Utilization of Personalized Machine-Learning to Screen for Dysglycemia from Ambulatory ECG, toward Noninvasive Blood Glucose Monitoring
Abstract
1. Introduction
2. Materials and Methods
2.1. Dataset Collection and Inclusion Criteria
2.2. Training and Validation Dataset
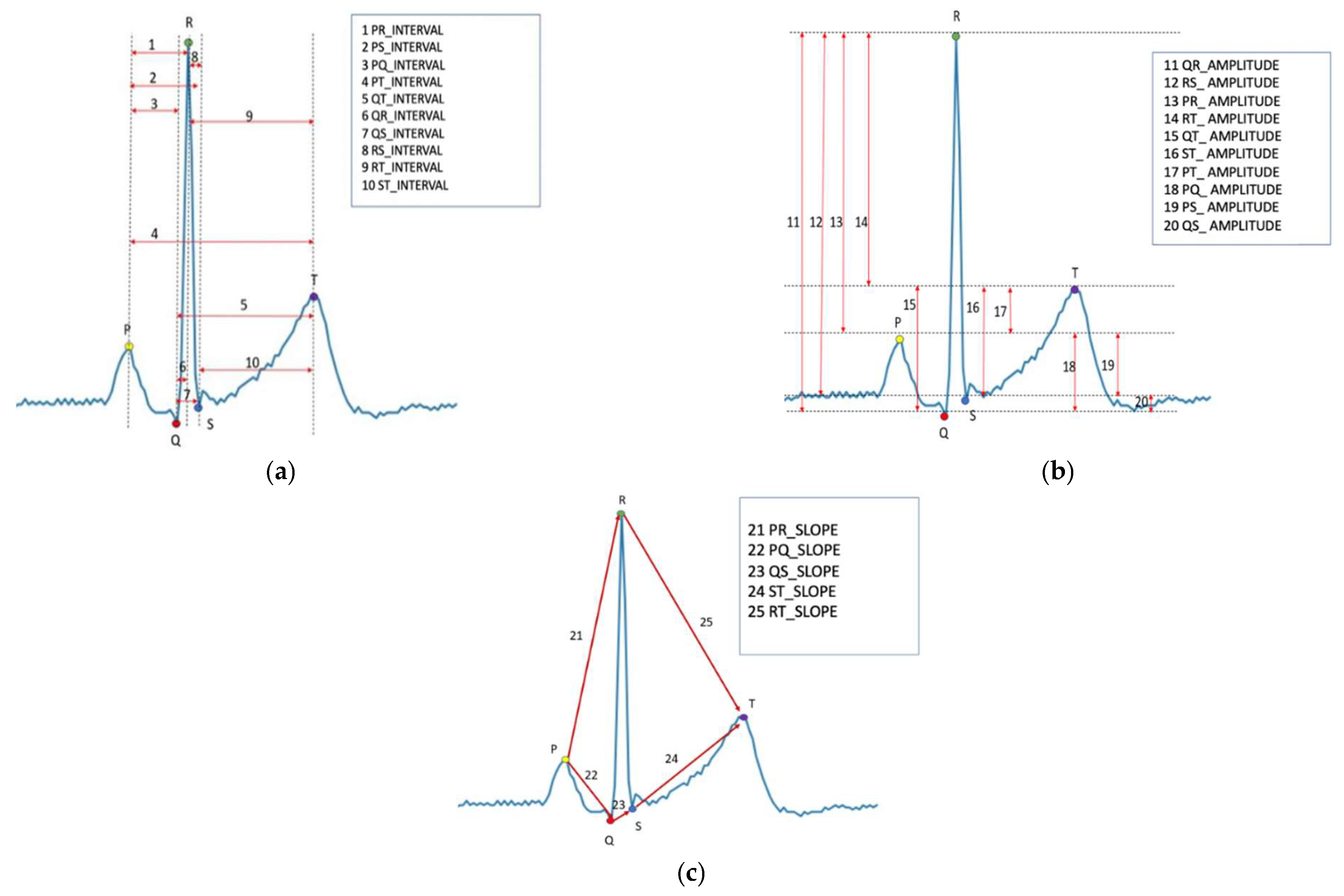
2.3. ECG Segmentation and Feature Extraction
2.4. Machine-Learning Algorithm
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Capes, S.E.; Hunt, D.; Malmberg, K.; Gerstein, H.C. Stress hyperglycaemia and increased risk of death after myocardial infarction in patients with and without diabetes: A systematic overview. Lancet 2000, 355, 773–778. [Google Scholar] [CrossRef]
- Sung, J.; Bochicchio, G.V.; Joshi, M.; Bochicchio, K.; Tracy, K.; Scalea, T.M. Admission hyperglycemia is predictive of outcome in critically ill trauma patients. J. Trauma 2005, 59, 80–83. [Google Scholar] [CrossRef]
- Krinsley, J.S. Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients. Mayo Clin. Proc. 2003, 78, 1471–1478. [Google Scholar] [CrossRef]
- Falciglia, M.; Freyberg, R.W.; Almenoff, P.L.; D’Alessio, D.A.; Render, M.L. Hyperglycemia-related mortality in critically ill patients varies with admission diagnosis. Crit. Care Med. 2009, 37, 3001–3009. [Google Scholar] [CrossRef]
- Armstrong, C. ADA Updates Standards of Medical Care for Patients with Diabetes Mellitus. Am. Fam. Physician 2017, 95, 40–43. [Google Scholar]
- Battelino, T.; Phillip, M.; Bratina, N.; Nimri, R.; Oskarsson, P.; Bolinder, J. Effect of continuous glucose monitoring on hypoglycemia in type 1 diabetes. Diabetes Care 2011, 34, 795–800. [Google Scholar] [CrossRef]
- Karter, A.J.; Ferrara, A.; Darbinian, J.A.; Ackerson, L.M.; Selby, J.V. Self-monitoring of blood glucose: Language and financial barriers in a managed care population with diabetes. Diabetes Care 2000, 23, 477–483. [Google Scholar] [CrossRef]
- Vincze, G.; Barner, J.C.; Lopez, D. Factors associated with adherence to self-monitoring of blood glucose among persons with diabetes. Diabetes Educ. 2004, 30, 112–125. [Google Scholar] [CrossRef]
- Cappon, G.; Vettoretti, M.; Sparacino, G.; Facchinetti, A. Continuous Glucose Monitoring Sensors for Diabetes Management: A Review of Technologies and Applications. Diabetes Metab. J. 2019, 43, 383–397. [Google Scholar] [CrossRef]
