Abstract
Background: Poor knowledge of antibiotic use drives poor antibiotic practices, but little is known about the influence of health information orientation (HIO) on knowledge of antibiotic use in the general public. Methods: We conducted a nationally-representative population-wide cross-sectional study (November 2020–January 2021), on a proportionately stratified random sample of 2004 Singapore residents aged ≥21 years. Multivariable logistic regression analysis was performed to assess the association between HIO and knowledge of antibiotic use. Results: Forty percent of respondents had low-levels of HIO (LL-HIO); they tended to be younger, not currently married, and did not have family/friends working in the healthcare sector. Respondents with LL-HIO (aOR 1.82, 95% CI 1.32–2.51, p < 0.001) were 82% more likely to have poor knowledge of antibiotic use. In particular, older adults aged ≥50 years with LL-HIO (aOR 1.81, 95% CI [1.32–2.51], p < 0.001) were much more likely to have poor knowledge than their HL-HIO counterparts. They were also less likely to use the Internet to seek health information and had poor eHealth efficacy. Conclusion: LL-HIO is independently associated with poor knowledge of antibiotic use. Educational strategies on antibiotic use should disseminate a consistent message through both online and offline platforms, involving traditional and non-traditional healthcare and non-healthcare influencers.
1. Introduction
The discovery of penicillin by Sir Alexander Fleming in 1928 heralded the era of antibiotics, saving countless lives by treating bacterial infections in humans. However, the often poorly regulated and widespread use of antibiotics, coupled with the lack of discovery of new antibiotic classes since the 1980s [1], have led to the imminence of a post-antibiotic era where increased drug resistance renders antibiotic treatment ineffective [2,3]. Lack of public awareness and knowledge of antimicrobial resistance (AMR) and poor knowledge of appropriate antibiotic use are major drivers of inappropriate antibiotic practices [4,5,6,7,8], prompting the World Health Organization (WHO) to list the improvement of awareness and understanding of AMR as one of the five key strategies in its 2015 Global Action Plan on Antimicrobial Resistance [9].
Despite various initiatives to raise public awareness, systematic reviews found that population-wide traditional mass-media AMR campaigns to educate the general public had not resulted in significant improvements in appropriate antibiotic use [10,11,12,13]. A more nuanced approach utilising a combination of strategies that target different sub-populations is evidently necessary to address knowledge and practice gaps, and improve antibiotic stewardship in the community. This is further supported by a previous study reporting the modifying effects of age on the association between poor knowledge of antibiotic use and AMR, respectively, and poor antibiotic practices, highlighting the need to tailor educational interventions by age [14].
The presence of online and social media platforms in this digital era has greatly shaped the health information seeking behaviours (HISBs) of the general public, as these platforms provide more convenient and time-efficient options to seek out answers. Most online health information consumers reported success in obtaining answers to their health-related questions and more than one-third (40%) believed that online sources of information are credible [15]. As such, online and social media platforms could serve as alternative health information dissemination modalities to the more traditional forms of mass campaigns, posters, brochures and advertisements through mainstream media.
Health information orientation (HIO) refers to an individual’s intrinsic interest in seeking out relevant health information for the purposes of making informed decisions regarding one’s health [16]. A high level of HIO (HL-HIO) indicates a desire to increase self-efficacy through the acquisition of relevant knowledge and information. In contrast, individuals with a low level of HIO (LL-HIO) demonstrate a lower proclivity to seek out health information and prefer to receive health information passively. While associations between HIO, HISB and health behaviours have been described [17,18,19], little is known about the influence of HIO on health knowledge, in particular, knowledge of antibiotic use.
Therefore, in this study, we sought to use a nationally representative population-wide cross-sectional survey to (1) explore the relationship between HIO and knowledge of antibiotic use, and (2) understand the online HISB of sub-populations with different levels of HIO, to identify educational delivery platforms to improve the knowledge of antibiotic use in the general public.
2. Materials and Methods
2.1. Study Design and Sampling Frame
A nationally-representative population-wide cross-sectional survey was conducted between November 2020 and January 2021, on a proportionately stratified random sample of Singapore citizens and permanent residents aged ≥21 years. Households were randomly selected from addresses with at least one Singapore resident, after stratifying by their predominant race, followed by broad dwelling type. Malays and Indians were oversampled to ensure representation of these minority groups in the final dataset. The household member with the most recent birthday was invited to take part in the study.
