Comparison Between Bond Strengths of a Resin Cement on Traditional Prosthetic Substrates and a 3D-Printed Resin for Permanent Restorations
Abstract
1. Introduction
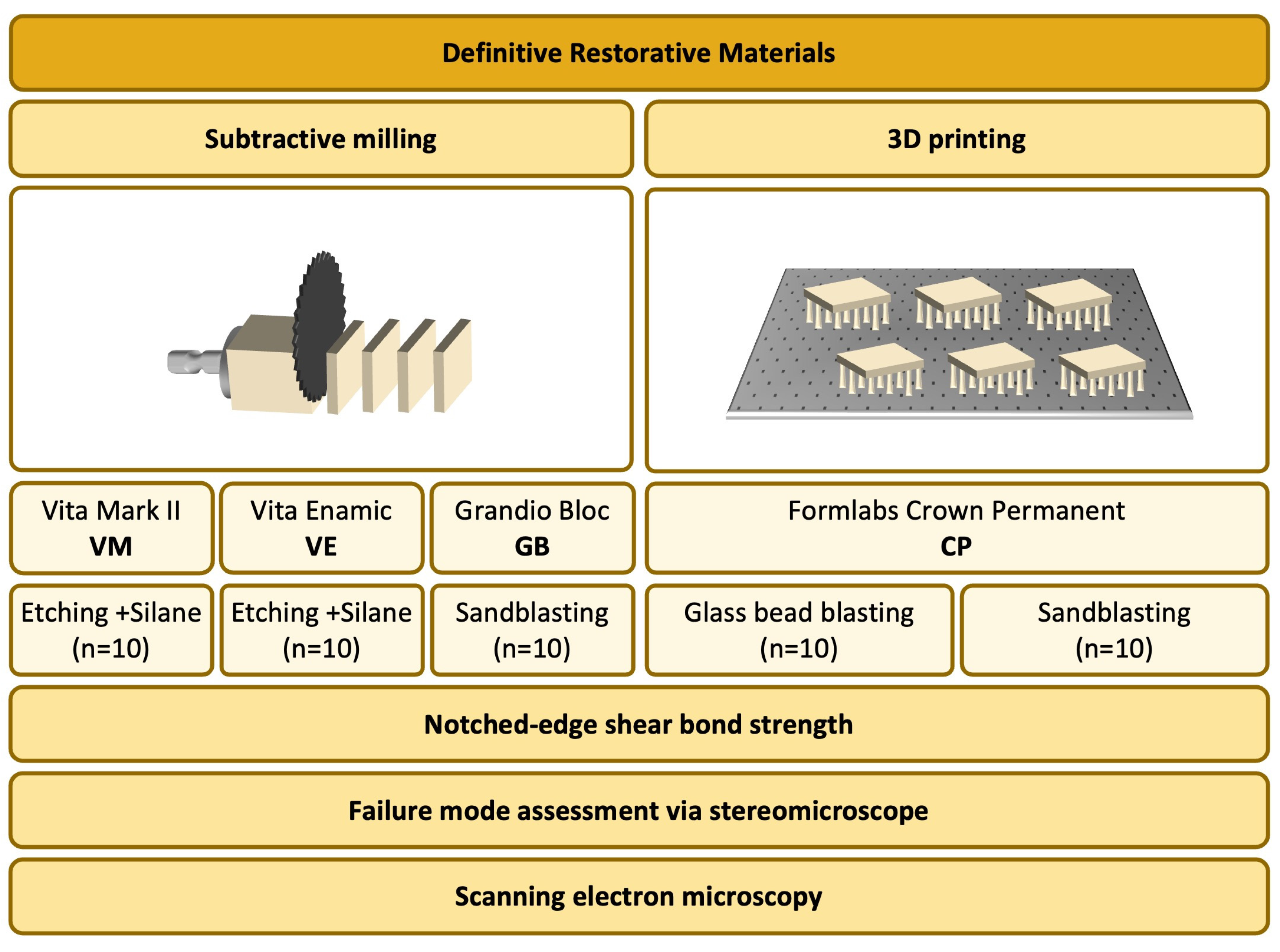
2. Materials and Methods
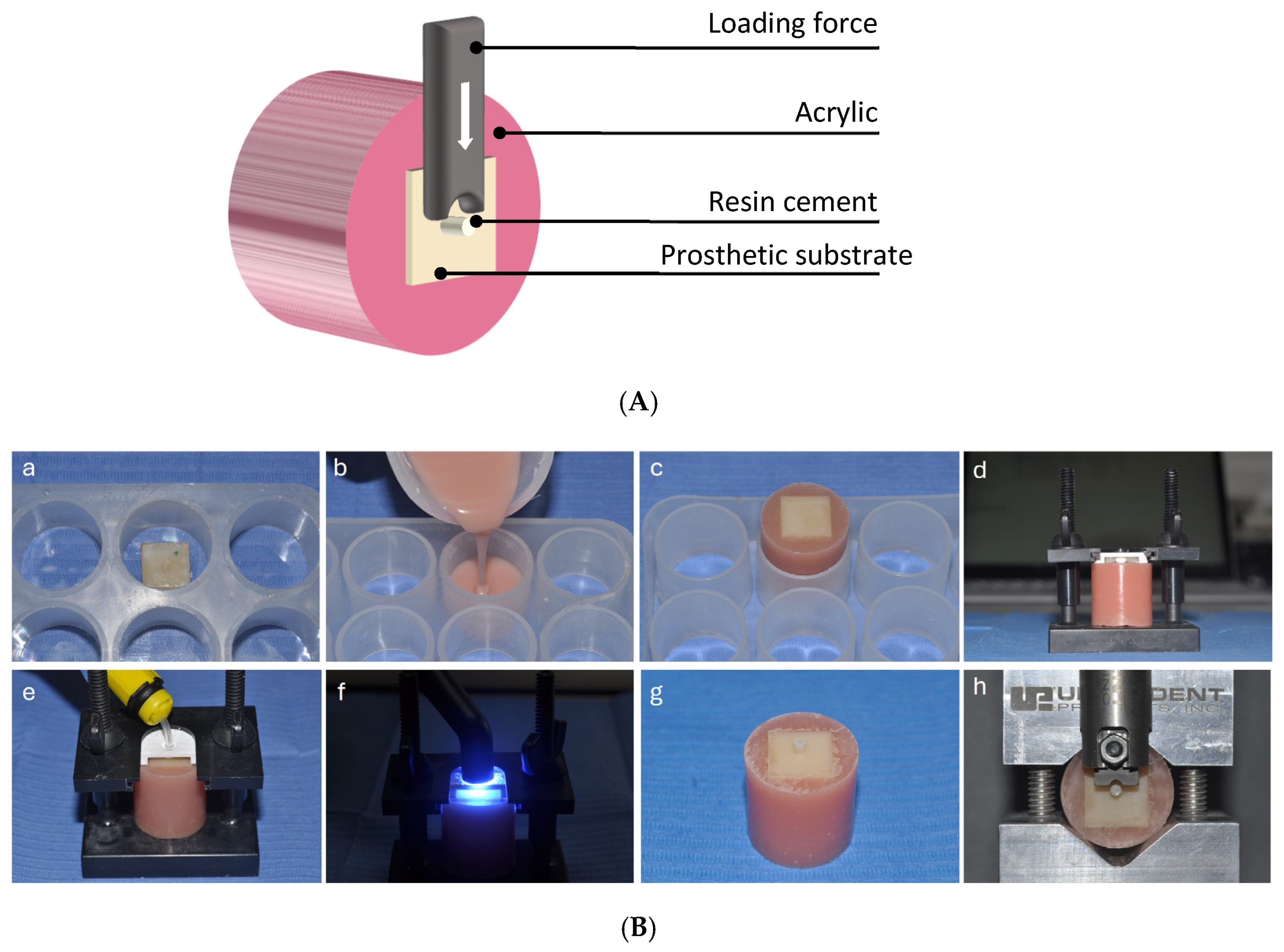
2.1. Specimen Preparation
