Application of Different Wavelengths of LED Lights in Antimicrobial Photodynamic Therapy for the Treatment of Periodontal Disease
Abstract
:1. Introduction
2. Periodontal Diseases
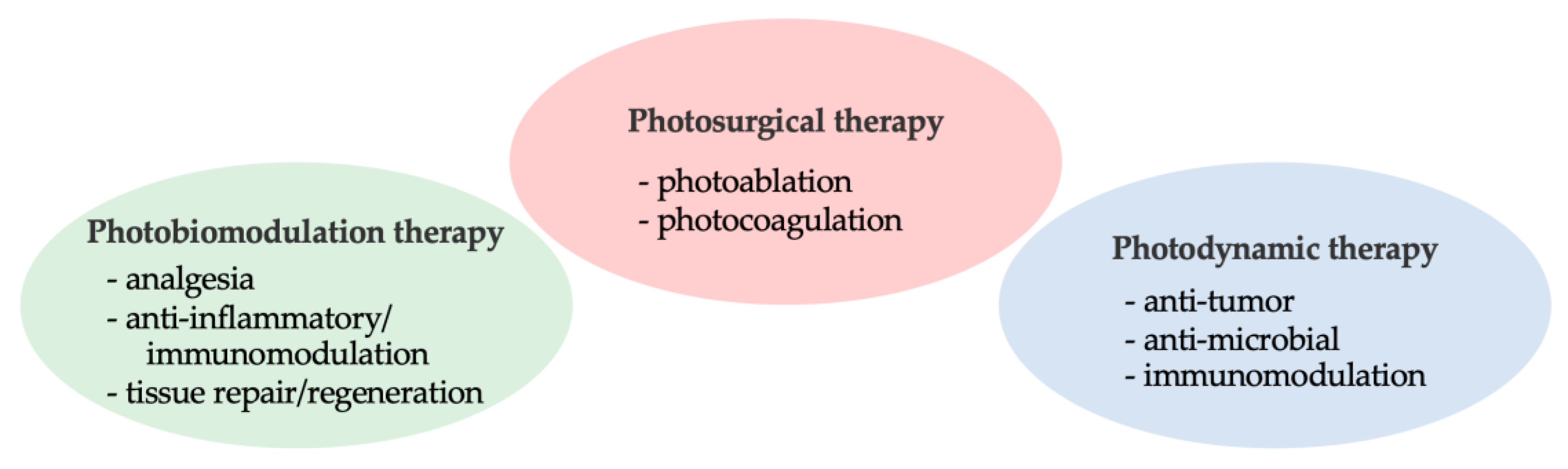
3. Phototherapy in Periodontics
4. Antimicrobial Effects of Various Wavelengths of LEDs
4.1. Search Strategy
4.2. Red Light/Infrared Light
| Reference | Study Participants (n) Study Design | Groups (n: Sites) Treatment Provided | Follow-Up Findings |
|---|---|---|---|
| Bassir et al., 2013 [41] | CP (16) Split-mouth |
|
|
| Pulikkotil et al., 2016 [42] | CP (16) Split-mouth |
|
|
| Husejinagic et al., 2019 [43] | Periodontitis (20) Split-mouth, RCT |
|
|
| Harmouche et al., 2019 [44] | Periodontitis (28) Split-mouth, RCT |
|
|
| Mongardini et al., 2014 [45] | CP (30); Residual pockets during SPT Split-mouth |
|
|
| Goh et al., 2017 [46] | Periodontitis (27); Residual pockets during SPT Split-mouth, RCT |
|
|
| Hormdee et al., 2020 [47] | Periodontitis (12) Split-mouth, RCT |
|
|
| Ivanaga et al., 2019 [48] | CP with type 2 DM (23); Residual pockets during SPT Split-mouth, RCT |
|
|
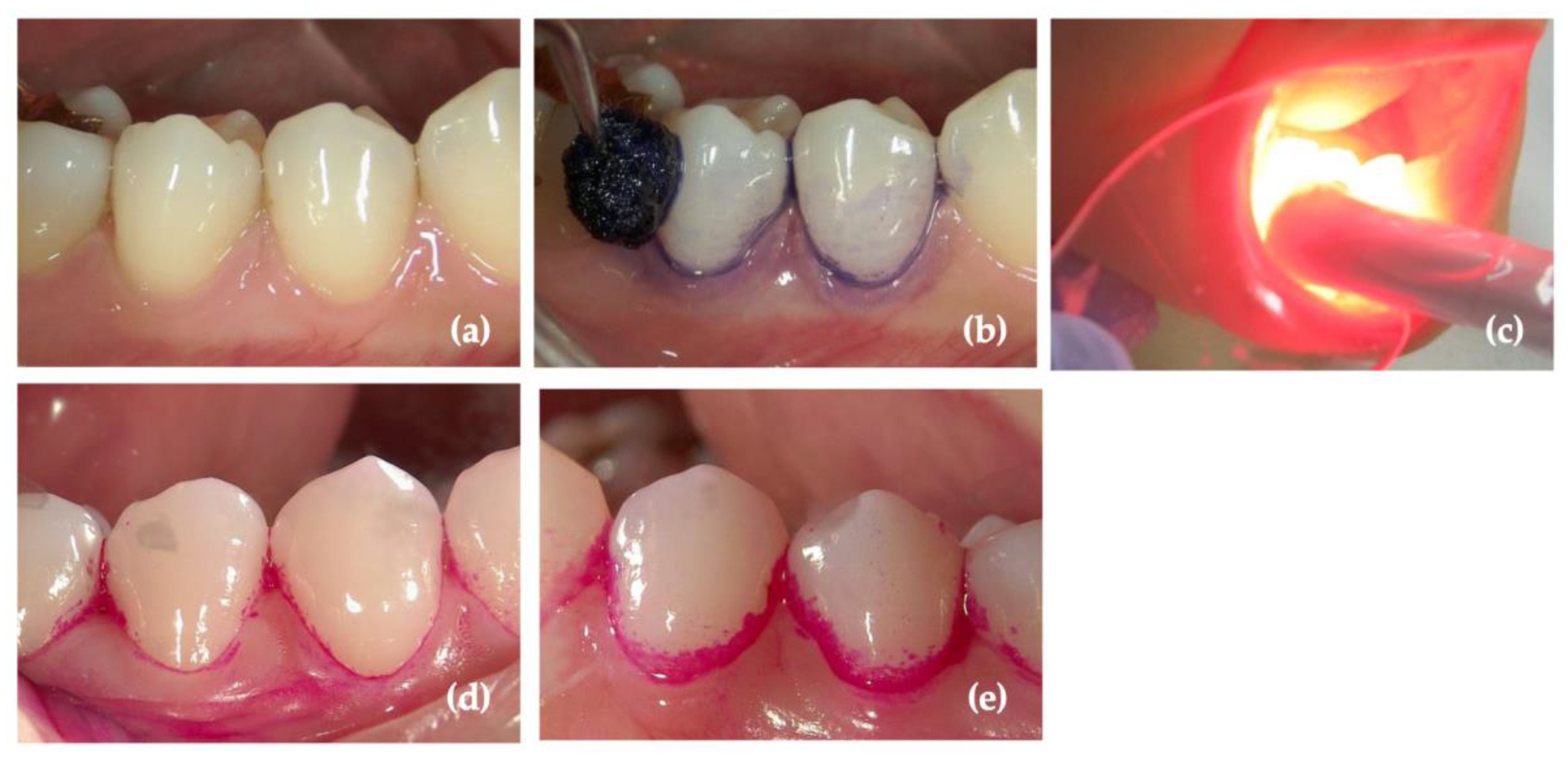
4.3. Blue Light
4.4. Green/Yellow Light
4.5. UV Light
5. Future Perspectives and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Aoki, A.; Mizutani, K.; Schwarz, F.; Sculean, A.; Yukna, R.A.; Takasaki, A.A.; Romanos, G.E.; Taniguchi, Y.; Sasaki, K.M.; Zeredo, J.L.; et al. Periodontal and peri-implant wound healing following laser therapy. Periodontol. 2000 2015, 68, 217–269. [Google Scholar] [CrossRef]
- Gholami, L.; Shahabi, S.; Jazaeri, M.; Hadilou, M.; Fekrazad, R. Clinical applications of antimicrobial photodynamic therapy in dentistry. Front. Microbiol. 2023, 13, 1020995. [Google Scholar] [CrossRef]
- Takasaki, A.A.; Aoki, A.; Mizutani, K.; Schwarz, F.; Sculean, A.; Wang, C.Y.; Koshy, G.; Romanos, G.; Ishikawa, I.; Izumi, Y. Application of antimicrobial photodynamic therapy in periodontal and peri-implant diseases. Periodontol. 2000 2009, 51, 109–140. [Google Scholar] [CrossRef]
- Chen, M.X.; Zhong, Y.J.; Dong, Q.Q.; Wong, H.M.; Wen, Y.F. Global, regional, and national burden of severe periodontitis, 1990-2019: An analysis of the Global Burden of Disease Study 2019. J. Clin. Periodontol. 2021, 48, 1165–1188. [Google Scholar] [CrossRef]
- Janakiram, C.; Dye, B.A. A public health approach for prevention of periodontal disease. Periodontol. 2000 2020, 84, 202–214. [Google Scholar] [CrossRef]
- Falcao, A.; Bullon, P. A review of the influence of periodontal treatment in systemic diseases. Periodontol. 2000 2019, 79, 117–128. [Google Scholar] [CrossRef]
