A National Survey of Dispensing Practice and Customer Knowledge on Antibiotic Use in Vietnam and the Implications
Abstract
:1. Introduction
2. Results
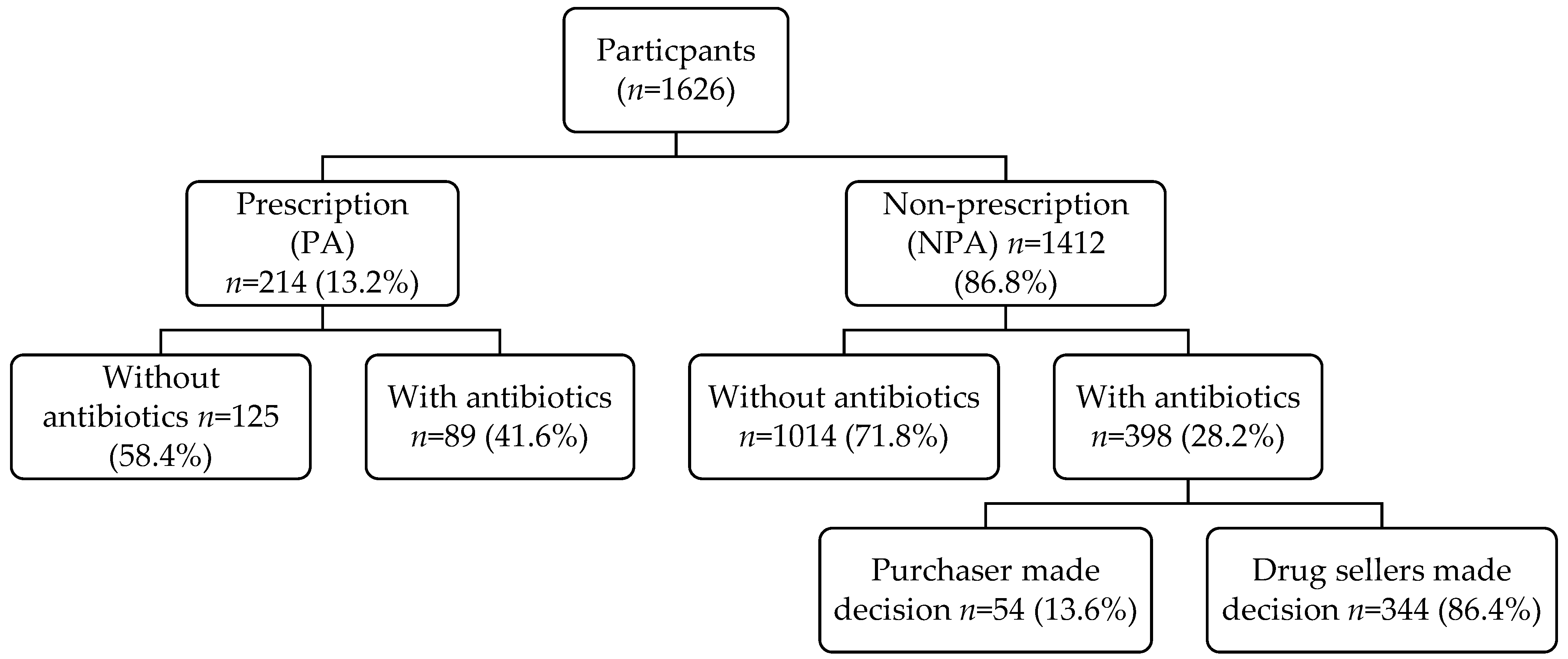
2.1. Study Population
2.2. Demographic Characteristics of Participants Purchasing Antibiotics
2.3. Pathological Classification for Purchased Antibiotics
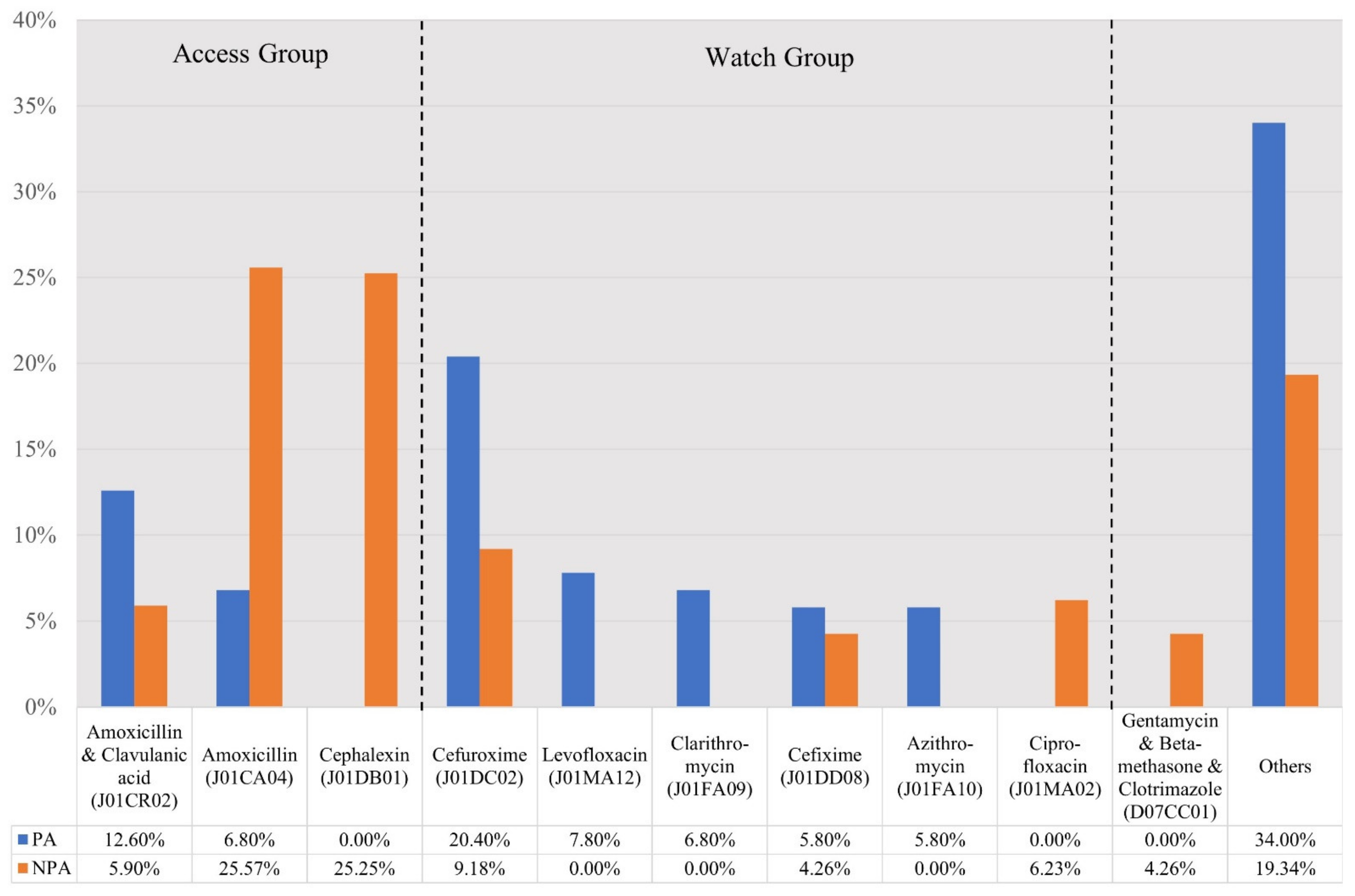
2.4. Type of Antibiotics Dispensed
2.5. Knowledge of Customers about Antibiotics
2.6. The Relationship between Participants’ Demographic Characteristics and Their Purchasing of Antibiotics
3. Discussion
Study Limitations
4. Materials and Methods
4.1. Study Setting
4.2. Ethical Considerations, Data Collection and Sample Population and Data Collection
4.3. Study Questionnaire
4.4. Data Management and Statistical Analysis
5. Conclusions and Recommendations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Antimicrobial Resistance Global Report on Surveillance: 2014 Summary. Available online: https://www.who.int/publications/i/item/WHO-HSE-PED-AIP-2014.2 (accessed on 28 June 2022).
