Managing Corneal Infections: Out with the old, in with the new?
Abstract
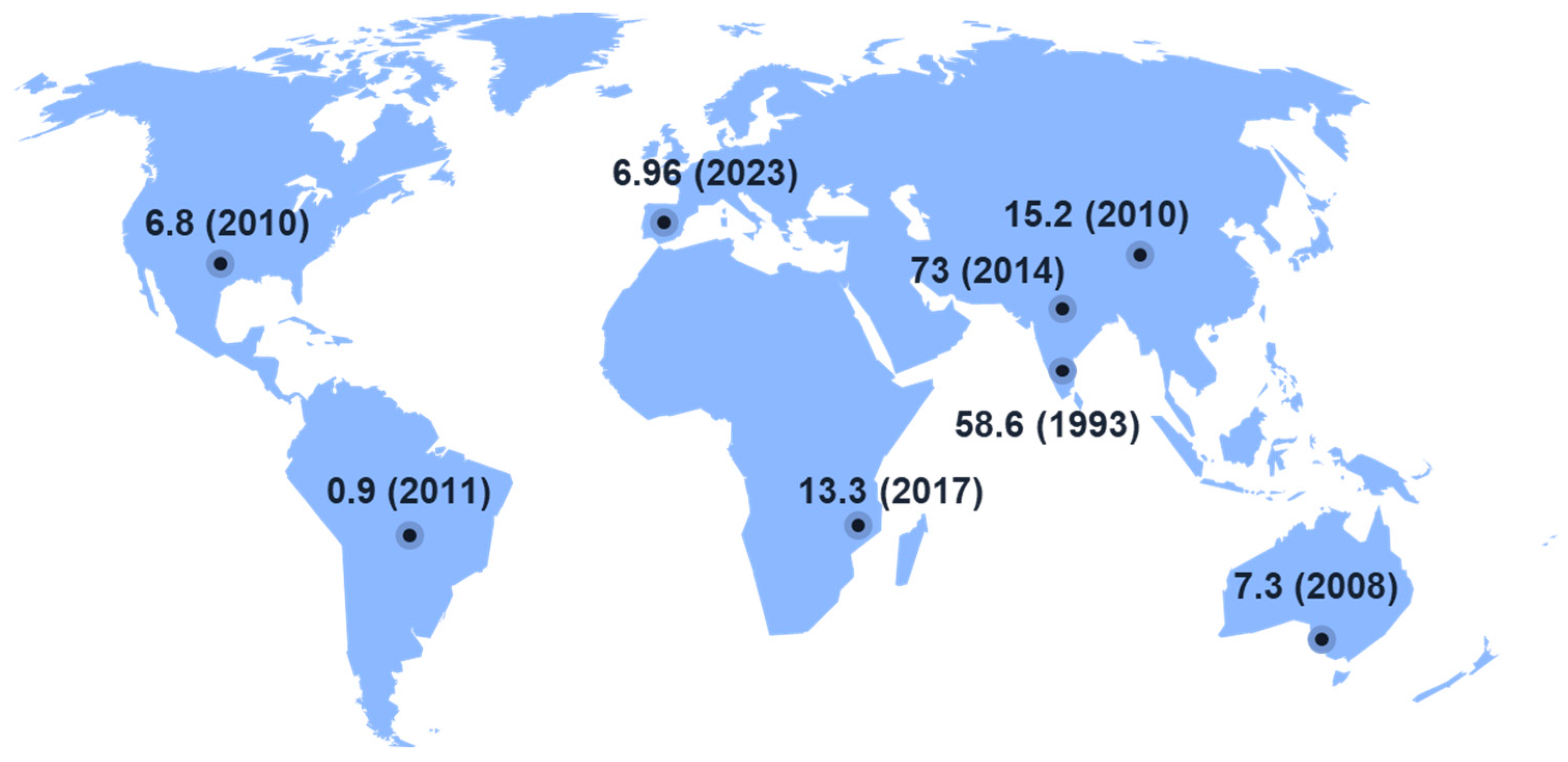
1. The Eye in Health and Disease
2. Ocular Infections and Therapeutic Challenges
3. Ocular Infections: Overcoming Therapeutic Challenges with Novel Treatments
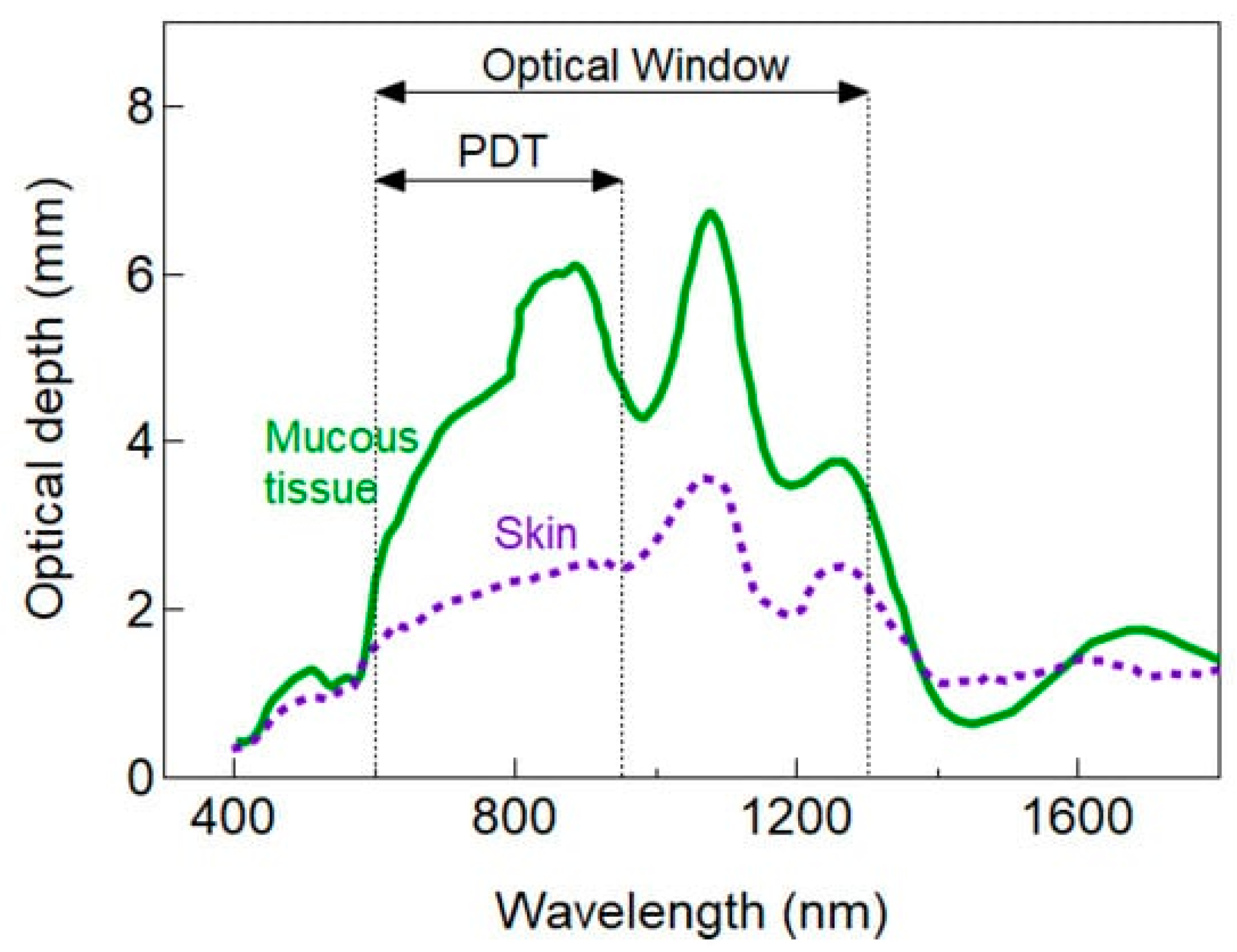
3.1. Light-Based Treatment Methods for Microbial Keratitis
3.1.1. Antimicrobial Photodynamic Therapy
3.1.2. Ultraviolet A plus Riboflavin
3.1.3. Red Light (660 nm) plus Methylene Blue
3.1.4. Red Light plus Toluidine Blue O
3.1.5. Red Light plus Chlorin e6
3.1.6. Green Light plus Rose Bengal
3.1.7. Ultraviolet C Light for the Treatment of Ocular Infection
3.1.8. Antimicrobial Blue Light for the Treatment of Microbial Keratitis
3.2. Phage Therapy as an Approach to Combat Microbial Keratitis
3.3. Probiotics to Eliminate Ocular Pathogens
4. Treatment of Ophthalmic Infections: Can We Shift the Paradigm?
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gipson, I. The ocular surface: The challenge to enable and protect vision: The Friedenwald lecture. Investig. Ophthalmol. Vis. Sci. 2007, 48, 4391–4398. [Google Scholar] [CrossRef] [PubMed]
- Morgan, P. Contemporary research in contact lens care. Contact Lens Anterior Eye 2013, 36, S22–S27. [Google Scholar] [CrossRef] [PubMed]
- Dong, Q.; Brulc, J.M.; Iovieno, A.; Bates, B.; Garoutte, A.; Miller, D.; Revanna, K.V.; Gao, X.; Antonopoulos, D.A.; Slepak, V.Z. Diversity of bacteria at healthy human conjunctiva. Investig. Ophthalmol. Vis. Sci. 2011, 52, 5408–5413. [Google Scholar] [CrossRef]
- Gregory, M.S. Innate Immune System and the Eye; Elsevier Ltd.: Amsterdam, The Netherlands, 2010; pp. 439–445. [Google Scholar]
- Narayanan, S.; Redfern, R.; Miller, W.; Nichols, K.; McDermott, A. Dry Eye Disease and Microbial Keratitis: Is There a Connection? Ocul. Surf. 2013, 11, 75–92. [Google Scholar] [CrossRef] [PubMed]
- Angus, A.A.; Lee, A.A.; Augustin, D.K.; Lee, E.J.; Evans, D.J.; Fleiszig, S.M.J. Pseudomonas aeruginosa Induces Membrane Blebs in Epithelial Cells, Which Are Utilized as a Niche for Intracellular Replication and Motility. Infect. Immun. 2008, 76, 1992. [Google Scholar] [CrossRef] [PubMed]
- Karsten, E.; Watson, S.L.; Foster, L.J.R. Diversity of microbial species implicated in keratitis: A review. Open Ophthalmol. J. 2012, 6, 110. [Google Scholar] [CrossRef]
- Marasini, S.; Swift, S.; Dean, S.; Ormonde, S.; Craig, J. Spectrum and sensitivity of bacterial keratitis isolates in Auckland. J. Ophthalmol. 2016, 2016, 3769341. [Google Scholar] [CrossRef]
- Sthapit, P.; Tuladhar, N.; Marasini, S.; Khoju, U.; Thapa, G. Bacterial conjunctivitis and use of antibiotics in Dhulikhel Hospital-Kathmandu University Hospital. Kathmandu Univ. Med. J. 2011, 9, 69–72. [Google Scholar] [CrossRef]
- Falavarjani, K.G.; Nekoozadeh, S.; Modarres, M.; Parvaresh, M.M.; Hashemi, M.; Soodi, R.; Alemzadeh, S.A. Isolates and antibiotic resistance of culture-proven endophthalmitis cases presented to a referral center in Tehran. Middle East Afr. J. Ophthalmol. 2012, 19, 361. [Google Scholar] [CrossRef]
