Repair Bond Strength of Composite Resin to Aged Resin and Glass-Matrix CAD/CAM Ceramic Materials Using Two Different Repair Systems
Abstract
:1. Introduction
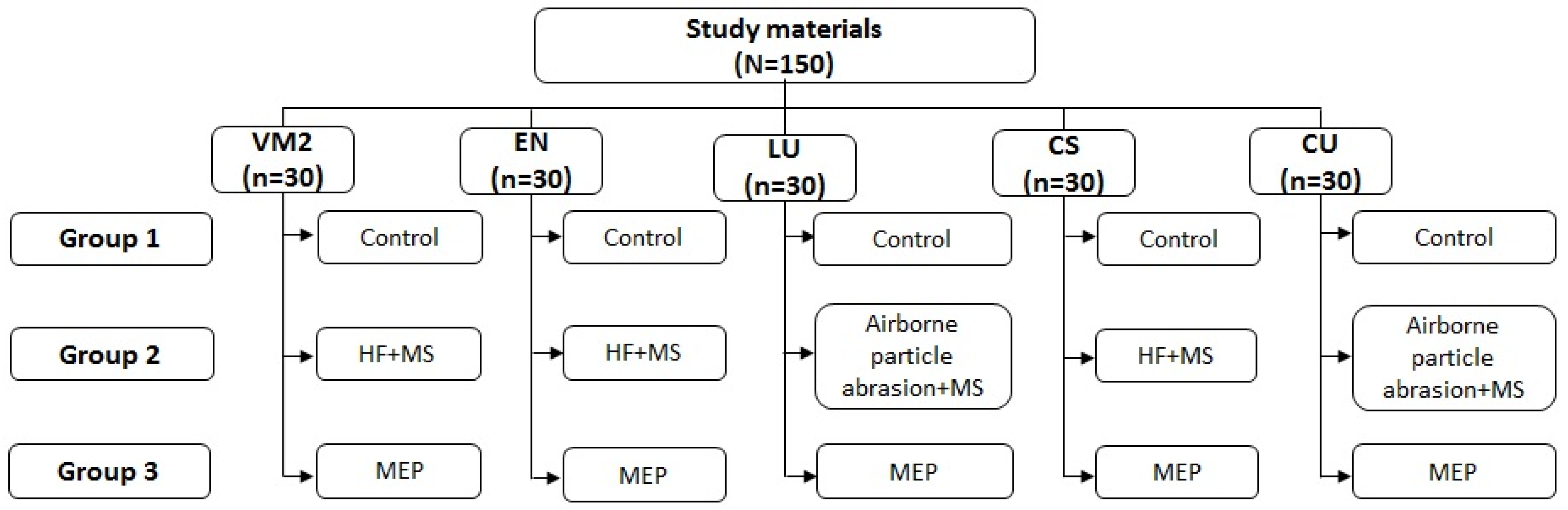
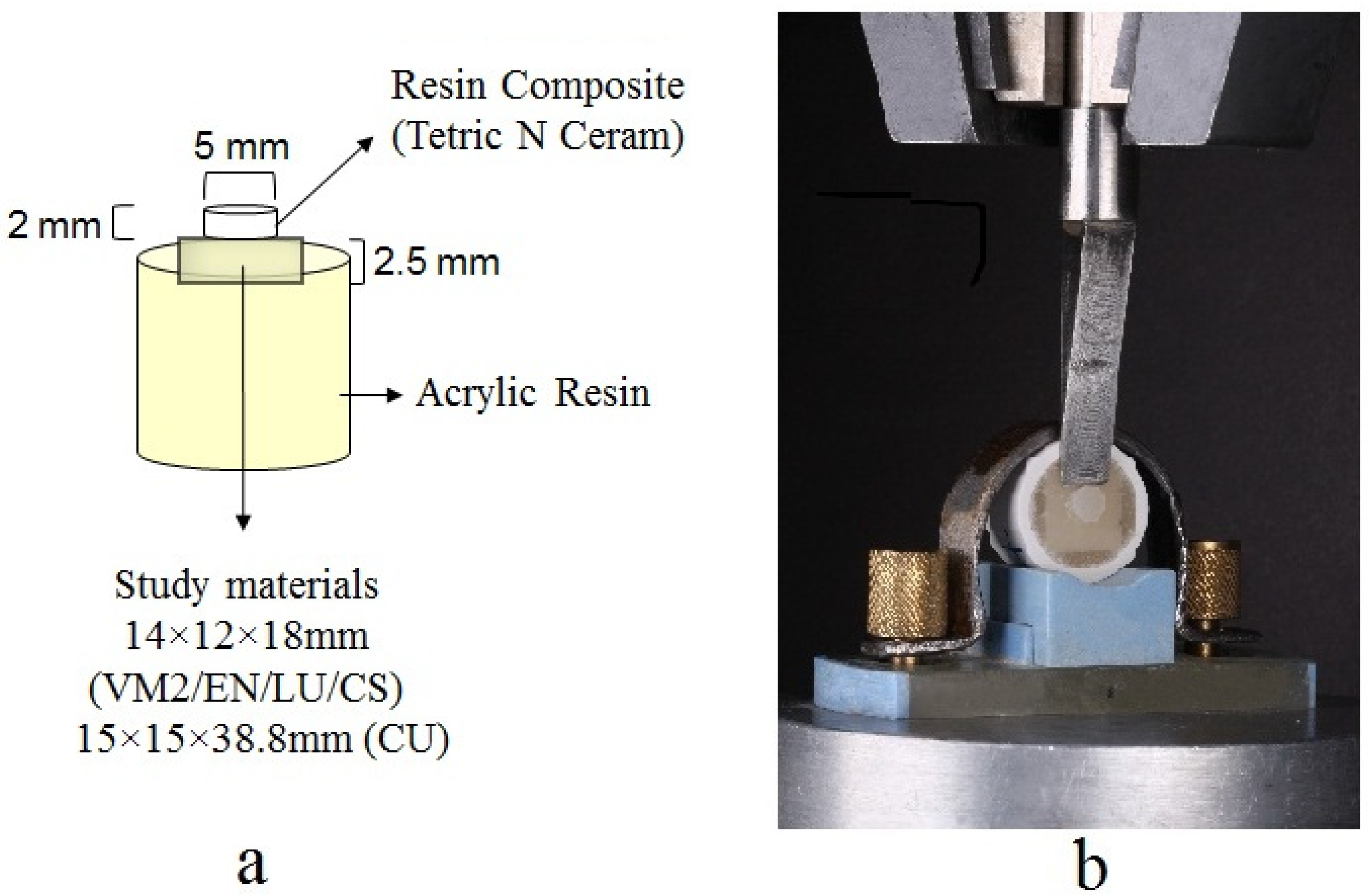
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Nomenclature
| ANOVA | Analysis of variance |
| APF | Aciduated phosphate fluoride |
| BisEMA | Ethoxylated bisphenol A dimethacrylate |
| BISEMPP | Bisphenol A bis (2-hydroxyethyl ether) dimethacrylate |
| BisGMA | bisphenol-A-glycidyldimethacrylate |
| BUDMA | 1,4-butanediol dimethacrylate |
| CAD/CAM | Computer-aided design/Computer-aided manufacturing |
| CS | Cerasmart |
| CU | Crystal Ultra |
| DMA | Dimethacrylate |
| EN | Vita Enamic |
| HF | Hydrofluoric Acid |
| H3PO4 | phosphoric acid |
| ISO | International Organization for Standardization |
| K2O | Potassium oxide |
| MEP | Monobond etch and primer |
| MS | Monobond-S |
| MPa | Megapascal |
| Na2O | Sodium oxide |
| N | Newton |
| SBS | Shear bond strength |
| SEM | Scanning Electron Microscopy |
| SiO2 | Silicon dioxide |
| SPSS | Statistical Package for the Social Sciences |
| TEGDMA | triethyleneglycoldimethacrylate |
| UDMA | Urethane Dimethacrylate |
| VM2 | Vitablocs Mark II |
Appendix A
| Source | Type III Sum of Squares | df | Mean Square | F | * Sig. |
|---|---|---|---|---|---|
| Corrected Model | 8953.94 | 14 | 639.56 | 118.60 | <0.001 |
| Intercept | 37,967.62 | 1 | 37,967.62 | 7040.84 | <0.001 |
| Material | 1191.53 | 4 | 297.88 | 55.24 | <0.001 |
| Repair system | 7327.79 | 2 | 3663.89 | 679.44 | <0.001 |
| Material * Repair system | 434.60 | 8 | 54.32 | 10.07 | <0.001 |
| Error | 727.98 | 135 | 5.39 | - | - |
| Total | 47,649.55 | 150 | - | - | - |
| Corrected Total | 9681.92 | 149 | - | - | - |
References
- Gracis, S.; Thompson, V.P.; Ferencz, J.L.; Silva, N.R.F.A.; Bonfante, E.A. A new classification system for all-ceramic and ceramic-like restorative materials. Int. J. Prosthodont. 2016, 28, 227–235. [Google Scholar] [CrossRef] [Green Version]
- Al Amri, M.D.; Labban, N.; Alhijji, S.; Alamri, H.; Iskandar, M.; Platt, J.A. In vitro evaluation of translucency and color stability of CAD/CAM polymer-infiltrated ceramic materials after accelerated aging. J. Prosthodont. 2020, 30, 318–328. [Google Scholar] [CrossRef]
