Prevalence and Antibiogram Pattern of Acinetobacter baumannii from 2013 to 2023 in a Tertiary Care Hospital in the Western Region of Saudi Arabia
Abstract
1. Introduction
2. Result
2.1. Distribution and Rate of Isolation
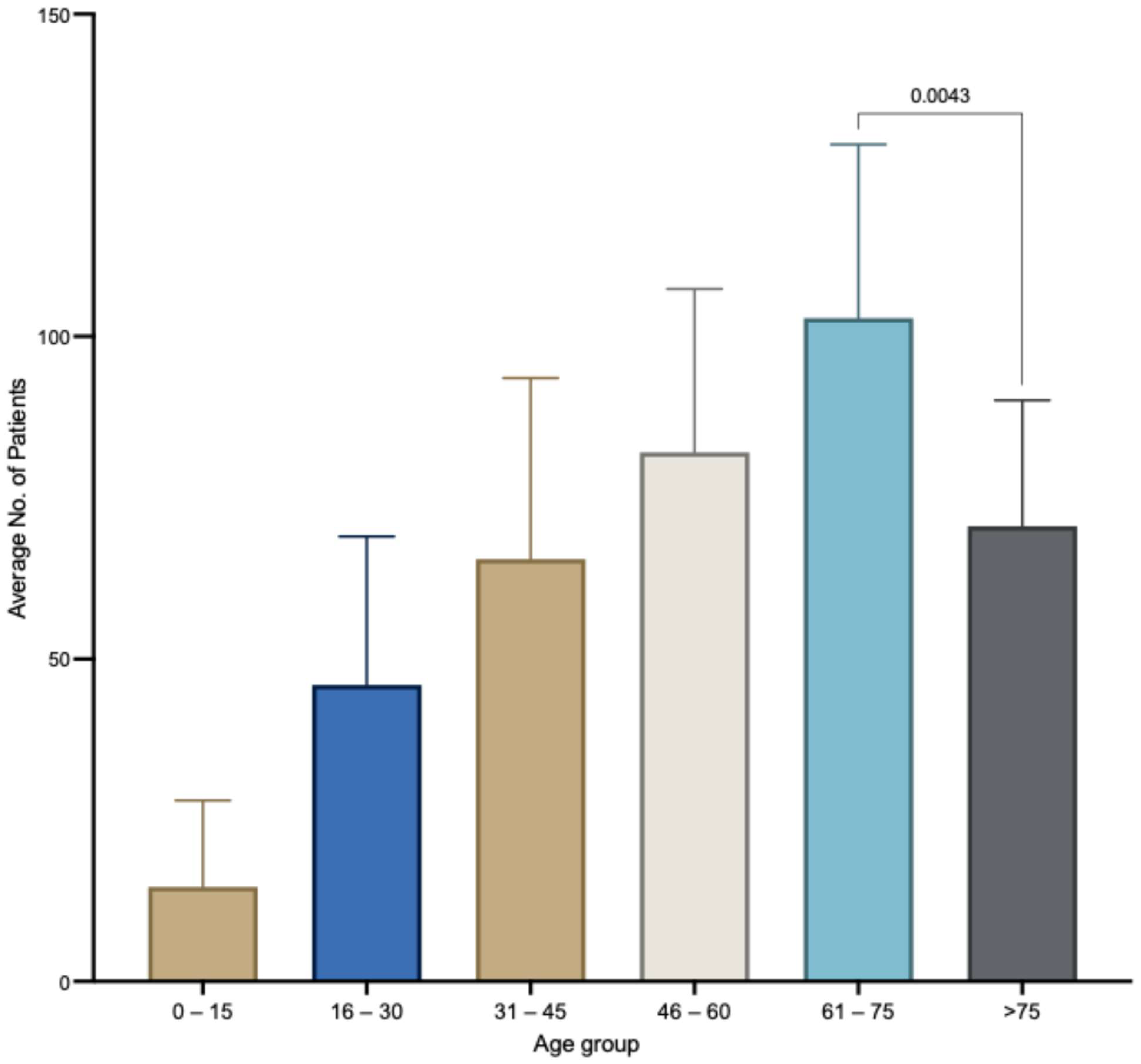
2.2. Patient Demographics
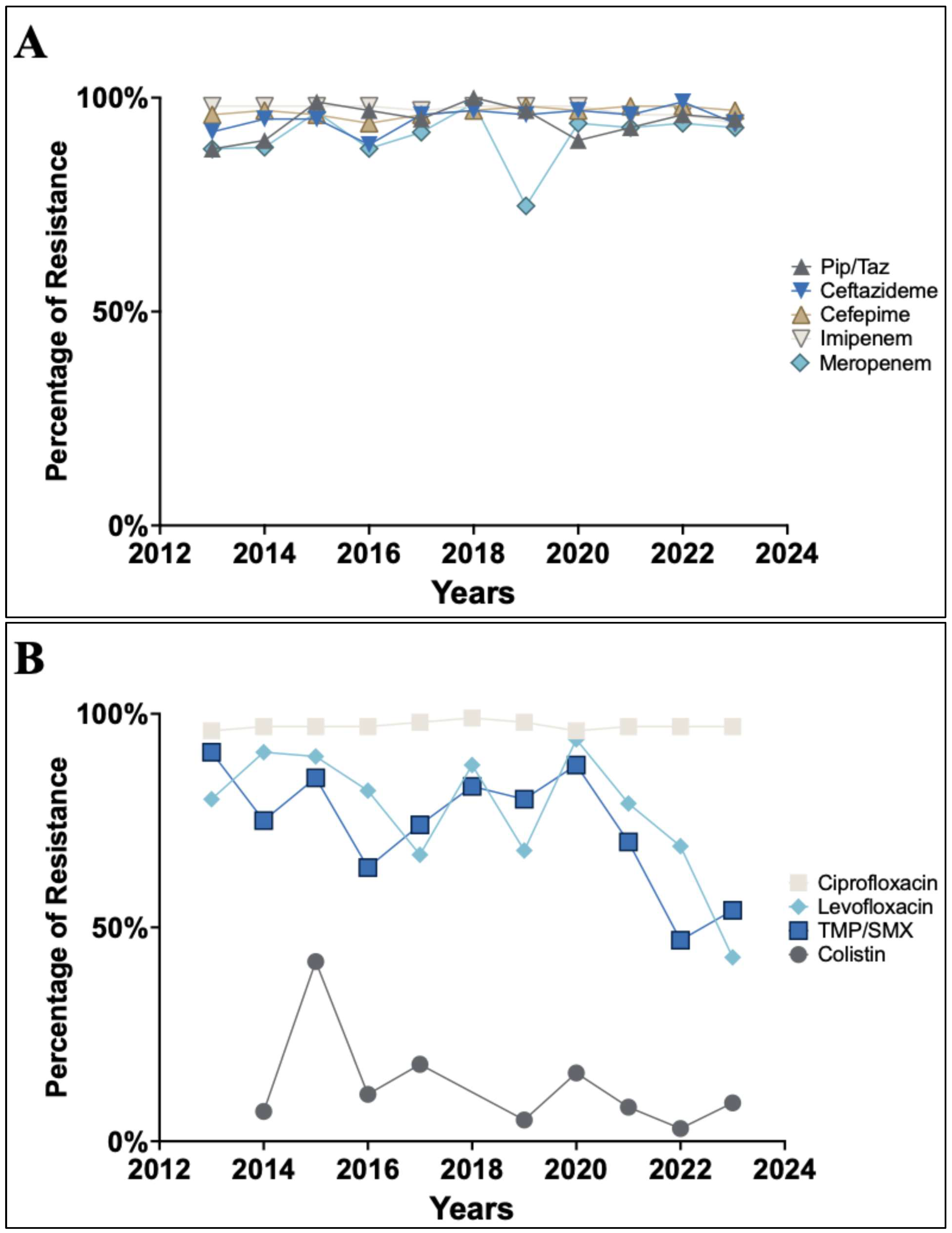
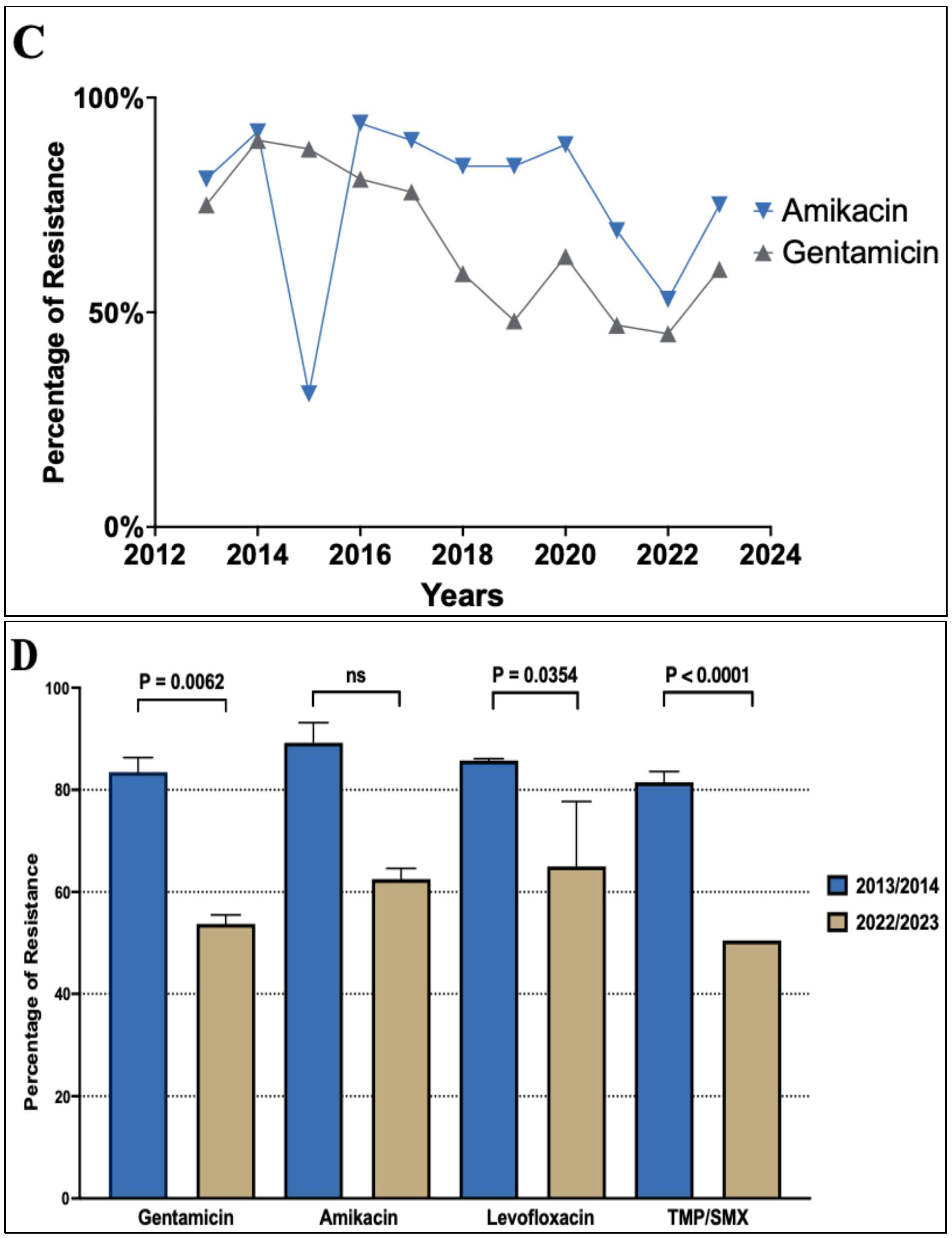
2.3. Antibiotic Susceptibility Profile of A. baumannii
2.4. Prevalence of Carbapenem-Resistant A. baumannii
3. Discussion
4. Materials and Method
4.1. Study Setting
4.2. Bacterial Isolates and Antibiotic Susceptibility
4.3. Statistics and Data Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Montefour, K.; Frieden, J.; Hurst, S.; Helmich, C.; Headley, D.; Martin, M.; Boyle, D.A. Acinetobacter baumannii: An Emerging Multidrug-Resistant Pathogen in Critical Care. Crit. Care Nurse 2008, 28, 15–25. [Google Scholar] [CrossRef]
- Wong, D.; Nielsen, T.B.; Bonomo, R.A.; Pantapalangkoor, P.; Luna, B.; Spellberg, B. Clinical and Pathophysiological Overview of Acinetobacter Infections: A Century of Challenges. Clin. Microbiol. Rev. 2017, 30, 409–447. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, M.E. Prevalence of Acinetobacter baumannii in Saudi Arabia: Risk Factors, Antimicrobial Resistance Patterns and Mechanisms of Carbapenem Resistance. Ann. Clin. Microbiol. Antimicrob. 2019, 18, 1. [Google Scholar] [CrossRef] [PubMed]
- Alrahmany, D.; Omar, A.F.; Alreesi, A.; Harb, G.; Ghazi, I.M. Acinetobacter baumannii Infection-Related Mortality in Hospitalized Patients: Risk Factors and Potential Targets for Clinical and Antimicrobial Stewardship Interventions. Antibiotics 2022, 11, 1086. [Google Scholar] [CrossRef]
- Aly, M.M.; Abu Alsoud, N.M.; Elrobh, M.S.; Al Johani, S.M.; Balkhy, H.H. High Prevalence of the PER-1 Gene among Carbapenem-Resistant Acinetobacter baumannii in Riyadh, Saudi Arabia. Eur. J. Clin. Microbiol. Infect. Dis. 2016, 35, 1759–1766. [Google Scholar] [CrossRef] [PubMed]
- Owen, L.; Laird, K. The Role of Textiles as Fomites in the Healthcare Environment: A Review of the Infection Control Risk. PeerJ 2020, 8, e9790. [Google Scholar] [CrossRef]
- Saliba, R.; Zahar, J.-R.; Dabar, G.; Riachy, M.; Karam-Sarkis, D.; Husni, R. Limiting the Spread of Multidrug-Resistant Bacteria in Low-to-Middle-Income Countries: One Size Does Not Fit All. Pathogens 2023, 12, 144. [Google Scholar] [CrossRef]
- Spellberg, B.; Bonomo, R.A. Airborne Assault. Crit. Care Med. 2013, 41, 2042–2044. [Google Scholar] [CrossRef]
- Peacock, S.J.; Parkhill, J.; Brown, N.M. Changing the Paradigm for Hospital Outbreak Detection by Leading with Genomic Surveillance of Nosocomial Pathogens. Microbiology 2018, 164, 1213–1219. [Google Scholar] [CrossRef]
- Almasaudi, S.B. Acinetobacter spp. as Nosocomial Pathogens: Epidemiology and Resistance Features. Saudi J. Biol. Sci. 2018, 25, 586–596. [Google Scholar] [CrossRef]
