Cognitive Performance and Its Associations with Dental Caries: Results from the Dental, Oral, Medical Epidemiological (DOME) Records-Based Nationwide Study
Abstract
Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Data Source
2.2. Study Population
2.3. Inclusion and Exclusion Criteria
2.4. Definition of Variables
2.4.1. Dependent Variables: Dental Parameters
- (1)
- The number of teeth in need of root canal treatments (RCT): (a) one RCT (D3310), (b) two RCT (D3320), (c) three or more RCT (D3330). The present study included the number of teeth in need of RCTs, which is the sum of these codes [18].
- (2)
- The number of teeth in need of extractions: extraction erupted tooth or exposed root (D7140) [18].
2.4.2. Independent Variables
Assessment of the General Intelligence Score (GIS)
General Intelligence Score (GIS)
- Arithmetic-R: assessment of mathematical reasoning, concentration, and concept manipulation.
- Otis-R: measurement of the understanding and execution of verbal instructions.
- Similarities-R: assessment of word analogies, verbal abstraction, and categorization.
- Raven’s Progressive Matrices-R: measurement of non-verbal abstract reasoning, and problem-solving abilities through visual–spatial shape analogies.
Socio-Demographic Variables
Health-Related Habits Variables
2.5. Statistical Analysis
3. Results
3.1. Socio-Demographic Characteristics and Health-Related Habits of the Study Population across the Four GIS Categories
3.2. The Dental Status of the Study Population across the Four General Intelligence score (GIS) Categories
4. Discussion
Strength and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, K.; Cascella, M.; Marwaha, R. Intellectual Disability; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Schaefer, J.D.; Caspi, A.; Belsky, D.W.; Harrington, H.; Houts, R.; Israel, S.; Levine, M.E.; Sugden, K.; Williams, B.; Poulton, R.; et al. Early-Life Intelligence Predicts Midlife Biological Age. J. Gerontol. B Psychol. Sci. Soc. Sci. 2016, 71, 968–977. [Google Scholar] [CrossRef]
- Twig, G.; Gluzman, I.; Tirosh, A.; Gerstein, H.C.; Yaniv, G.; Afek, A.; Derazne, E.; Tzur, D.; Karasik, A.; Gordon, B.; et al. Cognitive function and the risk for diabetes among young men. Diabetes Care. 2014, 37, 2982–2988. [Google Scholar] [CrossRef] [PubMed]
- Wallin, A.S.; Allebeck, P.; Gustafsson, J.E.; Hemmingsson, T. Childhood IQ and mortality during 53 years’ follow-up of Swedish men and women. J. Epidemiol. Community Health 2018, 72, 926–932. [Google Scholar] [CrossRef]
- Twig, G.; Tirosh, A.; Derazne, E.; Haklai, Z.; Goldberger, N.; Afek, A.; Gerstein, H.C.; Kark, J.D.; Cukierman-Yaffe, T. Cognitive function in adolescence and the risk for premature diabetes and cardiovascular mortality in adulthood. Cardiovasc. Diabetol. 2018, 17, 154. [Google Scholar] [CrossRef]
