Superiority of Multiple-Joint Space Width over Minimum-Joint Space Width Approach in the Machine Learning for Radiographic Severity and Knee Osteoarthritis Progression
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Dataset and Preprocessing
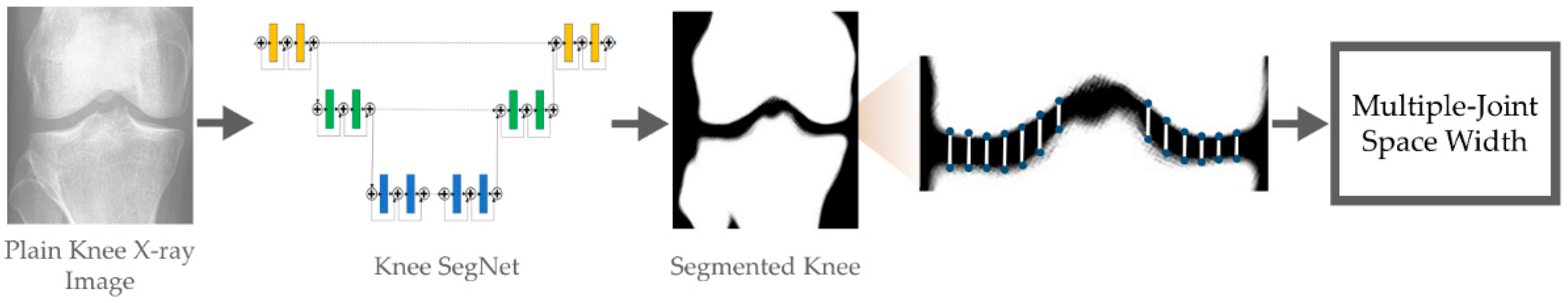
2.2. Bone Segmentation Using Deep Neural Network
2.3. Model Training
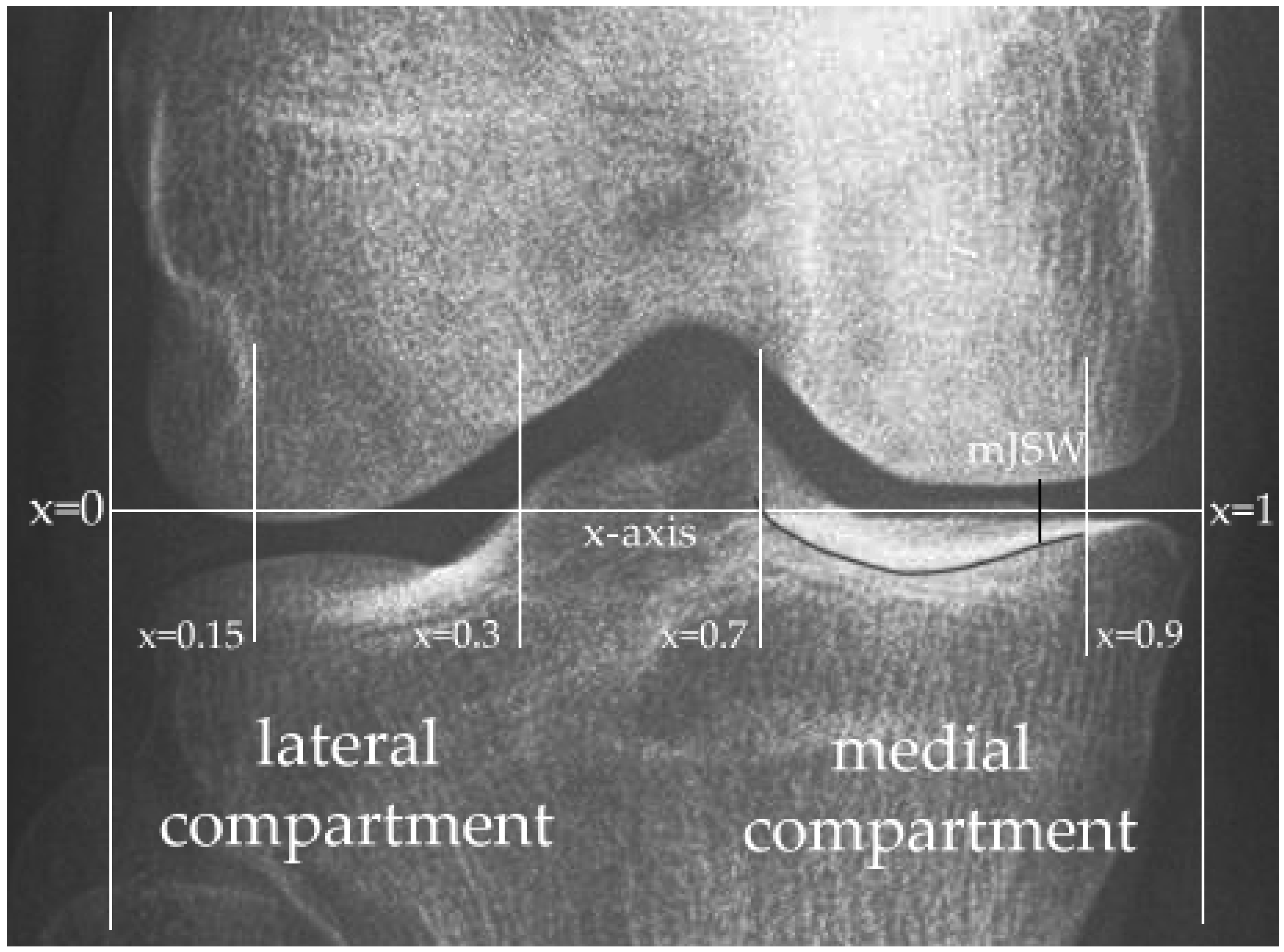
2.4. Quantitative Measurement
2.5. KOA Severity and Progression Prediction
3. Results
3.1. Reliability of the Annotations
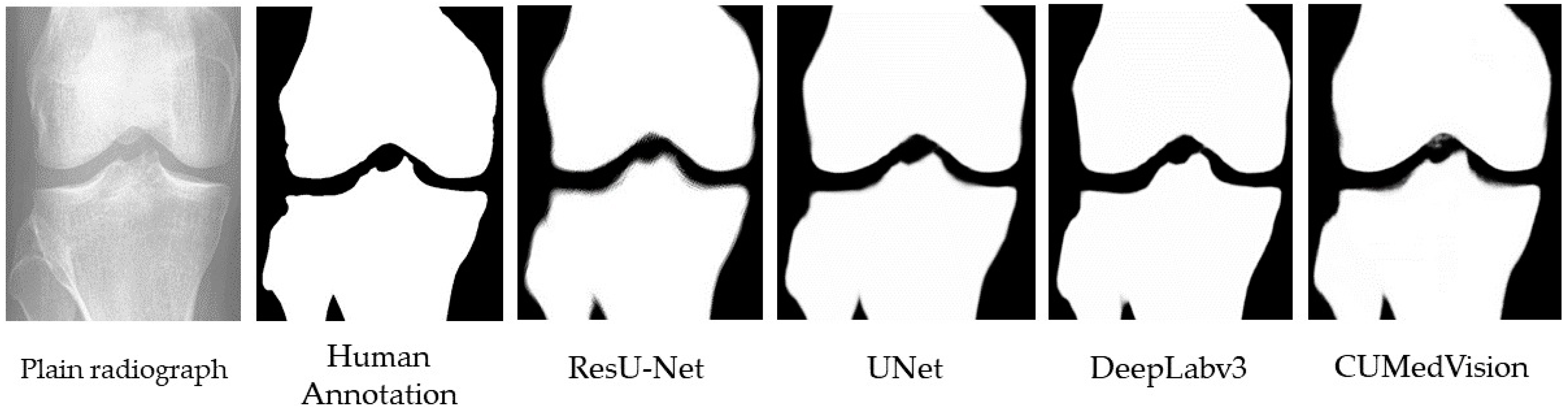
3.2. Bone Segmentation Performance Comparison
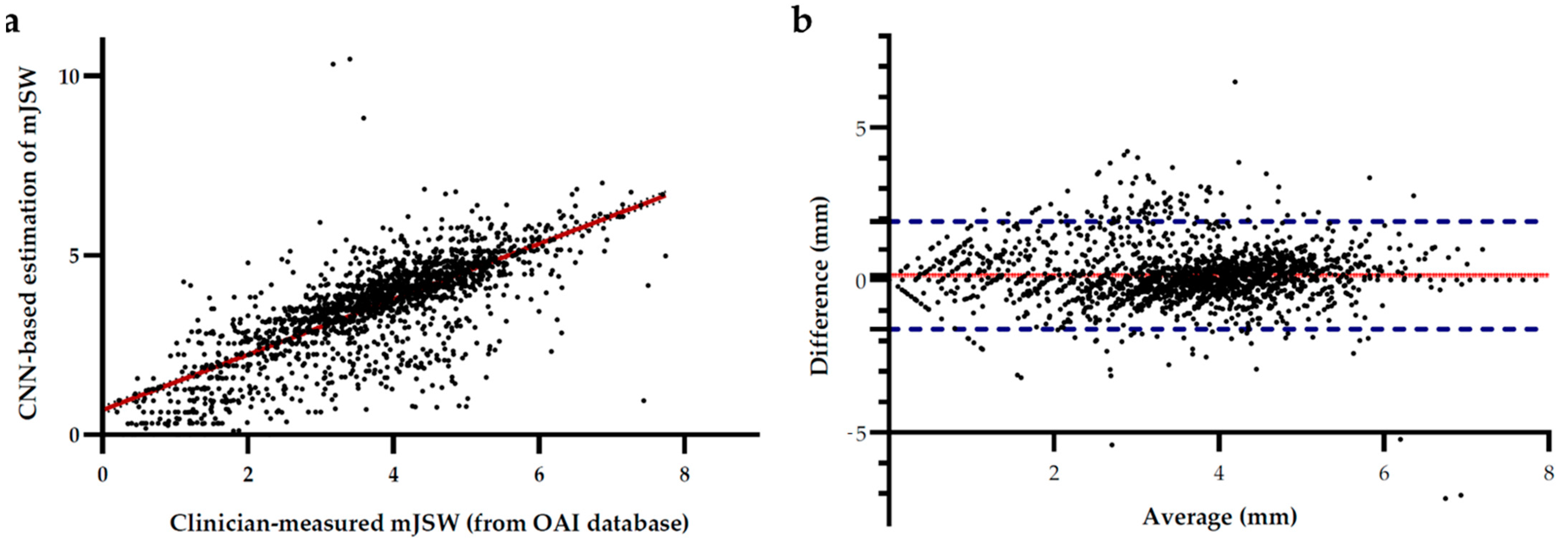
3.3. Automated Measurement of Joint Space Width
3.4. Prediction of KOA Severity and Progression
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Oka, H.; Muraki, S.; Akune, T.; Mabuchi, A.; Suzuki, T.; Yoshida, H.; Yamamoto, S.; Nakamura, K.; Yoshimura, N.; Kawaguchi, H. Fully automatic quantification of knee osteoarthritis severity on plain radiographs. Osteoarthr. Cartil. 2008, 16, 1300–1306. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gale, D.; Chaisson, C.; Totterman, S.; Schwartz, R.; Gale, M.; Felson, D. Meniscal subluxation: Association with osteoarthritis and joint space narrowing. Osteoarthr. Cartil. 1999, 7, 526–532. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Altman, R.; Gold, G. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthr. Cartil. 2007, 15, A1–A56. [Google Scholar] [CrossRef] [Green Version]
- Tiulpin, A.; Saarakkala, S. Automatic grading of individual knee osteoarthritis features in plain radiographs using deep convolutional neural networks. arXiv 2019, arXiv:1907.08020. [Google Scholar]
- Shamir, L.; Ling, S.; Scott, W.; Hochberg, M.; Ferrucci, L.; Goldberg, I. Early detection of radiographic knee osteoarthritis using computer-aided analysis. Osteoarthr. Cartil. 2009, 17, 1307–1312. [Google Scholar] [CrossRef] [Green Version]