- Ayoub Moubareck, C.; Hammoudi Halat, D. Insights into Acinetobacter baumannii: A Review of Microbiological, Virulence, and Resistance Traits in a Threatening Nosocomial Pathogen. Antibiotics 2020, 9, 119. [Google Scholar] [CrossRef] [PubMed]
- Morris, F.C.; Dexter, C.; Kostoulias, X.; Uddin, M.I.; Peleg, A.Y. The Mechanisms of Disease Caused by Acinetobacter baumannii. Front. Microbiol. 2019, 10, 1601. [Google Scholar] [CrossRef] [PubMed]
- Asif, M.; Alvi, I.A.; Rehman, S.U. Insight into Acinetobacter baumannii: Pathogenesis, Global Resistance, Mechanisms of Resistance, Treatment Options, and Alternative Modalities. Infect. Drug Resist. 2018, 11, 1249–1260. [Google Scholar] [CrossRef]
- Rizk, S.S.; Elwakil, W.H.; Attia, A.S. Antibiotic-Resistant Acinetobacter baumannii in Low-Income Countries (2000–2020): Twenty-One Years and Still below the Radar, Is It Not There or Can They Not Afford to Look for It? Antibiotics 2021, 10, 764. [Google Scholar] [CrossRef]
- Kyriakidis, I.; Vasileiou, E.; Pana, Z.D.; Tragiannidis, A. Acinetobacter baumannii Antibiotic Resistance Mechanisms. Pathogens 2021, 10, 373. [Google Scholar] [CrossRef]
- Mea, H.J.; Yong, P.V.C.; Wong, E.H. An Overview of Acinetobacter baumannii Pathogenesis: Motility, Adherence and Biofilm Formation. Microbiol. Res. 2021, 247, 126722. [Google Scholar] [CrossRef]
- Mortensen, B.L.; Skaar, E.P. The Contribution of Nutrient Metal Acquisition and Metabolism to Acinetobacter baumannii Survival within the Host. Front. Cell Infect. Microbiol. 2013, 3, 95. [Google Scholar] [CrossRef] [PubMed]
- Cook-Libin, S.; Sykes, E.M.E.; Kornelsen, V.; Kumar, A. Iron Acquisition Mechanisms and Their Role in the Virulence of Acinetobacter baumannii. Infect. Immun. 2022, 90, e00223-22. [Google Scholar] [CrossRef]
- Johnson, T.L.; Waack, U.; Smith, S.; Mobley, H.; Sandkvist, M. Acinetobacter baumannii Is Dependent on the Type II Secretion System and Its Substrate LipA for Lipid Utilization and in vivo Fitness. J. Bacteriol. 2016, 198, 711–719. [Google Scholar] [CrossRef]
- Elhosseiny, N.M.; Elhezawy, N.B.; Attia, A.S. Comparative Proteomics Analyses of Acinetobacter baumannii Strains ATCC 17978 and AB5075 Reveal the Differential Role of Type II Secretion System Secretomes in Lung Colonization and Ciprofloxacin Resistance. Microb. Pathog. 2019, 128, 20–27. [Google Scholar] [CrossRef]
- Lee, J.S.; Choi, C.H.; Kim, J.W.; Lee, J.C. Acinetobacter baumannii Outer Membrane Protein a Induces Dendritic Cell Death through Mitochondrial Targeting. J. Microbiol. 2010, 48, 387–392. [Google Scholar] [CrossRef] [PubMed]
- Repizo, G.D.; Gagné, S.; Foucault-Grunenwald, M.-L.; Borges, V.; Charpentier, X.; Limansky, A.S.; Gomes, J.P.; Viale, A.M.; Salcedo, S.P. Differential Role of the T6SS in Acinetobacter baumannii Virulence. PLoS ONE 2015, 10, e0138265. [Google Scholar] [CrossRef] [PubMed]
