Susceptibility Testing by Volatile Organic Compound Detection Direct from Positive Blood Cultures: A Proof-of-Principle Laboratory Study
Abstract
1. Introduction
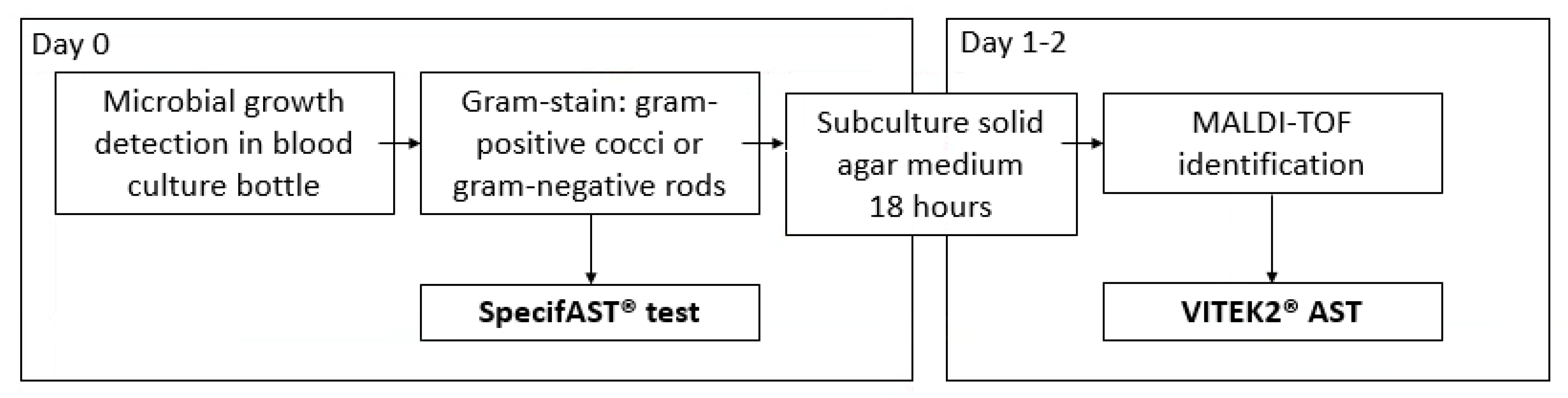
2. Methods
2.1. Objectives
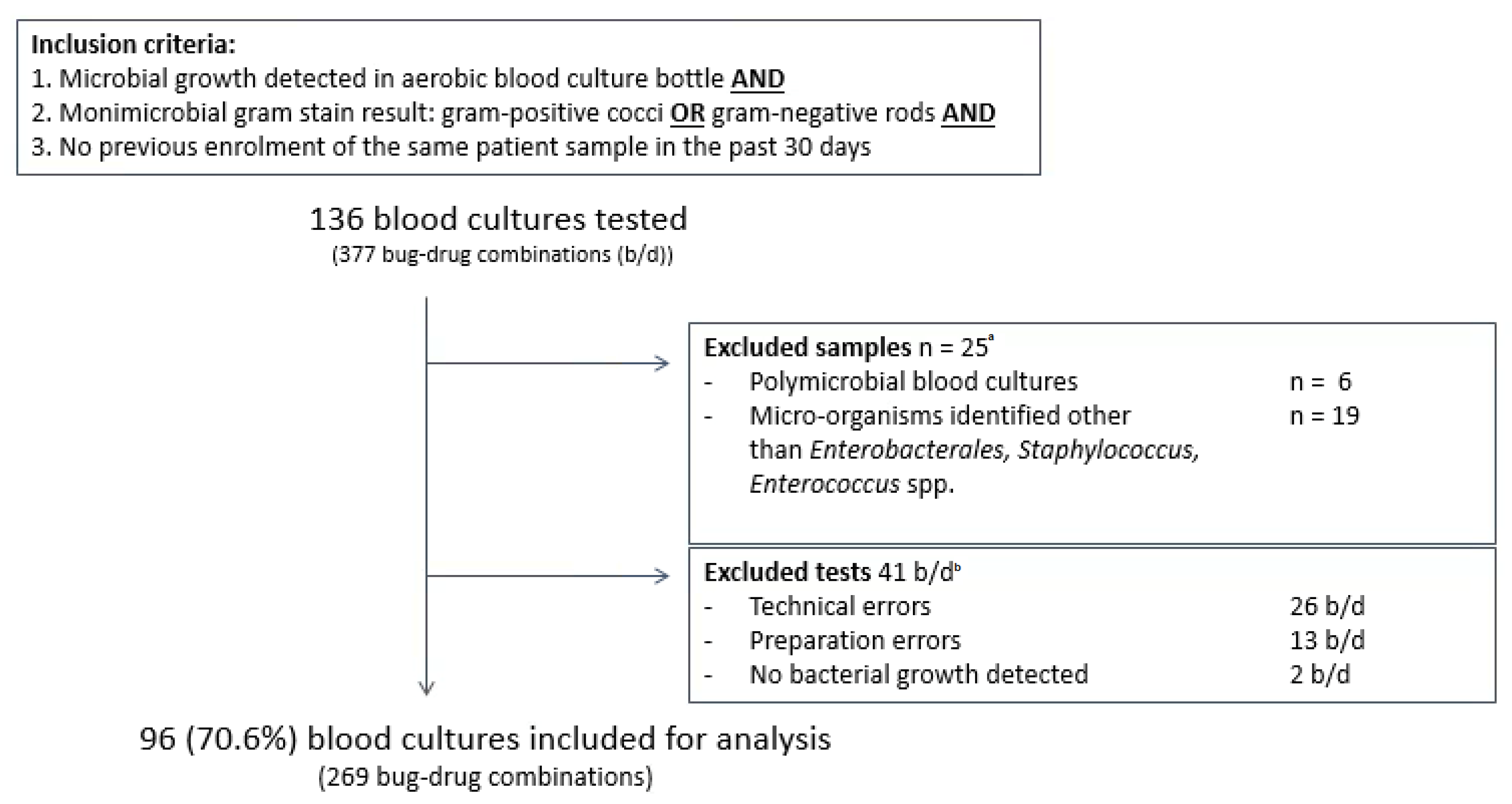
2.2. Sample Selection
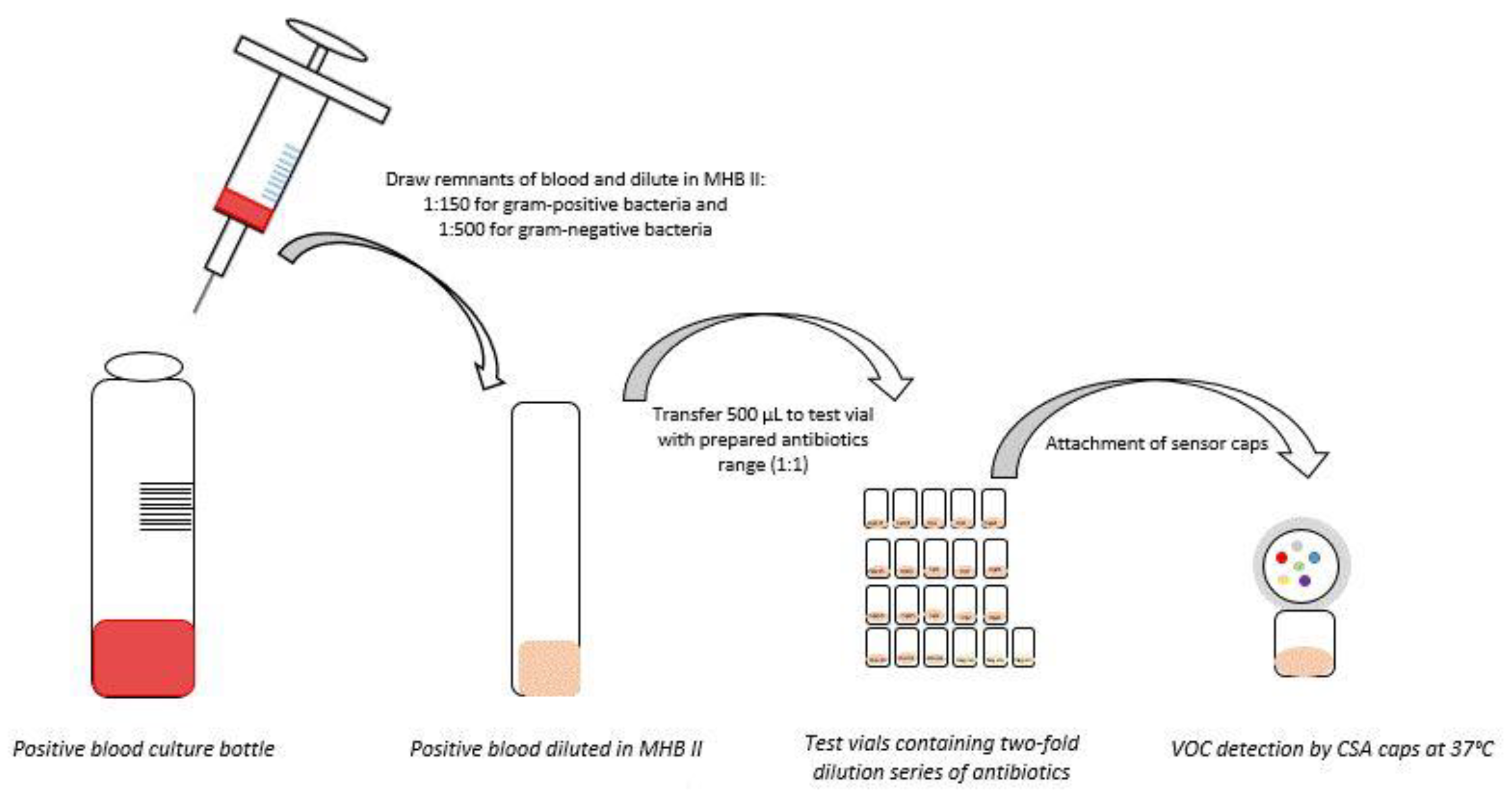
2.3. Sample Preparation for SpecifAST® Testing
2.4. SpecifAST® Testing
2.5. Comparator Method
2.6. Data Analysis
2.7. Ethical Considerations
3. Results
3.1. Primary Outcome SpecifAST® Performance
3.2. Secondary Outcomes: Analysis Time and Number of CFU
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kumar, A.; Ellis, P.; Arabi, Y.; Roberts, D.; Light, B.; Parrillo, J.E.; Dodek, P.; Wood, G.; Kumar, A.; Simon, D.; et al. Initiation of inappropriate antimicrobial therapy results in a fivefold reduction of survival in human septic shock. Chest 2009, 136, 1237–1248. [Google Scholar] [CrossRef] [PubMed]
- Adhikari, N.K.; Fowler, R.A.; Bhagwanjee, S.; Rubenfeld, G.D. Critical care and the global burden of critical illness in adults. Lancet 2010, 376, 1339–1346. [Google Scholar] [CrossRef]
- van Belkum, A.; Burnham, C.D.; Rossen, J.W.A.; Mallard, F.; Rochas, O.; Dunne, W.M., Jr. Innovative and rapid antimicrobial susceptibility testing systems. Nat. Rev. Microbiol. 2020, 18, 299–311. [Google Scholar] [CrossRef] [PubMed]
- Bard, J.D.; Lee, F. Why Can’t We Just Use PCR? The Role of Genotypic versus Phenotypic Testing for Antimicrobial Resistance Testing. Clin. Microbiol. Newslett. 2018, 40, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Dubourg, G.; Lamy, B.; Ruimy, R. Rapid phenotypic methods to improve the diagnosis of bacterial bloodstream infections: Meeting the challenge to reduce the time to result. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2018, 24, 935–943. [Google Scholar] [CrossRef]
