Impact of Education on Inappropriate Antibiotic Prescription for Respiratory Tract Infection Based on Physicians’ Justifications: A Web-Based Survey in Japan
Abstract
1. Introduction
2. Methods
2.1. Study Design and Participants
2.2. Fictional Scenarios and the Educational Film
2.3. Statistical Analysis
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Spellberg, B.; Guidos, R.; Gilbert, D.; Bradley, J.; Boucher, H.W.; Scheld, W.M.; Bartlett, J.G.; Edwards, J., Jr. The epidemic of antibiotic-resistant infections: A call to action for the medical community from the Infectious Diseases Society of America. Clin. Infect. Dis. 2008, 46, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Bell, B.G.; Schellevis, F.; Stobberingh, E.; Goossens, H.; Pringle, M. A systematic review and meta-analysis of the effects of antibiotic consumption on antibiotic resistance. BMC Infect. Dis. 2014, 14, 13. [Google Scholar] [CrossRef] [PubMed]
- Gonzales, R.; Steiner, J.F.; Sande, M.A. Antibiotic prescribing for adults with colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians. JAMA 1997, 278, 901–904. [Google Scholar] [CrossRef] [PubMed]
- Kasse, G.E.; Cosh, S.M.; Humphries, J.; Islam, M.S. Antimicrobial prescription pattern and appropriateness for respiratory tract infection in outpatients: A systematic review and meta-analysis. Syst. Rev. 2024, 13, 229. [Google Scholar] [CrossRef] [PubMed]
- McKay, R.; Mah, A.; Law, M.R.; McGrail, K.; Patrick, D.M. Systematic Review of Factors Associated with Antibiotic Prescribing for Respiratory Tract Infections. Antimicrob. Agents Chemother. 2016, 60, 4106–4118. [Google Scholar] [CrossRef]
- Smith, S.M.; Smucny, J.; Fahey, T. Antibiotics for acute bronchitis. JAMA 2014, 312, 2678–2679. [Google Scholar] [CrossRef]
- Komiya, K.; Kudoh, R.; Kaku, N.; Shindo, Y.; Hayashi, T.; Kasahara, K.; Oishi, T.; Ishiwada, N.; Ito, M.; Yotsuyanagi, H.; et al. Impact of Educational Films on Antibiotic Prescription among Physicians: A Web-Based Survey in Japan. Antibiotics 2024, 13, 724. [Google Scholar] [CrossRef]
- Shulman, S.T.; Bisno, A.L.; Clegg, H.W.; Gerber, M.A.; Kaplan, E.L.; Lee, G.; Martin, J.M.; Van Beneden, C. Executive Summary: Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2012, 55, 1279–1282. [Google Scholar] [CrossRef]
- Ishiwada, N.; Shinjoh, M.; Kusama, Y.; Arakawa, H.; Ohishi, T.; Saitoh, A.; Suzuki, A.; Tsutsumi, H.; Nishi, J.; Hoshino, T.; et al. Guidelines for the Management of Respiratory Infectious Diseases in Children in Japan 2022. Pediatr. Infect. Dis. J. 2023, 42, e369–e376. [Google Scholar] [CrossRef]
- Smith, M.P.; Lown, M.; Singh, S.; Ireland, B.; Hill, A.T.; Linder, J.A.; Irwin, R.S. Acute Cough Due to Acute Bronchitis in Immunocompetent Adult Outpatients: CHEST Expert Panel Report. Chest 2020, 157, 1256–1265. [Google Scholar] [CrossRef]
- Lee, R.A.; Centor, R.M.; Humphrey, L.L.; Jokela, J.A.; Andrews, R.; Qaseem, A.; Akl, E.A.; Bledsoe, T.A.; Forciea, M.A.; Haeme, R.; et al. Appropriate Use of Short-Course Antibiotics in Common Infections: Best Practice Advice From the American College of Physicians. Ann. Intern. Med. 2021, 174, 822–827. [Google Scholar] [CrossRef] [PubMed]