- Gales, A.C.; Seifert, H.; Gur, D.; Castanheira, M.; Jones, R.N.; Sader, H.S. Antimicrobial Susceptibility of Acinetobacter Calcoaceticus–Acinetobacter baumannii Complex and Stenotrophomonas Maltophilia Clinical Isolates: Results From the SENTRY Antimicrobial Surveillance Program (1997–2016). Open Forum Infect. Dis. 2019, 6 (Suppl. S1), S34–S46. [Google Scholar] [CrossRef]
- Cassini, A.; Högberg, L.D.; Plachouras, D.; Quattrocchi, A.; Hoxha, A.; Simonsen, G.S.; Colomb-Cotinat, M.; Kretzschmar, M.E.; Devleesschauwer, B.; Cecchini, M.; et al. Attributable Deaths and Disability-Adjusted Life-Years Caused by Infections with Antibiotic-Resistant Bacteria in the EU and the European Economic Area in 2015: A Population-Level Modelling Analysis. Lancet Infect. Dis. 2019, 19, 56–66. [Google Scholar] [CrossRef] [PubMed]
- Peleg, A.Y.; Seifert, H.; Paterson, D.L. Acinetobacter baumannii: Emergence of a Successful Pathogen. Clin. Microbiol. Rev. 2008, 21, 538–582. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.-F. Antimicrobial Resistance in Acinetobacter baumannii: From Bench to Bedside. World J. Clin. Cases 2014, 2, 787. [Google Scholar] [CrossRef]
- Poirel, L.; Bonnin, R.A.; Nordmann, P. Genetic Basis of Antibiotic Resistance in Pathogenic Acinetobacter Species. IUBMB Life 2011, 63, 1061–1067. [Google Scholar] [CrossRef]
- Zowawi, H.M.; Balkhy, H.H.; Walsh, T.R.; Paterson, D.L. β-Lactamase Production in Key Gram-Negative Pathogen Isolates from the Arabian Peninsula. Clin. Microbiol. Rev. 2013, 26, 361–380. [Google Scholar] [CrossRef]
- Baadani, A.M.; Thawadi, S.I.; El-Khizzi, N.A.; Omrani, A.S. Prevalence of Colistin and Tigecycline Resistance in Acinetobacter baumannii Clinical Isolates from 2 Hospitals in Riyadh Region over a 2-Year Period. Saudi Med. J. 2013, 34, 248–253. [Google Scholar]
- Said, K.B.; Al-Jarbou, A.N.; Alrouji, M. Surveillance of Antimicrobial Resistance among Clinical Isolates Recovered from a Tertiary Care Hospital in Al Qassim, Saudi Arabia. Int. J. Health Sci. 2014, 8, 3–12. [Google Scholar] [CrossRef]
- Cillóniz, C.; Dominedò, C.; Torres, A. Multidrug Resistant Gram-Negative Bacteria in Community-Acquired Pneumonia. Crit. Care 2019, 23, 79. [Google Scholar] [CrossRef] [PubMed]
- Gautam, D.; Dolma, K.G.; Khandelwal, B.; Mitsuwan, W.; Mahboob, T.; Pereira, M.L.; Nawaz, M.; Wiart, C.; Ardebili, A.; Siyadatpanah, A.; et al. Acinetobacter baumannii: An Overview of Emerging Multidrug-Resistant Pathogen. Med. J. Malaysia 2022, 77, 357–370. [Google Scholar]
- MJoly-Guillou, M.L.; Brun-Buisson, C. Epidemiology of Acinetobacter spp.: Surveillance and Management of Outbreaks. In Acinetobacter; CRC Press: Boca Raton, FL, USA, 1995. [Google Scholar]
- Meschiari, M.; Kaleci, S.; Orlando, G.; Selmi, S.; Santoro, A.; Bacca, E.; Menozzi, M.; Franceschini, E.; Puzzolante, C.; Bedini, A.; et al. Risk Factors for Nosocomial Rectal Colonization with Carbapenem-Resistant Acinetobacter baumannii in Hospital: A Matched Case–Control Study. Antimicrob. Resist. Infect. Control 2021, 10, 69. [Google Scholar] [CrossRef]