- Gornale, S.S.; Patravali, P.U.; Manza, R.R. Detection of osteoarthritis using knee x-ray image analyses: A machine vision based approach. Int. J. Comput. Appl. 2016, 145, 20–26. [Google Scholar]
- Tiulpin, A.; Melekhov, I.; Saarakkala, S. KNEEL: Knee Anatomical Landmark Localization Using Hourglass Networks. In Proceedings of the Proceedings of the IEEE International Conference on Computer Vision Workshops, Seoul, Korea, 27 October–2 November 2019; pp. 352–361. [Google Scholar]
- Petroudi, S.; Loizou, C.; Pantziaris, M.; Pattichis, C. Segmentation of the Common Carotid Intima-Media Complex in Ultrasound Images Using Active Contours. IEEE Trans. Biomed. Eng. 2012, 59, 3060–3069. [Google Scholar] [CrossRef]
- Goodfellow, I. Deep Learning; Bengio, Y., Courville, A., Eds.; The MIT Press: Cambridge, MA, USA, 2016. [Google Scholar]
- Tiulpin, A.; Klein, S.; Bierma-Zeinstra, S.M.A.; Thevenot, J.; Rahtu, E.; Van Meurs, J.; Oei, E.H.G.; Saarakkala, S. Multimodal Machine Learning-based Knee Osteoarthritis Progression Prediction from Plain Radiographs and Clinical Data. Sci. Rep. 2019, 9, 20038. [Google Scholar] [CrossRef]
- Wang, T.; Leung, K.; Cho, K.; Chang, G.; Deniz, C.M. Total knee replacement prediction using structural MRIs and 3D convolutional neural networks. In Proceedings of the International Conference on Medical Imaging with Deep Learning—Extended Abstract Track, London, UK, 8–10 July 2019. [Google Scholar]
- Tiulpin, A.; Finnilä, M.; Lehenkari, P.; Nieminen, H.J.; Saarakkala, S. Deep-learning for tidemark segmentation in human osteochondral tissues imaged with micro-computed tomography. In Proceedings of the International Conference on Advanced Concepts for Intelligent Vision Systems, Auckland, New Zealand, 10–14 February 2020; pp. 131–138. [Google Scholar]
