The Effect of Pharmacist-Led Intervention on Surgical Antibacterial Prophylaxis (SAP) at an Orthopedic Unit
Abstract
1. Introduction
2. Results
2.1. Patient’s Characteristics
2.2. SAP Characteristics and Pharmacist intervention
2.2.1. Agent Selection, Dosage
2.2.2. Timing and Duration of SAP
2.2.3. Antibiotic Exposure and Cost in SAP
2.2.4. Clinical Outcomes: LOS (Length of Stay) and SSIs
3. Discussion
3.1. Overall Guideline Adherence
3.2. Antibiotic Exposure and Cost
3.3. Clinical Outcomes
3.4. Limitations and Strengths of This Study
4. Materials and Methods
4.1. Study Design
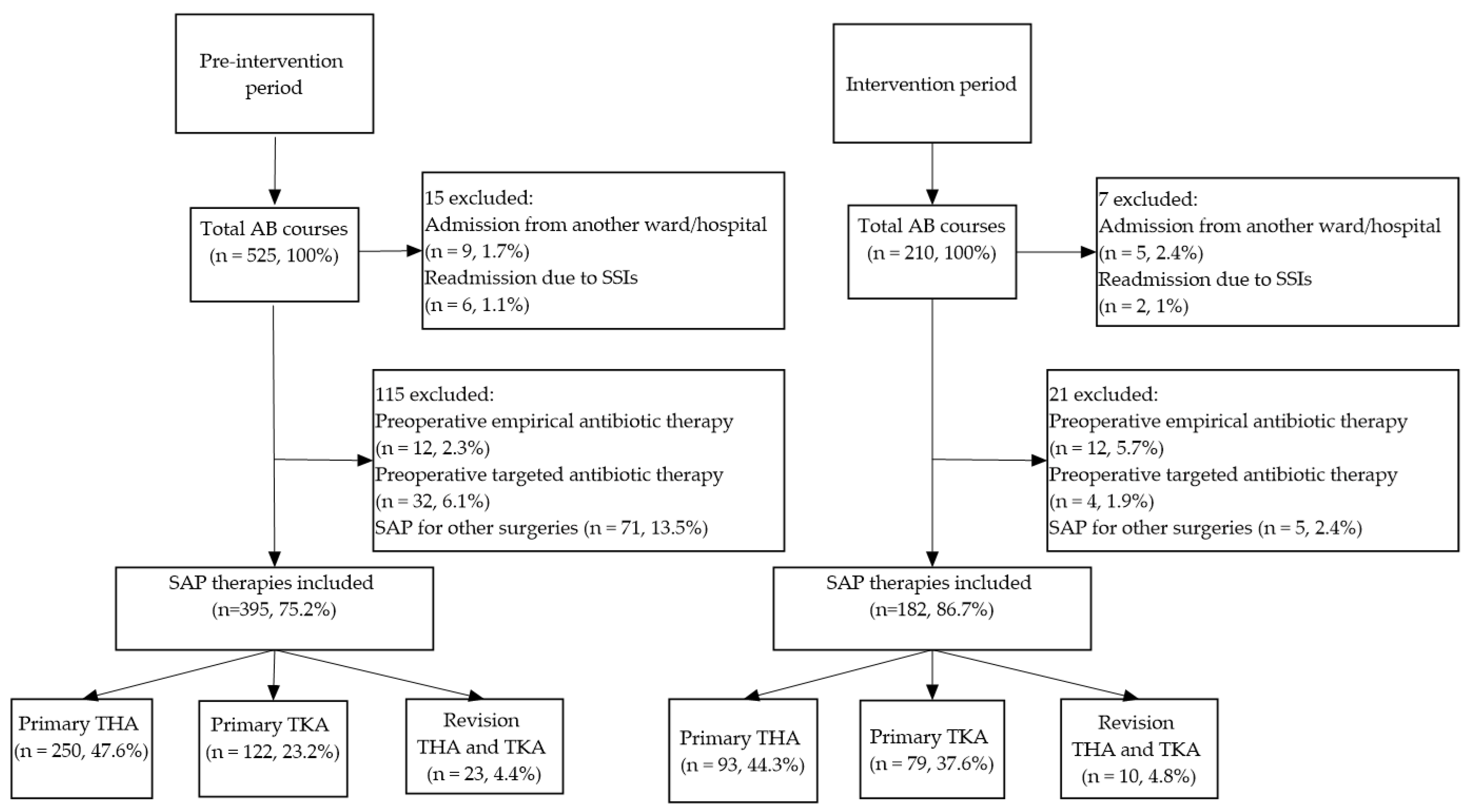
4.2. Study Population
4.3. Exclusion Criteria
4.4. Pre-Intervention and Intervention Period
4.5. Data Collection
4.6. Data Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Garner, J.S. CDC guideline for prevention of surgical wound infections, 1985. Supersedes guideline for prevention of surgical wound infections published in 1982. (Originally published in November 1985). Revised. Infect. Control 1986, 7, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Simmons, B.P. Guideline for prevention of surgical wound infections. Am. J. Infect. Control 1983, 11, 133–143. [Google Scholar] [CrossRef]
- Meehan, J.; Jamali, A.A.; Nguyen, H. Prophylactic antibiotics in hip and knee arthroplasty. J. Bone Jt. Surg. Am. 2009, 91, 2480–2490. [Google Scholar] [CrossRef]
- Swenson, E.R.; Bastian, N.D.; Nembhard, H.B.; Davis Iii, C.M. Reducing cost drivers in total joint arthroplasty: Understanding patient readmission risk and supply cost. Health Syst. (Basingstoke) 2018, 7, 135–147. [Google Scholar] [CrossRef]
- AlBuhairan, B.; Hind, D.; Hutchinson, A. Antibiotic prophylaxis for wound infections in total joint arthroplasty: A systematic review. J. Bone Jt. Surg. Br. 2008, 90, 915–919. [Google Scholar] [CrossRef] [PubMed]