- Elbehiry, A.; Marzouk, E.; Moussa, I.; Mushayt, Y.; Algarni, A.A.; Alrashed, O.A.; Alghamdi, K.S.; Almutairi, N.A.; Anagreyyah, S.A.; Alzahrani, A.; et al. The Prevalence of Multidrug-Resistant Acinetobacter baumannii and Its Vaccination Status among Healthcare Providers. Vaccines 2023, 11, 1171. [Google Scholar] [CrossRef] [PubMed]
- Wareth, G.; Brandt, C.; Sprague, L.D.; Neubauer, H.; Pletz, M.W. WGS Based Analysis of Acquired Antimicrobial Resistance in Human and Non-Human Acinetobacter baumannii Isolates from a German Perspective. BMC Microbiol. 2021, 21, 210. [Google Scholar] [CrossRef]
- Sánchez-Urtaza, S.; Ocampo-Sosa, A.; Molins-Bengoetxea, A.; El-Kholy, M.A.; Hernandez, M.; Abad, D.; Shawky, S.M.; Alkorta, I.; Gallego, L. Molecular Characterization of Multidrug Resistant Acinetobacter baumannii Clinical Isolates from Alexandria, Egypt. Front. Cell Infect. Microbiol. 2023, 13, 1208046. [Google Scholar] [CrossRef] [PubMed]
- Esposito, S.; De Simone, G. Update on the Main MDR Pathogens: Prevalence and Treatment Options. Infez. Med. 2017, 25, 301–310. [Google Scholar]
- Cavalieri, S.J.; Kwon, S.; Vivekanandan, R.; Ased, S.; Carroll, C.; Anthone, J.; Schmidt, D.; Baysden, M.; Destache, C.J. Effect of Antimicrobial Stewardship with Rapid MALDI-TOF Identification and Vitek 2 Antimicrobial Susceptibility Testing on Hospitalization Outcome. Diagn. Microbiol. Infect. Dis. 2019, 95, 208–211. [Google Scholar] [CrossRef]
- Al Mobarak, M.F.; Matbuli, R.M.; Meir, H.; Al Gehani, N.; El Toukhy, A.A.M.; Al Qureshey, K.F.; Mutwalli, A.H.; Abdulaziz, A.M.; Hadhoud, A. Antimicrobial Resistance Patterns among Acinetobacter baumannii Isolated from King Abdulaziz Hospital, Jeddah, Saudi Arabia, Four-Year Surveillance Study (2010–2013). Egypt J. Med. Microbiol. 2014, 38, 53–60. [Google Scholar] [CrossRef]
- WHO. WHO Bacterial Priority Pathogens List, 2024: Bacterial Pathogens of Public Health Importance to Guide Research, Development and Strategies to Prevent and Control Antimicrobial Resistance; WHO: Geneva, Switzerland, 2024; p. 72.
- Kharaba, A.; Abdelaziz Hussein, M.; Al-Hameed, F.; Mandourah, Y.; Almekhlafi, G.; Algethamy, H.; Hamdan, A.; Azem, M.; Fatani, J.; al Beshabshe, A.; et al. Acinetobacter baumannii in Saudi Arabia: The New Growing Threat. Saudi Crit. Care J. 2019, 3, 54. [Google Scholar] [CrossRef]
- Balkhy, H.H.; Assiri, A.M.; Al Mousa, H.; Al-Abri, S.S.; Al-Katheeri, H.; Alansari, H.; Abdulrazzaq, N.M.; Aidara-Kane, A.; Pittet, D.; Pittet, D.; et al. The Strategic Plan for Combating Antimicrobial Resistance in Gulf Cooperation Council States. J. Infect. Public Health 2016, 9, 375–385. [Google Scholar] [CrossRef]
- Gaifer, Z.; Fallatah, R.; Alanazi, A.; Alfagi, R.; Alharbi, L.; Osman, H. Prevalence, Risk Factors, and Outcome of Carbapenem-Resistant Acinetobacter Infections in a Community Hospital in Madinah, Saudi Arabia. Saudi J. Med. Med. Sci. 2024, 12, 306–313. [Google Scholar] [CrossRef]
