Hand Hygiene Practices during the COVID-19 Pandemic in Northern Italy: Assessment of Compliance Rates Measured by Direct Observation and Alcohol-Based Handrub Usage
Abstract
:1. Introduction
2. Results
3. Discussion
4. Materials and Methods
4.1. Study Design and Setting
4.2. HH Compliance – Definitions and Data Collection
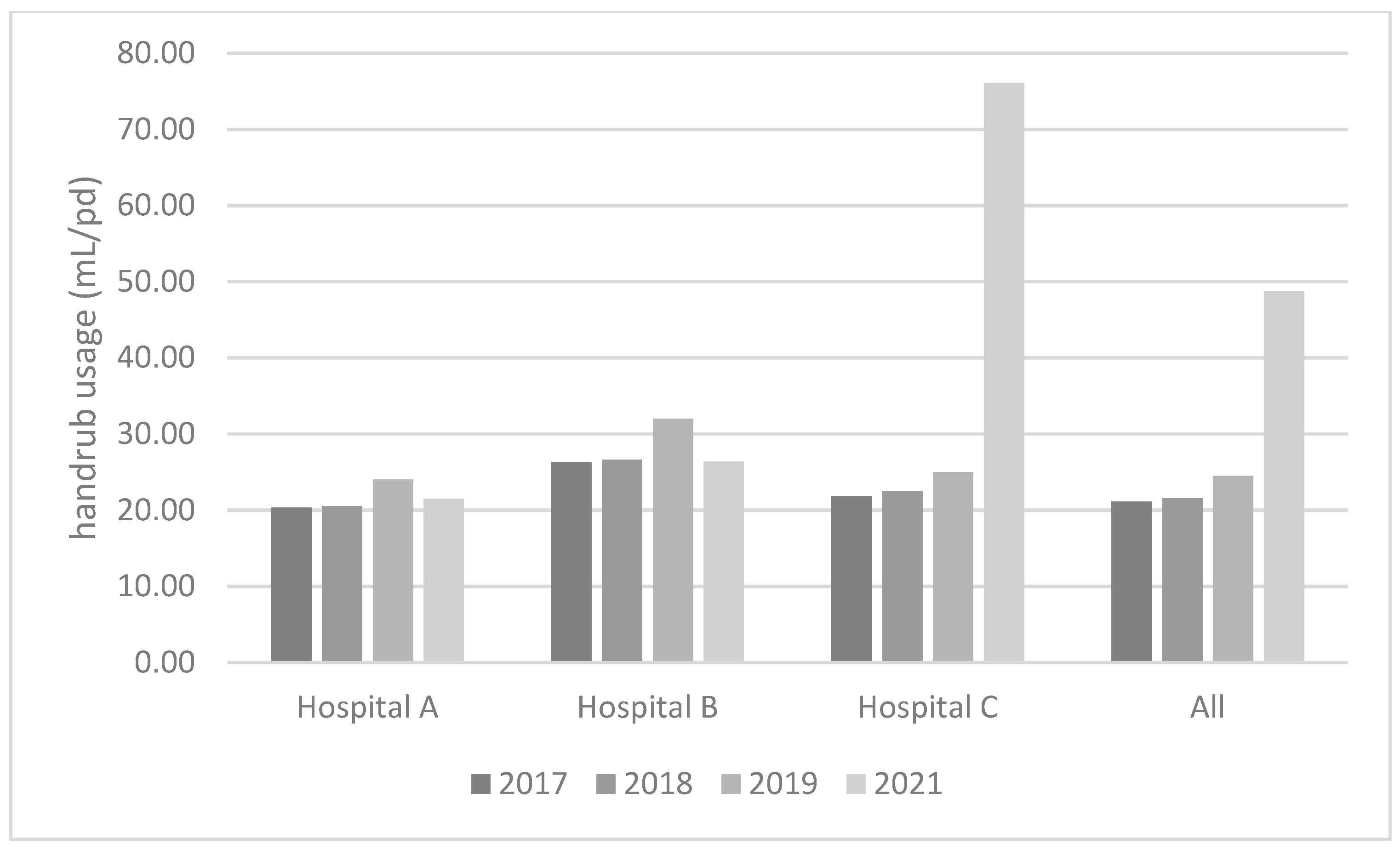
4.3. Alcohol-Based Handrub Usage
4.4. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care Is Safer Care; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Pittet, D.; Donaldson, L. Challenging the world: Patient safety and health care-associated infection. Int. J. Qual. Health Care 2006, 18, 4–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bordino, V.; Vicentini, C.; D’Ambrosio, A.; Quattrocolo, F.; Collaborating Group; Zotti, C.M. Burden of healthcare-associated infections in Italy: Incidence, attributable mortality and disability-adjusted life years (DALYs) from a nationwide study, 2016. J. Hosp. Infect. 2021, 113, 164–171. [Google Scholar] [CrossRef] [PubMed]
- Cassini, A.; Plachouras, D.; Eckmanns, T.; Abu Sin, M.; Blank, H.P.; Ducomble, T.; Haller, S.; Harder, T.; Klingeberg, A.; Sixtensson, M.; et al. Burden of Six Healthcare-Associated Infections on European Population Health: Estimating Incidence-Based Disability-Adjusted Life Years through a Population Prevalence-Based Modelling Study. PLoS Med. 2016, 13, e1002150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vicentini, C.; Bazzolo, S.; Gamba, D.; Zotti, C.M. Analysis of the Fatality Rate in Relation to Testing Capacity during the First 50 days of the COVID-19 Epidemic in Italy. Am. J. Trop. Med. Hyg. 2020, 103, 2382–2390. [Google Scholar] [CrossRef] [PubMed]
- WHO. Transmission of SARS-CoV-2: Implications for Infection Prevention Precautions; World Health Organization; Geneva, Switzerland, 2020; Available online: WHO/2019-nCoV/Sci_Brief/Transmission_modes/2020.3 (accessed on 27 September 2022).