- Bui, F.Q.; Almeida-da-Silva, C.L.C.; Huynh, B.; Trinh, A.; Liu, J.; Woodward, J.; Asadi, H.; Ojcius, D.M. Association between periodontal pathogens and systemic disease. Biomed. J. 2019, 42, 27–35. [Google Scholar] [CrossRef]
- Herrera, D.; Alonso, B.; Leon, R.; Roldan, S.; Sanz, M. Antimicrobial therapy in periodontitis: The use of systemic antimicrobials against the subgingival biofilm. J. Clin. Periodontol. 2008, 35, 45–66. [Google Scholar] [CrossRef]
- Valen, H.; Scheie, A.A. Biofilms and their properties. Eur. J. Oral Sci. 2018, 126, 13–18. [Google Scholar] [CrossRef]
- Quirynen, M.; Teughels, W.; van Steenberghe, D. Microbial shifts after subgingival debridement and formation of bacterial resistance when combined with local or systemic antimicrobials. Oral Dis. 2003, 9, 30–37. [Google Scholar] [CrossRef]
- Walker, C.B. The acquisition of antibiotic resistance in the periodontal microflora. Periodontol. 2000 1996, 10, 79–88. [Google Scholar] [CrossRef]
- Aoki, A.; Sasaki, K.M.; Watanabe, H.; Ishikawa, I. Lasers in nonsurgical periodontal therapy. Periodontol. 2000 2004, 36, 59–97. [Google Scholar] [CrossRef]
- Schwarz, F.; Aoki, A.; Becker, J.; Sculean, A. Laser application in non-surgical periodontal therapy: A systematic review. J. Clin. Periodontol. 2008, 35, 29–44. [Google Scholar] [CrossRef]
- Ebrahimi, P.; Hadilou, M.; Naserneysari, F.; Dolatabadi, A.; Tarzemany, R.; Vahed, N.; Nikniaz, L.; Fekrazad, R.; Gholami, L. Effect of photobiomodulation in secondary intention gingival wound healing-a systematic review and meta-analysis. BMC Oral Health 2021, 21, 258. [Google Scholar] [CrossRef]
- Lopes, C.C.A.; Limirio, J.; Zanatta, L.S.A.; Simamoto, V.R.N.; Dechichi, P.; Limirio, A. Effectiveness of photobiomodulation therapy on human bone healing in dentistry: A systematic review. Photobiomodul. Photomed. Laser Surg. 2022, 40, 440–453. [Google Scholar] [CrossRef]
- Mikami, R.; Mizutani, K.; Sasaki, Y.; Iwata, T.; Aoki, A. Patient-reported outcomes of laser-assisted pain control following non-surgical and surgical periodontal therapy: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0238659. [Google Scholar] [CrossRef]
- van Straten, D.; Mashayekhi, V.; de Bruijn, H.S.; Oliveira, S.; Robinson, D.J. Oncologic photodynamic therapy: Basic principles, current clinical status and future directions. Cancers 2017, 9, 19. [Google Scholar] [CrossRef]
- Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: One-year results of 2 randomized clinical trials—DTAP report. Treatment of Age-related Macular Degeneration with Photodynamic Therapy (TAP) Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: One-year results of 2 randomized clinical trials—TAP report. Treatment of age-related macular degeneration with photodynamic therapy (TAP) Study Group. Arch. Ophthalmol. 1999, 117, 1329–1345.
