Abstract
To investigate the persistence risk of Campylobacter spp. in poultry farms, and to study the virulence and antimicrobial resistance characteristics in the recovered strains, we collected 362 samples from breeding hen flocks, before and after disinfection. The virulence factors were investigated by targeting the genes; flaA, cadF, racR, virB11, pldA, dnaJ, cdtA, cdtB, cdtC, ciaB, wlaN, cgtB, and ceuE by PCR. Antimicrobial susceptibility was tested and genes encoding antibiotic resistance were investigated by PCR and MAMA-PCR. Among the analyzed samples, 167 (46.13%) were positive for Campylobacter. They were detected in 38.7% (38/98) and 3% (3/98) of environment samples before and after disinfection, respectively, and in 126 (75.9%) out of 166 feces samples. In total, 78 C. jejuni and 89 C. coli isolates were identified and further studied. All isolates were resistant to macrolids, tetracycline, quinolones, and chloramphenicol. However, lower rates were observed for beta-lactams [ampicillin (62.87%), amoxicillin-clavulanic acid (47.3%)] and gentamicin (0.6%). The tet(O) and the cmeB genes were detected in 90% of resistant isolates. The blaOXA-61 gene and the specific mutations in the 23S rRNA were detected in 87% and 73.5% of isolates, respectively. The A2075G and the Thr-86-Ile mutations were detected in 85% and 73.5% of macrolide and quinolone-resistant isolates, respectively. All isolates carried the flaA, cadF, CiaB, cdtA, cdtB, and cdtC genes. The virB11, pldA, and racR genes were frequent in both C. jejuni (89%, 89%, and 90%, respectively) and C. coli (89%, 84%, and 90%). Our findings highlight the high occurrence of Campylobacter strains exhibiting antimicrobial resistance with potential virulence traits in the avian environment. Thus, the improvement of biosecurity measures in poultry farms is essential to control bacterial infection persistence and to prevent the spread of virulent and resistant strains.
1. Introduction
Campylobacter spp. are a major cause of foodborne diarrheal illnesses in humans, and represent the main cause of infant enteric disease in developing countries. Campylobacteriosis is an important zoonosis, with infection occurring mainly through the ingestion of contaminated food and water, or direct contact with contaminated food animal species or their carcasses [1]. Out of the 17 species and the 6 subspecies of the genus Campylobacter spp., C. jejuni and C. coli are the most commonly documented species in human diseases. The infection causes inflammation, bloody diarrhea, cramps, fever, and pain. Even though the pathogenesis of Campylobacter spp. is yet unclear, various virulence factors, such as motility, adhesion, colonization, host cell invasion, and the production of cytolethal distending toxin were associated with their pathogenicity [1,2].
For a human Campylobacter infection, supportive antimicrobial therapies are typically not necessary; however, in the case of immunocompromised people, pregnant women, children, and the elderly, an antibiotic therapy could be needed. Fluoroquinolones (i.e., ciprofloxacin) and macrolides (erythromycin, azithromycin) are the most prescribed drugs for human campylobacteriosis; in addition, tetracycline and gentamicin are also effective against systemic infection with Campylobacter spp. [3]. These common antibiotics are frequently used in food animals, such as chicken, to prevent and reduce bacterial infections in farms and to improve the performance of the animals’ growth. Globally, these practices have been associated with high rates of antimicrobial resistance (AMR) in Campylobacter spp. isolated from animal sources. The loss of therapeutic effectiveness of antibiotics due to AMR spreading leads to higher rates of mortality and morbidity from infectious diseases both in humans and animals, generating serious socioeconomic and public health problems [3].
Campylobacter spp. infect several animals (cattle, sheep, pigs, birds, reptiles, and crustaceans, etc.); however, poultry are the main reservoir of these agents. The bacteria colonize the cecum, distal jejunum, and cloaca of birds, given their ability to live in the mucus and crypts of these organs. Most of Campylobacter species colonize and proliferate in the chicken gastrointestinal tract without any clinical symptoms [4,5]. They can survive and spread from one rearing cycle to the next despite their tremendous vulnerability in the breading farm. In addition, since chickens are coprophagic, inadequate biosecurity measures and an intensive production method are the main causes of infection spreading from infected chicken to others [6]. Consequently, fecal shedding of Campylobacter allows this pathogen to easily contaminate the carcasses during processing, which can ultimately lead to the transmission of Campylobacter to humans.
Campylobacter could also be introduced into flocks from the immediate environment of the buildings as well as from surrounding farms [7,8] by various vectors: insects, rodents, farmers or other persons entering the buildings during rearing, as well as equipment introduced from one building to another [9,10]. The litter also plays an important role as a source for contamination, indeed, these bacteria could survive for 10 days at 20 °C [11].
In Tunisia, as in other developing countries, data on the status of Campylobacter in poultry farms are limited. Today, it has become essential to take the problem of farm contamination into consideration, both for its impact on public health and for the significant economic repercussions for farmers. Although contamination of poultry meat is possible at all stages of the food chain, the rearing period represents a critical phase in the spreading of the bacteria. Therefore, the aim of this study was to investigate the persistence of Campylobacter spp. contamination in one Tunisian intensive breeding hen farm after cleaning and disinfection and to characterize virulence and antimicrobial resistance traits of the recovered Campylobacter strains.
2. Results
2.1. Biosecurity Measures
2.1.1. Environment of the Farm
In the environment of the visited farm, animals (cats and dogs), insects and reptiles, also known as vermin, were present. The studied farm is located near the villages that surround it, and close to traffic routes. The buildings (n = 28) are more than 20 m apart from each other. The areas around the buildings are paved, and the parking areas for delivery vehicles are always close to the building’s entrance (Supplementary file S1).
2.1.2. Characteristics of the Farm
The capacity of the breeding hen flocks varied between 2500 to 18,000 birds in each building, and the average surfaces varied from 500 to 1600 m2. The age of the sampled hens ranged from 42 days to 75 weeks. The floors were made of concrete and the litter was made of wood chips in all of the buildings. The ventilation system was automatic. The buildings contained an airlock separated into two zones with a pedestrian restroom at the entrance. The farm managers declared that they clean the airlock floor at least once a week (Supplementary file S1).
2.1.3. Sanitary Measures
The application of sanitary measures for environmental cleaning is done on a regular basis. The farm is distinguished by a high animal density per m2. In fact, at the time of installation (hens), the density in the breeding hen flocks ranged between 10 and 30 animal/m2. Water was supplied to the visited farm by the National Society for the Exploitation and Distribution of Water (SONED) network. Employees of the farm clean and disinfect the facilities. A sanitary vacuum is used, with a duration of 20 days.
2.1.4. Personnel Hygiene
The number of workers per building does not exceed two. A change of clothes and boots was not strictly respected (at least once a week).
According to the biosecurity data recovered from the questionnaire, the most applied biosecurity measures in this farm were locked buildings, visitor restriction, feed quality, united overalls and footwear for the workers, and the application of a disinfection program at the end of each rearing cycle. By contrast, the lowest applied measures were the high intensity of birds per m2, the isolation of the farm from animals (rodents, reptiles, dogs, cats, etc.), absence of disinfectant baths, low clothes property, and hand hygiene.
