Genetic Organization of Acquired Antimicrobial Resistance Genes and Detection of Resistance-Mediating Mutations in a Gallibacterium anatis Isolate from a Calf Suffering from a Respiratory Tract Infection
Abstract
1. Introduction
2. Results and Discussion
2.1. Antimicrobial Susceptibility Testing
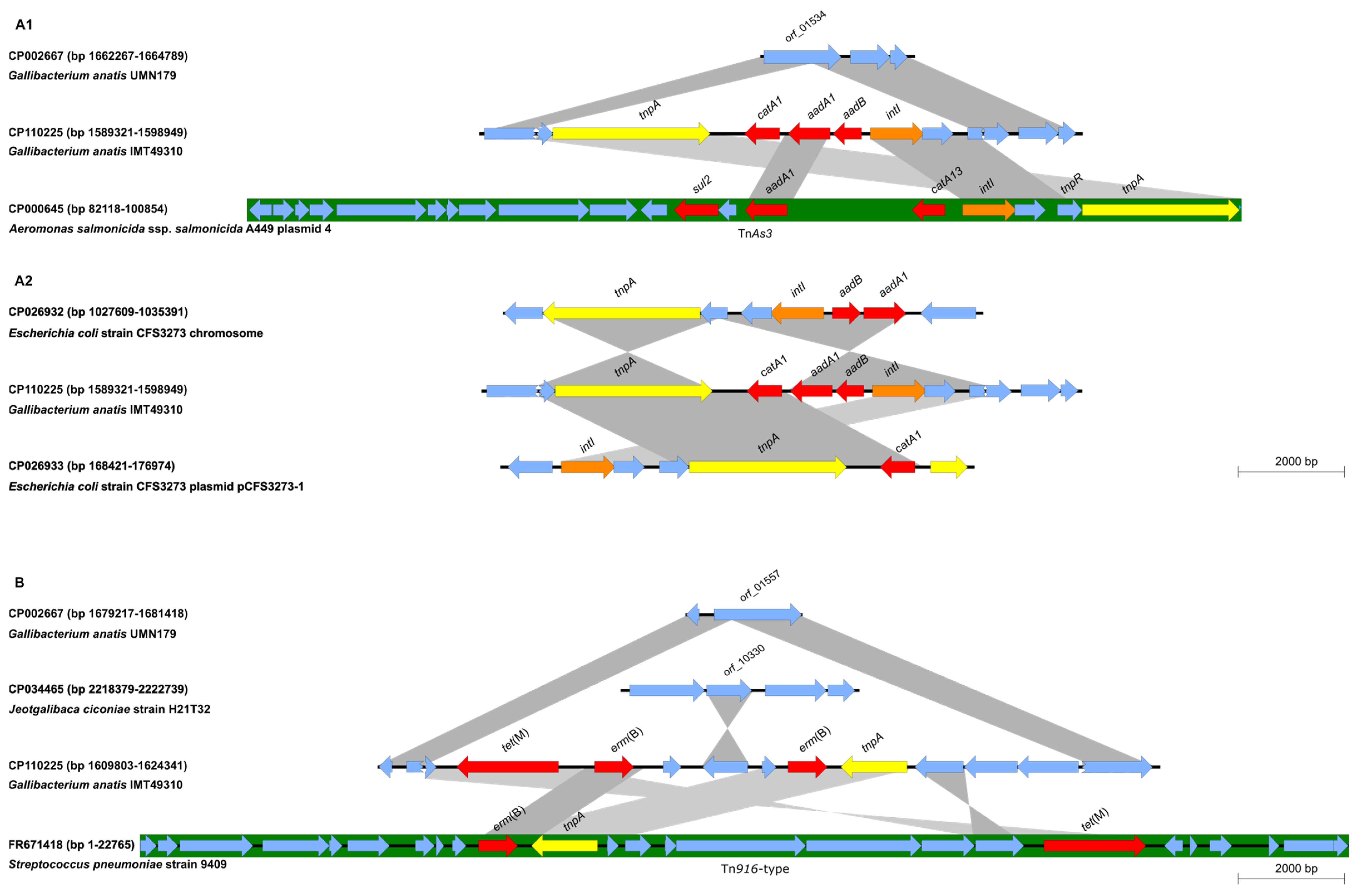
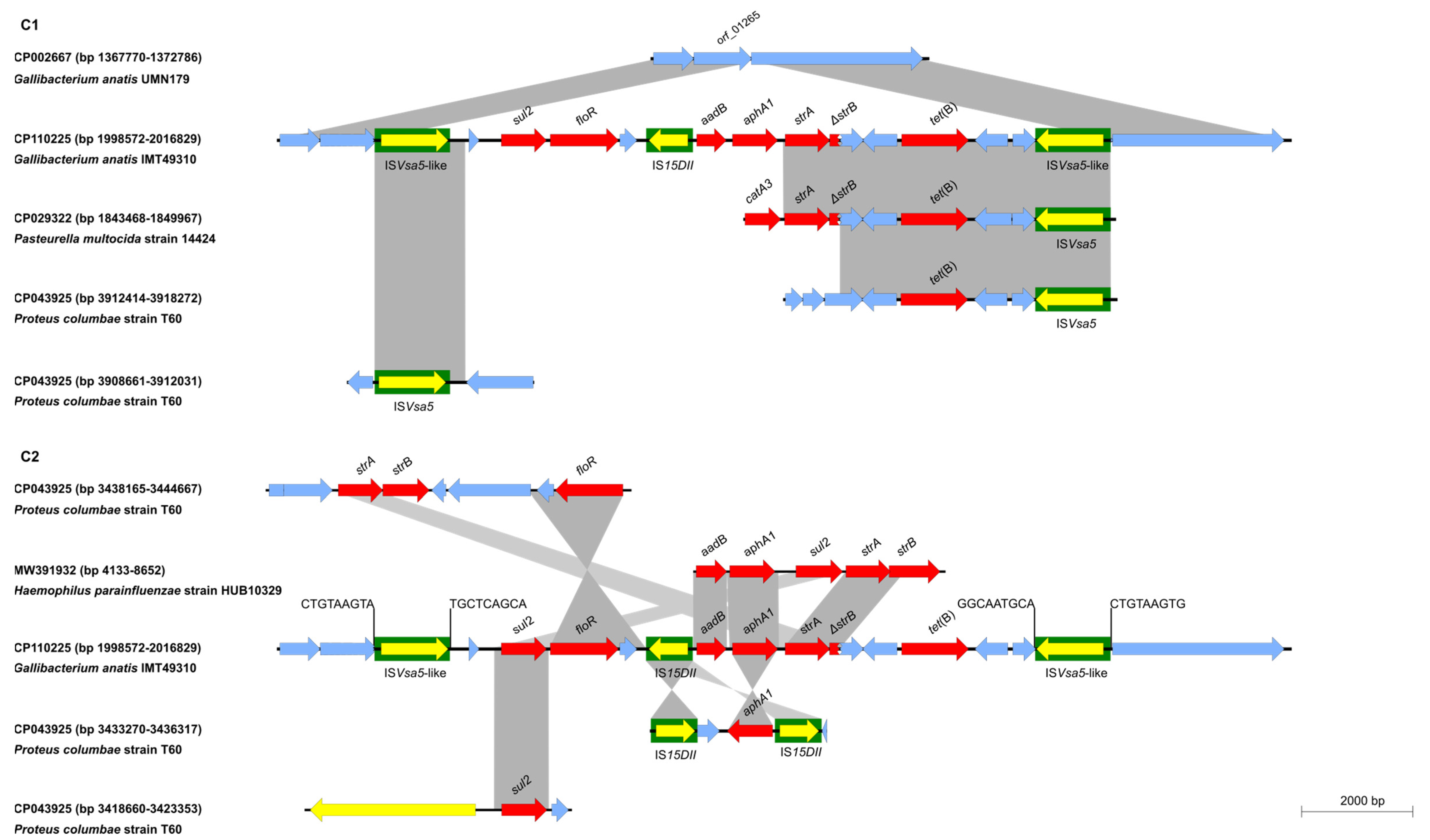
2.2. Sequence Analysis
3. Materials and Methods
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Krishnegowda, D.N.; Dhama, K.; Mariappan, A.K.; Munuswamy, P.; Yatoo, M.I.; Tiwari, R.; Karthik, K.; Bhatt, P.; Reddy, M.R. Etiology, epidemiology, pathology, and advances in diagnosis, vaccine development, and treatment of Gallibacterium anatis infection in poultry: A review. Vet. Q. 2020, 40, 16–34. [Google Scholar] [CrossRef] [PubMed]
- Bojesen, A.M.; Vazquez, M.E.; Bager, R.J.; Ifrah, D.; Gonzalez, C.; Aarestrup, F.M. Antimicrobial susceptibility and tetracycline resistance determinant genotyping of Gallibacterium anatis. Vet. Microbiol. 2011, 148, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.H.; Thornton, J.K.; Zhang, Y.; Mauel, M.J. A 5-year retrospective report of Gallibacterium anatis and Pasteurella multocida isolates from chickens in Mississippi. Poult. Sci. 2013, 92, 3166–3171. [Google Scholar] [CrossRef] [PubMed]
- Hess, C.; Grafl, B.; Bagheri, S.; Kaesbohrer, A.; Zloch, A.; Hess, M. Antimicrobial Resistance Profiling of Gallibacterium anatis from Layers Reveals High Number of Multiresistant Strains and Substantial Variability Even Between Isolates from the Same Organ. Microb. Drug Resist. 2020, 26, 169–177. [Google Scholar] [CrossRef] [PubMed]
