Household Knowledge of Clinical Risks, Storage, and Disposal of Leftover Antibiotics: A Multinational Study in Seven Developing Countries
Abstract
1. Introduction
2. Results
2.1. Sociodemographic Factors
2.2. Knowledge of Antibiotics, Uses, Resistance, and SMLA-Associated Risks
2.3. Storage and Disposal Methods of LAs
3. Discussion
Limitations
- The reliance on self-reported behaviors introduces potential social desirability bias, leading to the underestimation of inappropriate practices.
- The cross-sectional design precludes establishing causal relationships between knowledge and practices, limiting our ability to determine whether knowledge improvements precede behavioral changes.
- The sample’s demographic composition, predominantly consisting of young, highly educated females, limits the generalizability of the findings, particularly to lower-educated and rural groups, and may overestimate general awareness while underestimating unsafe practices.
- While the study employed validated knowledge assessment tools, the behavioral measures did not capture the frequency, duration, or contextual triggers of self-medication practices, which would offer more nuanced intervention targets.
- The multinational sampling approach may not reflect country-specific determinants that require tailored interventions. Country-stratified analyses with sufficient statistical power would enable more contextually appropriate recommendations while maintaining cross-national comparative insights.
4. Materials and Methods
4.1. Study Design and Participants
4.2. Measurements
4.2.1. Sociodemographic Characteristics
4.2.2. Knowledge About Antibiotic Use, Resistance, and Risks Associated with SMLA
4.2.3. Storage and Disposal of Leftover Antibiotics
4.3. Data Collection
4.4. Statistical Analysis
4.5. Sample Size Calculation
4.6. Ethical Approval
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AB | Antibiotics |
| LAs | Leftover antibiotics |
| SMLA | Self-medication with leftover antibiotics |
| SD | Standard deviation |
| HICI | Household crowding index |
| KAP | Knowledge, attitude, and practice |
| LMICs | Low- and middle-income countries |
| HICs | High-income countries |
| WHO | World Health Organization |
Appendix A
Appendix A.1. Knowledge of Antibiotics and Antibiotics Use
- -
- Antibiotics can cause allergic reactions.
- -
- Antibiotics can cause vomiting and nausea.
- -
- Antibiotics can cause diarrhea.
- -
- Antibiotics can cause abdominal pain.
- -
- Antibiotics can cause skin reactions (rashes/ulcers).
- -
- Antibiotics can cause liver toxicity.
- -
- Antibiotics can cause kidney toxicity.
- -
- If you have side effects during a course of antibiotics treatment, you should see your doctor immediately.
- -
- If you have a history of side effects or allergy to antibiotics, you should inform your doctor/pharmacist.
- -
- Antibiotics can cause imbalance in the body’s own bacterial flora (good bacteria).
- -
- It is okay to use leftover antibiotics from previous treatments.
- -
- It is okay to use antibiotics that were given to a friend or family member, as long as they are used to treat the same illness.
- -
- It is okay to save antibiotics for later use.
- -
- It is okay to buy antibiotics without a prescription.
- -
- I should stop taking antibiotics used for my treatment when I feel better.
Appendix A.2. Knowledge About Antibiotic Resistance
- -
- Many infections are becoming increasingly resistant to treatment by antibiotics.
- -
- Antibiotic resistance is an issue that could affect me and the future generation.
- -
- Antibiotic resistance is an issue in other countries but not in my country.
- -
- Antibiotic resistance is only a problem for people who take antibiotics regularly.
- -
- Bacteria which are resistant to antibiotics can be spread from person to person.
- -
- You can be a carrier of resistant bacteria and pass them to your friends and/or family members.
- -
- Antibiotic-resistant infections could make medical procedures like surgery, organ transplants, and cancer treatment much more dangerous.
- -
- If you become sick and your bacteria are resistant to your prescribed antibiotic, your illness could last longer.
- -
- Taking antibiotics unnecessarily may contribute to the development of antibiotic resistance.
- -
- Completing the course of antibiotic prescribed is important to completely kill the bacteria that cause your illness.
- -
- The use of antibiotics among animals can reduce the effect of antibiotics among humans.
- -
- Animals can act as carriers of resistant bacteria and pass them to human.
