Abstract
The number of pharmacokinetic (PK) models of meropenem is increasing. However, the daily role of these PK models in the clinic remains unclear, especially for critically ill patients. Therefore, we evaluated the published meropenem models on real-world ICU data to assess their suitability for use in clinical practice. All models were built in NONMEM and evaluated using prediction and simulation-based diagnostics for the ability to predict the subsequent meropenem concentrations without plasma concentrations (a priori), and with plasma concentrations (a posteriori), for use in therapeutic drug monitoring (TDM). Eighteen PopPK models were included for evaluation. The a priori fit of the models, without the use of plasma concentrations, was poor, with a prediction error (PE)% of the interquartile range (IQR) exceeding the ±30% threshold. The fit improved when one to three concentrations were used to improve model predictions for TDM purposes. Two models were in the acceptable range with an IQR PE% within ±30%, when two or three concentrations were used. The role of PK models to determine the starting dose of meropenem in this population seems limited. However, certain models might be suitable for TDM-based dose adjustment using two to three plasma concentrations.
1. Introduction
Meropenem is a broad-spectrum β-lactam antibiotic with an extensive and strong antibacterial activity, especially for drug-resistant Gram-negative bacteria [1,2]. It is often prescribed to treat patients with severe infections in intensive care units (ICU) [3,4,5]. The pharmacokinetic/pharmacodynamics (PK/PD) index that best predicts in vivo antimicrobial activity is the time during which the unbound plasma concentration remains above the minimum inhibitory concentration (MIC) of the pathogen (fT > MIC) [6,7]. A 1-log kill bacterial reduction is associated with a fT > MIC of at least 40% for meropenem [8,9]. However, this is still under debate, as some studies have suggested that a higher PK/PD target of 100% fT > 1-4x MIC is more appropriate for critically ill patients [10,11]. Currently, the standard dosing regimens are based solely on renal function and might not provide the optimal treatment for ICU patients. The variability in organ function between patients, but also within patients during their ICU stay, is relatively high compared to non-ICU patients. This may affect the PK parameters (e.g., the clearance) of antibiotics that are predominantly excreted renally, such as β-lactam antibiotics. Therefore, a standard meropenem dosing regimen may lead to meropenem concentrations outside of the therapeutic window [12,13].
One method to increase the treatment efficacy is through personalized dosing, for example via model-informed precision dosing (MIPD). The latter uses mathematical models, such as population pharmacokinetic (PopPK) models, to predict drug concentrations based on individual patient characteristics and previous drug concentrations. However, these PopPK models must first be validated in the target population to determine whether they can provide accurate drug concentration predictions. A suitable PopPK model can be used for a priori meropenem concentration prediction, which is based on individual patient characteristics to determine the optimal starting dose, but does not make use of measured drug concentrations [14]. Subsequently, when drug concentrations are available from therapeutic drug monitoring (TDM), this data can be used to further individualize and optimize the PopPK models for more precise predictions and dose adjustments [15].
Meropenem MIPD is gaining attention in clinical practice, and many meropenem PopPK models have been published by different medical centers around the world [16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41]. In addition to adult PopPK models, there are models developed for special populations such as pediatric and neonatal populations, [42,43,44,45,46,47,48,49,50] patients with augmented renal clearance (ARC) and patients with renal replacement therapy (RRT) [51,52,53,54,55,56,57,58]. The population used to develop these models varied widely, both in patient numbers and characteristics. Hence, external evaluation is of the utmost importance before applying these models to new target populations. Although several studies have evaluated pharmacokinetic models of meropenem, the patients included in these studies had a relatively sparse sampling of meropenem concentrations [59,60,61,62].
The aim of the study was to evaluate the applicability of published models to real-world ICU patients in Europe using the MIPD approach.
2. Results
2.1. Patient Characteristics
A total of 20 patients were included. The patient characteristics are summarized in Table 1. A wide range in white blood cell count (WBC), C-reactive protein (CRP), serum creatinine, and fluid balance were observed between the patients. About one-third of the patients (6/20) received renal replacement therapy (RRT) during meropenem treatment.

Table 1.
Patient baseline characteristics.
2.2. Population Pharmacokinetic Model Selection
A total of 18 models were included for evaluation after the literature search and article screening. The summary of these models can be found in Table 2. The meropenem PopPK models included in this study had many differences in model structure (e.g., number of compartments) as well as included covariates. Most meropenem models (13/18) were two-compartment pharmacokinetic models, and most (15/18) included creatinine-related covariates on meropenem clearance—creatinine clearance Cockcroft–Gault (CRCL(CG)), estimated glomerular filtration rate (eGFR), modification of diet in renal disease (MDRD) and serum creatinine (SCR), followed by weight on the volume of distribution—total body weight (TBW) and ideal body weight (IBW) (8/18). The covariates albumin, C-reactive protein (CRP), renal replacement therapy (RRT) and APACHE II score were model specific (Table 2).

Table 2.
Characteristics of included meropenem population pharmacokinetic models.
2.3. Model Evaluations
2.3.1. VPC Results of the Models
Visual predictive checks (VPCs) were used to visually evaluate the fit of the individual models. The VPC results of the eighteen models are shown in Figure 1. The concentration range observed in our clinical data was larger than expected from the model. All models showed an under prediction of the variability. Median peak concentrations (time after infusion 0–1 h) were underestimated in ten models (model 1, 2, 4, 8, 10, 11, 12, 13, 14, 18), where model 12 and 14 performed the worst. In contrast, three models (models 7, 9 and 17) slightly overestimated the median peak concentration. The fit of the median trough concentrations was better than that of the peak concentration, with six models (models 2, 11, 12, 13, 14, 16) underestimating the trough concentrations and one model (model 7) overestimating the trough concentration. For the median concentrations between the peak and trough period (time after infusion 1–6 h), five models (model 3, 7, 9, 17, 18) overestimated the observed concentrations and 1 model (model 12) underestimated the observed concentrations. Overall, models 5, 6 and 15 outperformed the other models based on the VPC fit results for median concentrations. However, these models have relatively wide 95% confidence intervals (shaded area) with respect to the other models.
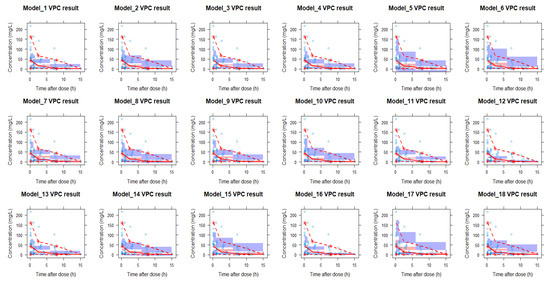
Figure 1.
