Knowledge, Attitudes and Practices of Veterinarians Towards Antimicrobial Resistance and Stewardship in Nigeria
Abstract
1. Introduction
2. Results
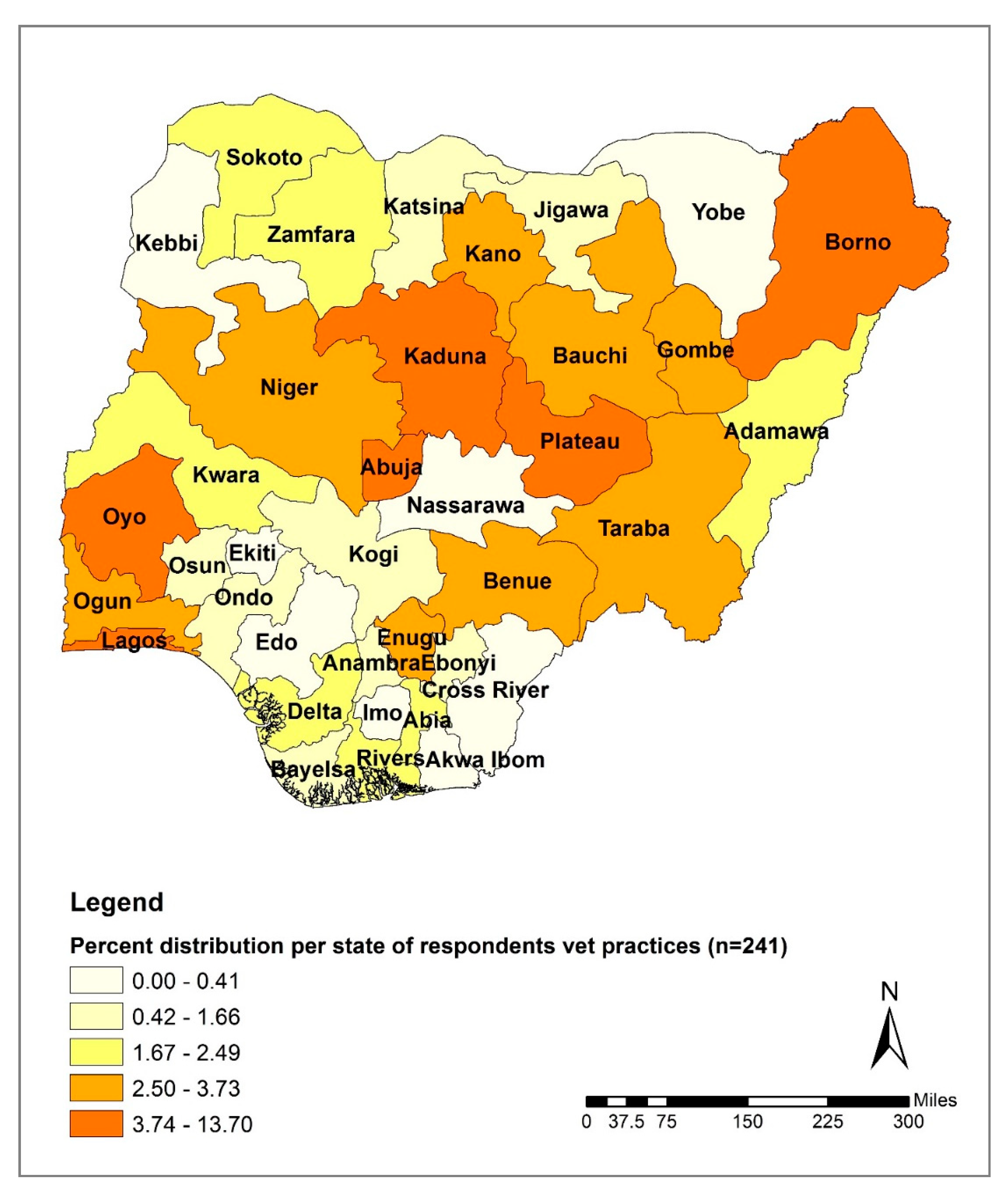
2.1. Demographic Information
2.2. Knowledge
2.3. Attitude
2.4. Practices Influencing Antibiotic Use
2.5. Relationship between the Use of AST before Antibiotic Treatment and Select Investigated Parameters
2.6. Relationship between Knowledge Level of Appropriate Antibiotic Use and AMR and Select Investigated Parameters
3. Discussion
4. Materials and Methods
4.1. Study Area
4.2. Study Population
4.3. Study Design
4.4. Sample Size
4.5. Data Collection
4.6. Data Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Antibiotic Resistance. 2008. Available online: https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance (accessed on 20 August 2018).
