Group B Streptococcus Early-Onset Disease: New Preventive and Diagnostic Tools to Decrease the Burden of Antibiotic Use
Abstract
1. Introduction
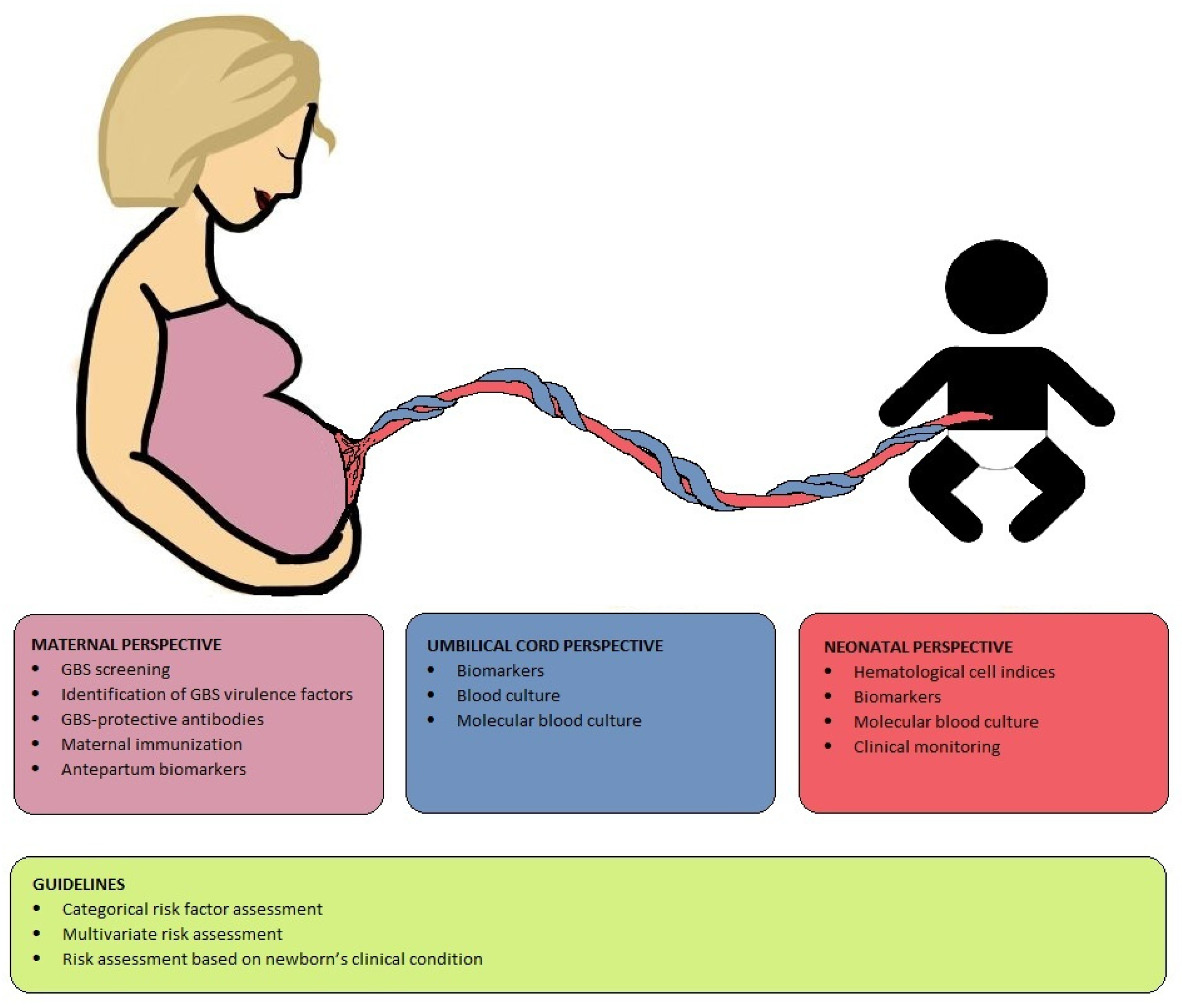
2. Maternal Perspective
2.1. GBS Prevention
2.2. Host–Pathogen Interactions in GBS Disease
2.3. Maternal Immunization
2.4. Antepartum Immunological Biomarkers
3. Umbilical Cord Perspective
3.1. Biomarkers
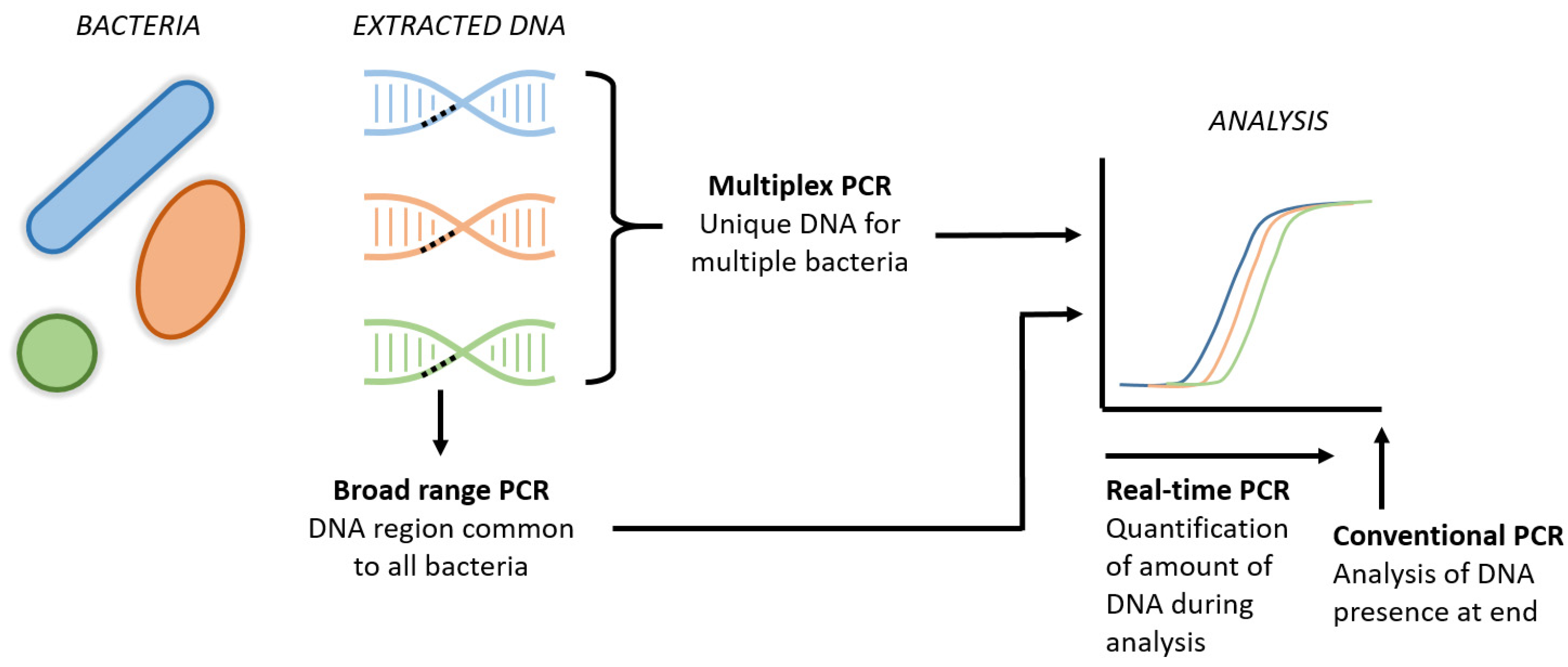
3.2. Blood Culture and Molecular Techniques
4. Newborn Perspective
4.1. Hematological Cell Indices
4.2. Biomarkers
4.3. Blood Culture and Molecular Techniques
4.4. Clinical Prediction and Monitoring
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Seale, A.C.; Bianchi-Jassir, F.; Russell, N.J.; Kohli-Lynch, M.; Tann, C.J.; Hall, J.; Madrid, L.; Blencowe, H.; Cousens, S.; Baker, C.J.; et al. Estimates of the Burden of Group B Streptococcal Disease Worldwide for Pregnant Women, Stillbirths, and Children. Clin. Infect. Dis. 2017, 65, S200–S219. [Google Scholar] [CrossRef]
- Vergnano, S.; Menson, E.; Smith, Z.; Kennea, N.; Embleton, N.; Clarke, P.; Watts, T.; Heath, P.T. Characteristics of Invasive Staphylococcus aureus in United Kingdom Neonatal Units. Pediatr. Infect. Dis. J. 2011, 30, 850–854. [Google Scholar] [CrossRef] [PubMed]
- Giannoni, E.; Dimopoulou, V.; Klingenberg, C.; Naver, L.; Nordberg, V.; Berardi, A.; El Helou, S.; Fusch, G.; Bliss, J.M.; Lehnick, D.; et al. Analysis of Antibiotic Exposure and Early-Onset Neonatal Sepsis in Europe, North America, and Australia. JAMA Netw. Open 2022, 5, e2243691. [Google Scholar] [CrossRef]
- Schrag, S.J.; Farley, M.M.; Petit, S.; Reingold, A.; Weston, E.J.; Pondo, T.; Hudson Jain, J.; Lynfield, R. Epidemiology of Invasive Early-Onset Neonatal Sepsis, 2005 to 2014. Pediatrics 2016, 138, e20162013. [Google Scholar] [CrossRef]
- Simonsen, K.A.; Anderson-Berry, A.L.; Delair, S.F.; Davies, H.D. Early-onset neonatal sepsis. Clin. Microbiol. Rev. 2014, 27, 21–47. [Google Scholar] [CrossRef] [PubMed]
- Giannoni, E.; Agyeman, P.K.; Stocker, M.; Posfay-Barbe, K.M.; Heininger, U.; Spycher, B.D.; Bernhard-Stirnemann, S.; Niederer-Loher, A.; Kahlert, C.R.; Donas, A.; et al. Neonatal Sepsis of Early Onset, and Hospital-Acquired and Community-Acquired Late Onset: A Prospective Population-Based Cohort Study. J. Pediatr. 2018, 201, 106–114.e4. [Google Scholar] [CrossRef]