2.2. Survey Data Collection
The survey package consisted of a hardcopy survey booklet, with instructions on how to complete the survey and also an optional web link for participants who preferred to complete the survey online. The survey was predominantly self-administered and disseminated via a drop-off/pick-up method. However, interviewers were also trained prior to data collection to administer the survey in a standardised manner for situations whereby interested participants, who were illiterate or with lower educational levels, requested assistance in completing the survey. Each uncontactable household was approached up to three times on different days and times of the week before being replaced with a neighbouring household of the same housing type.
The survey instrument was developed through the adaptation of other cross-sectional surveys reported in the literature, including the WHO Antibiotic Resistance: Multi-Country Public Awareness Survey [16,20,21,22,23], and was made available in the four main official languages: English, Malay, Mandarin, and Tamil. While the survey instrument included a wide range of questions such as self-reported antibiotic practices and experiences, attitudes towards antibiotics, antibiotic use, and AMR, only the question items on knowledge of antibiotic use, HIO, online HISB, eHealth literacy, healthy lifestyle behaviours, and adherence to infection prevention measures were used in this study. Basic demographic information was also included alongside.
Questions on HIO were based on a validated eight-item scale [16] presented on a 5-point Likert scale (1-Strongly disagree; 2-Disagree; 3-Neither agree nor disagree; 4-Agree; 5-Strongly agree). Responses to these eight statements were computed to a total composite score of 40, and respondents scoring 75% and above (i.e., score of 30 and above) were defined as having a high level of HIO (HL-HIO), while those with scores below 30 were defined as having a low level of HIO (LL-HIO). Knowledge questions on antibiotic use [20] were designed in the form of Yes/No or True/False/Don’t know, whereas questions on utilisation of online and social media platforms to determine online HISB and questions on eHealth literacy [22,23] were presented in the Yes/No format.
Questions on healthy lifestyle behaviours and adherence to infection prevention measures [16,21] were presented on a 5-point Likert scale (1-Never; 2-Rarely; 3-Occasionally; 4-Often; 5-Always). The questions on adherence to infection prevention measures were aligned with the Singapore Health Promotion Board’s F.I.G.H.T. campaign, which was rolled out in 2017 [24] to promote the adoption of good hygiene practices to help prevent the spread of infectious diseases through five key messages: Frequent hand washing, Immunisation, Go to the doctor, Home rest, Tissues and masks. Respondents were defined as having a high level of adoption of a healthy lifestyle when they provided all of the following responses to the five statements: “I consume fruits and vegetables” (Often/Always), “I smoke cigarettes” (Never), “I exercise at least three times a week” (Often/Always), “I take sugary drinks” (Never/Rarely/Occasionally), and “I have at least 7 hours of sleep every night” (Often/Always). Responses to infection prevention measures were combined with other infection prevention health-related questions in the questionnaire. Respondents were defined as having a high level of adherence to infection prevention measures according to national recommendations when they provided five out of six of the following responses: “Before the COVID-19 pandemic, I wash my hands with soap and water to prevent infections” (Often/Always), “I have received a flu vaccination in the last 12 months” (Yes), “Before the COVID-19 pandemic, when I feel unwell, I see a doctor to manage my symptoms” (Yes), “Before the COVID-19 pandemic, I stay at home and rest, when I have a cold/flu” (Often/Always), “I drink plenty of water, when I have a cold/flu” (Often/Always), and “Before the COVID-19 pandemic, I wear a mask when I have a cough or cold” (Often/Always).
2.3. Dependent Variable—Poor Knowledge of Antibiotic Use
Poor knowledge of antibiotic use was defined as not providing any of the following responses to the three statements adapted from the WHO Antibiotic Resistance: Multi-Country Public Awareness Survey [20]: “It is okay to use antibiotics that were given to a friend or family member, as long as they were used to treat the same illness” (False), “It is okay to buy the same antibiotics or request for them from a doctor, if they had helped you get better previously when you had the same symptoms” (False), and “You should stop antibiotics when you have taken all the antibiotics as directed once you have begun treatment” (Yes).
2.4. Data Analysis
Proportions were tabulated for categorical variables, whereas means (standard deviations, SD) were calculated for continuous variables and responses on a 5-point Likert scale. A chi-squared test was used to compare differences between proportions. A multivariable logistic regression was performed to assess for the independent association between HIO and poor knowledge of antibiotic use. Known confounders and other covariates, as selected through likelihood ratio tests and comparisons between the Akaike’s Information Criteria and Bayesian Information Criteria values, were included in the final regression model to adjust for potential confounding (Supplementary Table S1). Interactions between covariates were individually explored, and product terms were also included in the final model. Effect measure modification due to socio-demographic factors was further assessed. Statistical significance was defined as a p-value < 0.05. Statistical analyses were conducted in Stata version 14.0 (StataCorp LLC, College Station, TX, USA).