- World Health Organization (WHO). Global Action Plan on Antimicrobial Resistance. 2015, pp. 8–9. Available online: https://www.who.int/antimicrobial-resistance/publications/global-action-plan/en/ (accessed on 20 September 2018).
- Fosberg, K.J.; Reyes, A.; Wang, B.; Selleck, E.M.; Sommer, M.O.A.; Danta, G. The shared antibiotic resistome of soil bacteria and human pathogens. Science 2012, 337, 1107–1111. [Google Scholar] [CrossRef] [PubMed]
- Spoor, L.E.; McAdam, P.R.; Weinert, L.A.; Rambaut, A.; Hasman, H.; Aarestrup, F.M.; Kearns, A.M.; Larsen, A.R.; Skov, R.L.; Fitzgerald, J.R. Livestock origin for a human pandemic clone of community associated methicillin-resistant Staphylococcus aureus. MBio 2012, 4, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Ward, M.J.; Gibbons, C.L.; McAdam, P.R.; van Bunnik, B.A.D.; Girvan, E.K.; Edwards, G.F.; Fitzgerald, J.R.; Woolhouse, M.E.J. Time-scaled evolutionary analysis of the transmission and antibiotic resistance dynamics of Staphylococcus aureus CC398. Appl. Environ. Microbiol. 2014, 80, 7275–7282. [Google Scholar] [CrossRef]
- Mather, A.E.; Reid, S.W.J.; Maskell, D.J.; Parkhill, J.; Fookes, M.C.; Harris, S.R.; Brown, D.J.; Coia, J.E.; Mulvey, M.R.; Gilmour, M.W.; et al. Distinguishable epidemics of multidrug-resistant Salmonella Typhimurium DT104 in different hosts. Science 2013, 341, 1514–1517. [Google Scholar] [CrossRef]
- Chantziaras, I.; Boyen, F.; Callens, B.; Dewulf, J. Correlation between veterinary antimicrobial use and antimicrobial resistance in food-producing animals: A report on seven countries. J. Antimicrob. Chemother. 2014, 69, 827–834. [Google Scholar] [CrossRef] [PubMed]
- Van den Bogaard, A.E.; London, N.; Driessen, C.; Stobberingh, E.E. Antibiotic resistance of faecal Escherichia coli in poultry, poultry farmers and poultry slaughterers. J. Antimicrob. Chemother. 2001, 47, 763–771. [Google Scholar] [CrossRef] [PubMed]
- Aslam, B.; Wang, W.; Arshad, M.; Khurshid, M.; Muzammil, S.; Rasool, M.; Nisar, M.A.; Alvi, R.F.; Aslam, M.A.; Qamar, M.U.; et al. Antibiotic resistance: A rundown of a global crisis. Infect. Drug Resist. 2018, 11, 1645–1658. [Google Scholar] [CrossRef] [PubMed]
- Ansari, F.; Gray, K.; Nathwani, D.; Phillips, G.; Ogston, S.; Ramsay, C.; Davey, P. Outcomes of an intervention to improve hospital antibiotic prescribing: Interrupted time series with segmented regression analysis. J. Antimicrob. Chemother. 2003, 52, 842–848. [Google Scholar] [CrossRef]
- Carling, P.; Fung, T.; Killion, A.; Terrin, N.; Barza, M. Favorable impact of a multidisciplinary antibiotic management program conducted during 7 years. Infect. Control. Hosp. Epidemiol. 2003, 24, 699–706. [Google Scholar] [CrossRef]
- Ruttimann, S.; Keck, B.; Hartmeier, C.; Maetzel, A.; Bucher, H.C. Long-term antibiotic cost savings from a comprehensive intervention program in a medical department of a university-affiliated teaching hospital. Clin. Infect. Dis. 2004, 38, 348–356. [Google Scholar] [CrossRef]
- Dellit, T.H.; Owens, R.C.; McGowan, J.E.; Gerding, D.N.; Weinstein, R.A.; Burke, J.P.; Huskins, W.C.; Paterson, D.L.; Fishman, N.O.; Carpenter, C.F.; et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin. Infect. Dis. 2007, 44, 159–177. [Google Scholar] [CrossRef]
- Davey, P.; Brown, E.; Charani, E.; Fenelon, L.; Gould, I.M.; Holmes, A.; Ramsay, C.R.; Wiffen, P.J.; Wilcox, M. Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Syst. Rev. 2013, 4, 2. [Google Scholar]
- Centers for Disease Control (CDC). Core Elements of Hospital Antibiotic Stewardship Programs; US Department of Health and Human Services, CDC: Atlanta, GA, USA, 2014. Available online: http://www.cdc.gov/getsmart/healthcare/implementation/core-elements.html (accessed on 10 May 2019).
