Characterization and Therapeutic Potential of Bacteriophage-Encoded Polysaccharide Depolymerases with β Galactosidase Activity against Klebsiella pneumoniae K57 Capsular Type
Abstract
1. Introduction
2. Results and Discussion
2.1. Bacteriophages KpV79 and KpV767 Are Specific for Klebsiella pneumoniae of Capsular Type K57
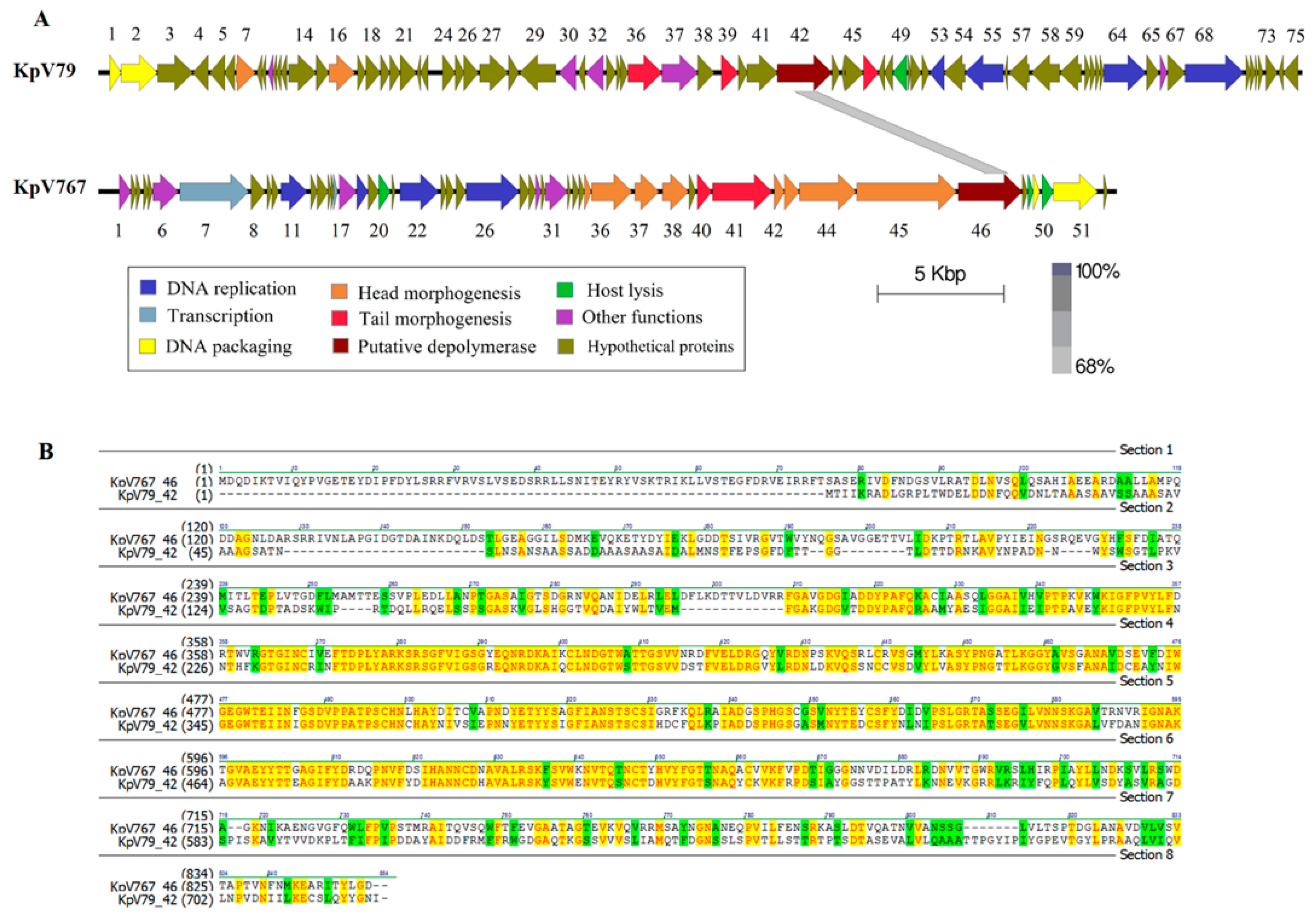
2.2. Genomes of Bacteriophages KpV79 and KpV767, Representing Distinct Taxonomic Groups, Contain Genes Encoding Polysaccharide Depolymerases with a High Level of Similarity at the Amino Acid Level
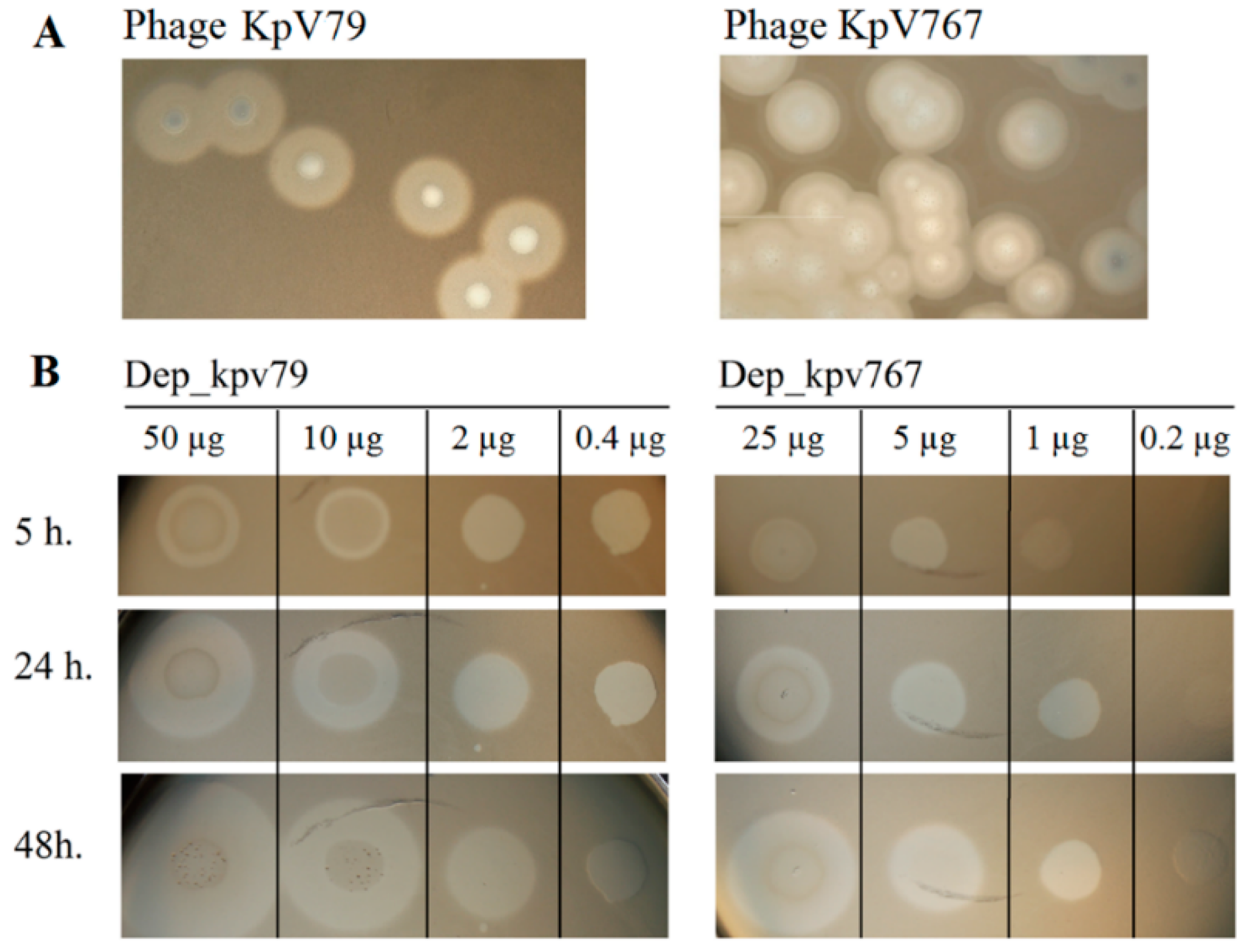
2.3. Depolymerases Dep_767 and Dep_79 Inhibit the Adsorption of Corresponding Bacteriophages on a Capsule of Bacterial Cells
2.4. Depolymerases Dep_kpv79 and Dep_kpv767 Specifically Cleave the β-Galactosidic Linkages in the K57 Capsular Polysaccharide of K. pneumoniae
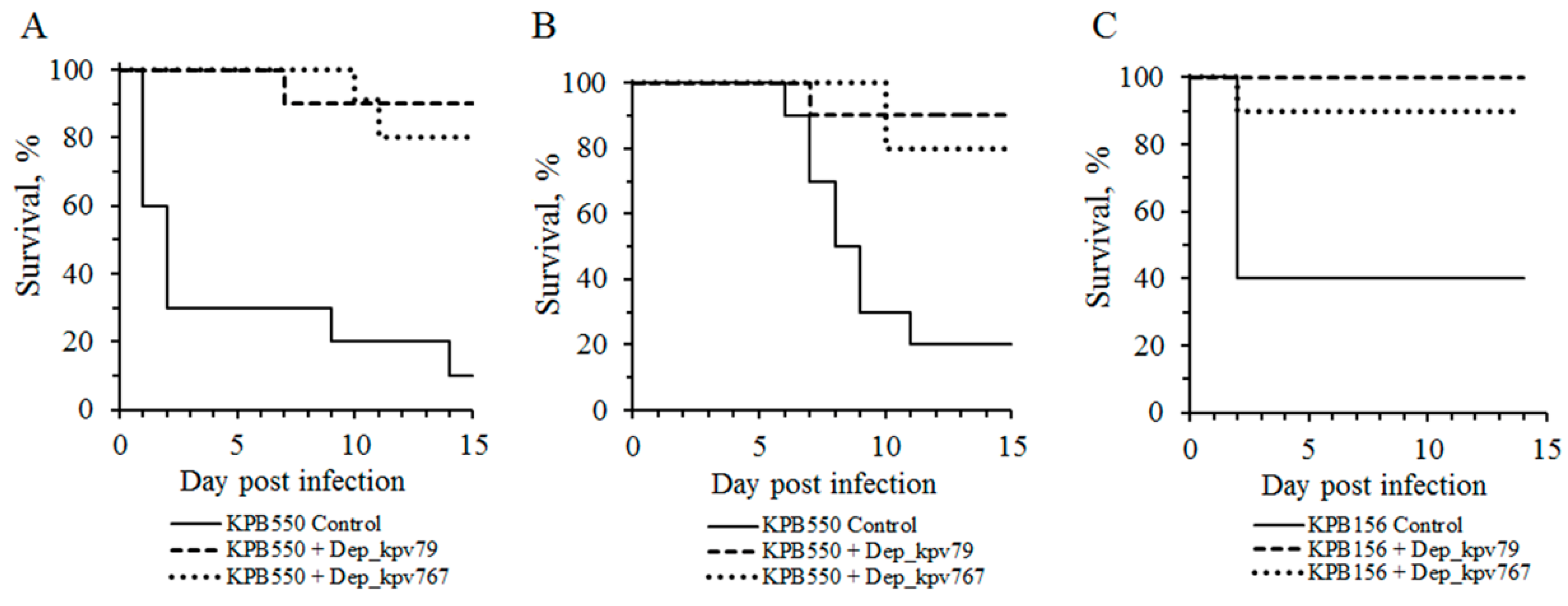
2.5. Capsule Depolymerases Are Effective Therapeutics in Mouse Infection Models
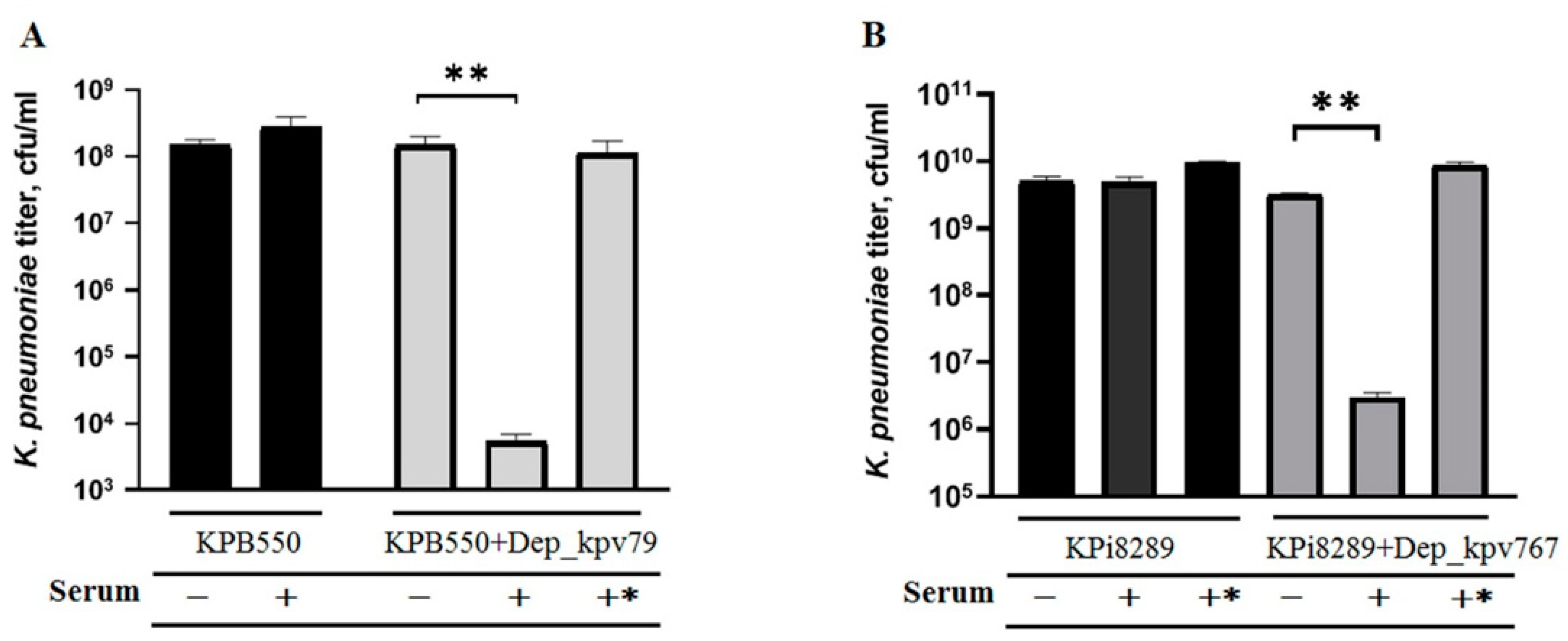
2.6. Depolymerases Increase Sensitivity to Serum-Complement-Mediated Killing
3. Materials and Methods
3.1. Bacterial Strains and Bacteriophages
3.2. Determination of the Host Range of Phage and Polysaccharide Depolymerase
3.3. Analysis of the Phage Genomes
3.4. Cloning of CPS Depolymerase Genes and Preparation of Recombinant Proteins
3.5. Determination of the Structures of the Oligosaccharides Derived by the Treatment of K. pneumoniae CPS with Phage Depolymerases
3.6. Phage Adsorption Inhibition Test and Phage Inactivation by CPS
3.7. In vivo K. pneumoniae Infection Models
3.8. Serum Complement Activity
3.9. Statistical Analysis
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Podschun, R.; Ullmann, U. Klebsiella spp. as nosocomial pathogens: Epidemiology, taxonomy, typing methods, and pathogenicity factors. Clin. Microbiol. Rev. 1998, 11, 589–603. [Google Scholar] [CrossRef] [PubMed]
