Abstract
This study analyzes the marginal bone loss (MBL) among dental implants characterized with non-threaded collar design (NT) when compared to the more classic micro-threaded collar design (MC) as such might reflect the future dentogengival esthetics, implant metal show, and mucositis. A total of 112 patients who received 311 implants have been included in the study and analyzed for their postoperative MBL using sequential periapical radiographs. The prevalence of postoperative peri-implant mucositis was recorded as well. The periapical radiographic comparison was performed between the immediate postoperative record and at the 24-month recall visit. Among the 311 implants, 124 (39.9%) had NT implants, and 187 (60.1%) had MC implants. Out of the 112 patients, 37 (44.6%) were females, and 10 (34.5%) were males included in the NT group. In contrast, 46 (55.4%) females and 19 (65.5%) males were in the MC group. The mean age among the two groups was 41.43 ± 15.900 and 46.68 ± 16.070, respectively. In contrast, the mean MBL among the groups were 0.544 ± 0.7129 and 0.061 ± 0.2648, respectively. The change in MBL was not positively correlated with gender (p-value = 0.154) or age (p-value = 0.115) in both groups. However, there was a significant difference (p-value = 0.001, X2 = 62.796, Df = 4) of MBL between the two implant systems themselves. The MBL was higher in people implanted with the NT system when compared to MC. Therefore, the MC implant system can be a better choice for marginal bone preservation, especially in restoring esthetically demanding areas in the mouth.
1. Introduction
Dental implantology is the field that studies the inter-relation and the existence of the metal inserted into the bone with continuous coexistence, which is known as osseointegration [1]. In contrast, the dental implant surface itself is a sophisticated medical product that has the continuous opportunity for improvement and manufactural variety. For this coexistence to last, several factors contribute to its failure or success, which could be implant-related (i.e., implant design, surface, or connection, etc.), patient-related (i.e., presence of local infection, injury, or a systematic disease), or operator-related (i.e., skills, knowledge, or expertise, etc.) [2,3]. Such would contribute to the definition of success or failure. In our study, marginal bone loss (MBL) is being investigated as it reflects the future dentogenigval relation, peri-implant mucositis, and metal show. All can be very worrisome in the anterior maxilla, a demanding cosmetic region.
A dental implant is usually composed of a fixture that is inserted into the bone and a crown that is connected to the fixture via an intermediate abutment, where each has its own criteria and specifications in order to keep a healthy dentogengival relation [4]. The implant fixture itself is an area of much research, as the design varies in different lines, including the body type, threads, and surface treatment. To minimize the osseointegration time, modification in the dental implant surface is continuously applied [1]. The implant fixture surface is mainly fabricated by titanium (Ti) or ceramics, having titanium to be the most common one all over the world [5]. The surface of the fixture can be treated by different techniques, such as; machined (high/low density), etched, sandblasted, or coated with osseointegrating stimulant. All are aimed to assure a stable osseointegration process and minimizes the peri-implant bone loss, which can contribute to failures [5]. The pathophysiology of osseointegration starts with inflammation at the implant-bone interface that promotes bone remodeling, called osteoconduction. Such is to achieve an amorphous layer that withdraws the healing process and attachment [1,4].
The surface modification on the Ti-implant at the micro level is the traditional approach for the microroughened technology. Sandblasted, large-gritted, and acid-etched surface or SLA is one of the most successful surface modifications in clinical dentistry regardless it being hydrophobic or hydrophilic [6]. The parameter for the approximate height of the sharp, pointed surface is 1.5–2 μm, as shown in atomic force microscopy analysis (AFM) and scanning electronic microscopy (SEM; topographically). Exposure of the Ti surface results in a more biocompatible layer (titanium oxide, TiO2), i.e., the implant is in its oxidized form. Topographically, this implant surface is recognized by the osteogenic potential, which improves cell adhesion. However, to date, there is no significant result to determine which surface modification is better for bone healing or if the anodized microporous surface is better than the irregular SLA surface for generating osteogenic cell response [7]. The issue is even more sophisticated when discussing the fixture collar design as a sole factor.