- Xie, R.; Zhang, X.D.; Zhao, Q.; Peng, B.; Zheng, J. Analysis of Global Prevalence of Antibiotic Resistance in Acinetobacter baumannii Infections Disclosed a Faster Increase in OECD Countries. Emerg. Microbes Infect. 2018, 7, 31. [Google Scholar] [CrossRef] [PubMed]
- Alzahrani, K.O.; Alshahrani, S.M.; Alajel, S.M. Evaluating the Effectiveness of the Ministry of Health Restriction Policy on Seasonal Antibiotic Consumption Trends in Saudi Arabia, 2016–2020. Front. Pharmacol. 2023, 14, 1242087. [Google Scholar] [CrossRef] [PubMed]
- Högberg, L.D.; Vlahović-Palčevski, V.; Pereira, C.; Weist, K.; Monnet, D.L. Decrease in Community Antibiotic Consumption during the COVID-19 Pandemic, EU/EEA, 2020. Eurosurveillance 2021, 26, 2101020. [Google Scholar] [CrossRef] [PubMed]
- Rezel-Potts, E.; L’Esperance, V.; Gulliford, M.C. Antimicrobial Stewardship in the UK during the COVID-19 Pandemic: A Population-Based Cohort Study and Interrupted Time-Series Analysis. Br. J. Gen. Pract. 2021, 71, e331–e338. [Google Scholar] [CrossRef]
- Al-Azzam, S.; Mhaidat, N.M.; Banat, H.A.; Alfaour, M.; Ahmad, D.S.; Muller, A.; Al-Nuseirat, A.; Lattyak, E.A.; Conway, B.R.; Aldeyab, M.A. An Assessment of the Impact of Coronavirus Disease (COVID-19) Pandemic on National Antimicrobial Consumption in Jordan. Antibiotics 2021, 10, 690. [Google Scholar] [CrossRef]
- Lowings, M.; Ehlers, M.M.; Dreyer, A.W.; Kock, M.M. High Prevalence of Oxacillinases in Clinical Multidrug-Resistant Acinetobacter baumannii Isolates from the Tshwane Region, South Africa—An Update. BMC Infect. Dis. 2015, 15, 521. [Google Scholar] [CrossRef]
- Momenah, A.M.; Bakri, R.A.; Jalal, N.A.; Ashgar, S.S.; Felemban, R.F.; Bantun, F.; Hariri, S.H.; Barhameen, A.A.; Faidah, H.; AL-Said, H.M. Antimicrobial Resistance Pattern of Pseudomonas Aeruginosa: An 11-Year Experience in a Tertiary Care Hospital in Makkah, Saudi Arabia. Infect. Drug Resist. 2023, 16, 4113–4122. [Google Scholar] [CrossRef]
- Bostanghadiri, N.; Narimisa, N.; Mirshekar, M.; Dadgar-Zankbar, L.; Taki, E.; Navidifar, T.; Darban-Sarokhalil, D. Prevalence of Colistin Resistance in Clinical Isolates of Acinetobacter baumannii: A Systematic Review and Meta-Analysis. Antimicrob. Resist. Infect. Control 2024, 13, 24. [Google Scholar] [CrossRef]
- Novović, K.; Jovčić, B. Colistin Resistance in Acinetobacter baumannii: Molecular Mechanisms and Epidemiology. Antibiotics 2023, 12, 516. [Google Scholar] [CrossRef] [PubMed]
- Jalal, N.A.; Al-Ghamdi, A.M.; Momenah, A.M.; Ashgar, S.S.; Bantun, F.; Bahwerth, F.S.; Hariri, S.H.; Johargy, A.K.; Barhameen, A.A.; Al-Said, H.M.; et al. Prevalence and Antibiogram Pattern of Klebsiella Pneumoniae in a Tertiary Care Hospital in Makkah, Saudi Arabia: An 11-Year Experience. Antibiotics 2023, 12, 164. [Google Scholar] [CrossRef] [PubMed]