- Chow, A.W.; Benninger, M.S.; Brook, I.; Brozek, J.L.; Goldstein, E.J.; Hicks, L.A.; Pankey, G.A.; Seleznick, M.; Volturo, G.; Wald, E.R.; et al. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2012, 54, e72–e112. [Google Scholar] [CrossRef]
- Wald, E.R.; Applegate, K.E.; Bordley, C.; Darrow, D.H.; Glode, M.P.; Marcy, S.M.; Nelson, C.E.; Rosenfeld, R.M.; Shaikh, N.; Smith, M.J.; et al. Clinical practice guideline for the diagnosis and management of acute bacterial sinusitis in children aged 1 to 18 years. Pediatrics 2013, 132, e262–e280. [Google Scholar] [CrossRef] [PubMed]
- Shulman, S.T.; Bisno, A.L.; Clegg, H.W.; Gerber, M.A.; Kaplan, E.L.; Lee, G.; Martin, J.M.; Van Beneden, C. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2012, 55, e86–e102. [Google Scholar] [CrossRef]
- Butler, C.C.; Rollnick, S.; Pill, R.; Maggs-Rapport, F.; Stott, N. Understanding the culture of prescribing: Qualitative study of general practitioners’ and patients’ perceptions of antibiotics for sore throats. BMJ 1998, 317, 637–642. [Google Scholar] [CrossRef]
- Moro, M.L.; Marchi, M.; Gagliotti, C.; Di Mario, S.; Resi, D. Why do paediatricians prescribe antibiotics? Results of an Italian regional project. BMC Pediatr. 2009, 9, 69. [Google Scholar] [CrossRef]
- Coenen, S.; Francis, N.; Kelly, M.; Hood, K.; Nuttall, J.; Little, P.; Verheij, T.J.; Melbye, H.; Goossens, H.; Butler, C.C. Are patient views about antibiotics related to clinician perceptions, management and outcome? A multi-country study in outpatients with acute cough. PLoS ONE 2013, 8, e76691. [Google Scholar] [CrossRef]
- Machowska, A.; Stålsby Lundborg, C. Drivers of Irrational Use of Antibiotics in Europe. Int. J. Environ. Res. Public Health 2018, 16, 27. [Google Scholar] [CrossRef]
- Meeker, D.; Knight, T.K.; Friedberg, M.W.; Linder, J.A.; Goldstein, N.J.; Fox, C.R.; Rothfeld, A.; Diaz, G.; Doctor, J.N. Nudging guideline-concordant antibiotic prescribing: A randomized clinical trial. JAMA Intern. Med. 2014, 174, 425–431. [Google Scholar] [CrossRef]
- Haenssgen, M.J.; Xayavong, T.; Charoenboon, N.; Warapikuptanun, P.; Khine Zaw, Y. The Consequences of AMR Education and Awareness Raising: Outputs, Outcomes, and Behavioural Impacts of an Antibiotic-Related Educational Activity in Lao PDR. Antibiotics 2018, 7, 95. [Google Scholar] [CrossRef]
- Okubo, Y.; Nishi, A.; Michels, K.B.; Nariai, H.; Kim-Farley, R.J.; Arah, O.A.; Uda, K.; Kinoshita, N.; Miyairi, I. The consequence of financial incentives for not prescribing antibiotics: A Japan’s nationwide quasi-experiment. Int. J. Epidemiol. 2022, 51, 1645–1655. [Google Scholar] [CrossRef]
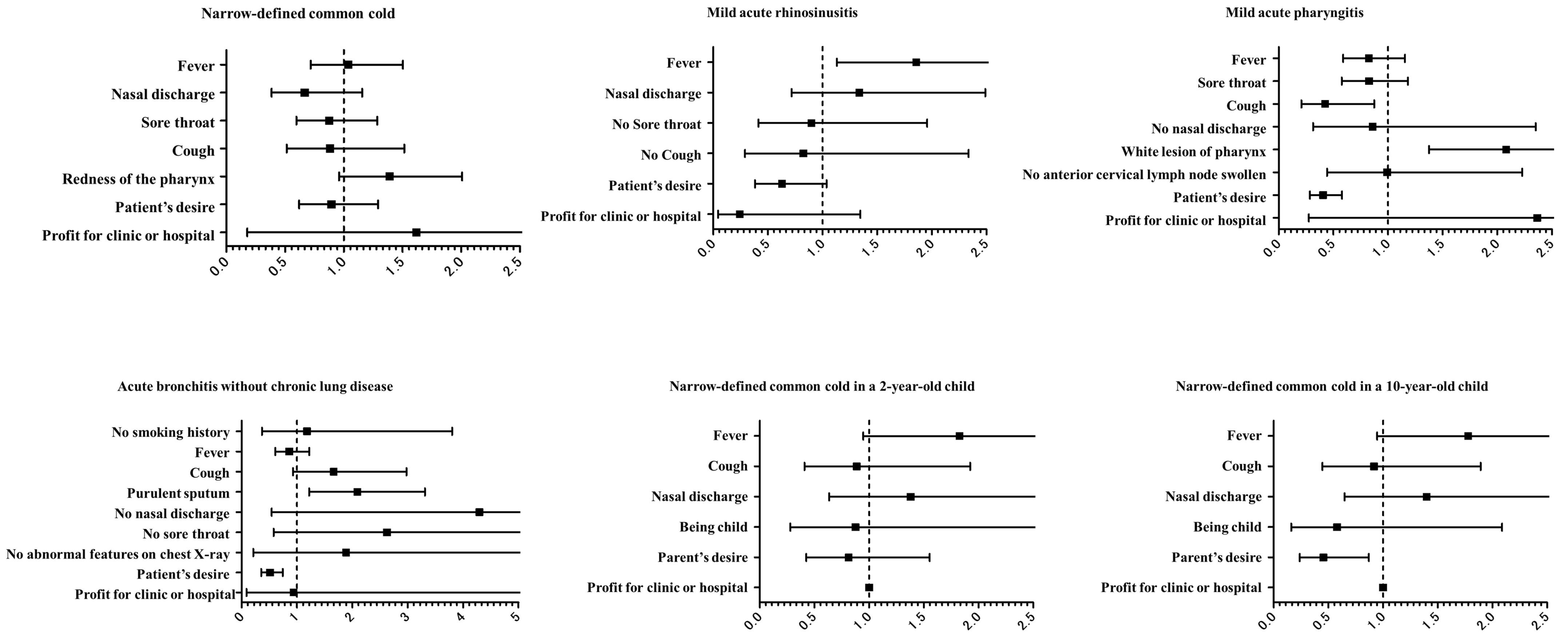
| Narrowly Defined Common Cold (n = 557) | Mild Acute Rhinosinusitis (n = 300) | Mild Acute Pharyngitis (n = 775) | |||
| Fever | 251 (45.1%) | Fever | 135 (45.0%) | Fever | 208 (26.8%) |
| Nasal discharge | 63 (11.3%) | Nasal discharge | 60 (20.0%) | Sore throat | 170 (21.9%) |