2.2. Bonding Procedure
2.3. Notched-Edge Shear Bond Strength Test
2.4. Failure Mode Assessment
2.5. Statistical Analysis
2.6. SEM Observation
3. Results
3.1. Notched-Edge Shear Bond Strength Test
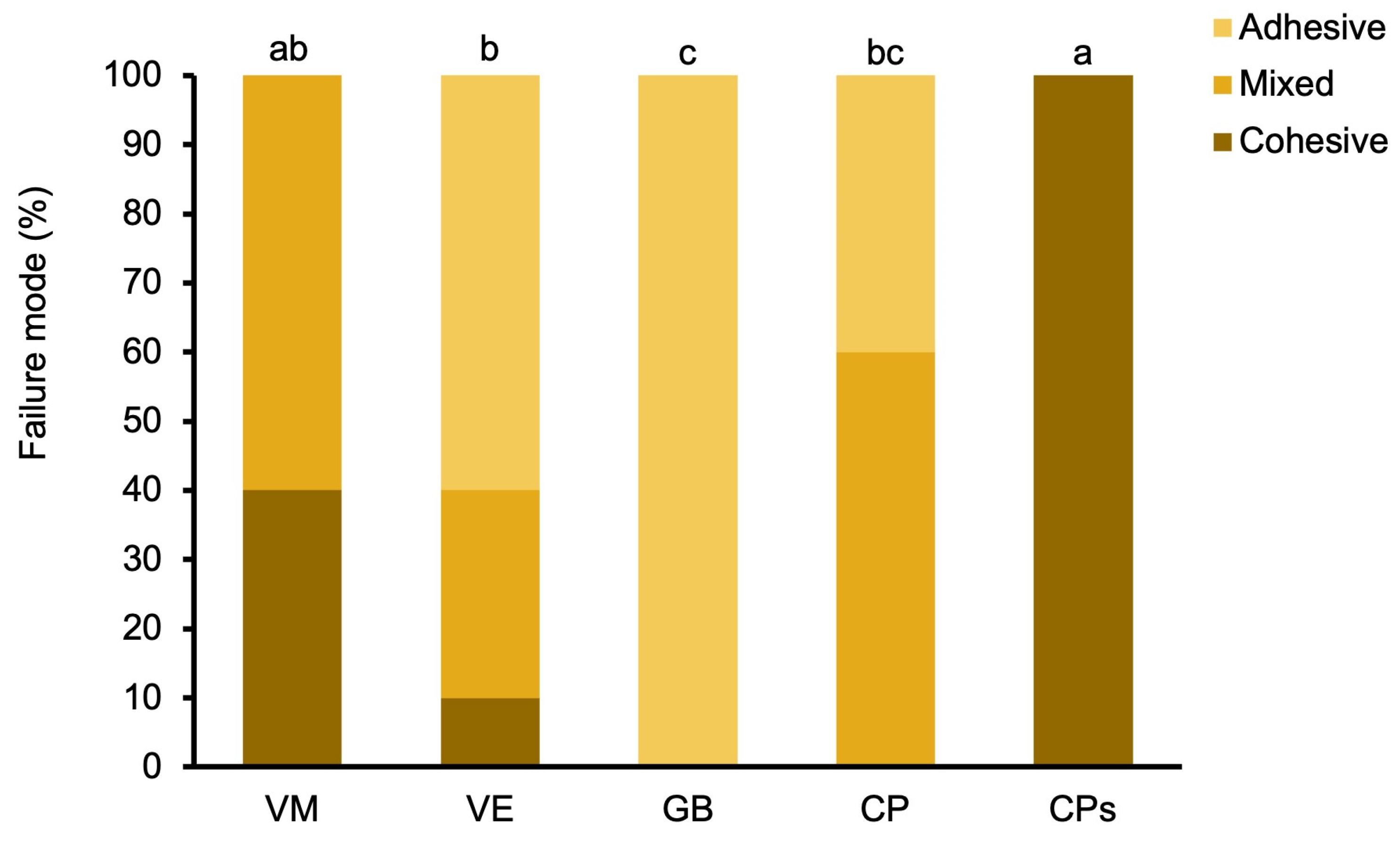
3.2. Failure Mode Assessment
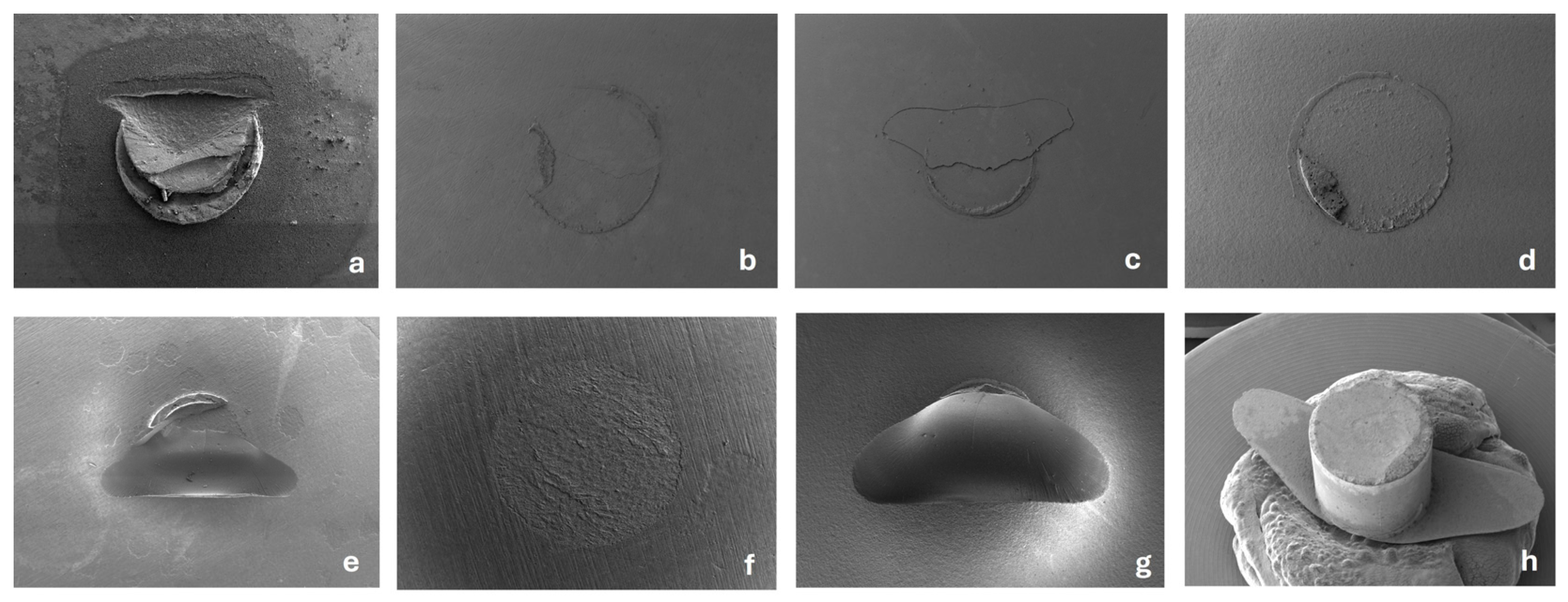
3.3. SEM Observation
4. Discussion
5. Conclusions
- The bond strength between Feldspathic ceramic and Rely X cement was shown to be higher than all the other materials/combinations tested. The CAD/CAM block resin, 3D-printed definitive resin and PICN performed similarly.