3. Results
3.1. Demographics of Survey Respondents
Out of 4791 households approached, 2004 (41.8%) responses were collected. Survey participants were largely similar in profile to the national population based on the 2020 Singapore Census, and the detailed breakdown is presented in Table 1.

Table 1.
Characteristics of 2004 Singapore residents surveyed between November 2020 and January 2021.
3.2. Health Information Orientation
The reliability of the HIO scale was high (Cronbach’s alpha = 0.8699). More than half of the respondents agreed or strongly agreed to each of the eight statements on HIO (Figure 1). A majority of the respondents agreed or strongly agreed that “it is important for me to be informed about health issues” (90%; mean = 4.13 [SD 0.61]), “I need to know about health issues so I can keep myself and my family healthy” (87%; mean = 4.07 [SD 0.65]) and “it is critical to be informed about health issues and stay healthy” (86%; mean = 4.05 [SD 0.65]). In total, 1203 (60%) respondents had HL-HIO.
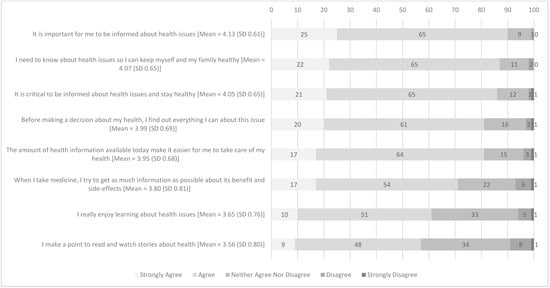
Figure 1.
Proportion of responses (%) from 2004 respondents on statements assessing health information orientation.
3.3. Characteristics of Respondents with High Level of HIO vs. Low Level of HIO
Respondents with HL-HIO and LL-HIO were found to have significant differences across several characteristics (Table 2). Compared to those with LL-HIO, respondents with HL-HIO were found to be older in age (HL-HIO 21–34 years: 28%; 35–49 years: 33%; ≥50 years: 39% vs. LL-HIO: 21–34 years: 35%; 35–49 years: 32%; ≥50 years: 33%, p = 0.001). There was a slightly smaller representation of Chinese in the HL-HIO group (70% vs. 75%, p = 0.011), whilst more were currently married in the HL-HIO group (66% vs. 58%, p < 0.001). A larger proportion of respondents in the HL-HIO group had family members or friends working in the healthcare sector (58% vs. 47%, p < 0.001) and have continuity of care with a regular doctor (65% vs. 56%, p < 0.001). Furthermore, respondents in the HL-HIO group were more likely to self-report the influence of religion on their health-seeking behaviours (30% vs. 22%, p < 0.001) and self-report their health rating as above average (69% vs. 58%, p < 0.001). They were also more likely to display high levels of adoption of a healthy lifestyle (20% vs. 11%, p < 0.001) and infection prevention measures (21% vs. 13%, p < 0.001), as compared to those in the LL-HIO group.

Table 2.
Characteristics of 2004 respondents with high level of HIO vs. low level of HIO.
3.4. Factors Associated with Poor Knowledge of Antibiotic Use
HIO, age, race, highest educational level, and marital status were independent factors associated with poor knowledge of antibiotic use (Table 3). Age was found to interact negatively with HIO (aged 35–49 years: aOR 0.67, 95% CI [0.42–1.06], n.s.; aged 21–34 years: aOR 0.61, 95% CI [0.39–0.97], p = 0.035, with reference to aged ≥50 years). Positive interactions between gender and adoption of a healthy lifestyle (Male: aOR 1.62, 95% CI [0.97–2.70], n.s.), and between self-reported influence of religion on health-seeking behaviour and continuity of care with a regular doctor (aOR 1.61, 95% CI [1.04–2.51], p = 0.034) were also observed. All interaction terms were included in the final model (Model 2).

Table 3.
Univariate and multivariable logistic regression analyses on factors associated with knowledge of antibiotic use (N = 2004).
After adjusting for potential confounders, respondents with LL-HIO (aOR 1.82, 95% CI [1.32–2.51], p < 0.001) were found to be 82% more likely to have poor knowledge of antibiotic use, as compared to those with HL-HIO. While there was an inverse dose-response relationship between age and knowledge of antibiotic use, only respondents aged 21–34 years (aOR 1.80, 95% CI [1.29–2.52], p = 0.001) were significantly more likely to have poor knowledge of antibiotic use, as compared to those aged ≥50 years. Non-Chinese (aOR 1.76, 95% CI [1.42–2.19], p < 0.001), less educated (aOR 1.86, 95% CI [1.50–2.31], p < 0.001), and those currently not married (aOR 1.28, 95% CI [1.04–1.57], p = 0.019) were also more likely to have poor knowledge of antibiotic use. Lastly, respondents without continuity of care with a regular doctor (aOR 1.17, 95% CI [0.93–1.46], n.s.) were more likely to have poor knowledge of antibiotic use.