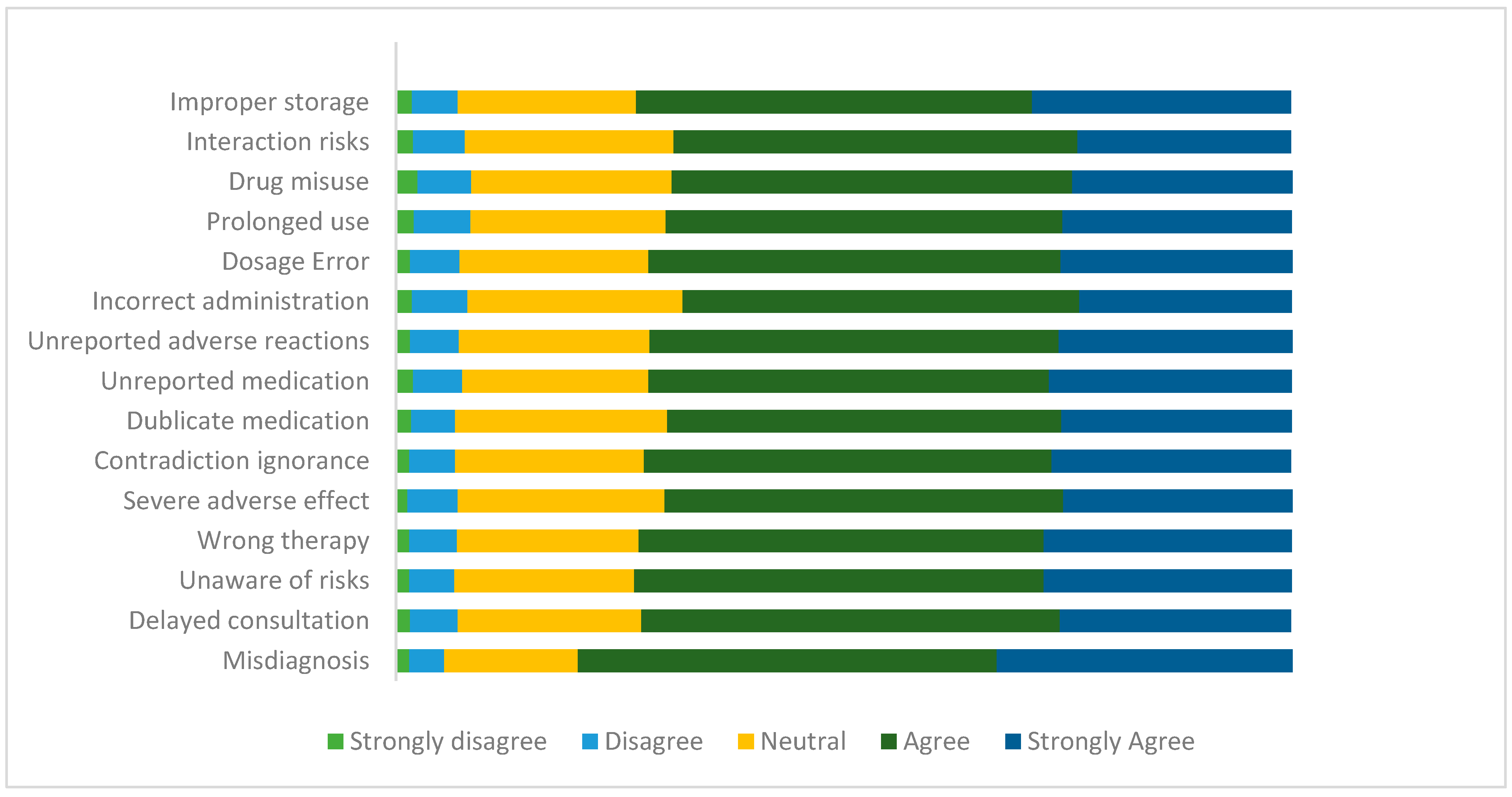
Appendix A.3. Knowledge About the Risks of SMLA
- -
- Incorrect self-diagnosis.
- -
- Failure to seek appropriate medical advice promptly.
- -
- Incorrect choice of therapy.
- -
- Failure to recognize special pharmacological risks.
- -
- Rare but severe adverse effects.
- -
- Failure to recognize or self-diagnosis contraindications, interactions, warnings, and precautions.
- -
- Failure to recognize that the same active substance is already being taken under a different name.
- -
- Failure to report current self-medication to the prescribing physician (double medication/harmful interaction).
- -
- Failure to recognize or report adverse drug reactions.
- -
- Incorrect route of administration.
- -
- Inadequate or excessive dosage.
- -
- Excessively prolonged use.
- -
- Risk of dependence and abuse.
- -
- Food and drug interaction.
- -
- Storage in incorrect conditions or beyond the recommended shelf life.