This study intends to analyze the fixture collar surface that is electro-treated, etched, actively hydrophilic, microroughened, and non-threaded. An example of such design is the Neoss Proactive® implant system, Harrogate, UK. Principally, the threads start about 1.9 mm away from the fixture head, and that collar area is designed to be non-threaded and microroughened. Such is claimed to have a better marginal bone preservation potential and dentogengival relation. A recent study by Yeo [4] suggested that the aforementioned design was predictable and has shown excellent results at the nanoscale in in vitro experiments, in vivo studies, and clinical use. However, the efficacy of this design needs to be studied and evaluated thoroughly. Hence, our study evaluates the performance of such a non-threaded implant collar when compared to the classic micro-threaded implant collar design.
2. Materials and Methods
After achieving the ethical approval from the institute’s research board and following the Helsinki declaration guides of research, a retrospective chart review of all the intended implant cases was performed through the electronic filing system in the center. All the healthy patients that had the intended implants placed with complete medical records and radiographic follow-ups were retrieved. Patients with medical systemic situations, not aware of a self-controlled vitamin D3 status, or smoking were excluded to minimize variables. All the included cases were performed in the same treatment settings and were performed by the 2-stage protocol. Cases that were performed using a one-stage protocol or by different surgical protocols were excluded from the study. The cases that had clear recall visit documentations and periapical radiographs for interpretations up to 24 months postoperatively were included to prevent recall bias. The pertinent data were then collected and analyzed using the SPSS software version 25. The study followed the STROBE guidelines for quality assurance (Figure 1).
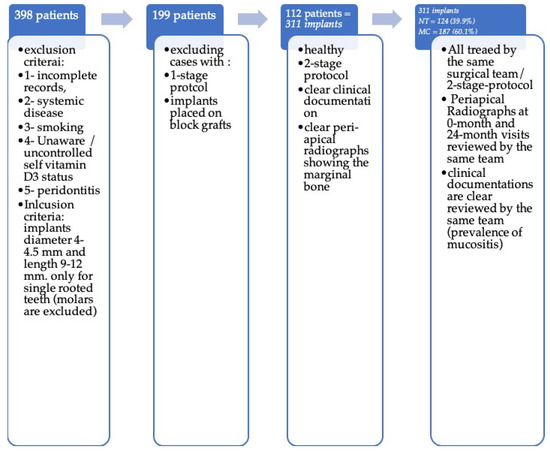
Figure 1.
A flow chart presenting the case inclusion/exclusion strategy.
The patients were divided into two groups on the basis of the implant system used, which were either NT or MC collar-implant-design. The surgical protocol was attempted by the same operator, starting with septic technique and chlorhexidine 0.2% mouthwash for 1 min preoperatively. Afterward, a conservative flap was raised under local anesthesia, and the bed was drilled using a low-speed contra-angle handpiece and cooling with sterile saline (0.9% NaCl) following the implant system protocol. All the implants were inserted with a torque of 30–45 Ncm (0.30–0.45 Nm), and cover screws were placed. The implant sizes ranged from 9 to 12 mm in length and 4.0–4.5 mm in diameter. Single interrupted sutures were placed to close the flap, and an immediate periapical radiograph was taken using a long cone positioner to assure proper and standardized angulation. A postoperative antibiotic for 5 days, analgesics, and chlorhexidine 0.2% mouth wash were prescribed. The periapical radiographs were assessed by the same assistant, and the bone level was calculated from the head of the cover screw going more apically at the mesial and distal aspect of the implant. An immediate postoperative radiograph was compared to the 24-month recall periapical radiograph for marginal bone loss (Figure 2). All the prosthetics were screw-retained single crowns, using Ti-base abutments and zirconium crowns. The dentogengival health status and the incidence of peri-implant mucositis were followed through the dental charts.
