Outpatient Parenteral Antimicrobial Therapy in a Tertiary Hospital in France: A Description of Service Models and Costs
Abstract
1. Introduction
2. Results
2.1. Participant Characteristics
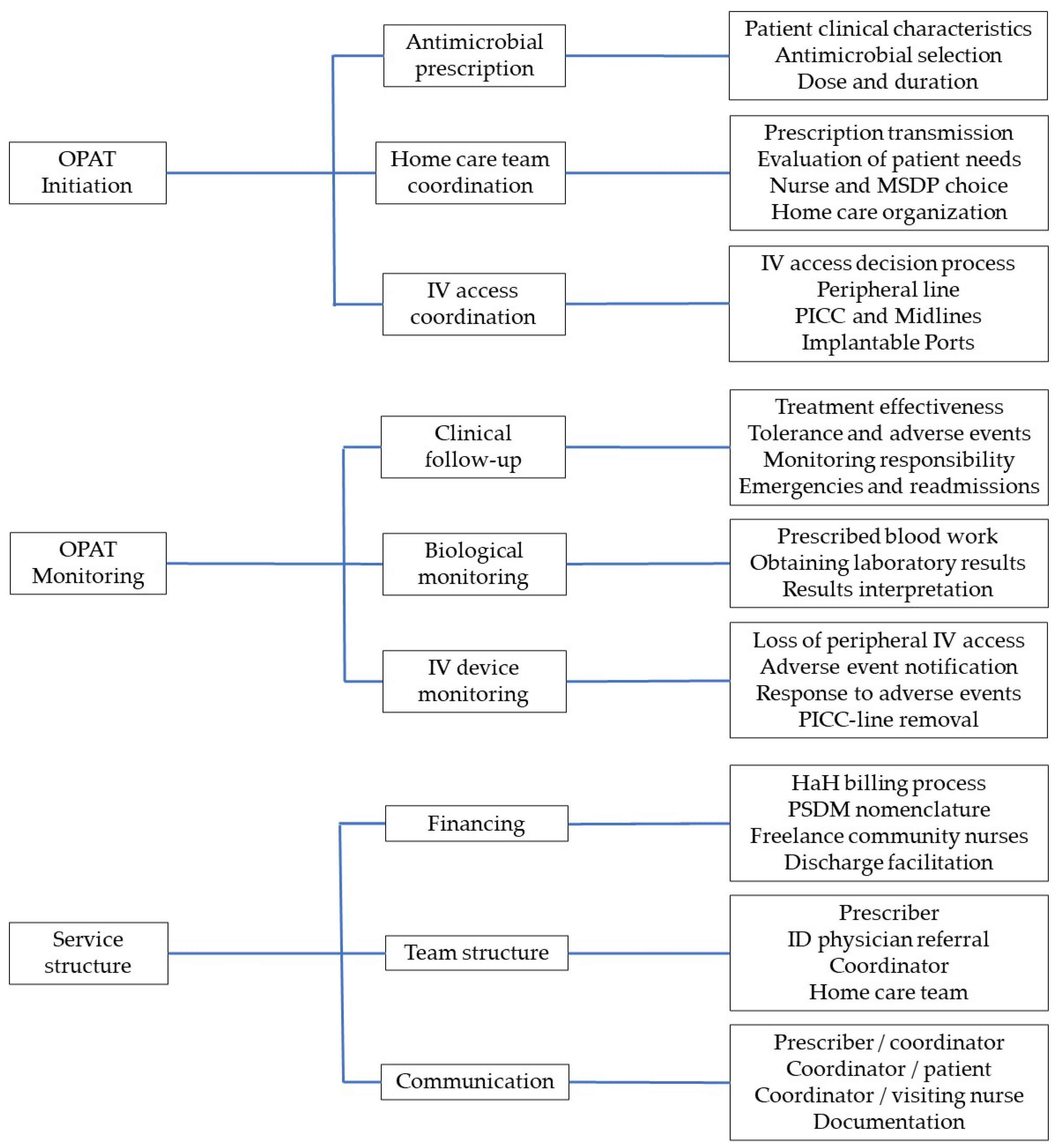
2.2. Overall OPAT Service Model Characteristics
2.3. Model Characteristics
2.3.1. Model A: ID Physician Referral and OPAT Coordination by MSDP
2.3.2. Model B: Acute Care Unit Prescriber and OPAT Coordination by MSDP
2.3.3. Model C: Nurse-Led OPAT Coordination
2.3.4. Model D: Discharge Facilitation Nurse and OPAT Coordination by MSDP
2.3.5. Model E: Hospital at Home
3. Discussion
4. Materials and Methods
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| OPAT | Outpatient Parenteral Antimicrobial Therapy |
| ID | Infectious Diseases |
| ED | Emergency Department |
| AE | Adverse Event |
| MSDP | Medical Service and Device Provider |
| HaH | Hospital at Home |
| PICC | Peripherally Inserter Central Catheter |
Appendix A
| D0 | D1 | D2 | D3 | D4 | D5 | D6 | D7 | |
|---|---|---|---|---|---|---|---|---|
| Patient evaluation and care planning | 1 | |||||||
| Infusion preparation, initiation, and 12 h monitoring | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| PICC line dressing change | 1 | |||||||
| Blood draw | 1 | |||||||
| Flat rate travel allowance | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Weekend surcharge | 1 |
| Billable Services | Unit Costs (EUR) | Units Per Week (n) | Total Weekly Costs (EUR) |
|---|---|---|---|
| Medical service and device provider | |||
| Home infusion one-time coordination fee | 229.0 | 1 | 229.0 |
| Weekly monitoring | 45.8 | 1 | 45.8 |
| Weekly equipment and supplies | 409.5 | 1 | 409.5 |
| Pharmacy, mean (min-max) | |||
| Piperacillin-tazobactam, 4 g | 9.75 | 21 | 204.75 |
| Normal saline, 240 mL daily | 3.03 | 7 | 21.21 |
| Visiting nurse | |||
| Patient evaluation and care planning | 12.6 | 1 | 12.6 |
| Infusion preparation and initiation | 44.1 | 7 | 308.7 |
| PICC line dressing change | 14.8 | 1 | 14.8 |
| Blood draw | 4.7 | 1 | 4.7 |
| Flat rate travel allowance | 2.8 | 7 | 19.6 |
| Weekend surcharge | 8.2 | 1 | 8.2 |
| Local laboratory blood test processing | |||
| Complete blood count | 5.2 | 1 | 5.2 |
| Serum electrolytes | 2.6 | 1 | 2.6 |
| Serum creatinine | 1.6 | 1 | 1.6 |
| Complete liver panel | 6.5 | 1 | 6.5 |
| C-reactive protein | 2.1 | 1 | 2.1 |
| Hospital-based outpatient nursing care | |||
| OPAT coordination | 12.6 | 1 | 12.6 |
| PICC line removal | 13.2 | 1 | 13.2 |
| Patient transportation for PICC line removal | 67.0 * | 2 | 134.0 |
| HaH, DRG daily rate during first week | 329.7 † | 7 | 2307.9 |
| Hospital-based discharge facilitation | 150.0 ‡ | 1 | 150.0 |