- Kömerik, N.; Wilson, M.; Poole, S. The effect of photodynamic action on two virulence factors of gram-negative bacteria. Photochem. Photobiol. 2000, 72, 676–680. [Google Scholar] [CrossRef]
- Braham, P.; Herron, C.; Street, C.; Darveau, R. Antimicrobial photodynamic therapy may promote periodontal healing through multiple mechanisms. J. Periodontol. 2009, 80, 1790–1798. [Google Scholar] [CrossRef]
- Kousis, P.C.; Henderson, B.W.; Maier, P.G.; Gollnick, S.O. Photodynamic therapy enhancement of antitumor immunity is regulated by neutrophils. Cancer Res. 2007, 67, 10501–10510. [Google Scholar] [CrossRef]
- Morgan, M.C.; Rashid, R.M. The effect of phototherapy on neutrophils. Int. Immunopharmacol. 2009, 9, 383–388. [Google Scholar] [CrossRef]
- Tanaka, M.; Mroz, P.; Dai, T.; Huang, L.; Morimoto, Y.; Kinoshita, M.; Yoshihara, Y.; Nemoto, K.; Shinomiya, N.; Seki, S.; et al. Photodynamic therapy can induce a protective innate immune response against murine bacterial arthritis via neutrophil accumulation. PLoS ONE 2012, 7, e39823. [Google Scholar] [CrossRef]
- Nakagawa, Y.; Homma, S.; Yamamoto, I.; Banno, M.; Nakazato, H.; Imanaga, H.; Yamamoto, N. In vivo and in vitro activation of macrophages with a cyanine photosensitizing dye, platonin. Cancer Immunol. Immunother. 1993, 37, 157–162. [Google Scholar] [CrossRef]
- King, D.E.; Jiang, H.; Simkin, G.O.; Obochi, M.O.; Levy, J.G.; Hunt, D.W. Photodynamic alteration of the surface receptor expression pattern of murine splenic dendritic cells. Scand. J. Immunol. 1999, 49, 184–192. [Google Scholar] [CrossRef]
- Preise, D.; Oren, R.; Glinert, I.; Kalchenko, V.; Jung, S.; Scherz, A.; Salomon, Y. Systemic antitumor protection by vascular-targeted photodynamic therapy involves cellular and humoral immunity. Cancer Immunol. Immunother. 2009, 58, 71–84. [Google Scholar] [CrossRef]
- Séguier, S.; Souza, S.L.; Sverzut, A.C.; Simioni, A.R.; Primo, F.L.; Bodineau, A.; Correa, V.M.; Coulomb, B.; Tedesco, A.C. Impact of photodynamic therapy on inflammatory cells during human chronic periodontitis. J. Photochem. Photobiol. B 2010, 101, 348–354. [Google Scholar] [CrossRef]
- Jiang, C.; Yang, W.; Wang, C.; Qin, W.; Ming, J.; Zhang, M.; Qian, H.; Jiao, T. Methylene Blue-Mediated Photodynamic Therapy Induces Macrophage Apoptosis via ROS and Reduces Bone Resorption in Periodontitis. Oxid. Med. Cell Longev. 2019, 2019, 1529520. [Google Scholar] [CrossRef]
- da Cruz Andrade, P.V.; Euzebio Alves, V.T.; de Carvalho, V.F.; De Franco Rodrigues, M.; Pannuti, C.M.; Holzhausen, M.; De Micheli, G.; Conde, M.C. Photodynamic therapy decrease immune-inflammatory mediators levels during periodontal maintenance. Lasers Med. Sci. 2017, 32, 9–17. [Google Scholar] [CrossRef]
- Salvi, G.E.; Stahli, A.; Schmidt, J.C.; Ramseier, C.A.; Sculean, A.; Walter, C. Adjunctive laser or antimicrobial photodynamic therapy to non-surgical mechanical instrumentation in patients with untreated periodontitis: A systematic review and meta-analysis. J. Clin. Periodontol. 2020, 47, 176–198. [Google Scholar] [CrossRef]
- Dalvi, S.; Benedicenti, S.; Salagean, T.; Bordea, I.R.; Hanna, R. Effectiveness of antimicrobial photodynamic therapy in the treatment of periodontitis: A systematic review and meta-analysis of in vivo human randomized controlled clinical trials. Pharmaceutics 2021, 13, 836. [Google Scholar] [CrossRef]
- Calciolari, E.; Ercal, P.; Dourou, M.; Akcali, A.; Tagliaferri, S.; Donos, N. The efficacy of adjunctive periodontal therapies during supportive periodontal care in patients with residual pockets. A systematic review and meta-analysis. J. Periodontal. Res. 2022, 57, 671–689. [Google Scholar] [CrossRef]
- Moro, M.G.; de Carvalho, V.F.; Godoy-Miranda, B.A.; Kassa, C.T.; Horliana, A.; Prates, R.A. Efficacy of antimicrobial photodynamic therapy (aPDT) for nonsurgical treatment of periodontal disease: A systematic review. Lasers Med. Sci. 2021, 36, 1573–1590. [Google Scholar] [CrossRef]
- Yoshida, A.; Sasaki, H.; Toyama, T.; Araki, M.; Fujioka, J.; Tsukiyama, K.; Hamada, N.; Yoshino, F. Antimicrobial effect of blue light using Porphyromonas gingivalis pigment. Sci. Rep. 2017, 7, 5225. [Google Scholar] [CrossRef]
