Factors Influencing Marginal Bone Loss around Dental Implants: A Narrative Review
Abstract
1. Introduction
2. Causes of Bone Loss around the Dental Implant
3. Material Properties
3.1. Titanium
3.2. Zirconium
4. Types of Implants
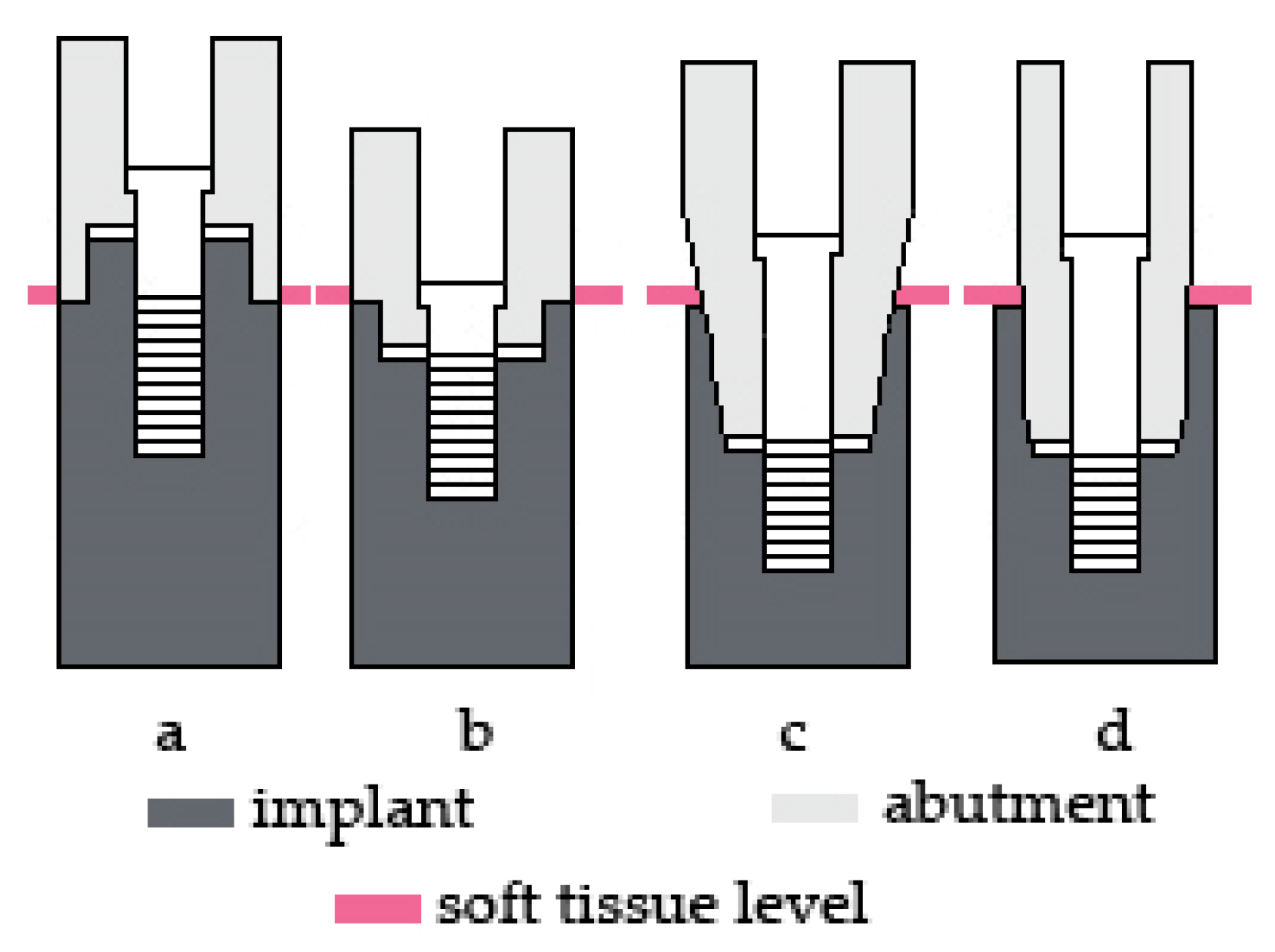
5. Location of Implant-Abutment Connection in Relation to the Bone Level
5.1. Subcrestal Implants
5.2. Bone-Level Implants
5.3. Tissue-Level Implants
5.4. Platform-Switching Concept
6. Types of Implant-Abutment Connections
6.1. External Connection
6.2. Internal Connection
6.3. Conical Connection
6.4. Tube-in-Tube Connection
7. Microgap between the Abutment and Implant
8. Implant Abutment for Cemented and Screwed Prosthetic Restorations
8.1. Abutments for Cemented Implant-Supported Restorations
8.2. Abutments for Screwed Implant-Supported Restorations
9. Implant and Abutment Surface at the Transmucosal Level—Their Influence on Peri-Implant Soft Tissue
10. Biological Aspect of Implant-Abutment Connection
10.1. Biological Width
10.2. Emergence Profile
11. Summary
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Moraschini, V.; Poubel, L.A.D.C.; Ferreira, V.F.; Barboza, E.D.S.P. Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: A systematic review. Int. J. Oral Maxillofac. Surg. 2015, 44, 377–388. [Google Scholar] [CrossRef]
- Gómez-de Diego, R.; Mang-de la Rosa, M.D.R.; Romero-Pérez, M.J.; Cutando-Soriano, A.; López-Valverde-centeno, A. Indications and contraindications of dental implants in medically compromised patients: Update. Med. Oral Patol. Oral Cir. Bucal 2014, 19, e483–e489. [Google Scholar] [CrossRef] [PubMed]
- Duttenhoefer, F.; Fuessinger, M.A.; Beckmann, Y.; Schmelzeisen, R.; Groetz, K.A.; Boeker, M. Dental implants in immunocompromised patients: A systematic review and meta-analysis. Int. J. Implant Dent. 2019, 5. [Google Scholar] [CrossRef] [PubMed]
- Ramesh, M.; Arun, R.; Priyadharshini, I. Journal of advanced medical and dental sciences research. J. Adv. Med. Dent. Sci. Res. 2018, 6, 129–133. [Google Scholar] [CrossRef]
- Raikar, S.; Talukdar, P.; Kumari, S.; Panda, S.; Oommen, V.; Prasad, A. Factors affecting the survival rate of dental implants: A retrospective study. J. Int. Soc. Prev. Community Dent. 2017, 7, 351. [Google Scholar] [CrossRef]
- Turri, A.; Rossetti, P.; Canullo, L.; Grusovin, M.; Dahlin, C. Prevalence of peri-implantitis in medically compromised patients and smokers: A systematic review. Int. J. Oral Maxillofac. Implants 2016, 31, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Parihar, A.; Madhuri, S.; Devanna, R.; Sharma, G.; Singh, R.; Shetty, K. Assessment of failure rate of dental implants in medically compromised patients. J. Fam. Med. Prim. Care 2020, 9, 883. [Google Scholar] [CrossRef]
- Donos, N.; Calciolari, E. Dental implants in patients affected by systemic diseases. Br. Dent. J. 2014, 217, 425–430. [Google Scholar] [CrossRef]
- Singh, R.; Parihar, A.; Vaibhav, V.; Kumar, K.; Singh, R.; Jerry, J. A 10 years retrospective study of assessment of prevalence and risk factors of dental implants failures. J. Fam. Med. Prim. Care 2020, 9, 1617. [Google Scholar] [CrossRef]
- Oswal, M.M.; Amasi, U.N.; Oswal, M.S.; Bhagat, A.S. Influence of three different implant thread designs on stress distribution: A three-dimensional finite element analysis. J. Indian Prosthodont. Soc. 2016, 16, 359–365. [Google Scholar] [CrossRef]
- Esposito, M.; Hirsch, J.M.; Lekholm, U.; Thomsen, P. Biological factors contributing to failures of osseointegrated oral implants. (I). Success criteria and epidemiology. Eur. J. Oral Sci. 1998, 106, 527–551. [Google Scholar] [CrossRef]
- Naveau, A.; Shinmyouzu, K.; Moore, C.; Avivi-Arber, L.; Jokerst, J.; Koka, S. Etiology and measurement of peri-implant crestal bone loss (CBL). J. Clin. Med. 2019, 8, 166. [Google Scholar] [CrossRef]
- Baggi, L.; Cappelloni, I.; Di Girolamo, M.; Maceri, F.; Vairo, G. The influence of implant diameter and length on stress distribution of osseointegrated implants related to crestal bone geometry: A three-dimensional finite element analysis. J. Prosthet. Dent. 2008, 100, 422–431. [Google Scholar] [CrossRef]