2.2. Contamination Rates of Campylobacter spp. in Breeding Hens and Environment before and after Cleaning and Disinfection
The rate of Campylobacter detection in the cloacal swabs of breeding hens was 75.9% (126/166); 70.63% of isolates were identified as C. jejuni (n = 89) and 29.36% as C. coli (n = 37). The percentage of infection in the flocks ranged from 14% to 56% per building (p < 001).
A total of 196 samples were collected from the environment of eight breeding hen buildings before and after cleaning and disinfection (Table 1). Before the void spaces, we collected 98 samples, from plates, nest boxes, and soil. Among them, 38 (38.7%) were Campylobacter spp.-positive, which were identified as C. coli.

Table 1.
Occurrence of Campylobacter in environment before and after disinfection.
Among the 98 environmental samples collected after cleaning and disinfection, only three boots were Campylobacter spp.-positive (3%; 3/98) (Table 1). The three were identified as C. coli. Taken together, 89 C. jejuni and 78 C. coli isolates were identified and further studied.
2.3. Antimicrobial Resistance Patterns
All Campylobacter isolates were resistant to erythromycin, ciprofloxacin, nalidixic acid, chloramphenicol, and tetracycline. To a lesser extent, resistance rates to β-lactams were about 62.87% toward ampicillin and 47.3% toward amoxicillin/clavulanic acid. The resistance rates in C. jejuni and C. coli isolates against ampicillin (47.19% and 81%, respectively) and amoxicillin/clavulanic acid (58.42% and 20.22%, respectively) differed significantly (p < 0.05). No significant difference was observed between both species for the other antibiotics (Table 2).

Table 2.
Percentage of resistant Campylobacter isolates.
Multidrug resistance to at least three antimicrobial classes was detected in all Campylobacter isolates, and 14.37%, 47.9%, and 30.53% of isolates were resistant to 4, 5, and 6 antimicrobial classes, respectively. When looking at the antimicrobial resistance patterns, five antimicrobial resistance patterns were found for all Campylobacter isolates, with the combination “AMP + CIP + NAL + ERY + TET + CHL” as the most common profile (39.52%). A significant higher percentage of C. coli isolates (83.3%) exhibited this resistance profile, compared with C. jejuni isolates (47.6%). The next most frequent pattern was the combined resistance to AMP, AMC, CIP, NAL, ERY, TET, and CHL, detected in 30.53% of isolates. The remaining patterns comprised less than 10% of isolates (Figure 1).
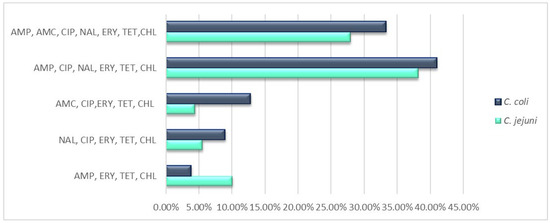
Figure 1.
Rates of antimicrobial resistance patterns of C. jejuni and C. coli isolates. Abbreviations: ERY, erythromycin; CIP, ciprofloxacin; NAL, nalidixic acid; TET, tetracycline; AMP, ampicillin; AMC, amoxicillin/clavulanic acid; CHL, chloramphenicol; GEN, gentamicin.
2.4. Detection of Antimicrobial Resistance Genes
The rates of antimicrobial resistance genes among resistant isolates of C. jejuni and C. coli were as follows: tet(O) (100% vs. 80%), cmeB (80% vs. 100%), and blaOXA-61 (81% vs. 93%), respectively. The aphA-3 gene was not detected (Figure 1). Interestingly, when testing these genes in susceptible isolates, the blaOXA-61 gene was detected in 41% of β-lactams-susceptible C. coli isolates. None of the other genes was detected in the sensitive isolates. In Cip and/or Nal resistant isolates, the analysis of the gyrA gene showed the presence of the Thr-86-Ile amino acid substitution in 90% of C. jejuni and 80% of C. coli isolates. Meanwhile, for the only C. jejuni isolate exhibiting susceptibility to both quinolones (Cip and Nal), the Thr-86-Ile substitution was not detected. Macrolide-resistant isolates were tested for the presence of the mutations A2074C and A2075G in the 23S rRNA gene. The mutation at position A2075G was found in 86% and 61% of C. jejuni and of C. coli isolates, respectively. While the A2074C mutation occurred in 14% and 27% of C. jejuni and C. coli isolates, respectively. Interestingly, 12% of C. coli isolates harbored mutations at both positions (A2074/2075) of the V region (Figure 2).
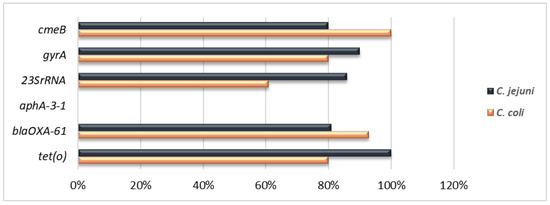
Figure 2.
Percentage and distribution of antimicrobial resistance determinants among C. jejuni and C. coli isolates. Antibiotics and resistance determinants: quinolones (gyrA), erythromycin (23SrRNA), β-lactams (blaOXA-61), tetracyclines (tet(O)), gentamicin (aphA-3), multidrug resistance (cmeB), resistance to ciprofloxacin or nalidixic acid or both and resistance to ampicillin or amoxicillin/clavulanic acid or both.
2.5. Prevalence of Genes Encodingvirulence Factors
All Campylobacter isolates (78 C. jejuni and 89 C. coli) were analyzed for virulotype (content of genes coding for virulence factors) and AR phenotypic profiles. All isolates (n = 167, 100%) harbored the flaA, cadF, ciaB, and cdt genes, followed closely by the racR gene (n = 160, 90%). A similar result was obtained when analyzing the 78 C. jejuni isolates. In addition, the flaA, cadF, ciaB, and cdt genes were present in all C. jejuni isolates (n = 78, 100%), followed by the dnaJ (n =73, 93.58%) and ceuE (n = 69, 88.46%) genes (Figure 3A). No discernible differences were found between both campylobacter species for the most prevalent virulence genes. Indeed, all isolates contained the flaA, cadF, racR, ciaB, and cdt genes, while the pldA gene was detected in 75 (84.26%) isolates. Interestingly, a significant difference was found for the ceuE gene, which was absent in all C. coli isolates but strongly present in C. jejuni (90.47%) (Figure 3B).
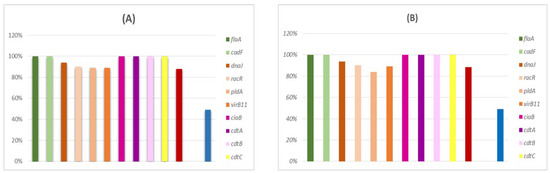
Figure 3.
Occurrence of virulence genes in Campylobacter isolates (n = 167). (A) In C. jejuni (n = 78) and (B) in C. coli (n = 89).