- Llor, C.; Bjerrum, L. Antimicrobial resistance: Risk associated with antibiotic overuse and initiatives to reduce the problem. Ther. Adv. Drug Saf. 2014, 5, 229–241. [Google Scholar] [CrossRef] [PubMed]
- Murray, C.J.L.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Robles Aguilar, G.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; et al. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef]
- Inoue, H. Strategic approach for combating antimicrobial resistance (AMR). Glob. Health Med. 2019, 1, 61–64. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, J. Review on Antimicrobial Resistance. Antimicrobial Resistance: Tackling a Crisis for the Health and Wealth of Nations. 2014. Available online: https://iiif.wellcomecollection.org/file/b28552179_AMR%20Tackling%20a%20crisis%20for%20the%20health%20and%20wealth%20of%20nations.pdf (accessed on 27 June 2022).
- Hofer, U. The cost of antimicrobial resistance. Nat. Rev. Microbiol. 2019, 17, 3. [Google Scholar] [CrossRef]
- The World Bank. Drug-Resistant Infections: A Threat to Our Economic Future. 2017. Available online: https://documents1.worldbank.org/curated/en/323311493396993758/pdf/final-report.pdf (accessed on 28 June 2022).
- Alhomoud, F.; Aljamea, Z.; Almahasnah, R.; Alkhalifah, K.; Basalelah, L.; Alhomoud, F.K. Self-medication and self-prescription with antibiotics in the Middle East-do they really happen? A systematic review of the prevalence, possible reasons, and outcomes. Int. J. Infect. Dis. 2017, 57, 3–12. [Google Scholar] [CrossRef]
- Ocan, M.; Obuku, E.A.; Bwanga, F.; Akena, D.; Richard, S.; Ogwal-Okeng, J.; Obua, C. Household antimicrobial self-medication: A systematic review and meta-analysis of the burden, risk factors and outcomes in developing countries. BMC Public Health 2015, 15, 742. [Google Scholar] [CrossRef]
- Auta, A.; Hadi, M.A.; Oga, E.; Adewuyi, E.O.; Abdu-Aguye, S.N.; Adeloye, D.; Strickland-Hodge, B.; Morgan, D.J. Global access to antibiotics without prescription in community pharmacies: A systematic review and meta-analysis. J. Infect. 2019, 78, 8–18. [Google Scholar] [CrossRef]
- Godman, B.; Egwuenu, A.; Haque, M.; Malande, O.O.; Schellack, N.; Kumar, S.; Saleem, Z.; Sneddon, J.; Hoxha, I.; Islam, S. Strategies to improve antimicrobial utilization with a special focus on developing countries. Life 2021, 11, 528. [Google Scholar] [CrossRef]
- Jacobs, T.G.; Robertson, J.; van den Ham, H.A.; Iwamoto, K.; Pedersen, H.B.; Mantel-Teeuwisse, A.K. Assessing the impact of law enforcement to reduce over-the-counter (OTC) sales of antibiotics in low-and middle-income countries; a systematic literature review. BMC Health Serv. Res. 2019, 19, 536. [Google Scholar] [CrossRef]
- Nguyen, C.; Grappasonni, I.; Scuri, S.; Nguyen, B.; Nguyen, T.; Petrelli, F. Immunization in Vietnam. Ann. Ig. 2019, 31, 291–305. [Google Scholar]
- Batista, A.D.; A Rodrigues, D.; Figueiras, A.; Zapata-Cachafeiro, M.; Roque, F.; Herdeiro, M.T. Antibiotic dispensation without a prescription worldwide: A systematic review. Antibiotics 2020, 9, 786. [Google Scholar] [CrossRef]
- Belachew, S.A.; Hall, L.; Erku, D.A.; Selvey, L.A. No prescription? No problem: Drivers of non-prescribed sale of antibiotics among community drug retail outlets in low and middle income countries: A systematic review of qualitative studies. BMC Public Health 2021, 21, 1056. [Google Scholar] [CrossRef]
- Do, N.T.; Vu, H.T.; Nguyen, C.T.; Punpuing, S.; Khan, W.A.; Gyapong, M.; Asante, K.P.; Munguambe, K.; Gómez-Olivé, F.X.; John-Langba, J. Community-based antibiotic access and use in six low-income and middle-income countries: A mixed-method approach. Lancet Glob. Health 2021, 9, e610–e619. [Google Scholar] [CrossRef]