Age modifies the effect of LL-HIO on knowledge of antibiotic use (Table 4). After adjusting for gender, race, highest educational level, marital status, continuity of care with a regular doctor, adherence to infection prevention measures, adoption of a healthy lifestyle, and self-reported influence of religion on health-seeking behaviour, we found that older adults aged ≥50 years with LL-HIO (aOR 1.81, 95% CI [1.32–2.51], p < 0.001) were 80% more likely to have poor knowledge of antibiotic use than those with HL-HIO in the same age group. Furthermore, we found that among individuals who self-reported influence of religion on their health-seeking behaviour, those who lacked continuity of care with a regular doctor (aOR 1.89, 95% CI [1.28–2.77], p = 0.001) were almost twice as likely to have poor knowledge of antibiotic use as those with continuity of care with a regular doctor (Table 5).

Table 4.
Association between poor knowledge of antibiotic use and health information orientation, according to age group (N = 2004).

Table 5.
Association between poor knowledge of antibiotic use and continuity of care with a regular doctor, according to self-reported influence of religion on health-seeking behaviour (N = 2004).
3.5. Online Health Information-Seeking Behaviours (HISBs) among Respondents with High and Low Levels of HIO
Respondents with HL-HIO were more likely to use the Internet for health-related information, as compared to those with a LL-HIO (Supplementary Table S2). Furthermore, respondents with HL-HIO also showed better self-efficacy, in particular, the ability to differentiate high-quality health resources from low-quality health resources on the Internet (60% vs. 44%, p < 0.001), and having the confidence to use information from the Internet to make health decisions (53% vs. 37%, p < 0.001).
Among those who sought health information online, the top three sources were Internet searches (69%), followed by government websites (61%), and hospitals or clinic websites (51%). Compared to respondents with LL-HIO, a significantly larger proportion of respondents with HL-HIO utilised online platforms including government websites (68% vs. 50%, p < 0.001) and hospital or clinic websites (56% vs. 42%, p < 0.001) (Figure 2).
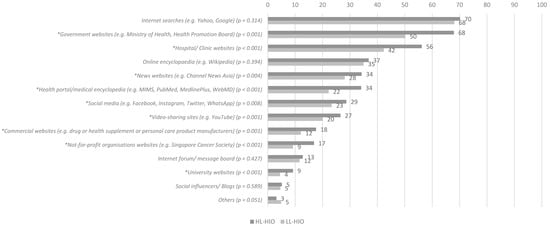
Figure 2.
Proportion (%) of 2004 respondents who utilised the following online platforms to seek health information. * indicates a statistically significant (p < 0.05) difference in proportions of respondents utilising each online platform to seek health information between HL-HIO and LL-HIO groups.
When stratified by age, respondents with LL-HIO and aged ≥50 years were least likely to utilise Internet searches (53% vs. 77% vs. 75%, p < 0.001) and hospital or clinic websites (33% vs. 46% vs. 47%, p = 0.001), as compared to respondents with LL-HIO but aged 35–49 years and 21–34 years, respectively (Supplementary Table S4). Of interest, there were no significant differences between age groups among respondents with LL-HIO on their utilisation of government websites to seek health information online (21–34 years old: 52%; 35–49 years old: 54%; ≥50 years old: 45%, p = 0.084).
4. Discussion
Our study has provided valuable insights into the positive association between HIO and knowledge of antibiotic use. Compared to individuals with HL-HIO, individuals with LL-HIO were 82% more likely to have a poor knowledge of antibiotic use. Previous studies have shown the effects of HIO on the adoption of behaviours, such as prevention against infection with the Middle East Respiratory Syndrome and on the use of health applications [25,26], but the association between HIO and health knowledge is novel. We have further elucidated the profiles of individuals with LL-HIO for targeted educational interventions. They tended to be younger in age, not currently married, without family members or friends working in the healthcare sector, and without continuity of care with a regular doctor. Younger adults tend to have diverse relationships and wide-ranging sources of information and are less likely to have healthcare encounters [27,28,29,30]. Although healthcare providers are their most trusted sources of health information, there is a need to identify and harness non-healthcare related influencers within their vast network of social contacts who could serve as trusted sources of health information [31,32,33].