- Der, G.; Batty, G.D.; Deary, I.J. The association between IQ in adolescence and a range of health outcomes at 40 in the 1979 US National Longitudinal Study of Youth. Intelligence 2009, 37, 573–580. [Google Scholar] [CrossRef]
- Navit, S.; Malhotra, G.; Jashina Singh, V.N.; Anshul, P.N. Interrelationship of intelligence quotient with caries and gingivitis. J. Int. Oral Health 2014, 6, 56–62. [Google Scholar]
- Dhanu, G.; Havale, R.; Shrutha, S.P.; Quazi, N.; Shafna, T.P.; Ahemd, A. Assessment of Intelligence Quotient using Raven’s Coloured Progressive Matrices among school children of Hyderabad Karnataka region and its correlation with prevalence of dental caries. J. Indian Soc. Pedod. Prev. Dent. 2019, 37, 25–30. [Google Scholar] [CrossRef]
- Thomson, W.M.; Broadbent, J.M.; Caspi, A.; Poulton, R.; Moffitt, T.E. Childhood IQ predicts age-38 oral disease experience and service-use. Community Dent. Oral Epidemiol. 2019, 47, 252–258. [Google Scholar] [CrossRef]
- Stewart, R.; Hirani, V. Dental health and cognitive impairment in an English national survey population. J. Am. Geriatr. Soc. 2007, 55, 1410–1414. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Clark, J.J.; Chen, H.; Naorungroj, S. Cognitive impairment, oral self-care function and dental caries severity in community-dwelling older adults. Gerodontology 2015, 32, 53–61. [Google Scholar] [CrossRef]
- Chen, X.; Xie, X.J.; Yu, L. The pathway from cognitive impairment to caries in older adults: A conceptual model. J. Am. Dent. Assoc. 2018, 149, 967–975. [Google Scholar] [CrossRef]
- Egashira, R.; Mizutani, S.; Yamaguchi, M.; Kato, T.; Umezaki, Y.; Oku, S.; Tamai, K.; Obata, T.; Naito, T. Low Tongue Strength and the Number of Teeth Present Are Associated with Cognitive Decline in Older Japanese Dental Outpatients: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 8700. [Google Scholar] [CrossRef]
- Egashira, R.; Umezaki, Y.; Mizutani, S.; Obata, T.; Yamaguchi, M.; Tamai, K.; Yoshida, M.; Makino, M.; Naito, T. Relationship between cerebral atrophy and number of present teeth in elderly individuals with cognitive decline. Exp. Gerontol. 2021, 144, 111189. [Google Scholar] [CrossRef]
- Delwel, S.; Binnekade, T.T.; Perez, R.S.; Hertogh, C.M.; Scherder, E.J.; Lobbezoo, F. Oral health and orofacial pain in older people with dementia: A systematic review with focus on dental hard tissues. Clin. Oral Investig. 2017, 21, 17–32. [Google Scholar] [CrossRef]
- Nadim, R.; Tang, J.; Dilmohamed, A.; Yuan, S.; Wu, C.; Bakre, A.T.; Partridge, M.; Ni, J.; Copeland, J.R.; Anstey, K.; et al. Influence of periodontal disease on risk of dementia: A systematic literature review and a meta-analysis. Eur. J. Epidemiol. 2020, 35, 821–833. [Google Scholar] [CrossRef]
- Sorensen, C.E.; Hansen, N.L.; Mortensen, E.L.; Lauritzen, M.; Osler, M.; Pedersen, A.M.L. Hyposalivation and Poor Dental Health Status Are Potential Correlates of Age-Related Cognitive Decline in Late Midlife in Danish Men. Front. Aging Neurosci. 2018, 10, 10. [Google Scholar] [CrossRef]