- Lindner, C.; Thiagarajah, S.; Wilkinson, J.M.; Wallis, G.A.; Cootes, T.F.; Consortium, a. Accurate bone segmentation in 2D radiographs using fully automatic shape model matching based on regression-voting. In Proceedings of the International Conference on Medical Image Computing and Computer-Assisted Intervention, Nagoya, Japan, 22–26 September 2013; pp. 181–189. [Google Scholar] [CrossRef]
- Thomson, J.; O’Neill, T.; Felson, D.; Cootes, T. Automated shape and texture analysis for detection of osteoarthritis from radiographs of the knee. In Proceedings of the International Conference on Medical Image Computing and Computer-Assisted Intervention, Munich, Germany, 5–9 October 2015; pp. 127–134. [Google Scholar] [CrossRef]
- Antony, J.; McGuinness, K.; Moran, K.; O’Connor, N.E. Automatic detection of knee joints and quantification of knee osteoarthritis severity using convolutional neural networks. In Proceedings of the International Conference on Machine Learning and Data Mining in Pattern Recognition, New York, NY, USA, 15–20 July 2017; pp. 376–390. [Google Scholar] [CrossRef] [Green Version]
- Norman, B.; Pedoia, V.; Noworolski, A.; Link, T.M.; Majumdar, S. Applying Densely Connected Convolutional Neural Networks for Staging Osteoarthritis Severity from Plain Radiographs. J. Digit. Imaging 2019, 32, 471–477. [Google Scholar] [CrossRef] [PubMed]
- Badrinarayanan, V.; Kendall, A.; Cipolla, R. SegNet: A Deep Convolutional Encoder-Decoder Architecture for Image Segmentation. IEEE Trans. Pattern Anal. Mach. Intell. 2017, 39, 2481–2495. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Qi, X.J.; Cheng, J.Z.; Heng, P.A. Deep contextual networks for neuronal structure segmentation. In Proceedings of the Thirtieth AAAI Conference on Artificial Intelligence, Phoenix, AZ, USA, 12–17 February 2016. [Google Scholar]
