Bloodstream Infections in Intensive Care Unit during Four Consecutive SARS-CoV-2 Pandemic Waves
Abstract
:1. Introduction
2. Results
2.1. Characteristics of the Study Population
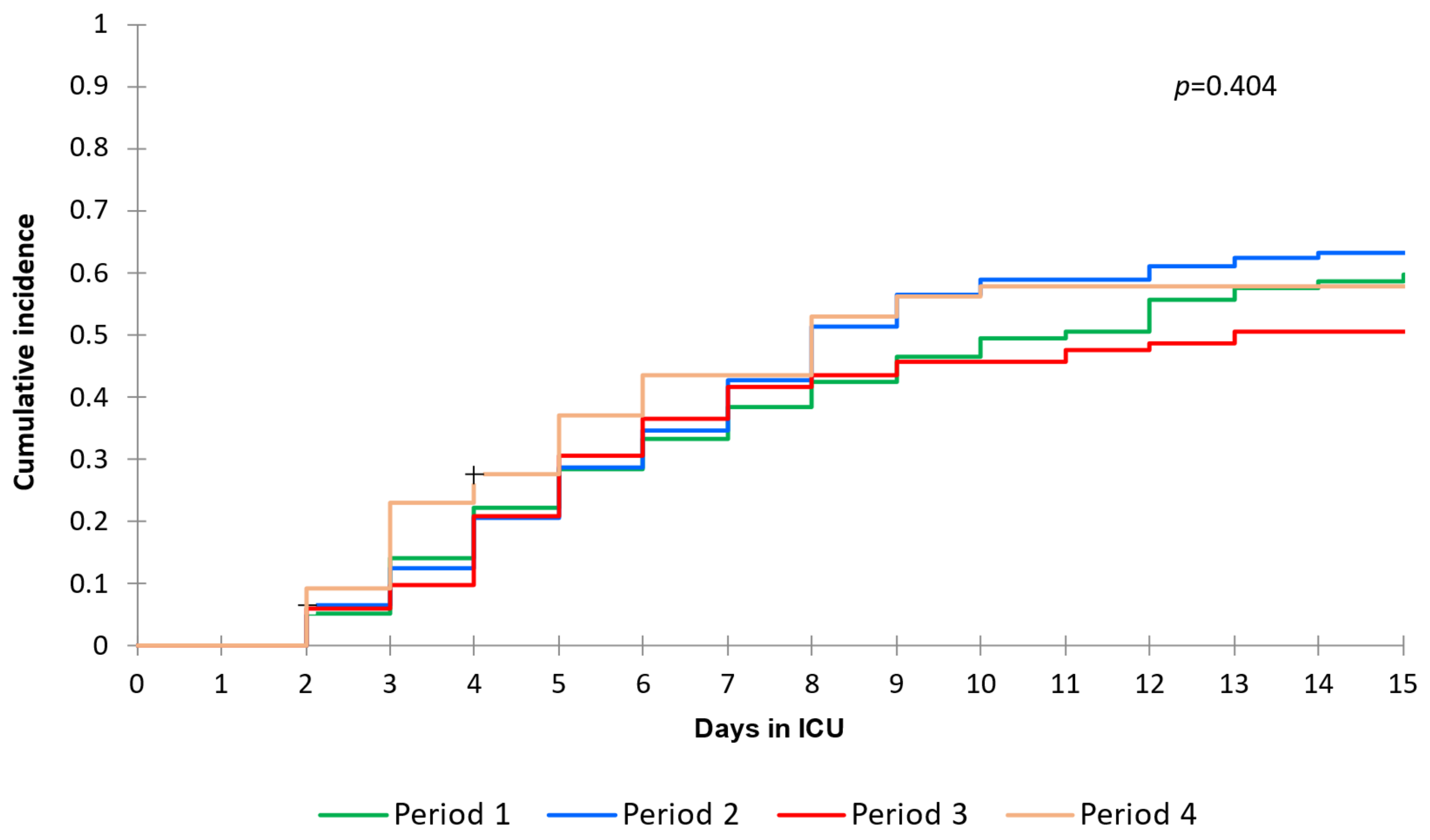
2.2. Bloodstream Infections Incidence
2.3. Epidemiology of BSI
3. Discussion
4. Materials and Methods
4.1. Study Design, Setting and Participants
4.2. Data Collection, Procedures and Definitions
4.3. Laboratory Procedures
4.4. Outcomes
4.5. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grasselli, G.; Pesenti, A.; Cecconi, M. Critical Care Utilization for the COVID-19 Outbreak in Lombardy, Italy: Early Experience and Forecast During an Emergency Response. J. Am. Med. Assoc. 2020, 323, 1545–1546. [Google Scholar] [CrossRef]
- Bonazzetti, C.; Rinaldi, M.; Giacomelli, A.; Colombo, R.; Ottolina, D.; Rimoldi, S.G.; Pagani, C.; Morena, V.; Ridolfo, A.L.; Vatamanu, O.; et al. Risk factors associated with bacteremia in COVID-19 patients admitted to intensive care unit: A retrospective multicenter cohort study. Infection 2022, 51, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Cataldo, M.A.; Tetaj, N.; Selleri, M.; Marchioni, L.; Capone, A.; Caraffa, E.; Di Caro, A.; Petrosillo, N. Incidence of bacterial and fungal bloodstream infections in COVID-19 patients in intensive care: An alarming “collateral effect”. J. Glob. Antimicrob. Resist. 2020, 23, 290–291. [Google Scholar] [CrossRef]
- AER_for_2017-HAI.pdf [Internet]. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/AER_for_2017-HAI.pdf (accessed on 6 June 2023).
- Bauer, K.A.; Puzniak, L.A.; Yu, K.C.; Finelli, L.; Moise, P.; Ai, C.; Watts, J.A.; Gupta, V. Epidemiology and outcomes of culture-positive bloodstream pathogens prior to and during the SARS-CoV-2 pandemic: A multicenter evaluation. BMC Infect. Dis. 2022, 22, 841. [Google Scholar] [CrossRef]
- Bhatt, P.J.; Shiau, S.; Brunetti, L.; Xie, Y.; Solanki, K.; Khalid, S.; Mohayya, S.; Au, P.H.; Pham, C.; Uprety, P.; et al. Risk Factors and Outcomes of Hospitalized Patients with Severe Coronavirus Disease 2019 (COVID-19) and Secondary Bloodstream Infections: A Multicenter Case-Control Study. Clin. Infect. Dis. 2020, 72, e995–e1003. [Google Scholar] [CrossRef] [PubMed]
- Hedberg, P.; Ternhag, A.; Giske, C.G.; Strålin, K.; Özenci, V.; Johansson, N.; Spindler, C.; Hedlund, J.; Mårtensson, J.; Nauclér, P. Ventilator-Associated Lower Respiratory Tract Bacterial Infections in COVID-19 Compared with Non-COVID-19 Patients. Crit. Care Med. 2022, 50, 825–836. [Google Scholar] [CrossRef] [PubMed]
- Rouzé, A.; Martin-Loeches, I.; Povoa, P.; Makris, D.; Artigas, A.; Bouchereau, M.; Lambiotte, F.; Metzelard, M.; Cuchet, P.; Geronimi, C.B. Relationship between SARS-CoV-2 infection and the incidence of ventilator-associated lower respiratory tract infections: A European multicenter cohort study. Intensive Care Med. 2021, 47, 188–198. [Google Scholar] [CrossRef]