Other characteristics more likely to be associated with LL-HIO are self-reported non-influence of religion on health-seeking behaviour, average or below average self-reported health rating, low-level of adoption of a healthy lifestyle and low adherence to infection prevention measures. The findings are concerning and there are calls for action to reach out to individuals with LL-HIO via passive channels of communication frequented by them, not only to increase their knowledge on antibiotic use and consequently antibiotic practice, but also to increase their adoption of healthy lifestyle and infection prevention behaviours. A previous study has shown that individuals with LL-HIO preferred passive information sources (such as the television and radio) to the Internet or newspapers/magazines [20]. Furthermore, based on the findings from a 10-year population-based survey conducted in Sweden, lower socio-economic status and lack of social support and informal caregiving were associated with poor health-seeking behaviour, i.e., seeking medical care in the study context [34]. Hence, there is a need for deeper and more extensive social outreach to actively disseminate health information, for example on appropriate antibiotic use and AMR, to these sub-populations, as they are less likely to present themselves to a healthcare facility or have interest to actively seek out health information. Contemporary communication channels such as social media posts by trusted healthcare providers, with interactive games and videos embedded could be considered to provide health information to this sub-population with LL-HIO [35].
Having LL-HIO was found to have a strong association with poor knowledge of antibiotic use, especially in adults aged ≥50 years. Only around 50% of this specific sub-population was observed to be utilising the Internet to obtain information on diseases, medications, illness and health management (Supplementary Table S3). As such, a low proportion of them reported the use of Internet-based platforms to look for health information (Supplementary Table S4), which could be attributable to poor eHealth or health literacy [15]. More than two-thirds of them were unable to differentiate the quality of Internet health resources and lacked the confidence to use these Internet-derived information to make health decisions. This suggests that for the purposes of disseminating health information, Internet-based platforms are less effective for older adults with LL-HIO due to the much lower Internet utilisation rates and barriers to utilise Internet-based information. Instead, there is a need for physical, social and healthcare touchpoints, with whom they have close and sustained relationships, to actively reach out to and educate this sub-population, using traditional non-Internet-based modalities such as posters or pamphlets and annual campaigns on appropriate antibiotic use to improve antibiotic practices [14]. Similar findings on the relationship between HIO, health information efficacy, and community participation in good preventive health behaviours have been previously reported, highlighting the importance of working with non-traditional communication platforms to reach out to specific segments of the community [36].
An interesting observation was that the continuity of care with a regular doctor halves (47%) the odds of having poor knowledge of antibiotic use in respondents who self-reported religious influence on their health-seeking behaviour, as compared to counterparts without continuity of care with a regular doctor. A study conducted in the Netherlands reported that individuals with a cultural predisposition to mistrust in information sources and have low concerns on AMR gained more awareness from an educational video developed by the National Institute for Public Health and the Environment than those who were culturally predisposed to trust and have high concerns on AMR [37]. This highlights the critical role of health authorities and healthcare professionals, such as doctors, as trusted sources of health information, and the need to empower them with tools to provide patients with accurate information on antibiotic use and AMR, through building trusting doctor-patient relationships established through continuity of care [38].
Furthermore, adults aged 21–34 years were also found to be more likely to have poor knowledge of antibiotic use. Such poor knowledge in these younger adults was previously shown to be associated with increased odds of having poor antibiotic practices by a factor of 6.6 [14]. While young adults were more likely to utilise Internet searches, government websites and hospital or clinic websites to seek health information, were confident in using the Internet to answer questions about health, and able to differentiate between high and low quality online health information (p < 0.05), their low-levels of HIO would hinder them from actively seeking out health information. Therefore, it is important for government bodies (e.g., the Ministry of Health and the Health Promotion Board), hospitals and clinics to utilise one-stop online platforms to periodically push out accurate, consistent and comprehensive health information, including that on appropriate antibiotic use [15] to avoid the need for these younger adults to have to take the extra effort to seek out information on antibiotic use.
Overall, our study supports existing literature that “one-size-fits-all” nationwide AMR campaigns are unlikely to be effective in raising awareness and improving antibiotic knowledge and practices [12,13], and highlights the importance of employing the right communication strategies for specific subpopulations due to the diversity in HIO profiles. Future AMR interventions should adopt a multi-pronged approach and employ various online and offline communications platforms and modalities, harnessing traditional and non-traditional healthcare and non-healthcare influencers.