- Paczosa, M.K.; Mecsas, J. Klebsiella pneumoniae: Going on the Offense with a Strong Defense. Microbiol. Mol. Biol. Rev. 2016, 80, 629–661. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.H.; Liu, Y.C.; Lee, S.S.; Yen, M.Y.; Chen, Y.S.; Wang, J.H.; Wann, S.R.; Lin, H.H. Primary liver abscess due to Klebsiella pneumoniae in Taiwan. Clin. Infect. Dis. 1998, 26, 1434–1438. [Google Scholar] [CrossRef]
- Turton, J.F.; Englender, H.; Gabriel, S.N.; Turton, S.E.; Kaufmann, M.E.; Pitt, T.L. Genetically similar isolates of Klebsiella pneumoniae serotype K1 causing liver abscesses in three continents. J. Med. Microbiol. 2007, 56, 593–597. [Google Scholar] [CrossRef] [PubMed]
- Cortes, G.; Borrell, N.; de Astorza, B.; Gómez, C.; Sauleda, J.; Albertí, S. Molecular analysis of the contribution of the capsular polysaccharide and the lipopolysaccharide O side chain to the virulence of Klebsiella pneumoniae in a murine model of pneumonia. Infect. Immun. 2002, 70, 2583–2590. [Google Scholar] [CrossRef] [PubMed]
- Domenico, P.; Salo, R.J.; Cross, A.S.; Cunha, B.A. Polysaccharide capsule-mediated resistance to opsonophagocytosis in Klebsiella pneumoniae. Infect. Immun. 1994, 62, 4495–4499. [Google Scholar] [CrossRef] [PubMed]
- Ørskov, I.; Fife-Asbury, M.A. New Klebsiella capsular antigen K82 and the deletion of five of those previously assigned. Int. J. Syst. Bacteriol. 1977, 27, 386–387. [Google Scholar] [CrossRef]
- Pan, Y.J.; Lin, T.L.; Chen, C.T.; Chen, Y.Y.; Hsieh, P.F.; Hsu, C.R.; Wu, M.C.; Wang, J.T. Genetic analysis of capsular polysaccharide synthesis gene clusters in 79 capsular types of Klebsiella spp. Sci. Rep. 2015, 5, 15573. [Google Scholar] [CrossRef]
- Wyres, K.L.; Wick, R.R.; Gorrie, C.; Jenney, A.; Follador, R.; Thomson, N.R.; Holt, K.E. Identification of Klebsiella capsule synthesis loci from whole genome data. Microb. Genom. 2016, 2, e000102. [Google Scholar] [CrossRef]
- Shon, A.S.; Bajwa, R.P.; Russo, T.A. Hypervirulent (hypermucoviscous) Klebsiella pneumoniae: A new and dangerous breed. Virulence 2013, 4, 107–118. [Google Scholar] [CrossRef]