- Backes, M.; Dingemans, S.A.; Dijkgraaf, M.G.W.; van den Berg, H.R.; van Dijkman, B.; Hoogendoorn, J.M.; Joosse, P.; Ritchie, E.D.; Roerdink, W.H.; Schots, J.P.M.; et al. Effect of Antibiotic Prophylaxis on Surgical Site Infections Following Removal of Orthopedic Implants Used for Treatment of Foot, Ankle, and Lower Leg Fractures: A Randomized Clinical Trial. JAMA 2017, 318, 2438–2445. [Google Scholar] [CrossRef] [PubMed]
- Butt, S.Z.; Ahmad, M.; Saeed, H.; Saleem, Z.; Javaid, Z. Post-surgical antibiotic prophylaxis: Impact of pharmacist’s educational intervention on appropriate use of antibiotics. J. Infect. Public Health 2019, 12, 854–860. [Google Scholar] [CrossRef]
- Bratzler, D.W.; Dellinger, E.P.; Olsen, K.M.; Perl, T.M.; Auwaerter, P.G.; Bolon, M.K.; Fish, D.N.; Napolitano, L.M.; Sawyer, R.G.; Slain, D.; et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am. J. Health Syst. Pharm. 2013, 70, 195–283. [Google Scholar] [CrossRef]
- Ierano, C.; Thursky, K.; Peel, T.; Rajkhowa, A.; Marshall, C.; Ayton, D. Influences on surgical antimicrobial prophylaxis decision making by surgical craft groups, anaesthetists, pharmacists and nurses in public and private hospitals. PLoS ONE 2019, 14, e0225011. [Google Scholar] [CrossRef]
- Abubakar, U.; Syed Sulaiman, S.A.; Adesiyun, A.G. Impact of pharmacist-led antibiotic stewardship interventions on compliance with surgical antibiotic prophylaxis in obstetric and gynecologic surgeries in Nigeria. PLoS ONE 2019, 14, e0213395. [Google Scholar] [CrossRef]
- Zhou, L.; Ma, J.; Gao, J.; Chen, S.; Bao, J. Optimizing Prophylactic Antibiotic Practice for Cardiothoracic Surgery by Pharmacists’ Effects. Medicine (Baltimore) 2016, 95, e2753. [Google Scholar] [CrossRef] [PubMed]
- Global Action Plan on Antimicrobial Resistance. World Health Organization, 2015. Available online: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance (accessed on 3 November 2021).