- Almoznino, G.; Kedem, R.; Turgeman, R.; Bader, T.; Yavnai, N.; Zur, D.; Shay, B. The Dental, Oral, Medical Epidemiological (DOME) Study: Protocol and Study Methods. Methods Inf. Med. 2020, 59, 119–130. [Google Scholar]
- Almoznino, G.; Baruch, O.K.; Kedem, R.; Protter, N.E.; Shay, B.; Yavnai, N.; Zur, D.; Mijiritsky, E.; Abramovitz, I. SOS Teeth: First Priority Teeth with Advanced Caries and Its Associations with Metabolic Syndrome among a National Representative Sample of Young and Middle-Aged Adults. J. Clin. Med. 2020, 9, 3170. [Google Scholar] [CrossRef]
- Almoznino, G.; Abramovitz, I.; Kessler Baruch, O.; Kedem, R.; Protter, N.E.; Levine, J.; Bader, T.; Yavnai, N.; Zur, D.; Mijiritsky, E.; et al. SOS Teeth: Age and Sex Differences in the Prevalence of First Priority Teeth among a National Representative Sample of Young and Middle-Aged Adults. Int. J. Environ. Res. Public Health 2020, 17, 4847. [Google Scholar] [CrossRef]
- Almoznino, G.; Zini, A.; Kedem, R.; Protter, N.E.; Zur, D.; Abramovitz, I. Hypertension and Its Associations with Dental Status: Data from the Dental, Oral, Medical Epidemiological (DOME) Nationwide Records-Based Study. J. Clin. Med. 2021, 10, 176. [Google Scholar] [CrossRef]
- ADA. ADA (American Dental Association) Guide to Dental Procedures Reported with Area of the Oral Cavity or Tooth Anatomy (or Both); Version 1; ADA: New York, NY, USA, 2018. [Google Scholar]
- Shelef, L.; Laur, L.; Fruchter, E. Characteristics of the suicidal soldier in the Israeli Defense Force-a review of literature. Disaster Mil. Med. 2015, 1, 10. [Google Scholar] [CrossRef]
- Levy, D.H.; Livny, A.; Sgan-Cohen, H.; Yavnai, N. The association between caries related treatment needs and socio-demographic variables among young Israeli adults: A record based cross sectional study. Isr. J. Health Policy Res. 2018, 7, 24. [Google Scholar] [CrossRef]
- Davidson, M.; Reichenberg, A.; Rabinowitz, J.; Weiser, M.; Kaplan, Z.; Mark, M. Behavioral and intellectual markers for schizophrenia in apparently healthy male adolescents. Am. J. Psychiatry 1999, 156, 1328–1335. [Google Scholar]
- Meydan, C.; Afek, A.; Derazne, E.; Tzur, D.; Twig, G.; Gordon, B.; Shamiss, A. Population-based trends in overweight and obesity: A comparative study of 2,148,342 Israeli male and female adolescents born 1950-1993. Pediatr. Obes. 2013, 8, 98–111. [Google Scholar] [CrossRef] [PubMed]
- Twig, G.; Livneh, A.; Vivante, A.; Afek, A.; Shamiss, A.; Derazne, E.; Tzur, D.; Ben-Zvi, I.; Tirosh, A.; Barchana, M.; et al. Mortality risk factors associated with familial Mediterranean fever among a cohort of 1.25 million adolescents.5. Ann. Rheum Dis. 2014, 73, 704–709. [Google Scholar] [CrossRef]