- The bond strength between Rely-X resin cement and 3D-printed definitive resin could be considered clinically sufficient considering the thresholds reported in the literature.
- The sandblasting procedure after pearl blasting did not improve the short-term bond strength of the 3D-printed definitive resin.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Roulet, J.-F.O.; Degrange, M. Adhesion: The Silent Revolution in Dentistry; Quintessence: Chicago, IL, USA, 2000. [Google Scholar]
- Perdigão, J.; Araujo, E.; Ramos, R.Q.; Gomes, G.; Pizzolotto, L. Adhesive dentistry: Current concepts and clinical considerations. J. Esthet. Restor. Dent. 2021, 33, 51–68. [Google Scholar] [CrossRef] [PubMed]
- Cadenaro, M.; Josic, U.; Maravić, T.; Mazzitelli, C.; Marchesi, G.; Mancuso, E.; Breschi, L.; Mazzoni, A. Progress in Dental Adhesive Materials. J. Dent. Res. 2023, 102, 254–262. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, C.; Gavriil, D. Predictable bonding of adhesive indirect restorations: Factors for success. Br. Dent. J. 2021, 231, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Skorulska, A.; Piszko, P.; Rybak, Z.; Szymonowicz, M.; Dobrzyński, M. Review on Polymer, Ceramic and Composite Materials for CAD/CAM Indirect Restorations in Dentistry-Application, Mechanical Characteristics and Comparison. Materials 2021, 14, 1592. [Google Scholar] [CrossRef] [PubMed]
- Galiatsatos, A.; Galiatsatos, P.; Bergou, D. Clinical Longevity of Indirect Composite Resin Inlays and Onlays: An Up to 9-Year Prospective Study. Eur. J. Dent. 2022, 16, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Unlu, N.; Gunal, S.; Ulker, M.; Ozer, F.; Blatz, M.B. Influence of operator experience on in vitro bond strength of dentin adhesives. J. Adhes. Dent. 2012, 14, 223–227. [Google Scholar] [PubMed]
- Santos, M.; Zare, E.; McDermott, P.; Santos Junior, G.C. Multifactorial Contributors to the Longevity of Dental Restorations: An Integrated Review of Related Factors. Dent. J. 2024, 12, 291. [Google Scholar] [CrossRef] [PubMed]
- Abad-Coronel, C.; Naranjo, B.; Valdiviezo, P. Adhesive Systems Used in Indirect Restorations Cementation: Review of the Literature. Dent. J. 2019, 7, 71. [Google Scholar] [CrossRef] [PubMed]
- Dioguardi, M.; Alovisi, M.; Troiano, G.; Caponio, C.V.A.; Baldi, A.; Rocca, G.T.; Comba, A.; Lo Muzio, L.; Scotti, N. Clinical outcome of bonded partial indirect posterior restorations on vital and non-vital teeth: A systematic review and meta-analysis. Clin. Oral Investig. 2021, 25, 6597–6621. [Google Scholar] [CrossRef] [PubMed]
- Alammar, A.; Kois, J.C.; Revilla-León, M.; Att, W. Additive Manufacturing Technologies: Current Status and Future Perspectives. J. Prosthodont. 2022, 31, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Methani, M.M.; Revilla-León, M.; Zandinejad, A. The potential of additive manufacturing technologies and their processing parameters for the fabrication of all-ceramic crowns: A review. J. Esthet. Restor. Dent. 2020, 32, 182–192. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Meyers, M.J.; Zandinejad, A.; Özcan, M. A review on chemical composition, mechanical properties, and manufacturing work flow of additively manufactured current polymers for interim dental restorations. J. Esthet. Restor. Dent. 2019, 31, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Çokakoğlu, S.; Karaokutan, I.; Buyuk, S.K. Effects of orientation and postprocessing on the bonding of 3-dimensional printed brackets to printable permanent crown resin. Am. J. Orthod. Dentofacial Orthop. 2025, 167, 362–370. [Google Scholar] [CrossRef] [PubMed]