- Winkler, S.; Morris, H.F.; Ochi, S. Implant survival to 36 months as related to length and diameter. Ann. Periodontol. 2000, 5, 22–31. [Google Scholar] [CrossRef]
- Chung, D.M.; Oh, T.J.; Lee, J.; Misch, C.E.; Wang, H.L. Factors affecting late implant bone loss: A retrospective analysis. J. Prosthet. Dent. 2007, 98, 215. [Google Scholar] [CrossRef]
- Monje, A.; Suarez, F.; Galindo-Moreno, P.; García-Nogales, A.; Fu, J.H.; Wang, H.L. A systematic review on marginal bone loss around short dental implants (<10 mm) for implant-supported fixed prostheses. Clin. Oral Implants Res. 2014, 25, 1119–1124. [Google Scholar] [CrossRef]
- Eazhil, R.; Swaminathan, S.; Gunaseelan, M.; Kannan, G.; Alagesan, C. Impact of implant diameter and length on stress distribution in osseointegrated implants: A 3D FEA study. J. Int. Soc. Prev. Community Dent. 2016, 6, 590–596. [Google Scholar] [CrossRef]
- Broggini, N.; McManus, L.M.; Hermann, J.S.; Medina, R.; Schenk, R.K.; Buser, D.; Cochran, D.L. Peri-implant inflammation defined by the implant-abutment interface. J. Dent. Res. 2006, 85, 473–478. [Google Scholar] [CrossRef]
- Lekholm, U.; Zarb, G. Patient selection and preparation. In Tissue Integrated Prostheses: Osseointegration in Clinical Dentistry; Branemark, P.-I., Zarb, G., Alberktsson, T., Eds.; Quintessence Publishing Company: Chicago, IL, USA, 1985; pp. 199–209. ISBN 0867151293. [Google Scholar]
- Abrahamsson, I.; Berglundh, T. Effects of different implant surfaces and designs on marginal bone-level alterations: A review. Clin. Oral Implants Res. 2009, 20, 207–215. [Google Scholar] [CrossRef]
- Li, J.; Yin, X.; Huang, L.; Mouraret, S.; Brunski, J.B.; Cordova, L.; Salmon, B.; Helms, J.A. Relationships among bone quality, implant osseointegration, and wnt signaling. J. Dent. Res. 2017, 96, 822–831. [Google Scholar] [CrossRef]
- Güven, S.S.; Cabbar, F.; Güler, N. Local and systemic factors associated with marginal bone loss around dental implants: A retrospective clinical study. Quintessence Int. 2020, 51, 128–141. [Google Scholar] [CrossRef]
- Eshkol-Yogev, I.; Tandlich, M.; Shapira, L. Effect of implant neck design on primary and secondary implant stability in the posterior maxilla: A prospective randomized controlled study. Clin. Oral Implants Res. 2019, 30, 1220–1228. [Google Scholar] [CrossRef] [PubMed]
- Prathapachandran, J.; Suresh, N. Management of peri-implantitis. Dent. Res. J. 2012, 9, 516. [Google Scholar] [CrossRef] [PubMed]
- Koo, K.T.; Khoury, F.; Leander Keeve, P.; Schwarz, F.; Ramanauskaite, A.; Sculean, A.; Romanos, G. Implant surface decontamination by surgical treatment of periimplantitis: A literature review. Implant Dent. 2019, 28, 173–176. [Google Scholar] [CrossRef] [PubMed]
- Hanif, A.; Qureshi, S.; Sheikh, Z.; Rashid, H. Complications in implant dentistry. Eur. J. Dent. 2017, 11, 135–140. [Google Scholar] [CrossRef]
- Rashid, H.; Sheikh, Z.; Vohra, F.; Hanif, A.; Glogauer, M. Peri-implantitis: A review of the disease and report of a case treated with allograft to achieve bone regeneration. Dent. Open J. 2015, 2, 87–97. [Google Scholar] [CrossRef]
- Roca-Millan, E.; Estrugo-Devesa, A.; Merlos, A.; Jané-Salas, E.; Vinuesa, T.; López-López, J. Systemic antibiotic prophylaxis to reduce early implant failure: A systematic review and meta-analysis. Antibiotics 2021, 10, 698. [Google Scholar] [CrossRef]
- Annibali, S.; Ripari, M.; LA Monaca, G.; Tonoli, F.; Cristalli, M.P. Local complications in dental implant surgery: Prevention and treatment. Oral Implantol. 2008, 1, 21–33. [Google Scholar]
- Shafie, H.R.; White, B.A. Implant Abutment Materials. In Clinical and Laboratory Manual of Dental Implant Abutments; John Wiley & Sons, Ltd.: Oxford, UK, 2014; pp. 1–16. [Google Scholar]
- Lim, J.Y.; Liu, X.; Vogler, E.A.; Donahue, H.J. Systematic variation in osteoblast adhesion and phenotype with substratum surface characteristics. J. Biomed. Mater. Res. Part A 2004, 68, 504–512. [Google Scholar] [CrossRef]