- Shi, L.; Chang, J.; Liu, X.; Zhai, P.; Hu, S.; Li, P.; Hayat, K.; Kabba, J.A.; Feng, Z.; Yang, C. Dispensing antibiotics without a prescription for acute cough associated with common cold at community pharmacies in shenyang, northeastern china: A cross-sectional study. Antibiotics 2020, 9, 163. [Google Scholar] [CrossRef]
- Nga, D.T.T.; Chuc, N.T.; Hoa, N.P.; Hoa, N.Q.; Nguyen, N.T.; Loan, H.T.; Toan, T.K.; Phuc, H.D.; Horby, P.; Van Yen, N.; et al. Antibiotic sales in rural and urban pharmacies in northern Vietnam: An observational study. BMC Pharmacol. Toxicol. 2014, 15, 6. [Google Scholar] [CrossRef]
- Nguyen, N.V.; Do, N.T.T.; Nguyen, C.T.K.; Tran, T.K.; Ho, P.D.; Nguyen, H.H.; Vu, H.T.L.; Wertheim, H.F.L.; van Doorn, H.R.; Lewycka, S. Community-level consumption of antibiotics according to the AWaRe (Access, Watch, Reserve) classification in rural Vietnam. JAC Antimicrob. Resist. 2020, 2, dlaa048. [Google Scholar] [CrossRef]
- Vietnam Ministry of Health. Decree 176/2013/ND-CP on Administrative Sanctions in the Medical Sector; Vietnam Ministry of Health: Hanoi, Vietnam, 2013. [Google Scholar]
- Vietnam Government. Decree 45/2005/NĐ-CP NĐ-CP, Prescribing Penalties for Administrative Violations in the Medical Sector; Vietnam Government: Hanoi, Vietnam, 2005. [Google Scholar]
- Vietnam Congress. Pharmaceutical Law; No.105/2016/QH13; Vietnam Congress: Hanoi, Vietnam, 2016. [Google Scholar]
- Vietnam Ministry of Health. Circular No. 15/2011/TT-BYT on Regulations on Organization and Operation of Drug Strore Establishments; Vietnam Ministry of Health: Hanoi, Vietnam, 2011. [Google Scholar]
- Nguyen, H.T.T.; Dinh, D.X.; Nguyen, V.M. Knowledge, attitude and practices of community pharmacists regarding COVID-19: A paper-based survey in Vietnam. PLoS ONE 2021, 16, e0255420. [Google Scholar] [CrossRef]
- Vietnam Ministry of Health. Circular No. 46/2011/TT-BYT on Regulations on Good Pharmacy Practice; Vietnam Ministry of Health: Hanoi, Vietnam, 2011. [Google Scholar]
- Vietnam Ministry of Health. Health Statistics Yearbook in 2018; Vietnam Ministry of Health: Hanoi, Vietnam, 2018. [Google Scholar]
- Miller, M.; Goodman, C. Performance of retail pharmacies in low- and middle-income Asian settings: A systematic review. Health Policy Plan. 2016, 31, 940–953. [Google Scholar] [CrossRef]
- Alrasheedy, A.A.; Alsalloum, M.A.; Almuqbil, F.A.; Almuzaini, M.A.; Aba Alkhayl, B.S.; Albishri, A.S.; Alharbi, F.F.; Alharbi, S.R.; Alodhayb, A.K.; Alfadl, A.A. The impact of law enforcement on dispensing antibiotics without prescription: A multi-methods study from Saudi Arabia. Expert Rev. Anti-Infect. Ther. 2020, 18, 87–97. [Google Scholar] [CrossRef]
- Zawahir, S.; Lekamwasam, S.; Aslani, P. Factors Related to Antibiotic Supply without a Prescription for Common Infections: A Cross-Sectional National Survey in Sri Lanka. Antibiotics 2021, 10, 6. [Google Scholar] [CrossRef]
- Versporten, A.; Zarb, P.; Caniaux, I.; Gros, M.-F.; Drapier, N.; Miller, M.; Jarlier, V.; Nathwani, D.; Goossens, H.; Koraqi, A. Antimicrobial consumption and resistance in adult hospital inpatients in 53 countries: Results of an internet-based global point prevalence survey. Lancet Glob. Health 2018, 6, e619–e629. [Google Scholar] [CrossRef]
- Ha, T.V.; Nguyen, A.M.T.; Nguyen, H.S.T. Self-medication practices among Vietnamese residents in highland provinces. J. Multidiscip. Healthc. 2019, 12, 493–502. [Google Scholar] [CrossRef]