3. Discussion
3.1. Prevalence of Campylobacter and Risk Factors
In this study, we focused on the risk factors contributing to the colonization of Campylobacter in breeding hens, in order to evaluate the control measures to be adopted to reduce the prevalence of Campylobacter colonization. The described factors are related to the farm management and the sanitary measures applied in the flocks. The survey in this poultry farm showed that several animals such as cats, dogs, insects, and reptiles have access to these facilities. It is well known that these animals can carry zoonotic pathogens [4].
The proximity of farms to rural villages is also a problem for the poultry sector in some cases. This results in the negative influence of certain human activities on the studied farm. The cohabitation of humans with these animals may carry the risk of increasing the possibility of human contamination [12]. The absence of an outer barrier on the farm gives free access of outside animals such as dogs and cats. This lack of a barrier at the farm level can be a factor in the degradation of hygiene at this farm. As a result, it might have a negative effect on productivity and possibly act as a vector for the spread of some zoonotic diseases to poultry [13]. Easy access to poultry facilities by dogs, cats, and reptiles significantly increases the risk of contamination. Those studies also indicated that any input to the farm is likely to carry the bacteria from infected units to others, as is the case for personnel in the absence of single-use boot swabs or equipment soiled by feces [12,14]. The same applies to vehicles driving around the building.
The cleaning of farms is an effective way to reduce and even eliminate certain pathogenic microorganisms. The studied farm consisted of 28 flocks, which were made of concrete floors and were easy to clean and disinfect and therefore not favorable to the survival and multiplication of pathogenic bacteria.
Our work showed that the poultry farm exhibited a density of poultry that was above regulatory levels, which is in accordance with the results of other authors who have reported that high density is a risk factor for contamination and facilitates the growth of certain pathogenic bacteria [15]. Furthermore, previous studies have also shown that crowding is a key factor in the introduction of pathogens into an environment [16]. Knowledge of these practices can help to reduce the risks in advance. In fact, Jussiau et al. [17] showed that when personnel perform their duties without consistently changing into new work clothing at least once a week and without using single-use boot covers, they promote the contamination of the farms by pathogenic Campylobacter spp.
The studied poultry production structure has a production system showing average health safety measures. The risk factors for Campylobacter infection in poultry products are real and are summarized, for example, by the precarious nature of the installations and the non-respect of hygiene rules by certain operators in the sector. Thus, the studied farm could be a potential source of dissemination of zoonotic infections mainly campylobacteriosis.
In the domain of food safety, Campylobacter represents an emerging threat with increasing importance over the last years. Therefore, in our work, we were interested in studying the prevalence of Campylobacter spp. in the feces of breeding hens. In the present study, our findings revealed a prevalence of 75.9% (126/166 samples) from which 70.6% and 29.36% were identified as C. jejuni and C. coli, respectively. C. jejuni was the predominant species recovered from poultry carcasses as reported in several studies worldwide [18]. When comparing the Campylobacter infection rate in the studied farm (39.4%), it showed that it was higher than rates observed in Greece (13.33%) [19] and in Australia (11%) [20], but it is lower than those observed in Finland (86%) [21], Italy (65%) [22], and Sri-Lanka (64%) [23].
Despite the various epidemiological studies carried out on Campylobacter contamination of farms, the sources and routes of contamination of chickens by this bacterium are still poorly understood. It is essential to consider the problem of farm contamination, both for its impact on public health and for the significant economic repercussions. Although contamination of meat is possible at all levels of the production chain, the rearing period is also a critical stage for the development of Campylobacter [24]. The knowledge of the modalities of contamination of poultry by Campylobacter during this period is therefore essential in order to prevent its development throughout the chain. To our knowledge, no study has been done in Tunisia on the factors of Campylobacter contamination in breeding hens’ flocks. Therefore, our objective in this study was to investigate the prevalence of Campylobacter in the environment of a poultry farm and to determine the possibility of isolating Campylobacter from environmental surfaces, flocks, and changing rooms after cleaning and disinfection procedures in flocks. Our study was conducted between May and June 2018, when the weather became dry, as it has been previously reported that Campylobacter survival was reduced in low humidity environments [25,26].
A total of 196 samples were collected from the farm environment before and after cleaning and disinfection of the flocks. Before and after the sanitation, we collected 98 environmental samples. The overall prevalence of Campylobacter spp., was 21% (41 isolates) all identified as C. coli. The predominance of C. coli in isolates from breeding hen flocks environments was in agreement with various surveys conducted in European countries, including Bulgaria, Hungary, Italy, Luxembourg, Malta, Portugal, Ireland, Spain, and Greece [27,28,29,30]. Of all the samples taken before cleaning, 38.7% (38/98) were positive for C. coli. The isolation rate in our study is in line with previous results in France [31,32]. From the total number of samples taken after cleaning, only 3% (3/98) were positive for C. coli which were isolated from the workers’ boots. The results indicate that transmission to the chickens can occur via the farmer (boots).
It has also been shown that the implementation of strict biosecurity measures (such as boot dips) has an effect on the prevalence of Campylobacter, reducing the transmission rate [33]. This observation corroborates with the results of Guerin et al. [33] and Facciolà et al. [34] showing the presence of Campylobacter in the immediate environment of farms.
Our findings are also explained by insufficient environmental conditions for cleaning and disinfection, poor hygiene conditions and ignorance of owners and workers. The persistence of Campylobacter after cleaning and disinfection of poultry farms is commonly reported in poultry industries and constitute a serious threat for human health [35,36]. To summarize, although poultry farming is evolving in Tunisia, there are still shortcomings in the management of the quality of the facilities and the application of good practices for the rearing and slaughter of poultry products.
3.2. Antimicrobial Resistances and Implicated Genes
The treatment of infections in humans and animals with antibiotics is being threatened by the emergence and spread of antimicrobial resistant bacteria. Inappropriate use of veterinary drugs in animal husbandry plays an important role in the rise of antimicrobial resistance rates in foodborne pathogens. Antibiotics are extremely used in high-volume in poultry production, whether to prevent bacterial infections or as growth promoter. Thus, antimicrobial resistance studies are essential to identify resistant Campylobacter strains in poultry and their environments. The spread of antimicrobial resistance worldwide is strongly linked to mobile genetic elements like plasmids and transposons, which can also carry virulence determinants [37].
Our research has shown that resistance to erythromycin, tetracycline, quinolones and ciprofloxacin is prevalent, which can significantly reduce the possibilities of treating infections caused by these strains. As these antibiotics have been on the market for a long time and have been frequently used in legal and illegal situations, high rates of resistance are highly expected. Similar high rates of resistance have been found in several other studies, particularly more recent ones [38,39]. In fact, the widespread use of these antibiotics in the management, treatment, and disease prevention of livestock enhances the selection and development of antimicrobial-resistant Campylobacter, which contributes to an increasing burden of antibiotic-resistant infections, with serious consequences for human health due to infection via food chain or direct contact of infected animals.