- Szalka, A. Az antibiotikum stewardship aktuális helyzete és feladatai. J. Hung. Interdiscip. Med. 2013, XII, 30–34. [Google Scholar]
- World Health Organization. Regional Office for Europe. 2018. Available online: https://apps.who.int/iris/bitstream/handle/10665/346593/WHO-EURO-2018-3014-42772-59680-hun.pdf?sequence=1 (accessed on 3 November 2021).
- Smith, B.P.; Fox, N.; Fakhro, A.; La Chant, M.; Pathak, A.S.; Ross, S.E.; Seamon, M.J. “SCIP” ping antibiotic prophylaxis guidelines in trauma: The consequences of noncompliance. J. Trauma. Acute. Care Surg. 2012, 73, 452–456; discussion 456. [Google Scholar] [CrossRef]
- Purba, A.K.R.; Setiawan, D.; Bathoorn, E.; Postma, M.J.; Dik, J.H.; Friedrich, A.W. Prevention of Surgical Site Infections: A Systematic Review of Cost Analyses in the Use of Prophylactic Antibiotics. Front. Pharmacol. 2018, 9, 776. [Google Scholar] [CrossRef]
- Mannien, J.; van Kasteren, M.E.; Nagelkerke, N.J.; Gyssens, I.C.; Kullberg, B.J.; Wille, J.C.; de Boer, A.S. Effect of optimized antibiotic prophylaxis on the incidence of surgical site infection. Infect. Control Hosp. Epidemiol. 2006, 27, 1340–1346. [Google Scholar] [CrossRef]
- Abdel-Aziz, A.; El-Menyar, A.; Al-Thani, H.; Zarour, A.; Parchani, A.; Asim, M.; El-Enany, R.; Al-Tamimi, H.; Latifi, R. Adherence of surgeons to antimicrobial prophylaxis guidelines in a tertiary general hospital in a rapidly developing country. Adv. Pharmacol. Sci. 2013, 2013, 842593. [Google Scholar] [CrossRef]
- Uckay, I.; Vernaz-Hegi, N.; Harbarth, S.; Stern, R.; Legout, L.; Vauthey, L.; Ferry, T.; Lubbeke, A.; Assal, M.; Lew, D.; et al. Activity and impact on antibiotic use and costs of a dedicated infectious diseases consultant on a septic orthopaedic unit. J. Infect. 2009, 58, 205–212. [Google Scholar] [CrossRef]
- Xie, C.; Mu, X.; Hu, Z.; Wang, W.; Huang, W.; Huang, G.; Wang, C.; Yin, D. Impact of pharmaceutical care in the orthopaedic department. J. Clin. Pharm. Ther. 2020, 45, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Classen, D.C.; Evans, R.S.; Pestotnik, S.L.; Horn, S.D.; Menlove, R.L.; Burke, J.P. The timing of prophylactic administration of antibiotics and the risk of surgical-wound infection. N. Engl. J. Med. 1992, 326, 281–286. [Google Scholar] [CrossRef]
- Gouvea, M.; Novaes, C.d.O.; Pereira, D.M.; Iglesias, A.C. Adherence to guidelines for surgical antibiotic prophylaxis: A review. Braz. J. Infect. Dis. 2015, 19, 517–524. [Google Scholar] [CrossRef]
- Tan, J.A.; Naik, V.N.; Lingard, L. Exploring obstacles to proper timing of prophylactic antibiotics for surgical site infections. Qual. Saf. Health Care 2006, 15, 32–38. [Google Scholar] [CrossRef]