- Mihu, M.R.; Martinez, L.R. Novel Therapies for Treatment of Multi-Drug Resistant Acinetobacter baumannii Skin Infections. Virulence 2011, 2, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Ayobami, O.; Willrich, N.; Harder, T.; Okeke, I.N.; Eckmanns, T.; Markwart, R. The Incidence and Prevalence of Hospital-Acquired (Carbapenem-Resistant) Acinetobacter baumannii in Europe, Eastern Mediterranean and Africa: A Systematic Review and Meta-Analysis. Emerg. Microbes Infect. 2019, 8, 1747–1759. [Google Scholar] [CrossRef]
- Kharaba, A.; Algethamy, H.; Hussein, M.; Al-Hameed, F.M.; Alghamdi, A.; Hamdan, A.; Fatani, J.; Elhazmi, A.; Alkhalaf, H.; Barghash, B.; et al. Incidence, Outcomes, and Predictors of Acinetobacter Infection in Saudi Arabian Critical Care Units. J. Crit. Care 2021, 66, 109–116. [Google Scholar] [CrossRef]
- Jung, J.Y.; Park, M.S.; Kim, S.E.; Park, B.H.; Son, J.Y.; Kim, E.Y.; Lim, J.E.; Lee, S.K.; Lee, S.H.; Lee, K.J.; et al. Risk Factors for Multi-Drug Resistant Acinetobacter baumannii bacteremia in Patients with Colonization in the Intensive Care Unit. BMC Infect. Dis. 2010, 10, 228. [Google Scholar] [CrossRef]
- Aljindan, R.; Bukharie, H.; Alomar, A.; Abdalhamid, B. Prevalence of Digestive Tract Colonization of Carbapenem-Resistant Acinetobacter baumannii in Hospitals in Saudi Arabia. J. Med. Microbiol. 2015, 64, 400–406. [Google Scholar] [CrossRef]
- Ma, C.; McClean, S. Mapping Global Prevalence of Acinetobacter baumannii and Recent Vaccine Development to Tackle It. Vaccines 2021, 9, 570. [Google Scholar] [CrossRef]
- Lewis, T.; Loman, N.J.; Bingle, L.; Jumaa, P.; Weinstock, G.M.; Mortiboy, D.; Pallen, M.J. High-Throughput Whole-Genome Sequencing to Dissect the Epidemiology of Acinetobacter baumannii Isolates from a Hospital Outbreak. J. Hosp. Infect. 2010, 75, 37–41. [Google Scholar] [CrossRef]
- Shenoy, E.S.; Pierce, V.M.; Sater, M.R.A.; Pangestu, F.K.; Herriott, I.C.; Anahtar, M.N.; Bramante, J.T.; Kwon, D.S.; Hawkins, F.R.; Suslak, D.; et al. Community-Acquired in Name Only: A Cluster of Carbapenem-Resistant Acinetobacter baumannii in a Burn Intensive Care Unit and Beyond. Infect. Control Hosp. Epidemiol. 2020, 41, 531–538. [Google Scholar] [CrossRef]
- CLSI. Performance Standards for Antimicrobial Disk Susceptibility Tests; Approved Standard, 11th ed.; CLSI: Wayne, PA, USA, 2012. [Google Scholar]


| Years | Inpatient | Outpatient | Total | ||||
|---|---|---|---|---|---|---|---|
| Burn | Pediatric | Medical Wards | Surgical Wards | ICUs | ER and Clinic | ||
| 2013 | 50 (6.5%) | 43 (5.9%) | 122 (16.9%) | 124 (17.1%) | 385 (53.2%) | 44 | 768 |
| 2014 | 20 (3.4%) | 8 (1.3%) | 90 (15.1%) | 157 (26.3%) | 321 (53.9%) | 32 | 628 |
| 2015 | 33 (4.8%) | 24 (3.5%) | 109 (16.0%) | 181 (26.5%) | 336 (49.2%) | 34 | 717 |
| 2016 | 11 (2.4%) | 5 (1.1%) | 127 (27.6%) | 67 (14.6%) | 250 (54.3%) | 8 | 468 |
| 2017 | 43 (9.0%) | 4 (0.8%) | 70 (14.6%) | 40 (8.4%) | 322 (67.2%) | 16 | 495 |
| 2018 | 32 (10.2%) | 6 (1.9%) | 50 (16.0%) | 62 (19.8%) | 163 (52.1%) | 27 | 340 |
| 2019 | 35 (9.3%) | 4 (1.1%) | 88 (23.3%) | 54 (14.3%) | 197 (52.1%) | 20 | 398 |