- Seal, D.V.; Kirkness, C.M.; Bennett, H.G.B.; Peterson, M.; Barr, D.; Browne, B.; Chawla, J.; Doig, W.; Dutton, G.; Dudgeon, J.; et al. Population-based cohort study of microbial keratitis in Scotland: Incidence and features. Contact Lens Anterior Eye 1999, 22, 49–57. [Google Scholar] [CrossRef]
- Green, M.; Apel, A.; Stapleton, F. Risk factors and causative organisms in microbial keratitis. Cornea 2008, 27, 22–27. [Google Scholar] [CrossRef]
- Ting, D.S.J.; Ho, C.S.; Cairns, J.; Elsahn, A.; Al-Aqaba, M.; Boswell, T.; Said, D.G.; Dua, H.S. 12-year analysis of incidence, microbiological profiles and in vitro antimicrobial susceptibility of infectious keratitis: The Nottingham Infectious Keratitis Study. Br. J. Ophthalmol. 2021, 105, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Gonzales, C.A.; Srinivasan, M.; Whitcher, J.P.; Smolin, G. Incidence of corneal ulceration in Madurai district, South India. Ophthalmic Epidemiol. 1996, 3, 159–166. [Google Scholar] [CrossRef]
- Upadhyay, M.; Karmacharya, P.; Koirala, S.; Shah, D.; Shakya, S.; Shrestha, J.; Bajracharya, H.; Gurung, C.; Whitcher, J. The Bhaktapur eye study: Ocular trauma and antibiotic prophylaxis for the prevention of corneal ulceration in Nepal. Br. J. Ophthalmol. 2001, 85, 388–392. [Google Scholar] [CrossRef] [PubMed]
- Joseph, J.; Sridhar, M.S.; Murthy, S.; Sharma, S. Clinical and microbiological profile of microsporidial keratoconjunctivitis in southern India. Ophthalmology 2006, 113, 531–537. [Google Scholar] [CrossRef] [PubMed]
- Key, J.E. Development of contact lenses and their worldwide use. Eye Contact Lens 2007, 33, 343–345. [Google Scholar] [CrossRef]
- Marasini, S.; Wang, M.T.; Swift, S.; Dean, S.J.; Ormonde, S.E.; Gamble, G.D.; Craig, J.P. Clinical and microbiological profile of Pseudomonas aeruginosa keratitis admitted to a New Zealand tertiary centre. Clin. Exp. Ophthalmol. 2018, 46, 441–444. [Google Scholar] [CrossRef]
- Stapleton, F.; Bakkar, M.; Carnt, N.; Chalmers, R.; Vijay, A.K.; Marasini, S.; Ng, A.; Tan, J.; Wagner, H.; Woods, C. BCLA CLEAR-Contact lens complications. Contact Lens Anterior Eye 2021, 44, 330–367. [Google Scholar] [CrossRef]
- Bourcier, T.; Thomas, F.; Borderie, V.; Chaumeil, C.; Laroche, L. Bacterial keratitis: Predisposing factors, clinical and microbiological review of 300 cases. Br. J. Ophthalmol. 2003, 87, 834. [Google Scholar] [CrossRef]
- Asbell, P.; Stenson, S. Ulcerative keratitis. Survey of 30 years’ laboratory experience. Arch. Ophthalmol.-Chic. 1982, 100, 77–80. [Google Scholar] [CrossRef] [PubMed]
- Mcclellan, K.A.; Bernard, P.J.; Billson, F.A. Microbial Investigations in Keratitis at the Sydney-Eye-Hospital. Aust. N. Z. J. Ophthalmol. 1989, 17, 413–416. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Liang, Y.; Deng, S.; Wang, Z.; Li, R.; Sun, X. Distribution of bacterial keratitis and emerging resistance to antibiotics in China from 2001 to 2004. Clin. Ophthalmol. 2008, 2, 575–579. [Google Scholar] [PubMed]
