A Novel Personalized Strategy for Hip Joint Flexion Assistance Based on Human Physiological State
Abstract
1. Introduction
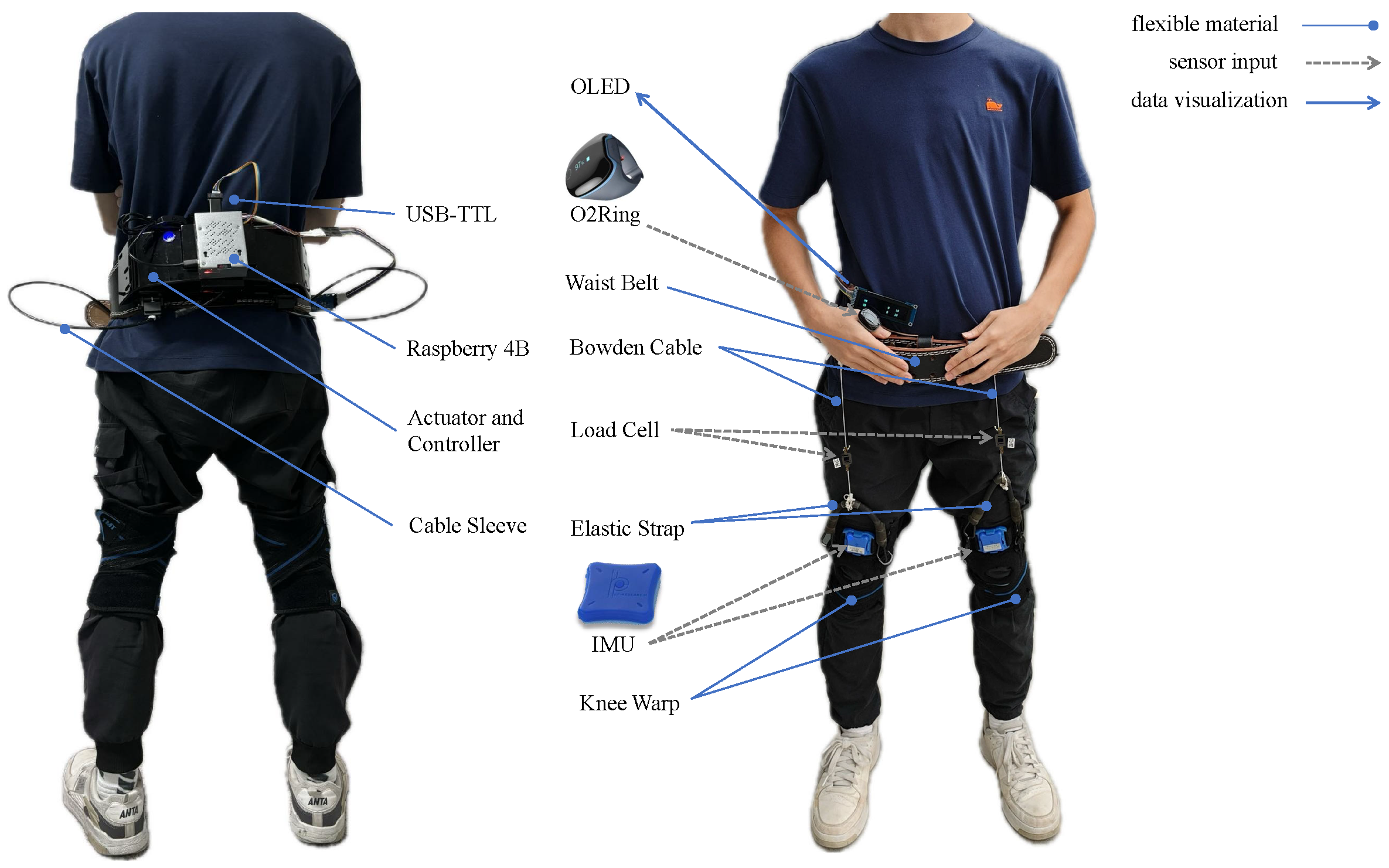
2. Exosuit Hardware Setup
2.1. Design of The Proposed Soft Exosuit
2.2. Data Acquisition System
3. Different Assistance Strategies in Different Status Conditions
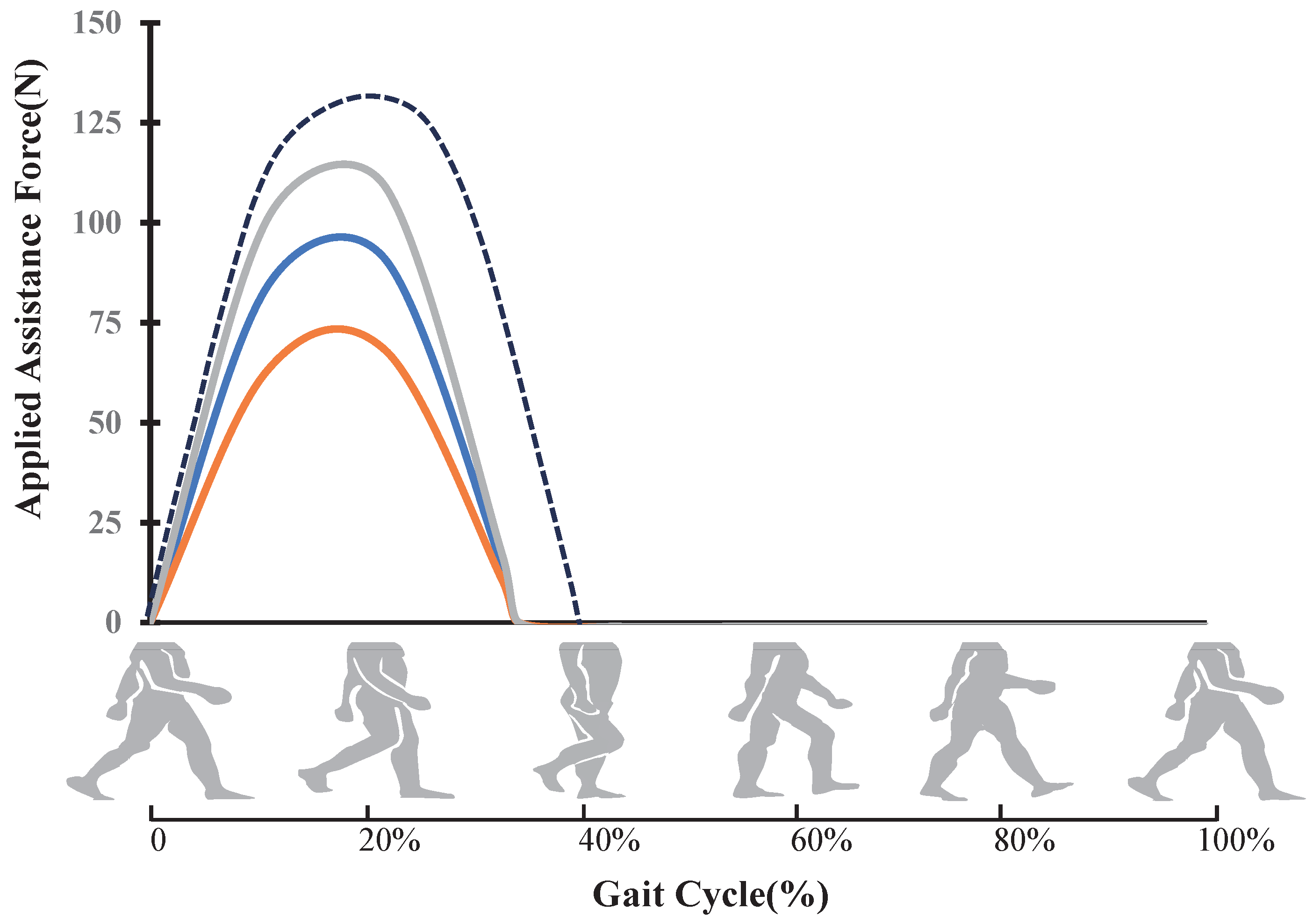
3.1. Hip Power-Assist Strategy
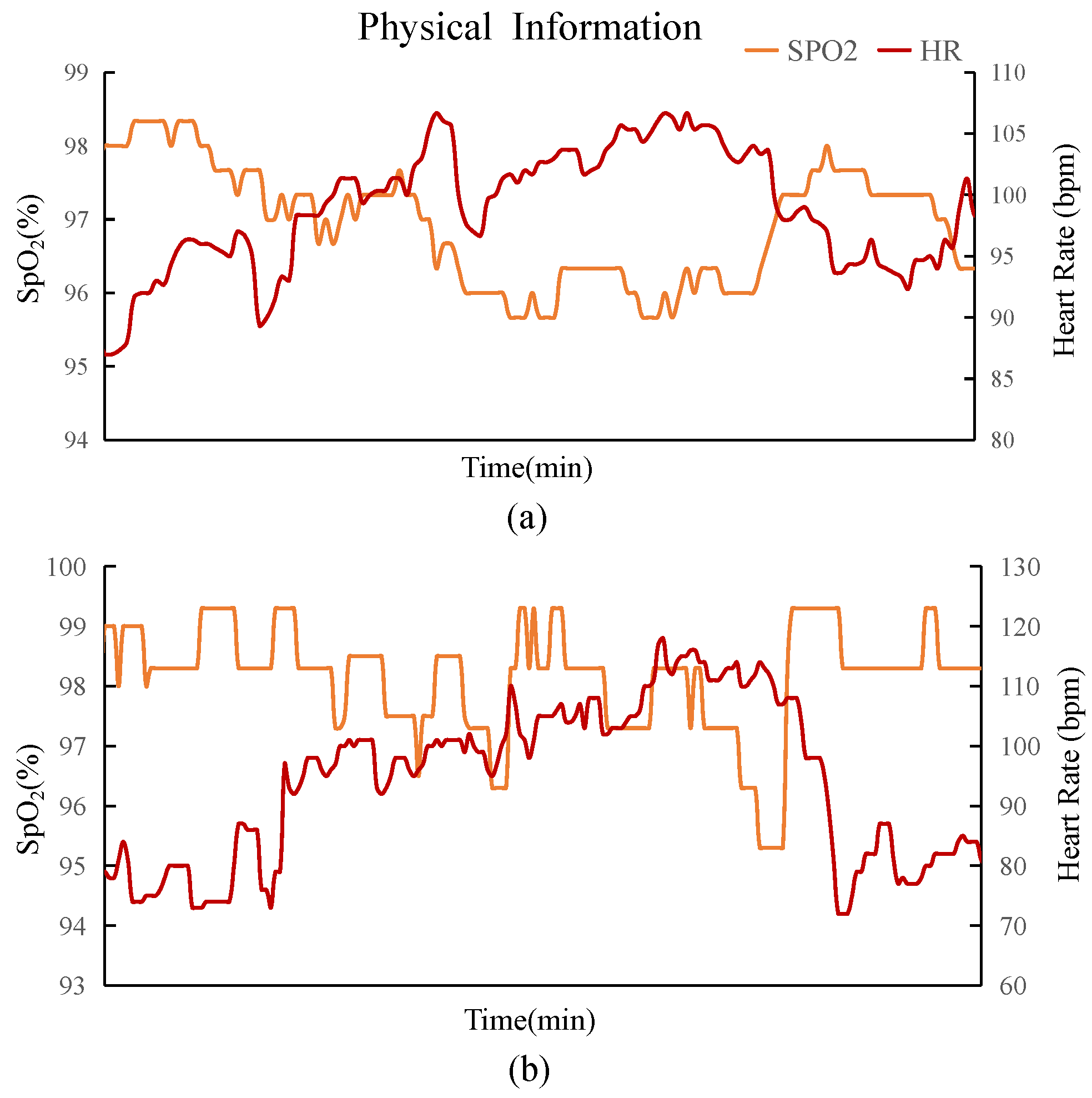
3.2. Fusion Control Strategy
4. Experimentation
4.1. Methods for Evaluating the Effectiveness of Human–Computer Interaction
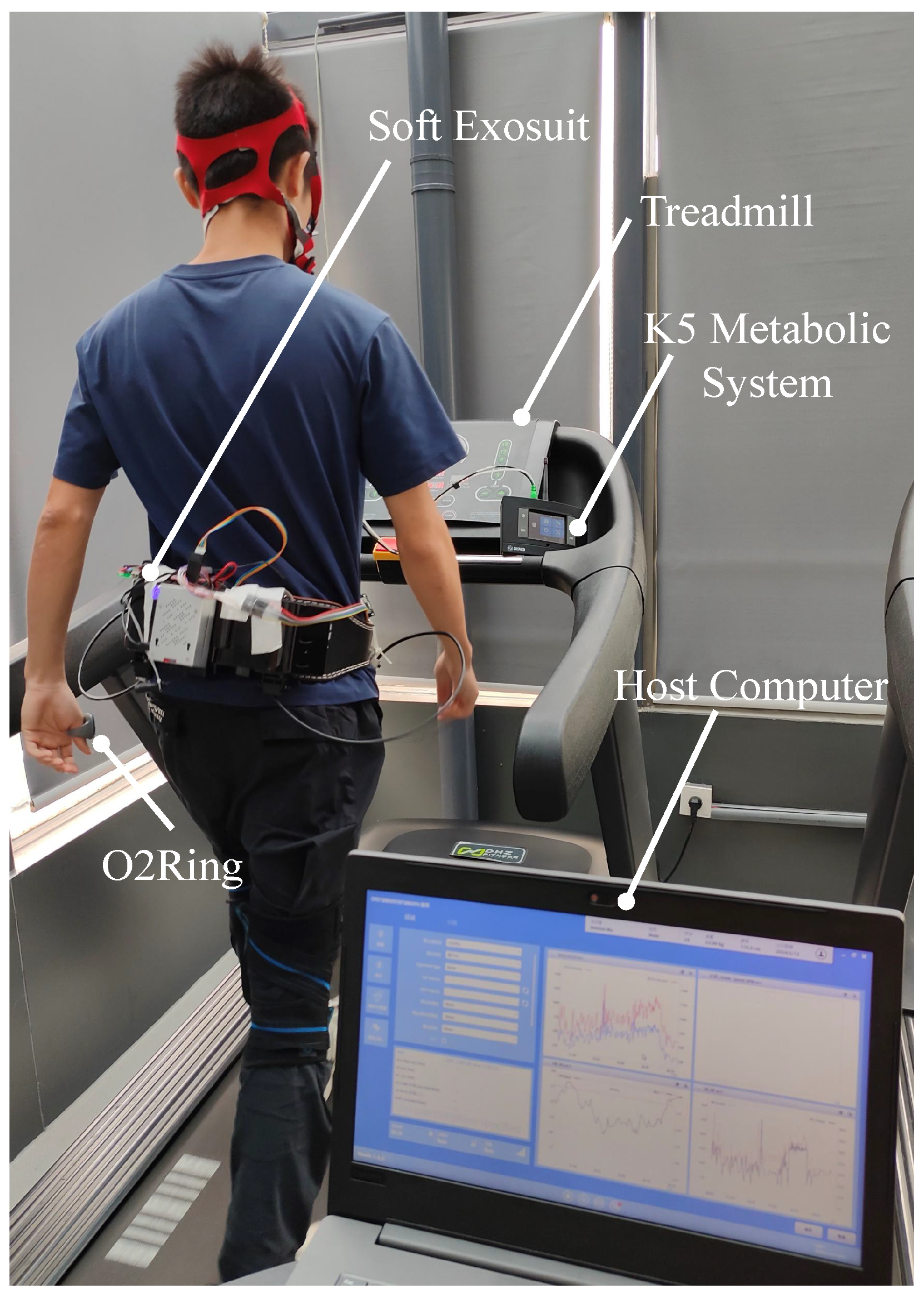
4.2. Metabolic Consumption Experiment
4.2.1. Experimental Setup of the Treadmill Walking Tests
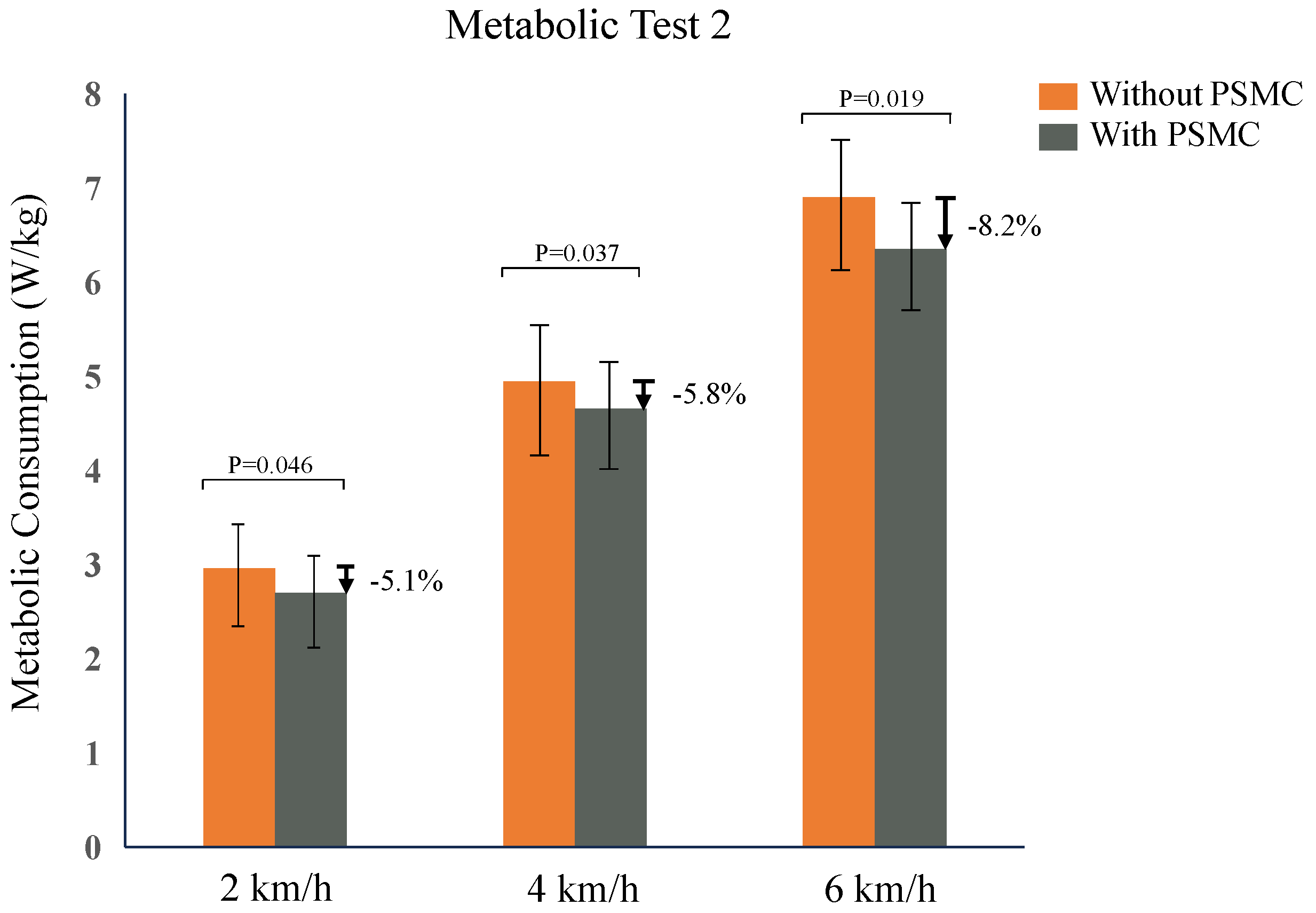
4.2.2. Metabolic Reduction by the Exosuit in Fixed-Speed Conditions
4.2.3. Metabolic Reduction by the Exosuit in Variable-Speed Conditions
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| HR | Heart rate |
| SpO2 | Blood oxygen saturation |
| IMU | Inertial Measurement Unit |
| STM32 | STMicroelectronics 32-bit Series Microcontroller Chip |
| PSMC | Physiological State Monitoring Control |
| EMG | Electromyography |
| PD | Proportional-derivative %TLA & Three-letter acronym % RMS & Root Mean Square |
References
- Xia, H.; Zhang, Y.; Rajabi, N.; Taleb, F.; Yang, Q.; Kragic, D.; Li, Z. Shaping high-performance wearable robots for human motor and sensory reconstruction and enhancement. Nat. Commun. 2024, 15, 1760. [Google Scholar] [CrossRef] [PubMed]
- Pantelopoulos, A.; Bourbakis, N.G. A survey on wearable sensor-based systems for health monitoring and prognosis. IEEE Trans. Syst. Man Cybern. Part C (Appl. Rev.) 2009, 40, 1–12. [Google Scholar] [CrossRef]