- Grau, S.; Echeverria-Esnal, D.; Gómez-Zorrilla, S.; Navarrete-Rouco, M.E.; Masclans, J.R.; Espona, M.; Gracia-Arnillas, M.P.; Duran, X.; Comas, M.; Horcajada, J.P.; et al. Evolution of Antimicrobial Consumption During the First Wave of COVID-19 Pandemic. Antibiotics 2021, 10, 132. [Google Scholar] [CrossRef]
- Castro-Lopes, A.; Correia, S.; Leal, C.; Resende, I.; Soares, P.; Azevedo, A.; Paiva, J.-A. Increase of Antimicrobial Consumption in a Tertiary Care Hospital during the First Phase of the COVID-19 Pandemic. Antibiotics 2021, 10, 778. [Google Scholar] [CrossRef]
- Giacomelli, A.; Ridolfo, A.L.; Oreni, L.; Vimercati, S.; Albrecht, M.; Cattaneo, D.; Rimoldi, S.G.; Rizzardini, G.; Galli, M.; Antinori, S. Consumption of antibiotics at an Italian university hospital during the early months of the COVID-19 pandemic: Were all antibiotic prescriptions appropriate? Pharmacol. Res. 2021, 164, 105403. [Google Scholar] [CrossRef]
- Bonazzetti, C.; Morena, V.; Giacomelli, A.; Oreni, L.B.; Casalini, G.; Galimberti, L.R.; Bolis, M.; Rimoldi, M.N.; Ballone, E.; Colombo, R.; et al. Unexpectedly High Frequency of Enterococcal Bloodstream Infections in Coronavirus Disease 2019 Patients Admitted to an Italian ICU: An Observational Study. Crit. Care Med. 2020, 49, e31–e40. [Google Scholar] [CrossRef]
- Giacobbe, D.R.; Labate, L.; Tutino, S.; Baldi, F.; Russo, C.; Robba, C.; Ball, L.; Dettori, S.; Marchese, A.; Dentone, C.; et al. Enterococcal bloodstream infections in critically ill patients with COVID-19: A case series. Ann. Med. 2021, 53, 1779–1786. [Google Scholar] [CrossRef]
- Posteraro, B.; De Angelis, G.; Menchinelli, G.; D’inzeo, T.; Fiori, B.; De Maio, F.; Cortazzo, V.; Sanguinetti, M.; Spanu, T. Risk Factors for Mortality in Adult COVID-19 Patients Who Develop Bloodstream Infections Mostly Caused by Antimicrobial-Resistant Organisms: Analysis at a Large Teaching Hospital in Italy. J. Clin. Med. 2021, 10, 1752. [Google Scholar] [CrossRef]
- DeVoe, C.; Segal, M.R.; Wang, L.; Stanley, K.; Madera, S.; Fan, J.; Schouest, J.; Graham-Ojo, R.; Nichols, A.; Prasad, P.A.; et al. Increased rates of secondary bacterial infections, including Enterococcus bacteremia, in patients hospitalized with coronavirus disease 2019 (COVID-19). Infect. Control. Hosp. Epidemiol. 2021, 43, 1416–1423. [Google Scholar] [CrossRef]
- McLaughlin, A.; Montoya, V.; Miller, R.L.; Mordecai, G.J.; Worobey, M.; Poon, A.F.; Joy, J.B.; Canadian COVID-19 Genomics Network (CanCOGen) Consortium. Genomic epidemiology of the first two waves of SARS-CoV-2 in Canada. eLife 2022, 11, e73896. [Google Scholar] [CrossRef] [PubMed]