- Reichenberg, A.; Weiser, M.; Rabinowitz, J.; Caspi, A.; Schmeidler, J.; Mark, M.; Kaplan, Z.; Davidson, M. A population-based cohort study of premorbid intellectual, language, and behavioral functioning in patients with schizophrenia, schizoaffective disorder, and nonpsychotic bipolar disorder. Am. J. Psychiatry. 2002, 159, 2027–2035. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Weiser, M.; Reichenberg, A.; Rabinowitz, J.; Nahon, D.; Kravitz, E.; Lubin, G.; Knobler, H.; Davidson, M.; Noy, S. Impaired reading comprehension and mathematical abilities in male adolescents with average or above general intellectual abilities are associated with comorbid and future psychopathology. J. Nerv. Ment Dis. 2007, 195, 883–890. [Google Scholar] [CrossRef] [PubMed]
- Stewart, R.; Sabbah, W.; Tsakos, G.; D’Aiuto, F.; Watt, R.G. Oral health and cognitive function in the Third National Health and Nutrition Examination Survey (NHANES III). Psychosom. Med. 2008, 70, 936–941. [Google Scholar] [CrossRef]
- Whalley, L.J.; Deary, I.J. Longitudinal cohort study of childhood IQ and survival up to age 76. BMJ. 2001, 322, 819. [Google Scholar] [CrossRef]
- Gillcrist, J.A.; Brumley, D.E.; Blackford, J.U. Community socioeconomic status and children’s dental health. J. Am. Dent. Assoc. 2001, 132, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Reisine, S.T.; Psoter, W. Socioeconomic status and selected behavioral determinants as risk factors for dental caries. J. Dent. Educ. 2001, 65, 1009–1016. [Google Scholar] [CrossRef]
- Jamieson, L.M.; Thomson, W.M. Adult oral health inequalities described using area-based and household-based socioeconomic status measures. J. Public Health Dent. 2006, 66, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Holst, D.; Schuller, A.A.; Aleksejuniene, J.; Eriksen, H.M. Caries in populations--a theoretical, causal approach. Eur. J. Oral Sci. 2001, 109, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Ueno, M.; Ohara, S.; Inoue, M.; Tsugane, S.; Kawaguchi, Y. Association between education level and dentition status in Japanese adults: Japan public health center-based oral health study. Community Dent. Oral Epidemiol. 2012, 40, 481–487. [Google Scholar] [CrossRef]
- Mohammadbeigi, A.; Arsangjang, S.; Mohammadsalehi, N.; Anbari, Z.; Ghaderi, E. Education-related Inequity in Access and Utilization of Oral Health Care in Iran. J. Family Med. Prim. Care. 2015, 4, 35–38. [Google Scholar]
- Shetty, N.; Mala, K.; Suprabha, B.S.; Shenoy, R. Association of level of education and utilization of restorative dental care among rural women in India: Cross-sectional study. Indian J. Dent. Res. 2017, 28, 642–645. [Google Scholar] [CrossRef]
- Moynihan, P.J.; Kelly, S.A. Effect on caries of restricting sugars intake: Systematic review to inform WHO guidelines. J. Dent. Res. 2014, 93, 8–18. [Google Scholar] [CrossRef]
- Wraw, C.; Der, G.; Gale, C.R.; Deary, I.J. Intelligence in youth and health behaviours in middle age. Intelligence 2018, 69, 71–86. [Google Scholar] [CrossRef]