- Walker, S.M. Long-term effects of neonatal pain. Semin. Fetal. Neonatal. Med. 2019, 24, 101005. [Google Scholar] [CrossRef]
- Reyman, M.; van Houten, M.A.; Watson, R.L.; Chu, M.; Arp, K.; de Waal, W.J.; Schiering, I.; Plotz, F.B.; Willems, R.J.L.; van Schaik, W.; et al. Effects of early-life antibiotics on the developing infant gut microbiome and resistome: A randomized trial. Nat. Commun. 2022, 13, 893. [Google Scholar] [CrossRef]
- Scott, F.I.; Horton, D.B.; Mamtani, R.; Haynes, K.; Goldberg, D.S.; Lee, D.Y.; Lewis, J.D. Administration of Antibiotics to Children Before Age 2 Years Increases Risk for Childhood Obesity. Gastroenterology 2016, 151, 120–129.e5. [Google Scholar] [CrossRef]
- Droste, J.H.; Wieringa, M.H.; Weyler, J.J.; Nelen, V.J.; Vermeire, P.A.; Van Bever, H.P. Does the use of antibiotics in early childhood increase the risk of asthma and allergic disease? Clin. Exp. Allergy 2000, 30, 1547–1553. [Google Scholar] [CrossRef] [PubMed]
- Zargari, I.; Adar, A.; Morag, I.; Pinhas-Hamiel, O.; Eyal, O.; Keidar, R.; Loewenthal, N.; Levy, M.; Dally-Gottfried, O.; Landau, Z.; et al. Early exposures and inherent factors in premature newborns are associated with type 1 diabetes. Pediatr. Res. 2022. [Google Scholar] [CrossRef]
- Urban-Chmiel, R.; Marek, A.; Stepien-Pysniak, D.; Wieczorek, K.; Dec, M.; Nowaczek, A.; Osek, J. Antibiotic Resistance in Bacteria-A Review. Antibiotics 2022, 11, 1079. [Google Scholar] [CrossRef]
- Mundal, H.S.; Ronnestad, A.; Klingenberg, C.; Stensvold, H.J.; Stordal, K. Antibiotic Use in Term and Near-Term Newborns. Pediatrics 2021, 148, e2021051339. [Google Scholar] [CrossRef] [PubMed]
- van der Weijden, B.M.; Achten, N.B.; Bekhof, J.; Evers, E.E.; Berk, M.; Kamps, A.W.A.; Rijpert, M.; Ten Tusscher, G.W.; van Houten, M.A.; Plotz, F.B. Multicentre study found that adherence to national antibiotic recommendations for neonatal early-onset sepsis was low. Acta Paediatr. 2021, 110, 791–798. [Google Scholar] [CrossRef]
- Cantey, J.B.; Baird, S.D. Ending the Culture of Culture-Negative Sepsis in the Neonatal ICU. Pediatrics 2017, 140, e20170044. [Google Scholar] [CrossRef]
- Fleiss, N.; Schwabenbauer, K.; Randis, T.M.; Polin, R.A. What’s new in the management of neonatal early-onset sepsis? Arch. Dis. Child Fetal. Neonatal. Ed. 2023, 108, 10–14. [Google Scholar] [CrossRef] [PubMed]