- Wittmann, D.H.; Schein, M. Let us shorten antibiotic prophylaxis and therapy in surgery. Am. J. Surg. 1996, 172, 26S–32S. [Google Scholar] [CrossRef]
- Broom, J.; Broom, A. Fear and hierarchy: Critical influences on antibiotic decision-making in the operating theatre. J. Hosp. Infect. 2018, 99, 124–126. [Google Scholar] [CrossRef]
- Broom, J.; Broom, A.; Kirby, E.; Post, J.J. Improvisation versus guideline concordance in surgical antibiotic prophylaxis: A qualitative study. Infection 2018, 46, 541–548. [Google Scholar] [CrossRef]
- Rohrer, F.; Maurer, A.; Noetzli, H.; Gahl, B.; Limacher, A.; Hermann, T.; Bruegger, J. Prolonged antibiotic prophylaxis use in elective orthopaedic surgery–A cross-sectional analysis. BMC Musculoskelet. Disord. 2021, 22, 420. [Google Scholar] [CrossRef]
- Bailly, P.; Lallemand, S.; Thouverez, M.; Talon, D. Multicentre study on the appropriateness of surgical antibiotic prophylaxis. J. Hosp. Infect. 2001, 49, 135–138. [Google Scholar] [CrossRef] [PubMed]
- Tourmousoglou, C.E.; Yiannakopoulou, E.C.; Kalapothaki, V.; Bramis, J.; St Papadopoulos, J. Adherence to guidelines for antibiotic prophylaxis in general surgery: A critical appraisal. J. Antimicrob. Chemother. 2007, 61, 214–218. [Google Scholar] [CrossRef] [PubMed]
- van Kasteren, M.E.; Kullberg, B.J.; de Boer, A.S.; Mintjes-de Groot, J.; Gyssens, I.C. Adherence to local hospital guidelines for surgical antimicrobial prophylaxis: A multicentre audit in Dutch hospitals. J. Antimicrob. Chemother. 2003, 51, 1389–1396. [Google Scholar] [CrossRef]
- El Hassan, M.; Elnour, A.A.; Farah, F.H.; Shehab, A.; Al Kalbani, N.M.; Asim, S.; Shehab, O.A.; Abdulla, R. Clinical pharmacists’ review of surgical antimicrobial prophylaxis in a tertiary hospital in Abu Dhabi. Int. J. Clin. Pharm. 2015, 37, 18–22. [Google Scholar] [CrossRef]
- Song, K.H.; Kim, E.S.; Kim, Y.K.; Jin, H.Y.; Jeong, S.Y.; Kwak, Y.G.; Cho, Y.K.; Sung, J.; Lee, Y.S.; Oh, H.B.; et al. Differences in the risk factors for surgical site infection between total hip arthroplasty and total knee arthroplasty in the Korean Nosocomial Infections Surveillance System (KONIS). Infect. Control Hosp. Epidemiol. 2012, 33, 1086–1093. [Google Scholar] [CrossRef]
- Tiri, B.; Bruzzone, P.; Priante, G.; Sensi, E.; Costantini, M.; Vernelli, C.; Martella, L.A.; Francucci, M.; Andreani, P.; Mariottini, A.; et al. Impact of Antimicrobial Stewardship Interventions on Appropriateness of Surgical Antibiotic Prophylaxis: How to Improve. Antibiotics 2020, 9, 168. [Google Scholar] [CrossRef]
- Indications for Antimicrobial Use. European Centre for Disease Prevention and Control. Available online: https://www.ecdc.europa.eu/en/healthcare-associated-infections-acute-care-hospitals/database/indications-antimicrobial-use (accessed on 10 November 2021).