- Yamamoto, T.; Kondo, K.; Misawa, J.; Hirai, H.; Nakade, M.; Aida, J.; Kondo, N.; Kawachi, I.; Hirata, Y. Dental status and incident falls among older Japanese: A prospective cohort study. BMJ Open 2012, 2, e001262. [Google Scholar] [CrossRef]
- Saito, S.; Ohi, T.; Murakami, T.; Komiyama, T.; Miyoshi, Y.; Endo, K.; Satoh, M.; Asayama, K.; Inoue, R.; Kikuya, M.; et al. Association between tooth loss and cognitive impairment in community-dwelling older Japanese adults: A 4-year prospective cohort study from the Ohasama study. BMC Oral Health 2018, 18, 142. [Google Scholar] [CrossRef] [PubMed]
- Delwel, S.; Scherder, E.J.A.; Perez, R.; Hertogh, C.; Maier, A.B.; Lobbezoo, F. Oral function of older people with mild cognitive impairment or dementia. J. Oral Rehabil. 2018, 45, 990–997. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, Y.; Arai, H.; Hirano, H.; Morishita, S.; Ohara, Y.; Edahiro, A.; Murakami, M.; Shimada, H.; Kikutani, T.; Suzuki, T. Oral function as an indexing parameter for mild cognitive impairment in older adults. Geriatr. Gerontol. Int. 2018, 18, 790–798. [Google Scholar] [CrossRef]
- Iwasaki, M.; Kimura, Y.; Ogawa, H.; Yamaga, T.; Ansai, T.; Wada, T.; Sakamoto, R.; Ishimoto, Y.; Fujisawa, M.; Okumiya, K.; et al. Periodontitis, periodontal inflammation, and mild cognitive impairment: A 5-year cohort study. J. Periodontal. Res. 2019, 54, 233–240. [Google Scholar] [CrossRef] [PubMed]
| Parameter | GIS Categories | Total (%) or Mean ± SD | p Value | ||||
|---|---|---|---|---|---|---|---|
| 1–3 | 4–5 | 6–7 | 8–9 | ||||
| Number (%) | 19,693 (14.9) | 44,717 (33.9) | 47,972 (36.4) | 19,545 (14.8) | 131,927 (100) | ||
| Age (years) | 21.1 ± 5.1 | 21.5 ±6.0 | 22.1 ±6.1 | 22.6 ±6.1 | 21.8 ±5.9 | <0.001 * | |
| Sex | Men | 15,309 (77.7) | 31,774 (71.1) | 35,795 (74.6) | 16,107 (82.4) | 98,985 (75.0) | <0.001 ˄ |
| Woman | 4384 (22.3) | 12,943 (28.9) | 12,177 (25.4) | 3438 (17.6) | 32,942 (25.0) | ||
| Education | High school | 18,581 (94.6) | 39,353 (88.1) | 39,497 (82.4) | 14,344 (73.5) | 111,775 (84.8) | <0.001 ˅ |
| Technician | 882 (4.5) | 3415 (7.6) | 2428 (5.1) | 605 (3.1) | 7330 (5.6) | ||
| Academics | 182 (0.9) | 1906 (4.3) | 6011 (12.5) | 4571 (23.4) | 12,670 (9.6) | ||
| SES | Low | 1708 (8.7) | 2127 (4.8) | 1449 (3.1) | 357 (1.9) | 5641 (4.3) | <0.001 ˅ |
| Medium | 12,392 (63.4) | 25,450 (57.3) | 22,575 (47.7) | 7886 (41. 2) | 68,303 (52.4) | ||
| High | 5454 (27.9) | 16,834 (37.9) | 23,329 (49.3) | 10,910 (57.0) | 56,527 (43.3) | ||
| Locality of residence | Urban Jewish | 18,076 (92.0) | 39,020 (87.5) | 39,934 (83.7) | 15,933 (82.2) | 112,963 (86.0) | <0.001 ˅ |
| Urban non-Jewish | 1569 (8.0) | 5499 (12.9) | 7495 (15.7) | 3272 (16.9) | 17,835 (13.6) | ||
| Rural | 12 (0.1) | 91 (0.2) | 301 (0.6) | 178 (0.9) | 582 (0.4) | ||
| Birth country | Western Europe | 245 (1.2) | 760 (1.7) | 1075 (2.2) | 592 (3.0) | 2672 (2.0) | <0.001 ˅ |