- Kim, J.; Porciuncula, F.; Yang, H.D.; Wendel, N.; Baker, T.; Chin, A.; Ellis, T.D.; Walsh, C.J. Soft robotic apparel to avert freezing of gait in Parkinson’s disease. Nat. Med. 2024, 30, 177–185. [Google Scholar] [CrossRef]
- Lee, S.H.; Kim, J.; Lim, B.; Lee, H.J.; Kim, Y.H. Exercise with a wearable hip-assist robot improved physical function and walking efficiency in older adults. Sci. Rep. 2023, 13, 7269. [Google Scholar] [CrossRef] [PubMed]
- Langer, A.; Gassner, L.; Hasenauer, S.; Gruber, J.; Wizany, L.; Pokan, R.; Maetzler, W.; Zach, H. How COVID-19 will boost remote exercise-based treatment in Parkinson’s disease: A narrative review. NPJ Park. Dis. 2021, 7, 25. [Google Scholar] [CrossRef]
- Lee, U.H.; Shetty, V.S.; Franks, P.W.; Tan, J.; Evangelopoulos, G.; Ha, S.; Rouse, E.J. User preference optimization for control of ankle exoskeletons using sample efficient active learning. Sci. Robot. 2023, 8, eadg3705. [Google Scholar] [CrossRef]
- Koginov, G.; Bergmann, L.; Xiloyannis, M.; Rohner, N.; Ngo, C.; Duarte, J.E.; Leonhardt, S.; Riener, R. Human-in-the-Loop Personalization of a Bi-Articular Wearable Robot’s Assistance for Downhill Walking. IEEE Trans. Med. Robot. Bionics 2023, 6, 328–339. [Google Scholar] [CrossRef]
- Hong, Y.J.; Lee, H.; Kim, J.; Lee, M.; Choi, H.J.; Hyeon, T.; Kim, D.H. Multifunctional wearable system that integrates sweat-based sensing and vital-sign monitoring to estimate pre-/post-exercise glucose levels. Adv. Funct. Mater. 2018, 28, 1805754. [Google Scholar] [CrossRef]
- Jung, H.H.; Lee, H.; Yea, J.; Jang, K.I. Wearable electrochemical sensors for real-time monitoring in diabetes mellitus and associated complications. Soft Sci. 2024, 4, 15. [Google Scholar] [CrossRef]