- Torres, N.; Chibi, B.; Middleton, L.; Solomon, V.; Mashamba-Thompson, T. Evidence of factors influencing self-medication with antibiotics in low and middle-income countries: A systematic scoping review. Public Health 2019, 168, 92–101. [Google Scholar] [CrossRef]
- Moura, M.L.; Boszczowski, I.; Mortari, N.; Barrozo, L.V.; Neto, F.C.; Lobo, R.D.; de Lima, A.C.P.; Levin, A.S. The impact of restricting over-the-counter sales of antimicrobial drugs: Preliminary analysis of national data. Medicine 2015, 94, e1605. [Google Scholar] [CrossRef]
- Lopes-Júnior, R.; de Sá Del Fiol, F.; Araujo, J.L.O.; de Toledo, M.I.; Barberato-Filho, S. Decrease in penicillin sales in Brazil after over-the-counter restrictions. Antimicrob. Agents Chemother. 2015, 59, 5862–5863. [Google Scholar] [CrossRef]
- Mattos, K.P.; Visacri, M.B.; Quintanilha, J.C.; Lloret, G.R.; Cursino, M.A.; Levin, A.S.; Levy, C.E.; Moriel, P. Brazil’s resolutions to regulate the sale of antibiotics: Impact on consumption and Escherichia coli resistance rates. J. Glob. Antimicrob. Resist. 2017, 10, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Santa-Ana-Tellez, Y.; Mantel-Teeuwisse, A.K.; Dreser, A.; Leufkens, H.G.; Wirtz, V.J. Impact of over-the-counter restrictions on antibiotic consumption in Brazil and Mexico. PLoS ONE 2013, 8, e75550. [Google Scholar] [CrossRef]
- Wirtz, V.; Herrera-Patino, J.; Santa-Ana-Tellez, Y.; Dreser, A.; Elseviers, M.; Vander Stichele, R. Analysing policy interventions to prohibit over-the-counter antibiotic sales in four Latin American countries. Trop. Med. Int. Health 2013, 18, 665–673. [Google Scholar] [CrossRef]
- Chang, J.; Xu, S.; Zhu, S.; Li, Z.; Yu, J.; Zhang, Y.; Zu, J.; Fang, Y.; Ross-Degnan, D. Assessment of non-prescription antibiotic dispensing at community pharmacies in China with simulated clients: A mixed cross-sectional and longitudinal study. Lancet Infect. Dis. 2019, 19, 1345–1354. [Google Scholar] [CrossRef]
- Vacca, C.P.; Niño, C.Y.; Reveiz, L. Restriction of antibiotic sales in pharmacies in Bogotá, Colombia: A descriptive study. Rev. Panam. Salud Publica 2011, 30, 586–591. [Google Scholar]
- Santa-Ana-Tellez, Y.; Mantel-Teeuwisse, A.K.; Leufkens, H.G.; Wirtz, V.J. Seasonal variation in penicillin use in Mexico and Brazil: Analysis of the impact of over-the-counter restrictions. Antimicrob. Agents Chemother. 2015, 59, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Kibuule, D.; Nambahu, L.; Sefah, I.; Kurdi, A.; Phuong, T.; Kwon, H.-Y.; Godman, B. Activities in Namibia to limit the prevalence and mortality from COVID-19 including community pharmacy activities and the implications. Sch. Acad. J. Pharm. 2021, 10, 82–92. [Google Scholar] [CrossRef]
- Kamati, M.; Godman, B.; Kibuule, D. Prevalence of self-medication for acute respiratory infections in young children in Namibia: Findings and implications. J. Res. Pharm. Pract. 2019, 8, 220. [Google Scholar]
- Marković-Peković, V.; Grubiša, N.; Burger, J.; Bojanić, L.; Godman, B. Initiatives to reduce nonprescription sales and dispensing of antibiotics: Findings and implications. J. Res. Pharm. Pract. 2017, 6, 120. [Google Scholar]
- Mokwele, R.N.; Schellack, N.; Bronkhorst, E.; Brink, A.J.; Schweickerdt, L.; Godman, B. Using mystery shoppers to determine practices pertaining to antibiotic dispensing without a prescription among community pharmacies in South Africa—A pilot survey. JAC Antimicrob. Resist. 2022, 4, dlab196. [Google Scholar] [CrossRef]
- Lei, X.; Jiang, H.; Liu, C.; Ferrier, A.; Mugavin, J. Self-Medication Practice and Associated Factors among Residents in Wuhan, China. Int. J. Environ. Res. Public Health 2018, 15, 68. [Google Scholar] [CrossRef]