Observed meropenem concentration–time data and the visual predictive check (VPC) of the 18 models. The blue brackets are the observed concentrations. The red line is the observed median and the two blue lines are the 5th and 95th percentiles of the observed data. The red shaded area is the 95% CI of the model predicted median and the purple shaded areas are the 95% CIs of the model-predicted 5th and 95th percentiles. Red lines above the shaded areas represents model underprediction and red lines under the respective areas represents overprediction of the models at those intervals Additionally, VPCs were stratified (Figure S1) on whether patients received renal replacement therapy or not (RRT versus non-RRT). Overall, the observed concentrations in the non-RRT group were lower than in the RRT group. In the non-RRT group, the median peak concentrations (at time after infusion 0–1 h) were underestimated for six models (model 2, 8, 10, 11, 12, 14, 18) and overestimated for three models (models 7, 9 and 17). Median trough concentrations (time after 6–15 h post-infusion) showed a better fit, with models 11 and 18 underestimating concentrations and model 7 overestimating concentrations. For the median concentrations between the peak and trough (time after infusion 1–6 h), thirteen models (model 1, 3, 4, 6, 7, 8, 9, 11, 13, 15, 16, 17, 18) overestimated the observed concentrations while one model (model 12) underestimated the observed concentrations. For the VPC plot of the RRT patients, the median peak concentrations (time after infusion 0–1 h) were underestimated in eight models (model 1, 2, 4, 10, 11, 12, 13, 18). For the median intermediate time concentrations (time after infusion 1–6 h) and median trough concentrations (time after infusion 6–15 h), all but model 14 and 17 underestimated the observed concentrations. Compared with the combined VPC analysis, model 5 performed best in the non-RRT group while model 14 performed best in the RRT group.
2.3.2. Goodness-of-fit (GoF) Plots
The population prediction versus observation GoF plots are shown in Figure 2. The population-predicted concentrations versus the observed concentrations were not symmetrically distributed around the unity line (where the prediction is equal to the observation). Overall, models 1 and 3 had relatively good fits, while models 7, 8, 9, 15, 16 and 18 showed relatively poor fits. We found that population-predicted concentrations were more likely to overestimate concentrations below 10 mg/L and underestimate concentrations above 50 mg/L. Of the eighteen models, models 2, 10, 12 and 14 showed a tendency to underestimate the observed concentrations, whereas models 7, 9 and 17 showed a tendency to overestimate concentrations.
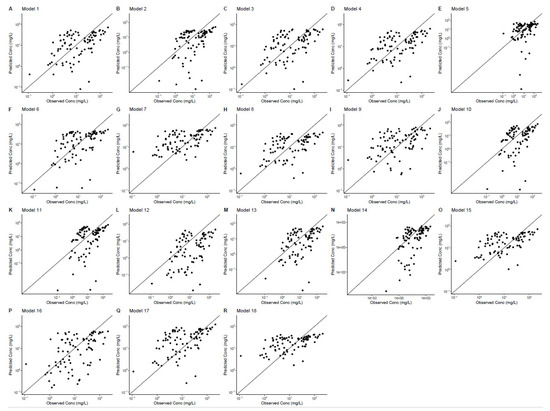
Figure 2.
The goodness-of-fit plots of the 18 models. Population predictive concentration (y-axis) versus observed concentration (x-axis).
The individual prediction versus observation GOF plots are shown in Figure 3. The GoF plots of the individual predictions showed a major improvement compared to the population predictions. Most of the points in Figure 4 were evenly distributed around the unity line. Among these models, models 4, 10 and 13 outperformed the other models and showed a good match between predicted and observed concentrations. Model 4, 10 and 13 were all two-compartment models. Both these three models used CRCL (CG) as a covariate on CL. In addition, model 10 used an APACHE score as covariate on Q and model 13 used total body weight as a covariate on V1.
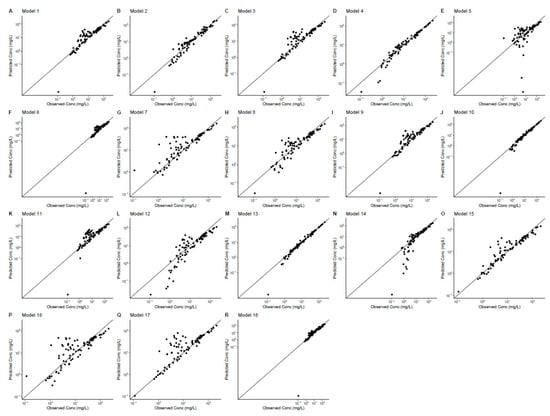
Figure 3.
Individual predictive goodness-of-fit plots for eighteen models. Individual-predicted concentrations (y-axis) versus observed concentrations.
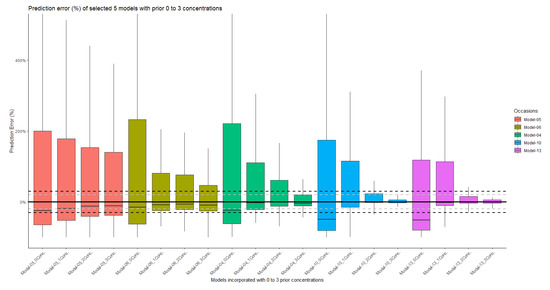
Figure 4.
Prediction errors of model 5, 6, 4, 10 and 13. For each model, none, one, two or three plasma concentrations were used to improve the model fit. The grey dashed line is the y = ±20%. The black dashed line is the y = ±30%.
2.3.3. Bias and Precision of the Population and Individual Predictions
The summary of the population prediction error (PEpred%) for each model is shown in Figure S2. The PE% range of the population prediction between the models was large. Overall, most models seem to underestimate the concentration. The individual prediction errors (PEipred%) are shown in Figure S3, which were similar to the results of Figure 3, where model 4, 10 and 13 performed better than the other models. By combining the performance VPC and GoF plot, we chose five models (model 5, 6, 4, 10, 13) as representative models to compare the population prediction error (PEpred%, with no meropenem plasma samples incorporated into model) and individual prediction error using different number of concentrations (PEipred1–3%, one to three meropenem plasma samples used to optimize the model). The results in Figure 4 showed that with the use of two or more prior concentrations in model 10 and 13, the interquartile range (IQR) of PEipred2–3% were within the acceptable range of ±30%. On the other hand, none of the models had a population PE% IQR within ±30% when no plasma concentrations were available to improve the fit. More detailed information for the individual prediction error can be found in Figure S4–S7.