- Sempionatto, J.R.; Lin, M.; Yin, L.; De La Paz, E.; Pei, K.; Sonsa-Ard, T.; de Loyola Silva, A.N.; Khorshed, A.A.; Zhang, F.; Tostado, N.; et al. An epidermal patch for the simultaneous monitoring of haemodynamic and metabolic biomarkers. Nat. Biomed. Eng. 2021, 5, 737–748. [Google Scholar] [CrossRef]
- Schäffer, K.; Ozkan-Aydin, Y.; Coad, M.M. Soft Wrist Exosuit Actuated by Fabric Pneumatic Artificial Muscles. IEEE Trans. Med. Robot. Bionics 2024, 6, 718–732. [Google Scholar] [CrossRef]
- Dinovitzer, H.; Shushtari, M.; Arami, A. Feedforward Control of Lower Limb Exoskeletons: Which Torque Profile Should We Use? IEEE Robot. Autom. Lett. 2023, 9, 382–389. [Google Scholar] [CrossRef]
- Nuckols, R.W.; Lee, S.; Swaminathan, K.; Orzel, D.; Howe, R.D.; Walsh, C.J. Individualization of exosuit assistance based on measured muscle dynamics during versatile walking. Sci. Robot. 2021, 6, eabj1362. [Google Scholar] [CrossRef]
- Luo, S.; Jiang, M.; Zhang, S.; Zhu, J.; Yu, S.; Dominguez Silva, I.; Wang, T.; Rouse, E.; Zhou, B.; Yuk, H.; et al. Experiment-free exoskeleton assistance via learning in simulation. Nature 2024, 630, 353–359. [Google Scholar] [CrossRef] [PubMed]
- Tricomi, E.; Mossini, M.; Missiroli, F.; Lotti, N.; Zhang, X.; Xiloyannis, M.; Roveda, L.; Masia, L. Environment-based assistance modulation for a hip exosuit via computer vision. IEEE Robot. Autom. Lett. 2023, 8, 2550–2557. [Google Scholar] [CrossRef]
- Wang, Z.; Yang, F.; Chen, L.; He, T.; Chen, C.; Wu, X. Individualization of Assistance Strategy for Hip Extension Assistance based on Emotion-in-the-Loop. In Proceedings of the 2023 IEEE International Conference on Robotics and Biomimetics (ROBIO), Koh Samui, Thailand, 4–9 December 2023; pp. 1–7. [Google Scholar]