- Achten, N.B.; Klingenberg, C.; Benitz, W.E.; Stocker, M.; Schlapbach, L.J.; Giannoni, E.; Bokelaar, R.; Driessen, G.J.A.; Brodin, P.; Uthaya, S.; et al. Association of Use of the Neonatal Early-Onset Sepsis Calculator With Reduction in Antibiotic Therapy and Safety: A Systematic Review and Meta-analysis. JAMA Pediatr. 2019, 173, 1032–1040. [Google Scholar] [CrossRef] [PubMed]
- Snoek, L.; van Kassel, M.N.; Krommenhoek, J.F.; Achten, N.B.; Plotz, F.B.; van Sorge, N.M.; Brouwer, M.C.; van de Beek, D.; Bijlsma, M.W.; NOGBS Study Group. Neonatal early-onset infections: Comparing the sensitivity of the neonatal early-onset sepsis calculator to the Dutch and the updated NICE guidelines in an observational cohort of culture-positive cases. eClinicalMedicine 2022, 44, 101270. [Google Scholar] [CrossRef]
- Morris, R.; Jones, S.; Banerjee, S.; Collinson, A.; Hagan, H.; Walsh, H.; Thornton, G.; Barnard, I.; Warren, C.; Reid, J.; et al. Comparison of the management recommendations of the Kaiser Permanente neonatal early-onset sepsis risk calculator (SRC) with NICE guideline CG149 in infants ≥34 weeks’ gestation who developed early-onset sepsis. Arch. Dis. Child Fetal. Neonatal. Ed. 2020, 105, 581–586. [Google Scholar] [CrossRef]
- van Kassel, M.N.; de Boer, G.; Teeri, S.A.F.; Jamrozy, D.; Bentley, S.D.; Brouwer, M.C.; van der Ende, A.; van de Beek, D.; Bijlsma, M.W. Molecular epidemiology and mortality of group B streptococcal meningitis and infant sepsis in the Netherlands: A 30-year nationwide surveillance study. Lancet Microbe 2021, 2, e32–e40. [Google Scholar] [CrossRef]
- Lamagni, T.L.; Keshishian, C.; Efstratiou, A.; Guy, R.; Henderson, K.L.; Broughton, K.; Sheridan, E. Emerging trends in the epidemiology of invasive group B streptococcal disease in England and Wales, 1991–2010. Clin. Infect. Dis. 2013, 57, 682–688. [Google Scholar] [CrossRef]
- Le Doare, K.; O’Driscoll, M.; Turner, K.; Seedat, F.; Russell, N.J.; Seale, A.C.; Heath, P.T.; Lawn, J.E.; Baker, C.J.; Bartlett, L.; et al. Intrapartum Antibiotic Chemoprophylaxis Policies for the Prevention of Group B Streptococcal Disease Worldwide: Systematic Review. Clin. Infect. Dis. 2017, 65, S143–S151. [Google Scholar] [CrossRef]
- Prevention of Group B Streptococcal Early-Onset Disease in Newborns: ACOG Committee Opinion Summary, Number 782. Obstet. Gynecol. 2019, 134, e19–e40.