- Chen, C.; Zhao, X.L.; Li, Z.H.; Zhu, Z.G.; Qian, S.H.; Flewitt, A.J. Current and Emerging Technology for Continuous Glucose Monitoring. Sensors 2017, 17, 182. [Google Scholar] [CrossRef]
- So, C.F.; Choi, K.S.; Wong, T.K.; Chung, J.W. Recent advances in noninvasive glucose monitoring. Med. Devices 2012, 5, 45–52. [Google Scholar]
- Juan, C.G.; Potelon, B.; Quendo, C.; Bronchalo, E. Microwave Planar Resonant Solutions for Glucose Concentration Sensing: A Systematic Review. Appl. Sci. 2021, 11, 7018. [Google Scholar] [CrossRef]
- Singh, J.P.; Larson, M.; O’Donnell, C.J.; Wilson, P.F.; Tsuji, H.; Lloyd-Jones, D.; Levy, D. Association of hyperglycemia with reduced heart rate variability (The Framingham Heart Study). Am. J. Cardiol. 2000, 86, 309–312. [Google Scholar] [CrossRef] [PubMed]
- Laptev, D.N.; Riabykina, G.V.; Seid-Guseĭnov, A.A. 24-hours monitoring of ECG and glucose level for detection of relations between glycemia and QT interval duration in patients with type 1 diabetes. Ter. Arkh. 2009, 81, 28–33. [Google Scholar]
- Tobore, I.; Li, J.; Kandwal, A.; Yuhang, L.; Nie, Z.; Wang, L. Statistical and spectral analysis of ECG signal towards achieving non-invasive blood glucose monitoring. BMC Med. Inform. Decis. Mak. 2019, 19, 266. [Google Scholar] [CrossRef]
- Hannun, A.Y.; Rajpurkar, P.; Haghpanahi, M.; Tison, G.H.; Bourn, C.; Turakhia, M.P.; Ng, A.Y. Cardiologist-level arrhythmia detection and classification in ambulatory electrocardiograms using a deep neural network. Nat. Med. 2019, 25, 65–69. [Google Scholar] [CrossRef]
- Attia, Z.I.; Noseworthy, P.A.; Lopez-Jimenez, F.; Asirvatham, S.J.; Deshmukh, A.J.; Gersh, B.J.; E Carter, R.; Yao, X.; A Rabinstein, A.; Erickson, B.J.; et al. An artificial intelligence-enabled ECG algorithm for the identification of patients with atrial fibrillation during sinus rhythm: A retrospective analysis of outcome prediction. Lancet 2019, 394, 8617. [Google Scholar] [CrossRef]
- Galloway, C.D.; Valys, A.V.; Shreibati, J.B.; Treiman, D.L.; Petterson, F.L.; Gundotra, V.P.; Albert, D.E.; Attia, Z.I.; Carter, R.E.; Asirvatham, S.J.; et al. Development and validation of a deep-learning model to screen for hyperkalemia from the electrocardiogram. JAMA Cardiol. 2019, 4, 428–436. [Google Scholar] [CrossRef]