- Aznar-Gimeno, R.; Paño-Pardo, J.R.; Esteban, L.M.; Labata-Lezaun, G.; Esquillor-Rodrigo, M.J.; Lanas, A.; Abadía-Gallego, D.; Diez-Fuertes, F.; Tellería-Orriols, C.; Del-Hoyo-Alonso, R.; et al. Changes in severity, mortality, and virus genome among a Spanish cohort of patients hospitalized with SARS-CoV-2. Sci. Rep. 2021, 11, 18844. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, Q.; Inchakalody, V.P.; Merhi, M.; Mestiri, S.; Taib, N.; El-Ella, D.M.A.; Bedhiafi, T.; Raza, A.; Al-Zaidan, L.; Mohsen, M.O.; et al. Emerging COVID-19 variants and their impact on SARS-CoV-2 diagnosis, therapeutics and vaccines. Ann. Med. 2022, 54, 524–540. [Google Scholar] [CrossRef]
- Li, M.; Wang, H.; Tian, L.; Pang, Z.; Yang, Q.; Huang, T.; Fan, J.; Song, L.; Tong, Y.; Fan, H. COVID-19 vaccine development: Milestones, lessons and prospects. Signal Transduct. Target. Ther. 2022, 7, 146. [Google Scholar] [CrossRef]
- Sturm, L.K.; Saake, K.; Roberts, P.B.; Masoudi, F.A.; Fakih, M.G. Impact of COVID-19 pandemic on hospital onset bloodstream infections (HOBSI) at a large health system. Am. J. Infect. Control. 2022, 50, 245–249. [Google Scholar] [CrossRef]
- Pérez-Granda, M.; Carrillo, C.; Rabadán, P.; Valerio, M.; Olmedo, M.; Muñoz, P.; Bouza, E. Increase in the frequency of catheter-related bloodstream infections during the COVID-19 pandemic: A plea for control. J. Hosp. Infect. 2022, 119, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Ripa, M.; Galli, L.; Poli, A.; Oltolini, C.; Spagnuolo, V.; Mastrangelo, A.; Muccini, C.; Monti, G.; De Luca, G.; Landoni, G.; et al. Secondary infections in patients hospitalized with COVID-19: Incidence and predictive factors. Clin Microbiol Infect. 2021, 27, 451–457. [Google Scholar] [CrossRef] [PubMed]
- Ippolito, G.; Nicastri, E.; Martini, L.; Petrosillo, N. Hospital infection control in Italy. Infection 2003, 31, 4–9. [Google Scholar]
- Langford, B.J.; So, M.; Leung, V.; Raybardhan, S.; Lo, J.; Kan, T.; Leung, F.; Westwood, D.; Daneman, N.; MacFadden, D.R.; et al. Predictors and microbiology of respiratory and bloodstream bacterial infection in patients with COVID-19: Living rapid review update and meta-regression. Clin. Microbiol. Infect. 2022, 28, 491–501. [Google Scholar] [CrossRef] [PubMed]
- Yap, F.H.; Gomersall, C.D.; Fung, K.S.; Ho, P.-L.; Ho, O.-M.; Lam, P.K.N.; Lam, D.T.C.; Lyon, D.J.; Joynt, G.M. Increase in methicillinresistant Staphylococcus aureus acquisition rate and change in pathogen pattern associated with an outbreak of severe acute respiratory syndrome. Clin. Infect Dis. 2004, 39, 511–516. [Google Scholar] [CrossRef]