| Total Variance Explained | ||||||
|---|---|---|---|---|---|---|
| Component | Initial Eigenvalues | Extraction Sums of Squared Loadings | ||||
| Total | % of Variance | Cumulative % | Total | % of Variance | Cumulative % | |
| 1 | 8.630 | 57.531 | 57.531 | 8.630 | 57.531 | 57.531 |
| 2 | 0.954 | 6.361 | 63.892 | |||
| 3 | 0.614 | 4.095 | 67.986 | |||
| 4 | 0.580 | 3.867 | 71.854 | |||
| 5 | 0.534 | 3.561 | 75.415 | |||
| 6 | 0.490 | 3.266 | 78.681 | |||
| 7 | 0.428 | 2.855 | 81.536 | |||
| 8 | 0.417 | 2.778 | 84.314 | |||
| 9 | 0.398 | 2.650 | 86.965 | |||
| 10 | 0.379 | 2.528 | 89.493 | |||
| 11 | 0.359 | 2.394 | 91.887 | |||
| 12 | 0.336 | 2.240 | 94.127 | |||
| 13 | 0.316 | 2.109 | 96.235 | |||
| 14 | 0.294 | 1.963 | 98.198 | |||
| 15 | 0.270 | 1.802 | 100.000 | |||
| Component Matrix | |
|---|---|
| Component | |
| 1 | |
| Misdiagnosis | 0.643 |
| Delayed consultation | 0.733 |
| Unaware of risks | 0.783 |
| Wrong therapy | 0.773 |
| Severe adverse effect | 0.728 |
| Contradiction ignorance | 0.778 |
| Duplicate medication | 0.769 |
| Unreported medication | 0.770 |
| Unreported adverse effect | 0.793 |
| Incorrect administration | 0.763 |
| Dosage error | 0.813 |
| Prolonged use | 0.777 |
| Drug misuse | 0.764 |
| Interaction risks | 0.724 |
| Improper storage | 0.753 |
References
- Ehsan, H. Antibiotic Resistance in Developing Countries: Emerging Threats and Policy Responses. Public Health Chall. 2025, 4, e70034. [Google Scholar] [CrossRef]
- GBD 2021. Antimicrobial Resistance Collaborators Global burden of bacterial antimicrobial resistance 1990–2021: A systematic analysis with forecasts to 2050. Lancet 2024, 404, 1199–1226. [Google Scholar] [CrossRef] [PubMed]
- Alhomoud, F.; Aljamea, Z.; Almahasnah, R.; Alkhalifah, K.; Basalelah, L.; Alhomoud, F.K. Self-medication and self-prescription with antibiotics in the Middle East—Do they really happen? A systematic review of the prevalence, possible reasons, and outcomes. Int. J. Infect. Dis. 2017, 57, 3–12. [Google Scholar] [CrossRef]
- Saadeh, W.; Chaccour, S.; Rahme, D.; Lahoud, N.; Saleh, N. The hidden dangers lurking at home: Unveiling the prevalence of leftover antibiotics and its associated factors among Lebanese households. Public Health Pract. 2024, 7, 100485. [Google Scholar] [CrossRef] [PubMed]
- Ocan, M.; Obuku, E.A.; Bwanga, F.; Akena, D.; Richard, S.; Ogwal-Okeng, J. Household antimicrobial self-medication: A systematic review and meta-analysis of the burden, risk factors and outcomes in developing countries. BMC Public Health 2015, 15, 742. [Google Scholar] [CrossRef]
- Shah, J.; Trautner, B.W.; Olmeda, K.; Laytner, L.A.; Faustinella, F.; Paasche-Orlow, M.K.; Grigoryan, L. A survey of patient practices regarding leftover antibiotics reveals a potential source of antibiotic overuse. Antimicrob. Agents Chemother. 2024, 68, e0046924. [Google Scholar] [CrossRef]
- Machongo, R.B.; Mipando, A.L.N. I don’t hesitate to use the left-over antibiotics for my child” practices and experiences with antibiotic use among caregivers of paediatric patients at Zomba central hospital in Malawi. BMC Pediatr. 2022, 22, 466. [Google Scholar] [CrossRef]
- Iskandar, K.; Molinier, L.; Hallit, S.; Sartelli, M.; Catena, F.; Coccolini, F.; Craig Hardcastle, T.; Roques, C.; Salameh, P. Drivers of antibiotic resistance transmission in low-and middle-income countries from a “one health” perspective—A review. Antibiotics 2020, 9, 372. [Google Scholar] [CrossRef]
- Mendoza, A.M.B.; Maliñana, S.A.A.; Maravillas, S.I.D.; Moniva, K.C.; Jazul, J.P. Relationship of self-medication and antimicrobial resistance (AMR) in low- and middle-income countries (LMICs): A scoping review. J. Public Health Emerg. 2025, 9, 6. [Google Scholar] [CrossRef]
- Bashaar, M.; Thawani, V.; Hassali, M.A.; Saleem, F. Disposal practices of unused and expired pharmaceuticals among general public in Kabul. BMC Public Health 2017, 17, 45. [Google Scholar]
- Khan, N.A.; Easwaran, V.; Orayj, K.; Venkatesan, K.; Alavudeen, S.S.; Alhadeer, S.A.; Al Nazih, A.A.; Al Afraa, I.H.S.; Hussein, A.T.; Alshahrani, S.M.; et al. A cross-sectional study on perceptions towards safe disposal of unused/expired medicines and its associated factors among the public in Saudi Arabia—A threat to the environment and health. PeerJ 2025, 13, 19258. [Google Scholar] [CrossRef]
- Ugoeze, K.; Alalor, C.; Ibezim, C.; Chinko, B.; Owonaro, P.; Anie, C.; Okoronkwo, N.; Mgbahurike, A.; Ofomata, C.; Alfred-Ugbenbo, D.; et al. Environmental and human health impact of antibiotics waste mismanagement: A review. Adv. Environ. Eng. Res. 2024, 5, 1–21. [Google Scholar] [CrossRef]
- Chen, L.; Zhao, X.; Li, R.; Yang, H. Integrated metabolomics and transcriptomics reveal the adaptive responses of Salmonella enterica serovar Typhimurium to thyme and cinnamon oils. Food Res. Int. 2022, 157, 111241. [Google Scholar] [CrossRef] [PubMed]
- Lundborg, C.S.; Tamhankar, A.J. Antibiotic residues in the environment of South East Asia. BMJ 2017, 358, j2440. [Google Scholar] [CrossRef]
- Naing, S.; Wijk, M.; Vila, J.; Ballesté-Delpierre, C. Understanding antimicrobial resistance from the perspective of public policy: A multinational knowledge, attitude, and perception survey to determine global awareness. Antibiotics 2021, 10, 1486. [Google Scholar] [CrossRef]
- Alyafei, A.; Easton-Carr, R. The health belief model of behavior change. In StatPearls; StatPearls Publishing: Saint Petersburg, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK606120/ (accessed on 1 May 2025).