The majority of isolates have antimicrobial resistance phenotypes that closely match the genetic mutations and genes that code for a corresponding resistance phenotype. The tet(O) gene, which produces the TetO ribosomal protection protein, has been linked to tetracycline resistance [40,41]. Our isolates showed a high rate of resistance to fluoroquinolones. The cmeABC operon, encoding for multidrug efflux, was detected in all our isolates irrespective of their resistance or susceptibility to quinolones/fluoroquinolones. The Thr-86-Ile substitution, which is frequently found in isolates resistant to quinolones and fluoroquinolones, is one of several point mutations in the QRDR of the GyrA protein that make up the second resistance process [42]. The gene encoding 23S rRNA had the two-point mutations A2075G and/or A2074C in all erythromycin-resistant Campylobacter isolates [42].
The erm (B) gene, was found in 55.55% [25/45: 47.61% (10/21) C. jejuni and 62.5% (15/24) C. coli]. The presence of this gene in Campylobacter isolates is noteworthy, as it was discovered on MDR gene islands co-harboring genes that encoded resistance to ampicillin, ciprofloxacin, and tetracycline [43]. These results are concerning because macrolides, in particular erythromycin and azithromycin, are the preferred antibiotics for treating human Campylobacter infections. β-lactam antibiotics, such as ampicillin, are intrinsically ineffective against Campylobacter spp. [43]. The primary mechanism of acquired ampicillin resistance is, in fact, enzymatic inactivation by the beta-lactamase encoding blaOXA-61 gene, which was found in 20% and 8% of β-lactam resistant C jejuni and C coli isolates, respectively. According to earlier reports [39,43], the majority of our isolates were gentamicin-susceptible. This may be due to its restricted use for systemic infections and the fact that it is not used in the production of poultry [39,40].
3.3. Occurrence of Virulence Genes
The pathogenicity of Campylobacter species is influenced by their virulome [44] so it is important to look into the virulence factors of avian Campylobacter for consumer safety.
This study revealed that all isolates had the genes cdtA, cdtB, and cdtC, which are essential for cytolethal distending toxin (CDT) expression, as well as flaA, cadF, and ciaB, which are related to adhesion, colonization, and invasion. These genes were found in similar frequencies to those previously reported from Korea [45] and Italy [34], but at higher levels than those previously reported from South Africa and Chile [46]. In cell models, Campylobacter adhesion and internalization are empowered by the presence of the cadF and ciaB genes [47]. According to research from South Africa [48], Japan [49], and Iran [50], C. jejuni had a higher rate of the pldA gene, which encodes the outer membrane phospholipase A.
4. Materials and Methods
4.1. Samples Collection
Our study was conducted in an intensive breeding hen farm located in the governorate of Nabeul in north-eastern Tunisia. Eight breeding hen flocks were monitored from May to June 2018. The ages of the breeding hens ranged from 42 to 75 weeks. The farm is one of the biggest poultry farms in Tunisia, encompassing 28 flocks and each flock houses 2300 to 18,000 birds, and covering 43 hectares. Birds had ad libitum access to feed and water. The diets were provided in mash form and consisted of corn-soybean meal, barley, bran, calcium carbonate, dicalcium phosphate, and vitamin and mineral supplements. For preventive purposes against infectious diseases, the following antibiotics are commonly used: enrofloxacine, florfenicol, doxycycline, oxytracycline, tiamulin, colistin, and trimethoprim-sulfadiazin. IODOSAN 30 (EWABO Chemikalien GmbH & Co. KG, Wietmarschen, Germany) and DEPTAL MCL (code 02080) (Kersia, Courcelles, Belgium) are used as the disinfectant for cleaning surfaces of flocks.
A total of 362 samples were taken from chickens’ cloacal swabs (n = 166) and the farm environment before (n = 98) and after (n = 98) the cleaning and disinfection of the buildings. Meaning, that before the cleaning period, the 264 collected samples encompassed 166 cloacal swabs and 98 environmental samples (rays, nest boxes, and from the ground). After the cleaning and disinfection step, we collected 98 environmental samples [trays, nests, plates, floor, doors, the changing rooms (blouses, boots, and flip flops)]. Environment samples were taken by smearing swabs soaked in Bolton Broth (Oxoid, Basingstoke, UK). In each flock, approximately 25 cloacal swabs were taken from five locations (four corners and the center).
4.2. Audit of Cleaning and Disinfection Procedures in Poultry Farm Buildings
To study the risk factors potentially linked to contamination by Campylobacter spp. a questionnaire was properly completed during the sample collection visits for the farm (Supplementary file S2). The farm visit frequency was dependent on the authorizations of the breeders. The epidemiological questionnaire comprised several questions. The questions were related to the description of the farm, the buildings (flocks); breeding characteristics and management; dead bird management measures; control of rodents and other domestic animals; biosecurity; operations personnel and visitors; vaccination and administration of antibiotics. The obtained scores were based on both personal observations and information collected from the employees and the responsible veterinarians. These notes were useful to establish possible correlations between the characteristics of the breeding and the contamination by Campylobacter spp.
4.3. Sample Transportation and Processing
According to the Good Execution Analysis (GBEA) Guide and the Standard NF EN ISO 15189 (version 2012) [51], the samples were transported in a cooler box with cold accumulators at 4 °C and brought to the laboratory within 4 h. When the samples arrived at the laboratory, they were all pre-enriched on the same day.
4.4. Culture and Growth Conditions
The isolation of Campylobacter was carried out according to the standard French method (AFNOR, La Plaine-saint-denis, France, 1996). All samples were subjected to a selective enrichment step in Bolton broth (Oxoid, Basingstoke, UK), in a microaerophilic atmosphere (5% O2, 10% CO2, 85% N2) using GENbox generators (BioMérieux, Craponne, France) at 42 °C during 18 h–24 h. Presumptive positive culture for Campylobacter were streaked on Karmali agar (Oxoid, Basingstoke, UK) and incubated for 48 h under the same conditions as described previously [52]. Under a light microscope and using oxidase/catalase assays, suspected colonies from each sample were examined for typical Campylobacter morphology and motility. Then, presumptive Campylobacter colonies were subjected to PCR analysis for genus and species identification.
4.5. DNA Extraction
For the PCR tests, the genomic DNA of collected isolates was extracted using the boiling method [39]. Campylobacter isolates were grown in 2 mL Bolton broth and plated on Karmali agar. Campylobacter colonies were then harvested and suspended in 100 μL TE buffer (10 mM Tris, 1 mM EDTA, pH 8.0). Cell suspensions were heated at 100 °C for 10 min and then cooled to room temperature. Thereafter, cell suspensions were pelleted by centrifugation at 8000 rpm for 5 min. The supernatant containing DNA was collected, transferred into a new tube, and then stored at −20 °C until use.
PCR amplification of a specific fragment of the 16S rDNA gene using the primers described by Linton et al. [53] was used to Campylobacter genus identification of isolates. Then, the isolates were identified as C. jejuni or C. coli by PCR assays based on amplification of the mapA and ceuE genes, respectively [54] (Supplementary file S3, Table S1).