References
- Mohammed, S.A.; Roberts, J.A.; Cotta, M.O.; Rogers, B.; Pollard, J.; Assefa, G.M.; Erku, D.; Sime, F.B. Safety and Efficacy of Outpatient Parenteral Antimicrobial Therapy: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Int. J. Antimicrob. Agents 2024, 64, 107263. [Google Scholar] [CrossRef] [PubMed]
- Wolie, Z.T.; Roberts, J.A.; Gilchrist, M.; McCarthy, K.; Sime, F.B. Current Practices and Challenges of Outpatient Parenteral Antimicrobial Therapy: A Narrative Review. J. Antimicrob. Chemother. 2024, 79, 2083–2102. [Google Scholar] [CrossRef]
- Mohammed, S.A.; Cotta, M.O.; Assefa, G.M.; Erku, D.; Sime, F. Barriers and Facilitators for the Implementation and Expansion of Outpatient Parenteral Antimicrobial Therapy: A Systematic Review. J. Hosp. Infect. 2024, 147, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Browning, S.; Loewenthal, M.R.; Freelander, I.; Dobson, P.M.; Schneider, K.; Davis, J.S. Safety of Prolonged Outpatient Courses of Intravenous Antibiotics: A Prospective Cohort Study. Clin. Microbiol. Infect. 2022, 28, 832–837. [Google Scholar] [CrossRef]
- Allison, G.M.; Muldoon, E.G.; Kent, D.M.; Paulus, J.K.; Ruthazer, R.; Ren, A.; Snydman, D.R. Prediction Model for 30-Day Hospital Readmissions Among Patients Discharged Receiving Outpatient Parenteral Antibiotic Therapy. Clin. Infect. Dis. 2014, 58, 812–819. [Google Scholar] [CrossRef]
- Brenneman, E.; Funaro, J.; Dicks, K.; Yarrington, M.; Lee, H.-J.; Erkanli, A.; Hung, F.; Drew, R. Utility of a Risk Assessment Model in Predicting 30 Day Unplanned Hospital Readmission in Adult Patients Receiving Outpatient Parenteral Antimicrobial Therapy. JAC Antimicrob. Resist. 2023, 5, dlad019. [Google Scholar] [CrossRef]
- Chapman, A.L.N.; Patel, S.; Horner, C.; Green, H.; Guleri, A.; Hedderwick, S.; Snape, S.; Statham, J.; Wilson, E.; Gilchrist, M.; et al. Updated Good Practice Recommendations for Outpatient Parenteral Antimicrobial Therapy (OPAT) in Adults and Children in the UK. JAC Antimicrob. Resist. 2019, 1, dlz026. [Google Scholar] [CrossRef] [PubMed]
- Norris, A.H.; Shrestha, N.K.; Allison, G.M.; Keller, S.C.; Bhavan, K.P.; Zurlo, J.J.; Hersh, A.L.; Gorski, L.A.; Bosso, J.A.; Rathore, M.H.; et al. 2018 Infectious Diseases Society of America Clinical Practice Guideline for the Management of Outpatient Parenteral Antimicrobial Therapy. Clin. Infect. Dis. 2019, 68, e1–e35. [Google Scholar] [CrossRef]
- Gauzit, R.; Castan, B.; Bonnet, E.; Bru, J.P.; Cohen, R.; Diamantis, S.; Faye, A.; Hitoto, H.; Issa, N.; Lebeaux, D.; et al. Anti-Infectious Treatment Duration: The SPILF and GPIP French Guidelines and Recommendations. Infect. Dis. Now. 2021, 51, 114–139. [Google Scholar] [CrossRef]