- Musuuza, J.S.; Watson, L.; Parmasad, V.; Putman-Buehler, N.; Christensen, L.; Safdar, N. Prevalence and outcomes of co-infection and superinfection with SARS-CoV-2 and other pathogens: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0251170. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.ecdc.europa.eu/en/publications-data/healthcare-associated-infections-intensive-care-units-2019 (accessed on 6 June 2023).
- Massart, N.; Maxime, V.; Fillatre, P.; Razazi, K.; Moine, P.; Legay, F.; Voiriot, G.; Amara, M.; Santi, F.; Nseir, S.; et al. Characteristics and prognosis of bloodstream infection in patients with COVID-19 admitted in the ICU: An ancillary study of the COVID-ICU study. Ann. Intensiv. Care 2021, 11, 183. [Google Scholar] [CrossRef]
- Grasselli, G.; Scaravilli, V.; Mangioni, D.; Scudeller, L.; Alagna, L.; Bartoletti, M.; Bellani, G.; Biagioni, E.; Bonfanti, P.; Bottino, N.; et al. Hospital-Acquired Infections in Critically Ill Patients With COVID-19. Chest 2021, 160, 454–465. [Google Scholar] [CrossRef]
- Kurt, A.F.; Mete, B.; Urkmez, S.; Demirkiran, O.; Dumanli, G.Y.; Bozbay, S.; Dilken, O.; Karaali, R.; Balkan, I.I.; Saltoğlu, N.; et al. Incidence, Risk Factors, and Prognosis of Bloodstream Infections in COVID-19 Patients in Intensive Care: A Single-Center Observational Study. J. Intensiv. Care Med. 2022, 37, 1353–1362. [Google Scholar] [CrossRef] [PubMed]
- Pasrija, R.; Naime, M. The deregulated immune reaction and cytokines release storm (CRS) in COVID-19 disease. Int. Immunopharmacol. 2021, 90, 107225. [Google Scholar] [CrossRef] [PubMed]
- COVID-ICU Group on behalf of the REVA Network and the COVID-ICU Investigators. Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: A prospective cohort study. Intensive Care Med. 2021, 47, 60–73. [Google Scholar] [CrossRef] [PubMed]
- Pandey, M.; May, A.; Tan, L.; Hughes, H.; Jones, J.P.; Harrison, W.; Bradburn, S.; Tyrrel, S.; Muthuswamy, B.; Berry, N.; et al. Comparative incidence of early and late bloodstream and respiratory tract co-infection in patients admitted to ICU with COVID-19 pneumonia versus Influenza A or B pneumonia versus no viral pneumonia: Wales multicentre ICU cohort study. Crit. Care 2022, 26, 158. [Google Scholar] [CrossRef] [PubMed]
- Dossett, L.A.; Dageforde, L.A.; Swenson, B.R.; Metzger, R.; Bonatti, H.; Sawyer, R.G.; May, A.K.; Tafelski, S.; Yi, H.; Ismaeel, F.; et al. Obesity and Site-Specific Nosocomial Infection Risk in the Intensive Care Unit. Surg. Infect. 2009, 10, 137–142. [Google Scholar] [CrossRef]
- Gasch, O.; Badia-Cebada, L.; Carmezim, J.; Vaqué, M.; Pomar, V.; Moreno, E.; Marrón, A.; Jiménez-Martínez, E.; García-Quesada, M.J.; Garcia-Alarcón, X.; et al. Effects of the COVID-19 Pandemic on Incidence and Epidemiology of Catheter-Related Bacteremia, Spain. Emerg. Infect. Dis. 2022, 28, 2181–2189. [Google Scholar] [CrossRef] [PubMed]