- Machen, A.; Drake, T.; Wang, Y.F. Same day identification and full panel antimicrobial susceptibility testing of bacteria from positive blood culture bottles made possible by a combined lysis-filtration method with MALDI-TOF VITEK mass spectrometry and the VITEK2 system. PLoS ONE 2014, 9, e87870. [Google Scholar] [CrossRef]
- Romero-Gómez, M.P.; Gómez-Gil, R.; Paño-Pardo, J.R.; Mingorance, J. Identification and susceptibility testing of microorganism by direct inoculation from positive blood culture bottles by combining MALDI-TOF and Vitek-2 Compact is rapid and effective. J. Infect. 2012, 65, 513–520. [Google Scholar] [CrossRef]
- Choi, J.; Jeong, H.Y.; Lee, G.Y.; Han, S.; Han, S.; Jin, B.; Lim, T.; Kim, S.; Kim, D.Y.; Kim, H.C.; et al. Direct, rapid antimicrobial susceptibility test from positive blood cultures based on microscopic imaging analysis. Sci. Rep. 2017, 7, 1148. [Google Scholar] [CrossRef]
- Puttaswamy, S.; Gupta, S.K.; Regunath, H.; Smith, L.P.; Sengupta, S. A Comprehensive Review of the Present and Future Antibiotic Susceptibility Testing (AST) Systems. Arch. Clin. Microbiol 2018, 9, 83. [Google Scholar] [CrossRef]
- Weisskopf, L.; Schulz, S.; Garbeva, P. Microbial volatile organic compounds in intra-kingdom and inter-kingdom interactions. Nat. Rev. Microbiol. 2021, 19, 391–404. [Google Scholar] [CrossRef]
- Schulz-Bohm, K.; Martín-Sánchez, L.; Garbeva, P. Microbial Volatiles: Small Molecules with an Important Role in Intra- and Inter-Kingdom Interactions. Front. Microbiol. 2017, 8, 2484. [Google Scholar] [CrossRef] [PubMed]
- Ratiu, I.A.; Ligor, T.; Bocos-Bintintan, V.; Buszewski, B. Mass spectrometric techniques for the analysis of volatile organic compounds emitted from bacteria. Bioanalysis 2017, 9, 1069–1092. [Google Scholar] [CrossRef] [PubMed]
- Steppert, I.; Schönfelder, J.; Schultz, C.; Kuhlmeier, D. Rapid in vitro differentiation of bacteria by ion mobility spectrometry. Appl. Microbiol. Biotechnol. 2021, 105, 4297–4307. [Google Scholar] [CrossRef] [PubMed]