- Karanika, S.; Paudel, S.; Grigoras, C.; Kalbasi, A.; Mylonakis, E. Systematic Review and Meta-analysis of Clinical and Economic Outcomes from the Implementation of Hospital-Based Antimicrobial Stewardship Programs. Antimicrob. Agents Chemother. 2016, 60, 4840–4852. [Google Scholar] [CrossRef]
- Baur, D.; Gladstone, B.P.; Burkert, F.; Carrara, E.; Foschi, F.; Dobele, S.; Tacconelli, E. Effect of antibiotic stewardship on the incidence of infection and colonisation with antibiotic-resistant bacteria and Clostridium difficile infection: A systematic review and meta-analysis. Lancet Infect. Dis. 2017, 17, 990–1001. [Google Scholar] [CrossRef]
- World Health Organization (WHO). WHO Global Strategy for Containment of Antimicrobial Resistance. Available online: http://www.who.int/csr/resources/publications/drugresist/en/EGlobal_Strat.pdf (accessed on 4 April 2019).
- Tseng, S.; Lee, C.; Lin, T.; Chang, S. Combating antimicrobial resistance: Antimicrobial stewardship program in Taiwan. J. Microbiol. Immunol. Infect. 2012, 45, 79–89. [Google Scholar] [CrossRef]
- Ogaji, I.; Odumosu, P.; Ngwuluka, C.; Onoja, V. Availability of veterinary pharmaceuticals and the role of pharmacists in health-care delivery services to animal patients in Plateau State. Niger. J. Pharm. Sci. 2010, 9, 66–72. [Google Scholar]
- Kingsley, P. Inscrutable medicines and marginal markets: Tackling substandard veterinary drugs in Nigeria. Pastor Res. Policy Pract. 2015, 5, 1–13. [Google Scholar] [CrossRef]
- National Agency for Food and Drug Administration and Control (NAFDAC). Available online: https://www.nafdac.gov.ng/veterinary-products/ (accessed on 4 July 2020).
- Federal Ministry of Agriculture and Rural Development, Environment and Health. National Action Plan for Antimicrobial Resistance 2017–2022. 2017; pp. 13–14. Available online: https://ncdc.gov.ng/themes/common/docs/protocols/77_1511368219.pdf (accessed on 4 September 2018).