| 2020 | 41 (11.0%) | 1 (0.3%) | 46 (12.3%) | 50 (13.4%) | 235 (63%) | 5 | 378 |
| 2021 | 67 (14.3%) | - | 117 (24.9%) | 63 (13.4%) | 222 (47.3%) | 6 | 475 |
| 2022 | 45 (8.8%) | - | 131 (25.5%) | 91 (17.7%) | 246 (48.0%) | 27 | 540 |
| 2023 | 44 (8.0%) | - | 154 (28.0%) | 95 (17.3%) | 257 (46.7%) | 20 | 570 |
| Total | 421 | 95 | 1104 | 984 | 2934 | 239 | 5777 |
| Sample Type, Quantity, and % | Year | Total | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | 2023 | |||
| Sputum | A.baumannii | 382 | 312 | 313 | 229 | 227 | 143 | 175 | 171 | 181 | 254 | 249 | 2636 |
| Total isolates | 1417 | 1173 | 1086 | 912 | 778 | 842 | 785 | 803 | 897 | 789 | 1079 | 10,561 | |
| % of A. baumannii | 27% | 27% | 29% | 25% | 29% | 17% | 22% | 21% | 20% | 32% | 23% | 25% | |
| Blood | A.baumannii | 78 | 66 | 89 | 68 | 107 | 38 | 61 | 76 | 100 | 80 | 110 | 873 |
| Total isolates | 1075 | 382 | 1015 | 972 | 1083 | 1083 | 1208 | 1075 | 2038 | 1200 | 1130 | 12,261 | |
| % of A. baumannii | 7% | 17% | 9% | 7% | 10% | 4% | 5% | 7% | 5% | 7% | 10% | 7% | |
| Catheter tip | A.baumannii | 16 | 15 | 4 | 2 | 4 | 4 | 4 | 3 | 7 | 3 | 7 | 69 |
| Total isolates | 117 | 78 | 58 | 76 | 67 | 54 | 45 | 40 | 65 | 41 | 37 | 678 | |
| % of A. baumannii | 14% | 19% | 7% | 3% | 6% | 7% | 9% | 8% | 11% | 7% | 19% | 10% | |
| Wound | A.baumannii | 172 | 167 | 224 | 120 | 129 | 117 | 128 | 100 | 147 | 129 | 131 | 1564 |
| Total isolates | 1563 | 1560 | 1442 | 1274 | 1164 | 1164 | 1136 | 881 | 1183 | 826 | 1150 | 13,343 | |
| % of A. baumannii | 11% | 11% | 16% | 9% | 11% | 10% | 11% | 11% | 12% | 16% | 11% | 12% | |
| Urine culture | A.baumannii | 26 | 11 | 23 | 11 | 10 | 12 | 3 | 6 | 16 | 24 | 15 | 157 |
| Total isolates | 1050 | 523 | 674 | 774 | 918 | 918 | 1136 | 565 | 948 | 593 | 786 | 8885 | |
| % of A. baumannii | 2% | 2% | 3% | 1% | 1% | 1% | 0% | 1% | 2% | 4% | 2% | 2% | |
| Others | A.baumannii | 94 | 57 | 64 | 38 | 18 | 26 | 27 | 22 | 24 | 50 | 58 | 478 |
| Total isolates | 874 | 812 | 759 | 714 | 917 | 917 | 769 | 665 | 959 | 625 | 924 | 8935 | |
| % of A. baumannii | 11% | 7% | 8% | 5% | 2% | 3% | 4% | 3% | 3% | 8% | 6% | 5% | |
| Total | A.baumannii | 768 | 628 | 717 | 468 | 495 | 340 | 398 | 378 | 475 | 540 | 570 | 5777 |
| Total isolates | 6096 | 4528 | 5034 | 4722 | 4927 | 4978 | 5079 | 4029 | 6090 | 4074 | 5106 | 54,663 | |
| % of A. baumannii | 13% | 14% | 14% | 10% | 10% | 7% | 8% | 9% | 8% | 13% | 11% | 11% | |
| Year | A. baumannii Isolates | Male | (%) | Female | (%) |
|---|---|---|---|---|---|
| 2013 | 768 | 538 | 70 | 230 | 30 |
| 2014 | 628 | 447 | 71 | 181 | 29 |
| 2015 | 717 | 474 | 66 | 243 | 34 |
| 2016 | 468 | 330 | 70 | 138 | 30 |
| 2017 | 495 | 326 | 66 | 169 | 34 |
| 2018 | 340 | 212 | 62 | 128 | 38 |
| 2019 | 398 | 247 | 62 | 151 | 38 |
| 2020 | 378 | 253 | 67 | 125 | 33 |
| 2021 | 475 | 319 | 67 | 156 | 33 |
| 2022 | 540 | 378 | 70 | 162 | 30 |
| 2023 | 570 | 393 | 68 | 177 | 32 |