- Fontana, C.R.; Abernethy, A.D.; Som, S.; Ruggiero, K.; Doucette, S.; Marcantonio, R.C.; Boussios, C.I.; Kent, R.; Goodson, J.M.; Tanner, A.C.; et al. The antibacterial effect of photodynamic therapy in dental plaque-derived biofilms. J. Periodontal Res. 2009, 44, 751–759. [Google Scholar] [CrossRef]
- Chui, C.; Hiratsuka, K.; Aoki, A.; Takeuchi, Y.; Abiko, Y.; Izumi, Y. Blue LED inhibits the growth of Porphyromonas gingivalis by suppressing the expression of genes associated with DNA replication and cell division. Lasers Surg. Med. 2012, 44, 856–864. [Google Scholar] [CrossRef]
- Demidova, T.N.; Hamblin, M.R. Effect of cell-photosensitizer binding and cell density on microbial photoinactivation. Antimicrob. Agents Chemother. 2005, 49, 2329–2335. [Google Scholar] [CrossRef]
- Sales, L.S.; Miranda, M.L.; de Oliveira, A.B.; Ferrisse, T.M.; Fontana, C.R.; Milward, M.; Brighenti, F.L. Effect of the technique of photodynamic therapy against the main microorganisms responsible for periodontitis: A systematic review of in-vitro studies. Arch. Oral Biol. 2022, 138, 105425. [Google Scholar] [CrossRef]
- de Sousa, G.R.; Soares, L.O.; Soares, B.M.; de Carvalho Cruz, R.; Uliana Junior, P.; Santiago, T.; Farias, L.M.; Magalhaes, P.P.; Silveira, L.B.; Almeida Lopes, L.; et al. In vitro evaluation of physical and chemical parameters involved in aPDT of Aggregatibacter actinomycetemcomitans. Lasers Med. Sci. 2022, 37, 391–401. [Google Scholar] [CrossRef]
- Akram, Z.; Shafqat, S.S.; Niaz, M.O.; Raza, A.; Naseem, M. Clinical efficacy of photodynamic therapy and laser irradiation as an adjunct to open flap debridement in the treatment of chronic periodontitis: A systematic review and meta-analysis. Photodermatol. Photoimmunol. Photomed. 2020, 36, 3–13. [Google Scholar] [CrossRef]
- Bassir, S.H.; Moslemi, N.; Jamali, R.; Mashmouly, S.; Fekrazad, R.; Chiniforush, N.; Shamshiri, A.R.; Nowzari, H. Photoactivated disinfection using light-emitting diode as an adjunct in the management of chronic periodontitis: A pilot double-blind split-mouth randomized clinical trial. J. Clin. Periodontol. 2013, 40, 65–72. [Google Scholar] [CrossRef]
- Pulikkotil, S.J.; Toh, C.G.; Mohandas, K.; Leong, K. Effect of photodynamic therapy adjunct to scaling and root planing in periodontitis patients: A randomized clinical trial. Aust. Dent. J. 2016, 61, 440–445. [Google Scholar] [CrossRef] [PubMed]
- Husejnagic, S.; Lettner, S.; Laky, M.; Georgopoulos, A.; Moritz, A.; Rausch-Fan, X. Photoactivated disinfection in periodontal treatment: A randomized controlled clinical split-mouth trial. J. Periodontol. 2019, 90, 1260–1269. [Google Scholar] [CrossRef] [PubMed]
- Harmouche, L.; Courval, A.; Mathieu, A.; Petit, C.; Huck, O.; Severac, F.; Davideau, J.L. Impact of tooth-related factors on photodynamic therapy effectiveness during active periodontal therapy: A 6-months split-mouth randomized clinical trial. Photodiagnosis Photodyn. Ther. 2019, 27, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Mongardini, C.; Di Tanna, G.L.; Pilloni, A. Light-activated disinfection using a light-emitting diode lamp in the red spectrum: Clinical and microbiological short-term findings on periodontitis patients in maintenance. A randomized controlled split-mouth clinical trial. Lasers Med. Sci. 2014, 29, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Goh, E.X.; Tan, K.S.; Chan, Y.H.; Lim, L.P. Effects of root debridement and adjunctive photodynamic therapy in residual pockets of patients on supportive periodontal therapy: A randomized split-mouth trial. Photodiagnosis. Photodyn. Ther. 2017, 18, 342–348. [Google Scholar] [CrossRef]
- Hormdee, D.; Rinsathorn, W.; Puasiri, S.; Jitprasertwong, P. Anti-early stage of bacterial recolonization effect of curcuma longa extract as photodynamic adjunctive treatment. Int. J. Dent. 2020, 2020, 8823708. [Google Scholar] [CrossRef]
- Ivanaga, C.A.; Miessi, D.M.J.; Nuernberg, M.A.A.; Claudio, M.M.; Garcia, V.G.; Theodoro, L.H. Antimicrobial photodynamic therapy (aPDT) with curcumin and LED, as an enhancement to scaling and root planing in the treatment of residual pockets in diabetic patients: A randomized and controlled split-mouth clinical trial. Photodiagnosis Photodyn. Ther. 2019, 27, 388–395. [Google Scholar] [CrossRef]