- The Dutch Society of Obstetrics and Gynaecology; The Dutch Pediatrics Association. Prevention and Treatment of Early-Onset Neonatal Infection (Adapted from NICE Guidelines); The Dutch Society of Obstetrics and Gynaecology: Utrecht, The Netherlands, 2017; pp. 1–97. [Google Scholar]
- Bedford Russell, A.R.; Kumar, R. Early onset neonatal sepsis: Diagnostic dilemmas and practical management. Arch. Dis. Child Fetal. Neonatal. Ed. 2015, 100, F350–F354. [Google Scholar] [CrossRef] [PubMed]
- Daniels, J.P.; Gray, J.; Pattison, H.M.; Gray, R.; Hills, R.K.; Khan, K.S.; Group, G.B.S.C. Intrapartum tests for group B streptococcus: Accuracy and acceptability of screening. BJOG 2011, 118, 257–265. [Google Scholar] [CrossRef]
- American Society for Microbiology. Guidelines for the Detection and Identification of Group B Streptococcus; American Society for Microbiology: Washington, NW, USA, 2020. [Google Scholar]
- Prevention of Early-onset Neonatal Group B Streptococcal Disease: Green-top Guideline No. 36. BJOG 2017, 124, e280–e305. [CrossRef]
- Kolkman, D.G.E.; Rijnders, M.E.B.; Wouters, M.; Dommelen, P.V.; de Groot, C.J.M.; Fleuren, M.A.H. Adherence to three different strategies to prevent early onset GBS infection in newborns. Women Birth 2020, 33, e527–e534. [Google Scholar] [CrossRef] [PubMed]
- Hansen, S.M.; Uldbjerg, N.; Kilian, M.; Sorensen, U.B. Dynamics of Streptococcus agalactiae colonization in women during and after pregnancy and in their infants. J. Clin. Microbiol. 2004, 42, 83–89. [Google Scholar] [CrossRef]
- Nederlandse Vereniging voor Kindergeneeskunde. Preventie en Behandeling van Early-Onset Neonatale Infecties. 2017. Available online: https://www.nvk.nl/themas/kwaliteit/richtlijnen/richtlijn?componentid=6881284& (accessed on 12 December 2022).
- Khalil, M.R.; Uldbjerg, N.; Thorsen, P.B.; Moller, J.K. Intrapartum PCR assay versus antepartum culture for assessment of vaginal carriage of group B streptococci in a Danish cohort at birth. PLoS ONE 2017, 12, e0180262. [Google Scholar] [CrossRef]
- Tazi, A.; Bellais, S.; Tardieux, I.; Dramsi, S.; Trieu-Cuot, P.; Poyart, C. Group B Streptococcus surface proteins as major determinants for meningeal tropism. Curr. Opin. Microbiol. 2012, 15, 44–49. [Google Scholar] [CrossRef]
- Zurn, K.; Lander, F.; Hufnagel, M.; Monecke, S.; Berner, R. Microarray Analysis of Group B Streptococci Causing Invasive Neonatal Early- and Late-onset Infection. Pediatr. Infect. Dis. J. 2020, 39, 449–453. [Google Scholar] [CrossRef]
- Fluegge, K.; Wons, J.; Spellerberg, B.; Swoboda, S.; Siedler, A.; Hufnagel, M.; Berner, R. Genetic differences between invasive and noninvasive neonatal group B streptococcal isolates. Pediatr. Infect. Dis. J. 2011, 30, 1027–1031. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.L. Genomic Insights Into the Distribution and Evolution of Group B Streptococcus. Front. Microbiol. 2019, 10, 1447. [Google Scholar] [CrossRef] [PubMed]
- Van Elzakker, E.; Yahiaoui, R.; Visser, C.; Oostvogel, P.; Muller, A.; Ho, Y.R.; Wu, J.J.; van Belkum, A. Epidemiology of and prenatal molecular distinction between invasive and colonizing group B streptococci in The Netherlands and Taiwan. Eur. J. Clin. Microbiol. Infect. Dis. 2009, 28, 921–928. [Google Scholar] [CrossRef]
- Almeida, A.; Rosinski-Chupin, I.; Plainvert, C.; Douarre, P.E.; Borrego, M.J.; Poyart, C.; Glaser, P. Parallel Evolution of Group B Streptococcus Hypervirulent Clonal Complex 17 Unveils New Pathoadaptive Mutations. mSystems 2017, 2, e00074-17. [Google Scholar] [CrossRef] [PubMed]
- Jamrozy, D.; Bijlsma, M.W.; de Goffau, M.C.; van de Beek, D.; Kuijpers, T.W.; Parkhill, J.; van der Ende, A.; Bentley, S.D. Increasing incidence of group B streptococcus neonatal infections in the Netherlands is associated with clonal expansion of CC17 and CC23. Sci. Rep. 2020, 10, 9539. [Google Scholar] [CrossRef]
- Chaguza, C.; Jamrozy, D.; Bijlsma, M.W.; Kuijpers, T.W.; van de Beek, D.; van der Ende, A.; Bentley, S.D. Population genomics of Group B Streptococcus reveals the genetics of neonatal disease onset and meningeal invasion. Nat. Commun. 2022, 13, 4215. [Google Scholar] [CrossRef] [PubMed]