- Awad, D.; Stawarczyk, B.; Liebermann, A.; Ilie, N. Translucency of esthetic dental restorative CAD/CAM materials and composite resins with respect to thickness and surface roughness. J. Prosthet. Dent. 2015, 113, 534–540. [Google Scholar] [CrossRef] [PubMed]
- Lauvahutanon, S.; Takahashi, H.; Shiozawa, M.; Iwasaki, N.; Asakawa, Y.; Oki, M.; Finger, W.J.; Arksornnukit, M. Mechanical properties of composite resin blocks for CAD/CAM. Dent. Mater. J. 2014, 33, 705–710. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lebon, N.; Tapie, L.; Vennat, E.; Mawussi, B. Influence of CAD/CAM tool and material on tool wear and roughness of dental prostheses after milling. J. Prosthet. Dent. 2015, 114, 236–247. [Google Scholar] [CrossRef]
- Ruse, N.; Sadoun, M. Resin-composite blocks for dental CAD/CAM applications. J. Dent. Res. 2014, 93, 1232–1234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bajraktarova-Valjakova, E.; Korunoska-Stevkovska, V.; Kapusevska, B.; Gigovski, N.; Bajraktarova-Misevska, C.; Grozdanov, A. Contemporary dental ceramic materials, a review: Chemical composition, physical and mechanical properties, indications for use. Open Access Maced. J. Med. Sci. 2018, 6, 1742–1755. [Google Scholar] [CrossRef] [Green Version]
- Della Bona, A.; Corazza, P.H.; Zhang, Y. Characterization of a polymer-infiltrated ceramic-network material. Dent. Mater. 2014, 30, 564–569. [Google Scholar] [CrossRef] [Green Version]
- Reich, S. Tooth-colored CAD/CAM monolithic restorations. Int. J. Comput. Dent. 2015, 18, 131–146. [Google Scholar]
- Goujat, A.; Abouelleil, H.; Colon, P.; Jeannin, C.; Pradelle, N.; Seux, D.; Grosgogeat, B. Mechanical properties and internal fit of 4 CAD-CAM block materials. J. Prosthet. Dent. 2017, 119, 384–389. [Google Scholar] [CrossRef]
- Awada, A.; Nathanson, D. Mechanical properties of resin-ceramic CAD/CAM restorative materials. J. Prosthet. Dent. 2015, 114, 587–593. [Google Scholar] [CrossRef] [PubMed]
- Koller, M.; Arnetzl, G.V.; Holly, L. Lava ultimate resin nano ceramic for CAD/ CAM: Customization case study. Int. J. Comput. Dent. 2012, 15, 159–164. [Google Scholar] [PubMed]