4.6. Antimicrobial Susceptibility Test
Antimicrobial susceptibility testing was performed on all isolates using the disk diffusion method on Mueller-Hinton medium (Bio Life, Milan, Italy) according to the recommendation of the Antibiogram Committee of French Society for Microbiology (CA-SFM) [55]. The following antibiotics were used (Oxoid, Basingstocken, UK): ampicillin (AMP,10 μg), amoxicillin/clavulanic acid (AMC, 10/20 μg), tetracycline (TET, 30 μg), erythromycin (ERY, 15 μg), gentamicin (GEN, 10 μg), chloramphenicol (CHL, 30 μg), nalidixic acid (NAL, 30 μg), and ciprofloxacin (CIP, 5 μg) [39]. The isolates were defined as multidrug-resistant (MDR) if they exhibited resistance to at least one agent belonging to three or more antimicrobial families [56].
4.7. Detection of Mutation(s) in the QRDR of gyrA and 23S rRNA Genes by PCR Mismatch Amplification Mutation Assay (MAMA-PCR)
A single point mutation Thr-86-Ile in the quinolone resistance-determining region (QRDR) of the gyrA gene was defined as the main cause of high-level resistance to quinolones. Campylobacter isolates were subjected to analysis by MAMA-PCR, as previously described for C. jejuni and C. coli isolates by Zirnstein et al. [57,58]. The resistance to macrolide (particularly to erythromycin) is mainly encoded by mutations in the V domain of the 23S rRNA gene, at the positions A2074C or A2075G. The detection of these mutations was also carried out by MAMA-PCR as described previously by Alonso et al. [59].
4.8. Detection of Their Resistance Determinants
All Campylobacter isolates were screened by PCR to detect the tet(O) (tetracyclines resistance), aphA-3 (aminoglycosides resistance), cmeB (multidrug efflux pump), and blaOXA-61 (β-lactams resistance) genes (Table S1). The PCR mixture (25 µL) consisted of 2.5 μL of DNA template, 0.2 μM of each primer (Carthagenomics Advanced Technologies, Borj Cédria, Tunisia), 0.2 mM dNTP (Promega, Charbonnières-les-Bains, France), 1X Dream DNA polymerase buffer, and 1U Dream Taq DNA polymerase (Thermo Scientific, Bordeaux, France).
4.9. Detection of Virulence Genes
All Campylobacter isolates were tested by PCR for the occurrence of the following virulence genes: flaA (motility), cadF, racR, virB11, pldA, dnaJ (adherence and colonization), cdtA, cdtB, cdtC (cytotoxin production), cgtB and wlaN (Guillain-Barré syndrome), ciaB (invasiveness), and ceuE encoding a lipoprotein in C. jejuni strains (Table S1).
4.10. Data Analysis
All collected data were analyzed using R software. The antimicrobial resistance analyses were performed by means of a Chi-square statistic (p < 0.05) [60]. This test is a nonparametric tool designed to compare frequency counts between two groups of different sample sizes; the selection criteria for significantly prevalent variance was a stringent p-value of 0.001 or less.
5. Conclusions
The present study revealed high levels of Campylobacter contamination in the studied breeding farm, with a predominance of C. jejuni and C. coli species. The recovered strains exhibited high levels of resistance to clinically relevant antimicrobial agents (i.e., erythromycin, ciprofloxacin, and tetracycline) and simultaneously harbored several virulence genes. The persistence of these strains after farm disinfection may present a significant risk of cross-contamination of new chicken batches and the spread of virulent and resistant strains throughout the poultry production chain. It is therefore essential to raise awareness among poultry farmers and to improve biosecurity practices to avoid the persistence and spread of infectious agents, including Campylobacter, in poultry farms.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/antibiotics12050890/s1, File S1: Results of the questionnaire. File S2: The questionnaire (in the French language). File S3: Table S1: Primers, amplification conditions, and references of investigated genes. References [53,57,58,59,61,62,63,64,65,66,67,68,69] are cited from the supplementary materials.
Author Contributions
Conceptualization, M.G. and A.M. methodology, M.G., A.B. and A.M.; validation, M.G. and A.M.; formal analysis, M.G.; investigation, M.G., A.B., S.H., A.A. and A.M.; data curation, M.G.; writing—original draft preparation, M.G.; writing—review and editing, M.G.; visualization, M.G. and A.M.; supervision, A.M.; project administration. All authors have read and agreed to the published version of the manuscript.
Funding
This work was financed by funding provided to the Laboratory of Epidemiology and Veterinary Microbiology (LR16IPT03) by the Tunisian Ministry of Higher Education and Scientific Research.
Institutional Review Board Statement
The study was approved by the Biomedical Ethics Committee of the Pasteur Institute of Tunis, with reference number: 2018/12/I/LR16IPT.
Data Availability Statement
The statistical data used to support the findings of this study are available from the corresponding author upon request.
Acknowledgments
We would like to acknowledge the veterinarians and workers in the studied farm for their contribution to collecting samples and responses to the questionnaire.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Igwaran, A.; Okoh, A.I. Human Campylobacteriosis: A Public Health Concern of Global Importance. Heliyon 2019, 5, e0281. [Google Scholar] [CrossRef] [PubMed]
- Bolton, D.J. Campylobacter Virulence and Survival Factors. Food Microbiol. 2015, 48, 99–108. [Google Scholar] [CrossRef]
- García-Fernández, A.; Dionisi, A.M.; Arena, S.; Iglesias-Torrens, Y.; Carattoli, A.; Luzzi, I. Human Campylobacteriosis in Italy: Emergence of Multi-Drug Resistance to Ciprofloxacin, Tetracycline, and Erythromycin. Front. Microbiol. 2018, 9, 1906. [Google Scholar] [CrossRef] [PubMed]
- Food, E.; Authority, S. The European Union Summary Report on Trends and Sources of Zoonoses, Zoonotic Agents and Food-Borne Outbreaks in 2017. EFSA J. 2018, 16, e05500. [Google Scholar]