| Sore throat | 190 (34.1%) | No sore throat | 31 (10.3%) | Cough | 31 (4.0%) |
| Cough | 71 (12.7%) | No cough | 16 (5.3%) | No nasal discharge | 17 (2.2%) |
| Redness of the pharynx | 304 (54.6%) | Patient’s desire | 176 (58.7%) | White lesion of pharynx | 668 (86.2%) |
| Patient’s desire | 264 (47.4%) | Profit for clinic or hospital | 6 (2.0%) | No anterior cervical lymph node swollen | 28 (3.6%) |
| Profit for clinic or hospital | 5 (0.9%) | Patient’s desire | 163 (21.0%) | ||
| Profit for clinic or hospital | 6 (0.8%) | ||||
| Acute Bronchitis Without Chronic Lung Disease (n = 688) | Narrowly Defined Common Cold in a 2-Year-Old Child (n = 153) | Narrowly Defined Common Cold in a 10-Year-Old Child (n = 168) | |||
| No smoking history | 14 (2.0%) | Fever | 66 (43.1%) | Fever | 87 (51.8%) |
| Fever | 198 (28.8%) | Cough | 33 (21.6%) | Cough | 41 (24.4%) |
| Cough | 70 (10.2%) | Nasal discharge | 35 (22.9%) | Nasal discharge | 38 (22.6%) |
| Purulent sputum | 603 (87.6%) | Being child | 13 (8.5%) | Being child | 10 (6.0%) |
| No nasal discharge | 10 (1.5%) | Parent’s desire | 86 (56.2%) | Parent’s desire | 92 (54.8%) |
| No sore throat | 13 (1.9%) | Profit for clinic or hospital | 2 (1.3%) | Profit for clinic or hospital | 0 (0.0%) |
| No abnormal features on chest X-ray | 5 (0.7%) | ||||
| Patient’s desire | 150 (21.8%) | ||||
| Profit for clinic or hospital | 3 (0.4%) | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kudoh, R.; Komiya, K.; Kaku, N.; Shindo, Y.; Hayashi, T.; Kasahara, K.; Oishi, T.; Ishiwada, N.; Ito, M.; Yotsuyanagi, H.; et al. Impact of Education on Inappropriate Antibiotic Prescription for Respiratory Tract Infection Based on Physicians’ Justifications: A Web-Based Survey in Japan. Antibiotics 2024, 13, 1022. https://doi.org/10.3390/antibiotics13111022
Kudoh R, Komiya K, Kaku N, Shindo Y, Hayashi T, Kasahara K, Oishi T, Ishiwada N, Ito M, Yotsuyanagi H, et al. Impact of Education on Inappropriate Antibiotic Prescription for Respiratory Tract Infection Based on Physicians’ Justifications: A Web-Based Survey in Japan. Antibiotics. 2024; 13(11):1022. https://doi.org/10.3390/antibiotics13111022
Chicago/Turabian StyleKudoh, Ryohei, Kosaku Komiya, Norihito Kaku, Yuichiro Shindo, Tatsuya Hayashi, Kei Kasahara, Tomohiro Oishi, Naruhiko Ishiwada, Makoto Ito, Hiroshi Yotsuyanagi, and et al. 2024. "Impact of Education on Inappropriate Antibiotic Prescription for Respiratory Tract Infection Based on Physicians’ Justifications: A Web-Based Survey in Japan" Antibiotics 13, no. 11: 1022. https://doi.org/10.3390/antibiotics13111022
APA StyleKudoh, R., Komiya, K., Kaku, N., Shindo, Y., Hayashi, T., Kasahara, K., Oishi, T., Ishiwada, N., Ito, M., Yotsuyanagi, H., Hasegawa, N., Tateda, K., Hotomi, M., & Yanagihara, K. (2024). Impact of Education on Inappropriate Antibiotic Prescription for Respiratory Tract Infection Based on Physicians’ Justifications: A Web-Based Survey in Japan. Antibiotics, 13(11), 1022. https://doi.org/10.3390/antibiotics13111022