- Ding, Y.; Galiana, I.; Asbeck, A.T.; De Rossi, S.M.M.; Bae, J.; Santos, T.R.T.; De Araujo, V.L.; Lee, S.; Holt, K.G.; Walsh, C. Biomechanical and physiological evaluation of multi-joint assistance with soft exosuits. IEEE Trans. Neural Syst. Rehabil. Eng. 2016, 25, 119–130. [Google Scholar] [CrossRef]
- Koller, J.R.; Gates, D.H.; Ferris, D.P.; Remy, C.D. ‘Body-in-the-Loop’Optimization of Assistive Robotic Devices: A Validation Study. In Proceedings of the Robotics: Science and Systems, Cambridge, MA, USA, 12–16 July 2016; Volume 2016, pp. 1–10. [Google Scholar]
- Ingraham, K.A.; Ferris, D.P.; Remy, C.D. Using portable physiological sensors to estimate energy cost for ‘body-in-the-loop’optimization of assistive robotic devices. In Proceedings of the 2017 IEEE Global Conference on Signal and Information Processing (GlobalSIP), Montreal, QC, Canada, 14–16 November 2017; pp. 413–417. [Google Scholar]
- Yang, F.; Chen, C.; Wang, Z.; Chen, H.; Liu, Y.; Li, G.; Wu, X. Vit-based terrain recognition system for wearable soft exosuit. Biomim. Intell. Robot. 2023, 3, 100087. [Google Scholar] [CrossRef]
- Jang, J.; Kim, K.; Lee, J.; Lim, B.; Shim, Y. Online gait task recognition algorithm for hip exoskeleton. In Proceedings of the 2015 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Hamburg, Germany, 28 September–2 October 2015; pp. 5327–5332. [Google Scholar] [CrossRef]
- Zhang, X.; Tricomi, E.; Missiroli, F.; Lotti, N.; Masia, L. Real-Time Assistive Control via IMU Locomotion Mode Detection in a Soft Exosuit: An Effective Approach to Enhance Walking Metabolic Efficiency. IEEE/ASME Trans. Mechatron. 2023, 29, 1797–1808. [Google Scholar] [CrossRef]