| East Europe | 1086 (5.5) | 2755 (6.2) | 2780 (5.8) | 1220 (6.2) | 7841 (5.9) | ||
| FSU | 374 (1.9) | 646 (1.4) | 504 (1.1) | 183 (0.9) | 1707 (0.3) | ||
| Asia | 52 (0.3) | 98 (0.2) | 62 (0.1) | 24 (0.1) | 236 (0.2) | ||
| East Asia | 32 (0.2) | 58 (0.1) | 44 (0.1) | 19 (0.1) | 153 (0.1) | ||
| Ethiopia | 1429 (7.3) | 611 (1.4) | 106 (0.2) | 8 (0.0) | 2154 (1.6) | ||
| Africa | 40 (0.2) | 104 (0.2) | 125 (0.3) | 50 (0.3) | 319 (0.2) | ||
| North America | 124 (0.6) | 629 (1.4) | 1255 (2.6) | 835 (4.3) | 2843 (2.2) | ||
| South America | 133 (0.7) | 335 (0.7) | 323 (0.7) | 165 (0.8) | 956 (0.7) | ||
| Oceania | 3 (0.0) | 17(0.0) | 45 (0.1) | 43 (0.2) | 108 (0.1) | ||
| Israel | 16,174 (82.1) | 38,698 (86.6) | 41,641 (86.8) | 16,396 (83.9) | 112,909 (85.6) | ||
| Smoking | No | 18,507 (94.0) | 42,160 (94.3) | 45,641 (95.1) | 18,883 (96.6) | 125,191 (94.9) | <0.001 ˄ |
| Yes | 1186 (6.0) | 2557 (5.7) | 2332 (4.9) | 662 (3.4) | 6736 (5.1) | ||
| Brushing teeth once a day | No | 3307 (35.3) | 6316 (31.9) | 5862 (29.3) | 2159 (27.1) | 17,644 (30.9) | <0.001 ˄ |
| Yes | 6052 (64.7) | 134,63 (68.1) | 14,171 (70.7) | 5810 (72.9) | 39,496 (69.1) | ||
| Cariogenic diet | No | 3083 (43.4) | 7326 (47.6) | 8046 (50.8) | 3448 (53.7) | 21,903 (48.9) | <0.001 ˄ |
| Yes | 4024 (56.6) | 8049 (52.4) | 7808 (49.2) | 2978 (46.3) | 22,859 (51.1) | ||
| Sweetened beverages | No | 4593 (49.1) | 10,946 (55.3) | 12,080 (60.3) | 5150 (64.6) | 32,769 (57.3) | <0.001 ˄ |
| Yes | 4766 (50.9) | 8833 (44.7) | 7953 (39.7) | 2819 (35.4) | 24,371 (42.7) | ||
| Parameter | GIS Categories (Mean ± SD or (%)) | Total Mean ± SD or (%) | p Value * | ||||
|---|---|---|---|---|---|---|---|
| 1–3 | 4–5 | 6–7 | 8–9 | ||||
| Decayed teeth | Mean ± SD | 3.14 ± 3.58 | 2.25 ± 2.87 | 1.75 ± 2.43 | 1.45 ± 2.19 | 2.09 ± 2.81 | <0.001 * |
| OR & 95% CI | 5.36 (5.06–5.68) | 2.19 (2.08–2.30) | 1.34 (1.27–1.41) | 1 | |||
| Missing teeth | Mean ± SD | 0.63 ± 1.24 | 0.58 ± 1.25 | 0.57 ± 1.38 | 0.51 ± 1.17 | 0.58 ± 1.29 | <0.001 * |
| OR & 95% CI | 1.65 (1.61–1.70) | 1.07 (1.04–1.11) | 1.06 (1.03–1.10) | 1 | |||
| Number of teeth in need of root canal treatment | Mean ± SD | 0.18 ± 0.60 | 0.09 ± 0.37 | 0.05 ± 0.28 | 0.04 ± 0.25 | 0.08 ± 0.37 | <0.001 * |
| OR & 95% CI | 1.15 (1.14–1.16) | 1.05 (1.04–1.05) | 1.01 (1.00–1.01) | 1 | |||
| Number of teeth in need of extractions | Mean ± SD | 0.22 ± 0.69 | 0.14 ± 0.52 | 0.11 ± 0.45 | 0.11 ± 0.45 | 0.14 ± 0.52 | <0.001 * |
| OR & 95% CI | 1.12 (1.11–1.13) | 1.03 (1.02–1.04) | 1.00 (0.99–1.01) | 1 | |||
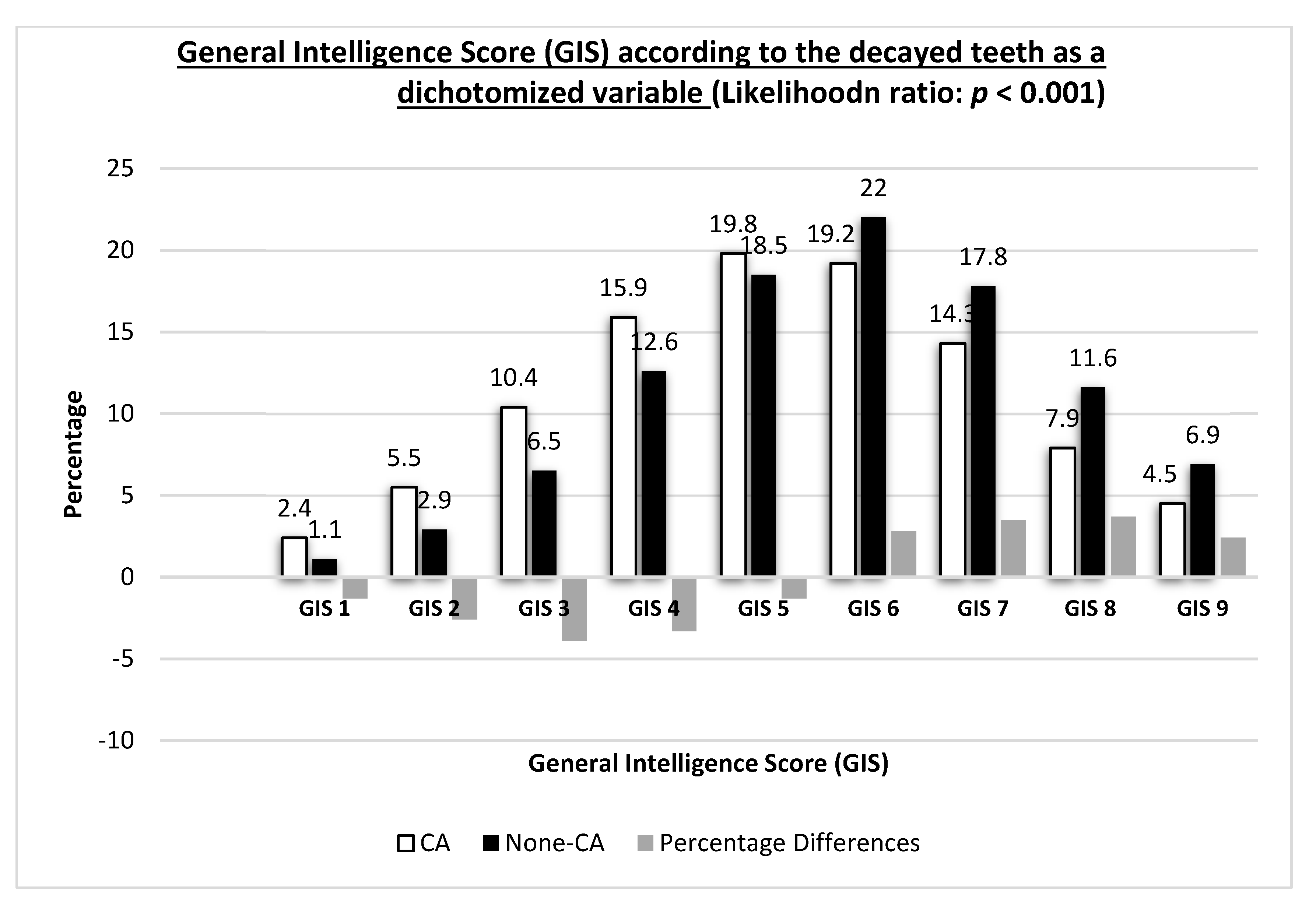
| Decayed teeth as a dichotomized variable | CA | 13,811 (76.0) | 26,844 (67.5) | 25,188 (60.4) | 9284 (54.7) | 75,127 (64.4) | <0.001 ** |
| None-CA | 4361 (24.0) | 12,936 (32.5) | 16,542 (39.6) | 7687 (45.3) | 41,526 (35.6) | ||
| Variable | GIS Categories | |||
|---|---|---|---|---|
| 1–3 | 4–5 | 6–7 | 8–9 | |