- Rakhuba, D.V.; Kolomiets, E.I.; Dey, E.S.; Novik, G.I. Bacteriophage receptors, mechanisms of phage adsorption and penetration into host cell. Pol. J. Microbiol. 2010, 59, 145–155. [Google Scholar] [CrossRef]
- Latka, A.; Maciejewska, B.; Majkowska-Skrobek, G.; Briers, Y.; Drulis-Kawa, Z. Bacteriophage-encoded virion-associated enzymes to overcome the carbohydrate barriers during the infection process. Appl. Microbiol. Biotechnol. 2017, 101, 3103–3119. [Google Scholar] [CrossRef] [PubMed]
- Pires, D.P.; Oliveira, H.; Melo, L.D.R.; Sillankorva, S.; Azeredo, J. Bacteriophage-encoded depolymerases: Their diversity and biotechnological applications. Appl. Microbiol. Biotechnol. 2016, 100, 2141–2151. [Google Scholar] [CrossRef] [PubMed]
- Brzozowska, E.; Pyra, A.; Pawlik, K.; Janik, M.; Górska, S.; Urbańska, N.; Drulis-Kawa, Z.; Gamian, A. Hydrolytic activity determination of Tail Tubular Protein A of Klebsiella pneumoniae bacteriophages towards saccharide substrates. Sci. Rep. 2017, 7, 18048. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.; Paff, M.L.; Molineux, I.J.; Bull, J.J. Therapeutic application of phage capsule depolymerases against K1, K5, and K30 capsulated E. coli in mice. Front. Microbiol. 2017, 8, 2257. [Google Scholar] [CrossRef]
- Chen, Y.; Sun, E.; Yang, L.; Song, J.; Wu, B. Therapeutic Application of Bacteriophage PHB02 and its Putative Depolymerase Against Pasteurella multocida Capsular Type A in Mice. Front. Microbiol. 2018, 9, 1678. [Google Scholar] [CrossRef]
- Olszak, T.; Shneider, M.M.; Latka, A.; Maciejewska, B.; Browning, C.; Sycheva, L.V.; Cornelissen, A.; Danis-Wlodarczyk, K.; Senchenkova, S.N.; Shashkov, A.S.; et al. The O-specific polysaccharide lyase from the phage LKA1 tailsike reduces Pseudomonas virulence. Sci. Rep. 2017, 7, 16302. [Google Scholar] [CrossRef]
- Hernandez-Morales, A.C.; Lessor, L.L.; Wood, T.L.; Migl, D.; Mijalis, E.M.; Cahill, J.; Russell, W.K.; Young, R.F.; Gill, J.J. Genomic and Biochemical Characterization of Acinetobacter Podophage Petty Reveals a Novel Lysis Mechanism and Tail-Associated Depolymerase Activity. J. Virol. 2018, 92, e01064-17. [Google Scholar] [CrossRef]