- Buetti, N.; Tabah, A.; Loiodice, A.; Aslan, A.T.; Montrucchio, G.; Cortegiani, A.; Saltoglu, N.; Kayaaslan, B.; Aksoy, F.; Murat, A.; et al. Different epidemiology of bloodstream infections in COVID-19 compared to non-COVID-19 critically ill patients: A descriptive analysis of the Eurobact II study. Crit. Care 2022, 26, 319. [Google Scholar] [CrossRef]
- Arias, C.A.; Murray, B.E. The rise of the Enterococcus: Beyond vancomycin resistance. Nat. Rev. Microbiol. 2012, 10, 266–278. [Google Scholar] [CrossRef]
- Amarsy, R.; Trystram, D.; Cambau, E.; Monteil, C.; Fournier, S.; Oliary, J.; Junot, H.; Sabatier, P.; Porcher, R.; Robert, J.; et al. Surging bloodstream infections and antimicrobial resistance during the first wave of COVID–19: A study in a large multihospital institution in the Paris region. Int. J. Infect. Dis. 2022, 114, 90–96. [Google Scholar] [CrossRef]
- Lamers, M.M.; Beumer, J.; van der Vaart, J.; Knoops, K.; Puschhof, J.; Breugem, T.I.; Ravelli, R.B.G.; van Schayck, J.P.; Mykytyn, A.Z.; Duimel, H.Q.; et al. SARS-CoV-2 productively infects human gut enterocytes. Science 2020, 369, 50–54. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.; He, L.; Zhang, Q.; Che, X.; Hou, J.; Wang, H.; Shen, H.; Qiu, L.; Li, Z.; Geng, J.; et al. Organ distribution of severe acute respiratory syndrome (SARS) associated coronavirus (SARSCoV) in SARS patients: Implications for pathogenesis and virus transmission pathways. J. Pathol. 2004, 203, 622–630. [Google Scholar] [CrossRef]
- Xiao, F.; Tang, M.; Zheng, X.; Liu, Y.; Li, X.; Shan, H. Evidence for Gastrointestinal Infection of SARS-CoV-2. Gastroenterology 2020, 158, 1831–1833.e3. [Google Scholar] [CrossRef] [PubMed]
- Polak, S.B.; Van Gool, I.C.; Cohen, D.; von der Thüsen, J.H.; van Paassen, J. A systematic review of pathological findings in COVID-19: A pathophysiological timeline and possible mechanisms of disease progression. Mod. Pathol. 2020, 33, 2128–2138. [Google Scholar] [CrossRef]
- Westerhoff, M.; Jones, D.; Hrycaj, S.M.; Chan, M.P.; Pantanowitz, L.; Tu, H.; Choi, K.; Greenson, J.; Lamps, L. Gastrointestinal Pathology in Samples from Coronavirus Disease 2019 (COVID-19)–Positive Patients. Arch. Pathol. Lab. Med. 2021, 145, 1062–1068. [Google Scholar] [CrossRef]
- Sloot, R.; Nsonwu, O.; Chudasama, D.; Rooney, G.; Pearson, C.; Choi, H.; Mason, E.; Springer, A.; Gerver, S.; Brown, C.; et al. Rising rates of hospital-onset Klebsiella spp. and Pseudomonas aeruginosa bacteraemia in NHS acute trusts in England: A review of national surveillance data, August 2020–February 2021. J. Hosp. Infect. 2021, 119, 175–181. [Google Scholar] [CrossRef]
- Rhoades, N.S.; Pinski, A.N.; Monsibais, A.N.; Jankeel, A.; Doratt, B.M.; Cinco, I.R.; Ibraim, I.; Messaoudi, I. Acute SARS-CoV-2 infection is associated with an increased abundance of bacterial pathogens, including Pseudomonas aeruginosa in the nose. Cell Rep. 2021, 36, 109637. [Google Scholar] [CrossRef]