- Chen, L.-C.; Papandreou, G.; Kokkinos, I.; Murphy, K.; Yuille, A.L. DeepLab: Semantic Image Segmentation with Deep Convolutional Nets, Atrous Convolution, and Fully Connected CRFs. IEEE Trans. Pattern Anal. Mach. Intell. 2017, 40, 834–848. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.-C.; Papandreou, G.; Schroff, F.; Adam, H. Rethinking atrous convolution for semantic image segmentation. arXiv 2017, arXiv:1706.05587. [Google Scholar]
- Ronneberger, O.; Fischer, P.; Brox, T. U-net: Convolutional networks for biomedical image segmentation. In Proceedings of the International Conference on Medical Image Computing and Computer-Assisted Intervention, Munich, Germany, 5–9 October 2015; pp. 234–241. [Google Scholar]
- Bayramoglu, N.; Nieminen, M.T.; Saarakkala, S. A Lightweight CNN and Joint Shape-Joint Space (JS2) Descriptor for Radiological Osteoarthritis Detection. In Medical Image Understanding and Analysis; Springer: Cham, Switzerland, 2020; pp. 331–345. [Google Scholar] [CrossRef]
- Mills, K.; Hettinga, B.A.; Pohl, M.B.; Ferber, R. Between-Limb Kinematic Asymmetry During Gait in Unilateral and Bilateral Mild to Moderate Knee Osteoarthritis. Arch. Phys. Med. Rehabilitation 2013, 94, 2241–2247. [Google Scholar] [CrossRef]
- Drozdzal, M.; Vorontsov, E.; Chartrand, G.; Kadoury, S.; Pal, C. The importance of skip connections in biomedical image segmentation. In Deep Learning and Data Labeling for Medical Applications; Springer: Heidelberg, Germany, 2016; pp. 179–187. [Google Scholar] [CrossRef] [Green Version]
- Zahra, E.; Ali, B.; Siddique, W. Medical Image Segmentation Using a U-Net type of Architecture. arXiv 2005, arXiv:05218.2020. [Google Scholar]
- Dunnhofer, M.; Antico, M.; Sasazawa, F.; Takeda, Y.; Camps, S.; Martinel, N.; Micheloni, C.; Carneiro, G.; Fontanarosa, D. Siam-U-Net: Encoder-decoder siamese network for knee cartilage tracking in ultrasound images. Med. Image Anal. 2020, 60, 101631. [Google Scholar] [CrossRef] [PubMed]
- He, K.; Zhang, X.; Ren, S.; Sun, J. Deep residual learning for image recognition. In Proceedings of the 2016 IEEE Conference on Computer Vision and Pattern Recognition (CVPR), Las Vegas, NV, USA, 27–30 June 2016; pp. 770–778. [Google Scholar]