This study has several strengths. Firstly, the proportionately stratified random sampling methodology avoided potential selection bias and cluster bias, and together with the oversampling of minority groups, a nationally representative sample population was achieved. The adaptation and incorporation of questions from validated scales and well-established questionnaires such as the eHEALS: eHealth literacy scale and WHO’s Antibiotic Resistance: Multi-Country Public Awareness Survey added to the reliability of the findings and allowed for international comparisons. The provision of survey booklets in the four main official languages in Singapore and the option for interviewer administration of the surveys further minimised selection bias by literacy and educational levels. Surveyors were also trained prior to data collection to prevent interviewer bias. Furthermore, this is the first nationally-representative survey conducted to profile HIO and assess the association of HIO with knowledge of antibiotic use to guide future interventions. However, we cannot exclude under- or over-reporting of responses due to social desirability bias, although it is likely to be reduced due to the anonymity of the survey. Also, there might be unknown and unmeasured confounders not included in the final multivariable logistic regression model. Although we are unable to draw conclusions on causality due to the cross-sectional nature of the study, we have found a strong association between HIO and knowledge of antibiotic use.
5. Conclusions
Poor knowledge on antibiotic use is associated with poor antibiotic use practices. Using a nationally representative population, we demonstrated that LL-HIO is independently associated with poor knowledge of antibiotic use, and further elucidated the profiles of individuals with LL-HIO and their online HISB. Older adults (≥50 years) with LL-HIO were most likely to have poor knowledge on antibiotic use and would benefit most from education via non-Internet-based passive information sources including regular healthcare providers and influencers within their social networks.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/antibiotics11060769/s1, Table S1: Model and variable selection for final multivariable logistic regression model assessing factors associated with poor knowledge of antibiotic use; Table S2: Proportion of 2004 respondents who agreed to the following statements on the use of the Internet to search for information on health-related matters, stratified by health information orientation; Table S3: Proportion of 2004 respondents who agreed to the following statements on the use of the Internet to search for information on health-related matters, stratified by health information orientation and age group; Table S4: Proportion of 2004 Singapore residents using different Internet-based platforms to look for health information, stratified by health information orientation and age group.
Author Contributions
Conceptualisation, A.C.; methodology, A.C.; formal analysis, H.G. and H.Y.L.; writing—original draft preparation, H.G. and H.Y.L.; writing—review and editing, A.C.; supervision, A.C.; project administration, H.G.; funding acquisition, A.C. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the National Medical Research Council Singapore, Health Services Research Grant (NMRC/HSRG/0083/2017).
Institutional Review Board Statement
Ethical approval for this study was obtained (reference number: 2017/01179) and all methods in this study were performed in accordance with the relevant guidelines and regulations from the National Healthcare Group Domain Specific Review Board, Singapore. All participants had provided informed consent to participate in the study.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
The study team would like to thank all members of the public who participated in our study, Mathew Mathews, Tan Gek Jee, Hong Gao Qiang, Er Kea Wee, Tang Hwee Noy and surveyors from Institute of Policy Studies Social Lab for their administrative and logistical support to complete the household survey, and Evonne Tay for her research administrative support to ensure the proper design and layout of the final survey booklet.
Conflicts of Interest
The authors declare that they have no competing interest.
References
- Hutching, M.; Truman, A.W.; Wilkinson, B. Antibiotics: Past, present and future. Curr. Opin. Microbiol. 2019, 51, 72–80. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Antibiotic Resistance. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance (accessed on 26 April 2022).
- Review on Antimicrobial Resistance. Antimicrobial Resistance: Tackling a Crisis for the Health and Wealth of Nations. 2014. Available online: https://amr-review.org/sites/default/files/AMR%20Review%20Paper%20-%20Tackling%20a%20crisis%20for%20the%20health%20and%20wealth%20of%20nations_1.pdf (accessed on 26 April 2022).