- Berrevoets, M.A.H.; Ten Oever, J.; Oerlemans, A.J.M.; Kullberg, B.J.; Hulscher, M.E.; Schouten, J.A. Quality Indicators for Appropriate Outpatient Parenteral Antimicrobial Therapy in Adults: A Systematic Review and RAND-Modified Delphi Procedure. Clin. Infect. Dis. 2020, 70, 1075–1082. [Google Scholar] [CrossRef]
- Le Maréchal, M.; Tebano, G.; Monnier, A.A.; Adriaenssens, N.; Gyssens, I.C.; Huttner, B.; Milanic, R.; Schouten, J.; Stanic Benic, M.; Versporten, A.; et al. Quality Indicators Assessing Antibiotic Use in the Outpatient Setting: A Systematic Review Followed by an International Multidisciplinary Consensus Procedure. J. Antimicrob. Chemother. 2018, 73, vi40–vi49. [Google Scholar] [CrossRef]
- Gilchrist, M.; Seaton, R.A. Outpatient Parenteral Antimicrobial Therapy and Antimicrobial Stewardship: Challenges and Checklists. J. Antimicrob. Chemother. 2015, 70, 965–970. [Google Scholar] [CrossRef] [PubMed]
- Emilie, C.; de Nocker, P.; Saïdani, N.; Gilchrist, M.; Seaton, R.A.; Patel, S.; Beraud, G.; Kofteridis, D.; Schouten, J.; Thilly, N.; et al. Survey of Delivery of Parenteral Antimicrobials in Non-Inpatient Settings across Europe. Int. J. Antimicrob. Agents 2022, 59, 106559. [Google Scholar] [CrossRef] [PubMed]
- Gilchrist, M.; Barr, D.; Drummond, F.; Muir, A.; Williams, J.; Scriven, J.; Snape, S.; Hemsley, C.; Durojaiye, C.O.; Patel, S.; et al. Outpatient Parenteral Antimicrobial Therapy (OPAT) in the UK: Findings from the BSAC National Outcomes Registry (2015-19). J. Antimicrob. Chemother. 2022, 77, 1481–1490. [Google Scholar] [CrossRef] [PubMed]
- Wolie, Z.T.; Roberts, J.A.; López-Cortés, L.E.; Mirón-Rubio, M.; Pollard, J.; Marizan Nor, A.N.; Abdul-Aziz, M.H.; Jamieson, C.; Seaton, R.A.; Gilchrist, M.; et al. Current Practices in Outpatient Parenteral Antimicrobial Therapy Programmes: An International Multi-Centre Survey. JAC Antimicrob. Resist. 2025, 7, dlaf075. [Google Scholar] [CrossRef]
- Triffault-Fillit, C.; Ferry, T.; Perpoint, T.; Adélaïde, L.; Le Ngoc Tho, S.; Ader, F.; Chidiac, C.; Valour, F. Outpatient Parenteral Antibiotic Therapy: Evaluation of Practices and Limits of Use in Rural Areas in France. Médecine Mal. Infect. 2018, 48, 130–135. [Google Scholar] [CrossRef]
- Lacroix, A.; Revest, M.; Patrat-Delon, S.; Lemaître, F.; Donal, E.; Lorléac’H, A.; Arvieux, C.; Michelet, C.; Tattevin, P. Traitement Parentéral Ambulatoire Des Endocardites Infectieuses: Une Stratégie Coût-Efficace [Outpatient Parenteral Antimicrobial Therapy for Infective Endocarditis: A Cost-Effective Strategy]. Médecine Mal. Infect. 2014, 44, 327–330. [Google Scholar] [CrossRef]