- Wei, B.; Yi, C.; Zhang, S.; Guo, H.; Zhu, J.; Ding, Z.; Jiang, F. Taking locomotion mode as prior: One algorithm-enabled gait events and kinematics prediction on various terrains. IEEE Sens. J. 2023, 23, 13072–13083. [Google Scholar] [CrossRef]
- Ingraham, K.A.; Remy, C.D.; Rouse, E.J. The role of user preference in the customized control of robotic exoskeletons. Sci. Robot. 2022, 7, eabj3487. [Google Scholar] [CrossRef]
- Selinger, J.C.; O’Connor, S.M.; Wong, J.D.; Donelan, J.M. Humans can continuously optimize energetic cost during walking. Curr. Biol. 2015, 25, 2452–2456. [Google Scholar] [CrossRef] [PubMed]
- Kitatani, R.; Ohata, K.; Takahashi, H.; Shibuta, S.; Hashiguchi, Y.; Yamakami, N. Reduction in energy expenditure during walking using an automated stride assistance device in healthy young adults. Arch. Phys. Med. Rehabil. 2014, 95, 2128–2133. [Google Scholar] [CrossRef] [PubMed]
- Chiu, M.C.; Wang, M.J. The effect of gait speed and gender on perceived exertion, muscle activity, joint motion of lower extremity, ground reaction force and heart rate during normal walking. Gait Posture 2007, 25, 385–392. [Google Scholar] [CrossRef]
- Chung, M.J.; Wang, M.J.J. The change of gait parameters during walking at different percentage of preferred walking speed for healthy adults aged 20–60 years. Gait Posture 2010, 31, 131–135. [Google Scholar]
- Horiuchi, M.; Kirihara, Y.; Fukuoka, Y.; Pontzer, H. Sex differences in respiratory and circulatory cost during hypoxic walking: Potential impact on oxygen saturation. Sci. Rep. 2019, 9, 9550. [Google Scholar] [CrossRef] [PubMed]
- Ingraham, K.A.; Ferris, D.P.; Remy, C.D. Using wearable physiological sensors to predict energy expenditure. In Proceedings of the 2017 International Conference on Rehabilitation Robotics (ICORR), London, UK, 17–20 July 2017; pp. 340–345. [Google Scholar]