- Bratzler, D.W.; Houck, P.M.; Richards, C.; Steele, L.; Dellinger, E.P.; Fry, D.E.; Wright, C.; Ma, A.; Carr, K.; Red, L. Use of antimicrobial prophylaxis for major surgery: Baseline results from the National Surgical Infection Prevention Project. Arch. Surg. 2005, 140, 174–182. [Google Scholar] [CrossRef] [PubMed]
- Chandrananth, J.; Rabinovich, A.; Karahalios, A.; Guy, S.; Tran, P. Impact of adherence to local antibiotic prophylaxis guidelines on infection outcome after total hip or knee arthroplasty. J. Hosp. Infect. 2016, 93, 423–427. [Google Scholar] [CrossRef]
- Argaw, N.A.; Shumbash, K.Z.; Asfaw, A.A.; Hawaze, S. Assessment of surgical antimicrobial prophylaxis in Orthopaedics and Traumatology Surgical Unit of a Tertiary Care Teaching Hospital in Addis Ababa. BMC Res. Notes 2017, 10, 160. [Google Scholar] [CrossRef] [PubMed]
- Nelson, C.L.; Green, T.G.; Porter, R.A.; Warren, R.D. One day versus seven days of preventive antibiotic therapy in orthopedic surgery. Clin. Orthop. Relat. Res. 1983, 258–263. [Google Scholar] [CrossRef]
- Meyer, E.; Schwab, F.; Pollitt, A.; Bettolo, W.; Schroeren-Boersch, B.; Trautmann, M. Impact of a change in antibiotic prophylaxis on total antibiotic use in a surgical intensive care unit. Infection 2010, 38, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Chen, H.; Zhu, S.; Liu, Y.; Yang, J.; Yuan, Z.; Yao, G.; Qiu, F. Efficacy and feasibility of a collaborative multidisciplinary program for antibiotic prophylaxis in clean wound surgery. Int. J. Clin. Pharm. 2018, 40, 150–159. [Google Scholar] [CrossRef] [PubMed]
- Avinash, M.; Rajasekaran, S.; Aiyer, S.N. Unplanned 90-day readmissions in a specialty orthopaedic unit-A prospective analysis of consecutive 12729 admissions. J. Orthop. 2017, 14, 236–240. [Google Scholar] [CrossRef]
- Taherpour, N.; Mehrabi, Y.; Seifi, A.; Eshrati, B.; Hashemi Nazari, S.S. Epidemiologic characteristics of orthopedic surgical site infections and under-reporting estimation of registries using capture-recapture analysis. BMC Infect. Dis. 2021, 21, 3. [Google Scholar] [CrossRef] [PubMed]
- Mabit, C.; Marcheix, P.S.; Mounier, M.; Dijoux, P.; Pestourie, N.; Bonnevialle, P.; Bonnomet, F.; French Society of Orthopaedic Surgery, T. Impact of a surgical site infection (SSI) surveillance program in orthopedics and traumatology. Orthop. Traumatol. Surg. Res. 2012, 98, 690–695. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Maksimovic, J.; Markovic-Denic, L.; Bumbasirevic, M.; Marinkovic, J.; Vlajinac, H. Surgical site infections in orthopedic patients: Prospective cohort study. Croat. Med. J. 2008, 49, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Starcevic, S.; Munitlak, S.; Mijovic, B.; Mikic, D.; Suljagic, V. Surgical site infection surveillance in orthopedic patients in the Military Medical Academy, Belgrade. Vojnosanit. Pregl. 2015, 72, 499–504. [Google Scholar] [CrossRef] [PubMed]
- Lewis, S.S.; Dicks, K.V.; Chen, L.F.; Bolognesi, M.P.; Anderson, D.J.; Sexton, D.J.; Moehring, R.W. Delay in diagnosis of invasive surgical site infections following knee arthroplasty versus hip arthroplasty. Clin. Infect Dis. 2015, 60, 990–996. [Google Scholar] [CrossRef]