- Baker, C.J.; Kasper, D.L. Correlation of maternal antibody deficiency with susceptibility to neonatal group B streptococcal infection. N. Engl. J. Med. 1976, 294, 753–756. [Google Scholar] [CrossRef]
- Fabbrini, M.; Rigat, F.; Rinaudo, C.D.; Passalaqua, I.; Khacheh, S.; Creti, R.; Baldassarri, L.; Carboni, F.; Anderloni, G.; Rosini, R.; et al. The Protective Value of Maternal Group B Streptococcus Antibodies: Quantitative and Functional Analysis of Naturally Acquired Responses to Capsular Polysaccharides and Pilus Proteins in European Maternal Sera. Clin. Infect. Dis. 2016, 63, 746–753. [Google Scholar] [CrossRef]
- Lin, F.Y.; Weisman, L.E.; Troendle, J.; Adams, K. Prematurity is the major risk factor for late-onset group B streptococcus disease. J. Infect. Dis. 2003, 188, 267–271. [Google Scholar] [CrossRef] [PubMed]
- Gori, A.; Harrison, O.B.; Mlia, E.; Nishihara, Y.; Chan, J.M.; Msefula, J.; Mallewa, M.; Dube, Q.; Swarthout, T.D.; Nobbs, A.H.; et al. Pan-GWAS of Streptococcus agalactiae Highlights Lineage-Specific Genes Associated with Virulence and Niche Adaptation. mBio 2020, 11, e00728-20. [Google Scholar] [CrossRef] [PubMed]
- Dzanibe, S.; Kwatra, G.; Adrian, P.V.; Kimaro-Mlacha, S.Z.; Cutland, C.L.; Madhi, S.A. Association between antibodies against group B Streptococcus surface proteins and recto-vaginal colonisation during pregnancy. Sci. Rep. 2017, 7, 16454. [Google Scholar] [CrossRef]
- Kwatra, G.; Adrian, P.V.; Shiri, T.; Buchmann, E.J.; Cutland, C.L.; Madhi, S.A. Serotype-specific acquisition and loss of group B streptococcus recto-vaginal colonization in late pregnancy. PLoS ONE 2014, 9, e98778. [Google Scholar] [CrossRef] [PubMed]
- Hillier, S.L.; Ferrieri, P.; Edwards, M.S.; Ewell, M.; Ferris, D.; Fine, P.; Carey, V.; Meyn, L.; Hoagland, D.; Kasper, D.L.; et al. A Phase 2, Randomized, Control Trial of Group B Streptococcus (GBS) Type III Capsular Polysaccharide-tetanus Toxoid (GBS III-TT) Vaccine to Prevent Vaginal Colonization With GBS III. Clin. Infect. Dis. 2019, 68, 2079–2086. [Google Scholar] [CrossRef] [PubMed]
- Absalon, J.; Simon, R.; Radley, D.; Giardina, P.C.; Koury, K.; Jansen, K.U.; Anderson, A.S. Advances towards licensure of a maternal vaccine for the prevention of invasive group B streptococcus disease in infants: A discussion of different approaches. Hum. Vaccin. Immunother. 2022, 18, 2037350. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, P.B.; Isbrucker, R.; Andrews, N.; Goldblatt, D.; Heath, P.T.; Izu, A.; Madhi, S.A.; Moulton, L.; Schrag, S.J.; Shang, N.; et al. Methodology for a correlate of protection for group B Streptococcus: Report from the Bill & Melinda Gates Foundation workshop held on 10 and 11 February 2021. Vaccine 2022, 40, 4283–4291. [Google Scholar]
- Shakib, J.; Buchi, K.; Smith, E.; Young, P.C. Management of newborns born to mothers with chorioamnionitis: Is it time for a kinder, gentler approach? Acad. Pediatr. 2015, 15, 340–344. [Google Scholar] [CrossRef]
- Kiser, C.; Nawab, U.; McKenna, K.; Aghai, Z.H. Role of guidelines on length of therapy in chorioamnionitis and neonatal sepsis. Pediatrics 2014, 133, 992–998. [Google Scholar] [CrossRef]
- Peng, C.C.; Chang, J.H.; Lin, H.Y.; Cheng, P.J.; Su, B.H. Intrauterine inflammation, infection, or both (Triple I): A new concept for chorioamnionitis. Pediatr. Neonatol. 2018, 59, 231–237. [Google Scholar] [CrossRef]
- van Leeuwen, L.; Fourie, E.; van den Brink, G.; Bekker, V.; van Houten, M. Biomarkers for the diagnosis of early onset neonatal sepsis: A systematic review and meta-analysis. Submitted. 2022. [Google Scholar]
- Howman, R.A.; Charles, A.K.; Jacques, A.; Doherty, D.A.; Simmer, K.; Strunk, T.; Richmond, P.C.; Cole, C.H.; Burgner, D.P. Inflammatory and haematological markers in the maternal, umbilical cord and infant circulation in histological chorioamnionitis. PLoS ONE 2012, 7, e51836. [Google Scholar] [CrossRef] [PubMed]