- Kunze-Szikszay, N.; Euler, M.; Kuhns, M.; Thieß, M.; Groß, U.; Quintel, M.; Perl, T. Headspace analyses using multi-capillary column-ion mobility spectrometry allow rapid pathogen differentiation in hospital-acquired pneumonia relevant bacteria. BMC Microbiol. 2021, 21, 69. [Google Scholar] [CrossRef] [PubMed]
- Boots, A.W.; Smolinska, A.; van Berkel, J.J.; Fijten, R.R.; Stobberingh, E.E.; Boumans, M.L.; Moonen, E.J.; Wouters, E.F.; Dallinga, J.W.; Van Schooten, F.J. Identification of microorganisms based on headspace analysis of volatile organic compounds by gas chromatography-mass spectrometry. J. Breath Res. 2014, 8, 027106. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Qiu, Z.; Wang, Y.; Yu, K.; Zheng, X.; Li, Y.; Liu, M.; Wang, G.; Guo, N.; Yang, M.; et al. Volatile Organic Compounds to Identify Infectious (Bacteria/Viruses) Diseases of the Central Nervous System: A Pilot Study. Eur. Neurol. 2021, 84, 325–332. [Google Scholar] [CrossRef]
- Maugeri, G.; Lychko, I.; Sobral, R.; Roque, A.C.A. Identification and Antibiotic-Susceptibility Profiling of Infectious Bacterial Agents: A Review of Current and Future Trends. Biotechnol. J. 2019, 14, e1700750. [Google Scholar] [CrossRef]
- Kangas, M.J.; Burks, R.M.; Atwater, J.; Lukowicz, R.M.; Williams, P.; Holmes, A.E. Colorimetric Sensor Arrays for the Detection and Identification of Chemical Weapons and Explosives. Crit. Rev. Anal. Chem. 2017, 47, 138–153. [Google Scholar] [CrossRef]
- Lim, S.H.; Mix, S.; Xu, Z.; Taba, B.; Budvytiene, I.; Berliner, A.N.; Queralto, N.; Churi, Y.S.; Huang, R.S.; Eiden, M.; et al. Colorimetric sensor array allows fast detection and simultaneous identification of sepsis-causing bacteria in spiked blood culture. J. Clin. Microbiol. 2014, 52, 592–598. [Google Scholar] [CrossRef]