- Pan, D.S.T.; Huang, J.H.; Lee, M.H.M.; Yu, Y.; Chen, M.I.-C.; Goh, E.H.; Jiang, L.; Chong, J.W.C.; Leo, Y.S.; Lee, T.H.; et al. Knowledge, attitudes, and practices towards antibiotic use in upper respiratory tract infections among patients seeking primary health care in Singapore. BMC Fam. Pract. 2016, 17, 148. [Google Scholar] [CrossRef] [Green Version]
- Shaikhan, F.; Rawaf, S.; Majeed, A.; Hassounah, S. Knowledge, attitude, perception and practice regarding antimicrobial use in upper respiratory tract infections in Qatar: A systematic review. J. R. Soc. Med. 2018, 9, 2054270418774971. [Google Scholar] [CrossRef] [PubMed]
- Choo, S.J.; Chang, C.T.; Lee, J.C.-Y.; Munisamy, V.; Tan, C.K.; Raj, J.D.; Taib, R.I.M.; Thong, K.S.; A Shafie, A. A cross-sectional study on public belief, knowledge and practice towards antibiotic use in the state of Perak, Malaysia. J. Infect. Dev. Ctries. 2018, 12, 960–969. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.M.; Chhoun, P.; Tuot, S.; Om, C.; Krang, S.; Ly, S.; Hsu, L.Y.; Yi, S.; Tam, C.C. Public knowledge, attitudes and practices surrounding antibiotic use and resistance in Cambodia. JAC Antimicrob. Resist. 2021, 3, dlaa115. [Google Scholar] [CrossRef] [PubMed]
- Gillani, A.H.; Chang, J.; Aslam, F.; Saeed, A.; Shukar, S.; Khanum, F.; Jairoun, A.; Nicholson, A.; Ibrahim, M.I.M.; Fang, Y. Public knowledge, attitude, and practice regarding antibiotics use in Punjab, Pakistan: A cross-sectional study. Expert Rev. Anti-Infect. Ther. 2021, 19, 399–411. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Action Plan on Antimicrobial Resistance. 2015. Available online: https://www.who.int/publications/i/item/9789241509763 (accessed on 26 April 2022).
- Mortazhejri, S.; Hong, P.J.; Yu, A.M.; Hong, B.Y.; Stacey, D.; Bhatia, R.S.; Grimshaw, J.M. Systematic review of patient-oriented interventions to reduce unnecessary use of antibiotics for upper respiratory tract infections. Syst. Rev. 2020, 9, 106. [Google Scholar] [CrossRef]
- Castro-Sánchez, E.; Chang, P.W.; Candel, R.V.; Escobedo, A.A.; Holmes, A.H. Health literacy and infectious diseases: Why does it matter? Int. J. Infect. Dis. 2016, 43, 103–110. [Google Scholar] [CrossRef] [Green Version]
- Price, L.; Gozdzielewska, L.; Young, M.; Smith, F.; Macdonald, J.; McParland, J.; Williams, L.; Langdridge, D.; Davis, M.D.M.; Flowers, P. Effectiveness of interventions to improve the public’s antimicrobial resistance awareness and behaviours associated with prudent use of antimicrobials: A systematic review. J. Antimicrob. Chemother. 2018, 73, 1464–1478. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lim, J.M.; Singh, S.R.; Duong, M.C.; Legido-Quigley, H.; Hsu, L.Y.; Tam, C.C. Impact of national interventions to promote responsible antibiotic use: A systematic review. J. Antimicrob. Chemother. 2020, 75, 14–29. [Google Scholar] [CrossRef] [Green Version]
- Guo, H.; Hildon, Z.J.-L.; Lye, D.C.B.; Straughan, P.T.; Chow, A. The Associations between Poor Antibiotic and Antimicrobial Resistance Knowledge and Inappropriate Antibiotic Use in the General Population Are Modified by Age. Antibiotics 2022, 11, 47. [Google Scholar] [CrossRef]
- Jia, X.; Pang, Y.; Liu, L.S. Online Health Information Seeking Behavior: A Systematic Review. Healthcare 2021, 9, 1740. [Google Scholar] [CrossRef] [PubMed]
- Dutta-Bergman, M.J. Primary Sources of Health Information: Comparisons in the Domain of Health Attitudes, Health Cognitions, and Health Behaviors. Health Commun. 2004, 16, 273–288. [Google Scholar] [CrossRef]
- Dutta-Bergman, M.J. Health attitudes, health cognitions, and health behaviors among Internet health information seekers: Population-based survey. J. Med. Internet Res. 2004, 6, e15. [Google Scholar] [CrossRef]
- Sheng, X.; Simpson, P.M. Seniors, health information, and the Internet: Motivation, ability, and Internet knowledge. Cyberpsychol. Behav. Soc. Netw. 2013, 16, 740–746. [Google Scholar] [CrossRef]
- Lee, S.T.; Dutta, M.J.; Luk, P.; Kaur-Gill, S.; Lin, J. Health Orientation as a Psychographic Framework for Understanding Physical Exercise Behavior. Health Commun. 2021, 1–8. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Antibiotic Resistance: Multi-Country Public Awareness Survey. 2015. Available online: https://apps.who.int/iris/handle/10665/194460 (accessed on 26 April 2022).
- The University of Hong Kong. General Public’s Knowledge, Attitude and Practice Survey on Antimicrobial Resistance. 2017. Available online: http://chp.gov.hk/files/pdf/kap_on_amr_main_report.pdf (accessed on 26 April 2022).