- El-Adawy, H.; Bocklisch, H.; Neubauer, H.; Hafez, M.H.; Hotzel, H. Identification, differentiation and antibiotic susceptibility of Gallibacterium isolates from diseased poultry. Ir. Vet. J. 2018, 71, 5. [Google Scholar] [CrossRef] [PubMed]
- Aubin, G.G.; Haloun, A.; Treilhaud, M.; Reynaud, A.; Corvec, S. Gallibacterium anatis Bacteremia in a Human. J. Clin. Microbiol. 2013, 51, 3897–3899. [Google Scholar] [CrossRef] [PubMed]
- van Driessche, L.; Vanneste, K.; Bogaerts, B.; de Keersmaecker, S.C.J.; Roosens, N.H.; Haesebrouck, F.; de Cremer, L.; Deprez, P.; Pardon, B.; Boyen, F. Isolation of Drug-Resistant Gallibacterium anatis from Calves with Unresponsive Bronchopneumonia, Belgium. Emerg. Infect. Dis. 2020, 26, 721–730. [Google Scholar] [CrossRef] [PubMed]
- Peel, D.S. The effect of Market Forces on Bovine Respiratory Disease. Vet. Clin. Food Anim. 2020, 36, 497–508. [Google Scholar] [CrossRef] [PubMed]
- Pardon, B.; Buczinski, S. Bovine Respiratory Disease What Progress has Been Made in Infectious Diagnosis? Vet. Clin. Food Anim. 2020, 36, 425–444. [Google Scholar] [CrossRef] [PubMed]
- Michael, G.B.; Bossé, J.T.; Schwarz, S. Antimicrobial resistance in Pasteurellaceae of veterinary origin. Microbiol. Spectr. 2018, 6, 331–363. [Google Scholar] [CrossRef] [PubMed]
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Disk and Dilution Susceptibility Tests for Bacteria Isolated from Animals-Fifth Edition: VET01S-Ed5; CLSI: Wayne, PA, USA, 2020. [Google Scholar]
- Johnson, T.J.; Fernandez-Alarcon, C.; Bojesen, A.M.; Nolan, L.K.; Trampel, D.W.; Seemann, T. Complete Genome Sequence of Gallibacterium anatis Strain UMN179, Isolated from a laying Hen with Peritonitis. J. Bacteriol. 2011, 193, 3676–3677. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, B.M.; Sinha, S.; Boyce, J.D.; Bojesen, A.M.; Mell, J.C.; Redfield, R.J. Natural transformation of Gallibacterium anatis. Appl. Environ. Microbiol. 2012, 78, 4914–4922. [Google Scholar] [CrossRef] [PubMed]