- Carey, J.R.; Suslick, K.S.; Hulkower, K.I.; Imlay, J.A.; Imlay, K.R.; Ingison, C.K.; Ponder, J.B.; Sen, A.; Wittrig, A.E. Rapid identification of bacteria with a disposable colorimetric sensing array. J. Am. Chem. Soc. 2011, 133, 7571–7576. [Google Scholar] [CrossRef]
- Shrestha, N.K.; Lim, S.H.; Wilson, D.A.; SalasVargas, A.V.; Churi, Y.S.; Rhodes, P.A.; Mazzone, P.J.; Procop, G.W. The combined rapid detection and species-level identification of yeasts in simulated blood culture using a colorimetric sensor array. PLoS ONE 2017, 12, e0173130. [Google Scholar] [CrossRef]
- Smart, A.; de Lacy Costello, B.; White, P.; Avison, M.; Batty, C.; Turner, C.; Persad, R.; Ratcliffe, N. Sniffing out resistance—Rapid identification of urinary tract infection-causing bacteria and their antibiotic susceptibility using volatile metabolite profiles. J. Pharm. Biomed. Anal. 2019, 167, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Wiesner, K.; Jaremek, M.; Pohle, R.; von Sicard, O.; Stuetz, E. Monitoring of Bacterial Growth and Rapid Evaluation of Antibiotic Susceptibility by Headspace Gas Analysis. Procedia Eng. 2014, 87, 332–335. [Google Scholar] [CrossRef]
- Allardyce, R.A.; Hill, A.L.; Murdoch, D.R. The rapid evaluation of bacterial growth and antibiotic susceptibility in blood cultures by selected ion flow tube mass spectrometry. Diagn. Microbiol. Infect. Dis. 2006, 55, 255–261. [Google Scholar] [CrossRef]
- (EUCAST), E.C.o.A.S.T. Clinical Breakpoints-Breakpoints and Guidance. Available online: https://www.eucast.org/clinical_breakpoints/ (accessed on 5 July 2021).
- Humphries, R.M.; Ambler, J.; Mitchell, S.L.; Castanheira, M.; Dingle, T.; Hindler, J.A.; Koeth, L.; Sei, K. CLSI Methods Development and Standardization Working Group Best Practices for Evaluation of Antimicrobial Susceptibility Tests. J. Clin. Microbiol. 2018, 56, e01934-17. [Google Scholar] [CrossRef]
- Archer, G.L.; Scott, J. Conjugative transfer genes in staphylococcal isolates from the United States. Antimicrob. Agents Chemother. 1991, 35, 2500–2504. [Google Scholar] [CrossRef][Green Version]