- Tangcharoensathien, V.; Chanvatik, S.; Kosiyaporn, H.; Kirivan, S.; Kaewkhankhaeng, W.; Thunyahan, A.; Lekagul, A. Population knowledge and awareness of antibiotic use and antimicrobial resistance: Results from national household survey 2019 and changes from 2017. BMC Public Health 2021, 21, 2188. [Google Scholar] [CrossRef]
- World Health Organization. Antibiotic resistance: Multi-country public awareness survey. In Antibiotic Resistance: Multi-Country Public Awareness Survey; World Health Organization: Geneva, Switzerland, 2015; Available online: https://iris.who.int/bitstream/handle/10665/194460/9789241509817_eng.pdf?sequence=1&isAllowed=y (accessed on 1 May 2025).
- Al-Mehmadi, B.; Alsubaie, S.; Al-Morikhi, O.; Alqahtani, F.; Almutairi, W.; Al-Mutairi, M.; Alotaibi, M.; Alenazi, S.; Alanazi, K. Knowledge and Attitude of self-medication with leftover antibiotics in Saudi Arabia: A cross-sectional study. F1000Research 2024, 12, 304. [Google Scholar] [CrossRef] [PubMed]
- Mallah, N.; Orsini, N.; Figueiras, A.; Takkouche, B. Education level and misuse of antibiotics in the general population: A systematic review and dose–response meta-analysis. Antimicrob. Resist. Infect. Control. 2022, 11, 24. [Google Scholar] [CrossRef] [PubMed]
- Naser, A.Y.; Aboutaleb, R.M.; Khaleel, A.; Alsairafi, Z.K.; Alwafi, H.; Qadus, S.; Itani, R.; El-Dahiyat, F.; Awaisu, A.; Awwad, O.; et al. Knowledge, attitude, and practices of pharmacy students in 7 Middle Eastern countries concerning antibiotic resistance: A cross-sectional study. Medicine 2024, 103, e39378. [Google Scholar] [CrossRef]
- Naser, A.Y.; Amara, N.; Daghash, A.; Naddaf, A. Medications disposal and medications storage in Jordan: A cross-sectional study. Int. J. Clin. Pract. 2021, 75, e13822. [Google Scholar] [CrossRef]
- Naser, A.Y. Cost-related nonadherence for prescription medications: A cross-sectional study in Jordan. Expert Rev. Pharmacoecon. Outcomes Res. 2022, 22, 497–503. [Google Scholar] [CrossRef]
- Eze, J. THE GLOBAL THREAT OF ANTIMICROBIAL RESISTANCE: A Silent Pandemic In Motion By Jude Eze. Available online: https://theconcourse.com.ng/the-global-threat-of-antimicrobial-resistance-a-silent-pandemic-in-motion-by-jude-eze/ (accessed on 1 May 2025).
- Rosenstock, I.M.; Strecher, V.J.; Becker, M.H. Social learning theory and the health belief model. Health Educ. Q. 1988, 15, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Champion, V.L.; Skinner, C.S. The health belief model. Health Behav. Health Educ. Theory Res. Pract. 2008, 4, 45–65. [Google Scholar]
- Ajekiigbe, V.O.; Agbo, C.E.; Ogieuhi, I.J.; Anthony, C.S.; Onuigbo, C.S.; Falayi, T.A.; Oluwapelumi, O.Z.; Amusa, O.; Adeniran, G.O.; Ogunleke, P.O.; et al. The increasing burden of global environmental threats: Role of antibiotic pollution from pharmaceutical wastes in the rise of antibiotic resistance. Discov. Public Health 2025, 22, 120. [Google Scholar] [CrossRef]
- Hamilton, R.A.; Ercolani, M.G.; Aggarwal, R.; Cooper, D.; Kelly, S.; Root, H.; Pabari, K.; Jamieson, C. Evaluation of antibiotics returned for safe disposal during and after a community pharmacy antibiotic amnesty campaign. JAC-Antimicrob. Resist. 2024, 6, dlae172. [Google Scholar] [CrossRef]
- Guo, H.; Hildon, Z.J.-L.; Lye, D.C.B.; Straughan, P.T.; Chow, A. The associations between poor antibiotic and antimicrobial resistance knowledge and inappropriate antibiotic use in the general population are modified by age. Antibiotics 2021, 11, 47. [Google Scholar] [CrossRef] [PubMed]
- Commission, E. Pharmaceutical Strategy for Europe 2023. Available online: https://health.ec.europa.eu/medicinal-products/pharmaceutical-strategy-europe_en (accessed on 1 May 2025).