- Schink, A.-K.; Hanke, D.; Semmler, T.; Brombach, J.; Bethe, A.; Lübke-Becker, A.; Teske, K.; Müller, K.E.; Schwarz, S. Novel multiresistance-mediating integrative and conjugative elements carrying unusual antimicrobial resistance genes in Mannheimia haemolytica and Pasteurella multocida. J. Antimicrob. Chemother. 2022, 77, 2033–2035. [Google Scholar] [CrossRef] [PubMed]
- Wick, R.R.; Judd, L.M.; Gorrie, C.L.; Holt, K.E. Unicycler: Resolving bacterial genome assemblies from short and long sequencing reads. PLoS Comput. Biol. 2017, 13, e1005595. [Google Scholar] [CrossRef] [PubMed]
- Bankevich, A.; Nurk, S.; Antipov, D.; Gurevich, A.A.; Dvorkin, M.; Kulikov, A.S.; Lesin, V.M.; Nikolenko, S.I.; Pham, S.; Prjibelski, A.D.; et al. SPAdes: A New Genome Assembly Algorithm and Its Applications to Single-Cell Sequencing. J. Comput. Biol. 2012, 19, 455–477. [Google Scholar] [CrossRef] [PubMed]
- Bortolaia, V.; Kaas, R.F.; Ruppe, E.; Roberts, M.C.; Schwarz, S.; Cattoir, V.; Phillippon, A.; Allesoe, R.L.; Rebelo, A.R.; Florensa, A.R.; et al. ResFinder 4.0 for predictionsof phenotypes from geneotypes. J. Antimicrob. Chemother. 2020, 75, 3491–3500. [Google Scholar] [CrossRef] [PubMed]
- Zankari, E.; Allesøe, R.; Joensen, K.G.; Cavaco, L.M.; Lund, O.; Aarestrup, F.M. PointFinder: A novel web tool for WGS-based detection of antimicrobial resistance associated with chromosomal point mutations in bacterial pathogens. J. Antimicrob. Chemother. 2017, 72, 2764–2768. [Google Scholar] [CrossRef] [PubMed]
- Camacho, C.; Coulouris, G.; Avagyan, V.; Ma, N.; Papadopoulos, J.; Bealer, K.; Madden, T.L. BLAST+: Architecture and applications. BMC Bioinform. 2009, 10, 421. [Google Scholar] [CrossRef] [PubMed]