- Mehl, C.; Gaβling, V.; Schultz-Langerhans, S.; Açil, Y.; Bähr, T.; Wiltfang, J.; Kern, M. Influence of four different abutment materials and the adhesive joint of two-piece abutments on cervical implant bone and soft tissue. Int. J. Oral Maxillofac. Implants 2016, 31, 1264–1272. [Google Scholar] [CrossRef]
- Welander, M.; Abrahamsson, I.; Berglundh, T. The mucosal barrier at implant abutments of different materials. Clin. Oral Implants Res. 2008, 19, 635–641. [Google Scholar] [CrossRef]
- Sailer, I.; Philipp, A.; Zembic, A.; Pjetursson, B.E.; Hämmerle, C.H.F.; Zwahlen, M. A systematic review of the performance of ceramic and metal implant abutments supporting fixed implant reconstructions. Clin. Oral Implants Res. 2009, 20, 4–31. [Google Scholar] [CrossRef]
- Osman, R.B.; Swain, M.V. A critical review of dental implant materials with an emphasis on titanium versus zirconia. Materials 2015, 8, 932–958. [Google Scholar] [CrossRef]
- Spies, B.C.; Sauter, C.; Wolkewitz, M.; Kohal, R.J. Alumina reinforced zirconia implants: Effects of cyclic loading and abutment modification on fracture resistance. Dent. Mater. 2015, 31, 262–272. [Google Scholar] [CrossRef] [PubMed]
- Bharate, V.; Kumar, Y.; Koli, D.; Pruthi, G.; Jain, V. Effect of different abutment materials (zirconia or titanium) on the crestal bone height in 1 year: Bone loss with implant abutment materials. J. Oral Biol. Craniofacial Res. 2020, 10, 372–374. [Google Scholar] [CrossRef]
- Baldassarri, M.; Hjerppe, J.; Romeo, D.; Fickl, S.; Thompson, V.P.; Stappert, C.F.J. Marginal accuracy of three implant-ceramic abutment configurations. Int. J. Oral Maxillofac. Implants 2012, 27, 537–543. [Google Scholar] [PubMed]
- Cavusoglu, Y.; Akça, K.; Gürbüz, R.; Cavit Cehreli, M. A pilot study of joint stability at the zirconium or titanium abutment/titanium implant interface. Int. J. Oral Maxillofac. Implants 2014, 29, 338–343. [Google Scholar] [CrossRef]
- Prithviraj, D.R.; Gupta, V.; Muley, N.; Sandhu, P. One-piece implants: Placement timing, surgical technique, loading protocol, and marginal bone loss. J. Prosthodont. 2013, 22, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Blank, E.; Grischke, J.; Winkel, A.; Eberhard, J.; Kommerein, N.; Doll, K.; Yang, I.; Stiesch, M. Evaluation of biofilm colonization on multi-part dental implants in a rat model. BMC Oral Health 2021, 21. [Google Scholar] [CrossRef]
- Hahn, J.A. Clinical and radiographic evaluation of one-piece implants used for immediate function. J. Oral Implantol. 2007, 33, 152–155. [Google Scholar] [CrossRef]
- Östman, P.O.; Hellman, M.; Albrektsson, T.; Sennerby, L. Direct loading of Nobel Direct® and Nobel Perfect® one-piece implants: A 1-year prospective clinical and radiographic study. Clin. Oral Implants Res. 2007, 18, 409–418. [Google Scholar] [CrossRef]
- Dorkhan, M.; Yücel-Lindberg, T.; Hall, J.; Svensäter, G.; Davies, J.R. Adherence of human oral keratinocytes and gingival fibroblasts to nano-structured titanium surfaces. BMC Oral Health 2014, 14, 75. [Google Scholar] [CrossRef]
- Palacios-Garzón, N.; Velasco-Ortega, E.; López-López, J. Bone loss in implants placed at subcrestal and crestal level: A systematic review and meta-analysis. Materials 2019, 12, 154. [Google Scholar] [CrossRef] [PubMed]
- Piattelli, A.; Vrespa, G.; Petrone, G.; Iezzi, G.; Annibali, S.; Scarano, A. Role of the microgap between implant and abutment: A retrospective histologic evaluation in monkeys. J. Periodontol. 2003, 74, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Sasada, Y.; Cochran, D. Implant-abutment connections: A review of biologic consequences and peri-implantitis implications. Int. J. Oral Maxillofac. Implants 2017, 32, 1296–1307. [Google Scholar] [CrossRef] [PubMed]
- Wallner, G.; Rieder, D.; Wichmann, M.; Heckmann, S. Peri-implant bone loss of tissue-level and bone-level implants in the esthetic zone with gingival biotype analysis. Int. J. Oral Maxillofac. Implants 2018, 33, 1119–1125. [Google Scholar] [CrossRef] [PubMed]
- Lopez, M.A.; Bassi, M.A.; Confalone, L.; Gaudio, R.M.; Lombardo, L.; Lauritano, D. Retrospective study on bone-level and soft-Tissue-level cylindrical implants. J. Biol. Regul. Homeost. Agents 2016, 30, 43–48. [Google Scholar] [PubMed]