- Lin, T.L.; Hsieh, P.F.; Huang, Y.T.; Lee, W.C.; Tsai, Y.T.; Su, P.A.; Pan, Y.J.; Hsu, C.R.; Wu, M.C.; Wang, J.T. Isolation of a bacteriophage and its depolymerase specific for K1 capsule of Klebsiella pneumoniae: Implication in typing and treatment. J. Infect. Dis. 2014, 210, 1734–1744. [Google Scholar] [CrossRef]
- Majkowska-Skrobek, G.; Łątka, A.; Berisio, R.; Maciejewska, B.; Squeglia, F.; Romano, M.; Lavigne, R.; Struve, C.; Drulis-Kawa, Z. Capsule-Targeting Depolymerase, Derived from Klebsiella KP36 Phage, as a Tool for the Development of Anti-Virulent Strategy. Viruses 2016, 8, 324. [Google Scholar] [CrossRef]
- Hsieh, P.F.; Lin, H.H.; Lin, T.L.; Chen, Y.Y.; Wang, J.T. Two T7-like Bacteriophages, K5-2 and K5-4, Each Encodes Two Capsule Depolymerases: Isolation and Functional Characterization. Sci. Rep. 2017, 7, 4624. [Google Scholar] [CrossRef]
- Majkowska-Skrobek, G.; Latka, A.; Berisio, R.; Squeglia, F.; Maciejewska, B.; Briers, Y.; Drulis-Kawa, Z. Phage-Borne depolymerases decrease Klebsiella pneumoniae resistance to innate defense mechanisms. Front. Microbiol. 2018, 9, 2517. [Google Scholar] [CrossRef]
- Pan, Y.J.; Lin, T.L.; Lin, Y.T.; Su, P.A.; Chen, C.T.; Hsieh, P.F.; Hsu, C.R.; Chen, C.C.; Hsieh, Y.C.; Wang, J.T. Identification of capsular types in carbapenem-resistant Klebsiella pneumoniae strains by wzc sequencing and implications for capsule depolymerase treatment. Antimicrob. Agents Chemother. 2015, 59, 1038–1047. [Google Scholar] [CrossRef]
- Solovieva, E.V.; Myakinina, V.P.; Kislichkina, A.A.; Krasilnikova, V.M.; Verevkin, V.V.; Mochalov, V.V.; Lev, A.I.; Fursova, N.K.; Volozhantsev, N.V. Comparative genome analysis of novel Podoviruses lytic for hypermucoviscous Klebsiella pneumoniae of K1, K2, and K57 capsular types. Virus Res. 2018, 243, 10–18. [Google Scholar] [CrossRef]