- Siguier, P.; Perochon, J.; Lestrade, L.; Mahillon, J.; Chandler, M. ISFinder: The reference centre for bacterial insertion sequences. Nucl. Acids Res. 2006, 34, D32–D36. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schink, A.-K.; Hanke, D.; Semmler, T.; Roschanski, N.; Schwarz, S. Genetic Organization of Acquired Antimicrobial Resistance Genes and Detection of Resistance-Mediating Mutations in a Gallibacterium anatis Isolate from a Calf Suffering from a Respiratory Tract Infection. Antibiotics 2023, 12, 294. https://doi.org/10.3390/antibiotics12020294
Schink A-K, Hanke D, Semmler T, Roschanski N, Schwarz S. Genetic Organization of Acquired Antimicrobial Resistance Genes and Detection of Resistance-Mediating Mutations in a Gallibacterium anatis Isolate from a Calf Suffering from a Respiratory Tract Infection. Antibiotics. 2023; 12(2):294. https://doi.org/10.3390/antibiotics12020294
Chicago/Turabian StyleSchink, Anne-Kathrin, Dennis Hanke, Torsten Semmler, Nicole Roschanski, and Stefan Schwarz. 2023. "Genetic Organization of Acquired Antimicrobial Resistance Genes and Detection of Resistance-Mediating Mutations in a Gallibacterium anatis Isolate from a Calf Suffering from a Respiratory Tract Infection" Antibiotics 12, no. 2: 294. https://doi.org/10.3390/antibiotics12020294
APA StyleSchink, A.-K., Hanke, D., Semmler, T., Roschanski, N., & Schwarz, S. (2023). Genetic Organization of Acquired Antimicrobial Resistance Genes and Detection of Resistance-Mediating Mutations in a Gallibacterium anatis Isolate from a Calf Suffering from a Respiratory Tract Infection. Antibiotics, 12(2), 294. https://doi.org/10.3390/antibiotics12020294