- Wong, S.C.; AuYeung, C.Y.; Lam, G.M.; Leung, E.L.; Chan, V.M.; Yuen, K.Y.; Cheng, V.C. Is it possible to achieve 100 percent hand hygiene compliance during the coronavirus disease. J. Hosp. Infect. 2020, 105, 779–781. [Google Scholar] [CrossRef] [PubMed]
- Moore, L.D.; Robbins, G.; Quinn, J.; Arbogast, J.W. The impact of COVID-19 pandemic on hand hygiene performance in hospitals. Am. J. Infect. Control 2021, 49, 30–33. [Google Scholar] [CrossRef]
- Makhni, S.; Umscheid, C.A.; Soo, J.; Chu, V.; Bartlett, A.; Landon, E.; Marrs, R. Hand Hygiene Compliance Rate During the COVID-19 Pandemic. JAMA Intern. Med. 2021, 181, 1006–1008. [Google Scholar] [CrossRef]
- Monnet, D.L.; Harbarth, S. Will coronavirus disease (COVID-19) have an impact on antimicrobial resistance? Eurosurveillance 2020, 25, 2001886. [Google Scholar] [CrossRef]
- Stevens, M.P.; Doll, M.; Pryor, R.; Godbout, E.; Cooper, K.; Bearman, G. Impact of COVID-19 on traditional healthcare-associated infection prevention efforts. Infect. Control Hosp. Epidemiol. 2020, 41, 946–947. [Google Scholar] [CrossRef] [Green Version]
- Sax, H.; Allegranzi, B.; Uçkay, I.; Larson, E.; Boyce, J.; Pittet, D. ‘My five moments for hand hygiene’: A user-centred design approach to understand, train, monitor and report hand hygiene. J. Hosp. Infect. 2007, 67, 9–21. [Google Scholar] [CrossRef]
- Boyce, J.M. Hand hygiene compliance monitoring: Current perspectives from the USA. J. Hosp. Infect. 2008, 70, 2–7. [Google Scholar] [CrossRef]
- Lai, X.; Wang, X.; Yang, Q.; Xu, X.; Tang, Y.; Liu, C.; Tan, L.; Lai, R.; Wang, H.; Zhang, X.; et al. Will healthcare workers improve infection prevention and control behaviors as COVID-19 risk emerges and increases, in China? Antimicrob. Resist. Infect. Control 2020, 9, 83. [Google Scholar] [CrossRef]
- Kingston, L.; Connell, N.H.O.; Dunne, C.P. Hand hygiene-related clinical trials reported since 2010: A systematic review. J. Hosp. Infect. 2016, 92, 309–320. [Google Scholar] [CrossRef]
- Wetzker, W.; Walter, J.; Bunte-Schönberger, K.; Schwab, F.; Behnke, M.; Gastmeier, P.; Reichardt, C. Hand rub consumption has almost doubled in 132 german hospitals over 9 years. Infect. Control Hosp. Epidemiol. 2017, 38, 870–872. [Google Scholar] [CrossRef]
- Wetzker, W.; Bunte-Schönberger, K.; Walter, J.; Pilarski, G.; Gastmeier, P.; Reichardt, C. Compliance with hand hygiene: Reference data from the national hand hygiene campaign in Germany. J. Hosp. Infect. 2016, 92, 328–331. [Google Scholar] [CrossRef]
- Magnus, T.P.; Marra, A.R.; Camargo, T.Z.; Victor Eda, S.; da Costa, L.S.; Cardoso, V.J.; dos Santos, O.F.; Edmond, M.B. Measuring hand hygiene compliance rates in different special care settings: A comparative study of methodologies. Int. J. Infect. Dis. 2015, 33, 205–208. [Google Scholar] [CrossRef] [Green Version]
- Randle, J.; Arthur, A.; Vaughan, N. Twenty-four-hour observational study of hospital hand hygiene compliance. J. Hosp. Infect. 2010, 76, 252–255. [Google Scholar] [CrossRef]
- Eckmanns, T.; Bessert, J.; Behnke, M.; Gastmeier, P.; Ruden, H. Compliance with antiseptic hand rub use in intensive care units: The Hawthorne effect. Infect. Control Hosp. Epidemiol. 2006, 27, 931–934. [Google Scholar] [CrossRef]
- Borg, M.A.; Benbachir, M.; Cookson, B.D.; Redjeb, S.B.; Elnasser, Z.; Rasslan, O.; Gür, D.; Daoud, Z.; Bagatzouni, D.P. Self-protection as a driver for hand hygiene among healthcare workers. Infect. Control Hosp. Epidemiol. 2009, 30, 578–580. [Google Scholar] [CrossRef]