- Krueger, M.; Nauck, M.S.; Sang, S.; Hentschel, R.; Wieland, H.; Berner, R. Cord blood levels of interleukin-6 and interleukin-8 for the immediate diagnosis of early-onset infection in premature infants. Neonatology 2001, 80, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Froeschle, G.M.; Bedke, T.; Boettcher, M.; Huber, S.; Singer, D.; Ebenebe, C.U. T cell cytokines in the diagnostic of early-onset sepsis. Pediatr. Res. 2021, 90, 191–196. [Google Scholar] [CrossRef]
- Su, H.; Chang, S.S.; Han, C.M.; Wu, K.Y.; Li, M.C.; Huang, C.Y.; Lee, C.L.; Wu, J.Y.; Lee, C.C. Inflammatory markers in cord blood or maternal serum for early detection of neonatal sepsis-a systemic review and meta-analysis. J. Perinatol. 2014, 34, 268–274. [Google Scholar] [CrossRef]
- Eichberger, J.; Resch, B. Reliability of Interleukin-6 Alone and in Combination for Diagnosis of Early Onset Neonatal Sepsis: Systematic Review. Front. Pediatr. 2022, 10, 840778. [Google Scholar] [CrossRef]
- Mithal, L.B.; Palac, H.L.; Yogev, R.; Ernst, L.M.; Mestan, K.K. Cord Blood Acute Phase Reactants Predict Early Onset Neonatal Sepsis in Preterm Infants. PLoS ONE 2017, 12, e0168677. [Google Scholar] [CrossRef] [PubMed]
- Seliem, W.; Sultan, A.M. Presepsin as a predictor of early onset neonatal sepsis in the umbilical cord blood of premature infants with premature rupture of membranes. Pediatr. Int. 2018, 60, 428–432. [Google Scholar] [CrossRef]
- Berner, R.; Furll, B.; Stelter, F.; Drose, J.; Muller, H.P.; Schutt, C. Elevated levels of lipopolysaccharide-binding protein and soluble CD14 in plasma in neonatal early-onset sepsis. Clin. Diagn. Lab. Immunol. 2002, 9, 440–445. [Google Scholar] [CrossRef]
- Klingenberg, C.; Kornelisse, R.F.; Buonocore, G.; Maier, R.F.; Stocker, M. Culture-Negative Early-Onset Neonatal Sepsis—At the Crossroad Between Efficient Sepsis Care and Antimicrobial Stewardship. Front. Pediatr. 2018, 6, 285. [Google Scholar] [CrossRef] [PubMed]
- Kellogg, J.A.; Ferrentino, F.L.; Goodstein, M.H.; Liss, J.; Shapiro, S.L.; Bankert, D.A. Frequency of low level bacteremia in infants from birth to two months of age. Pediatr. Infect. Dis. J. 1997, 16, 381–385. [Google Scholar] [CrossRef]
- Garcia-Prats, J.A.; Cooper, T.R.; Schneider, V.F.; Stager, C.E.; Hansen, T.N. Rapid detection of microorganisms in blood cultures of newborn infants utilizing an automated blood culture system. Pediatrics 2000, 105, 523–527. [Google Scholar] [CrossRef] [PubMed]
- Huber, S.; Hetzer, B.; Crazzolara, R.; Orth-Holler, D. The correct blood volume for paediatric blood cultures: A conundrum? Clin. Microbiol. Infect. 2020, 26, 168–173. [Google Scholar] [CrossRef]
- Gaur, A.; Giannini, M.A.; Flynn, P.M.; Boudreaux, J.W.; Mestemacher, M.A.; Shenep, J.L.; Hayden, R.T. Optimizing blood culture practices in pediatric immunocompromised patients: Evaluation of media types and blood culture volume. Pediatr. Infect. Dis. J. 2003, 22, 545–552. [Google Scholar] [CrossRef] [PubMed]
- Ohnishi, T.; Kamimaki, I.; Kobayashi, R.; Nakatogawa, K.; Amemiya, A.; Mishima, Y.; Asato, S.; Shikoro, N.; Nakazawa, M. Verification of blood volume for blood culture and detection rate in pediatrics. J. Infect. Chemother. 2020, 26, 471–474. [Google Scholar] [CrossRef]
- Quinones Cardona, V.; Lowery, V.; Cooperberg, D.; Anday, E.K.; Carey, A.J. Eliminating Contamination in Umbilical Cord Blood Culture Sampling for Early-Onset Neonatal Sepsis. Front. Pediatr. 2021, 9, 794710. [Google Scholar] [CrossRef]
- Dierikx, T.H.; van Kaam, A.; de Meij, T.G.J.; de Vries, R.; Onland, W.; Visser, D.H. Umbilical cord blood culture in neonatal early-onset sepsis: A systematic review and meta-analysis. Pediatr. Res. 2022, 92, 362–372. [Google Scholar] [CrossRef] [PubMed]
- Gude, S.S.; Peddi, N.C.; Vuppalapati, S.; Venu Gopal, S.; Marasandra Ramesh, H.; Gude, S.S. Biomarkers of Neonatal Sepsis: From Being Mere Numbers to Becoming Guiding Diagnostics. Cureus 2022, 14, e23215. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wang, Z.; Zhang, M.; Lou, Z.; Deng, J.; Li, Q. Diagnostic value of mean platelet volume for neonatal sepsis: A systematic review and meta-analysis. Medicine 2020, 99, e21649. [Google Scholar] [CrossRef]