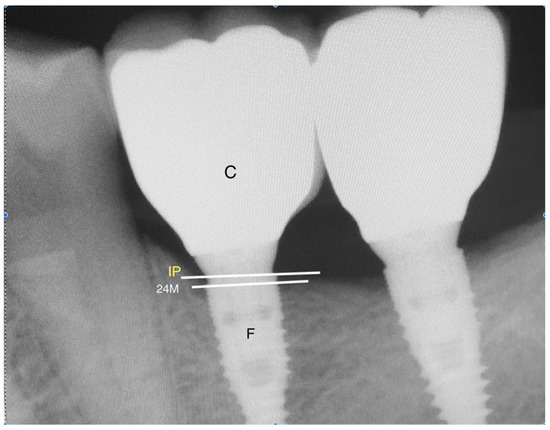
Figure 2.
A periapical digital radiograph at 24-month recall; F, implant fixture; IP, implant peak; C, crown; 24M, bone level at 24-month recall visit.
The marginal bone level (MBL) was compared on the images immediately after the implant placement and at the 24-month recall visit looking for any changes at a marginal bone level calculated by millimeters through the digital imaging system (radio-visiography analysis). The mean and frequencies of the variables were obtained, and a chi-square test was performed to find a correlation of MBL with various factors.
3. Results
The total number of participants that fulfilled the criteria was 112, who received a total of 311 implants at single-rooted tooth position (Table 1). Thereafter, 124 (39.9%) had NT implants, and 187 (60.1%) had MC implants. Out of the 112 patients, 37 (44.6%) females and 10 (34.5%) males were included in the NT group. In contrast, 46 (55.4%) females and 19 (65.5%) males were in the MC group. The mean age among the two groups was 41.43 ± 15.900 and 46.68 ± 16.070, respectively. Whereas, the mean MBL among the two groups was 0.544 ± 0.7129 and 0.061 ± 0.2648, respectively (Figure 3). The change in MBL was not significantly correlated with sex (p-value = 0.154) or age (p-value = 0.115) in both groups.

Table 1.
Demographics and MBL measurement for NT and MC implants.
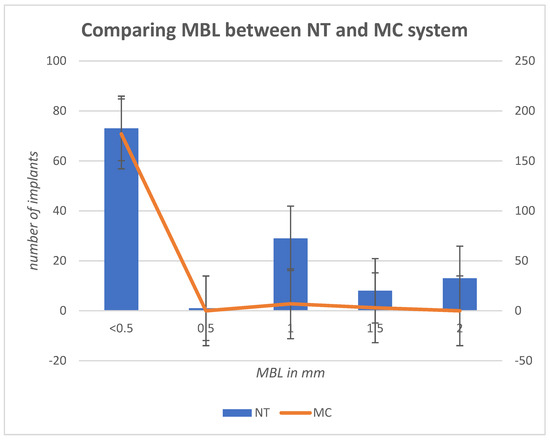
Figure 3.
A bar chart presenting the relation of MBL in mm between the two implant systems. The NT bars are showing more MBL when compared to the NT system.
Table 2 shows the results of chi-square test showed significant difference (p-value = 0.001, X2 = 62.796, Df = 4) of MBL among the two implant systems. It was found that 73 (58.9%) of the NT group showed 0.5 mm MBL on the radiographs when compared to 177 (94.7%) in the MC implants that had 0.5 MBL. None of the MC group had 2 mm of MBL, whereas 13 (10.5%) in NT showed an MBL of 2 mm. It was shown that 30% of the NT implants had 0.5–1.5 mm of MBL when compared to only 5% in the MC group. Based on the results, it can be said that patients with MC surfaces have more stable marginal bone levels when compared to NT implants.

Table 2.
Association between MBL in mm and the implant type.
The recall visits evaluated the status of the dentogengival relation and if any peri-implant mucositis is recorded. Table 3 shows the prevalence of the peri-implant mucositis in the NT group, which recorded two and four cases, at the 12-month and 24-month recall visits, respectively (a cumulative of 4.8%). While at the MT group, we recorded one and two cases, at 12-month and 24-month recall visits, respectively (a cumulative of 1.6%). The prevalence was found to be low, which is likely related to the shorter follow-up visits of 24-month when compared to longer recalls. Longer recalls of 3–5 years are expected to disclose more clinical outcomes.