- Giavarina, D. Understanding Bland Altman analysis. Biochem. Medica 2015, 25, 141–151. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, T.; Guestrin, C. Xgboost: A scalable tree boosting system. In Proceedings of the KDD ’16: The 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–17 August 2016; pp. 785–794. [Google Scholar]
- Bartko, J.J. The Intraclass Correlation Coefficient as a Measure of Reliability. Psychol. Rep. 1966, 19, 3–11. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 327, 307–310. [Google Scholar] [CrossRef]
- Lindner, C.; Thiagarajah, S.; Wilkinson, J.M.; Wallis, G.A.; Cootes, T.F.; Consortium, a. Accurate fully automatic femur segmentation in pelvic radiographs using regression voting. In Proceedings of the International Conference on Medical Image Computing and Computer-Assisted Intervention, Nice, France, 1–5 October 2012; pp. 353–360. [Google Scholar] [CrossRef] [Green Version]
- Hesamian, M.H.; Jia, W.; He, X.; Kennedy, P. Deep Learning Techniques for Medical Image Segmentation: Achievements and Challenges. J. Digit. Imaging 2019, 32, 582–596. [Google Scholar] [CrossRef] [Green Version]
- Mahapatra, D.; Ge, Z.; Sedai, S.; Chakravorty, R. Joint Registration And Segmentation Of Xray Images Using Generative Adversarial Networks. In Proceedings of the 2018 International Conference on Machine Learning and Machine Intelligence, Hanoi, Vietnam, 28–30 September 2018; pp. 73–80. [Google Scholar] [CrossRef]
- Neumann, G.; Hunter, D.; Nevitt, M.; Chibnik, L.; Kwoh, K.; Chen, H.; Harris, T.; Satterfield, S.; Duryea, J. Location specific radiographic joint space width for osteoarthritis progression. Osteoarthr. Cartil. 2009, 17, 761–765. [Google Scholar] [CrossRef] [Green Version]