- Bashkatov, A.; Genina, E.; Kochubey, V.; Tuchin, V. Optical properties of human skin, subcutaneous and mucous tissues in the wavelength range from 400 to 2000 nm. J. Phys. D Appl. Phys. 2005, 38, 2543–2555. [Google Scholar] [CrossRef]
- Ronay, V.; Buchalla, W.; Sahrmann, P.; Attin, T.; Schmidlin, P.R. In vitro evaluation of the oxidation efficacy of transgingival photodynamic therapy. Acta Odontol. Scand. 2013, 71, 1216–1220. [Google Scholar] [CrossRef]
- Wenzler, J.S.; Bocher, S.; Frankenberger, R.; Braun, A. Feasibility of transgingival laser irradiation for antimicrobial photodynamic therapy. Photodiagnosis Photodyn. Ther. 2019, 28, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, Y.; Hayashi, J.I.; Fujimura, T.; Iwamura, Y.; Yamamoto, G.; Nishida, E.; Ohno, T.; Okada, K.; Yamamoto, H.; Kikuchi, T.; et al. New irradiation method with indocyanine green-loaded nanospheres for inactivating periodontal pathogens. Int. J. Mol. Sci. 2017, 18, 154. [Google Scholar] [CrossRef] [PubMed]
- Schär, D.; Ramseier, C.A.; Eick, S.; Mettraux, G.; Salvi, G.E.; Sculean, A. Transgingival photodynamic therapy (tg-aPDT) adjunctive to subgingival mechanical instrumentation in supportive periodontal therapy. A randomized controlled clinical study. Photodiagnosis Photodyn. Ther. 2020, 32, 101971. [Google Scholar] [CrossRef] [PubMed]
- Ichinose-Tsuno, A.; Aoki, A.; Takeuchi, Y.; Kirikae, T.; Shimbo, T.; Lee, M.C.; Yoshino, F.; Maruoka, Y.; Itoh, T.; Ishikawa, I.; et al. Antimicrobial photodynamic therapy suppresses dental plaque formation in healthy adults: A randomized controlled clinical trial. BMC Oral Health 2014, 14, 152. [Google Scholar] [CrossRef] [PubMed]
- Hasanain, F.A.; Nassar, H.M. Utilizing Light Cure Units: A Concise Narrative Review. Polymers 2021, 13, 1596. [Google Scholar] [CrossRef] [PubMed]
- Kunz, D.; Wirth, J.; Sculean, A.; Eick, S. In- vitro-activity of additive application of hydrogen peroxide in antimicrobial photodynamic therapy using LED in the blue spectrum against bacteria and biofilm associated with periodontal disease. Photodiagnosis Photodyn. Ther. 2019, 26, 306–312. [Google Scholar] [CrossRef]
- Yuan, L.; Wang, Y.; Zong, Y.; Dong, F.; Zhang, L.; Wang, G.; Dong, H.; Wang, Y. Response of genes related to iron and porphyrin transport in Porphyromonas gingivalis to blue light. J. Photochem. Photobiol. B 2023, 241, 112670. [Google Scholar] [CrossRef]
- Chui, C.; Aoki, A.; Takeuchi, Y.; Sasaki, Y.; Hiratsuka, K.; Abiko, Y.; Izumi, Y. Antimicrobial effect of photodynamic therapy using high-power blue light-emitting diode and red-dye agent on Porphyromonas gingivalis. J. Periodontal Res. 2013, 48, 696–705. [Google Scholar] [CrossRef]
- Uekubo, A.; Hiratsuka, K.; Aoki, A.; Takeuchi, Y.; Abiko, Y.; Izumi, Y. Effect of antimicrobial photodynamic therapy using rose bengal and blue light-emitting diode on Porphyromonas gingivalis in vitro: Influence of oxygen during treatment. Laser Ther. 2016, 25, 299–308. [Google Scholar] [CrossRef]
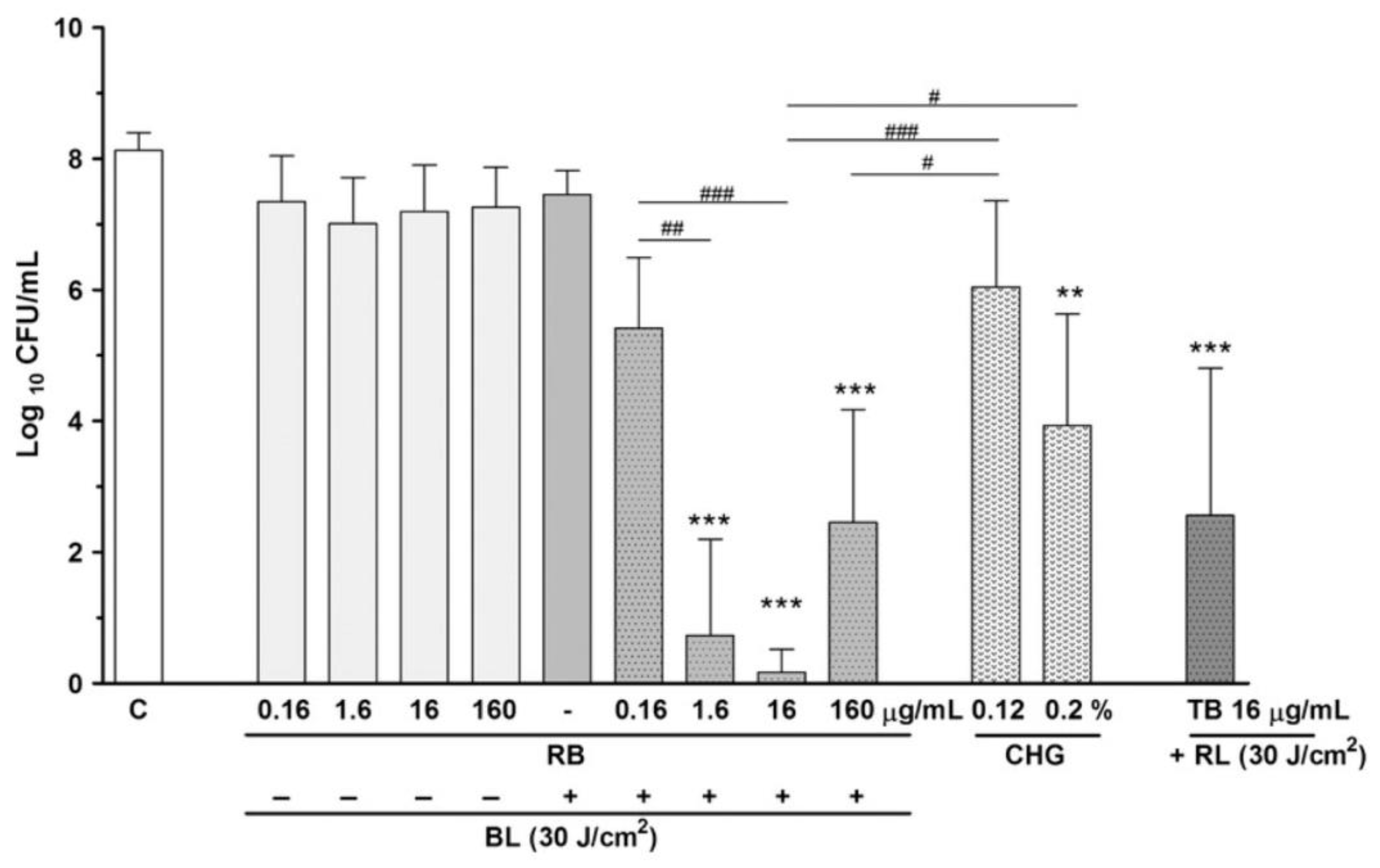
- Wang, D.; Pan, H.; Yan, Y.; Zhang, F. Rose bengal-mediated photodynamic inactivation against periodontopathogens in vitro. Photodiagnosis Photodyn. Ther. 2021, 34, 102250. [Google Scholar] [CrossRef]
- Najafi, S.; Khayamzadeh, M.; Paknejad, M.; Poursepanj, G.; Kharazi Fard, M.J.; Bahador, A. An in vitro comparison of antimicrobial effects of curcumin-based photodynamic therapy and chlorhexidine, on Aggregatibacter actinomycetemcomitans. J. Lasers Med. Sci. 2016, 7, 21–25. [Google Scholar] [CrossRef] [PubMed]