- York, M.K.; Gibbs, L.; Chehab, F.; Brooks, G.F. Comparison of PCR detection of mecA with standard susceptibility testing methods to determine methicillin resistance in coagulase-negative staphylococci. J. Clin. Microbiol. 1996, 34, 249–253. [Google Scholar] [CrossRef]
- Morris, C.P.; Simner, P.J. Tailoring Antimicrobial Susceptibility Testing to Individual Species of Coagulase-Negative Staphylococci: Next Up, Staphylococcus epidermidis. J. Clin. Microbiol. 2019, 57, e01391-19. [Google Scholar] [CrossRef]
- Naccache, S.N.; Callan, K.; Burnham, C.A.; Wallace, M.A.; Westblade, L.F.; Dien Bard, J. Evaluation of Oxacillin and Cefoxitin Disk Diffusion and Microbroth Dilution Methods for Detecting mecA-Mediated β-Lactam Resistance in Contemporary Staphylococcus epidermidis Isolates. J. Clin. Microbiol. 2019, 57, e00961-19. [Google Scholar] [CrossRef]
- Archer, G.L.; Climo, M.W. Antimicrobial susceptibility of coagulase-negative staphylococci. Antimicrob. Agents Chemother. 1994, 38, 2231–2237. [Google Scholar] [CrossRef]
- Dickinson, T.M.; Archer, G.L. Phenotypic expression of oxacillin resistance in Staphylococcus epidermidis: Roles of mecA transcriptional regulation and resistant-subpopulation selection. Antimicrob. Agents Chemother. 2000, 44, 1616–1623. [Google Scholar] [CrossRef] [PubMed]
- Marsik, F.J. Antimicrobial Susceptibility Testing. In Textbook of Diagnostic Microbiology, 4th ed.; Mahon, C.R., Lehman, D.C., Manuselis, G., Eds.; Saunders Elsevier: Maryland Heights, MO, USA, 2011; pp. 276–314. [Google Scholar]
- Jorgensen, J.H.; Ferraro, M.J. Antimicrobial susceptibility testing: A review of general principles and contemporary practices. Clin. Infect. Dis. 2009, 49, 1749–1755. [Google Scholar] [CrossRef] [PubMed]
- M07-A11; Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically, 10th ed.; Approved Standard. Clinical and Laboratory Standards Institute, Wayne, PA, USA: 2018.