- Hermans, D.; Pasmans, F.; Messens, W.; Martel, A.; Van Immerseel, F.; Rasschaert, G.; Heyndrickx, M.; Van Deun, K.; Haesebrouck, F. Poultry as a Host for the Zoonotic Pathogen Campylobacter jejuni. Vector Borne Zoonotic Dis. 2012, 12, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Pielsticker, C.; Glünder, G.; Rautenschlein, S. Colonization Properties of Campylobacter Jejuni in Chickens. Eur. J. Microbiol. Immunol. 2012, 2, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Jacobs-Reitsma, W.F. Aspects of Epidemiology of Campylobacter in Poultry. Vet. Q 1997, 19, 113–117. [Google Scholar] [CrossRef]
- Van De Giessen, A.W.; Tilburg, J.J.H.C.; Ritmeester, W.S.; Van Der Plas, J. Reduction of Campylobacter Infections in Broiler Flocks by Application of Hygiene Measures. Epidemiol. Infect. 1998, 121, 57–66. [Google Scholar] [CrossRef]
- Puterflam, J.; Bouvarel, I.R.; Ragot, O.; Drouet, M. Contamination des élévages de poulets de chair par Campylobacter: Est-ce une fatalité. Sci. Technol. Avic. 2005, 53, 12–19. [Google Scholar]
- Van De Giessen, A.W.; Bloemberg, B.P.M.; Ritmeester, W.S.; Tilburg, J.J.H.C. Epidemiological Study on Risk Factors and Risk Reducing Measures for Campylobacter Infections in Dutch Broiler Flocks. Epidemiol. Infect. 1996, 117, 245–250. [Google Scholar] [CrossRef]
- Shane, S.M. The Significance of Campylobacter Jejuni Infection in Poultry: A Review. Avian Pathol. 1992, 21, 189–213. [Google Scholar] [CrossRef] [PubMed]
- FAO. CÔTE D’IVOIRE: Revue Du Secteur Avicole; FAO: Rome, Italy, 2008; p. 77. [Google Scholar]
- Van Immerseel, F.; Boyen, F.; Gantois, I.; Timbermont, L.; Bohez, L.; Pasmans, F.; Haesebrouck, F.; Ducatelle, R. Supplementation of Coated Butyric Acid in the Feed Reduces Colonization and Shedding of Salmonella in Poultry. Poult. Sci. 2005, 84, 1851–1856. [Google Scholar] [CrossRef] [PubMed]
- Badji, A.; Lo, M.M.; Alambedji, R.B. Facteurs de Risque Liés à l’apparition de La Maladie de Gumboro En Aviculture Semi-Intensive Au Sénégal. Int. J. Biol. Chem. Sci. 2017, 11, 1551. [Google Scholar] [CrossRef]
- Hendrix, S.L.; Clark, A.; Nygaard, I.; Aragaki, A.; Barnabei, V.; McTiernan, A. Pelvic Organ Prolapse in the Women’s Health Initiative: Gravity and Gravidity. Am. J. Obstet. Gynecol. 2002, 186, 1160–1166. [Google Scholar] [CrossRef] [PubMed]
- Kaci, M.; Sadoun, T.; Cimmino, S. Crystallinity Measurements of Unstabilized and HALS-Stabilized LDPE Films Exposed to Natural Weathering by FT-IR, DSC and WAXS Analyses. Int. J. Polym. Anal. Charact. 2001, 6, 455–464. [Google Scholar] [CrossRef]
- Jussiau, R.; Papet, A.; Rigal, J. Amélioration Génétique des Animaux D’élevage (Edition 2013); Educagri Editions: Dijon, France, 2013. [Google Scholar]
- Wei, B.; Kang, M.; Jang, H.K. Genetic Characterization and Epidemiological Implications of Campylobacter Isolates from Wild Birds in South Korea. Transbound. Emerg. Dis. 2019, 66, 56–65. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.K.; Rigby, D.; Burton, M.; Millman, C.; Williams, N.J.; Jones, T.R.; Wigley, P.; O’Brien, S.J.; Cross, P. Restaurant Cooking Trends and Increased Risk for Campylobacter Infection. Emerg. Infect. Dis. 2016, 22, 1208–1215. [Google Scholar] [CrossRef]
- Novoa Rama, E.; Bailey, M.; Jones, D.R.; Gast, R.K.; Anderson, K.; Brar, J.; Taylor, R.; Oliver, H.F.; Singh, M. Prevalence, Persistence, and Antimicrobial Resistance of Campylobacter Spp. from Eggs and Laying Hens Housed in Five Commercial Housing Systems. Foodborne Pathog. Dis. 2018, 15, 506–516. [Google Scholar] [CrossRef]
- Sulonen, J.; Kärenlampi, R.; Holma, U.; Hänninen, M.L. Campylobacter in Finnish Organic Laying Hens in Autumn 2003 and Spring 2004. Poult. Sci. 2007, 86, 1223–1228. [Google Scholar] [CrossRef]
- Dipineto, L.; Gargiulo, A.; Russo, T.P.; De Luca Bossa, L.M.; Borrelli, L.; Menna, L.F.; Fioretti, A. Campylobacter Jejuni, Campylobacter Coli, and Cytolethal Distending Toxin Genes in Laying Hens. Avian Dis. 2011, 55, 103–105. [Google Scholar] [CrossRef]
- Kalupahana, R.S.; Kottawatta, K.S.A.; Kanankege, K.S.T.; Van Bergen, M.A.P.; Abeynayake, P.; Wagenaar, J.A. Colonization of Campylobacter Spp. in Broiler Chickens and Laying Hens Reared in Tropical Climates with Low-Biosecurity Housing. Appl. Environ. Microbiol. 2013, 79, 393–395. [Google Scholar] [CrossRef] [PubMed]
- Van Asselt, M.; Poortvliet, P.M.; Ekkel, E.D.; Kemp, B.; Stassen, E.N. Risk Perceptions of Public Health and Food Safety Hazards in Poultry Husbandry by Citizens, Poultry Farmers and Poultry Veterinarians. Poult. Sci. 2018, 97, 607–619. [Google Scholar] [CrossRef] [PubMed]
- Ishihara, K.; Yamamoto, T.; Satake, S.; Takayama, S.; Kubota, S.; Negishi, H.; Kojima, A.; Asai, T.; Sawada, T.; Takahashi, T.; et al. Comparison of Campylobacter Isolated from Humans and Food-Producing Animals in Japan. J. Appl. Microbiol. 2006, 100, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Neves, R.A.F.; Santiago, T.C.; Carvalho, W.F.; Silva, E.d.S.; da Silva, P.M.; Nascimento, S.M. Impacts of the Toxic Benthic Dinoflagellate Prorocentrum Lima on the Brown Mussel Perna Perna: Shell-Valve Closure Response, Immunology, and Histopathology. Mar. Environ. Res. 2019, 146, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Pergola, S.; Franciosini, M.P.; Comitini, F.; Ciani, M.; De Luca, S.; Bellucci, S.; Menchetti, L.; Casagrande Proietti, P. Genetic Diversity and Antimicrobial Resistance Profiles of Campylobacter Coli and Campylobacter Jejuni Isolated from Broiler Chicken in Farms and at Time of Slaughter in Central Italy. J. Appl. Microbiol. 2017, 122, 1348–1356. [Google Scholar] [CrossRef]
- Mezher, Z.; Saccares, S.; Marcianò, R.; de Santis, P.; Flores Rodas, E.M.; De Angelis, V.; Condoleo, R. Occurrence of Campylobacter Spp. In Poultry Meat at Retail and Processing Plants’ Levels in Central Italy. Ital. J. Food Saf. 2016, 5, 47–49. [Google Scholar] [CrossRef]
- Sahin, O.; Kassem, I.I.; Shen, Z.; Lin, J.; Rajashekara, G.; Zhang, Q. Campylobacter in Poultry: Ecology and Potential Interventions. Avian Dis. 2015, 59, 185–200. [Google Scholar] [CrossRef]