- Mahdi, Z.; Habiboallh, G.; Mahbobeh, N.N.; Mina, Z.J.; Majid, Z.; Nooshin, A. Lethal effect of blue light-activated hydrogen peroxide, curcumin and erythrosine as potential oral photosensitizers on the viability of Porphyromonas gingivalis and Fusobacterium nucleatum. Laser Ther. 2015, 24, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Saitawee, D.; Teerakapong, A.; Morales, N.P.; Jitprasertwong, P.; Hormdee, D. Photodynamic therapy of Curcuma longa extract stimulated with blue light against Aggregatibacter actinomycetemcomitans. Photodiagnosis Photodyn. Ther. 2018, 22, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Lin, J.; Zhang, Z.; Xu, B.; Bi, L. Antimicrobial effect of photodynamic therapy using sinoporphyrin sodium and 390-400 nm light-emitting diode on Porphyromonas gingivalis in vitro. Lasers Med. Sci. 2021, 36, 153–164. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, A.; Inaba, K.; Sasaki, H.; Hamada, N.; Yoshino, F. Impact on Porphyromonas gingivalis of antimicrobial photodynamic therapy with blue light and Rose Bengal in plaque-disclosing solution. Photodiagnosis Photodyn. Ther. 2021, 36, 102576. [Google Scholar] [CrossRef] [PubMed]
- Soukos, N.S.; Som, S.; Abernethy, A.D.; Ruggiero, K.; Dunham, J.; Lee, C.; Doukas, A.G.; Goodson, J.M. Phototargeting oral black-pigmented bacteria. Antimicrob. Agents Chemother. 2005, 49, 1391–1396. [Google Scholar] [CrossRef]
- Feuerstein, O.; Ginsburg, I.; Dayan, E.; Veler, D.; Weiss, E.I. Mechanism of visible light phototoxicity on Porphyromonas gingivalis and Fusobacterium nucleatum. Photochem. Photobiol. 2005, 81, 1186–1189. [Google Scholar] [CrossRef]
- Feuerstein, O.; Persman, N.; Weiss, E.I. Phototoxic effect of visible light on Porphyromonas gingivalis and Fusobacterium nucleatum: An in vitro study. Photochem. Photobiol. 2004, 80, 412–415. [Google Scholar] [CrossRef]
- Izzo, A.D.; Walsh, J.T. Light-induced modulation of Porphyromonas gingivalis growth. J. Photochem. Photobiol. B 2004, 77, 63–69. [Google Scholar] [CrossRef]
- Lee, J.; Song, H.Y.; Ahn, S.H.; Song, W.; Seol, Y.J.; Lee, Y.M.; Koo, K.T. In vitro investigation of the antibacterial and anti-inflammatory effects of LED irradiation. J. Periodontal Implant Sci. 2022, 53, 110–119. [Google Scholar] [CrossRef]
- Soukos, N.S.; Mulholland, S.E.; Socransky, S.S.; Doukas, A.G. Photodestruction of human dental plaque bacteria: Enhancement of the photodynamic effect by photomechanical waves in an oral biofilm model. Lasers Surg. Med. 2003, 33, 161–168. [Google Scholar] [CrossRef]
- Enwemeka, C.S. Antimicrobial blue light: An emerging alternative to antibiotics. Photomed. Laser Surg. 2013, 31, 509–511. [Google Scholar] [CrossRef]
- Enwemeka, C.S.; Bumah, V.V.; Castel, J.C.; Suess, S.L. Pulsed blue light, saliva and curcumin significantly inactivate human coronavirus. J. Photochem. Photobiol. B 2022, 227, 112378. [Google Scholar] [CrossRef]
- Bumah, V.V.; Morrow, B.N.; Cortez, P.M.; Bowman, C.R.; Rojas, P.; Masson-Meyers, D.S.; Suprapto, J.; Tong, W.G.; Enwemeka, C.S. The importance of porphyrins in blue light suppression of Streptococcus agalactiae. J. Photochem. Photobiol. B 2020, 212, 111996. [Google Scholar] [CrossRef]
- Ashkenazi, H.; Malik, Z.; Harth, Y.; Nitzan, Y. Eradication of Propionibacterium acnes by its endogenic porphyrins after illumination with high intensity blue light. FEMS Immunol. Med. Microbiol. 2003, 35, 17–24. [Google Scholar] [CrossRef]
- Masson-Meyers, D.S.; Bumah, V.V.; Biener, G.; Raicu, V.; Enwemeka, C.S. The relative antimicrobial effect of blue 405 nm LED and blue 405 nm laser on methicillin-resistant Staphylococcus aureus in vitro. Lasers Med. Sci. 2015, 30, 2265–2271. [Google Scholar] [CrossRef]
- Araújo, N.C.; Fontana, C.R.; Gerbi, M.E.; Bagnato, V.S. Overall-mouth disinfection by photodynamic therapy using curcumin. Photomed. Laser Surg. 2012, 30, 96–101. [Google Scholar] [CrossRef]
- Ricci Donato, H.A.; Pratavieira, S.; Grecco, C.; Brugnera-Junior, A.; Bagnato, V.S.; Kurachi, C. Clinical comparison of two photosensitizers for oral cavity decontamination. Photomed. Laser Surg. 2017, 35, 105–110. [Google Scholar] [CrossRef]
- Genina, E.A.; Titorenko, V.A.; Belikov, A.V.; Bashkatov, A.N.; Tuchin, V.V. Adjunctive dental therapy via tooth plaque reduction and gingivitis treatment by blue light-emitting diodes tooth brushing. J. Biomed. Opt. 2015, 20, 128004. [Google Scholar] [CrossRef]
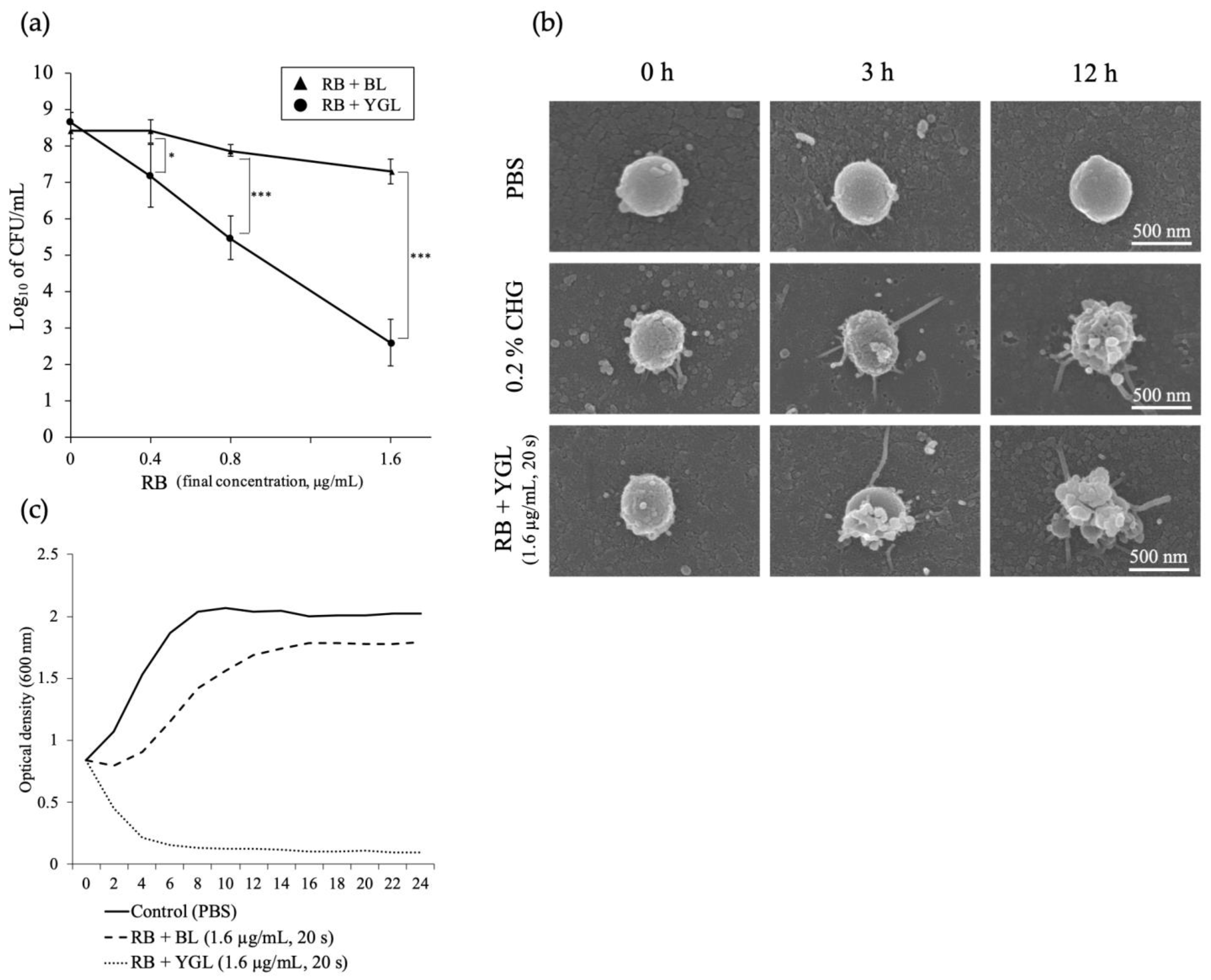
- Kitanaka, Y.; Takeuchi, Y.; Hiratsuka, K.; Aung, N.; Sakamaki, Y.; Nemoto, T.; Meinzer, W.; Izumi, Y.; Iwata, T.; Aoki, A. The effect of antimicrobial photodynamic therapy using yellow-green LED and rose bengal on Porphyromonas gingivalis. Photodiagnosis Photodyn. Ther. 2020, 32, 102033. [Google Scholar] [CrossRef]