- O’Reilly, D.; Murphy, C.A.; Drew, R.; El-Khuffash, A.; Maguire, P.B.; Ainle, F.N.; Mc Callion, N. Platelets in pediatric and neonatal sepsis: Novel mediators of the inflammatory cascade. Pediatr. Res. 2022, 91, 359–367. [Google Scholar] [CrossRef]
- Eichberger, J.; Resch, E.; Resch, B. Diagnosis of Neonatal Sepsis: The Role of Inflammatory Markers. Front. Pediatr. 2022, 10, 840288. [Google Scholar] [CrossRef]
- Hincu, M.A.; Zonda, G.I.; Stanciu, G.D.; Nemescu, D.; Paduraru, L. Relevance of Biomarkers Currently in Use or Research for Practical Diagnosis Approach of Neonatal Early-Onset Sepsis. Children 2020, 7, 309. [Google Scholar] [CrossRef] [PubMed]
- Balayan, S.; Chauhan, N.; Chandra, R.; Kuchhal, N.K.; Jain, U. Recent advances in developing biosensing based platforms for neonatal sepsis. Biosens. Bioelectron. 2020, 169, 112552. [Google Scholar] [CrossRef]
- Jyoti, A.; Kumar, S.; Kumar Srivastava, V.; Kaushik, S.; Govind Singh, S. Neonatal sepsis at point of care. Clin. Chim. Acta 2021, 521, 45–58. [Google Scholar] [CrossRef] [PubMed]
- Tiozzo, C.; Mukhopadhyay, S. Noninfectious influencers of early-onset sepsis biomarkers. Pediatr. Res. 2022, 91, 425–431. [Google Scholar] [CrossRef]
- Dongen, O.R.E.; van Leeuwen, L.M.; de Groot, P.K.; Vollebregt, K.; Schiering, I.; Wevers, B.A.; Euser, S.M.; van Houten, M.A. Umbilical Cord Procalcitonin to Detect Early-Onset Sepsis in Newborns: A Promising Biomarker. Front. Pediatr. 2021, 9, 779663. [Google Scholar] [CrossRef]
- Poggi, C.; Lucenteforte, E.; Petri, D.; De Masi, S.; Dani, C. Presepsin for the Diagnosis of Neonatal Early-Onset Sepsis: A Systematic Review and Meta-analysis. JAMA Pediatr. 2022, 176, 750–758. [Google Scholar] [CrossRef] [PubMed]
- van Maldeghem, I.; Nusman, C.M.; Visser, D.H. Soluble CD14 subtype (sCD14-ST) as biomarker in neonatal early-onset sepsis and late-onset sepsis: A systematic review and meta-analysis. BMC Immunol. 2019, 20, 17. [Google Scholar] [CrossRef]
- Maddaloni, C.; De Rose, D.U.; Santisi, A.; Martini, L.; Caoci, S.; Bersani, I.; Ronchetti, M.P.; Auriti, C. The Emerging Role of Presepsin (P-SEP) in the Diagnosis of Sepsis in the Critically Ill Infant: A Literature Review. Int. J. Mol. Sci. 2021, 22, 12154. [Google Scholar] [CrossRef]
- Sinha, M.; Jupe, J.; Mack, H.; Coleman, T.P.; Lawrence, S.M.; Fraley, S.I. Emerging Technologies for Molecular Diagnosis of Sepsis. Clin. Microbiol. Rev. 2018, 31, e00089-17. [Google Scholar] [CrossRef]
- Pammi, M.; Flores, A.; Versalovic, J.; Leeflang, M.M. Molecular assays for the diagnosis of sepsis in neonates. Cochrane Database Syst. Rev. 2017, 2, CD011926. [Google Scholar] [CrossRef]
- Yu, R.; Zhou, Q.; Jiang, S.; Mei, Y.; Wang, M. Combination of 16S rRNA and procalcitonin in diagnosis of neonatal clinically suspected sepsis. J. Int. Med. Res. 2020, 48, 300060519892418. [Google Scholar] [CrossRef]
- Stranak, Z.; Berka, I.; Korcek, P.; Urbanek, J.; Laznickova, T.; Stanek, L. Bacterial DNA detection in very preterm infants assessed for risk of early onset sepsis. J. Perinat. Med. 2022, 50, 356–362. [Google Scholar] [CrossRef] [PubMed]
- Budding, A.E.; Hoogewerf, M.; Vandenbroucke-Grauls, C.M.; Savelkoul, P.H. Automated Broad-Range Molecular Detection of Bacteria in Clinical Samples. J. Clin. Microbiol. 2016, 54, 934–943. [Google Scholar] [CrossRef] [PubMed]
- Hayes, R.; Hartnett, J.; Semova, G.; Murray, C.; Murphy, K.; Carroll, L.; Plapp, H.; Hession, L.; O’Toole, J.; McCollum, D.; et al. Neonatal sepsis definitions from randomised clinical trials. Pediatr. Res. 2021. [Google Scholar] [CrossRef] [PubMed]
- Escobar, G.J.; Puopolo, K.M.; Wi, S.; Turk, B.J.; Kuzniewicz, M.W.; Walsh, E.M.; Newman, T.B.; Zupancic, J.; Lieberman, E.; Draper, D. Stratification of risk of early-onset sepsis in newborns ≥ 34 weeks’ gestation. Pediatrics 2014, 133, 30–36. [Google Scholar] [CrossRef]