- Daher, R.; Ardu, S.; di Bella, E.; Krejci, I.; Duc, O. Efficiency of 3D printed composite resin restorations compared with subtractive materials: Evaluation of fatigue behavior, cost, and time of production. J. Prosthet. Dent. 2024, 131, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Shin, Y.; Kim, I.-H.; Song, J.S. In Vitro Study on the Bond Strength Between 3D-Printed Resin and Resin Cement for Pediatric Crown Restoration. J. Korean Acad. Pediatr. Dent. 2023, 50, 104–112. [Google Scholar] [CrossRef]
- Ersöz, B.; Aydın, N.; Ezmek, B.; Karaoğlanoğlu, S.; Çal İ, K. Effect of Surface Treatments Applied to 3D Printed Permanent Resins on Shear Bond Strength. J. Clin. Exp. Dent. 2024, 16, e1059–e1066. [Google Scholar] [CrossRef] [PubMed]
- Graf, T.; Erdelt, K.J.; Güth, J.F.; Edelhoff, D.; Schubert, O.; Schweiger, J. Influence of Pre-Treatment and Artificial Aging on the Retention of 3D-Printed Permanent Composite Crowns. Biomedicines 2022, 10, 2186. [Google Scholar] [CrossRef] [PubMed]
- Aktas, N.; Bankoglu Güngör, M. Effects of 3D-Printing Technology and Cement Type on the Fracture Resistance of Permanent Resin Crowns for Primary Teeth. Int. J. Prosthodont. 2024, 37, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Lim, N.K.; Shin, S.Y. Bonding of conventional provisional resin to 3D printed resin: The role of surface treatments and type of repair resins. J. Adv. Prosthodont. 2020, 12, 322–328. [Google Scholar] [CrossRef] [PubMed]
- Lunkad, H.; Sayed, M.E.; Alhazmi, A.E.; Alwadani, B.; Shafei, A.M.; Ayoub, M.N.; Shabi, M.M.A.; Mesawa, S.A.; Abdulfatah, B.A.; Alqarni, H.; et al. The Effect of the Digital Manufacturing Technique, Preparation Taper, and Cement Type on the Retention of Aged Anterior Provisional Crowns: An In Vitro Study. Appl. Sci. 2022, 12, 12714. [Google Scholar] [CrossRef]
- Formlabs. Formlabs Crown Permanent Safety Data Sheet. 2021. Available online: https://formlabs-media.formlabs.com/datasheets/ENUS_Safety_Data_Sheet_-_Permanent_Crown.pdf (accessed on 4 May 2025).
- Formlabs. Formlabs Crown Permanent Technical Data Sheet. 2020. Available online: https://formlabs-media.formlabs.com/datasheets/2002482-TDS-ENUS-0.pdf (accessed on 15 October 2024).
- Kirmali, O.; Barutcugil, C.; Harorli, O.; Kapdan, A.; Er, K. Resin cement to indirect composite resin bonding: Effect of various surface treatments. Scanning 2015, 37, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Tribst, J.P.M.; Veerman, A.; Pereira, G.K.R.; Kleverlaan, C.J.; Dal Piva, A.M.O. Comparative Strength Study of Indirect Permanent Restorations: 3D-Printed, Milled, and Conventional Dental Composites. Clin. Pract. 2024, 14, 1940–1952. [Google Scholar] [CrossRef] [PubMed]
- Pfeffer, S.; Jacker-Guhr, S.; Geurtsen, W.; Pfeffer, T.; Lührs, A. Microtensile bond strength of luting cements to a 3D printable composite–an in vitro study. Zahnärztl J. Int. 2020, 2, 229–239. [Google Scholar]
- ISO 29022:2013; S-E: Dentistry—Adhesion—Notched-Edge Shear Bond Strength Test. SIS Förlag AB: Stockholm, Sweden, 2013.
- Formlabs. Formlabs Crown Permanent Instructions for Use. 2025. Available online: https://media.formlabs.com/m/73a550261e0ab65b/original/-ENUS-Permanent-Crown-Resin-Instructions-for-Use.pdf (accessed on 15 October 2024).