- Pan, Y.J.; Lin, T.L.; Chen, Y.Y.; Lai, P.H.; Tsai, Y.T.; Hsu, C.R.; Hsieh, P.F.; Lin, Y.T.; Wang, J.T. Identification of three podoviruses infecting Klebsiella encoding capsule depolymerases that digest specific capsular types. Microb. Biotechnol. 2019, 12, 472–486. [Google Scholar] [CrossRef]
- Pan, Y.J.; Lin, T.L.; Chen, C.C.; Tsai, Y.T.; Cheng, Y.H.; Chen, Y.Y.; Hsieh, P.F.; Lin, Y.T.; Wang, J.T. Klebsiella Phage ΦK64-1 Encodes Multiple Depolymerases for Multiple Host Capsular Types. J. Virol. 2017, 91, e02457-16. [Google Scholar] [CrossRef]
- Knirel, Y.A.; Shneider, M.M.; Popova, A.V.; Kasimova, A.A.; Senchenkova, S.N.; Shashkov, A.S.; Chizhov, A.O. Mechanisms of Acinetobacter baumannii Capsular Polysaccharide Cleavage by Phage Depolymerases. Biochemistry 2020, 85, 567–574. [Google Scholar] [CrossRef]
- Lee, I.M.; Tu, I.F.; Yang, F.L.; Ko, T.P.; Liao, J.H.; Lin, N.T.; Wu, C.Y.; Ren, C.T.; Wang, A.H.; Chang, C.M.; et al. Structural basis for fragmenting the exopolysaccharide of Acinetobacter baumannii by bacteriophage ΦAB6 tailspike protein. Sci. Rep. 2017, 17, 42711. [Google Scholar] [CrossRef]
- Kamerling, J.P.; Lindberg, B.; Lönngren, J.; Nimmich, W. Structural studies of the Klebsiella type 57 capsular polysaccharide. Acta Chem. Scand. 1975, 29, 593–598. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jansson, P.E.; Kenne, L.; Widmalm, G. Computer-assisted structural analysis of polysaccharides with an extended version of CASPER using 1H- and 13C-n.m.r. data. Carbohydr. Res. 1989, 188, 169–191. [Google Scholar] [CrossRef]
- Dutton, G.G.S.; Parolis, H.; Parolis, L.A.S. The structural elucidation of the capsular polysaccharide of Klebsiella K68. Carbohydr. Res. 1986, 152, 249–259. [Google Scholar] [CrossRef]
- Borzilov, A.I.; Myakinina, V.P.; Korobova, O.V.; Kombarova, T.I.; Krasilnikova, V.M.; Verevkin, V.V.; Volozhantsev, N.V. Evaluation of preventive and therapeutic efficacy of Klebsiella pneumoniae bacteriophage vB_KpnP_KpV289 on the model of acute sepsis in mice. Bacteriology 2017, 2, 73–77. [Google Scholar] [CrossRef]