- Elong Ekambi, G.A.; Okalla Ebongue, C.; Penda, I.C.; Nnanga Nga, E.; Mpondo Mpondo, E.; Eboumbou Moukoko, C.E. Knowledge, practices and attitudes on antibiotics use in Cameroon: Self-medication and prescription survey among children, adolescents and adults in private pharmacies. PLoS ONE 2019, 14, e0212875. [Google Scholar] [CrossRef]
- Alghadeer, S.; Aljuaydi, K.; Babelghaith, S.; Alhammad, A.; Alarifi, M.N. Self-medication with antibiotics in Saudi Arabia. Saudi Pharm. J. 2018, 26, 719–724. [Google Scholar] [CrossRef]
- Mukokinya, M.M.A.; Opanga, S.; Oluka, M.; Godman, B. Dispensing of antimicrobials in Kenya: A cross-sectional pilot study and its implications. J. Res. Pharm. Pract. 2018, 7, 77. [Google Scholar]
- Vietnam Ministry of Health. Guidelines for the Use of Antibiotics Issued Together with Decision No. 708/QD-BYT; Vietnam Ministry of Health: Hanoi, Vietnam, 2015. [Google Scholar]
- Do, T.; Foulon, V.; Thuy, L.; Tien, L.; Anderson, C. Factors impacting on customer satisfaction with community pharmacies in Vietnam. Pharm. Sci. Asia 2021, 14, 164–174. [Google Scholar]
- Nguyen, H.H.; Ho, D.P.; Vu, T.L.H.; Tran, K.T.; Tran, T.D.; Nguyen, T.K.C.; van Doorn, H.R.; Nadjm, B.; Kinsman, J.; Wertheim, H. “I can make more from selling medicine when breaking the rules”–understanding the antibiotic supply network in a rural community in Viet Nam. BMC Public Health 2019, 19, 1560. [Google Scholar] [CrossRef] [PubMed]
- Panda, A.; Pradhan, S.; Mohapatra, G.; Mohapatra, J. Drug-related problems associated with self-medication and medication guided by prescription: A pharmacy-based survey. Indian J. Pharmacol. 2016, 48, 515–521. [Google Scholar] [CrossRef] [PubMed]
- Bennadi, D. Self-medication: A current challenge. J. Basic Clin. Pharm. 2013, 5, 19–23. [Google Scholar] [CrossRef]
- Gerber, J.S.; Ross, R.K.; Bryan, M.; Localio, A.R.; Szymczak, J.E.; Wasserman, R.; Barkman, D.; Odeniyi, F.; Conaboy, K.; Bell, L. Association of broad-vs narrow-spectrum antibiotics with treatment failure, adverse events, and quality of life in children with acute respiratory tract infections. JAMA 2017, 318, 2325–2336. [Google Scholar] [CrossRef]
- Shallcross, L.J.; Davies, D.S.C. Antibiotic overuse: A key driver of antimicrobial resistance. Br. J. Gen. Pract. 2014, 64, 604–605. [Google Scholar] [CrossRef]
- Hussain, I.; Majeed, A.; Imran, I.; Ullah, M.; Hashmi, F.K.; Saeed, H.; Chaudhry, M.O.; Rasool, M.F. Knowledge, Attitude, and Practices Toward COVID-19 in Primary Healthcare Providers: A Cross-Sectional Study from Three Tertiary Care Hospitals of Peshawar, Pakistan. J. Community Health 2021, 46, 441–449. [Google Scholar] [CrossRef]
- Stefania, S.; Fabio, P.; Elisabetta, T.; Thi, T.C.N.; Iolanda, G. European university students of pharmacy: Survey on the use of pharmaceutical drugs. Acta Bio Med. Atenei Parm. 2019, 90, 83. [Google Scholar]
- Nguyen, C.T.T.; Scuri, S.; Nguyen, B.T.; Petrelli, F.; Grappasonni, I. Levels of understanding of the rules of correct medical usage among vietnamese pharmacy students: A cross-sectional study. J. Prev. Med. Hyg. 2018, 59, E261–E266. [Google Scholar] [CrossRef]
- Awad, A.I.; Aboud, E.A. Knowledge, Attitude and Practice towards Antibiotic Use among the Public in Kuwait. PLoS ONE 2015, 10, e0117910. [Google Scholar] [CrossRef]
- Islahudin, F.; Tamezi, A.M.; Shah, N.M. Knowledge, Attitudes and Practices about Antibiotic Use Among the General Public in Malaysia. Southeast Asian J. Trop. Med. Public Health 2014, 45, 1474–1482. [Google Scholar]
- WHO. Multi-Country Public Awareness Survey; World Health Organization: Geneva, Switzerland, 2015; Available online: https://apps.who.int/iris/handle/10665/194460 (accessed on 18 June 2022).