- Tuft, S.J.; Matheson, M. In vitro antibiotic resistance in bacterial keratitis in London. Br. J. Ophthalmol. 2000, 84, 687–691. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Dawson, C.R.; Togni, B. Herpes simplex eye infections: Clinical manifestations, pathogenesis and management. Surv. Ophthalmol. 1976, 21, 121–135. [Google Scholar] [CrossRef]
- Choong, K.; Walker, N.J.; Apel, A.J.; Whitby, M. Aciclovir-resistant herpes keratitis. Clin. Exp. Ophthalmol. 2010, 38, 309–313. [Google Scholar] [CrossRef]
- Farooq, A.V.; Shukla, D. Herpes simplex epithelial and stromal keratitis: An epidemiologic update. Surv. Ophthalmol. 2012, 57, 448–462. [Google Scholar] [CrossRef]
- Morfin, F.; Thouvenot, D. Herpes simplex virus resistance to antiviral drugs. J. Clin. Virol. 2003, 26, 29–37. [Google Scholar] [CrossRef]
- Moshirfar, M.; Kelkar, N.; Peterson, T.; Bradshaw, J.; Parker, L.; Ronquillo, Y.C.; Hoopes, P.C. The Impact of Antiviral Resistance on Herpetic Keratitis. Eye Contact Lens 2022, 49, 127–134. [Google Scholar] [CrossRef]
- Al-Badriyeh, D.; Neoh, C.F.; Stewart, K.; Kong, D.C.M. Clinical utility of voriconazole eye drops in ophthalmic fungal keratitis. Clin. Ophthalmol. 2010, 4, 391–405. [Google Scholar]
- Tu, E.Y.; McCartney, D.L.; Beatty, R.F.; Springer, K.L.; Levy, J.; Edward, D. Successful treatment of resistant ocular fusariosis with posaconazole (SCH-56592). Am. J. Ophthalmol. 2007, 143, 222–227.e221. [Google Scholar] [CrossRef]
- Altun, A.; Kurna, S.; Sengor, T.; Altun, G.; Olcaysu, O.; Aki, S.; Simsek, M. Effectiveness of posaconazole in recalcitrant fungal keratitis resistant to conventional antifungal drugs. Case Rep. Ophthalmol. Med. 2014, 2014, 701653. [Google Scholar] [CrossRef]
- Dart, J.K.; Saw, V.P.; Kilvington, S. Acanthamoeba keratitis: Diagnosis and treatment update 2009. Am. J. Ophthalmol. 2009, 148, 487–499.e2. [Google Scholar] [CrossRef] [PubMed]
- Iovieno, A.; Oechsler, R.A.; Ledee, D.R.; Miller, D.; Alfonso, E.C. Drug-resistant severe Acanthamoeba keratitis caused by rare T5 Acanthamoeba genotype. Eye Contact Lens 2010, 36, 183–184. [Google Scholar] [CrossRef]
- Green, M.; Apel, A.; Stapleton, F. A Longitudinal Study of Trends in Keratitis in Australia. Cornea 2008, 27, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Saeed, A.; Arcy, F.; Stack, J.; Collum, L.M.; Power, W.; Beatty, S. Risk Factors, Microbiological Findings, and Clinical Outcomes in Cases of Microbial Keratitis Admitted to a Tertiary Referral Center in Ireland. Cornea 2009, 28, 285–292. [Google Scholar] [CrossRef]
- Burton, M.J.; Pithuwa, J.; Okello, E.; Afwamba, I.; Onyango, J.J.; Oates, F.; Chevallier, C.; Hall, A.B. Microbial keratitis in East Africa: Why are the outcomes so poor? Ophthalmic Epidemiol. 2011, 18, 158–163. [Google Scholar] [CrossRef]
- Keay, L.; Edwards, K.; Naduvilath, T.; Taylor, H.R.; Snibson, G.R.; Forde, K.; Stapleton, F. Microbial keratitis: Predisposing factors and morbidity. Ophthalmology 2006, 113, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Por, Y.M.; Mehta, J.S.; Chua, J.L.; Koh, T.-H.; Khor, W.B.; Fong, A.C.; Lim, J.W.; Heng, W.J.; Loh, R.S.; Lim, L. Acanthamoeba keratitis associated with contact lens wear in Singapore. Am. J. Ophthalmol. 2009, 148, 7–12.e12. [Google Scholar] [CrossRef]