- Rolland, L.; Mainguy, A.; Boissier, S.; Ki Zerbo, M.; Tardivel, A.; Sébillotte, M.; Cailleaux, M.; Patrat-Delon, S.; Revest, M.; Tattevin, P. A Pilot Project of Expert Nurses for the Follow-up of Complex Intravenous Antimicrobial Treatment. Infect. Dis. Now. 2023, 53, 104670. [Google Scholar] [CrossRef]
- Reidy, P.; Breslin, T.; Muldoon, E. Outpatient Parenteral Antimicrobial Therapy (OPAT) across the World: A Comparative Analysis-What Lessons Can We Learn? JAC Antimicrob. Resist. 2024, 6, dlae111. [Google Scholar] [CrossRef]
- Durojaiye, O.C.; Fiori, C.; Cartwright, K. Delivery of Outpatient Parenteral Antimicrobial Therapy (OPAT) in an Ever-Changing National Health Service (UK): Benefits, Barriers, and Opportunities. Antibiotics 2025, 14, 451. [Google Scholar] [CrossRef]
- Raux, S.; Communaux, A.; Talarmin, J.P.; Khatchatourian, L. Optimizing Outpatient Parenteral Antimicrobial Therapy (OPAT): A Survey of Community Nurses’ Practices in France. Infect. Dis. Now. 2025, 55, 105088. [Google Scholar] [CrossRef] [PubMed]
- Muldoon, E.G.; Snydman, D.R.; Penland, E.C.; Allison, G.M. Are We Ready for an Outpatient Parenteral Antimicrobial Therapy Bundle? A Critical Appraisal of the Evidence. Clin. Infect. Dis. 2013, 57, 419–424. [Google Scholar] [CrossRef] [PubMed]
- Tice, A.D.; Rehm, S.J.; Dalovisio, J.R.; Bradley, J.S.; Martinelli, L.P.; Graham, D.R.; Gainer, R.B.; Kunkel, M.J.; Yancey, R.W.; Williams, D.N.; et al. Practice Guidelines for Outpatient Parenteral Antimicrobial Therapy. IDSA Guidelines. Clin. Infect. Dis. 2004, 38, 1651–1672. [Google Scholar] [CrossRef]
- Gilchrist, M.; Franklin, B.D.; Patel, J.P. An Outpatient Parenteral Antibiotic Therapy (OPAT) Map to Identify Risks Associated with an OPAT Service. J. Antimicrob. Chemother. 2008, 62, 177–183. [Google Scholar] [CrossRef]
- Agnihotri, G.; Gross, A.E.; Seok, M.; Yen, C.Y.; Khan, F.; Ebbitt, L.M.; Gay, C.; Bleasdale, S.C.; Sikka, M.K.; Trotter, A.B. Decreased Hospital Readmissions after Programmatic Strengthening of an Outpatient Parenteral Antimicrobial Therapy (OPAT) Program. Antimicrob. Steward. Healthc. Epidemiol. 2023, 3, e33. [Google Scholar] [CrossRef]
- Deng, H.; Gross, A.E.; Trotter, A.B.; Touchette, D.R. Cost Evaluation of a Nurse Coordinated Outpatient Parenteral Antimicrobial Therapy (OPAT) Program. Antimicrob. Steward. Healthc. Epidemiol. 2023, 3, e252. [Google Scholar] [CrossRef]
- Hamad, Y.; Lane, M.A.; Beekmann, S.E.; Polgreen, P.M.; Keller, S.C. Perspectives of United States-Based Infectious Diseases Physicians on Outpatient Parenteral Antimicrobial Therapy Practice. Open Forum Infect. Dis. 2019, 6, ofz363. [Google Scholar] [CrossRef]