- Borzilov, A.I.; Volozhantsev, N.V.; Korobova, O.V.; Kombarova, T.I.; Myakinina, V.P.; Krasilnikova, V.M.; Verevkin, V.V.; Svetoch, E.A.; Dyatlov, I.A. The effectiveness of bacteriophage KpV289 in treatment of acute pneumonia and a hip infection caused by Klebsiella pneumoniae in mice. Infekc. Bolezni (Infect. Dis.) 2017, 15, 48–56. [Google Scholar] [CrossRef]
- Liu, Y.; Leung, S.; Huang, Y.; Guo, Y.; Jiang, N.; Li, P.; Chen, J.; Wang, R.; Bai, C.; Mi, Z.; et al. Identification of Two Depolymerases From Phage IME205 and Their Antivirulent Functions on K47 Capsule of Klebsiella pneumoniae. Front. Microbiol. 2020, 11, 218. [Google Scholar] [CrossRef] [PubMed]
- Aziz, R.K.; Bartels, D.; Best, A.A.; DeJongh, M.; Disz, T.; Edwards, R.A.; Formsma, K.; Gerdes, S.; Glass, E.M.; Kubal, M.; et al. The RAST server: Rapid annotations using subsystems technology. BMC Genomics 2008, 9, 75. [Google Scholar] [CrossRef]
- Altschul, S.F.; Gish, W.; Miller, W.; Myers, E.W.; Lipman, D.J. Basic local alignment search tool. J. Mol. Biol. 1990, 215, 403–410. [Google Scholar] [CrossRef]
- Sullivan, M.J.; Petty, N.K.; Beatson, S.A. Easyfig: A genome comparison visualizer. Bioinformatics 2011, 27, 1009–1010. [Google Scholar] [CrossRef]
- Söding, J.; Biegert, A.; Lupas, A.N. The HHpred interactive server for protein homology detection and structure prediction. Nucleic Acids Res. 2005, 33, 244–248. [Google Scholar] [CrossRef]
- Volozhantsev, N.V.; Shpirt, A.M.; Kislichkina, A.A.; Shashkov, A.S.; Verevkin, V.V.; Fursova, N.K.; Knirel, Y.A. Structure and gene cluster of the capsular polysaccharide of multidrug resistant carbapenemase OXA-48-producing Klebsiella pneumoniae strain KPB536 of the genetic line ST147. Res. Microbiol. 2020, 171, 74–79. [Google Scholar] [CrossRef]
- Prokhorov, N.S.; Riccio, C.; Zdorovenko, E.L.; Shneider, M.M.; Browning, C.; Knirel, Y.A.; Leiman, P.G.; Letarov, A.V. Function of bacteriophage G7C esterase tailspike in host cell adsorption. Mol. Microbiol. 2017, 105, 385–398. [Google Scholar] [CrossRef]


| Characteristics | KpV79 | KpV767 |
|---|---|---|
| Isolation source | sewage | sewage |
| Isolation date | Feb-2016 | Nov-2015 |