- Minciullo, L.; Cootes, T. Fully automated shape analysis for detection of Osteoarthritis from lateral knee radiographs. In Proceedings of the 2016 23rd International Conference on Pattern Recognition (ICPR), Cancún, Mexico, 4–8 December 2016; pp. 3787–3791. [Google Scholar]
- Haverkamp, D.J.; Schiphof, D.; Bierma-Zeinstra, S.M.; Weinans, H.; Waarsing, J.H. Variation in joint shape of osteoarthritic knees. Arthritis Rheum. 2011, 63, 3401–3407. [Google Scholar] [CrossRef] [PubMed]
- Dupuis, D.; Beynnon, B.; Richard, M.; Novotny, J.; Skelly, J.; Cooper, S. Precision and accuracy of joint space width measurements of the medial compartment of the knee using standardized MTP semi-flexed radiographs. Osteoarthr. Cartil. 2003, 11, 716–724. [Google Scholar] [CrossRef] [Green Version]
- Chan, T.F.; Vese, L.A. Active contours without edges. IEEE Trans. Image Process. 2001, 10, 266–277. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lindner, C.; Thiagarajah, S.; Wilkinson, J.M.; The Consortium; Wallis, G.A.; Cootes, T. Fully Automatic Segmentation of the Proximal Femur Using Random Forest Regression Voting. IEEE Trans. Med. Imaging 2013, 32, 1462–1472. [Google Scholar] [CrossRef]
- Gielis, W.; Weinans, H.; Welsing, P.; van Spil, W.; Agricola, R.; Cootes, T.; de Jong, P.; Lindner, C. An automated workflow based on hip shape improves personalized risk prediction for hip osteoarthritis in the CHECK study. Osteoarthr. Cartil. 2020, 28, 62–70. [Google Scholar] [CrossRef] [Green Version]
| Models | Mean IoU | Validation Loss | Training Loss | Over-Fitting |
|---|---|---|---|---|
| CUMedVision | 0.973 | 0.047 | 0.008 | 0.830 |
| U-Net | 0.594 | 0.410 | 0.409 | 0.002 |
| DeepLabv3 | 0.989 | 0.011 | 0.005 | 0.545 |
| ResU-Net-18 (ours) | 0.989 | 0.006 | 0.004 | 0.333 |
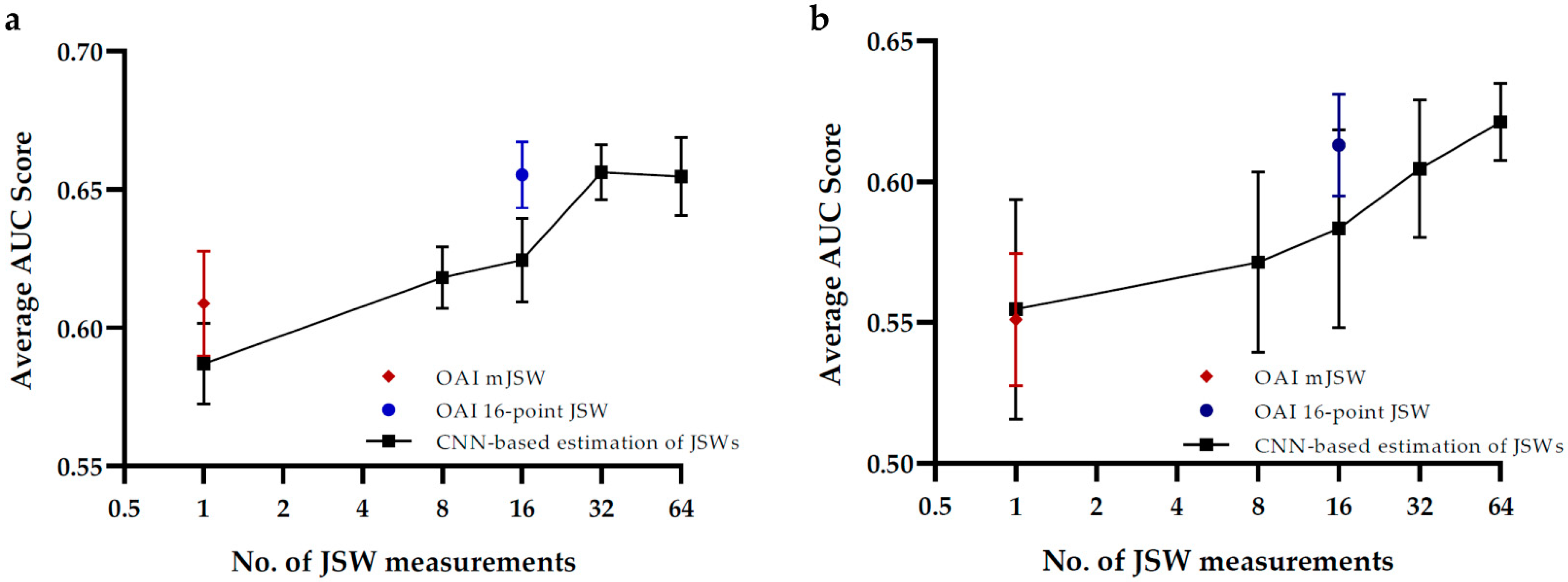
| Macro Average F1 | Average AUC | p-Value of AUC Comparison | ||
|---|---|---|---|---|
| Minimum-JSW (single-point) | CNN-based Estimation | 0.311 (± 0.020) | 0.587 (± 0.017) | 0.1225 |