2.4. Simulation of Pharmacokinetic Profiles
To evaluate the differences in the pharmacokinetic profiles of the models, simulations were performed with each model for three standard patients with different renal functions (normal renal function, enhanced renal function, and impaired renal function). The results of the simulations of steady-state concentrations (30–40 h after dose) are shown in Figure 5. In patients with normal renal function (Figure 5a), the simulated steady-state peak meropenem concentrations ranged from 25 to 78 mg/L, while the measured steady-state trough concentrations ranged from 0.07 to 9 mg/L. For the simulation of patients with enhanced renal function (Figure 5b), all but three models (model 5, model 9 and model 16) showed lower concentrations compared to the patients with normal renal function, with steady trough concentration ranges from 0.003 to 7.1 mg/L. For simulations in patients with impaired renal function (Figure 5c), drug concentrations were higher in patients with impaired renal function than in patients with normal renal function, with peak concentrations ranging from 42–127 mg/L and trough concentrations ranging from 2.4–45 mg/L.
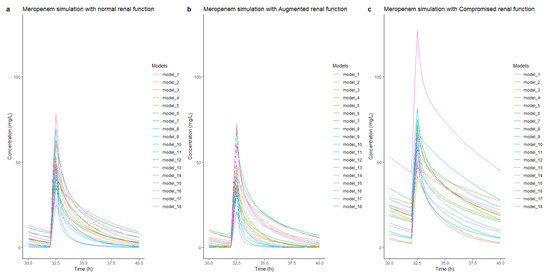
Figure 5.
Steady-state concentrations and time simulation of the three typical patients with different renal functions: normal renal function (a), augmented renal function (b), and impaired renal function (c). The simulations were all based on a standard patient (55 years, 180 cm, 80 kg, APACHE II score 24, albumin 25 g/L, serum creatinine 100 umol/L). All received a meropenem dose of 1 g q8 h for 40 h. Steady-state concentrations were shown at the fourth dose (30–40 h after first dose).
3. Discussion
This is the first study of meropenem MIPD applied to real-world critically ill adult patients in Europe. According to our results, none of the eighteen models seem to be able to provide relatively accurate initial dose guidance without plasma concentrations using only the model with the patient characteristics as covariates. For TDM-based dose adjustment, only two models (models 10 and 13) showed results within the acceptable range of ±30%, although this required at least two concentrations to be included. This demonstrates the importance of model validation prior to use. To guide meropenem dosing in critically ill patients, prior drug concentrations may be necessary to provide adequate predictions.
The results of the simulation of these models showed that the predictive performance of the pharmacokinetic models of meropenem varied widely. Although most of these models were based on critically ill patients, the model structure and associated covariates were diverse. Protein binding would most likely not be a major factor as only ~2% is bound to plasma proteins [63]. Based on the results of the simulation, the effect of increased renal clearance on meropenem concentrations appeared to be less than that of impaired renal function. The greater emphasis on impaired renal function in these models may be due to the fact that patients in these studies were more likely to have a decreased rather than an increased renal function compared with normal individuals. As shown in Table 2, although the creatinine clearance in the different studies ranged from 3–357 mL/min, the median value of renal clearance in these models ranged from 30 to 100 mL/min, which is lower than normal renal function. Most models implemented a form of creatinine clearance as a covariate on meropenem clearance (e.g., MDRD, CRCL Cockcroft–Gault, CKD-EPI). However, these estimations are not a good representation of the actual creatinine clearance in critically ill ICU patients. More precise estimation methods for renal clearance might further reduce model misspecification [64].
The VPC results and population prediction versus observation GoF plots showed that the models provided a poor fit in the absence of information regarding individual drug concentrations. This suggested that these models could not accurately guide the initial doses in our patients. Although model 1, 5, 6, 8, 11 and 13 have been externally validated in other studies [51,59,60,61], the models were not able to fit our data well. This might be due to possible differences in our patient baseline/characteristics. In our study, our patients appeared to be divided into two groups, one with relatively high concentrations and the other with relatively low concentrations. However, the variability/dispersion of concentrations in our study could not be differentiated by using patients’ renal clearance or any of the other covariates in the published models. This may explain the underperformance of all models and the greater likelihood of overestimating concentrations below 10 mg/L and underestimating concentrations above 50 mg/L in the population. The fit of the models using individual plasma concentrations showed a vast improvement. This suggested that some models may be suitable for TDM-based dose adjustment. However, only a small number of models showed good predictive performance. It is therefore of utmost importance to validate the model on the intended target population.
The results of the predictive power accuracy analysis of the five most representative models were consistent with those of the VPC and GoF plots. None of these models had good a priori predictive power to discriminate between potentially high- or low-concentration groups in our ICU population. Therefore, we should be cautious about using the current PopPK models to guide individualized meropenem dosing in ICU patients during the initial dosing phase in the absence of meropenem concentrations. Without samples, the range of the prediction error was very large, ranging from −80% to 500%. However, when combined with TDM, the range of PE% decreased severely. Two models (model 10 and 13) performed the best in our study. These two models showed prediction errors within an acceptable range (PE% IQR within ±30%) when at least two concentrations were available. This might indicate that dense sampling (at least two samples per dosing occasion) for meropenem TDM in critically ill patients might be necessary to have adequate predictions and therefore more reliable dose-adjustment recommendations.
Our results were similar to those of Yang N. et al. [62], who showed that the current models were not suitable for daily meropenem dosing guidance for ICU patients. However, there were still some differences. First, the characteristics of ICU patients in hospitals in the Netherlands may differ from those in Asian hospitals. This might explain the differences in PE% range for models which were evaluated in both studies (model 1, 5, 6, 11, 13). In addition, the blood samples in our dataset were sampled more densely, which provided additional areas of the pharmacokinetic profile of meropenem. In the model prediction analysis, up to three plasma concentrations were available to improve the model fit and compare model performance. Lastly, our study included additional models for evaluation, and since we used NONMEM software for coding, we only included parametric models to ensure reliable results. The included models were all developed in a population in the ICU to reduce the amount of extrapolation to our population of critically ill ICU patients.
In summary, the models that were available from the literature performed poorly in our population, especially in the absence of individual meropenem concentrations, hence implying that MIPD is not suitable for guiding patients’ doses based purely on model and patient characteristics. Hence, it will most likely not perform well at initiation of the treatment when no meropenem concentrations are available. The number of patients were limited; however, if the fit is poor for these real-world patients, it is unlikely that the performance of the total population would be adequate. However, two of these models provided predictions in the acceptable range of ±30% when at least two or more concentrations were used to tailor the model fit. The use for TDM purposes, by taking meropenem concentrations into account, might be suitable. However, this warrants further confirmation, for example via a prospective study. The study also confirms the importance of TDM and model validation for the implementation of meropenem PopPK models in ICU patients.