- Psaltikidis, E.M.; Silva, E.N.d.; Bustorff-Silva, J.M.; Moretti, M.L.; Resende, M.R. Economic Evaluation of Outpatient Parenteral Antimicrobial Therapy: A Systematic Review. Expert. Rev. Pharmacoecon. Outcomes Res. 2017, 17, 355–375. [Google Scholar] [CrossRef]
- Conley, J.; O’Brien, C.W.; Leff, B.A.; Bolen, S.; Zulman, D. Alternative Strategies to Inpatient Hospitalization for Acute Medical Conditions: A Systematic Review. JAMA Intern. Med. 2016, 176, 1693–1702. [Google Scholar] [CrossRef]
- Bouygard, A.; Lavigne, C.; Remay, F. Missions des Prestataires de Services et Distributeurs de Matériel; Inspection Générale des Affaires Sociales: Paris, France, 2020. [Google Scholar]
- Certification des Prestataires de Services et Distributeurs de Matériel (PSDM): La HAS Publie le Référentiel. Available online: https://www.has-sante.fr/jcms/p_3525164/fr/certification-des-prestataires-de-services-et-distributeurs-de-materiel-psdm-la-has-publie-le-referentiel (accessed on 24 December 2024).
- Boese, C.K.; Lechler, P.; Frink, M.; Hackl, M.; Eysel, P.; Ries, C. Cost-Analysis of Inpatient and Outpatient Parenteral Antimicrobial Therapy in Orthopaedics: A Systematic Literature Review. World J. Clin. Cases 2019, 7, 1825–1836. [Google Scholar] [CrossRef]
- Dimitrova, M.; Gilchrist, M.; Seaton, R.A. Outpatient Parenteral Antimicrobial Therapy (OPAT) versus Inpatient Care in the UK: A Health Economic Assessment for Six Key Diagnoses. BMJ Open 2021, 11, e049733. [Google Scholar] [CrossRef] [PubMed]
- Staples, J.A.; Ho, M.; Ferris, D.; Hayek, J.; Liu, G.; Tran, K.C.; Sutherland, J.M. Outpatient Versus Inpatient Intravenous Antimicrobial Therapy: A Population-Based Observational Cohort Study of Adverse Events and Costs. Clin. Infect. Dis. 2022, 75, 1921–1929. [Google Scholar] [CrossRef] [PubMed]
- Or, Z.; Gandré, C.; Seppänen, A.; Hernandez-Quevedo, C.; Webb, E.; Chevreul, K. France: Health System Summary, 2024; European Observatory on Health Systems and Policies: Copenhagen, Denmark, 2024. [Google Scholar]
- Schoonenboom, J.; Johnson, R.B. How to Construct a Mixed Methods Research Design. Kolner Z. Soziol. Sozpsychol. 2017, 69, 107–131. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.R. A General Inductive Approach for Analyzing Qualitative Evaluation Data. American Journal of Evaluation. Am. J. Eval. 2006, 27, 237–246. [Google Scholar] [CrossRef]
- Nomenclatures: La NGAP et la LPP. Available online: https://www.ameli.fr/paris/infirmier/exercice-liberal/facturation-remuneration/nomenclatures-ngap-lpp (accessed on 24 February 2025).
- Le Codage des Actes Biologiques—NABM. Available online: https://www.ameli.fr/paris/medecin/exercice-liberal/facturation-remuneration/consultations-actes/nomenclatures-codage/codage-actes-biologiques-nabm (accessed on 24 February 2025).