- Jiang, S.; Street, R.L. Pathway Linking Internet Health Information Seeking to Better Health: A Moderated Mediation Study. Health Commun. 2017, 32, 1024–1031. [Google Scholar] [CrossRef]
- Norman, C.D.; Skinner, H.A. eHEALS: The eHealth literacy scale. J. Med. Internet Res. 2006, 8, e27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singapore Health Promotion Board. FIGHT the Spread of Infectious Diseases. 2017. Available online: https://www.healthhub.sg/programmes/52/Fight_The_Spread (accessed on 26 April 2022).
- Kim, K.; Lee, I. The Influence of Health Information Orientation, E-Health Literacy, and Anxiety on Health Behaviour among Parents with School Age Children: Focusing on MERS Prevention Behaviour. J. Nurs. Health Care 2015, 3, 2. [Google Scholar]
- Cho, J.; Park, D.; Lee, H.E. Cognitive Factors of Using Health Apps: Systematic Analysis of Relationships Among Health Consciousness, Health Information Orientation, eHealth Literacy, and Health App Use Efficacy. J. Med. Internet Res. 2014, 16, e125. [Google Scholar] [CrossRef]
- Wrzus, C.; Hänel, M.; Wagner, J.; Neyer, F.J. Social network changes and life events across the life span: A meta-analysis. Psychol. Bull. 2013, 139, 53–80. [Google Scholar] [CrossRef] [PubMed]
- Carstensen, L.L. Socioemotional selectivity theory: Social activity in life-span context. Annu. Rev. Gerontol. Geriatr. 1991, 11, 195–217. [Google Scholar]
- Carstensen, L.L. Social and emotional patterns in adulthood: Support for socioemotional selectivity theory. Psychol. Aging 1992, 7, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Carstensen, L.L. Evidence for a life-span theory of socioemotional selectivity. Curr. Dir. Psychol. Sci. 1995, 4, 151–156. [Google Scholar] [CrossRef]
- Rutgers University-Camden. Camden Barbers Become Messengers of COVID-19 Vaccine Importance, Thanks to Innovative Collaboration. 2021. Available online: https://news.camden.rutgers.edu/2021/07/camden-barbers-become-trusted-messengers-of-covid-19-vaccine-importance-thanks-to-innovative-collaboration/ (accessed on 9 May 2022).
- Eley, N.T.; Namey, E.; McKenna, K.; Johnson, A.C.; Guest, G. Beyond the Individual: Social and Cultural Influences on the Health-Seeking Behaviours of African American Men. Am. J. Mens Health 2019, 13, 1557988319829953. [Google Scholar] [CrossRef] [Green Version]
- Victor, R.G.; Lynch, K.; Li, N.; Blyler, C.; Muhammad, E.; Handler, J.; Brettler, J.; Rashid, M.; Hsu, B.; Foxx-Drew, D.; et al. A Cluster-Randomized Trial of Blood-Pressure Reduction in Black Barbershops. N. Engl. J. Med. 2018, 378, 1291–1301. [Google Scholar] [CrossRef]
- Berglund, E.; Lytsy, P.; Westerling, R. Living environment, social support, and informal caregiving are associated with healthcare seeking behaviour and adherence to medication treatment: A cross-sectional population study. Health Soc. Care Community 2019, 27, 1260–1270. [Google Scholar] [CrossRef]
- Parveen, S.; Garzon-Orjuela, N.; Amin, D.; McHugh, P.; Vellinga, A. Public Health Interventions to Improve Antimicrobial Resistance Awareness and Behavioural Change Associated with Antimicrobial Use: A Systematic Review Exploring the Use of Social Media. Antibiotics 2022, 11, 669. [Google Scholar] [CrossRef] [PubMed]
- Basu, A.; Dutta, M.J. The Relationship Between Health Information Seeking and Community Participation: The Roles of Health Information Orientation and Efficacy. Health Commun. 2008, 21, 70–79. [Google Scholar] [CrossRef]
- Van Rijn, M.; Haverkate, M.; Achterberg, P.; Timen, A. The public uptake of information about antibiotic resistance in the Netherlands. Public Underst. Sci. 2019, 28, 486–503. [Google Scholar] [CrossRef] [Green Version]
- Guo, H.; Hildon, Z.J.-L.; Loh, V.W.K.; Sundram, M.; Bin Ibrahim, M.A.; Tang, W.E.; Chow, A. Exploring antibiotic prescribing in public and private primary care settings in Singapore: A qualitative analysis informing theory and evidence-based planning for value-driven intervention design. BMC Fam. Pract. 2021, 22, 205. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).