- Paiva, J.-A.; Pereira, J.M.; Tabah, A.; Mikstacki, A.; de Carvalho, F.B.; Koulenti, D.; Ruckly, S.; Çakar, N.; Misset, B.; Dimopoulos, G.; et al. Characteristics and risk factors for 28-day mortality of hospital acquired fungemias in ICUs: Data from the EUROBACT study. Crit. Care 2016, 20, 53. [Google Scholar] [CrossRef]
- Antinori, S.; Bonazzetti, C.; Gubertini, G.; Capetti, A.; Pagani, C.; Morena, V.; Rimoldi, S.; Galimberti, L.; Sarzi-Puttini, P.; Ridolfo, A.L. Tocilizumab for cytokine storm syndrome in COVID-19 pneumonia: An increased risk for candidemia? Autoimmun. Rev. 2020, 19, 102564. [Google Scholar] [CrossRef]
- Colaneri, M.; Giusti, E.M.; Genovese, C.; Galli, L.; Lombardi, A.; Gori, A. Mortality of Patients with Candidemia and COVID-19: A Systematic Review with Meta-analysis. Open Forum Infect. Dis. 2023, 10, ofad358. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.epicentro.iss.it/coronavirus/sars-cov-2-sorveglianza-dati (accessed on 6 June 2023).
- Giacomelli, A.; Righini, E.; Micheli, V.; Pinoli, P.; Bernasconi, A.; Rizzo, A.; Oreni, L.; Ridolfo, A.L.; Antinori, S.; Ceri, S.; et al. SARS-CoV-2 viremia and COVID-19 mortality: A prospective observational study. PLoS ONE 2023, 18, e0281052. [Google Scholar] [CrossRef] [PubMed]
- Horan, T.C.; Andrus, M.; Dudeck, M.A. CDC/NHSN surveillance definition of health care–associated infection and criteria for specific types of infections in the acute care setting. Am. J. Infect. Control. 2008, 36, 309–332. [Google Scholar] [CrossRef]
- Laupland, K.; Kirkpatrick, A.; Church, D.; Ross, T.; Gregson, D. Intensive-care-unit-acquired bloodstream infections in a regional critically ill population. J. Hosp. Infect. 2004, 58, 137–145. [Google Scholar] [CrossRef] [PubMed]
- The European Committee on Antimicrobial Susceptibility Testing (EUCAST). Clinical Breakpoints and Dosing of Antibiotics. The European Committee on Antimicrobial Susceptibility Testing. Breakpoint Tables for Interpretation of MICs and Zone Diameters. Version 12.0. 2022. Available online: http://www.eucast.org (accessed on 6 June 2023).
| Characteristics | Overall n = 404 | W1 n = 99 | W2 n = 137 | W3 n = 102 | W4 n = 66 | p-Value |
|---|---|---|---|---|---|---|
| Age, median (IQR) | 63 (56, 70) | 61 (50, 69) | 65 (58, 72) | 64 (56, 72) | 64 (58, 69) | 0.018 |
| Female sex at birth, n (%) | 109 (27.0) | 22 (22.2) | 33 (24.1) | 31 (30.4) | 23 (34.8) | 0.222 |
| Italian, n (%) | 317 (78.5) | 83 (83.8) | 103 (75.2) | 73 (71.6) | 58 (87.9) | 0.031 |
| Comorbidities, n (%) | ||||||
| Obesity | 146 (36.1) | 26 (26.3) | 47 (34.3) | 45 (44.1) | 28 (42.4) | 0.040 |