- John, F.P. Antimicrobial use in food and companion animals. Anim. Heal. Res. Rev. 2008, 9, 127–133. [Google Scholar]
- Kariuki, S.; Dougan, G. Antibacterial resistance in sub-Saharan Africa: An underestimated emergency. Ann. N. Y. Acad. Sci. 2014, 14, 1323. [Google Scholar] [CrossRef]
- Speksnijder, D.C.; Jaarsma, D.A.C.; Verheij, T.J.M.; Wagenaar, J.A. Attitudes and perceptions of Dutch veterinarians on their role in the reduction of antimicrobial use in farm animals. Prev. Vet. Med. 2015, 121, 365–373. [Google Scholar] [CrossRef]
- Coyne, L.A.; Latham, S.M.; Dawson, S.; Donald, I.J.; Pearson, R.B.; Smith, R.F.; Williams, N.J.; Pinchbeck, G.L. Antimicrobial use practices, attitudes and responsibilities in UK farm animal veterinary surgeons. Prev. Vet. Med. 2018, 161, 115–126. [Google Scholar] [CrossRef]
- Id, J.M.N.; Zhuo, A.; Govendir, M.; Rowbotham, S.J.; Labbate, M.; Degeling, C.; Gilbert, G.L.; Dominey-Howes, D.; Ward, M.P. Factors influencing the behaviour and perceptions of Australian veterinarians towards antibiotic use and antimicrobial resistance. PLoS ONE 2019, 14, e0223534. [Google Scholar] [CrossRef]
- Schneider, S.; Salm, F.; Vincze, S.; Moeser, A.; Petruschke, I.; Schmücker, K.; Ludwig, N.; Hanke, R.; Schröder, C.; Gropmann, A.; et al. Perceptions and attitudes regarding antibiotic resistance in Germany: A cross-sectoral survey amongst physicians, veterinarians, farmers and the general public. J. Antimicrob. Chemother. 2018, 73, 1984–1988. [Google Scholar] [CrossRef] [PubMed]
- Anyanwu, M.U.; Kolade, O.A. Veterinarians’ Perception, Knowledge and Practices of Antibiotic Stewardship in Enugu State Southeast, Nigeria. Notale Sci. Biol. 2018, 9, 321–331. [Google Scholar] [CrossRef]
- Odetokun, I.A.; Akpabio, U.; Alhaji, N.B.; Biobaku, K.T.; Oloso, N.O.; Ghali-Mohammed, I.; Biobaku, A.J.; Adetunji, V.O.; Fasina, F.O. Knowledge of Antimicrobial Resistance among Veterinary Students and Their Personal Antibiotic Use Practices: A National Cross-Sectional Survey. Antibiotics (Basel, Switzerland) 2019, 8, 243. [Google Scholar] [CrossRef]
- Dyar, O.J.; Hills, H.; Seitz, L.T.; Perry, A.; Ashiruredope, D. Assessing the Knowledge, Attitudes and Behaviors of Human and Animal Health Students towards Antibiotic Use and Resistance: A Pilot Cross-Sectional Study in the UK. Antibiotics 2018, 7, 10. [Google Scholar] [CrossRef]
- Seymour, E.H.; Jones, G.M.; McGilliard, M.L. Persistence of Residues in Milk Following Antibiotic Treatment of Dairy Cattle. J. Dairy Sci. 1988, 71, 2292–2296. [Google Scholar] [CrossRef]
- Kang’ethe, E.K.; Aboge, G.O.; Arimi, S.M.; Kanja, L.W.; Omore, A.O.; McDermott, J.J. Investigation of the risk of consuming marketed milk with antimicrobial residues in Kenya. Food Control. 2005, 16, 349–355. [Google Scholar] [CrossRef]
- Dewdney, J.M.; Maes, L.; Raynaud, J.P.; Blanc, F.; Scheid, J.P.; Jackson, T.; Lens, S.; Verschueren, C. Risk assessment of antibiotic residues of β-lactams and macrolides in food products with regard to their immuno-allergic potential. Food Chem. Toxicol. 1991, 29, 477–483. [Google Scholar] [CrossRef]
- Vázquez-Moreno, L.; Bermúdez, M.C.; Languré, A.A.; Higuera-Ciapara, I.; Díaz De Aguayo, M.; Flores, E. Antibiotic Residues and Drug Resistant Bacteria in Beef, and Chicken Tissues. J. Food Sci. 1990, 55, 632–634. [Google Scholar] [CrossRef]
- Pena, A.; Serrano, C.; Réu, C.; Baeta, L.; Calderón, V.; Silveira, I.; Sousa, J.C.; Peixe, L. Antibiotic residues in edible tissues and antibiotic resistance of faecal Escherichia coli in pigs from Portugal. Food Addit. Contam. A 2007, 21, 749–755. [Google Scholar] [CrossRef]
- Bokma, J.; Dewulf, J.; Deprez, P.; Pardon, B. Risk factors for antimicrobial use in food-producing animals: Disease prevention and socio-economic factors as the main drivers? VLAAMS DIERGEN TIJDS 2018, 87, 188–200. [Google Scholar] [CrossRef]
- Wierup, M. The control of microbial diseases in animals: Alternatives to the use of antibiotics. Int. J. Antimicrob. Agents 2000, 14, 315–319. [Google Scholar] [CrossRef]
- Robinson, T.P.; Bu, D.P.; Carrique-Mas, J.; Fèvre, E.M. Antibiotic resistance: Mitigation opportunities in livestock sector development. Camb. Univ. Press 2017, 11, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Finley, R.L.; Collignon, P.; Larsson, D.G.J.; McEwen, S.A.; Li, X.; Gaze, W.H.; Reid-Smith, R.; Timinouni, M.; Graham, D.W.; Topp, E. The Scourge of Antibiotic Resistance: The Important Role of the Environment. Clin. Infect. Dis. 2013, 57, 704–710. [Google Scholar] [CrossRef] [PubMed]
- Manyi-Loh, C.; Mamphweli, S.; Meyer, E.; Okoh, A. Antibiotic Use in Agriculture and Its Consequential Resistance in Environmental Sources: Potential Public Health Implications. Molecules 2018, 23, 795. [Google Scholar] [CrossRef]
- European Medicines Agency (EMA) and European Food Safety Authority (EFSA). EMA and EFSA Joint Scientific Opinion on measures to reduce the need to use antimicrobial agents in animal husbandry in the European Union, and the resulting impacts on food safety (RONAFA). [EMA/CVMP/570771/2015]. EFSA J. 2017, 15, e04666. Available online: https://www.efsa.europa.eu/en/efsajournal/pub/4666 (accessed on 23 March 2020).