- COM(2019) 128 Final; Strategic Approach to Pharmaceuticals in the Environment. Communication from the Commission to the European Parliament, the Council and the European Economic and Social Committee, European Union Strategic Approach to Pharmaceuticals in the Environment, Brussels; European Union: Luxembourg, 2019.
- Rogowska, J.; Zimmermann, A. Household pharmaceutical waste disposal as a global problem—A review. Int. J. Environ. Res. Public Health 2022, 19, 15798. [Google Scholar] [CrossRef]
- Muflih, S.M.; Al-Azzam, S.; Karasneh, R.A.; Bleidt, B.A.; Conway, B.R.; Bond, S.E.; Aldeyab, M.A. Public knowledge of antibiotics, self-medication, and household disposal practices in Jordan. Expert Rev. Anti. Infect. Ther. 2023, 21, 477–487. [Google Scholar] [CrossRef]
- Ajzen, I.; Driver, B.L. Prediction of leisure participation from behavioral, normative, and control beliefs: An application of the theory of planned behavior. Leis. Sci. 1991, 13, 185–204. [Google Scholar] [CrossRef]
- Bhakuni, H.; Abimbola, S. Epistemic injustice in academic global health. Lancet Glob. Health 2021, 9, e1465–e1470. [Google Scholar] [CrossRef] [PubMed]
- Osborne, R.H.; Cheng, C.C.; Nolte, S.; Elmer, S.; Besancon, S.; Budhathoki, S.S.; Debussche, X.; Dias, S.; Kolarčik, P.; Loureiro, M.I.; et al. Health literacy measurement: Embracing diversity in a strengths-based approach to promote health and equity, and avoid epistemic injustice. BMJ Global Health 2022, 7, e009623. [Google Scholar] [CrossRef]
- Fricker, M. Epistemic Injustice: Power and the Ethics of Knowing; Oxford University Press: Oxford, UK, 2007. [Google Scholar] [CrossRef]
- Broom, A.; Peterie, M.; Kenny, K.; Broom, J.; Kelly-Hanku, A.; Lafferty, L.; Treloar, C.; Applegate, T. Vulnerability and antimicrobial resistance. Crit. Public Health 2023, 33, 308–317. [Google Scholar] [CrossRef]
- Littlejohn, S.W.; Foss, K.A. Gender role theory. Encycl. Commun. Theory 2009, 1, 434–436. [Google Scholar]
- Rieker, P.P.; Bird, C.E.; Lang, M.E. Understanding gender and health. In Handbook of Medical Sociology, 6th ed.; Old Patters, New Trends, and Future Directions; Vanderbilt University Press: Nashville, TN, USA, 2010; pp. 52–74. [Google Scholar]
- Rieker, P.P.; Read, J.G. The health gender gap: A constrained choice explanation. In The Psychology of Gender and Health; Academic Press: Cambridge, MA, USA, 2017; pp. 85–118. [Google Scholar]
- Horne, R.; Chapman, S.C.; Parham, R.; Freemantle, N.; Forbes, A.; Cooper, V. Understanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: A meta-analytic review of the Necessity-Concerns Framework. PLoS ONE 2013, 8, 80633. [Google Scholar] [CrossRef]
- Ross, A.; Meacham, P.J.; Waswa, J.P.; Joshi, M.P.; Hafner, T.; Godby, S.; Johnson, C.; Londhe, S.; Aibo, D.; Kwikiriza, G.; et al. Behavioral Nudges to Encourage Appropriate Antimicrobial Use Among Health Professionals in Uganda. Antibiotics 2024, 13, 1016. [Google Scholar] [CrossRef]
- Ruiz-Ramos, J.; Escolà-Vergé, L.; Monje-López, Á.E.; Herrera-Mateo, S.; Rivera, A. The interventions and challenges of antimicrobial stewardship in the emergency department. Antibiotics 2023, 12, 1522. [Google Scholar] [CrossRef]
- Melki, I.S. Household crowding index: A correlate of socioeconomic status and inter-pregnancy spacing in an urban setting. J. Epidemiol. Community Health 2004, 58, 476–480. [Google Scholar] [CrossRef]
- Kosiyaporn, H.; Chanvatik, S.; Issaramalai, T.; Kaewkhankhaeng, W.; Kulthanmanusorn, A.; Saengruang, N.; Tangcharoensathien, V. Surveys of knowledge and awareness of antibiotic use and antimicrobial resistance in general population: A systematic review. PLoS ONE 2020, 15, 0227973. [Google Scholar] [CrossRef] [PubMed]
- Wong, L.P.; Alias, H.; Husin, S.A.; Ali, Z.B.; Sim, B.; Ponnampalavanar, S.S.L.S. Factors influencing inappropriate use of antibiotics: Findings from a nationwide survey of the general public in Malaysia. PLoS ONE 2021, 16, 0258698. [Google Scholar] [CrossRef] [PubMed]
- Bhat, M.J.; Al-qahtani, M.; Badawi, A.S.; Asiri, G.B.; Alhmare, A.M.; Rashid, A.; Altalhiyyah, K.S.; Alwimny, A.A. Awareness and Knowledge of Antibiotic Resistance and Risks of Self-Medication with Antibiotics Among the Aseer Region Population, Saudi Arabia, 2023. Cureus 2023, 15, e40762. [Google Scholar] [CrossRef] [PubMed]
- Bianco, A.; Licata, F.; Zucco, R.; Papadopoli, R.; Pavia, M. Knowledge and practices regarding antibiotics use. Evol. Med. Public Health 2020, 2020, 129–138. [Google Scholar] [CrossRef] [PubMed]
- Ansari, M.; Alanazi, A.; Moin, A. Consumers’ awareness, attitude and associated factors towards self-medication in Hail, Saudi Arabia. PLoS ONE 2020, 15, e0232322. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guidelines for the Regulatory Assessment of Medicinal Products for Use in Self-Medication. Available online: https://iris.who.int/items/468d79f6-9788-4296-9bc9-68014166373d (accessed on 1 May 2025).