- Mills, R. View 1: Corneal scraping and combination antibiotic therapy is indicated. Br. J. Ophthalmol. 2003, 87, 1167–1169. [Google Scholar] [CrossRef]
- Morlet, N.; Daniell, M. View 2: Empirical fluoroquinolone therapy is sufficient initial treatment. Br. J. Ophthalmol. 2003, 87, 1169–1172. [Google Scholar] [CrossRef]
- Davis, B.D. Mechanism of bactericidal action of aminoglycosides. Microbiol. Rev. 1987, 51, 341. [Google Scholar] [CrossRef]
- Barriere, S.; Flaherty, J. Third-generation cephalosporins: A critical evaluation. Clin. Pharm. 1983, 3, 351–373. [Google Scholar] [CrossRef]
- Pestova, E.; Millichap, J.J.; Noskin, G.A.; Peterson, L.R. Intracellular targets of moxifloxacin: A comparison with other fluoroquinolones. J. Antimicrob. Chemother. 2000, 45, 583–590. [Google Scholar] [CrossRef]
- Wong, T.; Ormonde, S.; Gamble, G.; McGhee, C. Severe infective keratitis leading to hospital admission in New Zealand. Br. J. Ophthalmol. 2003, 87, 1103–1108. [Google Scholar] [CrossRef] [PubMed]
- McAllum, P.J.; McGhee, C.N. Prescribing trends in infectious keratitis: A survey of New Zealand ophthalmologists. Clin. Exp. Ophthalmol. 2003, 31, 496–504. [Google Scholar] [CrossRef] [PubMed]
- Austin, A.; Schallhorn, J.; Geske, M.; Mannis, M.; Lietman, T.; Rose-Nussbaumer, J. Empirical treatment of bacterial keratitis: An international survey of corneal specialists. BMJ Open Ophthalmol. 2017, 2, e000047. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.K.; Melton, R.; Asbell, P.A. Antibiotic resistance among ocular pathogens: Current trends from the ARMOR surveillance study (2009–2016). Clin. Optom. 2019, 11, 15–26. [Google Scholar] [CrossRef]
- Chalita, M.R.; Höfling-Lima, A.L.; Paranhos, A.; Schor, P.; Belfort, R. Shifting trends in in vitro antibiotic susceptibilities for common ocular isolates during a period of 15 years. Am. J. Ophthalmol. 2004, 137, 43–51. [Google Scholar] [CrossRef]
- Fong, C.-F.; Hu, F.-R.; Tseng, C.-H.; Wang, I.J.; Chen, W.-L.; Hou, Y.-C. Antibiotic Susceptibility of Bacterial Isolates from Bacterial Keratitis Cases in a University Hospital in Taiwan. Am. J. Ophthalmol. 2007, 144, 682–689.e1. [Google Scholar] [CrossRef]
- Sand, D.; She, R.; Shulman, I.A.; Chen, D.S.; Schur, M.; Hsu, H.Y. Microbial Keratitis in Los Angeles: The Doheny Eye Institute and the Los Angeles County Hospital Experience: The Doheny Eye Institute and the Los Angeles County Hospital Experience. Ophthalmology 2015, 122, 918–924. [Google Scholar] [CrossRef]
- Yeh, D.L.; Stinnett, S.S.; Afshari, N.A. Analysis of bacterial cultures in infectious keratitis, 1997 to 2004. Am. J. Ophthalmol. 2006, 142, 1066. [Google Scholar] [CrossRef]
- Goldstein, M.H.; Kowalski, R.P.; Gordon, Y.J. Emerging fluoroquinolone resistance in bacterial keratitis: A 5-year review. Ophthalmology 1999, 106, 1313. [Google Scholar] [CrossRef] [PubMed]
- Kunimoto, D.Y.; Sharma, S.; Garg, P.; Rao, G.N. In vitro susceptibility of bacterial keratitis pathogens to ciprofloxacin: Emerging resistance. Ophthalmology 1999, 106, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Alexandrakis, G.; Alfonso, E.C.; Miller, D. Shifting trends in bacterial keratitis in South Florida and emerging resistance to fluoroquinolones. Ophthalmology 2000, 107, 1497–1502. [Google Scholar] [CrossRef] [PubMed]