Table 3.
The prevalence of peri-implant mucositis after 6, 12, and 24 months.
4. Discussion
In this study, a total of 112 patients received 311 implants were analyzed for marginal bone preservation among implant surface with different collar designs. They were divided into two groups, i.e., non-threaded collar (NT) and micro-threaded collar (MC) designs, to compare the marginal bone loss between the two groups. The majority of the patients were females, whereas the sex had no effect on the bone loss in either implant system. The patients’ age varied to the range of 17 to 80 years; however, such also was not significantly associated with the MBL in both groups. In contrast, the type of implant used was significantly affecting the outcome of the bone loss within 24 months after implantation. The patients who had MC collars showed significantly more stable marginal bone levels when compared to the NT collars.
Marginal bone stability is an important aspect of implant care that is affected by variable factors, most importantly, primary stability [3,6]. The implant primary stability depends on the fixture’s geometric features at the initial contact surface, the preparation efficacy, and the bone type [8]. In contrast, the osseointegration depends on the fixture’s surface topography (micro and macroscopic level) when in touch with the bone wall [9,10]. On the other hand, many factors do contribute to MBL and peri-implantitis, such as poor bone quality, immediate loading, heavy smoking, and an infected surgical site [3,10,11]. Hence, the exclusion criteria in our study were tight in order to rule out as many variables as possible. The fixture’s shape itself can affect the force distribution and implant-bone contact surface area. It was reported that non-threaded implants with cylinder-shaped fixtures had a higher failure rate when compared to conical implants. It is claimed that conical implant design has a better force distribution toward the surrounding bone as it simulates the normal root shape [3,11]. As bone-implant contact is a major factor influencing bone healing and the osseointegration process [12], variations in the implant surface were introduced either chemically (acid-etching), mechanically (grit blasting), or by combining both to improve the process. Lately, the roughness of the Ti surface has been increased by biomechanically sandblasting it. Previous studies have reported that the roughened implant surface is better than the smooth one as it provides better anchorage to the bone through the macrophage-cell-surface adhesion and osteoblast-phenotyping at the mesenchymal cell population level [13,14]. Alternatively, higher implant Ti wear was seen in roughened surface implant compared to the smooth and such proven to have no clinical implications so far [2]. The clinical case significance might be different in patients with periodontal disease. It was reported in a meta-analysis review that using machined or moderately roughened implant surfaces did not have any clinical significance among preoperative periodontitis. Such results could be attributed to the heterogenicity of the involved literature and multiple confounding factors that were involved [15]. It was reported that the serum level of vitamin D3 is another measure to consider when analyzing the predictability of marginal bone loss. It was suggested that cases with serum levels lower than <30 ng/mL be considered as a contributing factor to marginal bone loss [16]. However, such serum record was not included in our study, as it is not believed to be a standard of care for all patients presented for implant therapy. However, vitamin D3 was considered in our center via the preoperative systemic check-up, self-awareness, and health care maintenance.
The research presented has some limitations, such as the retrospective nature, opposing tooth information, the time frame of a 24-month recalls, and possibly not having a clear vitamin D3 record. For better assertion, prospective randomized controlled trials are suggested to evaluate the marginal bone level when using different collar designs. More prolonged follow-up time reaching 5 years is needed to evaluate the possible marginal bone loss, peri-implant mucositis, and the jeopardy at the esthetic zone via metal show.
5. Conclusions
In conclusion, it can be said that the micro-threaded implant collar design (MC) is a better choice to manage esthetically demanding areas in the oral cavity, such as the anterior maxillary region, as it showed more stable peri-implant marginal bone status when compared to the non-threaded collar design (NT) that showed a worrisome marginal loss, in our study. Further studies are suggested to incorporate factors such as grafting, vitamin D3 status, oral hygiene, smoking status, and the soft tissue variables to evaluate the effect of these factors on the outcome.