- Blum, I.R.; Jagger, D.C.; Wilson, N.H.F. Defective dental restorations: To repair or not to repair? part 2: All–ceramics and porcelain fused to metal systems. Dent. Updat. 2011, 38, 150–158. [Google Scholar] [CrossRef] [PubMed]
- Kimmich, M.; Stappert, C.F. Intraoral treatment of veneering porcelain chipping of fixed dental restorations: A review and clinical application. J. Am. Dent. Assoc. 2013, 144, 31–44. [Google Scholar] [CrossRef] [Green Version]
- Reston, E.G.; Filho, S.C.; Arossi, G.; Cogo, R.B.; Rocha Cdos, S.; Closs, L.Q. Repairing ceramic restorations: Final solution or alternative procedure? Oper. Dent. 2008, 33, 461–466. [Google Scholar] [CrossRef]
- Özcan, M.; Vallittu, P.K. Effect of surface conditioning methods on the bond strength of luting cement to ceramics. Dent. Mater. 2003, 19, 725–731. [Google Scholar] [CrossRef] [Green Version]
- Elsaka, S.E. Repair bond strength of resin composite to a novel CAD/CAM hybrid ceramic using different repair systems. Dent. Mater. J. 2015, 34, 161–167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bertolini, J.C. Hydrofluoric acid: A review of toxicity. J. Emerg. Med. 1992, 10, 163–168. [Google Scholar] [CrossRef]
- Özcan, M.; Allahbeickaraghi, A.; Dündar, M. Possible hazardous effects of hydrofluoric acid and recommendations for treatment approach: A review. Clin. Oral Investig. 2011, 16, 15–23. [Google Scholar] [CrossRef] [PubMed]
- El-Damanhoury, H.M.; Gaintantzopoulou, M.D. Self-etching ceramic primer versus hydrofluoric acid etching: Etching efficacy and bonding performance. J. Prosthodont. Res. 2018, 62, 75–83. [Google Scholar] [CrossRef]
- Della Bona, A.; Shen, C.; Anusavice, K.J. Work of adhesion of resin on treated lithia disilicate-based ceramic. Dent. Mater. 2004, 20, 338–344. [Google Scholar] [CrossRef]
- Labban, N.; Al Amri, M.; Alhijji, S.; Alnafaiy, S.; Alfouzan, A.; Iskandar, M.; Feitosa, S. Influence of toothbrush abrasion and surface treatments on the color and translucency of resin infiltrated hybrid ceramics. J. Adv. Prosthodont. 2021, 13, 1–11. [Google Scholar] [CrossRef]
- Sarah, A.M.; Nawaf, L.; Ahmed, M.; Huda, A.H.; Abdullah, S.A.; Wejdan, A. Biaxial flexural strength and hardness of resin-matrix ceramic CAD/CAM materials. Ceram.-Silikáty 2021, in press. [Google Scholar] [CrossRef]