| Pneumological comorbidities | 38 (9.4) | 5 (5.1) | 19 (13.9) | 7 (6.9) | 7 (10.6) | 0.098 |
| Cardiovascular comorbidities | 218 (54.0) | 49 (49.5) | 83 (60.6) | 49 (48.0) | 37 (56.1) | 0.189 |
| Metabolic diseases | 151 (37.4) | 31 (31.3) | 55 (40.1) | 35 (34.3) | 30 (45.5) | 0.235 |
| Diabetes | 73 (18.1) | 13 (13.1) | 25 (18.2) | 18 (17.6) | 17 (25.8) | 0.233 |
| Nephrological comorbidities | 28 (6.9) | 8 (8.1) | 10 (7.3) | 4 (3.9) | 6 (9.1) | 0.544 |
| Oncological comorbidities | 35 (8.7) | 6 (6.1) | 11 (8.0) | 11 (10.8) | 7 (10.6) | 0.612 |
| Immunological comorbidities | 27 (6.7) | 10 (10.1) | 7 (5.1) | 4 (3.9) | 6 (9.1) | 0.235 |
| Liver diseases | 5 (1.2) | 0 (0.0) | 3 (2.2) | 2 (2.0) | 0 (0.0) | 0.318 |
| Number of comorbidities, n (%) | ||||||
| 0 | 117 (29.0) | 30 (30.3) | 38 (27.7) | 33 (32.4) | 16 (24.2) | 0.228 |
| 1 | 132 (32.7) | 37 (37.4) | 35 (25.5) | 37 (36.3) | 23 (34.8) | |
| 2 | 107 (26.5) | 25 (25.3) | 43 (31.4) | 23 (22.5) | 16 (24.2) | |
| 3+ | 48 (11.9) | 7 (7.1) | 21 (15.3) | 9 (8.8) | 11 (16.7) | |
| SOFA score, median (IQR) | 8 (4, 10) | 9 (7, 12) | 9 (7, 10) | 7 (3, 8) | 5 (3, 7) | <0.001 |
| Treatments received, n (%) | ||||||
| Tocilizumab | 45 (11.1) | 38 (38.4) | 1 (0.7) | 6 (5.9) | 0 (0.0) | <0.001 |
| Remdesivir | 109 (27.0) | 49 (49.5) | 21 (15.3) | 23 (22.5) | 16 (24.2) | <0.001 |
| Heparin | 311 (77.0) | 42 (42.4) | 122 (89.1) | 91 (89.2) | 56 (84.8) | <0.001 |
| Steroids | 277 (68.6) | 19 (19.2) | 130 (94.9) | 75 (73.5) | 53 (80.3) | <0.001 |
| N° vaccine doses anti-SARS-CoV-2, n (%) W3 (n = 100) W4 (n = 66) | ||||||
| 0 | - | - | - | 87 (87.0) | 36 (54.5) | |
| 1 | - | - | - | 10 (10.0) | 7 (10.6) | |
| 2 | - | - | - | 3 (3.0) | 15 (22.7) | |
| 3 | - | - | - | 0 (0.0) | 8 (12.1) | |
| Days from symptoms to ICU access, median (IQR) | 11 (7, 14) | 11 (8, 15) | 10 (7, 13) | 11 (7, 14) | 10 (8, 13) | 0.136 |
| Days from hospitalization to ICU access, median (IQR) | 1 (0, 5) | 2 (0, 5) | 2 (0, 5) | 1 (0, 3) | 1 (0, 5) | 0.067 |
| Length of stay in ICU, median (IQR) | 11 (6, 22) | 12 (7, 17) | 11 (5, 22) | 11 (5, 22) | 11 (6, 24) | 0.976 |
| MV requirement, n(%) | 344 (85.1) | 87 (87.9) | 118 (86.1) | 87 (85.3) | 52 (78.8) | 0.423 |
| Length of MV (n =344), median (IQR) | 11 (6, 21) | 11 (7, 18) | 11 (6, 24) | 11 (5, 20) | 10 (6, 20) | 0.881 |
| Mortality, n (%) | 174 (43.1) | 53 (53.5) | 70 (51.1) | 30 (29.4) | 21 (31.8) | <0.001 |
| Overall n (%) | W1 n (%) | W2 n (%) | W3 n (%) | W4 n (%) | |
|---|---|---|---|---|---|
| 489 (100) | 94 (100) | 222 (100) | 112 (100) | 61 (100) | |
| Gram positive | 365 (74.6) | 74 (78.7) | 159 (71.6) | 88 (78.6) | 44 (72.1) |
| Enterocuccus spp. | 211 (43.1) | 54 (57.4) | 97 (43.7) | 40 (35.7) | 20 (32.7) |
| VRE | 24 (4.9) | 5 (5.3) | 14 (6.3) | 5 (4.5) | 0 (0) |