- Schulz-Bohm, K.; Zweers, H.; de Boer, W.; Garbeva, P. A fragrant neighborhood: Volatile mediated bacterial interactions in soil. Front. Microbiol. 2015, 6, 1212. [Google Scholar] [CrossRef] [PubMed]
- Robinson, E.D.; Stilwell, A.; Attai, A.E.; Donohue, L.E.; Shah, M.D.; Hill, B.K.; Elliott, Z.S.; Poulter, M.; Brewster, F.; Cox, H.L.; et al. Implementation of a Rapid Phenotypic Susceptibility Platform for Gram-Negative Bloodstream Infections with Paired Antimicrobial Stewardship Intervention: Is the Juice Worth the Squeeze? Clin. Infect. Dis. 2021, 73, 783–792. [Google Scholar] [CrossRef]
- Charnot-Katsikas, A.; Tesic, V.; Love, N.; Hill, B.; Bethel, C.; Boonlayangoor, S.; Beavis, K.G. Use of the Accelerate Pheno System for Identification and Antimicrobial Susceptibility Testing of Pathogens in Positive Blood Cultures and Impact on Time to Results and Workflow. J. Clin. Microbiol. 2018, 56, e01166-17. [Google Scholar] [CrossRef]
- Marschal, M.; Bachmaier, J.; Autenrieth, I.; Oberhettinger, P.; Willmann, M.; Peter, S. Evaluation of the Accelerate Pheno System for Fast Identification and Antimicrobial Susceptibility Testing from Positive Blood Cultures in Bloodstream Infections Caused by Gram-Negative Pathogens. J. Clin. Microbiol. 2017, 55, 2116–2126. [Google Scholar] [CrossRef]
| Micro-Organism Group | Antimicrobial Agent | Specifast® Concentration Range | VITEK2® Concentration Range |
|---|---|---|---|
| Enterobacterales spp. | Ciprofloxacin Cefotaxime Meropenem | 0.25–4 μg/mL 0.25–64 μg/mL 0.25–16 μg/mL | 0.25–4 μg/mL 0.25–64 μg/mL 0.25–16 μg/mL |
| Staphylococcus spp. | Oxacillin + 2% NaCl a Vancomycin Cefoxitin | 0.25–4 μg/mL 0.5–32 μg/mL 6 μg/mL | 0.25–4 μg/mL 0.5–32 μg/mL 6 μg/mL |
| Enterococcus spp. | Ampicillin Vancomycin | 2–32 μg/mL 0.5–64 μg/mL | 2–32 μg/mL 0.5–32 μg/mL |
| Enterobacterales spp. | N = 46 |
|---|---|
| Citrobacter freundii | 1 (2.2%) |
| Klebsiella aerogenes | 1 (2.2%) |
| Escherichia coli | 28 (60.9%) |
| Klebsiella pneumoniae | 9 (19.6%) |
| Klebsiella variicola | 3 (6.5%) |
| Morganella morganii | 3 (6.5%) |
| Proteus mirabilis | 1 (2.2%) |
| Salmonella typhi | 1 (2.2%) |
| Enterococcus spp. | N = 10 |
| Enterococcus faecalis | 3 (30.0%) |
| Enterococcus faecium | 7 (70%) |
| Staphylococcus spp. | N = 40 |
| Staphylococcus aureus | 12 (30.0%) |
| Staphylococcus epidermidis | 13 (32.5%) |
| Staphylococcus hominis | 11 (27.5%) |
| Staphylococcus capitis | 4 (10.0%) |
| Antimicrobial Agent | Number of Clinical Blood Cultures Tested | Number of AB Tested (B/D) | CA | VME | ME | mE | R | TTR (h) SpecifAST Mean (SD) | TTR (h) VITEK2 a Mean (SD) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Enterobacterales spp. | Cefotaxime | 45 (46.9%) | 45 (16.7%) | 45 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | 7 (15.6%) | ||