- Pandita, A.; Murphy, C. Microbial keratitis in Waikato, New Zealand. Clin. Exp. Ophthalmol. 2011, 39, 393–397. [Google Scholar] [CrossRef] [PubMed]
- Orlans, H.; Hornby, S.; Bowler, I. In vitro antibiotic susceptibility patterns of bacterial keratitis isolates in Oxford, UK: A 10-year review. Eye 2011, 25, 489–493. [Google Scholar] [CrossRef]
- Constantinou, M.; Daniell, M.; Snibson, G.R.; Vu, H.T.; Taylor, H.R. Clinical efficacy of moxifloxacin in the treatment of bacterial keratitis: A randomized clinical trial. Ophthalmology 2007, 114, 1622–1629. [Google Scholar] [CrossRef]
- Parmar, P.; Salman, A.; Kalavathy, C.M.; Kaliamurthy, J.; Prasanth, D.A.; Thomas, P.A.; Jesudasan, C.A.N. Comparison of topical gatifloxacin 0.3% and ciprofloxacin 0.3% for the treatment of bacterial keratitis. Am. J. Ophthalmol. 2006, 141, 282–286.e281. [Google Scholar] [CrossRef]
- Conly, J.; Johnston, B. Where are all the new antibiotics? The new antibiotic paradox. Can. J. Infect. Dis. Med. Microbiol. 2005, 16, 159–160. [Google Scholar] [CrossRef] [PubMed]
- Ling, L.L.; Schneider, T.; Peoples, A.J.; Spoering, A.L.; Engels, I.; Conlon, B.P.; Mueller, A.; Schäberle, T.F.; Hughes, D.E.; Epstein, S. A new antibiotic kills pathogens without detectable resistance. Nature 2015, 517, 455–459. [Google Scholar] [CrossRef]
- Marasini, S.; Leanse, L.G.; Dai, T. Can microorganisms develop resistance against light based anti-infective agents? Adv. Drug Deliv. Rev. 2021, 175, 113822. [Google Scholar] [CrossRef] [PubMed]
- Dutescu, I.A.; Hillier, S.A. Encouraging the development of new antibiotics: Are financial incentives the right way forward? A systematic review and case study. Infect. Drug Resist. 2021, 14, 415–434. [Google Scholar] [CrossRef] [PubMed]
- Hutchings, M.I.; Truman, A.W.; Wilkinson, B. Antibiotics: Past, present and future. Curr. Opin. Microbiol. 2019, 51, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Sun, D.; Gao, W.; Hu, H.; Zhou, S. Why 90% of clinical drug development fails and how to improve it? Acta Pharm. Sin. B 2022, 12, 3049–3062. [Google Scholar] [CrossRef] [PubMed]
- Elbasha, E.H. Deadweight loss of bacterial resistance due to overtreatment. Health Econ. 2003, 12, 125–138. [Google Scholar] [CrossRef]
- Manente, R.; Santella, B.; Pagliano, P.; Santoro, E.; Casolaro, V.; Borrelli, A.; Capunzo, M.; Galdiero, M.; Franci, G.; Boccia, G. Prevalence and Antimicrobial Resistance of Causative Agents to Ocular Infections. Antibiotics 2022, 11, 463. [Google Scholar] [CrossRef]
- Chiang, M.-C.; Chern, E. More than Antibiotics: Latest Therapeutics in the Treatment and Prevention of Ocular Surface Infections. J. Clin. Med. 2022, 11, 4195. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Outbreak of Extensively Drug-Resistant Pseudomonas aeruginosa Associated with Artificial Tears. 2023. Available online: https://www.cdc.gov/hai/outbreaks/crpa-artificial-tears.html (accessed on 14 July 2023).