- D’Arcangelo, C.; Vanini, L.; Casinelli, M.; Frascaria, M.; De Angelis, F.; Vadini, M.; D’Amario, M. Adhesive Cementation of Indirect Composite Inlays and Onlays: A Literature Review. Compend. Contin. Educ. Dent. 2015, 36, 570–577, quiz 578. [Google Scholar] [PubMed]
- Özcan, M.; Volpato, C.A.M. Current perspectives on dental adhesion: (3) Adhesion to intraradicular dentin: Concepts and applications. Jpn. Dent. Sci. Rev. 2020, 56, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Perdigão, J. Current perspectives on dental adhesion: (1) Dentin adhesion—Not there yet. Jpn. Dent. Sci. Rev. 2020, 56, 190–207. [Google Scholar] [CrossRef] [PubMed]
- Madrigal, E.L.; Tichy, A.; Hosaka, K.; Ikeda, M.; Nakajima, M.; Tagami, J. The effect of curing mode of dual-cure resin cements on bonding performance of universal adhesives to enamel, dentin and various restorative materials. Dent. Mater. J. 2021, 40, 446–454. [Google Scholar] [CrossRef] [PubMed]
- Fabian Fonzar, R.; Goracci, C.; Carrabba, M.; Louca, C.; Ferrari, M.; Vichi, A. Influence of Acid Concentration and Etching Time on Composite Cement Adhesion to Lithium-silicate Glass Ceramics. J. Adhes. Dent. 2020, 22, 175–182. [Google Scholar] [PubMed]
- Bayazıt, E. Microtensile Bond Strength of Self-Adhesive Resin Cements to CAD/CAM Resin-Matrix Ceramics Prepared with Different Surface Treatments. Int. J. Prosthodont. 2019, 32, 433–438. [Google Scholar] [CrossRef] [PubMed]
- Scholz, K.J.; Bittner, A.; Cieplik, F.; Hiller, K.A.; Schmalz, G.; Buchalla, W.; Federlin, M. Micromorphology of the Adhesive Interface of Self-Adhesive Resin Cements to Enamel and Dentin. Materials 2021, 14, 492. [Google Scholar] [CrossRef] [PubMed]
- Butler, S.; Santos, G.C.; Santos, M.J.C. Do high translucency zirconia shades contribute to the degree of conversion of dual-cure resin cements? Quintessence Int. 2021, 53, 8–14. [Google Scholar] [PubMed]
- Erzurumlu, Z.U.; Sagirkaya, C.E.; Erzurumlu, K. Evaluation of radiopacities of CAD/CAM restorative materials and resin cements by digital radiography. Clin. Oral Investig. 2021, 25, 5735–5741. [Google Scholar] [CrossRef] [PubMed]
- Astasov-Frauenhoffer, M.; Glauser, S.; Fischer, J.; Schmidli, F.; Waltimo, T.; Rohr, N. Biofilm formation on restorative materials and resin composite cements. Dent. Mater. 2018, 34, 1702–1709. [Google Scholar] [CrossRef] [PubMed]
- Vichi, A.; Fabian Fonzar, R.; Carrabba, M.; Louca, C.; Scotti, N.; Mazzitelli, C.; Breschi, L.; Goracci, C. Comparison between Hydrofluoric Acid and Single-Component Primer as Conditioners on Resin Cement Adhesion to Lithium Silicate and Lithium Disilicate Glass Ceramics. Materials 2021, 14, 6776. [Google Scholar] [CrossRef] [PubMed]
- Donmez, M.B.; Çakmak, G.; Yılmaz, D.; Schimmel, M.; Abou-Ayash, S.; Yilmaz, B.; Peutzfeldt, A. Bond strength of additively manufactured composite resins to dentin and titanium when bonded with dual-polymerizing resin cements. J. Prosthet. Dent. 2024, 132, 1067.e1061–1067.e1068. [Google Scholar] [CrossRef] [PubMed]
- Emsermann, I.; Eggmann, F.; Krastl, G.; Weiger, R.; Amato, J. Influence of Pretreatment Methods on the Adhesion of Composite and Polymer Infiltrated Ceramic CAD-CAM Blocks. J. Adhes. Dent. 2019, 21, 433–443. [Google Scholar] [PubMed]
- Peçanha, M.M.; Amaral, M.; Baroudi, K.; Frizzera, F.; Vitti, R.; Silva-Concilio, L. Improving the bonding stability between resin cements and zirconia-based ceramic using different surface treatments. Int. J. Prosthodont. 2022, 35, 414–419. [Google Scholar] [CrossRef] [PubMed]
- Straface, A.; Rupp, L.; Gintaute, A.; Fischer, J.; Zitzmann, N.U.; Rohr, N. HF etching of CAD/CAM materials: Influence of HF concentration and etching time on shear bond strength. Head Face Med. 2019, 15, 21. [Google Scholar] [CrossRef] [PubMed]