| Staphylococcus aureus | 40 (8.2) | 7 (7.4) | 17 (7.6) | 9 (8) | 7 (11.5) |
| MRSA | 15 (3.1) | 5 (5.3) | 6 (2.7) | 2 (1.8) | 2 (3.3) |
| CoNS | 136 (27.8) | 25 (26.6) | 46 (20.7) | 44 (39.2) | 21 (34.4) |
| Viridans group Streptococci | 10 (2) | 0 (0) | 4 (1.8) | 3 (2.7) | 3 (4.9) |
| Gram negative | 196 (40) | 29 (30.8) | 101 (45.5) | 41 (36.6) | 25 (40.9) |
| Enterobacterales | 108 (22) | 19 (20.2) | 52 (23.4) | 21 (18.7) | 16 (26.2) |
| ESBL+ | 23 (4.7) | 6 (6.3) | 4 (1.8) | 7 (6.2) | 6 (9.8) |
| CPE | 14 (2.9) | 10 (10.6) | 3 (1.3) | 1 (1) | 0 (0) |
| Enterobacter spp. | 47 (9.6) | 6 (6.4) | 31 (13.9) | 5 (4.5) | 5 (8.2) |
| Pseudomonas aeruginosa | 51 (10.4) | 3 (3.2) | 20 (9) | 17 (15.2) | 11 (18) |
| MDR | 14 (2.9) | 1 (1.1) | 7 (3.1) | 5 (4.5) | 1 (1.6) |
| Strenotrophomonas maltophilia | 2 (0.4) | 1 (1.1) | 1 (0.4) | 0 (0) | 0 (0) |
| Acinetobacter spp. | 6 (1.2) | 1 (1.1) | 2 (1) | 2 (1.8) | 1 (1.6) |
| Yeasts | 10 (2) | 3 (3.2) | 3 (1.3) | 1 (0.9) | 3 (4.9) |
| C. albicans | 7 (1.4) | 3 (3.2) | 3 (1.3) | 1 (0.9) | 0 (0) |
| C. glabrata | 1 (0.2) | 0 (0) | 0 (0) | 0 (0) | 1 (1.6) |
| C. tropicalis | 2 (0.4) | 0 (0) | 0 (0) | 1 (0.9) | 1 (1.6) |
| C. parapsilosis | 1 (0.2) | 0 (0) | 0 (0) | 0 (0) | 1 (1.6) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pozza, G.; Casalini, G.; Ciubotariu, C.L.; Giacomelli, A.; Galimberti, M.; Zacheo, M.; Rabbione, A.; Pieruzzi, M.; Oreni, L.; Galimberti, L.; et al. Bloodstream Infections in Intensive Care Unit during Four Consecutive SARS-CoV-2 Pandemic Waves. Antibiotics 2023, 12, 1448. https://doi.org/10.3390/antibiotics12091448
Pozza G, Casalini G, Ciubotariu CL, Giacomelli A, Galimberti M, Zacheo M, Rabbione A, Pieruzzi M, Oreni L, Galimberti L, et al. Bloodstream Infections in Intensive Care Unit during Four Consecutive SARS-CoV-2 Pandemic Waves. Antibiotics. 2023; 12(9):1448. https://doi.org/10.3390/antibiotics12091448
Chicago/Turabian StylePozza, Giacomo, Giacomo Casalini, Cosmin Lucian Ciubotariu, Andrea Giacomelli, Miriam Galimberti, Martina Zacheo, Andrea Rabbione, Margherita Pieruzzi, Letizia Oreni, Laura Galimberti, and et al. 2023. "Bloodstream Infections in Intensive Care Unit during Four Consecutive SARS-CoV-2 Pandemic Waves" Antibiotics 12, no. 9: 1448. https://doi.org/10.3390/antibiotics12091448
APA StylePozza, G., Casalini, G., Ciubotariu, C. L., Giacomelli, A., Galimberti, M., Zacheo, M., Rabbione, A., Pieruzzi, M., Oreni, L., Galimberti, L., Colombo, R., Rizzardini, G., Pagani, C., Rimoldi, S. G., Bonazzetti, C., Ridolfo, A. L., & Antinori, S. (2023). Bloodstream Infections in Intensive Care Unit during Four Consecutive SARS-CoV-2 Pandemic Waves. Antibiotics, 12(9), 1448. https://doi.org/10.3390/antibiotics12091448