- Lazzara, R.J.; Porter, S.S. Platform switching: A new concept in implant dentistry for controlling postrestorative crestal bone levels. Int. J. Periodontics Restorative Dent. 2006, 26, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Zandim-Barcelos, D.L.; De Carvalho, G.G.; Sapata, V.M.; Villar, C.C.; Hämmerle, C.; Romito, G.A. Implant-based factor as possible risk for peri-implantitis. Braz. Oral Res. 2019, 33, 1–10. [Google Scholar] [CrossRef] [PubMed]
- DI Girolamo, M.; Calcaterra, R.; DI Gianfilippo, R.; Arcuri, C.; Baggi, L. Bone level changes around platform switching and platform matching implants: A systematic review with meta-analysis. Oral Implantol. 2016, 9, 1–10. [Google Scholar] [CrossRef]
- Yang, T.-C.; Maeda, Y. The biomechanical effect of platform switching on external- and internal-connection implants. Int. J. Oral Maxillofac. Implants 2013, 28, 143–147. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Enkling, N.; Jöhren, P.; Katsoulis, J.; Bayer, S.; Jervøe-Storm, P.M.; Mericske-Stern, R.; Jepsen, S. Influence of platform switching on bone-level alterations: A three-year randomized clinical trial. J. Dent. Res. 2013, 92, 139S–145S. [Google Scholar] [CrossRef] [PubMed]
- Farronato, D.; Santoro, G.; Canullo, L.; Botticelli, D.; Maiorana, C.; Lang, N.P. Establishment of the epithelial attachment and connective tissue adaptation to implants installed under the concept of “platform switching”: A histologic study in minipigs. Clin. Oral Implants Res. 2012, 23, 90–94. [Google Scholar] [CrossRef]
- Alonso-González, R.; Aloy-Prósper, A.; Peñarrocha-Oltra, D.; Peñarrocha-Diago, M.A.; Peñarrocha-Diago, M. Marginal bone loss in relation to platform switching implant insertion depth: An update. J. Clin. Exp. Dent. 2012, 4. [Google Scholar] [CrossRef]
- Pita, M.S.; Anchieta, R.B.; Barão, V.A.R.; Garcia, I.R.; Pedrazzi, V.; Assunção, W.G. Prosthetic platforms in implant dentistry. J. Craniofac. Surg. 2011, 22, 2327–2331. [Google Scholar] [CrossRef]
- Brånemark, P.I.; Hansson, B.O.; Adell, R.; Breine, U.; Lindström, J.; Hallén, O.; Ohman, A. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand. J. Plast. Reconstr. Surg. Suppl. 1977, 16, 1–132. [Google Scholar]
- Lorenzoni, F.C.; Coelho, P.G.; Bonfante, G.; Carvalho, R.M.; Silva, N.R.F.A.; Suzuki, M.; Silva, T.L.; Bonfante, E.A. Sealing capability and SEM observation of the implant-abutment interface. Int. J. Dent. 2011, 2011. [Google Scholar] [CrossRef] [PubMed]
- D’Ercole, S.; Scarano, A.; Perrotti, V.; Mulatinho, J.; Piattelli, A.; Iezzi, G.; Tripodi, D. Implants with internal hexagon and conical implant-abutment connections: An in vitro study of the bacterial contamination. J. Oral Implantol. 2014, 40, 31–36. [Google Scholar] [CrossRef]
- Article, R. Evolution of External and internal implant to. Int. J. Oral Implantol. Clin. Res. 2012, 3, 122–129. [Google Scholar] [CrossRef]
- Gaviria, L.; Salcido, J.P.; Guda, T.; Ong, J.L. Current trends in dental implants. J. Korean Assoc. Oral Maxillofac. Surg. 2014, 40, 50. [Google Scholar] [CrossRef] [PubMed]
- Nicolas-Silvente, A.I.; Velasco-Ortega, E.; Ortiz-Garcia, I.; Jimenez-Guerra, A.; Monsalve-Guil, L.; Ayuso-Montero, R.; Gil, J.; Lopez-Lopez, J. Influence of connection type and platform diameter on titanium dental implants fatigue: Non-axial loading cyclic test analysis. Int. J. Environ. Res. Public Health 2020, 17, 8988. [Google Scholar] [CrossRef] [PubMed]
- Tsuge, T.; Hagiwara, Y.; Matsumura, H. Marginal fit and microgaps of implant-abutment interface with internal anti-rotation configuration. Dent. Mater. J. 2008, 27, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Asvanund, P.; Morgano, S.M. Photoelastic stress analysis of external versus internal implant-abutment connections. J. Prosthet. Dent. 2011, 106, 266–271. [Google Scholar] [CrossRef]
- Black, D.L.; Turkyilmaz, I.; Lien, W.; Chong, C.H. Evaluation of the sealing capability of the internal conical connections of implants with titanium and zirconia abutments. J. Contemp. Dent. Pract. 2017, 18, 915–922. [Google Scholar] [CrossRef]