- Møller, K.I.; Kongshoj, B.; Philipsen, P.A.; Thomsen, V.O.; Wulf, H.C. How Finsen’s light cured lupus vulgaris. Photodermatol. Photoimmunol. Photomed. 2005, 21, 118–124. [Google Scholar] [CrossRef]
- Foote, C.S. Definition of type I and type II photosensitized oxidation. Photochem. Photobiol. 1991, 54, 659. [Google Scholar] [CrossRef]
- Redmond, R.W.; Kochevar, I.E. Spatially resolved cellular responses to singlet oxygen. Photochem. Photobiol. 2006, 82, 1178–1186. [Google Scholar] [CrossRef]
- Dai, T.; Huang, Y.-Y.; Hamblin, M.R. Photodynamic therapy for localized infections—State of the art. Photodiagnosis Photodyn. Ther. 2009, 6, 170–188. [Google Scholar] [CrossRef] [PubMed]
- Calixto, G.M.F.; Bernegossi, J.; De Freitas, L.M.; Fontana, C.R.; Chorilli, M. Nanotechnology-based drug delivery systems for photodynamic therapy of cancer: A review. Molecules 2016, 21, 342. [Google Scholar] [CrossRef] [PubMed]
- Algorri, J.F.; Ochoa, M.; Roldán-Varona, P.; Rodríguez-Cobo, L.; López-Higuera, J.M. Light technology for efficient and effective photodynamic therapy: A critical review. Cancers 2021, 13, 3484. [Google Scholar] [CrossRef] [PubMed]
- Marasini, S.; Zhang, A.C.; Dean, S.J.; Swift, S.; Craig, J.P. Safety and efficacy of UV application for superficial infections in humans: A systematic review and meta-analysis. Ocul. Surf. 2021, 21, 331–344. [Google Scholar] [CrossRef]
- Wollensak, G.; Wilsch, M.; Spoerl, E.; Seiler, T. Collagen fiber diameter in the rabbit cornea after collagen crosslinking by riboflavin/UVA. Cornea 2004, 23, 503–507. [Google Scholar] [CrossRef]
- Richoz, O.; Kling, S.; Hoogewoud, F.; Hammer, A.; Tabibian, D.; Francois, P.; Schrenzel, J.; Hafezi, F. Antibacterial efficacy of accelerated photoactivated chromophore for keratitis–corneal collagen cross-linking (PACK-CXL). J. Refract. Surg. 2014, 30, 850–854. [Google Scholar] [CrossRef] [PubMed]
- Ludema, C.; Cole, S.R.; Poole, C.; Smith, J.S.; Schoenbach, V.J.; Wilhelmus, K.R. Association between unprotected ultraviolet radiation exposure and recurrence of ocular herpes simplex virus. Am. J. Epidemiol. 2014, 179, 208–215. [Google Scholar] [CrossRef]
- Songsantiphap, C.; Vanichanan, J.; Chatsuwan, T.; Asawanonda, P.; Boontaveeyuwat, E. Methylene Blue–Mediated Antimicrobial Photodynamic Therapy Against Clinical Isolates of Extensively Drug Resistant Gram-Negative Bacteria Causing Nosocomial Infections in Thailand, An In Vitro Study. Front. Cell. Infect. Microbiol. 2022, 12, 929242. [Google Scholar] [CrossRef]
- Langford, M.P.; Sebren, A.R.; Burch, M.A.; Redens, T.B. Methylene Blue Inhibits Acute Hemorrhagic Conjunctivitis Virus Production and Induction of Caspase-3 Mediated Human Corneal Cell Cytopathy. Clin. Ophthalmol. 2020, 14, 4483–4492. [Google Scholar] [CrossRef]
- Shih, M.-H.; Huang, F.-C. Effects of photodynamic therapy on rapidly growing nontuberculous mycobacteria keratitis. Investig. Ophthalmol. Vis. Sci. 2011, 52, 223–229. [Google Scholar] [CrossRef]
- Li, Y.; Du, J.; Huang, S.; Wang, S.; Wang, Y.; Lei, L.; Zhang, C.; Huang, X. Antimicrobial Photodynamic Effect of Cross-Kingdom Microorganisms with Toluidine Blue O and Potassium Iodide. Int. J. Mol. Sci. 2022, 23, 11373. [Google Scholar] [CrossRef] [PubMed]
- Biberoglu, K.; Yuksel, M.; Onder, S.; Tacal, O. Effects of toluidine blue O and methylene blue on growth and viability of pancreatic cancer cells. Drug Dev. Res. 2022, 83, 900–909. [Google Scholar] [CrossRef] [PubMed]
- Vahabi, S.; Fekrazad, R.; Ayremlou, S.; Taheri, S.; Zangeneh, N. The effect of antimicrobial photodynamic therapy with radachlorin and toluidine blue on streptococcus mutans: An in vitro study. J. Dent. 2011, 8, 48. [Google Scholar]
- Shen, J.; Liang, Q.; Su, G.; Zhang, Y.; Wang, Z.; Baudouin, C.; Labbé, A. In vitro effect of toluidine blue antimicrobial photodynamic chemotherapy on staphylococcus epidermidis and staphylococcus aureus isolated from ocular surface infection. Transl. Vis. Sci. Technol. 2019, 8, 45. [Google Scholar] [CrossRef]
- Luke-Marshall, N.R.; Hansen, L.A.; Shafirstein, G.; Campagnari, A.A. Antimicrobial photodynamic therapy with chlorin e6 is bactericidal against biofilms of the primary human otopathogens. Msphere 2020, 5, 10–128. [Google Scholar] [CrossRef]
- de Carvalho, G.G.; Mateo, R.P.; e Silva, R.C.; Huacho, P.M.M.; de Souza Rastelli, A.N.; de Oliveira, K.T.; Marcantonio, R.A.C.; Zandim-Barcelos, D.L.; Spolidorio, D.M.P. Chlorin-based photosensitizer under blue or red-light irradiation against multi-species biofilms related to periodontitis. Photodiagnosis Photodyn. Ther. 2023, 41, 103219. [Google Scholar] [CrossRef]
- Winkler, K.; Simon, C.; Finke, M.; Bleses, K.; Birke, M.; Szentmáry, N.; Hüttenberger, D.; Eppig, T.; Stachon, T.; Langenbucher, A. Photodynamic inactivation of multidrug-resistant Staphylococcus aureus by chlorin e6 and red light (λ = 670 nm). J. Photochem. Photobiol. B Biol. 2016, 162, 340–347. [Google Scholar] [CrossRef]