- Crous, A.; Abrahamse, H. The signalling effects of photobiomodulation on osteoblast proliferation, maturation and differentiation: A review. Stem Cell Rev. Rep. 2021, 17, 1570–1589. [Google Scholar] [CrossRef] [PubMed]
- Batista, L.F.Z.; Kaina, B.; Meneghini, R.; Menck, C.F.M. How DNA lesions are turned into powerful killing structures: Insights from UV-induced apoptosis. Mutat. Res. 2009, 681, 197–208. [Google Scholar] [CrossRef] [PubMed]
- de Gruijl, F.R. Photocarcinogenesis: UVA vs UVB. Methods Enzymol. 2000, 319, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Pfeifer, G.P.; You, Y.H.; Besaratinia, A. Mutations induced by ultraviolet light. Mutat. Res. 2005, 571, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Takada, A.; Matsushita, K.; Horioka, S.; Furuichi, Y.; Sumi, Y. Bactericidal effects of 310 nm ultraviolet light-emitting diode irradiation on oral bacteria. BMC Oral Health 2017, 17, 96. [Google Scholar] [CrossRef] [PubMed]
- Aung, N.; Aoki, A.; Takeuchi, Y.; Hiratsuka, K.; Katagiri, S.; Kong, S.; Shujaa Addin, A.; Meinzer, W.; Sumi, Y.; Izumi, Y. The effects of ultraviolet light-emitting diodes with different wavelengths on periodontopathic bacteria in vitro. Photobiomodul. Photomed. Laser Surg. 2019, 37, 288–297. [Google Scholar] [CrossRef] [PubMed]
- Patrizi, A.; Raone, B.; Ravaioli, G.M. Management of atopic dermatitis: Safety and efficacy of phototherapy. Clin. Cosmet. Investig. Dermatol. 2015, 8, 511–520. [Google Scholar] [CrossRef]
- Shintani, Y.; Yasuda, Y.; Kobayashi, K.; Maeda, A.; Morita, A. Narrowband ultraviolet B radiation suppresses contact hypersensitivity. Photodermatol. Photoimmunol. Photomed. 2008, 24, 32–37. [Google Scholar] [CrossRef]
- Lapolla, W.; Yentzer, B.A.; Bagel, J.; Halvorson, C.R.; Feldman, S.R. A review of phototherapy protocols for psoriasis treatment. J. Am. Acad. Dermatol. 2011, 64, 936–949. [Google Scholar] [CrossRef]
- Schweintzger, N.; Gruber-Wackernagel, A.; Reginato, E.; Bambach, I.; Quehenberger, F.; Byrne, S.N.; Wolf, P. Levels and function of regulatory T cells in patients with polymorphic light eruption: Relation to photohardening. Br. J. Dermatol. 2015, 173, 519–526. [Google Scholar] [CrossRef]
- Deng, J.; Lu, C.; Zhao, Q.; Chen, K.; Ma, S.; Li, Z. The Th17/Treg cell balance: Crosstalk among the immune system, bone and microbes in periodontitis. J. Periodontal Res. 2022, 57, 246–255. [Google Scholar] [CrossRef] [PubMed]
- Ebersole, J.L.; Kirakodu, S.; Novak, M.J.; Stromberg, A.J.; Shen, S.; Orraca, L.; Gonzalez-Martinez, J.; Burgos, A.; Gonzalez, O.A. Cytokine gene expression profiles during initiation, progression and resolution of periodontitis. J. Clin. Periodontol. 2014, 41, 853–861. [Google Scholar] [CrossRef] [PubMed]
- Greene, A.C.; Shehabeldin, M.; Gao, J.; Balmert, S.C.; Ratay, M.; Sfeir, C.; Little, S.R. Local induction of regulatory T cells prevents inflammatory bone loss in ligature-induced experimental periodontitis in mice. Sci. Rep. 2022, 12, 5032. [Google Scholar] [CrossRef]
- Wang, L.; Wang, J.; Jin, Y.; Gao, H.; Lin, X. Oral administration of all-trans retinoic acid suppresses experimental periodontitis by modulating the Th17/Treg imbalance. J. Periodontol. 2014, 85, 740–750. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, A.; Shindell, E.; Jordan, F.; Baeva, L.; Pfefer, J.; Godar, D.E. UV radiation increases carcinogenic risks for oral tissues compared to skin. Photochem. Photobiol. 2013, 89, 1193–1198. [Google Scholar] [CrossRef]
- Breger, J.; Baeva, L.; Agrawal, A.; Shindell, E.; Godar, D.E. UVB-induced inflammatory cytokine release, DNA damage and apoptosis of human oral compared with skin tissue equivalents. Photochem. Photobiol. 2013, 89, 665–670. [Google Scholar] [CrossRef]
- Araújo, P.V.; Teixeira, K.I.; Lanza, L.D.; Cortes, M.E.; Poletto, L.T. In vitro lethal photosensitization of S. mutans using methylene blue and toluidine blue O as photosensitizers. Acta Odontol. Latinoam. 2009, 22, 93–97. [Google Scholar]
- Lin, J.; Bi, L.J.; Zhang, Z.G.; Fu, Y.M.; Dong, T.T. Toluidine blue-mediated photodynamic therapy of oral wound infections in rats. Lasers Med. Sci. 2010, 25, 233–238. [Google Scholar] [CrossRef]