| Model 1-unadjusted decayed teeth vs. GIS categories | ||||
| OR and 95% CI | 5.36 (5.06–5.68) | 2.19 (2.08–2.30) | 1.34 (1.27–1.41) | 1 |
| p value | <0.001 | <0.001 | <0.001 | |
| Model 2-Model 1 adjusted for age | ||||
| OR and 95% CI | 5.27 (4.97–5.58) | 2.22 (2.11–2.33) | 1.34 (1.29–1.42) | 1 |
| p value | <0.001 | <0.001 | <0.001 | |
| Model 3-adjusted for age and sex | ||||
| OR and 95% CI | 5.23 (4.93–5.54) | 2.15 (2.05–2.26) | 1.33 (1.26–1.39) | 1 |
| p value | <0.001 | <0.001 | <0.001 | |
| Model 4-adjusted for age, sex and education | ||||
| OR and 95% CI | 5.11 (4.81–5.42) | 2.18 (2.07–2.29) | 1.33 (1.27–1.41) | 1 |
| p value | <0.001 | <0.001 | <0.001 | |
| Model 5-adjusted for age, sex and education and SES | ||||
| OR and 95% CI | 4.25 (4.00–4.52) | 1.96 (1.86–2.07) | 1.28 (1.21–1.34) | 1 |
| p value | <0.001 | <0.001 | <0.001 | |
| Model 6-adjusted for age, sex and education, SES, and locality | ||||
| OR and 95% CI | 4.12 (3.88–4.38) | 1.93 (1.83–2.03) | 1.27 (1.21–1.34) | 1 |
| p value | <0.001 | <0.001 | <0.001 | |
| Model 7-adjusted for age, sex and education, SES, locality, and birth country | ||||
| OR and 95% CI | 4.16 (3.91–4.43) | 1.93 (1.83–2.03) | 1.27 (1.21–1.34) | 1 |
| p value | <0.001 | <0.001 | <0.001 | |
| Model 8-adjusted for age, sex and education, SES, locality, birth country, and smoking | ||||
| OR and 95% CI | 4.13 (3.89–4.39) | 1.92 (1.82–2.02) | 1.27 (1.21–1.33) | 1 |
| p value | <0.001 | <0.001 | <0.001 | |
| Model 9-adjusted for age, sex and education, SES, locality, birth country, smoking, and teeth brushing | ||||
| OR and 95% CI | 4.14 (3.73–4.58) | 1.86 (1.70–2.03) | 1.22 (1.12–1.33) | 1 |
| p value | <0.001 | <0.001 | <0.001 | |
| Model 10-adjusted for age, sex and education, SES and locality, birth country, smoking, teeth brushing, and cariogenic diet | ||||
| OR and 95% CI | 4.02 (3.63–4.46) | 1.82 (1.67–1.99) | 1.21 (1.11–1.32) | 1 |
| p value | <0.001 | <0.001 | <0.001 | |
| Model 11-adjusted for age, sex and education, SES and locality, birth country, smoking, teeth brushing, cariogenic diet, and sweetened beverages | ||||
| OR and 95% CI | 3.75 (3.38–4.16) | 1.75 (1.60–1.91) | 1.19 (1.09–1.29) | 1 |
| p value | <0.001 | <0.001 | <0.001 | |
| Parameter | B | Std. Error | p Value | Exp(B) and 95% Wald Confidence Interval for | Collinearity Statistics | |
|---|---|---|---|---|---|---|
| Tolerance | VIF | |||||
| (Intercept) | 1.88 | 0.16 | <0.001 | 6.59 (4.79–9.06) | ||
| GIS 1–3 vs. GIS 8–9 | 1.32 | 0.05 | <0.001 | 3.75 (3.38–4.16) | 0.74 | 1.34 |
| GIS 4–5 vs. GIS 8–9 | 0.56 | 0.04 | <0.001 | 1.75 (1.60–1.91) | 0.74 | 1.34 |
| GIS 6–7 vs. GIS 8–9 | 0.17 | 0.04 | <0.001 | 1.19 (1.09–1.29) | 0.80 | 1.24 |
| Age | −0.009 | 0.003 | 0.021 | 0.99 (0.98–0.99) | 0.38 | 2.39 |
| Sex: Male vs. female | 0.17 | 0.03 | <0.001 | 1.19 (1.12–1.26) | 0.94 | 1.06 |
| Education: high school vs. academic | 0.15 | 0.06 | 0.460 | 1.05 (0.92–1.20) | 0.69 | 1.43 |