Our study had some limitations. First, the sample size was limited and data was collected on one dosing occasion. Therefore, the effect of variability between occasions could not be taken into account. Second, since this study was limited to parametric models, future work can be extended by nonparametric models.
4. Materials and Methods
4.1. Clinical Data
A total of 86 blood samples from 20 ICU patients, obtained in the EXPAT trial (Netherlands Trial Registry, NTR 5632), was used for model external validation [13]. The study protocol was approved by the Erasmus MC Medical Ethics Committee (EXPAT, NL53551.078.15) and informed consent was obtained from all patients or their legal representatives [13]. All enrolled patients were admitted to the ICU between January 2016 and June 2017 and received intermittent intravenous meropenem (2–4 g per day) for the treatment of an infection. On day 2 after the start of meropenem treatment, five venous blood samples were collected: 15–30 min before the next dose infusion (trough concentration, Cmin), 15–30 min after the end of infusion (peak concentration, Cmax), 1 h and 3 h after the end of infusion, and at 15–30 min before the administration of the next dose (second Cmin). In addition to the samples used for pharmacokinetic analysis, the following additional data were collected: patient demographics (age, sex, and actual/ideal body weight), patients’ diagnosis, renal replacement therapy (type of RRT and RRT session timetables), fluid balance (input/output), APACHE II and SOFA score, and biochemistry results. Creatinine clearance was calculated using the Cockcroft–Gault (CG) equation [65], glomerular filtration rate with MDRD [66], and CKD-EPI formula [67]. All this information was recorded at baseline (prior to sampling) and on the day of sampling.
Meropenem concentrations in blood samples were quantified as previously described [68]. All samples were thawed 30 min before analysis and analyzed using an ultra-performance liquid chromatography-tandem mass spectrometry (UPLC-MS/MS) method. A total of 50 μL of plasma was mixed with 150 μL of formic acid and 800 μL of internal standard solution. After samples were centrifuged and transferred to auto-sampler vial, 4 μL of extract was injected into the UPLC-MS/MS system. The lower limit of quantification (LLOQ) and upper limit of quantification (ULOQ) were 0.174 mg/L and 34.8 mg/L, respectively.
4.2. Population Pharmacokinetic Model Selection
A literature search was conducted (up to June 2022) on PubMed and Embase database to assess the available literature on meropenem PopPK models in adult ICU patients. The models in the publications were manually screened. The inclusion criteria were: parametric population pharmacokinetic models, adults and ICU patients, PK model code or sufficient information to rebuild the model in NONMEM. The exclusion criteria were: nonparametric models, pediatric or neonatal patient population models, burn patient population models, steady-state models missing volume of distribution parameter and some other models that use covariates that are not available in our population. Detailed search strategy can be found in Supplementary Materials (Text S1). All the selected meropenem models were encoded and analyzed using NONMEM® 7.4 (Icon Development Solutions, Hanover, MD, USA).
4.3. Model Evaluations
4.3.1. VPC Results of the Models
The global fit of the population pharmacokinetic models were evaluated using visual predictive checks (VPCs) generated in Perl speaks NONMEM (PsN) (version 4.7.0) [69], and the data were later analyzed using the Xpose4 R package (version 1.0.1) in R (version 4.0.5). VPCs were further analyzed by stratifying patients on whether or not they received renal replacement therapy (RRT). For each model, 500 iterations of simulations were used.
4.3.2. Goodness-of-Fit Plot
The diagnostic goodness-of-fit (GOF) plots were implemented for model comparison, plotted using R package Xpose4. The population-predicted concentration versus observed concentration and the individual-predicted concentration versus observed concentration were plotted for each model.
4.3.3. Bias and Precision of Model Predictions
Bias was assessed using relative prediction error (PE%), determined by the difference between observed concentration (Cobs) and population-predicted concentration (Cpred) or individual-predicted concentration (Cipred). The population prediction error (PEpred%) and the individual prediction error (PEipred%) were calculated using Equation (1) and Equation (2), respectively [70,71].
The PE% was used for evaluating the prediction accuracy of each model. The Pepred% indicated the prediction accuracy after initial dosing with no prior concentration information, based solely on patient characteristics. The PEipred1–3% implied a prediction accuracy of TDM-based dose adjustments by taking one to three concentrations into account. The PE% was considered acceptable if the IQR of PE% was within 30%.
The root mean square error (RMSE) was used to evaluate the model precision. The RMSE was computed with the PE% to show the how far the predicted values were from the observed values in a regression analysis (Equation (3)) [72].
4.4. Simulation of Pharmacokinetic Profiles
For each selected/screened population pharmacokinetic model, the pharmacokinetics of meropenem were simulated under three typical renal function statuses (normal renal function creatinine clearance (CRCL) of 100 mL/min, augmented renal function CRCL of 200 mL/min, and impaired renal function CRCL of 20 mL/min) in standard patients. Apart from the renal function difference, the standard patient’s conditions were the same for all three patients: male, 55 years of age, weight of 80 kg, ideal body weight of 70 kg, height of 180 cm, albumin level of 25 g/L, APACHE score of 24, with sepsis. The simulated administration method of meropenem was 3 times a day, 1 g each time, intravenously infused with an infusion duration of 30 min. For models using CRCL as covariate, we used a CRCL(CG) (Cockcroft–Gault equation) estimation.
5. Conclusions
The predictive performance of the evaluated PK models available from the literature showed high variability and poor predictive power in our population of critically ill patients in the absence of individual meropenem concentrations. This might be due to the heterogeneity of this population with models that are probably too stringent. However, the use of individual meropenem concentrations showed a major improvement. Two models provided predictions within an acceptable range of ±30%, although this required at least two plasma concentrations to improve the model fit. In this population, the PK models did not seem well suited to predict the starting dose (with no prior plasma concentrations), but might be useful for TDM purposes when at least two samples are available. However, this is based on a limited number of patients from a very heterogenetic population. This study also shows the importance of validating models on the intended target population, since the performance of different models can vary to a large extent.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/antibiotics12020383/s1, Figure S1: Meropenem stratified VPC, Figure S2: Population prediction errors of the models, Figure S3: Individual prediction errors of the models, Figure S4: Individual prediction errors after the models included one trough concentration, Figure S5: Individual prediction errors after the models included two concentrations (trough and peak), Figure S6: Individual prediction errors after the models included three concentrations (trough and peak and in between), Figure S7: The RMSE of the models under different number of concentrations, Text S1: Literature search strategy.