- Nasiry Khanlar, L.; Revilla-León, M.; Barmak, A.B.; Ikeda, M.; Alsandi, Q.; Tagami, J.; Zandinejad, A. Surface roughness and shear bond strength to composite resin of additively manufactured interim restorative material with different printing orientations. J. Prosthet. Dent. 2023, 129, 788–795. [Google Scholar] [CrossRef] [PubMed]
- Wiedenmann, F.; Klören, M.; Edelhoff, D.; Stawarczyk, B. Bond strength of CAD-CAM and conventional veneering materials to different frameworks. J. Prosthet. Dent. 2021, 125, 664–673. [Google Scholar] [CrossRef] [PubMed]
- Sirisha, K.; Rambabu, T.; Shankar, Y.R.; Ravikumar, P. Validity of bond strength tests: A critical review: Part I. J. Conserv. Dent. 2014, 17, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Sirisha, K.; Rambabu, T.; Ravishankar, Y.; Ravikumar, P. Validity of bond strength tests: A critical review-Part II. J. Conserv. Dent. 2014, 17, 420–426. [Google Scholar] [CrossRef] [PubMed]
- Chiang, M.L.; Birlbauer, S.; Lo, Y.F.; Pitchika, V.; Crispin, A.; Ilie, N.; Hickel, R.; Kühnisch, J. Which Factors Influence the Shear Bond Strength of Sealant Materials? J. Adhes. Dent. 2016, 18, 397–404. [Google Scholar] [PubMed]
- Barkmeier, W.W.; Tsujimoto, A.; Latta, M.A.; Takamizawa, T.; Radniecki, S.M.; Garcia-Godoy, F. Effect of mold enclosure and chisel design on fatigue bond strength of dental adhesive systems. Eur. J. Oral Sci. 2022, 130, e12864. [Google Scholar] [CrossRef] [PubMed]
- Eick, J.D.; Gwinnett, A.J.; Pashley, D.H.; Robinson, S.J. Current concepts on adhesion to dentin. Crit. Rev. Oral Biol. Med. 1997, 8, 306–335. [Google Scholar] [CrossRef] [PubMed]
- Kiremitçi, A.; Yalçin, F.; Gökalp, S. Bonding to enamel and dentin using self-etching adhesive systems. Quintessence Int. 2004, 35, 367–370. [Google Scholar] [PubMed]
- Dimitriadis, K.; Tulyaganov, D.U.; Agathopoulos, S. Evaluation of bond strength between zirconia milled ceramic material and veneered dental porcelain. Eur. J. Oral Sci. 2024, 132, e12989. [Google Scholar] [CrossRef] [PubMed]
- ISO 9693:2019; Dentistry: Compatibility Testing for Metal-Ceramic and Ceramic-Ceramic Systems. International Organization for Standardization: Geneva, Switzerland, 2019.
- Papadopoulos, C.; Dionysopoulos, D.; Pahinis, K.; Koulaouzidou, E.; Tolidis, K. Microtensile Bond Strength Between Resin-Matrix CAD/CAM Ceramics and Resin Cement after Various Surface Modifications and Artificial Aging. J. Adhes. Dent. 2021, 23, 255–265. [Google Scholar] [PubMed]
- Şenol, M.; Gürbüz, A.; Oyar, P. Bond strength of conventional resin-based adhesive cement and self-adhesive resin cement to CAD-CAM restorative materials. BMC Oral Health 2025, 25, 296. [Google Scholar] [CrossRef] [PubMed]
- Hu, M.; Weiger, R.; Fischer, J. Comparison of two test designs for evaluating the shear bond strength of resin composite cements. Dent. Mater. 2016, 32, 223–232. [Google Scholar] [CrossRef] [PubMed]
- Blatz, M.B.; Conejo, J.; Alammar, A.; Ayub, J. Current Protocols for Resin-Bonded Dental Ceramics. Dent. Clin. N. Am. 2022, 66, 603–625. [Google Scholar] [CrossRef] [PubMed]
- Alnafaiy, S.M.; Labban, N.; Albaijan, R.; AlKahtani, R.N.; Al-Aali, K.A.; Abozaed, H.W.; Alturki, N.Y.; Alenezi, J.E. Evaluation of Shear Bond Strength and Failure Modes of Lithium Disilicate Ceramic Veneering Material to Different High-Performance Polymers. Polymers 2025, 17, 554. [Google Scholar] [CrossRef] [PubMed]
- Guggenbühl, S.; Alshihri, A.; Al-Haj Husain, N.; Özcan, M. Adhesion of Resin-Resin and Resin-Lithium Disilicate Ceramic: A Methodological Assessment. Materials 2021, 14, 3870. [Google Scholar] [CrossRef] [PubMed]