- Macedo, J.P.; Pereira, J.; Vahey, B.R.; Henriques, B.; Benfatti, C.A.M.; Magini, R.S.; López-López, J.; Souza, J.C.M. Morse taper dental implants and platform switching: The new paradigm in oral implantology. Eur. J. Dent. 2016, 10, 148–154. [Google Scholar] [CrossRef]
- Gil, F.J.; Herrero-Climent, M.; Lázaro, P.; Rios, J.V. Implant-abutment connections: Influence of the design on the microgap and their fatigue and fracture behavior of dental implants. J. Mater. Sci. Mater. Med. 2014, 25, 1825–1830. [Google Scholar] [CrossRef]
- Schmitt, C.M.; Nogueira-Filho, G.; Tenenbaum, H.C.; Lai, J.Y.; Brito, C.; Döring, H.; Nonhoff, J. Performance of conical abutment (Morse Taper) connection implants: A systematic review. J. Biomed. Mater. Res. Part A 2014, 102, 552–574. [Google Scholar] [CrossRef]
- Ceruso, F.M.; Barnaba, P.; Mazzoleni, S.; Ottria, L.; Gargari, M.; Zuccon, A.; Bruno, G.; Di Fiore, A. Implant-abutment connections on single crowns: A systematic review. ORAL Implantol. 2017, 10, 349–353. [Google Scholar] [CrossRef]
- Steinebrunner, L.; Wolfart, S.; Ludwig, K.; Kern, M. Implant-abutment interface design affects fatigue and fracture strength of implants. Clin. Oral Implants Res. 2008, 19, 1276–1284. [Google Scholar] [CrossRef]
- Balik, A.; Karatas, M.O.; Keskin, H. Effects of different abutment connection designs on the stress distribution around five different implants: A 3-dimensional finite element analysis. J. Oral Implantol. 2012, 38, 491–496. [Google Scholar] [CrossRef]
- Nassar, H.I.; Abdalla, M.F. Bacterial leakage of different internal implant/abutment connection. Futur. Dent. J. 2015, 1, 1–5. [Google Scholar] [CrossRef]
- Souza, A.B.; Alshihri, A.M.; Kämmerer, P.W.; Araújo, M.G.; Gallucci, G.O. Histological and micro-CT analysis of peri-implant soft and hard tissue healing on implants with different healing abutments configurations. Clin. Oral Implants Res. 2018, 29, 1007–1015. [Google Scholar] [CrossRef]
- Kano, S.C.; Binon, P.P.; Curtis, D.A. A classification system to measure the implant-abutment microgap. Int. J. Oral Maxillofac. Implants 2007, 22, 879–885. [Google Scholar]
- Kofron, M.D.; Carstens, M.; Fu, C.; Wen, H.B. In vitro assessment of connection strength and stability of internal implant-abutment connections. Clin. Biomech. 2019, 65, 92–99. [Google Scholar] [CrossRef]
- Assenza, B.; Tripodi, D.; Scarano, A.; Perrotti, V.; Piattelli, A.; Iezzi, G.; D’Ercole, S. Bacterial leakage in implants with different implant–abutment connections: An In Vitro Study. J. Periodontol. 2012, 83, 491–497. [Google Scholar] [CrossRef]
- He, Y.; Fok, A.; Aparicio, C.; Teng, W. Contact analysis of gap formation at dental implant-abutment interface under oblique loading: A numerical-experimental study. Clin. Implant Dent. Relat. Res. 2019, 21, 741–752. [Google Scholar] [CrossRef]
- Hermann, J.S.; Schoolfield, J.D.; Schenk, R.K.; Buser, D.; Cochran, D.L. Influence of the size of the microgap on crestal bone changes around titanium implants. A histometric evaluation of unloaded non-submerged implants in the canine mandible. J. Periodontol. 2001, 72, 1372–1383. [Google Scholar] [CrossRef]
- Molinero-Mourelle, P.; Cascos-Sanchez, R.; Yilmaz, B.; Lam, W.Y.H.; Pow, E.H.N.; Del Río Highsmith, J.; Gómez-Polo, M. Effect of fabrication technique on the microgap of CAD/CAM cobalt-chrome and zirconia abutments on a conical connection implant: An in vitro study. Materials 2021, 14, 2348. [Google Scholar] [CrossRef]
- Shadid, R.; Sadaqa, N. A comparison between screw-and cement-retained implant prostheses. A literature review. J. Oral Implantol. 2012, 38, 298–307. [Google Scholar] [CrossRef]
- Linkevicius, T.; Vindasiute, E.; Puisys, A.; Peciuliene, V. The influence of margin location on the amount of undetected cement excess after delivery of cement-retained implant restorations. Clin. Oral Implants Res. 2011, 22, 1379–1384. [Google Scholar] [CrossRef]
- Shi, J.Y.; Ni, J.; Zhuang, L.F.; Zhang, X.M.; Fan, L.F.; Lai, H.C. Peri-implant conditions and marginal bone loss around cemented and screw-retained single implant crowns in posterior regions: A retrospective cohort study with up to 4 years follow-up. PLoS ONE 2018, 13, e0191717. [Google Scholar] [CrossRef]