- WHO. Anatomical Therapeutic Chemical (ATC) Classification. Available online: https://www.who.int/tools/atc-ddd-toolkit/atc-classification (accessed on 18 June 2022).
- Sharland, M.; Pulcini, C.; Harbarth, S.; Zeng, M.; Gandra, S.; Mathur, S.; Magrini, N. Classifying antibiotics in the WHO Essential Medicines List for optimal use—be AWaRe. Lancet Infect. Dis. 2018, 18, 18–20. [Google Scholar] [CrossRef]
- Hsia, Y.; Lee, B.R.; Versporten, A.; Yang, Y.; Bielicki, J.; Jackson, C.; Newland, J.; Goossens, H.; Magrini, N.; Sharland, M.; et al. Use of the WHO Access, Watch, and Reserve classification to define patterns of hospital antibiotic use (AWaRe): An analysis of paediatric survey data from 56 countries. Lancet Glob. Health 2019, 7, e861–e871. [Google Scholar] [CrossRef]
- Schellack, N.; Strydom, M.; Pepper, M.S.; Herd, C.L.; Hendricks, C.L.; Bronkhorst, E.; Meyer, J.C.; Padayachee, N.; Bangalee, V.; Truter, I.; et al. Social Media and COVID-19-Perceptions and Public Deceptions of Ivermectin, Colchicine and Hydroxychloroquine: Lessons for Future Pandemics. Antibiotics 2022, 11, 445. [Google Scholar] [CrossRef]
| Country | Summary of Initiatives and Their Outcomes |
|---|---|
| Brazil—private and public pharmacies [33,34,35] |
|
| Chile [36,37] |
|
| China [38] |
|
| Colombia [37,39] |
|
| Mexico [36,40] |
|
| Namibia [41,42] |
|
| Republic of Srpska [43] |
|
| Saudi Arabia [28] |
|
| Sri Lanka [29] |
|
| South Africa [44] |
|
| Venezuela [37] |
|
| Characteristics | N (%) | p-Value | ||
|---|---|---|---|---|
| Prescription | Non-Prescription | Total | ||
| Median age (IQR) (n = 470) | 35 (20–78) | 35 (18–70) | 35 (18–78) | 0.511 |
| Gender (n = 480) | ||||
| Male | 29 (33.0%) | 141 (36.0%) | 170 (35.4%) | 0.593 |
| Female | 59 (67.0%) | 251 (64.0%) | 310 (64.6%) | |
| Levels of education (n = 444) | ||||
| High school or lower | 44 (55.7%) | 254 (69.6%) | 298 (67.1%) | 0.007 |
| College | 12 (15.2%) | 58 (15.9%) | 70 (15.8%) | |
| University | 23 (29.1%) | 53 (14.5%) | 76 (17.1%) | |
| Occupation (n = 465) | ||||
| Freelance work | 38 (46.3%) | 251 (65.5%) | 289 (62.2%) | <0.001 |
| Public sector employee | 21 (25.6%) | 58 (15.1%) | 79 (17.0%) | |
| Others | 23 (28.1%) | 74 (19.4%) | 97 (20.8%) | |
| Pathological Classification | N (%) | ||
|---|---|---|---|
| Prescription (n = 83) | Non-Prescription (n = 391) | Total (n = 474) | |
| Respiratory | 39 (43.8) | 260 (65.3) | 299 (61.4) |
| Digestive | 12 (13.5) | 52 (13.1) | 64 (13.1) |
| Eye | 7 (7.9) | 22 (5.5) | 29 (6.0) |
| Skin | 4 (4.5) | 17 (4.3) | 21 (4.3) |
| Genito-urinary | 6 (6.7) | 8 (2.0) | 14 (2.9) |
| Musculo-skeletal | 2 (2.2) | 8 (2.0) | 10 (2.1) |
| Ear | 2 (2.2) | 2 (0.5) | 4 (0.8) |
| Nervous | 0 (0) | 4 (1.0) | 4 (0.8) |
| Metabolism | 2 (2.2) | 1 (0.3) | 3 (0.6) |
| Pregnancy | 2 (2.2) | 1 (0.3) | 3 (0.6) |
| Others | 7 (7.8) | 16 (4.0) | 23 (4.7) |
| Questions | N (%) | p-Value | ||
|---|---|---|---|---|
| Prescription | Non-Prescription | Total | ||