- Lambe, K.A.; Lydon, S.; Madden, C.; Vellinga, A.; Hehir, A.; Walsh, M.; O’Connor, P. Hand Hygiene Compliance in the ICU: A Systematic Review. Crit. Care Med. 2019, 47, 1251–1257. [Google Scholar] [CrossRef]
- McLaws, M.L.; Kwok, Y.L.A. Hand hygiene compliance rates: Fact or fiction? Am. J. Infect. Control 2018, 46, 876–880. [Google Scholar] [CrossRef] [PubMed]
- Marra, A.R.; Moura, D.F., Jr.; Paes, A.T.; dos Santos, O.F.; Edmond, M.B. Measuring rates of hand hygiene adherence in the intensive care setting: A comparative study of direct observation, product usage, and electronic counting devices. Infect. Control Hosp. Epidemiol. 2010, 31, 796–801. [Google Scholar] [CrossRef] [PubMed]
- Branch-Elliman, W.; Snyder, G.M.; King, A.D.; Baldini, L.M.; Dooley, K.M.; Yassa, D.S.; Wright, S.B. Correlation of Hand Hygiene Compliance Measured by Direct Observation with Estimates Obtained from Product Usage. Infect. Control Hosp. Epidemiol. 2018, 39, 746–749. [Google Scholar] [CrossRef] [PubMed]
| N of Observations | Compliance Rate | |
|---|---|---|
| Ward type | ||
| Medical unit | 620 | 49% |
| Day Hospital | 857 | 75% |
| Surgical unit | 712 | 70% |
| Intensive care unit | 692 | 76% |
| HCW category | ||
| Nurse | 1869 | 72% |
| Physician | 596 | 59% |
| Ancillary staff | 384 | 66% |
| Others | 32 | 72% |
| Indication for HH | ||
| Moment 1 | 780 | 58% |
| Moment 2 | 193 | 67% |
| Moment 3 | 126 | 69% |
| Moment 4 | 718 | 67% |
| Moment 5 | 1063 | 77% |
| OR (95% CI) | p | |
|---|---|---|
| Ward type | ||
| Medical unit | REF. | |
| Day Hospital | 2.62 (2.07–3.32) | <0.01 |
| Surgical unit | 2.15 (1.7–2.72) | <0.01 |
| Intensive care unit | 3.32 (2.6–4.24) | <0.01 |
| HCW category | ||
| Nurse | REF. | |
| Physician | 0.68 (0.55–0.84) | <0.01 |
| Ancillary staff | 0.88 (0.68–1.14) | 0.359 |
| Others | 1.01 (0.44–2.29) | 0.974 |
| Indication for HH | ||
| Moment 1 | REF. | |
| Moment 2 | 1.38 (0.97–1.95) | 0.068 |
| Moment 3 | 1.46 (0.96–2.22) | 0.070 |
| Moment 4 | 1.41 (1.13–1.75) | 0.002 |
| Moment 5 | 2.37 (1.92–2.93) | <0.01 |
| Mean Handrub Consumption (Range), mL/Patient-Day | |
|---|---|
| Medical wards | 32.1 (30.84–33.15) |
| Day Hospitals | 7.86 (4.48–14.38) |
| Surgical wards | 52.64 (12.82–125.64) |
| Intensive care units | 73.93 (30.15–158.42) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vicentini, C.; Libero, G.; Bordino, V.; Zotti, C.M. Hand Hygiene Practices during the COVID-19 Pandemic in Northern Italy: Assessment of Compliance Rates Measured by Direct Observation and Alcohol-Based Handrub Usage. Antibiotics 2022, 11, 1510. https://doi.org/10.3390/antibiotics11111510
Vicentini C, Libero G, Bordino V, Zotti CM. Hand Hygiene Practices during the COVID-19 Pandemic in Northern Italy: Assessment of Compliance Rates Measured by Direct Observation and Alcohol-Based Handrub Usage. Antibiotics. 2022; 11(11):1510. https://doi.org/10.3390/antibiotics11111510
Chicago/Turabian StyleVicentini, Costanza, Giulia Libero, Valerio Bordino, and Carla Maria Zotti. 2022. "Hand Hygiene Practices during the COVID-19 Pandemic in Northern Italy: Assessment of Compliance Rates Measured by Direct Observation and Alcohol-Based Handrub Usage" Antibiotics 11, no. 11: 1510. https://doi.org/10.3390/antibiotics11111510
APA StyleVicentini, C., Libero, G., Bordino, V., & Zotti, C. M. (2022). Hand Hygiene Practices during the COVID-19 Pandemic in Northern Italy: Assessment of Compliance Rates Measured by Direct Observation and Alcohol-Based Handrub Usage. Antibiotics, 11(11), 1510. https://doi.org/10.3390/antibiotics11111510