- Wu, M.-F.; Deichelbohrer, M.; Tschernig, T.; Laschke, M.W.; Szentmáry, N.; Hüttenberger, D.; Foth, H.-J.; Seitz, B.; Bischoff, M. Chlorin e6 mediated photodynamic inactivation for multidrug resistant Pseudomonas aeruginosa keratitis in mice in vivo. Sci. Rep. 2017, 7, 44537. [Google Scholar] [CrossRef]
- Leanse, L.G.; Goh, X.S.; Cheng, J.-X.; Hooper, D.C.; Dai, T. Dual-wavelength photo-killing of methicillin-resistant Staphylococcus aureus. JCI Insight 2020, 5, 11. [Google Scholar] [CrossRef]
- Vera, C.; Gallucci, M.N.; Marioni, J.; Sosa Morales, M.C.; Martino, D.M.; Nunez Montoya, S.; Borsarelli, C.D. “On-Demand” Antimicrobial Photodynamic Activity through Supramolecular Photosensitizers Built with Rose Bengal and (p-Vinylbenzyl) triethylammomium Polycation Derivatives. Bioconjugate Chem. 2022, 33, 463–472. [Google Scholar] [CrossRef]
- Kurosu, M.; Mitachi, K.; Yang, J.; Pershing, E.V.; Horowitz, B.D.; Wachter, E.A.; Lacey, J.W., III; Ji, Y.; Rodrigues, D.J. Antibacterial activity of pharmaceutical-grade rose bengal: An application of a synthetic dye in antibacterial therapies. Molecules 2022, 27, 322. [Google Scholar] [CrossRef]
- Hung, J.-H.; Wang, Z.-X.; Lo, Y.-H.; Lee, C.-N.; Chang, Y.; Chang, R.Y.; Huang, C.-C.; Wong, T.-W. Rose Bengal-mediated photodynamic therapy to inhibit Candida albicans. JoVE J. Vis. Exp. 2022, 181, e63558. [Google Scholar]
- Wang, D.; Pan, H.; Yan, Y.; Zhang, F. Rose bengal-mediated photodynamic inactivation against periodontopathogens in vitro. Photodiagnosis Photodyn. Ther. 2021, 34, 102250. [Google Scholar] [CrossRef]
- Durkee, H.; Arboleda, A.; Aguilar, M.C.; Martinez, J.D.; Alawa, K.A.; Relhan, N.; Maestre-Mesa, J.; Amescua, G.; Miller, D.; Parel, J.-M. Rose bengal photodynamic antimicrobial therapy to inhibit Pseudomonas aeruginosa keratitis isolates. Lasers Med. Sci. 2020, 35, 861–866. [Google Scholar] [CrossRef]
- Adre, E.; Durkee, H.; Arboleda, A.; Alawa, K.; Maestre, J.; Mintz, K.J.; Leblanc, R.M.; Amescua, G.; Parel, J.M.; Miller, D. Rose Bengal and Riboflavin mediated photodynamic antimicrobial therapy against selected South Florida Nocardia keratitis isolates. Transl. Vis. Sci. Technol. 2022, 11, 29. [Google Scholar] [CrossRef]
- Halili, F.; Arboleda, A.; Durkee, H.; Taneja, M.; Miller, D.; Alawa, K.A.; Aguilar, M.C.; Amescua, G.; Flynn, H.W., Jr.; Parel, J.-M. Rose bengal–and riboflavin-mediated photodynamic therapy to inhibit methicillin-resistant Staphylococcus aureus keratitis isolates. Am. J. Ophthalmol. 2016, 166, 194–202. [Google Scholar] [CrossRef] [PubMed]
- Sepulveda-Beltran, P.A.; Levine, H.; Altamirano, D.S.; Martinez, J.D.; Durkee, H.; Mintz, K.; Leblanc, R.; Tóthová, J.D.A.; Miller, D.; Parel, J.-M. Rose Bengal Photodynamic Antimicrobial Therapy: A review of the intermediate term clinical and surgical outcomes. Am. J. Ophthalmol. 2022, 243, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Naranjo, A.; Arboleda, A.; Martinez, J.D.; Durkee, H.; Aguilar, M.C.; Relhan, N.; Nikpoor, N.; Galor, A.; Dubovy, S.R.; Leblanc, R. Rose Bengal photodynamic antimicrobial therapy for patients with progressive infectious keratitis: A pilot clinical study. Am. J. Ophthalmol. 2019, 208, 387–396. [Google Scholar] [CrossRef]
- Dai, T.; Garcia, B.; Murray, C.K.; Vrahas, M.S.; Hamblin, M.R. UVC light prophylaxis for cutaneous wound infections in mice. Antimicrob. Agents Chemother. 2012, 56, 3841–3848. [Google Scholar] [CrossRef]
- Dai, T.; Murray, C.K.; Vrahas, M.S.; Baer, D.G.; Tegos, G.P.; Hamblin, M.R. Ultraviolet C light for Acinetobacter baumannii wound infections in mice: Potential use for battlefield wound decontamination? J. Trauma Acute Care Surg. 2012, 73, 661. [Google Scholar] [CrossRef] [PubMed]
- Marasini, S.; Dean, S.J.; Swift, S.; Perera, J.; Rupenthal, I.D.; Wang, T.; Read, H.; Craig, J.P. Preclinical confirmation of UVC efficacy in treating infectious keratitis. Ocul. Surf. 2022, 25, 76–86. [Google Scholar] [CrossRef] [PubMed]
- Marasini, S.; Mugisho, O.O.; Swift, S.; Read, H.; Rupenthal, I.D.; Dean, S.J.; Craig, J.P. Effect of therapeutic UVC on corneal DNA: Safety assessment for potential keratitis treatment. Ocul. Surf. 2021, 20, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Chang, Q.; Ferrer-Espada, R.; Leanse, L.G.; Goh, X.S.; Wang, X.; Gelfand, J.A.; Dai, T. Photoinactivation of Moraxella catarrhalis using 405-nm blue light: Implications for the treatment of otitis media. Photochem. Photobiol. 2020, 96, 611–617. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Kochevar, I.E.; Behlau, I.; Zhao, J.; Wang, F.; Wang, Y.; Sun, X.; Hamblin, M.R.; Dai, T. Antimicrobial blue light therapy for infectious keratitis: Ex vivo and in vivo studies. Investig. Ophthalmol. Vis. Sci. 2017, 58, 586–593. [Google Scholar] [CrossRef]
- Leanse, L.G.; Goh, X.S.; Dai, T. Quinine improves the fungicidal effects of antimicrobial blue light: Implications for the treatment of cutaneous candidiasis. Lasers Surg. Med. 2020, 52, 569–575. [Google Scholar] [CrossRef]