- Kim, J.; Lee, G.; Heimgartner, R.; Arumukhom Revi, D.; Karavas, N.; Nathanson, D.; Galiana, I.; Eckert-Erdheim, A.; Murphy, P.; Perry, D.; et al. Reducing the metabolic rate of walking and running with a versatile, portable exosuit. Science 2019, 365, 668–672. [Google Scholar] [CrossRef]
- Ferris, D.P.; Sawicki, G.S.; Daley, M.A. A physiologist’s perspective on robotic exoskeletons for human locomotion. Int. J. Humanoid Robot. 2007, 4, 507–528. [Google Scholar] [CrossRef] [PubMed]
- Siviy, C.; Baker, L.M.; Quinlivan, B.T.; Porciuncula, F.; Swaminathan, K.; Awad, L.N.; Walsh, C.J. Opportunities and challenges in the development of exoskeletons for locomotor assistance. Nat. Biomed. Eng. 2023, 7, 456–472. [Google Scholar] [CrossRef]
- Lee, G.; Kim, J.; Panizzolo, F.; Zhou, Y.; Baker, L.; Galiana, I.; Malcolm, P.; Walsh, C. Reducing the metabolic cost of running with a tethered soft exosuit. Sci. Robot. 2017, 2, eaan6708. [Google Scholar] [CrossRef]
- Kim, J.; Quinlivan, B.T.; Deprey, L.A.; Arumukhom Revi, D.; Eckert-Erdheim, A.; Murphy, P.; Orzel, D.; Walsh, C.J. Reducing the energy cost of walking with low assistance levels through optimized hip flexion assistance from a soft exosuit. Sci. Rep. 2022, 12, 11004. [Google Scholar] [CrossRef]
- Ding, Y.; Kim, M.; Kuindersma, S.; Walsh, C.J. Human-in-the-loop optimization of hip assistance with a soft exosuit during walking. Sci. Robot. 2018, 3, eaar5438. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Chen, J.; Ji, Y.; Jin, W.; Liu, J.; Zhang, J. Evaluation of lower leg muscle activities during human walking assisted by an ankle exoskeleton. IEEE Trans. Ind. Inform. 2020, 16, 7168–7176. [Google Scholar] [CrossRef]