- World Health Organization (WHO), Regional Office for South-East Asia. Step-by-step approach for development and implementation of hospital antibiotic policy and standard treatment guidelines. WHO Regional Office for South-East Asia. 2011, pp. 21–24. Available online: https://apps.who.int/iris/handle/10665/205912 (accessed on 10 January 2020).
- De Briyne, N.; Atkinson, J.; Pokludová, L.; Borriello, S.P.; Price, S. Factors influencing antibiotic prescribing habits and use of sensitivity testing amongst veterinarians in Europe. Vet. Rec. 2013, 173, 475. [Google Scholar] [CrossRef]
- Leekha, S.; Terrell, C.L.; Edson, R.S. General principles of antimicrobial therapy. Mayo Clin. Proc. 2011, 86, 156–167. [Google Scholar] [CrossRef]
- Beović, B. Emperic Antibiotic Therapy [Internet]. European Society of Clinical Microbiology and Infectious Diseases. 2019. Available online: http://esgap.escmid.org/?page_id=389 (accessed on 7 July 2020).
- Aliu, Y.O. Nigerian Veterinary formulary. In Handbook of essential veterinary drugs, biologics, and chemicals, 1st ed.; Aliu, Y.O., Ed.; Veterinary Council of Nigeria: Abuja, Nigeria, 2007. [Google Scholar]
- Luseba, D.; Rwambo, P. Review of the policy, regulatory & administrative framework for delivery of livestock health products and services in West and Central Africa. GALVmed. 2015. Available online: http://www.galvmed.org/wp-content/uploads/2015/09/East-Africa-Review-of-Policy-Regulatory-and-Administrative-Framework-for-Delivery-of-Livestock-Health-Products-and-Services-March-2015.pdf (accessed on 11 November 2019).
- The World Bank In Nigeria [Internet]. 2019. Available online: https://www.worldbank.org/en/country/nigeria/overview (accessed on 4 July 2019).
- Lwanga, S.; Lemeshow, S. Sample Size Determination in Health Studies: A Practical Manual, 1st ed.; World Health Organization: Geneva, Switzerland, 1991; Available online: https://apps.who.int/iris/bitstream/handle/10665/40062/9241544058_%28p1-p22%29.pdf?sequence=1&isAllowed=y (accessed on 8 December 2018).