- Nomenclatures: Ameli.fr. Available online: http://www.codage.ext.cnamts.fr/codif/bdm_it/index_presentation.php?p_site=AMELI (accessed on 24 February 2025).
| Unit/Department | Profession | Gender | Age (Years) | Experience in Unit | Roles in OPAT Service |
|---|---|---|---|---|---|
| Orthopedics | Physician | Female | 40 | 6 years | Prescription |
| Pulmonology | Physician | Female | 52 | 22 years | Prescription |
| Pulmonology | Specialist Nurse | Female | 54 | 3 months | Coordination Monitoring Telephone triage |
| Infectious Diseases | Physician | Male | 37 | 5 years | Prescription Monitoring |
| Diabetes | Physician | Female | 34 | 3 years | Prescription |
| HaH | Manager | Female | 55 | 11 years | Coordination Team management |
| HaH | Physician | Male | 35 | 2 years | Prescription |
| HaH | Physician | Male | 41 | 6 years | Prescription Monitoring |
| Hospital discharge facilitation | Nurse | Female | 26 | 4 months | Coordination Monitoring |
| MSDP | Nurse | Female | 46 | 4 years | Coordination Monitoring |
| Model | OPAT Initiation | OPAT Monitoring | OPAT Service Structure |
|---|---|---|---|
| A 50 per year | Prescription: In acute care unit, by ID physician Discharge coordination: MSDP IV access coordination: By attending physician or ID physician prior to discharge | Clinical follow-up: Evaluation of treatment effectiveness and tolerance by ID physician. Response to AE in outpatient visit, in ED, or on readmission Biological monitoring: Patient discharged after tolerance verified. Local laboratory if required; results difficult to obtain IV device monitoring: By visiting nurse. Response to AE in ED or acute care unit. PICC line removal by ID physician or in acute care unit as outpatient | Financing: MSDP coordination fee and supplies, local pharmacy, freelance visiting nurse Team structure: Two ID physicians. Coordination externalized to MSDP Communication: ID physician can be reached (phone, email) by patient, visiting nurse, and MSDP during working hours Documentation: By ID physician, in electronic medical record accessible by acute care referral physician |
| B 3 to 10 per year | Prescription: By attending physician in acute care unit; ID referral not systematic Discharge coordination: MSDP IV access coordination: By attending physician prior to discharge | Clinical follow-up: Evaluation of treatment effectiveness by MSDP and during next scheduled visit with attending physician. Tolerance evaluated by MSDP. Response to AE in outpatient visit, in ED, or on readmission Biological monitoring: Patient discharged after tolerance verified. Local laboratory if required; results difficult to obtain IV device monitoring: By visiting nurse. Response to AE in ED or acute care unit. PICC line removal in acute care unit as outpatient | Financing: MSDP coordination fee and supplies, local pharmacy, freelance visiting nurse Team structure: Attending physicians (variable); coordination externalized to MSDP Communication: Attending physician can be reached (phone, email) by MSDP during working hours. MSDP relays nurse and patient concerns Documentation: In hospital electronic medical record on discharge and during next patient visit |
| C 450 per year | Prescription: By attending physician with expertise in antimicrobial therapy; no ID referral Discharge coordination: Specialist nurse in acute care unit IV access coordination: By specialist nurse prior to discharge or as outpatient | Clinical follow-up: Evaluation of treatment tolerance and effectiveness by specialist nurse during first week and at end of OPAT, by specialist nurse or during next scheduled visit with attending physician. Response to AE and PICC line removal in acute care unit as outpatient Biological monitoring: Patient discharged after tolerance verified. Local laboratory if required; results obtained by specialist nurse IV device monitoring: By visiting nurse. Response to AE and PICC line removal in unit as outpatient by specialist nurse | Financing: Specialist nurse coordination fee, MSDP coordination fee and supplies, local pharmacy, freelance visiting nurse. Outpatient PICC line removal fee Team structure: Five attending physicians, four specialist nurses Communication: Specialist nurses can be reached (phone, email) by patient and visiting nurse Documentation: In hospital electronic medical record throughout OPAT |