- Santos, D.F.; Silveira, M.P.; Camargo, A.L.; Matijasevich, A.; Santos, I.S.; Barros, A.J.; Bertoldi, A.D. Unsafe storage of household medicines: Results from a cross-sectional study of four-year-olds from the 2004 Pelotas birth cohort. Brazil. BMC Pediatr. 2019, 19, 235. [Google Scholar] [CrossRef] [PubMed]
- Michael, I.; Ogbonna, B.; Sunday, N.; Anetoh, M.; Matthew, O. Assessment of disposal practices of expired and unused medications among community pharmacies in Anambra State southeast Nigeria: A mixed study design. J. Pharm. Policy Pract. 2019, 28, 2656–2662. [Google Scholar] [CrossRef]
- Sitotaw, B.; Philipos, W. Knowledge, Attitude, Practices on Antibiotic Use and Disposal Ways in Sidama Region, Ethiopia: A Community-Based Cross-Sectional Survey. Sci. World J. 2023, 2023, 8774634. [Google Scholar] [CrossRef]
- World Health Organization. WHODAS 2.0 Translation Package (Version 1.0). Translation and Linguistic Evaluation Protocol and Supporting Material; World Health Organization: Geneva, Switzerland, 2023. [Google Scholar]
- Goodyear, M.D.; Krleza-Jeric, K.; Lemmens, T. The declaration of Helsinki. BMJ 2007, 335, 624–625. [Google Scholar] [CrossRef]
| Characteristic | n | % | |
|---|---|---|---|
| Country | |||
| Egypt | 1505 | 47.2 | |
| Lebanon | 488 | 15.3 | |
| Jordan | 421 | 13.2 | |
| Serbia | 240 | 7.5 | |
| Bangladesh | 236 | 7.4 | |
| Brazil | 182 | 5.7 | |
| Gender | |||
| Female | 1963 | 61.5 | |
| Male | 1228 | 38.5 | |
| Marital Status | |||
| Single | 2027 | 63.5 | |
| Married | 1083 | 33.9 | |
| Divorced | 58 | 1.8 | |
| Widow | 23 | 0.7 | |
| Education | |||
| Uneducated | 16 | 0.5 | |
| Primary School | 47 | 1.5 | |
| Middle School | 91 | 2.9 | |
| High School | 416 | 13 | |
| University | 2621 | 82.1 | |
| Healthcare provider | |||
| No | 2177 | 68.2 | |
| Yes | 1014 | 31.8 | |
| HHCI 1 | |||
| <1 (no crowding) | 1190 | 37.3 | |
| ≥1 (crowding) | 2001 | 62.7 | |
| Mean ± S.D. 2 | Minimum | Maximum | |
| Age (years) | 29.3 ± 10.6 | 18 | 98 |
| Knowledge Scales | Mean ± S.D. | Minimum | Maximum |
|---|---|---|---|
| Knowledge of AB and AB use 1 | 54.4 ± 8.4 | 17 | 75 |
| Knowledge about AB resistance 2 | 43.3 ± 6.1 | 20 | 60 |
| Knowledge about risks associated with SMLA 3 | 58.4 ± 10.3 | 15 | 75 |
| Knowledge About Clinical Risks Associated with SMLA | ||||
|---|---|---|---|---|
| Variable | Mean ± S.D. | 95% IC | Test | p-Value |
| Country | 43.5 | <0.001 | ||
| Egypt (n = 1505) | 59.3 ± 10.2 | 58.8–59.8 | ||
| Lebanon (n = 488) | 58.6 ± 10.0 | 57.8–59.6 | ||
| Jordan (n = 421) | 54.6 ± 9.0 | 53.8–55.5 | ||
| Serbia (n = 240) | 64.3 ± 10.6 | 63.0–65.7 | ||
| Bangladesh (n = 236) | 52.0 ± 8.5 | 50.9–53.1 | ||
| Brazil (n = 182) | 59.9 ± 9.3 | 58.5–61.2 | ||
| India (n = 119) | 58.1 ± 11.2 | 56.0–60.1 | ||
| Gender | 8.38 | <0.001 | ||
| Female (n = 1963) | 59.6 ± 10.4 | 59.2–60.1 | ||
| Male (n = 1229) | 56.5 ± 9.8 | 55.9–57.1 | ||
| Marital status | 5.77 | <0.001 | ||
| Single (n = 2027) | 59.2 ± 10.2 | 58.7–59.6 | ||
| Ever married (n = 1164) | 57.1 ± 10.5 | 56.5–57.7 | ||
| Education level | 27.23 | <0.001 | ||
| Low or no education (n = 63) | 52.8 ± 9.7 | 50.4–55.3 | ||