- Pedersen, M.J.; Nielsen, C.V. Improving survey response rates in online panels: Effects of low-cost incentives and cost-free text appeal interventions. Soc. Sci. Comput. Rev. 2016, 34, 229–243. [Google Scholar] [CrossRef]
| Variable | Response | Frequency (n = 241) | Percentage (%) |
|---|---|---|---|
| Gender | Female | 49 | 20.3 |
| Male | 192 | 79.7 | |
| Age group | 18–24 years old | 1 | 0.4 |
| 25–34 years old | 116 | 48.1 | |
| 35–44 years old | 85 | 35.3 | |
| 45–54 years old | 27 | 11.2 | |
| 55–64 years old | 12 | 5.0 | |
| 65 years and above | 0 | 0 | |
| Prefer not to say | 0 | 0 | |
| University of training | Ahmadu Bello University (ABU), Zaria | 69 | 28.6 |
| University of Maiduguiri | 60 | 24.9 | |
| University of Nigeria Nsukka (UNN) | 31 | 12.9 | |
| Usmanu Danfodiyo University, Sokoto (UDUS) | 27 | 11.2 | |
| University of Ibadan (UI), Ibadan | 27 | 11.2 | |
| Federal University of Agriculture Makurdi (FUAM) | 9 | 3.7 | |
| Federal University of Agriculture, Abeokuta (FUNAAB) | 8 | 3.3 | |
| Other | 8 | 3.3 | |
| University of Abuja | 2 | 0.8 | |
| Highest level of education | Veterinary degree (DVM, etc.) | 152 | 63.1 |
| MSc/MPH | 61 | 25.3 | |
| Fellow, College of Veterinary Surgeon (FCVS) | 6 | 2.5 | |
| PhD | 16 | 6.6 | |
| Other | 6 | 2.5 | |
| Type of employment | Private practice | 92 | 38.2 |
| Government employee | 75 | 31.1 | |
| Teaching | 25 | 10.4 | |
| Non-governmental organization employee | 22 | 9.1 | |
| Research | 15 | 6.2 | |
| Other | 12 | 5.0 | |
| Years registered as a vet surgeon | 0–<5 years | 87 | 36.1 |
| 5–10 years | 75 | 31.1 | |
| 10–15 years | 30 | 12.4 | |
| 15–20 years | 18 | 7.5 | |
| 21 and above | 28 | 11.6 | |
| Prefer not to say | 3 | 1.2 | |
| Type of veterinary practice * | Mixed practice (large, small or exotic animals) | 97 | 40.2 |
| Poultry practice (chicken, turkey) | 94 | 39.0 | |
| Small animal practice (dogs, cats, rabbits) | 87 | 36.1 | |
| Large animal practice (cattle, horse, goat, sheep, pig) | 75 | 31.1 | |
| Fish practice | 29 | 12.0 | |
| Do not practice | 15 | 6.2 | |
| Other practice | 11 | 4.6 | |
| Exotics practice (parrots, tortoise, snakes, etc.) | 8 | 3.3 | |
| Wildlife practice (wild animals) | 6 | 2.5 | |
| Location of veterinary practice by geopolitical zone | North Central | 69 | 28.6 |
| North West | 49 | 20.3 | |
| North East | 46 | 19.1 | |
| South West | 39 | 16.2 | |
| South East | 21 | 8.7 | |
| South South | 17 | 7.1 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adekanye, U.O.; Ekiri, A.B.; Galipó, E.; Muhammad, A.B.; Mateus, A.; La Ragione, R.M.; Wakawa, A.; Armson, B.; Mijten, E.; Alafiatayo, R.; et al. Knowledge, Attitudes and Practices of Veterinarians Towards Antimicrobial Resistance and Stewardship in Nigeria. Antibiotics 2020, 9, 453. https://doi.org/10.3390/antibiotics9080453
Adekanye UO, Ekiri AB, Galipó E, Muhammad AB, Mateus A, La Ragione RM, Wakawa A, Armson B, Mijten E, Alafiatayo R, et al. Knowledge, Attitudes and Practices of Veterinarians Towards Antimicrobial Resistance and Stewardship in Nigeria. Antibiotics. 2020; 9(8):453. https://doi.org/10.3390/antibiotics9080453
Chicago/Turabian StyleAdekanye, Usman O., Abel B. Ekiri, Erika Galipó, Abubakar Bala Muhammad, Ana Mateus, Roberto M. La Ragione, Aliyu Wakawa, Bryony Armson, Erik Mijten, Ruth Alafiatayo, and et al. 2020. "Knowledge, Attitudes and Practices of Veterinarians Towards Antimicrobial Resistance and Stewardship in Nigeria" Antibiotics 9, no. 8: 453. https://doi.org/10.3390/antibiotics9080453
APA StyleAdekanye, U. O., Ekiri, A. B., Galipó, E., Muhammad, A. B., Mateus, A., La Ragione, R. M., Wakawa, A., Armson, B., Mijten, E., Alafiatayo, R., Varga, G., & Cook, A. J. C. (2020). Knowledge, Attitudes and Practices of Veterinarians Towards Antimicrobial Resistance and Stewardship in Nigeria. Antibiotics, 9(8), 453. https://doi.org/10.3390/antibiotics9080453