| Ciprofloxacin | 44 (45.8%) | 44 (16.4%) | 44 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | 9 (20.5%) | |||
| Meropenem | 45 (46.9%) | 45 (16.7%) | 45 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |||
| Total | 46 (47.9%) | 134 (49.8%) | 134 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | 16 (11.9%) | 2.8 (0.6) | 9.8 (2.6) | |
| Staphylococcus spp. | Cefoxitin | 38 (39.6%) | 38 (14.1%) | 34 (89.4%) | 4 (25%) | 0 (0%) | n.a. | 16 (42.1%) | ||
| Oxacillin | 39 (40.6%) | 39 (14.5%) | 34 (87.1%) | 1 (7.1%) | 4 (16%) | 0 (0%) | 14 (35.9%) | |||
| Vancomycin | 39 (40.6%) | 39 (14.5%) | 37 (94.9%) | 0 (0%) | 2 (5.1%) | 0 (0%) | 0 (0%) | |||
| Total | 40 (41.7%) | 116 (43.1%) | 105 (90.5%) | 5 (16.7%) | 6 (7.0%) | 0 (0%) | 30 (25.9%) | 3.4 (1.1) | 11.5 (2.4) | |
| Enterococcus spp. | Ampicillin | 10 (10.4%) | 9 (3.3%) | 8 (88.9%) | 0 (0%) | 0 (0%) | 1 (11.1%) | 5 (55.6%) | ||
| Vancomycin | 10 (10.4%) | 10 (3.7%) | 10 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0.4%) | |||
| Total | 10 (10.4%) | 19 (7.1%) | 18 (94.7%) | 0 (0%) | 0 (0%) | 1 (1.7%) | 6 (31.6%) | 3.2 (0.5) | 8.8 (1.6) | |
| Overall | 96 (100%) | 269 (100%) | 257 (95.5%) | 5 (9.6%) | 6 (2.8%) | 1 (0.4%) | 52 (19.3%) | 3.1 (0.9) | 10.5 (2.6) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuil, S.D.; Hidad, S.; Schneeberger, C.; Singh, P.; Rhodes, P.; de Jong, M.D.; Visser, C.E. Susceptibility Testing by Volatile Organic Compound Detection Direct from Positive Blood Cultures: A Proof-of-Principle Laboratory Study. Antibiotics 2022, 11, 705. https://doi.org/10.3390/antibiotics11060705
Kuil SD, Hidad S, Schneeberger C, Singh P, Rhodes P, de Jong MD, Visser CE. Susceptibility Testing by Volatile Organic Compound Detection Direct from Positive Blood Cultures: A Proof-of-Principle Laboratory Study. Antibiotics. 2022; 11(6):705. https://doi.org/10.3390/antibiotics11060705
Chicago/Turabian StyleKuil, Sacha Daniëlle, Soemeja Hidad, Caroline Schneeberger, Pragya Singh, Paul Rhodes, Menno Douwe de Jong, and Caroline Elisabeth Visser. 2022. "Susceptibility Testing by Volatile Organic Compound Detection Direct from Positive Blood Cultures: A Proof-of-Principle Laboratory Study" Antibiotics 11, no. 6: 705. https://doi.org/10.3390/antibiotics11060705
APA StyleKuil, S. D., Hidad, S., Schneeberger, C., Singh, P., Rhodes, P., de Jong, M. D., & Visser, C. E. (2022). Susceptibility Testing by Volatile Organic Compound Detection Direct from Positive Blood Cultures: A Proof-of-Principle Laboratory Study. Antibiotics, 11(6), 705. https://doi.org/10.3390/antibiotics11060705