- Puopolo, K.M.; Draper, D.; Wi, S.; Newman, T.B.; Zupancic, J.; Lieberman, E.; Smith, M.; Escobar, G.J. Estimating the probability of neonatal early-onset infection on the basis of maternal risk factors. Pediatrics 2011, 128, e1155-63. [Google Scholar] [CrossRef]
- Benitz, W.E.; Achten, N.B. Technical assessment of the neonatal early-onset sepsis risk calculator. Lancet Infect. Dis. 2021, 21, e134–e140. [Google Scholar] [CrossRef] [PubMed]
- Moons, K.G.; Kengne, A.P.; Grobbee, D.E.; Royston, P.; Vergouwe, Y.; Altman, D.G.; Woodward, M. Risk prediction models: II. External validation, model updating, and impact assessment. Heart 2012, 98, 691–698. [Google Scholar] [CrossRef]
- Jenkins, D.A.; Martin, G.P.; Sperrin, M.; Riley, R.D.; Debray, T.P.A.; Collins, G.S.; Peek, N. Continual updating and monitoring of clinical prediction models: Time for dynamic prediction systems? Diagn. Progn. Res. 2021, 5, 1. [Google Scholar] [CrossRef]
- Achten, N.B.; Plotz, F.B.; Klingenberg, C.; Stocker, M.; Bokelaar, R.; Bijlsma, M.; Giannoni, E.; van Rossum, A.M.C.; Benitz, W.E. Stratification of Culture-Proven Early-Onset Sepsis Cases by the Neonatal Early-Onset Sepsis Calculator: An Individual Patient Data Meta-Analysis. J. Pediatr. 2021, 234, 77–84.e8. [Google Scholar] [CrossRef]
- Berardi, A.; Bedetti, L.; Spada, C.; Lucaccioni, L.; Frymoyer, A. Serial clinical observation for management of newborns at risk of early-onset sepsis. Curr. Opin. Pediatr. 2020, 32, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Vatne, A.; Klingenberg, C.; Oymar, K.; Ronnestad, A.E.; Manzoni, P.; Rettedal, S. Reduced Antibiotic Exposure by Serial Physical Examinations in Term Neonates at Risk of Early-onset Sepsis. Pediatr. Infect. Dis. J. 2020, 39, 438–443. [Google Scholar] [CrossRef] [PubMed]
- Berardi, A.; Buffagni, A.M.; Rossi, C.; Vaccina, E.; Cattelani, C.; Gambini, L.; Baccilieri, F.; Varioli, F.; Ferrari, F. Serial physical examinations, a simple and reliable tool for managing neonates at risk for early-onset sepsis. World J. Clin. Pediatr. 2016, 5, 358–364. [Google Scholar] [CrossRef]
- Puopolo, K.M.; Benitz, W.E.; Zaoutis, T.E.; Committee on Fetus and Newborn; Committee on Infectious Diseases; Cummings, J.; Juul, S.; Hand, I.; Eichenwald, E.; Poindexter, B.; et al. Management of Neonates Born at ≥35 0/7 Weeks’ Gestation With Suspected or Proven Early-Onset Bacterial Sepsis. Pediatrics 2018, 142, e20182894. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nusman, C.M.; Snoek, L.; van Leeuwen, L.M.; Dierikx, T.H.; van der Weijden, B.M.; Achten, N.B.; Bijlsma, M.W.; Visser, D.H.; van Houten, M.A.; Bekker, V.; et al. Group B Streptococcus Early-Onset Disease: New Preventive and Diagnostic Tools to Decrease the Burden of Antibiotic Use. Antibiotics 2023, 12, 489. https://doi.org/10.3390/antibiotics12030489
Nusman CM, Snoek L, van Leeuwen LM, Dierikx TH, van der Weijden BM, Achten NB, Bijlsma MW, Visser DH, van Houten MA, Bekker V, et al. Group B Streptococcus Early-Onset Disease: New Preventive and Diagnostic Tools to Decrease the Burden of Antibiotic Use. Antibiotics. 2023; 12(3):489. https://doi.org/10.3390/antibiotics12030489
Chicago/Turabian StyleNusman, Charlotte M., Linde Snoek, Lisanne M. van Leeuwen, Thomas H. Dierikx, Bo M. van der Weijden, Niek B. Achten, Merijn W. Bijlsma, Douwe H. Visser, Marlies A. van Houten, Vincent Bekker, and et al. 2023. "Group B Streptococcus Early-Onset Disease: New Preventive and Diagnostic Tools to Decrease the Burden of Antibiotic Use" Antibiotics 12, no. 3: 489. https://doi.org/10.3390/antibiotics12030489
APA StyleNusman, C. M., Snoek, L., van Leeuwen, L. M., Dierikx, T. H., van der Weijden, B. M., Achten, N. B., Bijlsma, M. W., Visser, D. H., van Houten, M. A., Bekker, V., de Meij, T. G. J., van Rossem, E., Felderhof, M., & Plötz, F. B. (2023). Group B Streptococcus Early-Onset Disease: New Preventive and Diagnostic Tools to Decrease the Burden of Antibiotic Use. Antibiotics, 12(3), 489. https://doi.org/10.3390/antibiotics12030489