Author Contributions
Conceptualization, L.L., S.D.T.S., T.M.J.E., A.A., B.C.P.K., N.G.M.H., H.E., A.E.M. and B.C.M.d.W.; acquisition of data, T.M.J.E., A.A.; formal analysis, L.L. and S.D.T.S.; writing—original draft preparation, L.L.; writing—review and editing, S.D.T.S., T.M.J.E., A.A., B.C.P.K., N.G.M.H., H.E., A.E.M. and B.C.M.d.W.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the principles of the Declaration of Helsinki (version October 2008) and approved by the Erasmus MC Medical Ethics Committee (EX-PAT, NL53551.078.15).
Informed Consent Statement
Informed consent was obtained from all patients or their legal representatives involved in the study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgments
Letao Li acknowledges the China Scholarship Council for the support by State Scholarship Fund No. 201908500113.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Sanders, C.C.; Sanders, W.E., Jr.; Thomson, K.S.; Iaconis, J.P. Meropenem: Activity against resistant gram-negative bacteria and interactions with beta-lactamases. J. Antimicrob. Chemother. 1989, 24 (Suppl. A), 187–196. [Google Scholar] [CrossRef] [PubMed]
- Joly-Guillou, M.L.; Kempf, M.; Cavallo, J.D.; Chomarat, M.; Dubreuil, L.; Maugein, J.; Muller-Serieys, C.; Roussel-Delvallez, M. Comparative in vitro activity of Meropenem, Imipenem and Piperacillin/tazobactam against 1071 clinical isolates using 2 different methods: A French multicentre study. BMC Infect. Dis. 2010, 10, 72. [Google Scholar] [CrossRef] [PubMed]
- Ye, X.; Wang, F.; Zeng, W.; Ding, Y.; Lv, B. Comparison of empirical high-dose and low-dose of meropenem in critically ill patients with sepsis and septic shock: A randomized controlled study protocol. Medicine 2020, 99, e22829. [Google Scholar] [CrossRef] [PubMed]
- Zhanel, G.G.; Simor, A.E.; Vercaigne, L.; Mandell, L.; Canadian Carbapenem Discussion Group. Imipenem and meropenem: Comparison of in vitro activity, pharmacokinetics, clinical trials and adverse effects. Can. J. Infect. Dis. 1998, 9, 215–228. [Google Scholar] [CrossRef]
- Zhanel, G.G.; Wiebe, R.; Dilay, L.; Thomson, K.; Rubinstein, E.; Hoban, D.J.; Noreddin, A.M.; Karlowsky, J.A. Comparative review of the carbapenems. Drugs 2007, 67, 1027–1052. [Google Scholar] [CrossRef]
- Zhu, L.L.; Zhou, Q. Optimal infusion rate in antimicrobial therapy explosion of evidence in the last five years. Infect. Drug Resist. 2018, 11, 1105–1117. [Google Scholar] [CrossRef]
- Chen, M.; Buurma, V.; Shah, M.; Fahim, G. Evaluation of studies on extended versus standard infusion of beta-lactam antibiotics. Am. J. Health Syst. Pharm. 2019, 76, 1383–1394. [Google Scholar] [CrossRef]
- Nicolau, D.P. Pharmacokinetic and pharmacodynamic properties of meropenem. Clin. Infect. Dis. 2008, 47 (Suppl. S1), S32–S40. [Google Scholar] [CrossRef]
- Mattoes, H.M.; Kuti, J.L.; Drusano, G.L.; Nicolau, D.P. Optimizing antimicrobial pharmacodynamics: Dosage strategies for meropenem. Clin. Ther. 2004, 26, 1187–1198. [Google Scholar] [CrossRef]
- Pea, F.; Viale, P. Bench-to-bedside review: Appropriate antibiotic therapy in severe sepsis and septic shock—Does the dose matter? Crit. Care 2009, 13, 214. [Google Scholar] [CrossRef]
- Li, C.; Du, X.; Kuti, J.L.; Nicolau, D.P. Clinical pharmacodynamics of meropenem in patients with lower respiratory tract infections. Antimicrob. Agents Chemother. 2007, 51, 1725–1730. [Google Scholar] [CrossRef]
- Hellinger, W.C.; Brewer, N.S. Carbapenems and monobactams: Imipenem, meropenem, and aztreonam. Mayo Clin. Proc. 1999, 74, 420–434. [Google Scholar] [CrossRef]
- Abdulla, A.; Dijkstra, A.; Hunfeld, N.G.M.; Endeman, H.; Bahmany, S.; Ewoldt, T.M.J.; Muller, A.E.; van Gelder, T.; Gommers, D.; Koch, B.C.P. Failure of target attainment of beta-lactam antibiotics in critically ill patients and associated risk factors: A two-center prospective study (EXPAT). Crit. Care 2020, 24, 558. [Google Scholar] [CrossRef]
- Monteiro, J.F.; Hahn, S.R.; Gonçalves, J.; Fresco, P. Vancomycin therapeutic drug monitoring and population pharmacokinetic models in special patient subpopulations. Pharmacol. Res. Perspect. 2018, 6, e00420. [Google Scholar] [CrossRef]
- Crass, R.L.; Cojutti, P.G.; Pai, M.P.; Pea, F. Reappraisal of Linezolid Dosing in Renal Impairment To Improve Safety. Antimicrob. Agents Chemother. 2019, 63, e00605-19. [Google Scholar] [CrossRef]
- Li, X.; Wang, X.; Wu, Y.; Sun, S.; Chen, K.; Lu, Y.; Wang, Q.; Zhao, Z. Plasma and cerebrospinal fluid population pharmacokinetic modeling and simulation of meropenem after intravenous and intrathecal administration in postoperative neurosurgical patients. Diagn. Microbiol. Infect. Dis. 2019, 93, 386–392. [Google Scholar] [CrossRef]
- Lu, C.; Zhang, Y.; Chen, M.; Zhong, P.; Chen, Y.; Yu, J.; Wu, X.; Wu, J.; Zhang, J. Population Pharmacokinetics and Dosing Regimen Optimization of Meropenem in Cerebrospinal Fluid and Plasma in Patients with Meningitis after Neurosurgery. Antimicrob. Agents Chemother. 2016, 60, 6619–6625. [Google Scholar] [CrossRef]
- Ehmann, L.; Zoller, M.; Minichmayr, I.K.; Scharf, C.; Huisinga, W.; Zander, J.; Kloft, C. Development of a dosing algorithm for meropenem in critically ill patients based on a population pharmacokinetic/pharmacodynamic analysis. Int. J. Antimicrob. Agents 2019, 54, 309–317. [Google Scholar] [CrossRef]