- Hanssen, A.D.; Osmon, D.R. The use of prophylactic antimicrobial agents during and after hip arthroplasty. Clin. Orthop. Relat. Res. 1999, 369, 124–138. [Google Scholar] [CrossRef] [PubMed]
- van Kasteren, M.E.; Mannien, J.; Ott, A.; Kullberg, B.J.; de Boer, A.S.; Gyssens, I.C. Antibiotic prophylaxis and the risk of surgical site infections following total hip arthroplasty: Timely administration is the most important factor. Clin. Infect. Dis. 2007, 44, 921–927. [Google Scholar] [CrossRef] [PubMed]
- Ribed, A.; Monje, B.; Garcia-Gonzalez, X.; Sanchez-Somolinos, M.; Sanz-Ruiz, P.; Rodriguez-Gonzalez, C.G.; Sanjurjo-Saez, M. Improving surgical antibiotic prophylaxis adherence and reducing hospital readmissions: A bundle of interventions including health information technologies. Eur. J. Hosp. Pharm. 2020, 27, 237–242. [Google Scholar] [CrossRef]
- Willems, L.; Simoens, S.; Laekeman, G. Follow-up of antibiotic prophylaxis: Impact on compliance with guidelines and financial outcomes. J. Hosp. Infect. 2005, 60, 333–339. [Google Scholar] [CrossRef]
| Parameters | Pre-Intervention Period N = 395 (%) | Intervention Period N = 182 (%) | p-Values |
|---|---|---|---|
| Age (Mean ± SD)—years | 65 ± 10.9 | 66 ± 10.5 | 0.292 |
| 18–65 | 174 (44.1%) | 75 (41.2%) | 0.685 |
| 65+ | 221 (55.9%) | 107 (58.8%) | 0.738 |
| Gender | |||
| Male | 151 (38.2%) | 70 (38.5%) | 0.971 |
| Female | 244 (61.8%) | 112 (61.5%) | 0.979 |
| Median body weight (range)-kg | 59.9 (35–105) | 62.1 (28–160) | 0.675 |
| Diagnosis primary arthroplasty | |||
| Osteoarthritis | 161 (40.8%) | 73 (40.1%) | 0.346 |
| Osteonecrosis | 195 (49.4%) | 93 (51.1%) | 0.823 |
| Others * | 16 (4%) | 6 (3.3%) | 0.671 |
| Surgical procedure | |||
| THA | 250 (63.3%) | 93 (51.1%) | 0.156 |
| TKA | 122 (30.9%) | 79 (43.4%) | 0.044 |
| Revision hip arthroplasty | 19 (4.8%) | 7 (3.8%) | 0.619 |
| Revision knee arthroplasty | 4 (1%) | 3 (1.7%) | 0.522 |
| Parameters | Pre-Intervention Period N = 395 (%) | Intervention Period N = 182 (%) | Increase/ Decrease % | p-Values |
|---|---|---|---|---|
| Number of antibiotics used simultaneously: 1 | 371 (93.9%) | 173 (95.1%) | 1.2% | 0.925 |
| Number of antibiotics used simultaneously: 2–3 | 24 (6.1%) | 9 (4.9%) | −1.2% | 0.607 |
| Guideline adherent antibiotic | 350 (88.6%) | 164 (90.1%) | 1.5% | 0.897 |
| Cefuroxime | 348 (88.1%) | 160 (87.9%) | −0.2% | 0.987 |
| Cefuroxime + amikacin | 2 (0.5%) | 4 (2.2%) | 1.7% | 0.066 |
| Guideline non-adherent antibiotic | 45 (11.4%) | 18 (9.9%) | −1.5% | 0.629 |
| Co-amoxiclav | 1 (0.3%) | - | −0.3% | 0.497 |
| Ciprofloxacin | 22 (5.6%) | 13 (7.1%) | 1.5% | 0.490 |
| beta-lactams or FQ + metronidazole | 20 (5%) | 4 (2.2%) | −2.8% | 0.122 |
| beta-lactams or FQ + rifampin | 1 (0.3%) | - | −0.3% | 0.497 |
| FQ + amikacin | 1 (0.3%) | 1 (0.6%) | 0.3% | 0.575 |
| Guideline-adherent agent(s) | 350 (88.6%) | 164 (90.1%) | 1.5% | 0.897 |