- Diaz, M.A.; Voss, M.; Dillen, A.; Tassignon, B.; Flynn, L.; Geeroms, J.; Meeusen, R.; Verstraten, T.; Babič, J.; Beckerle, P.; et al. Human-in-the-loop optimization of wearable robotic devices to improve human–robot interaction: A systematic review. IEEE Trans. Cybern. 2022, 53, 7483–7496. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Seo, K.; Lim, B.; Jang, J.; Kim, K.; Choi, H. Effects of assistance timing on metabolic cost, assistance power, and gait parameters for a hip-type exoskeleton. In Proceedings of the 2017 International Conference on Rehabilitation Robotics (ICORR), London, UK, 17–20 July 2017; pp. 498–504. [Google Scholar]
- Brockway, J. Derivation of formulae used to calculate energy expenditure in man. Hum. Nutr. Clin. Nutr. 1987, 41, 463–471. [Google Scholar] [PubMed]
- Wang, Z.; Chen, C.; Yang, F.; Liu, Y.; Li, G.; Wu, X. Real-time gait phase estimation based on neural network and assistance strategy based on simulated muscle dynamics for an ankle exosuit. IEEE Trans. Med. Robot. Bionics 2023, 5, 100–109. [Google Scholar] [CrossRef]
- Monteiro, S.; Figueiredo, J.; Fonseca, P.; Vilas-Boas, J.P.; Santos, C.P. Human-in-the-Loop Optimization of Knee Exoskeleton Assistance for Minimizing User’s Metabolic and Muscular Effort. Sensors 2024, 24, 3305. [Google Scholar] [CrossRef]
- Poggensee, K.L.; Collins, S.H. Lower limb biomechanics of fully trained exoskeleton users reveal complex mechanisms behind the reductions in energy cost with human-in-the-loop optimization. Front. Robot. AI 2024, 11, 1283080. [Google Scholar] [CrossRef]



| Part | Location | Mass (kg) |
|---|---|---|