- Delattre, I.K.; Musuamba, F.T.; Jacqmin, P.; Taccone, F.S.; Laterre, P.F.; Verbeeck, R.K.; Jacobs, F.; Wallemacq, P. Population pharmacokinetics of four β-lactams in critically ill septic patients comedicated with amikacin. Clin. Biochem. 2012, 45, 780–786. [Google Scholar] [CrossRef]
- Li, C.; Kuti, J.L.; Nightingale, C.H.; Nicolau, D.P. Population pharmacokinetic analysis and dosing regimen optimization of meropenem in adult patients. J. Clin. Pharmacol. 2006, 46, 1171–1178. [Google Scholar] [CrossRef]
- Kim, Y.K.; Lee, D.H.; Jeon, J.; Jang, H.J.; Kim, H.K.; Jin, K.; Lim, S.N.; Lee, S.S.; Park, B.S.; Kim, Y.W.; et al. Population Pharmacokinetic Analysis of Meropenem after Intravenous Infusion in Korean Patients with Acute Infections. Clin. Ther. 2018, 40, 1384–1395. [Google Scholar] [CrossRef] [PubMed]
- Minichmayr, I.K.; Roberts, J.A.; Frey, O.R.; Roehr, A.C.; Kloft, C.; Brinkmann, A. Development of a dosing nomogram for continuous-infusion meropenem in critically ill patients based on a validated population pharmacokinetic model. J. Antimicrob. Chemother. 2018, 73, 1330–1339. [Google Scholar] [CrossRef] [PubMed]
- Usman, M.; Frey, O.R.; Hempel, G. Population pharmacokinetics of meropenem in elderly patients: Dosing simulations based on renal function. Eur. J. Clin. Pharmacol. 2017, 73, 333–342. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.T.; He, B.; Shen, N.; Liang, Y.; Sun, L.N. Meropenem Dosing Based on a Population Pharmacokinetic-Pharmacodynamic Model in Elderly Patients with Infection of the Lower Respiratory Tract. Drugs Aging 2017, 34, 115–121. [Google Scholar] [CrossRef]
- Chung, E.K.; Cheatham, S.C.; Fleming, M.R.; Healy, D.P.; Kays, M.B. Population Pharmacokinetics and Pharmacodynamics of Meropenem in Nonobese, Obese, and Morbidly Obese Patients. J. Clin. Pharmacol. 2017, 57, 356–368. [Google Scholar] [CrossRef]
- Mattioli, F.; Fucile, C.; Del Bono, V.; Marini, V.; Parisini, A.; Molin, A.; Zuccoli, M.L.; Milano, G.; Danesi, R.; Marchese, A.; et al. Population pharmacokinetics and probability of target attainment of meropenem in critically ill patients. Eur. J. Clin. Pharmacol. 2016, 72, 839–848. [Google Scholar] [CrossRef]
- Ramon-Lopez, A.; Allen, J.M.; Thomson, A.H.; Dheansa, B.S.; James, S.E.; Hanlon, G.W.; Stewart, B.; Davies, J.G. Dosing regimen of meropenem for adults with severe burns: A population pharmacokinetic study with Monte Carlo simulations. J. Antimicrob. Chemother. 2015, 70, 882–890. [Google Scholar] [CrossRef]
- Doh, K.; Woo, H.; Hur, J.; Yim, H.; Kim, J.; Chae, H.; Han, S.; Yim, D.S. Population pharmacokinetics of meropenem in burn patients. J. Antimicrob. Chemother. 2010, 65, 2428–2435. [Google Scholar] [CrossRef]
- Frippiat, F.; Musuamba, F.T.; Seidel, L.; Albert, A.; Denooz, R.; Charlier, C.; Van Bambeke, F.; Wallemacq, P.; Descy, J.; Lambermont, B.; et al. Modelled target attainment after meropenem infusion in patients with severe nosocomial pneumonia: The PROMESSE study. J. Antimicrob. Chemother. 2015, 70, 207–216. [Google Scholar] [CrossRef]
- Ulldemolins, M.; Soy, D.; Llaurado-Serra, M.; Vaquer, S.; Castro, P.; Rodríguez, A.H.; Pontes, C.; Calvo, G.; Torres, A.; Martín-Loeches, I. Meropenem population pharmacokinetics in critically ill patients with septic shock and continuous renal replacement therapy: Influence of residual diuresis on dose requirements. Antimicrob. Agents Chemother. 2015, 59, 5520–5528. [Google Scholar] [CrossRef]
- Jaruratanasirikul, S.; Thengyai, S.; Wongpoowarak, W.; Wattanavijitkul, T.; Tangkitwanitjaroen, K.; Sukarnjanaset, W.; Jullangkoon, M.; Samaeng, M. Population pharmacokinetics and Monte Carlo dosing simulations of meropenem during the early phase of severe sepsis and septic shock in critically ill patients in intensive care units. Antimicrob. Agents Chemother. 2015, 59, 2995–3001. [Google Scholar] [CrossRef]
- Roberts, J.A.; Kirkpatrick, C.M.; Roberts, M.S.; Robertson, T.A.; Dalley, A.J.; Lipman, J. Meropenem dosing in critically ill patients with sepsis and without renal dysfunction: Intermittent bolus versus continuous administration? Monte Carlo dosing simulations and subcutaneous tissue distribution. J. Antimicrob. Chemother. 2009, 64, 142–150. [Google Scholar] [CrossRef]
- Kees, M.G.; Minichmayr, I.K.; Moritz, S.; Beck, S.; Wicha, S.G.; Kees, F.; Kloft, C.; Steinke, T. Population pharmacokinetics of meropenem during continuous infusion in surgical ICU patients. J. Clin. Pharmacol. 2016, 56, 307–315. [Google Scholar] [CrossRef]
- Muro, T.; Sasaki, T.; Hosaka, N.; Umeda, Y.; Takemoto, S.; Yamamoto, H.; Kamimura, H.; Higuchi, S.; Karube, Y. Population pharmacokinetic analysis of meropenem in Japanese adult patients. J. Clin. Pharm. Ther. 2011, 36, 230–236. [Google Scholar] [CrossRef]
- Trang, M.; Griffith, D.C.; Bhavnani, S.M.; Loutit, J.S.; Dudley, M.N.; Ambrose, P.G.; Rubino, C.M. Population Pharmacokinetics of Meropenem and Vaborbactam Based on Data from Noninfected Subjects and Infected Patients. Antimicrob. Agents Chemother. 2021, 65, e0260620. [Google Scholar] [CrossRef]