| Guideline-adherent agent, dosage | 341 (86.3%) | 162 (89%) | 2.7% | 0.815 |
| Guideline-adherent agent, dosage, and duration | 8 (2%) | 106 (58.2%) | 56.2% | ˂0.001 |
| Duration of prophylaxis—days (Mean ± SD/Median) | 4.08 ± 2.08 (3) | 2.42 ± 1.90 (1) | −42.9% | ˂0.001 |
| One day prophylaxis | 9 (2.3%) | 113 (62.1%) | 59.8% | ˂0.001 |
| Three days prophylaxis | 135 (34.2%) | 20 (11%) | −33.2% | ˂0.001 |
| Over five days prophylaxis | 72 (18.2%) | 12 (6.6%) | −11.6% | ˂0.001 |
| Guideline adherent duration | 20 (5%) | 117 (64.3%) | 59.3% | ˂0.001 |
| Primary arthroplasties | 8 (2%) | 111 (61%) | 59% | ˂0.001 |
| Revision arthroplasties | 12 (3%) | 6 (3.3%) | 0.3% | 0.872 |
| DDD/patient (Mean ± SD) | 6.07 ± 0.05 | 3.58 ± 4.33 | −41% | ˂0.001 |
| LOS—days (Mean ± SD/Median) | 11.22 ± 6.96 (9) | 7.62 ± 3.02 (7) | −37.2% | ˂0.001 |
| SSIs onset—days (Mean ± SD/Median) | 8.91 ± 5.75 (8) | 8.5 ± 6.61 (8) | −3% | 0.170 |
| Suspected SSIs | 43 (11.6%) | 4 (2.3%) | −9.3% | ˂0.001 |
| Confirmed SSIs | 11 (3%) | 2 (1.2%) | −1.8% | 0.214 |
| Need for postoperative antibiotic treatment due to SSIs | 77 (19.5%) | 5 (2.7%) | −16.8% | ˂0.001 |
| Prophylactic antibiotic cost/patient—HUF (Mean ± SD) | 9278.79 ± 6094.29 | 3598.16 ± 3354.55 | −54.8% | ˂0.001 |
| Primary Arthroplasties | 8768.70 ± 4478.91 | 3162.23 ± 2641.7 | −56.2% | ˂0.001 |
| Revision Arthroplasties | 17,528.96 ± 15,852.28 | 9793.4 ± 6732.08 | −50.5% | 0.070 |
| Active Agent | Dose (Adults) | Duration | |
|---|---|---|---|
| In Primary Arthroplasties | In Revision Arthroplasties | ||
| cefazolin | 1–2 g iv q8h | up to 24 h | up to 5 days |
| cefuroxime | 1.5 g/750 mg iv q8h | ||
| clindamycin | 600/400 mg iv q8h | ||
| vancomycin | 500 mg iv q6h | ||
| 1 gmg iv q12h | |||
| amikacin | 15 mg/kg/day iv q8–12h | ||
| gentamicin | 3–6 mg/kg/day iv q12–24h | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fésüs, A.; Benkő, R.; Matuz, M.; Kungler-Gorácz, O.; Fésüs, M.Á.; Bazsó, T.; Csernátony, Z.; Kardos, G. The Effect of Pharmacist-Led Intervention on Surgical Antibacterial Prophylaxis (SAP) at an Orthopedic Unit. Antibiotics 2021, 10, 1509. https://doi.org/10.3390/antibiotics10121509
Fésüs A, Benkő R, Matuz M, Kungler-Gorácz O, Fésüs MÁ, Bazsó T, Csernátony Z, Kardos G. The Effect of Pharmacist-Led Intervention on Surgical Antibacterial Prophylaxis (SAP) at an Orthopedic Unit. Antibiotics. 2021; 10(12):1509. https://doi.org/10.3390/antibiotics10121509
Chicago/Turabian StyleFésüs, Adina, Ria Benkő, Mária Matuz, Orsolya Kungler-Gorácz, Márton Á. Fésüs, Tamás Bazsó, Zoltán Csernátony, and Gábor Kardos. 2021. "The Effect of Pharmacist-Led Intervention on Surgical Antibacterial Prophylaxis (SAP) at an Orthopedic Unit" Antibiotics 10, no. 12: 1509. https://doi.org/10.3390/antibiotics10121509
APA StyleFésüs, A., Benkő, R., Matuz, M., Kungler-Gorácz, O., Fésüs, M. Á., Bazsó, T., Csernátony, Z., & Kardos, G. (2021). The Effect of Pharmacist-Led Intervention on Surgical Antibacterial Prophylaxis (SAP) at an Orthopedic Unit. Antibiotics, 10(12), 1509. https://doi.org/10.3390/antibiotics10121509