- Haffajee, A.D.; Socransky, S.S. Microbial etiological agents of destructive periodontal diseases. Periodontol. 2000 1994, 5, 78–111. [Google Scholar] [CrossRef]
- Hajishengallis, G.; Lamont, R.J. Polymicrobial communities in periodontal disease: Their quasi-organismal nature and dialogue with the host. Periodontol. 2000 2021, 86, 210–230. [Google Scholar] [CrossRef]
- Arany, P.R. Craniofacial wound healing with photobiomodulation therapy: New insights and current challenges. J. Dent. Res. 2016, 95, 977–984. [Google Scholar] [CrossRef] [PubMed]
- Dompe, C.; Moncrieff, L.; Matys, J.; Grzech-Lesniak, K.; Kocherova, I.; Bryja, A.; Bruska, M.; Dominiak, M.; Mozdziak, P.; Skiba, T.H.I.; et al. Photobiomodulation-underlying mechanism and clinical applications. J. Clin. Med. 2020, 9, 1724. [Google Scholar] [CrossRef] [PubMed]
- Lesniewski, A.; Estrin, N.; Romanos, G.E. Comparing the use of diode lasers to light-emitting diode phototherapy in oral soft and hard tissue procedures: A literature review. Photobiomodul. Photomed. Laser Surg. 2022, 40, 522–531. [Google Scholar] [CrossRef] [PubMed]
- Nikinmaa, S.; Alapulli, H.; Auvinen, P.; Vaara, M.; Rantala, J.; Kankuri, E.; Sorsa, T.; Meurman, J.; Patila, T. Dual-light photodynamic therapy administered daily provides a sustained antibacterial effect on biofilm and prevents Streptococcus mutans adaptation. PLoS ONE 2020, 15, e0232775. [Google Scholar] [CrossRef] [PubMed]
- Street, C.N.; Pedigo, L.A.; Loebel, N.G. Energy dose parameters affect antimicrobial photodynamic therapy-mediated eradication of periopathogenic biofilm and planktonic cultures. Photomed. Laser Surg. 2010, 28, S61–S66. [Google Scholar] [CrossRef] [PubMed]
- de Freitas, M.T.M.; Soares, T.T.; Aragao, M.G.B.; Lima, R.A.; Duarte, S.; Zanin, I.C.J. Effect of photodynamic antimicrobial chemotherapy on mono- and multi-species cariogenic biofilms: A literature review. Photomed. Laser Surg. 2017, 35, 239–245. [Google Scholar] [CrossRef]
- Teixeira, A.H.; Pereira, E.S.; Rodrigues, L.K.; Saxena, D.; Duarte, S.; Zanin, I.C. Effect of photodynamic antimicrobial chemotherapy on in vitro and in situ biofilms. Caries Res. 2012, 46, 549–554. [Google Scholar] [CrossRef]
- Petelin, M.; Perkic, K.; Seme, K.; Gaspirc, B. Effect of repeated adjunctive antimicrobial photodynamic therapy on subgingival periodontal pathogens in the treatment of chronic periodontitis. Lasers Med. Sci. 2015, 30, 1647–1656. [Google Scholar] [CrossRef]
- Ramanauskaite, E.; Moraschini, V.; Machiulskiene, V.; Sculean, A. Clinical efficacy of single and multiple applications of antimicrobial photodynamic therapy in periodontal maintenance: A systematic review and network meta-analysis. Photodiagnosis Photodyn. Ther. 2021, 36, 102435. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Takeuchi, Y.; Aoki, A.; Hiratsuka, K.; Chui, C.; Ichinose, A.; Aung, N.; Kitanaka, Y.; Hayashi, S.; Toyoshima, K.; Iwata, T.; et al. Application of Different Wavelengths of LED Lights in Antimicrobial Photodynamic Therapy for the Treatment of Periodontal Disease. Antibiotics 2023, 12, 1676. https://doi.org/10.3390/antibiotics12121676
Takeuchi Y, Aoki A, Hiratsuka K, Chui C, Ichinose A, Aung N, Kitanaka Y, Hayashi S, Toyoshima K, Iwata T, et al. Application of Different Wavelengths of LED Lights in Antimicrobial Photodynamic Therapy for the Treatment of Periodontal Disease. Antibiotics. 2023; 12(12):1676. https://doi.org/10.3390/antibiotics12121676
Chicago/Turabian StyleTakeuchi, Yasuo, Akira Aoki, Koichi Hiratsuka, Chanthoeun Chui, Akiko Ichinose, Nay Aung, Yutaro Kitanaka, Sakura Hayashi, Keita Toyoshima, Takanori Iwata, and et al. 2023. "Application of Different Wavelengths of LED Lights in Antimicrobial Photodynamic Therapy for the Treatment of Periodontal Disease" Antibiotics 12, no. 12: 1676. https://doi.org/10.3390/antibiotics12121676
APA StyleTakeuchi, Y., Aoki, A., Hiratsuka, K., Chui, C., Ichinose, A., Aung, N., Kitanaka, Y., Hayashi, S., Toyoshima, K., Iwata, T., & Arakawa, S. (2023). Application of Different Wavelengths of LED Lights in Antimicrobial Photodynamic Therapy for the Treatment of Periodontal Disease. Antibiotics, 12(12), 1676. https://doi.org/10.3390/antibiotics12121676