- Lonsdale, D.O.; Kipper, K.; Baker, E.H.; Barker, C.I.S.; Oldfield, I.; Philips, B.J.; Johnston, A.; Rhodes, A.; Sharland, M.; Standing, J.F. β-Lactam antimicrobial pharmacokinetics and target attainment in critically ill patients aged 1 day to 90 years: The ABDose study. J. Antimicrob. Chemother. 2020, 75, 3625–3634. [Google Scholar] [CrossRef]
- Shekar, K.; Fraser, J.F.; Taccone, F.S.; Welch, S.; Wallis, S.C.; Mullany, D.V.; Lipman, J.; Roberts, J.A.; Investigators, A.E.S. The combined effects of extracorporeal membrane oxygenation and renal replacement therapy on meropenem pharmacokinetics: A matched cohort study. Crit. Care 2014, 18, 565. [Google Scholar] [CrossRef]
- Lan, J.; Wu, Z.; Wang, X.; Wang, Y.; Yao, F.; Zhao, B.X.; Wang, Y.; Chen, J.; Chen, C. Population Pharmacokinetics Analysis and Dosing Simulations Of Meropenem in Critically Ill Patients with Pulmonary Infection. J. Pharm. Sci. 2022, 111, 1833–1842. [Google Scholar] [CrossRef]
- Niibe, Y.; Suzuki, T.; Yamazaki, S.; Uchida, M.; Suzuki, T.; Takahashi, N.; Hattori, N.; Nakada, T.A.; Ishii, I. Identification of factors affecting meropenem pharmacokinetics in critically ill patients: Impact of inflammation on clearance. J. Infect. Chemother. 2022, 28, 532–538. [Google Scholar] [CrossRef]
- Lee, D.H.; Kim, H.S.; Park, S.; Kim, H.I.; Lee, S.H.; Kim, Y.K. Population Pharmacokinetics of Meropenem in Critically Ill Korean Patients and Effects of Extracorporeal Membrane Oxygenation. Pharmaceutics 2021, 13, 1861. [Google Scholar] [CrossRef]
- Alsultan, A.; Dasuqi, S.A.; Aljamaan, F.; Omran, R.A.; Syed, S.A.; AlJaloud, T.; AlAhmadi, A.; Alqahtani, S.; Hamad, M.A. Pharmacokinetics of meropenem in critically ill patients in Saudi Arabia. Saudi Pharm. J. 2021, 29, 1272–1277. [Google Scholar] [CrossRef] [PubMed]
- Tan, W.W.; Watt, K.M.; Boakye-Agyeman, F.; Cohen-Wolkowiez, M.; Mok, Y.H.; Yung, C.F.; Chan, Y.H. Optimal Dosing of Meropenem in a Small Cohort of Critically Ill Children Receiving Continuous Renal Replacement Therapy. J. Clin. Pharmacol. 2021, 61, 744–754. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.M.; Chen, X.Y.; Bi, J.; Wang, M.Y.; Xu, B.P.; Tang, B.H.; Li, C.; Zhao, W.; Shen, A.D. Reappraisal of the Optimal Dose of Meropenem in Critically Ill Infants and Children: A Developmental Pharmacokinetic-Pharmacodynamic Analysis. Antimicrob. Agents Chemother. 2020, 64, e00760-20. [Google Scholar] [CrossRef] [PubMed]
- Rapp, M.; Urien, S.; Foissac, F.; Béranger, A.; Bouazza, N.; Benaboud, S.; Bille, E.; Zheng, Y.; Gana, I.; Moulin, F.; et al. Population pharmacokinetics of meropenem in critically ill children with different renal functions. Eur. J. Clin. Pharmacol. 2020, 76, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Smith, P.B.; Cohen-Wolkowiez, M.; Castro, L.M.; Poindexter, B.; Bidegain, M.; Weitkamp, J.H.; Schelonka, R.L.; Ward, R.M.; Wade, K.; Valencia, G.; et al. Population pharmacokinetics of meropenem in plasma and cerebrospinal fluid of infants with suspected or complicated intra-abdominal infections. Pediatr. Infect. Dis. J. 2011, 30, 844–849. [Google Scholar] [CrossRef]
- Bradley, J.S.; Sauberan, J.B.; Ambrose, P.G.; Bhavnani, S.M.; Rasmussen, M.R.; Capparelli, E.V. Meropenem pharmacokinetics, pharmacodynamics, and Monte Carlo simulation in the neonate. Pediatr. Infect. Dis. J. 2008, 27, 794–799. [Google Scholar] [CrossRef]
- Du, X.; Li, C.; Kuti, J.L.; Nightingale, C.H.; Nicolau, D.P. Population pharmacokinetics and pharmacodynamics of meropenem in pediatric patients. J. Clin. Pharmacol. 2006, 46, 69–75. [Google Scholar] [CrossRef]
- Parker, E.M.; Hutchison, M.; Blumer, J.L. The pharmacokinetics of meropenem in infants and children: A population analysis. J. Antimicrob. Chemother. 1995, 36, 63–71. [Google Scholar] [CrossRef]
- Muhari-Stark, E.; Chen, X.; Sherwin, C.M.T.; Wang, Y.; Wang, J.; Yao, L. Association of Meropenem Clearance, Covariates and Estimated Glomerular Filtration Rate in Neonates. Clin. Pharmacol. Drug Dev. 2017, 6 (Suppl. S1), 3–72. [Google Scholar]
- Ikawa, K.; Morikawa, N.; Ikeda, K.; Miki, M.; Kobayashi, M. Population pharmacokinetics and pharmacodynamics of meropenem in Japanese pediatric patients. J. Infect. Chemother. 2010, 16, 139–143. [Google Scholar] [CrossRef]
- Tamatsukuri, T.; Ohbayashi, M.; Kohyama, N.; Kobayashi, Y.; Yamamoto, T.; Fukuda, K.; Nakamura, S.; Miyake, Y.; Dohi, K.; Kogo, M. The exploration of population pharmacokinetic model for meropenem in augmented renal clearance and investigation of optimum setting of dose. J. Infect. Chemother. 2018, 24, 834–840. [Google Scholar] [CrossRef]
- Niibe, Y.; Suzuki, T.; Yamazaki, S.; Suzuki, T.; Takahashi, N.; Hattori, N.; Nakada, T.A.; Oda, S.; Ishii, I. Population Pharmacokinetic Analysis of Meropenem in Critically Ill Patients with Acute Kidney Injury Treated with Continuous Hemodiafiltration. Ther. Drug Monit. 2020, 42, 588–594. [Google Scholar] [CrossRef]
- Onichimowski, D.; Będźkowska, A.; Ziółkowski, H.; Jaroszewski, J.; Borys, M.; Czuczwar, M.; Wiczling, P. Population pharmacokinetics of standard-dose meropenem in critically ill patients on continuous renal replacement therapy: A prospective observational trial. Pharmacol. Rep. 2020, 72, 719–729. [Google Scholar] [CrossRef]