- Gul, P.; Altınok-Uygun, L. Repair bond strength of resin composite to three aged CAD/CAM blocks using different repair systems. J. Adv. Prosthodont. 2020, 12, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Stün, Ö.; Büyükhatipoğlu, I.K.; Seçilmiş, A. Shear bond strength of repair systems to new Cad/Cam restorative materials. J. Prosthodont. 2018, 27, 748–754. [Google Scholar]
- Anusavice, K.J. Standardizing failure, success, and survival decisions in clinical studies of ceramic and metal-ceramic fixed dental prostheses. Dent. Mater. 2012, 18, 102–111. [Google Scholar] [CrossRef] [Green Version]
- Khoroushi, M.; Shirban, F.; Shirban, M. Marginal microleakage and morphological characteristics of a solvent-free one-step self-etch adhesive (B1SF). J. Dent. 2013, 10, 32–40. [Google Scholar]
- Morresi, A.L.; D’Amario, M.; Capogreco, M.; Gatto, R.; Marzo, G.; D’Arcangelo, C.; Monaco, A. Thermal cycling for restorative materials: Does a standardized protocol exist in laboratory testing? A literature review. J. Mech. Behav. Biomed. Mater. 2014, 29, 295–308. [Google Scholar] [CrossRef] [PubMed]
- Subaşı, M.G.; Alp, G.; Johnston, W.M.; Yilmaz, B. Effects of fabrication and shading technique on the color and translucency of new-generation translucent zirconia after coffee thermocycling. J. Prosthet. Dent. 2018, 120, 603–608. [Google Scholar] [CrossRef]
- Gale, M.; Darvell, B. Thermal cycling procedures for laboratory testing of dental restorations. J. Dent. 1999, 27, 89–99. [Google Scholar] [CrossRef]
- Ozcan, M.; Niedermeier, W. Clinical study on the reasons for and location of failures of metal-ceramic restorations and survival of repairs. Int. J. Prosthodont. 2002, 15, 299–302. [Google Scholar] [PubMed]
- Szep, S.; Gerhardt, T.; Gockel, H.W.; Ruppel, M.; Metzeltin, D.; Heidemann, D. In vitro dentinal surface reaction of 9.5% buffered hydrofluoric acid in repair of ceramic restorations: A scanning electron microscopic investigation. J. Prosthet. Dent. 2000, 83, 668–674. [Google Scholar] [CrossRef]
- Ozcan, M.; Valandro, L.F.; Amaral, R.; Leite, F.; Bottino, M.A. Bond strength durability of a resin composite on a reinforced ceramic using various repair systems. Dent. Mater. 2009, 25, 1477–1483. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Escobar, M.; Henriques, B.; Fredel, M.C.; Silva, F.S.; Özcan, M.; Souza, J.C. Adhesion of peek to resin-matrix composites used in dentistry: A short review on surface modification and bond strength. J. Adhes. Sci. Technol. 2020, 34, 1241–1252. [Google Scholar] [CrossRef]
