11–−0.0054 | 0.95 | 0.079 | 0.0429 | 0.64 | 0.48–0.80 |
| mRNFL-GCL-IPL | |||||||
| multivariate logistic regression | |||||||
| Superior and inferior subfields (S1, S2, I1, I2) | 0.42 | <0.0001 | 0.85 | 0.73–0.97 | |||
| Macular retinal nerve fibre layer (mRNFL) | |||||||
| Univariate logistic regression | |||||||
| Inner superior (S1) | −0.027 | −0.14–0.016 | 0.97 | 0.010 | 0.31 | 0.53 | 0.36–0.70 |
| Outer superior (S2) | −0.11 | −0.20–−0.028 | 0.90 | 0.13 | 0.0048 | 0.64 | 0.47–0.82 |
| Inner inferior (I1) | −0.028 | −0.14–0.011 | 0.91 | 0.013 | 0.25 | 0.54 | 0.37–0.70 |
| Outer inferior (I2) | −0.090 | −017–−0.027 | 0.91 | 0.14 | 0.0030 | 0.68 | 0.52–0.84 |
| Ganglion cell layer (GCL) | |||||||
| Univariate logistic regression | |||||||
| Inner superior (S1) | −0.11 | −0.20–−0.045 | 0.89 | 0.18 | 0.0006 | 0.74 | 0.60–0.89 |
| Outer superior (S2) | −0.22 | −0.37–−0.091 | 0.8 | 0.19 | 0.0004 | 0.71 | 0.57–0.86 |
| Inner inferior (I1) | −0.098 | −0.17–−0.039 | 0.91 | 0.17 | 0.0009 | 0.75 | 0.60–0.89 |
| Outer inferior (I2) | −0.2 | −0.35–−0.084 | 0.81 | 0.19 | 0.0005 | 0.76 | 0.62–0.89 |
| Inner plexiform layer (IPL) | |||||||
| Univariate logistic regression | |||||||
| Inner superior (S1) | −0.12 | −0.25–−0.026 | 0.88 | 0.096 | 0.0126 | 0.66 | 0.51–0.80 |
| Outer superior (S2) | −0.19 | −0.37–−0.033 | 0.83 | 0.086 | 0.0173 | 0.67 | 0.52–0.83 |
| Inner inferior (I1) | −0.11 | −0.22–−0.030 | 0.89 | 0.11 | 0.0072 | 0.67 | 0.50–0.84 |
| Outer inferior (I2) | −0.17 | −0.34–−0.022 | 0.84 | 0.08 | 0.0233 | 0.68 | 0.53–0.83 |
| Sector/Subfield | Sensitivity at | ||
|---|---|---|---|
| Specificity ≥ 80% | Specificity ≥ 90% | Specificity ≥ 95% | |
| Peripapillary retinal nerve fibre layer (pRNFL) | |||
| Multivariate logistic regression | |||
| All sectors | 74% | 74% | 63% |
| Univariate logistic regression | |||
| Average | 63% | 53% | 42% |
| Superior | 53% | 42% | 42% |
| Inferior | 68% | 58% | 42% |
| mRNFL–GCL–IPL | |||
| Multivariate logistic regression | |||
| Superior and inferior subfields (S1, S2, I1, I2) | 74% | 68% | 63% |
| Macular retinal nerve fibre layer (mRNFL) | |||
| univariate logistic regression | |||
| Inner superior (S1) | 42% | 21% | 11% |
| Outer superior (S2) | 53% | 47% | 42% |
| Inner inferior (I1) | 32% | 21% | 11% |
| Outer inferior (I2) | 47% | 37% | 26% |
| Ganglion cell layer (GCL) | |||
| univariate logistic regression | |||
| Inner superior (S1) | 63% | 32% | 32% |
| Outer superior (S2) | 47% | 42% | 42% |
| Inner inferior (I1) | 63% | 42% | 26% |
| Outer inferior (I2) | 58% | 47% | 42% |
| Inner plexiform layer (IPL) | |||
| univariate logistic regression | |||
| Inner superior (S1) | 32% | 26% | 26% |
| Outer superior (S2) | 58% | 37% | 16% |
| Inner inferior (I1) | 42% | 37% | 32% |
| Outer inferior (I2) | 47% | 37% | 16% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lever, M.; Halfwassen, C.; Unterlauft, J.D.; Bechrakis, N.E.; Manthey, A.; Böhm, M.R.R. The Paediatric Glaucoma Diagnostic Ability of Optical Coherence Tomography: A Comparison of Macular Segmentation and Peripapillary Retinal Nerve Fibre Layer Thickness. Biology 2021, 10, 260. https://doi.org/10.3390/biology10040260
Lever M, Halfwassen C, Unterlauft JD, Bechrakis NE, Manthey A, Böhm MRR. The Paediatric Glaucoma Diagnostic Ability of Optical Coherence Tomography: A Comparison of Macular Segmentation and Peripapillary Retinal Nerve Fibre Layer Thickness. Biology. 2021; 10(4):260. https://doi.org/10.3390/biology10040260
Chicago/Turabian StyleLever, Mael, Christian Halfwassen, Jan Darius Unterlauft, Nikolaos E. Bechrakis, Anke Manthey, and Michael R. R. Böhm. 2021. "The Paediatric Glaucoma Diagnostic Ability of Optical Coherence Tomography: A Comparison of Macular Segmentation and Peripapillary Retinal Nerve Fibre Layer Thickness" Biology 10, no. 4: 260. https://doi.org/10.3390/biology10040260
APA StyleLever, M., Halfwassen, C., Unterlauft, J. D., Bechrakis, N. E., Manthey, A., & Böhm, M. R. R. (2021). The Paediatric Glaucoma Diagnostic Ability of Optical Coherence Tomography: A Comparison of Macular Segmentation and Peripapillary Retinal Nerve Fibre Layer Thickness. Biology, 10(4), 260. https://doi.org/10.3390/biology10040260