| Moderate education (n = 507) | 56.1 ± 10.5 | 55.1–57.0 | ||
| Higher education (n = 2621) | 59.0 ± 10.2 | 58.6–59.4 | ||
| Crowding index | −0.25 | 0.802 | ||
| No crowding (n = 1190) | 58.4 ± 10.5 | 57.8–59.0 | ||
| Crowding (n = 2001) | 58.5 ± 10.2 | 58.0–58.9 | ||
| Healthcare provider | −8.79 | <0.001 | ||
| No (n = 2177) | 57.3 ± 10.2 | 56.9–57.8 | ||
| Yes (n = 1014) | 60.7 ± 10.2 | 60.1–61.4 | ||
| Pearson’s correlation coefficient | p-value | |||
| Age | −0.09 | <0.001 | ||
| Knowledge of AB and AB use | 0.47 | <0.001 | ||
| Knowledge of AB resistance | 0.46 | <0.001 | ||
| LA Administration Risks | ||||
|---|---|---|---|---|
| Unstandardized B | Standardized Beta | 95% CI | p-Value | |
| Country Egypt (reference) | ||||
| Lebanon | 0.06 | 0 | −0.84, 0.95 | 0.904 |
| Jordan | −2.16 | −0.07 | −3.12, −1.24 | <0.001 |
| Serbia | 1.72 | 0.04 | 0.47, 2.97 | 0.007 |
| Bangladesh | −3.64 | −0.09 | −4.92, −2.37 | <0.001 |
| Brazil | 0.42 | 0.01 | −0.96; 1.80 | 0.553 |
| Gender Female (reference) | ||||
| Male | −1.13 | −0.05 | −1.77, −0.48 | <0.001 |
| Marital status Single (reference) | ||||
| Ever married | −0.44 | −0.02 | −1.30, 0.43 | 0.323 |
| Education level High (reference) | ||||
| Low education | −0.46 | −0.01 | −2.73, 1.80 | 0.689 |
| Moderate education | −1.1 | −0.04 | −2.00, −0.20 | 0.016 |
| Healthcare provider No (reference) | ||||
| Yes | −0.33 | −0.02 | −1.04, 0.39 | 0.372 |
| Age | −0.02 | −0.02 | −0.06, 0.02 | 0.381 |
| Knowledge of AB and their use | 0.34 | 0.28 | 0.30, 0.39 | <0.001 |
| Knowledge of AB resistance | 0.45 | 0.27 | 0.39, 0.51 | <0.001 |
| Storage | Disposal | |||||
|---|---|---|---|---|---|---|
| Correct n = 1758 | Incorrect n = 1433 | Correct n = 699 | Incorrect n = 2492 | |||
| n (%) | n (%) | p-Value | n (%) | n (%) | p-Value | |
| Country | <0.001 | <0.001 | ||||
| Egypt | 878 (58.3) | 627 (41.7) | 302 (20.1) | 1203 (79.9) | ||
| Lebanon | 285 (58.4) | 203 (41.6) | 84 (17.2) | 404 (82.8) | ||
| Jordan | 226 (53.7) | 195 (46.3) | 30 (7.1) | 391 (92.9) | ||
| Serbia | 127 (52.9) | 113 (47.1) | 146 (60.8) | 94 (39.2) | ||
| Bangladesh | 85 (36.0) | 151 (64.0) | 63 (26.7) | 173 (73.3) | ||
| Brazil | 88 (48.4) | 94 (51.6) | 50 (27.5) | 132 (72.5) | ||
| India | 69 (58.0) | 50 (42.0) | 24 (20.2) | 95 (79.8) | ||
| Gender | 0.031 | 0.218 | ||||
| Female | 1111 (56.6) | 852 (43.4) | 416 (21.2) | 1547 (78.8) | ||
| Male | 647 (52.7) | 581 (47.3) | 283 (23.0) | 945 (77.0) | ||
| Marital status | 0.541 | 0.595 | ||||
| Single | 1125 (55.5) | 902 (44.5) | 450 (22.2) | 1577 (77.8) | ||
| Ever married | 633 (54.4) | 531 (45.6) | 249 (21.4) | 915 (78.6) | ||
| Education level | 0.011 | 0.721 | ||||
| Low/none | 23 (36.5) | 40 (63.5) | 15 (23.8) | 48 (76.2) | ||
| Moderate | 278 (54.8) | 229 (45.2) | 117 (23.1) | 390 (76.9) | ||
| High | 1457 (55.6) | 1164 (44.4) | 567 (21.6) | 2054 (78.4) | ||
| Crowding index | 0.74 | <0.001 | ||||
| No crowding | 563 (55.5) | 451 (44.5) | 310 (26.1) | 880 (73.9) | ||
| Crowding | 1195 (54.9) | 982 (45.1) | 389 (19.4) | 1612 (80.6) | ||
| Healthcare provider | 0.39 | <0.001 | ||||
| Yes | 644 (54.1) | 546 (45.9) | 291 (28.7) | 723 (71.3) | ||
| No | 1114 (55.7) | 887 (44.3) | 408 (18.7) | 1769 (81.3) | ||