- Çulhaoğlu, A.K.; Özkır, S.E.; Şahin, V.; Yılmaz, B.; Kılıçarslan, M.A. Effect of various treatment modalities on surface characteristics and shear bond strengths of polyetheretherketone-based core materials. J. Prosthodont. 2017, 29, 136–141. [Google Scholar] [CrossRef] [PubMed]
- Güngör, M.B.; Nemli, S.K.; Bal, B.T.; Ünver, S.; Doğan, A. Effect of surface treatments on shear bond strength of resin composite bonded to CAD/CAM resin-ceramic hybrid materials. J. Adv. Prosthodont. 2016, 8, 259–266. [Google Scholar] [CrossRef] [Green Version]
- Wiegand, A.; Stucki, L.; Hoffmann, R.; Attin, T.; Stawarczyk, B. Repairability of CAD/CAM high-density PMMA- and composite-based polymers. Clin. Oral Investig. 2015, 19, 2007–2013. [Google Scholar] [CrossRef]
- Siqueira, F.S.; Alessi, R.S.; Cardenas, A.F.; Kose, C.; Bandeca, M.C.; Gomes, J.C. New single-bottle ceramic primer: 6-month case report and laboratory performance. J. Contemp Dent. Pract. 2016, 17, 1033–1039. [Google Scholar] [CrossRef] [Green Version]
- Duzyol, M.; Sagsoz, O.; Sagsoz, N.P.; Akgul, N.; Yildiz, M. The effect of surface treatments on the bond strength between CAD/CAM blocks and composite resin. J. Prosthodont. 2015, 25, 466–471. [Google Scholar] [CrossRef]
- Thammajaruk, P.; Inokoshi, M.; Chong, S.; Guazzato, M. Bonding of composite cements to zirconia: A systematic review and meta-analysis of in vitro studies. J. Mech. Behav. Biomed. Mater. 2018, 80, 258–268. [Google Scholar] [CrossRef]


| Material | Manufacturer | Composition |
|---|---|---|
| CAD/CAM Ceramics | ||
| Vitablocs Mark II (VM2) | Vita Zahnfabrik, H. Rauter GmbH & Co, Bad Säckingen, Germany | Feldspathic ceramic (56–64% SiO2, 20–23%, Al2O3, 6–9% Na2O, 6–8% K2O) |
| Vita Enamic (EN) | Vita Zahnfabrik, H. Rauter GmbH & Co, Bad Säckingen, Germany | Cross-linked polymer (BisGMA, UDMA) (14 wt.%) and feldspathic ceramic enriched with Al2O3 (86 wt.%) |
| Lava Ultimate Restorative (LU) | 3M ESPE St. Paul, MN, USA | Matrix: BisGMA, UDMA, BisEMA, TEGDMA Filler: silica, zirconia nanoparticles and zirconia/silica nanoclusters (80 wt.%) |