- Grensemann, J.; Busse, D.; König, C.; Roedl, K.; Jäger, W.; Jarczak, D.; Iwersen-Bergmann, S.; Manthey, C.; Kluge, S.; Kloft, C.; et al. Acute-on-chronic liver failure alters meropenem pharmacokinetics in critically ill patients with continuous hemodialysis: An observational study. Ann. Intensive Care 2020, 10, 48. [Google Scholar] [CrossRef]
- Padullés Zamora, A.; Juvany Roig, R.; Leiva Badosa, E.; Sabater Riera, J.; Pérez Fernández, X.L.; Cárdenas Campos, P.; Rigo Bonin, R.; Alía Ramos, P.; Tubau Quintano, F.; Sospedra Martinez, E.; et al. Optimized meropenem dosage regimens using a pharmacokinetic/pharmacodynamic population approach in patients undergoing continuous venovenous haemodiafiltration with high-adsorbent membrane. J. Antimicrob. Chemother. 2019, 74, 2979–2983. [Google Scholar] [CrossRef]
- Hanberg, P.; Öbrink-Hansen, K.; Thorsted, A.; Bue, M.; Tøttrup, M.; Friberg, L.E.; Hardlei, T.F.; Søballe, K.; Gjedsted, J. Population Pharmacokinetics of Meropenem in Plasma and Subcutis from Patients on Extracorporeal Membrane Oxygenation Treatment. Antimicrob. Agents Chemother. 2018, 62, e02390-17. [Google Scholar] [CrossRef]
- Burger, R.; Guidi, M.; Calpini, V.; Lamoth, F.; Decosterd, L.; Robatel, C.; Buclin, T.; Csajka, C.; Marchetti, O. Effect of renal clearance and continuous renal replacement therapy on appropriateness of recommended meropenem dosing regimens in critically ill patients with susceptible life-threatening infections. J. Antimicrob. Chemother. 2018, 73, 3413–3422. [Google Scholar] [CrossRef]
- Isla, A.; Rodríguez-Gascón, A.; Trocóniz, I.F.; Bueno, L.; Solinís, M.A.; Maynar, J.; Sánchez-Izquierdo, J.A.; Pedraz, J.L. Population pharmacokinetics of meropenem in critically ill patients undergoing continuous renal replacement therapy. Clin. Pharmacokinet. 2008, 47, 173–180. [Google Scholar] [CrossRef]
- Dhaese, S.A.M.; Farkas, A.; Colin, P.; Lipman, J.; Stove, V.; Verstraete, A.G.; Roberts, J.A.; De Waele, J.J. Population pharmacokinetics and evaluation of the predictive performance of pharmacokinetic models in critically ill patients receiving continuous infusion meropenem: A comparison of eight pharmacokinetic models. J. Antimicrob. Chemother. 2019, 74, 432–441. [Google Scholar] [CrossRef]
- Wang, Y.L.; Guilhaumou, R.; Blin, O.; Velly, L.; Marsot, A. External evaluation of population pharmacokinetic models for continuous administration of meropenem in critically ill adult patients. Eur. J. Clin. Pharmacol. 2020, 76, 1281–1289. [Google Scholar] [CrossRef]
- Chan Kwong, A.; O’Jeanson, A.; Khier, S. Model-Informed Therapeutic Drug Monitoring of Meropenem in Critically Ill Patients: Improvement of the Predictive Ability of Literature Models with the PRIOR Approach. Eur. J. Drug Metab. Pharmacokinet. 2021, 46, 415–426. [Google Scholar] [CrossRef] [PubMed]
- Yang, N.; Wang, J.; Xie, Y.; Ding, J.; Wu, C.; Liu, J.; Pei, Q. External Evaluation of Population Pharmacokinetic Models to Inform Precision Dosing of Meropenem in Critically Ill Patients. Front. Pharmacol. 2022, 13, 838205. [Google Scholar] [CrossRef] [PubMed]
- AstraZeneca. MERREM® IV (Meropenem for Injection), for Intravenous Use. 1996. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/050706s037lbl.pdf (accessed on 9 February 2023).
- Baptista, J.P.; Neves, M.; Rodrigues, L.; Teixeira, L.; Pinho, J.; Pimentel, J. Accuracy of the estimation of glomerular filtration rate within a population of critically ill patients. J. Nephrol. 2014, 27, 403–410. [Google Scholar] [CrossRef] [PubMed]
- Cockcroft, D.W.; Gault, M.H. Prediction of creatinine clearance from serum creatinine. Nephron 1976, 16, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Levey, A.S.; Coresh, J.; Greene, T.; Stevens, L.A.; Zhang, Y.L.; Hendriksen, S.; Kusek, J.W.; Van Lente, F.; Chronic Kidney Disease Epidemiology Collaboration. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann. Intern. Med. 2006, 145, 247–254. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., 3rd; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Abdulla, A.; Bahmany, S.; Wijma, R.A.; van der Nagel, B.C.H.; Koch, B.C.P. Simultaneous determination of nine β-lactam antibiotics in human plasma by an ultrafast hydrophilic-interaction chromatography-tandem mass spectrometry. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 2017, 1060, 138–143. [Google Scholar] [CrossRef]
- Lindbom, L.; Pihlgren, P.; Jonsson, N. PsN-Toolkit—A collection of computer intensive statistical methods for non-linear mixed effect modeling using NONMEM. Comput. Methods Programs Biomed. 2005, 79, 241–257. [Google Scholar] [CrossRef]
- Sheiner, L.B.; Beal, S.L. Some suggestions for measuring predictive performance. J. Pharmacokinet. Biopharm. 1981, 9, 503–512. [Google Scholar] [CrossRef]
- Guang, W.; Baraldo, M.; Furlanut, M. Calculating percentage prediction error: A user’s note. Pharmacol. Res. 1995, 32, 241–248. [Google Scholar] [CrossRef]
- Vozeh, S.; Uematsu, T.; Hauf, G.F.; Follath, F. Performance of Bayesian feedback to forecast lidocaine serum concentration: Evaluation of the prediction error and the prediction interval. J. Pharmacokinet. Biopharm. 1985, 13, 203–212. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).