| Education: technicians vs. academic | 0.37 | 0.07 | <0.001 | 1.44 (1.25–1.69) | 0.48 | 2.05 |
| SES: low vs. high | 1.35 | 0.07 | <0.001 | 3.86 (3.36–4.44) | 0.95 | 1.05 |
| SES: medium vs. high | 0.36 | 0.02 | <0.001 | 1.43 (1.36–1.52) | 0.92 | 1.07 |
| Locality: Urban non-Jewish vs. urban Jewish | −0.24 | 0.04 | <0.001 | 0.78 (0.72–0.85) | 0.97 | 1.02 |
| Locality: Rural vs. urban Jewish | 0.53 | 0.32 | 0.106 | 1.70 (0.89–3.23) | 0.98 | 1.01 |
| Birth country Western Europe vs. native Israeli | 0.56 | 0.05 | <0.001 | 1.76 (1.59–1.93) | 0.98 | 1.01 |
| Birth country East Europe vs. native Israeli | 1.04 | 0.11 | <0.001 | 2.84 (2.28–3.55) | 0.98 | 1.01 |
| Birth country Asia vs. native Israeli | 0.21 | 0.22 | 0.350 | 1.23 (0.79–1.92) | 0.99 | 1.002 |
| Birth country Ethiopia vs. native Israeli | −0.22 | 0.11 | 0.040 | 0.80 (0.64–0.98) | 0.96 | 1.04 |
| Birth country Africa vs. native Israeli | −0.19 | 0.28 | 0.946 | 0.98 (0.56–1.71) | 0.99 | 1.001 |
| Birth country North America vs. native Israeli | −0.35 | 0.10 | <0.001 | 0.70 (0.57–0.85) | 0.99 | 1.01 |
| Birth country South America vs. native Israeli | −0.33 | 0.16 | 0.837 | 0.96 (0.70–1.32) | 0.99 | 1.002 |
| Smoking | 0.026 | 0.07 | 0.704 | 1.02 (0.89–1.17) | 0.79 | 1.25 |
| Brushing teeth less than once a day | 0.52 | 0.04 | <0.001 | 1.68 (1.55–1.82) | 0.98 | 1.01 |
| Cariogenic diet | 0.17 | 0.03 | <0.001 | 1.18 (1.11–1.26) | 0.72 | 1.37 |
| Sweetened beverages | 0.45 | 0.03 | <0.001 | 1.009 (1.001–1.016) | 0.71 | 1.40 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abramovitz, I.; Zini, A.; Atzmoni, M.; Kedem, R.; Zur, D.; Protter, N.E.; Almoznino, G. Cognitive Performance and Its Associations with Dental Caries: Results from the Dental, Oral, Medical Epidemiological (DOME) Records-Based Nationwide Study. Biology 2021, 10, 178. https://doi.org/10.3390/biology10030178
Abramovitz I, Zini A, Atzmoni M, Kedem R, Zur D, Protter NE, Almoznino G. Cognitive Performance and Its Associations with Dental Caries: Results from the Dental, Oral, Medical Epidemiological (DOME) Records-Based Nationwide Study. Biology. 2021; 10(3):178. https://doi.org/10.3390/biology10030178
Chicago/Turabian StyleAbramovitz, Itzhak, Avraham Zini, Matan Atzmoni, Ron Kedem, Dorit Zur, Noam E. Protter, and Galit Almoznino. 2021. "Cognitive Performance and Its Associations with Dental Caries: Results from the Dental, Oral, Medical Epidemiological (DOME) Records-Based Nationwide Study" Biology 10, no. 3: 178. https://doi.org/10.3390/biology10030178
APA StyleAbramovitz, I., Zini, A., Atzmoni, M., Kedem, R., Zur, D., Protter, N. E., & Almoznino, G. (2021). Cognitive Performance and Its Associations with Dental Caries: Results from the Dental, Oral, Medical Epidemiological (DOME) Records-Based Nationwide Study. Biology, 10(3), 178. https://doi.org/10.3390/biology10030178