- Leanse, L.G.; Zeng, X.; Dai, T. Potentiated antimicrobial blue light killing of methicillin resistant Staphylococcus aureus by pyocyanin. J. Photochem. Photobiol. B Biol. 2021, 215, 112109. [Google Scholar] [CrossRef]
- Hatfull, G.F.; Dedrick, R.M.; Schooley, R.T. Phage therapy for antibiotic-resistant bacterial infections. Annu. Rev. Med. 2022, 73, 197–211. [Google Scholar] [CrossRef]
- Gibb, B.; Hyman, P.; Schneider, C.L. The many applications of engineered bacteriophages—An overview. Pharmaceuticals 2021, 14, 634. [Google Scholar] [CrossRef]
- Luong, T.; Salabarria, A.-C.; Roach, D.R. Phage therapy in the resistance era: Where do we stand and where are we going? Clin. Ther. 2020, 42, 1659–1680. [Google Scholar] [CrossRef]
- Furusawa, T.; Iwano, H.; Hiyashimizu, Y.; Matsubara, K.; Higuchi, H.; Nagahata, H.; Niwa, H.; Katayama, Y.; Kinoshita, Y.; Hagiwara, K. Phage therapy is effective in a mouse model of bacterial equine keratitis. Appl. Environ. Microbiol. 2016, 82, 5332–5339. [Google Scholar] [CrossRef]
- Fukuda, K.; Ishida, W.; Uchiyama, J.; Rashel, M.; Kato, S.-I.; Morita, T.; Muraoka, A.; Sumi, T.; Matsuzaki, S.; Daibata, M. Pseudomonas aeruginosa keratitis in mice: Effects of topical bacteriophage KPP12 administration. PLoS ONE 2012, 7, e47742. [Google Scholar] [CrossRef]
- Fadlallah, A.; Chelala, E.; Legeais, J.-M. Corneal infection therapy with topical bacteriophage administration. Open Ophthalmol. J. 2015, 9, 167. [Google Scholar] [CrossRef]
- Berg, G.; Rybakova, D.; Fischer, D.; Cernava, T.; Vergès, M.-C.C.; Charles, T.; Chen, X.; Cocolin, L.; Eversole, K.; Corral, G.H. Microbiome definition re-visited: Old concepts and new challenges. Microbiome 2020, 8, 103. [Google Scholar] [CrossRef]
- Chiang, M.-C.; Chern, E. Ocular surface microbiota: Ophthalmic infectious disease and probiotics. Front. Microbiol. 2022, 13, 952473. [Google Scholar] [CrossRef]
- Akova, B.; Kıvanç, S.; Kıvanç, M. Antibiofilm effect of probiotic lactic acid bacteria against Bacillus spp. obtained from the ocular surface. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 7799–7805. [Google Scholar]
- Mohamed, S.; Elmohamady, M.N.; Abdelrahman, S.; Amer, M.M.; Abdelhamid, A.G. Antibacterial effects of antibiotics and cell-free preparations of probiotics against Staphylococcus aureus and Staphylococcus epidermidis associated with conjunctivitis. Saudi Pharm. J. 2020, 28, 1558–1565. [Google Scholar] [CrossRef]
- Ruíz, F.O.; Pascual, L.; Giordano, W.; Barberis, L. Bacteriocins and other bioactive substances of probiotic lactobacilli as biological weapons against Neisseria gonorrhoeae. Pathog. Dis. 2015, 73, ftv013. [Google Scholar] [CrossRef]
- Mallika, P.; Asok, T.; Faisal, H.; Aziz, S.; Tan, A.; Intan, G. Neonatal conjunctivitis–A review. Malays. Fam. Physician Off. J. Acad. Fam. Physicians Malays. 2008, 3, 77. [Google Scholar]
- Sridhar, M.S. Anatomy of cornea and ocular surface. Indian J. Ophthalmol. 2018, 66, 190. [Google Scholar] [CrossRef]
- Cougnard-Gregoire, A.; Merle, B.M.; Aslam, T.; Seddon, J.M.; Aknin, I.; Klaver, C.C.; Garhöfer, G.; Layana, A.G.; Minnella, A.M.; Silva, R. Blue Light Exposure: Ocular Hazards and Prevention—A Narrative Review. Ophthalmol. Ther. 2023, 12, 755–788. [Google Scholar] [CrossRef]
- Hyman, P.; Abedon, S.T. Bacteriophage host range and bacterial resistance. Adv. Appl. Microbiol. 2010, 70, 217–248. [Google Scholar]
- Oliveira, V.C.; Bim, F.L.; Monteiro, R.M.; Macedo, A.P.; Santos, E.S.; Silva-Lovato, C.H.; Paranhos, H.F.; Melo, L.D.; Santos, S.B.; Watanabe, E. Identification and characterization of new bacteriophages to control multidrug-resistant Pseudomonas aeruginosa biofilm on endotracheal tubes. Front. Microbiol. 2020, 11, 580779. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Wang, Q.; Hu, X.; Liu, W. Current status of probiotics as supplements in the prevention and treatment of infectious diseases. Front. Cell. Infect. Microbiol. 2022, 12, 167. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marasini, S.; Craig, J.P.; Dean, S.J.; Leanse, L.G. Managing Corneal Infections: Out with the old, in with the new? Antibiotics 2023, 12, 1334. https://doi.org/10.3390/antibiotics12081334
Marasini S, Craig JP, Dean SJ, Leanse LG. Managing Corneal Infections: Out with the old, in with the new? Antibiotics. 2023; 12(8):1334. https://doi.org/10.3390/antibiotics12081334
Chicago/Turabian StyleMarasini, Sanjay, Jennifer P. Craig, Simon J. Dean, and Leon G. Leanse. 2023. "Managing Corneal Infections: Out with the old, in with the new?" Antibiotics 12, no. 8: 1334. https://doi.org/10.3390/antibiotics12081334
APA StyleMarasini, S., Craig, J. P., Dean, S. J., & Leanse, L. G. (2023). Managing Corneal Infections: Out with the old, in with the new? Antibiotics, 12(8), 1334. https://doi.org/10.3390/antibiotics12081334