- Marinou, I.; Bersimis, S.; Ioannidis, A.; Nicolaou, C.; Mitroussia-Ziouva, A.; Legakis, N.J.; Chatzipanagiotou, S. Identification and Antimicrobial Resistance of Campylobacter Species Isolated from Animal Sources. Front. Microbiol. 2012, 3, 58. [Google Scholar] [CrossRef]
- Puterflam, J.; Michel, J.; Hocking, P.M.; Picard, M. Effects of Genotype and Feed Restriction on the Time-Budgets of Broiler Breeders at Different Ages. Appl. Anim. Behav. Sci. 2006, 98, 100–113. [Google Scholar] [CrossRef]
- Snelling, W.J.; Matsuda, M.; Moore, J.E.; Dooley, J.S.G. Under the Microscope: Campylobacter Jejuni. Lett. Appl. Microbiol. 2005, 41, 297–302. [Google Scholar] [CrossRef]
- Guérin, F.; Abril, G. Significance of Pelagic Aerobic Methane Oxidation in the Methane and Carbon Budget of a Tropical Reservoir. J. Geophys. Res. 2007, 112, 1–14. [Google Scholar] [CrossRef]
- Fani, F.; Aminshahidi, M.; Firoozian, N.; Rafaatpour, N. Prevalence, Antimicrobial Resistance, and Virulence-Associated Genes of Campylobacter Isolates from Raw Chicken Meat in Shiraz, Iran. Iran. J. Vet. Res. 2019, 20, 283–288. [Google Scholar] [PubMed]
- Morgan, R.B.; Sierra–Arguello, Y.M.; Perdoncini, G.; Borges, K.A.; Furian, T.Q.; Gomes, M.J.P.; Lima, D.; Salle, C.T.P.; Moraes, H.L.S.; Nascimento, V.P. Comparison of Transport Crates Contamination with Campylobacter spp. before and after the Cleaning and Disinfection Procedure in Broiler Slaughterhouses. Poult. Sci. 2022, 101, 101909. [Google Scholar] [CrossRef] [PubMed]
- Peyrat, M.B.; Soumet, C.; Maris, P.; Sanders, P. Phenotypes and Genotypes of Campylobacter Strains Isolated after Cleaning and Disinfection in Poultry Slaughterhouses. Vet. Microbiol. 2008, 128, 313–326. [Google Scholar] [CrossRef]
- Hasan, M.M.; Talukder, S.; Mandal, A.K.; Tasmim, S.T.; Parvin, M.S.; Ali, M.Y.; Sikder, M.H.; Islam, M.T. Prevalence and Risk Factors of Campylobacter Infection in Broiler and Cockerel Flocks in Mymensingh and Gazipur Districts of Bangladesh. Prev. Vet. Med. 2020, 180, 105034. [Google Scholar] [CrossRef]
- Insights, C. Relationships between Virulence Genes and Antibiotic Resistance Phenotypes/Genotypes in Campylobacter Spp. Foods 2022, 11, 3554. [Google Scholar]
- Gharbi, M.; Béjaoui, A.; Ben Hamda, C.; Jouini, A.; Ghedira, K.; Zrelli, C.; Hamrouni, S.; Aouadhi, C.; Bessoussa, G.; Ghram, A.; et al. Prevalence and Antibiotic Resistance Patterns of Campylobacter Spp. Isolated from Broiler Chickens in the North of Tunisia. Biomed Res. Int. 2018, 2018, 7943786. [Google Scholar] [CrossRef]
- Elhadidy, M.; Miller, W.G.; Arguello, H.; álvarez-Ordóñez, A.; Duarte, A.; Dierick, K.; Botteldoorn, N. Genetic Basis and Clonal Population Structure of Antibiotic Resistance in Campylobacter Jejuni Isolated from Broiler Carcasses in Belgium. Front. Microbiol. 2018, 9, 1014. [Google Scholar] [CrossRef]
- Lynch, C.T.; Lynch, H.; Burke, S.; Hawkins, K.; Buttimer, C.; Mc Carthy, C.; Egan, J.; Whyte, P.; Bolton, D.; Coffey, A.; et al. Antimicrobial Resistance Determinants Circulating among Thermophilic Campylobacter Isolates Recovered from Broilers in Ireland Over a One-Year Period. Antibiotics 2020, 9, 308. [Google Scholar] [CrossRef]
- Fraqueza, M.J.; Martins, A.; Borges, A.C.; Fernandes, M.H.; Fernandes, M.J.; Vaz, Y.; Bessa, R.J.B.; Barreto, A.S. Antimicrobial Resistance among Campylobacter Spp. Strains Isolated from Different Poultry Production Systems at Slaughterhouse Level. Poult. Sci. 2014, 93, 1578–1586. [Google Scholar] [CrossRef]
- Bolinger, H.K.; Zhang, Q.; Miller, W.G.; Kathariou, S. Lack of Evidence for Erm(B) Infiltration into Erythromycin-Resistant Campylobacter Coli and Campylobacter Jejuni from Commercial Turkey Production in Eastern North Carolina: A Major Turkey-Growing Region in the United States. Foodborne Pathog. Dis. 2018, 15, 698–700. [Google Scholar] [CrossRef] [PubMed]
- Han, X.; Guan, X.; Zeng, H.; Li, J.; Huang, X.; Wen, Y.; Zhao, Q.; Huang, X.; Yan, Q.; Huang, Y. Prevalence, Antimicrobial Resistance Profiles and Virulence-Associated Genes of Thermophilic Campylobacter Spp. Isolated from Ducks in a Chinese Slaughterhouse. Food Control 2019, 104, 157–166. [Google Scholar] [CrossRef]
- Oh, J.-Y.; Kwon, Y.-K.; Wei, B.; Jang, H.-K.; Lim, S.-K.; Kim, C.-H.; Jung, S.-C.; Kang, M.-S. Epidemiological Relationships of Campylobacter Jejuni Strains Isolated from Humans and Chickens in South Korea. J. Microbiol. 2017, 55, 13–20. [Google Scholar] [CrossRef]
- Otigbu, A.C.; Clarke, A.M.; Fri, J.; Akanbi, E.O.; Njom, H.A. Antibiotic Sensitivity Profiling and Virulence Potential of Campylobacter Jejuni Isolates from Estuarine Water in the Eastern Cape Province, South Africa. Int. J. Environ. Res. Public Health 2018, 15, 925. [Google Scholar] [CrossRef]
- Ramires, T.; de Oliveira, M.G.; Kleinubing, N.R.; de Fátima Rauber Würfel, S.; Mata, M.M.; Iglesias, M.A.; Lopes, G.V.; Dellagostin, O.A.; da Silva, W.P. Genetic Diversity, Antimicrobial Resistance, and Virulence Genes of Thermophilic Campylobacter Isolated from Broiler Production Chain. Brazilian J. Microbiol. 2020, 51, 2021–2032. [Google Scholar] [CrossRef] [PubMed]
- Pillay, S.; Amoako, D.G.; Abia, A.L.K.; Somboro, A.M.; Shobo, C.O.; Perrett, K.; Bester, L.A.; Essack, S.Y. Characterisation of Campylobacter Spp. Isolated from Poultry in KwaZulu-Natal, South Africa. Antibiotics 2020, 9, 42. [Google Scholar] [CrossRef] [PubMed]
- Datta, S.; Niwa, H.; Itoh, K. Age-Dependent Variation of Virulence-Associated Genes Retained in Campylobacter Jejuni Isolated from Chickens in a Poultry Farm. J. Vet. Med. Sci. 2009, 71, 1247–1249. [Google Scholar] [CrossRef]
- Khoshbakht, R.; Tabatabaei, M.; Hosseinzadeh, S.; Shekarforoush, S.S.; Aski, H.S. Distribution of Nine Virulence-Associated Genes in Campylobacter Jejuni and C. Coli Isolated from Broiler Feces in Shiraz, Southern Iran. Foodborne Pathog. Dis. 2013, 10, 764–770. [Google Scholar] [CrossRef]
- ISO 10272-1 (Annex E); Microbiology of Food And Animal Feeding Stuffs: Horizontal Method for Detection and Enu-Mera-Tion of Campylobacter Spp. I. Detection Method. International Organization for Standardization: Geneva, Switzerland, 2006.