| D 10 per year | Prescription: By attending physician in acute care unit; no ID referral Discharge coordination: Discharge facilitator nurse and MSDP IV access coordination: By attending physician prior to discharge | Clinical follow-up: Evaluation of treatment effectiveness during next scheduled visit with attending physician. Tolerance evaluated by MSDP and discharge facilitator (redundancy). Response to severe AE in ED or on readmission Biological monitoring: Patient discharged after tolerance verified. Local laboratory if required; results difficult to obtain IV device monitoring: By visiting nurse. Response to AE in ED or acute care unit PICC line removal in acute care unit as outpatient | Financing: Discharge facilitation fee, MSDP coordination fee and supplies, local pharmacy, freelance visiting nurse Team structure: Attending physicians (variable); coordination externalized to discharge facilitator Communication: Attending physician can be reached (phone, email) by MSDP during working hours. MSDP relays nurse and patient concerns, often without notifying discharge facilitator Documentation: In hospital electronic medical record on discharge and during next patient visit |
| E 30 per year | Prescription: By attending physician in acute care unit, with or without ID referral Discharge coordination: HaH discharge coordinator and liaison nurse IV access coordination: By attending physician prior to discharge or HaH physician | Clinical follow-up: Daily evaluation of treatment tolerance and effectiveness by HaH nursing team and physician. Response to AE through HaH services, in ED, or on readmission if severe Biological monitoring: As needed, through nearest laboratory within network IV device monitoring: By visiting nurse. Response to AE in ED or acute care unit. PICC line removal by HaH nurse | Financing: Patient Diagnosis Group baseline fee, adjusted for dependency score and treatment time, including all antimicrobials, equipment, and supplies Team structure: HaH physicians on call 24 h a day. HaH nurse coordinators are distributed throughout hospital network and liaison nurses and HaH nurses are distributed by geographical sector; 40% of care is contracted out to freelance community nurses Communication: HaH physician can be reached by phone 24/7 Documentation: In electronic medical record specific to HaH—not accessible to acute care unit |
| Services Billed to National Health Insurance | MSDP (Models A and B) | Nurse-Led (Model C) | Discharge Facilitation (Model D) | Hospital at Home (Model E) |
|---|---|---|---|---|
| Medical service and device provider | ||||
| Home infusion one-time set-up fee | 229 | 229 | 229 | - |
| Weekly monitoring | 46 | 46 | 46 | - |
| Weekly devices and supplies | 410 | 410 | 410 | - |
| Pharmacy | 226 | 226 | 226 | - |
| Visiting nurse | 369 | 369 | 369 | - |
| Local laboratory blood test processing | 18 | 18 | 18 | - |
| Hospital-based outpatient nursing care | ||||
| OPAT coordination | - | 13 | - | - |
| PICC line removal | 13 | 13 | 13 | - |
| Patient transportation for PICC line removal | 134 * | 134 * | 134 * | - |
| HaH, first week | - | - | - | 2308 † |
| Hospital-based discharge facilitation | - | - | 150 ‡ | - |
| Total | 1445 | 1458 | 1595 | 2308 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Burnet, E.; Le Bras, A.; Roucoux, G.; Dupont, C.; Canouï, E.; Leclaire, C.; Zerbit, J.; Burgel, P.R.; Martin, C.; Durand-Zaleski, I.; et al. Outpatient Parenteral Antimicrobial Therapy in a Tertiary Hospital in France: A Description of Service Models and Costs. Antibiotics 2025, 14, 971. https://doi.org/10.3390/antibiotics14100971
Burnet E, Le Bras A, Roucoux G, Dupont C, Canouï E, Leclaire C, Zerbit J, Burgel PR, Martin C, Durand-Zaleski I, et al. Outpatient Parenteral Antimicrobial Therapy in a Tertiary Hospital in France: A Description of Service Models and Costs. Antibiotics. 2025; 14(10):971. https://doi.org/10.3390/antibiotics14100971
Chicago/Turabian StyleBurnet, Espérie, Alicia Le Bras, Guillaume Roucoux, Christian Dupont, Etienne Canouï, Clément Leclaire, Jérémie Zerbit, Pierre Régis Burgel, Clémence Martin, Isabelle Durand-Zaleski, and et al. 2025. "Outpatient Parenteral Antimicrobial Therapy in a Tertiary Hospital in France: A Description of Service Models and Costs" Antibiotics 14, no. 10: 971. https://doi.org/10.3390/antibiotics14100971
APA StyleBurnet, E., Le Bras, A., Roucoux, G., Dupont, C., Canouï, E., Leclaire, C., Zerbit, J., Burgel, P. R., Martin, C., Durand-Zaleski, I., & Duracinsky, M. (2025). Outpatient Parenteral Antimicrobial Therapy in a Tertiary Hospital in France: A Description of Service Models and Costs. Antibiotics, 14(10), 971. https://doi.org/10.3390/antibiotics14100971