| Batteries | Waist | 0.55 |
| Actuator | Waist | 0.214 |
| Raspberry pi | Waist | 0.106 |
| MCU | Waist | 0.08 |
| Waist belt | Waist | 0.30 |
| IMU | Thigh | 0.024 |
| Load cells | Thigh | 0.05 |
| Wraps | Thigh | 0.22 |
| O2Ring ring | Finger | 0.015 |
| Subjects | Age (Years) | Gender | Height (cm) | Weight (kg) | Physiological State Test (Y/N) |
|---|---|---|---|---|---|
| A | 24 | Male | 170 | 75 | |
| B | 25 | Male | 173 | 66 | |
| C | 23 | Male | 175 | 70 | Y |
| D | 25 | Male | 172 | 52 | |
| E | 25 | Male | 176 | 65 | Y |
| F | 26 | Male | 177 | 74 | |
| G | 26 | Male | 165 | 58 | |
| H | 27 | Male | 182 | 75 | Y |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, B.; Chen, C.; Wang, S.; Chen, H.; Wang, Z.; Liu, Y.; He, T.; Zhang, J.; Wu, X. A Novel Personalized Strategy for Hip Joint Flexion Assistance Based on Human Physiological State. Biosensors 2024, 14, 418. https://doi.org/10.3390/bios14090418
Wu B, Chen C, Wang S, Chen H, Wang Z, Liu Y, He T, Zhang J, Wu X. A Novel Personalized Strategy for Hip Joint Flexion Assistance Based on Human Physiological State. Biosensors. 2024; 14(9):418. https://doi.org/10.3390/bios14090418
Chicago/Turabian StyleWu, Beixian, Chunjie Chen, Sheng Wang, Hui Chen, Zhuo Wang, Yao Liu, Tingwei He, Jiale Zhang, and Xinyu Wu. 2024. "A Novel Personalized Strategy for Hip Joint Flexion Assistance Based on Human Physiological State" Biosensors 14, no. 9: 418. https://doi.org/10.3390/bios14090418
APA StyleWu, B., Chen, C., Wang, S., Chen, H., Wang, Z., Liu, Y., He, T., Zhang, J., & Wu, X. (2024). A Novel Personalized Strategy for Hip Joint Flexion Assistance Based on Human Physiological State. Biosensors, 14(9), 418. https://doi.org/10.3390/bios14090418