| Genome length, bp | 47,760 | 40,395 |
| Total genes | 75 | 52 |
| Predicted PS depolymerase gene | kpv79_42 | kpv767_46 |
| The number of strains lysed by phage | ||
| K57 type (n = 21) | 18 b + 3 c | 10 b + 10 c |
| Not-K57 type (n = 229) a | 0 | 0 |
| # | Strain | HV Phenotype | The Efficiency of Plating (EOP) a | Spot-Test b | ||
|---|---|---|---|---|---|---|
| KpV79 | KpV767 | Dep79 | Dep767 | |||
| 1 | KPB1106-2 | − | H | H | ++ | +++ |
| 2 | KPB156 | + | H | H | ++ | + |
| 3 | KPB335 | − | L | T | ++ | + |
| 4 | KPB500 | − | L | - | +/− | − |
| 5 | KPB542-15 | − | M | H | ++ | ++ |
| 6 | KPB550 | − | L | T | ++ | ++ |
| 7 | KPB567 | + | L | T | ++ | ++ |
| 8 | KPB584 | − | T | T | ++ | + |
| 9 | KPB612-1 | + | L | T | ++ | ++ |
| 10 | KPB690 | + | L | T | +++ | ++ |
| 11 | KPB697-1 | − | T | T | ++ | ++ |
| 12 | KPB742 | − | H | H | ++ | ++ |
| 13 | KPB757 | + | L | T | +++ | +++ |
| 14 | KPB774-1 | − | H | H | +++ | +++ |
| 15 | KPB811 | + | T | T | ++ | ++ |
| 16 | KPBP1 | − | M | H | +++ | +++ |
| 17 | KPi112 | − | H | H | ++ | + |
| 18 | KPi4605 | − | H | H | +++ | +++ |
| 19 | KPi4891 | − | H | H | +++ | +++ |
| 20 | KPi8289 | + | H | L | +++ | +++ |
| 21 | KPX4 | − | H | T | ++ | + |
| Residue | H-1 | H-2 | H-3 | H-4 | H-5 | H-6 |
|---|---|---|---|---|---|---|
| C-1 | C-2 | C-3 | C-4 | C-5 | C-6 (6a, 6b) | |
| CPS | ||||||
| →3)–β–δ–Γαλπ–(1→ | 4.66 | 3.64 | 3.72 | 4.01 | 3.63 | 3.77, 3.83 |
| A | 105.7 | 71 | 78 | 65.9 | 76.3 | 62.5 |
| →2)–α–δ–Μανπ–(1→ | 5.21 | 4.05 | 4.02 | 3.77 | 4.01 | 3.75, 3,84 |
| B | 96.2 | 81.2 | 71.6 | 68.4 | 74.1 | 62.3 |
| →3,4)–±–δ–ΓαλπA–(1→ | 5.21 | 4.07 | 4.16 | 4.63 | 4.57 | |
| C | 102.1 | 69.5 | 78.4 | 79 | 72.2 | 174.7 |
| α-d-Manp-(1→ | 4.99 | 3.87 | 3.82 | 3.69 | 4.02 | 3.80, 3,89 |
| D | 101.5 | 71.4 | 71.6 | 68 | 74 | 62.2 |
| OS | ||||||
| →3)–α–δ–Γαλπ | 5.28 | 3.91 | 3.94 | 4.19 | n.f. | 3.73–3.88 |
| Aα | 93.6 | 68.1 | 74.5 | 66.3 | n.f. | 62.5 |
| →3)–β–δ–Γαλπ | 4.61 | 3.56 | 3.73 | 4.12 | 3.65 | 3.73–3.88 |