| Cerasmart (CS) | GC America, Alsip, IL, USA | Matrix: BisMEPP, UDMA, DMA Filler: silica and barium glass nanoparticles (71 wt.%) |
| Crystal Ultra (CU) | Digital Dental, Scottsdale, AZ, USA | Cross-linked polymer (BisGMA, UDMA, BUDMA) (30 wt.%) and ceramic-like inorganic silicate glass fillers (70 wt.%) |
| Repair Systems | ||
| Monobond-S (MS) | Ivoclar Vivadent AG, Schaan, Liechtenstien | Ethanol,3-trimethoxysilylpropyl methacrylate, methacrylated phosphoric acid ester, disulfide acrylate |
| Monobond Etch & Prime (MEP) | Ivoclar Vivadent AG, Schaan, Liechtenstien | Buthanol, tetrabutylammonium dihydrogen trifluoride, methacrylated phosphoric acid ester, bis(triethoxysilyl)ethane |
| Heliobond | Ivoclar Vivadent AG, Schaan, Liechtenstien | Bis-GMA and TEGDMA (99 wt.%), catalysts and stabilizers <1% |
| Tetric N Ceram | Ivoclar Vivadent AG, Schaan, Liechtenstien | DMA (17–18 wt.%), filler load 82–83 wt.%, catalysts, stabilizers and pigments (<1.0 wt.%) |
| Materials | Groups | ||
|---|---|---|---|
| Control | MS | MEP | |
| VM2 | 4.30 ± 0.59 A,a | 19.18 ± 3.71 B,a | 12.80 ± 0.67 C,a |
| EN | 4.97 ± 1.14 A,a,b | 20.52 ± 1.39 B,a | 17 ± 1.15 B,b |
| LU | 6.52 ± 1.12 A,b | 20.59 ± 2.41 B,a | 15.83 ± 2.3 C,a,b |
| CS | 4.36 ± 1.31 A,a, | 25.67 ± 1.58 B,b | 23.86 ± 2.05 B,c |
| CU | 8.14 ± 3.96 A,b | 27.09 ± 1.11 B,b | 24.50 ± 3.06 B,c |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alnafaiy, S.; Labban, N.; Maawadh, A.; Alshehri, H.; Albaijan, R. Repair Bond Strength of Composite Resin to Aged Resin and Glass-Matrix CAD/CAM Ceramic Materials Using Two Different Repair Systems. Coatings 2021, 11, 1331. https://doi.org/10.3390/coatings11111331
Alnafaiy S, Labban N, Maawadh A, Alshehri H, Albaijan R. Repair Bond Strength of Composite Resin to Aged Resin and Glass-Matrix CAD/CAM Ceramic Materials Using Two Different Repair Systems. Coatings. 2021; 11(11):1331. https://doi.org/10.3390/coatings11111331
Chicago/Turabian StyleAlnafaiy, Sarah, Nawaf Labban, Ahmed Maawadh, Huda Alshehri, and Refal Albaijan. 2021. "Repair Bond Strength of Composite Resin to Aged Resin and Glass-Matrix CAD/CAM Ceramic Materials Using Two Different Repair Systems" Coatings 11, no. 11: 1331. https://doi.org/10.3390/coatings11111331