- Gharbi, M.; Béjaoui, A.; Hamda, C.B.; Ghedira, K.; Ghram, A.; Maaroufi, A. Distribution of Virulence and Antibiotic Resistance Genes in Campylobacter Jejuni and Campylobacter Coli Isolated from Broiler Chickens in Tunisia. J. Microbiol. Immunol. Infect. 2022, 55, 1273–1282. [Google Scholar] [CrossRef]
- Linton, D.; Owen, R.J.; Stanley, J. Rapid Identification by PCR of the Genus Campylobacter and of Five Campylobacter Species Enteropathogenic for Man and Animals. Res. Microbiol. 1996, 147, 707–718. [Google Scholar] [CrossRef]
- Denis, M.; Soumet, C.; Rivoal, K.; Ermel, G.; Blivet, D.; Salvat, G.; Colin, P. Development of a M-PCR Assay for Simultaneous Identification of Campylobacter Jejuni and C. Coli. Lett. Appl. Microbiol. 1999, 29, 406–410. [Google Scholar] [CrossRef] [PubMed]
- CA-SFM. Comité de l’Antibiogramme-Société Française de Microbiologie, V 1.0, Mai. Int. J. Antimicrob. Agents. 2022, 21, 119. [Google Scholar]
- Magiorakos, A.P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-Resistant, Extensively Drug-Resistant and Pandrug-Resistant Bacteria: An International Expert Proposal for Interim Standard Definitions for Acquired Resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef] [PubMed]
- Zirnstein, G.; Helsel, L.; Li, Y.; Swaminathan, B.; Besser, J. Characterization of GyrA Mutations Associated with Fluoroquinolone Resistance in Campylobacter Coli by DNA Sequence Analysis and MAMA PCR. FEMS Microbiol. Lett. 2000, 190, 1–7. [Google Scholar] [CrossRef]
- Zirnstein, G.; Li, Y.; Swaminathan, B.; Angulo, F. Ciprofloxacin Resistance in Campylobacter Jejuni Isolates: Detection of GyrA Resistance Mutations by Mismatch Amplification Mutation Assay PCR and DNA Sequence Analysis. J. Clin. Microbiol. 1999, 37, 3276–3280. [Google Scholar] [CrossRef]
- Alonso, R.; Mateo, E.; Churruca, E.; Martinez, I.; Girbau, C.; Fernández-Astorga, A. MAMA-PCR Assay for the Detection of Point Mutations Associated with High-Level Erythromycin Resistance in Campylobacter Jejuni and Campylobacter Coli Strains. J. Microbiol. Methods 2005, 63, 99–103. [Google Scholar] [CrossRef]
- Mchugh, M.L. Lessons in Biostatistics The Chi-Square Test of Independence. Biochem. Med. 2013, 23, 143–149. [Google Scholar] [CrossRef]
- Denis, M.; Refrégier-Petton, J.; Laisney, M.J.; Ermel, G.; Salvat, G. Campylobacter contamination in French chicken production from farm to consumers. Use of a PCR assay for detection and identification of Campylobacter jejuni and Camp. coli. J. Appl. Microbiol. 2001, 91, 255–267. [Google Scholar] [CrossRef]
- Asakura, M.; Samosornsuk, W.; Hinenoya, A.; Misawa, N.; Nishimura, K.; Matsuhisa, A.; Yamasaki, S. Development of a cytolethal distending toxin (cdt) gene-based species-specific multiplex PCR assay for the detection and identification of Campylobacter jejuni, Campylobacter coli and Campylobacter fetus. FEMS Immun. Med. Microbiol. 2008, 52, 260–266. [Google Scholar] [CrossRef]
- Pratt, A.; Korolik, V. Tetracycline resistance of Australian Campylobacter jejuni and Campylobacter coli isolates. J. Antimicrobial Chemother. 2005, 55, 452–460. [Google Scholar] [CrossRef]
- Olah, P.A.; Doetkott, C.; Fakhr, M.K.; Logue, C.M. Prevalence of the Campylobacter multi-drug efflux pump (CmeABC) in Campylobacter spp. Isolated from freshly processed Turkeys. Food Microbiol. 2006, 23, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Obeng, A.S.; Rickard, H.; Sexton, M.; Pang, Y.; Peng, H.; Barton, M. Antimicrobial susceptibilities and resistance genes in Campylobacter strains isolated from poultry and pigs in Australia. J. Appl. Microbiol. 2012, 113, 294–307. [Google Scholar] [CrossRef] [PubMed]
- Datta, S.; Niwa, H.; Itoh, K. Prevalence of 11 pathogenic genes of Campylobacter jejuni by PCR in strains isolated from humans, poultry meat and broiler and bovine faeces. J. Med. Microbiol. 2003, 52 Pt 4, 345–348. [Google Scholar] [CrossRef] [PubMed]
- Konkel, M.E.; Gray, S.A.; Kim, B.J.; Garvis, S.G.; Yoon, J. Identification of the enteropathogens Campylobacter jejuni and Campylobacter coli based on the cadF virulence gene and its product. J. Clin. Microbiol. 1999, 37, 510–517. [Google Scholar] [CrossRef] [PubMed]
- Hickey, T.E.; McVeigh, A.L.; Scott, D.A.; Michielutti, R.E.; Bixby, A.; Carroll, S.A.; Bourgeois, A.L.; Guerry, P. Campylobacter jejuni cytolethal distending toxin mediates release of interleukin-8 from intestinal epithelial cells. Infection Immun. 2000, 68, 6535–6541. [Google Scholar] [CrossRef]
- Gonzalez, I.; Grant, K.A.; Richardson, P.T.; Park, S.F.; Collins, M.D. Specific identification of the enteropathogens Campylobacter jejuni and Campylobacter coli by using a PCR test based on the ceuE gene encoding a putative virulence determinant. J. Clin. Microbiol. 1997, 35, 759–763. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).