- Heo, Y.-K.; Lim, Y.-J. A newly designed screw- and cement-retained prosthesis and its abutments. Int. J. Prosthodont. 2015, 28, 612–614. [Google Scholar] [CrossRef]
- Kim, S.G.; Chung, C.H.; Son, M.K. Effect of cement washout on loosening of abutment screws and vice versa in screw- and cement- retained implant-supported dental prosthesis. J. Adv. Prosthodont. 2015, 7, 207–213. [Google Scholar] [CrossRef]
- Kano, S.C.; Binon, P.; Bonfante, G.; Curtis, D.A. Effect of casting procedures on screw loosening in UCLA-type abutments. J. Prosthodont. 2006, 15, 77–81. [Google Scholar] [CrossRef]
- Kourtis, S.; Damanaki, M.; Kaitatzidou, S.; Kaitatzidou, A.; Roussou, V. Loosening of the fixing screw in single implant crowns: Predisposing factors, prevention and treatment options. J. Esthet. Restor. Dent. 2017, 29, 233–246. [Google Scholar] [CrossRef]
- Abdelhamed, M.I.; Galley, J.D.; Bailey, M.T.; Johnston, W.M.; Holloway, J.; Mcglumphy, E.; Leblebicioglu, B. A comparison of zirconia and titanium abutments for microleakage. Clin. Implant Dent. Relat. Res. 2015, 17, e643–e651. [Google Scholar] [CrossRef]
- Ongun, S.; Kurtulmus-Yilmaz, S.; Meriç, G.; Ulusoy, M. A comparative study on the mechanical properties of a polymer-infiltrated ceramic-network material used for the fabrication of hybrid abutment. Materials 2018, 11, 1681. [Google Scholar] [CrossRef]
- Agustín-Panadero, R.; Bustamante-Hernández, N.; Labaig-Rueda, C.; Fons-Font, A.; Fernández-Estevan, L.; Solá-Ruíz, M.F. Influence of biologically oriented preparation technique on peri-implant tissues; prospective randomized clinical trial with three-year follow-up. Part II: Soft tissues. J. Clin. Med. 2019, 8, 2223. [Google Scholar] [CrossRef]
- Mangano, F.; Margiani, B.; Admakin, O. A novel full-digital protocol (SCAN-PLAN-MAKE-DONE®) for the design and fabrication of implant-supported monolithic translucent zirconia crowns cemented on customized hybrid abutments: A retrospective clinical study on 25 patients. Int. J. Environ. Res. Public Health 2019, 16, 317. [Google Scholar] [CrossRef]
- Cervino, G.; Fiorillo, L.; Iannello, G.; Santonocito, D.; Risitano, G.; Cicciù, M. Sandblasted and acid etched titanium dental implant surfaces systematic review and confocal microscopy evaluation. Materials 2019, 12, 1763. [Google Scholar] [CrossRef]
- Nothdurft, F.P.; Fontana, D.; Ruppenthal, S.; May, A.; Aktas, C.; Mehraein, Y.; Lipp, P.; Kaestner, L. Differential behavior of fibroblasts and epithelial cells on structured implant abutment materials: A comparison of materials and surface topographies. Clin. Implant Dent. Relat. Res. 2015, 17, 1237–1249. [Google Scholar] [CrossRef]
- Elias, C.N.; Oshida, Y.; Lima, J.H.C.; Muller, C.A. Relationship between surface properties (roughness, wettability and morphology) of titanium and dental implant removal torque. J. Mech. Behav. Biomed. Mater. 2008, 1, 234–242. [Google Scholar] [CrossRef]
- da Cruz, M.B.; Marques, J.F.; Fernandes, B.F.; Costa, M.; Miranda, G.; da Mata, A.D.S.P.; Carames, J.M.M.; Silva, F.S. Gingival fibroblasts behavior on bioactive zirconia and titanium dental implant surfaces produced by a functionally graded technique. J. Appl. Oral Sci. 2020, 28, 1–10. [Google Scholar] [CrossRef]
- Nicolas-Silvente, A.I.; Velasco-Ortega, E.; Ortiz-Garcia, I.; Monsalve-Guil, L.; Gil, J.; Jimenez-Guerra, A. Influence of the titanium implant surface treatment on the surface roughness and chemical composition. Materials 2020, 13, 314. [Google Scholar] [CrossRef]
- Del Fabbro, M.; Taschieri, S.; Canciani, E.; Addis, A.; Musto, F.; Weinstein, R.; Dellavia, C. Osseointegration of titanium implants with different rough surfaces: A histologic and histomorphometric study in an adult minipig model. Implant Dent. 2017, 26, 357–366. [Google Scholar] [CrossRef]
- Albrektsson, T.; Wennerberg, A. Oral implant surfaces: Part 1--review focusing on topographic and chemical properties of different surfaces and in vivo responses to them. Int. J. Prosthodont. 2004, 17, 536–543. [Google Scholar] [PubMed]