| Aβ | 97.3 | 71.7 | 77.9 | 65.8 | 76.3 | 62.4 |
| →2)–α–δ–Μανπ–(1→ | 5.22 | 4.02 | 4.03 | 3.78 | 3.84 | 3.73–3.88 |
| B | 96.1 | 81 | 71.7 | 68.4 | 74 | 62.2 |
| →4)–α–δ–ΓαλπA–(1→ | 5.18 | 3.87 | 4.02 | 4.4 | 4.39 | |
| C | 102.1 | 70.1 | 70.3 | 80.5 | 72.6 | n.f. |
| α-d-Manp-(1→ | 4.91 | 3.92 | 3.85 | 3.67 | 3.98 | 3.73–3.88 |
| D | 102.4 | 71.5 | 71.5 | 68 | 74.2 | 62.2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
V. Volozhantsev, N.; M. Shpirt, A.; I. Borzilov, A.; V. Komisarova, E.; M. Krasilnikova, V.; S. Shashkov, A.; V. Verevkin, V.; A. Knirel, Y. Characterization and Therapeutic Potential of Bacteriophage-Encoded Polysaccharide Depolymerases with β Galactosidase Activity against Klebsiella pneumoniae K57 Capsular Type. Antibiotics 2020, 9, 732. https://doi.org/10.3390/antibiotics9110732
V. Volozhantsev N, M. Shpirt A, I. Borzilov A, V. Komisarova E, M. Krasilnikova V, S. Shashkov A, V. Verevkin V, A. Knirel Y. Characterization and Therapeutic Potential of Bacteriophage-Encoded Polysaccharide Depolymerases with β Galactosidase Activity against Klebsiella pneumoniae K57 Capsular Type. Antibiotics. 2020; 9(11):732. https://doi.org/10.3390/antibiotics9110732
Chicago/Turabian StyleV. Volozhantsev, Nikolay, Anna M. Shpirt, Alexander I. Borzilov, Ekaterina V. Komisarova, Valentina M. Krasilnikova, Alexander S. Shashkov, Vladimir V. Verevkin, and Yuriy A. Knirel. 2020. "Characterization and Therapeutic Potential of Bacteriophage-Encoded Polysaccharide Depolymerases with β Galactosidase Activity against Klebsiella pneumoniae K57 Capsular Type" Antibiotics 9, no. 11: 732. https://doi.org/10.3390/antibiotics9110732
APA StyleV. Volozhantsev, N., M. Shpirt, A., I. Borzilov, A., V. Komisarova, E., M. Krasilnikova, V., S. Shashkov, A., V. Verevkin, V., & A. Knirel, Y. (2020). Characterization and Therapeutic Potential of Bacteriophage-Encoded Polysaccharide Depolymerases with β Galactosidase Activity against Klebsiella pneumoniae K57 Capsular Type. Antibiotics, 9(11), 732. https://doi.org/10.3390/antibiotics9110732