| Radiologist measurement | 0.402 (± 0.030) | 0.624 (± 0.017) | ||
| 16-point JSWs | CNN-based Estimation | 0.337 (± 0.027) | 0.609 (± 0.022) | 0.0063 |
| Radiologist measurement | 0.454 (± 0.024) | 0.655 (± 0.014) |
| Average F1 | Average AUC | p-Value of AUC Comparison | ||
|---|---|---|---|---|
| Minimum-JSW (single-point) | CNN-based Estimation | 0.484 (± 0.041) | 0.554 (± 0.039) | 0.898 |
| Radiologist measurement | 0.544 (± 0.032) | 0.583 (± 0.040) | ||
| 16-point JSWs | CNN-based Estimation | 0.480 (± 0.041) | 0.551 (± 0.024) | 0.1816 |
| Radiologist measurement | 0.562(± 0.044) | 0.613 (± 0.018) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheung, J.C.-W.; Tam, A.Y.-C.; Chan, L.-C.; Chan, P.-K.; Wen, C. Superiority of Multiple-Joint Space Width over Minimum-Joint Space Width Approach in the Machine Learning for Radiographic Severity and Knee Osteoarthritis Progression. Biology 2021, 10, 1107. https://doi.org/10.3390/biology10111107
Cheung JC-W, Tam AY-C, Chan L-C, Chan P-K, Wen C. Superiority of Multiple-Joint Space Width over Minimum-Joint Space Width Approach in the Machine Learning for Radiographic Severity and Knee Osteoarthritis Progression. Biology. 2021; 10(11):1107. https://doi.org/10.3390/biology10111107
Chicago/Turabian StyleCheung, James Chung-Wai, Andy Yiu-Chau Tam, Lok-Chun Chan, Ping-Keung Chan, and Chunyi Wen. 2021. "Superiority of Multiple-Joint Space Width over Minimum-Joint Space Width Approach in the Machine Learning for Radiographic Severity and Knee Osteoarthritis Progression" Biology 10, no. 11: 1107. https://doi.org/10.3390/biology10111107
APA StyleCheung, J. C.-W., Tam, A. Y.-C., Chan, L.-C., Chan, P.-K., & Wen, C. (2021). Superiority of Multiple-Joint Space Width over Minimum-Joint Space Width Approach in the Machine Learning for Radiographic Severity and Knee Osteoarthritis Progression. Biology, 10(11), 1107. https://doi.org/10.3390/biology10111107