- Naves, M.; Menezes, H.; Magalhães, D.; Ferreira, J.; Ribeiro, S.; de Mello, J.; Costa, H. Effect of macrogeometry on the surface topography of dental implants. Int. J. Oral Maxillofac. Implants 2015, 30, 789–799. [Google Scholar] [CrossRef]
- Al-Nawas, B.; Götz, H. Three-dimensional topographic and metrologic evaluation of dental implants by confocal laser scanning microscopy. Clin. Implant Dent. Relat. Res. 2003, 5, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Gehrke, P.; Tabellion, A.; Fischer, C. Microscopical and chemical surface characterization of CAD/CAM zircona abutments after different cleaning procedures. A qualitative analysis. J. Adv. Prosthodont. 2015, 7, 151. [Google Scholar] [CrossRef] [PubMed]
- Canullo, L.; Menini, M.; Santori, G.; Rakic, M.; Sculean, A.; Pesce, P. Titanium abutment surface modifications and peri-implant tissue behavior: A systematic review and meta-analysis. Clin. Oral Investig. 2020, 24, 1113–1124. [Google Scholar] [CrossRef]
- Blázquez-Hinarejos, M.; Ayuso-Montero, R.; Álvarez-López, J.M.; Manzanares-Céspedes, M.C.; López-López, J. Histological differences in the adherence of connective tissue to laser-treated abutments and standard abutments for dental implants. An experimental pilot study in humans. Med. Oral Patol. Oral Cir. Bucal 2017, 22, e774–e779. [Google Scholar] [CrossRef]
- Ivanovski, S.; Lee, R. Comparison of peri-implant and periodontal marginal soft tissues in health and disease. Periodontology 2000 2018, 76, 116–130. [Google Scholar] [CrossRef]
- Sanz-Martín, I.; Sanz-Sánchez, I.; Carrillo de Albornoz, A.; Figuero, E.; Sanz, M. Effects of modified abutment characteristics on peri-implant soft tissue health: A systematic review and meta-analysis. Clin. Oral Implants Res. 2018, 29, 118–129. [Google Scholar] [CrossRef]
- Canullo, L.; Pesce, P.; Patini, R.; Antonacci, D.; Tommasato, G. What are the effects of different abutment morphologies on peri-implant hard and soft tissue behavior? A systematic review and meta-analysis. Int. J. Prosthodont. 2020, 33, 297–306. [Google Scholar] [CrossRef]
- Montemezzi, P.; Ferrini, F.; Pantaleo, G.; Gherlone, E.; Capparè, P. Dental implants with different neck design: A prospective clinical comparative study with 2-year follow-up. Materials 2020, 13, 1029. [Google Scholar] [CrossRef]
- Hung, K.Y.; Lin, Y.C.; Feng, H.P. The effects of acid etching on the nanomorphological surface characteristics and activation energy of titanium medical materials. Materials 2017, 10, 1164. [Google Scholar] [CrossRef]
- Canullo, L.; Annunziata, M.; Pesce, P.; Tommasato, G.; Nastri, L.; Guida, L. Influence of abutment material and modifications on peri-implant soft-tissue attachment: A systematic review and meta-analysis of histological animal studies. J. Prosthet. Dent. 2020, 1–11. [Google Scholar] [CrossRef]
- Schwarz, F.; Ferrari, D.; Herten, M.; Mihatovic, I.; Wieland, M.; Sager, M.; Becker, J. Effects of surface hydrophilicity and microtopography on early stages of soft and hard tissue integration at non-submerged titanium implants: An immunohistochemical study in dogs. J. Periodontol. 2007, 78, 2171–2184. [Google Scholar] [CrossRef]
- Guarnieri, R.; Serra, M.; Bava, L.; Grande, M.; Farronato, D.; Iorio-Siciliano, V. The impact of a laser-microtextured collar on crestal bone level and clinical parameters under various placement and loading protocols. Int. J. Oral Maxillofac. Implants 2014, 29, 354–363. [Google Scholar] [CrossRef]
- Nicholson, J.W. Titanium Alloys for Dental Implants: A Review. Prosthesis 2020, 2, 100–116. [Google Scholar] [CrossRef]
- Aloy-Prósper, A.; Maestre-Ferrín, L.; Peñarrocha-Oltra, D.; Peñarrocha-Diago, M. Marginal bone loss in relation to the implant neck surface: An update. Med. Oral Patol. Oral Cir. Bucal 2011, 16, 365–368. [Google Scholar] [CrossRef]
- Zitzmann, N.U.; Abrahamsson, I.; Berglundh, T.; Lindhe, J. Soft tissue reactions to plaque formation at implant abutments with different surface topography: An experimental study in dogs. J. Clin. Periodontol. 2002, 29, 456–461. [Google Scholar] [CrossRef]