Funding
This research received no external funding.
Institutional Review Board Statement
The research was approved by the IRB committee in the institute. The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board (Ethics Committee) of King Abdulaziz University (124–17 date 1 September 2018).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Provided and presented in the article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Albrektsson, T.; Wennerberg, A. On osseointegration in relation to implant surfaces. Clin. Implant. Dent. Relat. Res. 2019, 21, 4–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Naghshbandi, J. The influence of local and systemic factors upon dental implant osseointegration: A critical review. Saudi J. Oral Sci. 2020, 7, 65. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Reasons for failures of oral implants. J. Oral Rehabil. 2014, 41, 443–476. [Google Scholar] [CrossRef] [PubMed]
- Yeo, I.S. Modifications of dental implant surfaces at the micro- and nano-level for enhanced osseointegration. Materials 2019, 13, 89. [Google Scholar] [CrossRef] [Green Version]
- Abraham, C.M. A brief historical perspective on dental implants, their surface coatings and treatments. Open Dent. J. 2014, 8, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Nicolau, P.; Guerra, F.; Reis, R.; Krafft, T.; Benz, K.; Jackowski, J. 10-year outcomes with immediate and early loaded implants with a chemically modified SLA surface. Quintessence Int. 2018, 50, 114–124. [Google Scholar] [CrossRef] [PubMed]
- Cooper, L.F. A role for surface topography in creating and maintaining bone at titanium endosseous implants. J. Prosthet. Dent. 2000, 84, 522–534. [Google Scholar] [CrossRef] [PubMed]
- Sennerby, L.; Meredith, N. Implant stability measurements using resonance frequency analysis: Biological and biomechanical aspects and clinical implications. Periodontology 2008, 47, 51–66. [Google Scholar] [CrossRef]
- Ogle, O.E. Implant surface material, design, and osseointegration. Dent. Clin. N. Am. 2015, 59, 505–520. [Google Scholar] [CrossRef] [PubMed]
- Stanford, C.M. Biomechanical and functional behavior of implants. Adv. Dent. Res. 1999, 13, 88–92. [Google Scholar] [CrossRef] [PubMed]
- Romanos, G.E.; Basha-Hijazi, A.; Gupta, B.; Ren, Y.-F.; Malmstrom, H. Role of clinician’s experience and implant design on implant stability. An ex vivo study in artificial soft bones. Clin. Implant. Dent. Relat. Res. 2012, 16, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Shah, F.; Thomsen, P.; Palmquist, A. A review of the impact of implant biomaterials on Osteocytes. J. Dent. Res. 2018, 97, 977–986. [Google Scholar] [CrossRef] [PubMed]
- Conserva, E.; Pisciotta, A.; Borghi, F.; Nasi, M.; Pecorini, S.; Bertoni, L.; De Pol, A.; Consolo, U.; Carnevale, G. Titanium surface properties influence the biological activity and fasl expression of craniofacial stromal cells. Stem Cells Int. 2019, 2019, 4670560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saghiri, M.; Asatourian, A.; Garcia-Godoy, F.; Sheibani, N. The role of angiogenesis in implant dentistry part I: Review of titanium alloys, surface characteristics and treatments. Med. Oral Patol. Oral Cir. Bucal 2016, 21, e514–e525. [Google Scholar] [CrossRef]
- Dank, A.; Aartman, I.H.A.; Wismeijer, D.; Tahmaseb, A. Effect of dental implant surface roughness in patients with a history of periodontal disease: A systematic review and meta-analysis. Int. J. Implant. Dent. 2019, 5, 33. [Google Scholar] [CrossRef]
- Kwiatek, J.; Jaroń, A.; Trybek, G. Impact of the 25-hydroxycholecalciferol concentration and vitamin d deficiency treatment on changes in the bone level at the implant site during the process of osseointegration: A prospective, randomized, controlled clinical trial. J. Clin. Med. 2021, 10, 526. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).