| ‘According to you, it is illegal for purchasing of antibiotics without a doctor’s prescription?’ | 25 (29.8%) | 72 (19.2%) | 97 (21.1%) | 0.032 |
| ‘In the future, do you agree to visit the doctor for having a prescription when purchasing antibiotics at the pharmacy/drugstore?’ | ||||
| Agree | 56 (63.8%) | 160 (44.2%) | 216 (48.6%) | 0.000 |
| Partly agree | 17 (20.7%) | 127 (35.1%) | 144 (32.4%) | |
| Disagree/Not sure | 9 (11.0%) | 75 (20.7%) | 84 (18.9%) | |
| ‘According to you, normally, how long should antibiotics be taken?’ | 44 (50.6%) | 143 (37.6%) | 187 (40.0%) | 0.026 |
| ‘According to you, does not taking antibiotics for long enough lead to antibiotic resistance?’ | 44 (54.3%) | 164 (47.4%) | 208 (48.7%) | 0.262 |
| ‘Have you ever known/heard about “antibiotic resistance”?’ | 53 (59.6%) | 200 (53.2%) | 253 (54.4%) | 0.279 |
| ‘Is antibiotic resistance a serious problem in the community?’ | ||||
| Agree | 47 (63.5%) | 162 (50.3%) | 209 (52.8%) | 0.104 |
| Partly agree | 7 (9.5%) | 33 (10.2%) | 30 (10.1%) | |
| Disagree/Not sure | 20 (27.0%) | 127 (39.4%) | 147 (37.1%) | |
| Demographic Characteristic | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
| Gender | ||||
| Male Female | Ref. 1.143 (0.70–1.87) | 0.593 | ||
| Age | ||||
| <35 years ≥35 years | Ref. 0.919 (0.57–1.47) | 0.725 | ||
| Occupation | ||||
| Freelance work Others (Non-freelance work) | Ref. 0.436 (0.274–0.696) | 0.000 | 0.52 (0.83–0.96) | 0.017 |
| Educational level | ||||
| ≤Graduated high school College University | Ref. 0.837 (0.416–1.685) 0.399 (0.222–0.716) | 0.619 0.002 | 0.952 (0.51–2.01) 0.494 (0.25–0.96) | 0.899 0.039 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nguyen, T.T.P.; Do, T.X.; Nguyen, H.A.; Nguyen, C.T.T.; Meyer, J.C.; Godman, B.; Skosana, P.; Nguyen, B.T. A National Survey of Dispensing Practice and Customer Knowledge on Antibiotic Use in Vietnam and the Implications. Antibiotics 2022, 11, 1091. https://doi.org/10.3390/antibiotics11081091
Nguyen TTP, Do TX, Nguyen HA, Nguyen CTT, Meyer JC, Godman B, Skosana P, Nguyen BT. A National Survey of Dispensing Practice and Customer Knowledge on Antibiotic Use in Vietnam and the Implications. Antibiotics. 2022; 11(8):1091. https://doi.org/10.3390/antibiotics11081091
Chicago/Turabian StyleNguyen, Thuy Thi Phuong, Thang Xuan Do, Hoang Anh Nguyen, Cuc Thi Thu Nguyen, Johanna Catharina Meyer, Brian Godman, Phumzile Skosana, and Binh Thanh Nguyen. 2022. "A National Survey of Dispensing Practice and Customer Knowledge on Antibiotic Use in Vietnam and the Implications" Antibiotics 11, no. 8: 1091. https://doi.org/10.3390/antibiotics11081091
APA StyleNguyen, T. T. P., Do, T. X., Nguyen, H. A., Nguyen, C. T. T., Meyer, J. C., Godman, B., Skosana, P., & Nguyen, B. T. (2022). A National Survey of Dispensing Practice and Customer Knowledge on Antibiotic Use in Vietnam and the Implications. Antibiotics, 11(8), 1091. https://doi.org/10.3390/antibiotics11081091