- Manicone, P.F.; Raffaelli, L.; Ghassemian, M.; D’Addona, A. Soft and hard tissue management in implant therapy—Part II: Prosthetic concepts. Int. J. Biomater. 2012, 2012, 356817. [Google Scholar] [CrossRef][Green Version]
- Nowzari, H.; Yi, K.; Chee, W.; Rich, S.K. Immunology, microbiology, and virology following placement of NobelPerfectscalloped dental implants: Analysis of a case series. Clin. Implant Dent. Relat. Res. 2008, 10, 157–165. [Google Scholar] [CrossRef]
- Galárraga-Vinueza, M.E.; Tangl, S.; Bianchini, M.; Magini, R.; Obreja, K.; Gruber, R.; Schwarz, F. Histological characteristics of advanced peri-implantitis bone defects in humans. Int. J. Implant Dent. 2020, 6. [Google Scholar] [CrossRef]
- Schminke, B.; Vom Orde, F.; Gruber, R.; Schliephake, H.; Bürgers, R.; Miosge, N. The pathology of bone tissue during peri-implantitis. J. Dent. Res. 2015, 94, 354–361. [Google Scholar] [CrossRef]
- Tumedei, M.; Piattelli, A.; Degidi, M.; Mangano, C.; Iezzi, G. A narrative review of the histological and histomorphometrical evaluation of the peri-implant bone in loaded and unloaded dental implants. A 30-year experience (1988–2018). Int. J. Environ. Res. Public Health 2020, 17, 2088. [Google Scholar] [CrossRef]
- Goracci, C.; Sadek, F.T.; Monticelli, F.; Cardoso, P.E.C.; Ferrari, M. Microtensile bond strength of self-etching adhesives to enamel and dentin. J. Adhes. Dent. 2004, 6, 313–318. [Google Scholar]
- Rodríguez-Ciurana, X.; Vela-Nebot, X.; Segalà-Torres, M.; Rodado-Alonso, C.; Méndez-Blanco, V.; Mata-Bugueroles, M. Biomechanical repercussions of bone resorption related to biologic width: A finite element analysis of three implant-abutment configurations. Int. J. Periodontics Restorative Dent. 2009, 29, 479–487. [Google Scholar] [CrossRef]
- Al Rezk, F.; Trimpou, G.; Lauer, H.-C.; Weigl, P.; Krockow, N. Response of soft tissue to different abutment materials with different surface topographies: A review of the literature. Gen. Dent. 2018, 66, 18–25. [Google Scholar]
- Delgado-Ruiz, R.; Romanos, G. Potential causes of titanium particle and ion release in implant dentistry: A systematic review. Int. J. Mol. Sci. 2018, 19, 3585. [Google Scholar] [CrossRef]
- Molina, A.; Sanz-Sánchez, I.; Martín, C.; Blanco, J.; Sanz, M. The effect of one-time abutment placement on interproximal bone levels and peri-implant soft tissues: A prospective randomized clinical trial. Clin. Oral Implants Res. 2017, 28, 443–452. [Google Scholar] [CrossRef]
- Bressan, E.; Grusovin, M.G.; D’Avenia, F.; Neumann, K.; Sbricoli, L.; Luongo, G.; Esposito, M. The influence of repeated abutment changes on peri-implant tissue stability: 3-year post-loading results from a multicentre randomised controlled trial. Eur. J. Oral Implantol. 2017, 10, 373–390. [Google Scholar]
- Dornbush, J.R.; Reiser, G.M.; Ho, D.K. Platform switching and abutment emergence profile modification on peri-implant soft tissue. Alpha Omegan 2014, 107, 28–32. [Google Scholar]
- Canullo, L.; Pellegrini, G.; Allievi, C.; Trombelli, L.; Annibali, S.; Dellavia, C. Soft tissues around long-term platform switching implant restorations: A histological human evaluation. Preliminary results. J. Clin. Periodontol. 2011, 38, 86–94. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kowalski, J.; Lapinska, B.; Nissan, J.; Lukomska-Szymanska, M. Factors Influencing Marginal Bone Loss around Dental Implants: A Narrative Review. Coatings 2021, 11, 865. https://doi.org/10.3390/coatings11070865
Kowalski J, Lapinska B, Nissan J, Lukomska-Szymanska M. Factors Influencing Marginal Bone Loss around Dental Implants: A Narrative Review. Coatings. 2021; 11(7):865. https://doi.org/10.3390/coatings11070865
Chicago/Turabian StyleKowalski, Jakub, Barbara Lapinska, Joseph Nissan, and Monika Lukomska-Szymanska. 2021. "Factors Influencing Marginal Bone Loss around Dental Implants: A Narrative Review" Coatings 11, no. 7: 865. https://doi.org/10.3390/coatings11070865
APA StyleKowalski, J., Lapinska, B., Nissan, J., & Lukomska-Szymanska, M. (2021). Factors Influencing Marginal Bone Loss around Dental Implants: A Narrative Review. Coatings, 11(7), 865. https://doi.org/10.3390/coatings11070865