| Mean ± SD | Mean ± SD | p-value | Mean ± SD | Mean ± SD | p-value | |
| Age | 29.5 ± 11.02 | 29.1 ± 10.2 | 0.277 | 29.2 ± 13.7 | 29.7 ± 11.6 | 0.278 |
| Knowledge about AB and AB use | 53.5 ± 8.4 | 55.4 ± 8.4 | <0.001 | 56.4 ± 8.9 | 53.8 ± 8.2 | <0.001 |
| Knowledge about AB resistance | 43.3 ± 6.1 | 43.4 ± 6.1 | 0.490 | 45.2 ± 6.3 | 42.8 ± 5.9 | <0.001 |
| Correct Practice Regarding Antibiotic Storage | Correct Practice Regarding Antibiotic Disposal | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI 1 | p-Value | |
| Country Egypt (reference) | ||||||
| Lebanon | 1.12 | 0.76–1.64 | 0.56 | 1.16 | 0.72–1.86 | 0.55 |
| Jordan | 1.11 | 0.73–1.67 | 0.62 | 1.39 | 0.83–2.33 | 0.21 |
| Serbia | 0.87 | 0.57–1.32 | 0.5 | 3.19 | 1.77–5.75 | <0.001 |
| Bangladesh | 1.03 | 0.65–1.63 | 0.9 | 0.18 | 0.11–0.31 | <0.001 |
| Brazil | 0.46 | 0.29–0.74 | 0.001 | 0.63 | 0.37–1.09 | 0.1 |
| India | 0.79 | 0.49–1.27 | 0.33 | 0.78 | 0.44–1.37 | 0.39 |
| Gender Female (reference) | ||||||
| Male | 1.16 | 1.00–1.35 | 0.05 | |||
| Educational level Low or none (reference) | ||||||
| Moderate education | 0.59 | 0.34–1.01 | 0.04 | |||
| Higher education | 1.03 | 0.84–1.27 | 0.99 | |||
| Crowding index No (reference) | 0.87 | 0.72–1.06 | 0.16 | |||
| Yes | ||||||
| Healthcare provider No (reference) | 1.85 | 1.52–2.26 | <0.001 | |||
| Yes | ||||||
| Knowledge of AB and AB use | 0.96 | 0.95–0.97 | <0.001 | 1.00 | 0.99–1.01 | 0.84 |
| Knowledge of AB resistance | 1.02 | 1.00–1.03 | 0.025 | 0.97 | 0.95–0.98 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iskandar, K.; Kotb, R.; Cherfane, M.; Yeretzian, J.; Bou Dib, J.; Chahine, B.; Hallit, S.; Amin, R.; Bahlol, M.; Fekih-Romdhane, F.; et al. Household Knowledge of Clinical Risks, Storage, and Disposal of Leftover Antibiotics: A Multinational Study in Seven Developing Countries. Antibiotics 2025, 14, 1212. https://doi.org/10.3390/antibiotics14121212
Iskandar K, Kotb R, Cherfane M, Yeretzian J, Bou Dib J, Chahine B, Hallit S, Amin R, Bahlol M, Fekih-Romdhane F, et al. Household Knowledge of Clinical Risks, Storage, and Disposal of Leftover Antibiotics: A Multinational Study in Seven Developing Countries. Antibiotics. 2025; 14(12):1212. https://doi.org/10.3390/antibiotics14121212
Chicago/Turabian StyleIskandar, Katia, Reham Kotb, Michelle Cherfane, Joumana Yeretzian, Julia Bou Dib, Bahia Chahine, Souheil Hallit, Rohul Amin, Mohamed Bahlol, Feten Fekih-Romdhane, and et al. 2025. "Household Knowledge of Clinical Risks, Storage, and Disposal of Leftover Antibiotics: A Multinational Study in Seven Developing Countries" Antibiotics 14, no. 12: 1212. https://doi.org/10.3390/antibiotics14121212
APA StyleIskandar, K., Kotb, R., Cherfane, M., Yeretzian, J., Bou Dib, J., Chahine, B., Hallit, S., Amin, R., Bahlol, M., Fekih-Romdhane, F., Hamed, F., Helmy, M., Irfan, M., Murugaiyan, J., Naser, A. Y., Taybeh, E. O., Pavlović, N., Rahme, D., Akl, M., ... Van Dongen, M. (2025). Household Knowledge of Clinical Risks, Storage, and Disposal of Leftover Antibiotics: A Multinational Study in Seven Developing Countries. Antibiotics, 14(12), 1212. https://doi.org/10.3390/antibiotics14121212