| Total | 5777 | 3917 | 67 | 1860 | 33 |
| Antibiotic | Year-Wise Prevalence (%) of Resistant A. baumannii | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | 2023 | |
| Ampicillin | 98.8 | NED | 100% | 100% | 100% | 88.2 | 99 | 100 | NED | 73.3 | 99.4 |
| Piperacillin/Tazobactam | 88.2 | 90.0 | 100 | 97.4% | 95.9 | 100 | 97.0 | 90.0 | 93.9 | 96.3 | 95.0 |
| Ceftazidime | 92.0 | 95.9 | 95.6 | 89.9% | 96.2 | 97.5 | 96.8 | 97.7 | 96.8 | 99.1 | 94.1 |
| Cefotaxime | 96.2 | 96.7 | 98.8 | 96.1% | 96.5 | 100 | 100 | 89.5 | 100 | 100 | NED |
| Cefepime | 96.5 | 97.3 | 96.7 | 94.5% | 96.6 | 97.5 | 98.6 | 97.4 | 98.0 | 98.4 | 97.9 |
| Imipenem | 98.2 | 98.9 | 98.3 | 97.4% | 96.2 | 98.7 | 98.6 | 98.6 | 96.9 | 96.0 | 94.6 |
| Meropenem | 88.4 | 96.6 | 88.1 | 91.9% | 91.0 | 98.7 | 74.7 | 94.4 | 93.2 | 94.9 | 93.8 |
| Gentamicin | 75.6 | 90.7 | 88.3 | 81.2 | 78.7 | 59 | 48.5 | 63.2 | 47.0 | 45.6 | 60.7 |
| Amikacin | 81.4 | 92.4 | 31.4 | 94.9 | 90.2 | 84.6 | 84.5 | 89.3 | 69.0 | 53.8 | 74.8 |
| Ciprofloxacin | 96.4 | 97.2 | 97.1 | 97.1 | 98.7 | 99.3 | 98.3 | 96.5 | 97.6 | 97.5 | 97.3 |
| Levofloxacin | 80.2 | 91.8 | 90.8 | 82.0 | 67.6 | 88.4 | 68.9 | 94.6 | 79.7 | 69.0 | 43.4 |
| Colistin | NED | 7.1 | 42.9 | 11.3 | 18.3 | NED | 5.3 | 16.5 | 8.3 | 3.7 | 9.3 |
| TMP/SMX | 91.0 | 75.7 | 85.9 | 64.5 | 74.3 | 83.0 | 80.0 | 88.8 | 70.8 | 47.0 | 54.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alharbi, O.; Al-Said, H.M.; Ashgar, S.S.; Jalal, N.A.; Faidah, H.; Momenah, A.M.; Johargy, A.K.; Bantun, F.; Qashqari, F.S.; Faidah, O.H.; et al. Prevalence and Antibiogram Pattern of Acinetobacter baumannii from 2013 to 2023 in a Tertiary Care Hospital in the Western Region of Saudi Arabia. Antibiotics 2025, 14, 274. https://doi.org/10.3390/antibiotics14030274
Alharbi O, Al-Said HM, Ashgar SS, Jalal NA, Faidah H, Momenah AM, Johargy AK, Bantun F, Qashqari FS, Faidah OH, et al. Prevalence and Antibiogram Pattern of Acinetobacter baumannii from 2013 to 2023 in a Tertiary Care Hospital in the Western Region of Saudi Arabia. Antibiotics. 2025; 14(3):274. https://doi.org/10.3390/antibiotics14030274
Chicago/Turabian StyleAlharbi, Ohood, Hamdi M. Al-Said, Sami S. Ashgar, Naif A. Jalal, Hani Faidah, Aiman M. Momenah, Ayman K. Johargy, Farkad Bantun, Fadi S. Qashqari, Omar Hani Faidah, and et al. 2025. "Prevalence and Antibiogram Pattern of Acinetobacter baumannii from 2013 to 2023 in a Tertiary Care Hospital in the Western Region of Saudi Arabia" Antibiotics 14, no. 3: 274. https://doi.org/10.3390/antibiotics14030274
APA StyleAlharbi, O., Al-Said, H. M., Ashgar, S. S., Jalal, N. A., Faidah, H., Momenah, A. M., Johargy, A. K., Bantun, F., Qashqari, F. S., Faidah, O. H., Bukhari, M. A., & Ibrahem, K. (2025). Prevalence and Antibiogram Pattern of Acinetobacter baumannii from 2013 to 2023 in a Tertiary Care Hospital in the Western Region of Saudi Arabia. Antibiotics, 14(3), 274. https://doi.org/10.3390/antibiotics14030274