- Mao, Z.; Schmidt, F.; Beuer, F.; Yassine, J.; Hey, J.; Prause, E. Effect of surface treatment strategies on bond strength of additively and subtractively manufactured hybrid materials for permanent crowns. Clin. Oral Investig. 2024, 28, 371. [Google Scholar] [CrossRef] [PubMed]
- Lankes, V.; Reymus, M.; Mayinger, F.; Coldea, A.; Liebermann, A.; Hoffmann, M.; Stawarczyk, B. Three-Dimensional Printed Resin: Impact of Different Cleaning Protocols on Degree of Conversion and Tensile Bond Strength to a Composite Resin Using Various Adhesive Systems. Materials 2023, 16, 3580. [Google Scholar] [CrossRef] [PubMed]
- Soto-Montero, J.; Romano, B.d.C.; Noronha, M.d.S.; André, C.B.; Giannini, M. Microtensile bond strength of resin cements to 3-D printed and milled temporary restorative resins. Odovtos Int. J. Dent. Sci. 2023, 25, 82–98. [Google Scholar] [CrossRef]
- Gad, M.M.; Albazroun, Z.; Aldajani, F.; Elakel, A.M.; El Zayat, M.; Akhtar, S.; Khan, S.Q.; Ali, S.; Rahoma, A.M. Repair Bond Strength of Conventionally and Digitally Fabricated Denture Base Resins to Auto-Polymerized Acrylic Resin: Surface Treatment Effects In Vitro. Materials 2022, 15, 9062. [Google Scholar] [CrossRef] [PubMed]
- Kizilirmak, B.; Tunçdemİr, A.R. The effect of gastric acid on the bonding of 3D printed and CAD/CAM denture acrylics to denture teeth. Sci. Rep. 2025, 15, 16648. [Google Scholar] [CrossRef] [PubMed]
- Montenbruck, L.; Lüchtenborg, J.; Elgezawi, M.; Keßler, A.; Kaisarly, D. Influence of pretreatment strategies on the tensile bond strength of 3D printed composite resins for definitive cementation to dentin. J. Prosthet. Dent. 2025. [Google Scholar] [CrossRef] [PubMed]
| Fabrication Method | Material (Product Name, Manufacturer) | Code | Composition |
|---|---|---|---|
| Subtractive milling | Feldspar ceramic (VITABLOC Mark II, VITA Zahnfabrik) | VM | SiO2, Al2O3, Na2O, K2O, CaO, TiO2 |
| Polymer-infiltrated ceramic network (VITA Enamic, VITA Zahnfabrik) | VE | UDMA, TEGDMA, glass ceramic sintered network (SiO2, Al2O3, Na2O, K2O, B2O3, ZrO2, CaO) | |
| Nanohybrid resin composite (Grandio Blocs, VOCO GmbH) | GB | UDMA, DMA Dimethacrylates, glass ceramics, silica | |
| 3D printing | Methacrylic acid ester-based resin (Crown Permanent, Formlabs GmbH) | CP | Bis-EMA, salinized glass |
| Source of Variation | df | Sum of Squares | Mean Square | F-Value | p-Value |
|---|---|---|---|---|---|
| Between Groups | 4 | 509.738 | 127.435 | 12.283 | <0.001 |
| Residual | 45 | 466.859 | 10.375 | ||
| Total | 49 | 976.597 |
| Material | Mean ± St. Dev. (MPa) |
|---|---|
| VM | 30.3 ± 1.8 a |
| CPs | 25.2 ± 3.8 b |
| GB | 24.5 ± 3.3 bc |
| CP | 23.0 ± 3.8 bc |
| VE | 20.6 ± 3.0 c |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vichi, A.; Al-Johani, H.; Balestra, D.; Louca, C. Comparison Between Bond Strengths of a Resin Cement on Traditional Prosthetic Substrates and a 3D-Printed Resin for Permanent Restorations. Coatings 2025, 15, 896. https://doi.org/10.3390/coatings15080896
Vichi A, Al-Johani H, Balestra D, Louca C. Comparison Between Bond Strengths of a Resin Cement on Traditional Prosthetic Substrates and a 3D-Printed Resin for Permanent Restorations. Coatings. 2025; 15(8):896. https://doi.org/10.3390/coatings15080896
Chicago/Turabian StyleVichi, Alessandro, Hanan Al-Johani, Dario Balestra, and Chris Louca. 2025. "Comparison Between Bond Strengths of a Resin Cement on Traditional Prosthetic Substrates and a 3D-Printed Resin for Permanent Restorations" Coatings 15, no. 8: 896. https://doi.org/10.3390/coatings15080896
APA StyleVichi, A., Al-Johani, H., Balestra, D., & Louca, C. (2025). Comparison Between Bond Strengths of a Resin Cement on Traditional Prosthetic Substrates and a 3D-Printed Resin for Permanent Restorations. Coatings, 15(8), 896. https://doi.org/10.3390/coatings15080896