- Mujahid, O.; Contreras, I.; Vehi, J. Machine Learning Techniques for Hypoglycemia Prediction: Trends and Challenges. Sensors 2021, 21, 546. [Google Scholar] [CrossRef]
- Kodama, S.; Fujihara, K.; Shiozaki, H.; Horikawa, C.; Yamada, M.H.; Sato, T.; Yaguchi, Y.; Yamamoto, M.; Kitazawa, M.; Iwanaga, M.; et al. Ability of Current Machine Learning Algorithms to Predict and Detect Hypoglycemia in Patients with Diabetes Mellitus: Meta-analysis. JMIR Diabetes 2021, 6, e22458. [Google Scholar] [CrossRef]
- Moody, B.; Moody, G.; Villarroel, M.; Clifford, G.; Silva, I. MIMIC-III Waveform Database Matched Subset (version 1.0). PhysioNet 2020. [Google Scholar] [CrossRef]
- Johnson, A.E.W.; Pollard, T.J.; Shen, L.; Lehman, L.-W.H.; Feng, M.; Ghassemi, M.; Moody, B.; Szolovits, P.; Celi, L.A.; Mark, R.G. MIMIC-III, a freely accessible critical care database. Sci. Data 2016, 3, 160035. [Google Scholar] [CrossRef] [PubMed]
- Carreiras, C.; Alves, A.P.; Lourenço, A.; Canento, F.; Silva, H.; Fred, A. BioSPPy-Biosignal Processing in Python. 2015. Available online: https://github.com/PIA-Group/BioSPPy/ (accessed on 7 December 2022).
- Lee, G.; Gommers, R.; Wohlfahrt, K.; Wasilewski, F.; O’Leary, A.; Nahrstaedt, H.; Sauvé, A.; Agrawal, A.; Pelt, D.M.; Oliveira, H.; et al. PyWavelets/pywt: V1.4.1. Zenodo 2022. [Google Scholar] [CrossRef]
- Wagner, J.; Malchoff, C.; Abbott, G. Invasiveness as a barrier to self-monitoring of blood glucose in diabetes. Diabetes Technol. Ther. 2005, 7, 612–619. [Google Scholar] [CrossRef] [PubMed]
- Isakadze, N.; Martin, S.S. How useful is the smartwatch ECG? Trends Cardiovasc. Med. 2020, 30, 442–448. [Google Scholar] [CrossRef]
- Gruden, G.; Giunti, S.; Barutta, F.; Chaturvedi, N.; Witte, D.R.; Tricarico, M.; Fuller, J.H.; Cavallo Perin, P.; Bruno, G. QTc interval prolongation is independently associated with severe hypoglycemic attacks in type 1 diabetes from the EURODIAB IDDM complications study. Diabetes Care 2012, 35, 125–127. [Google Scholar] [CrossRef][Green Version]
- Pickham, D.; Flowers, E.; Drew, B.J. Hyperglycemia is associated with corrected QT prolongation and mortality in acutely ill patients. J. Cardiovasc. Nurs. 2014, 29, 264–270. [Google Scholar] [CrossRef]
- Pan, G.Z.; Xie, J.; Tian, X.F.; Yang, S.W.; Zhou, Y.J. The Impact of Different Plasma Glucose Levels on Heart Rate in Experimental Rats with Acute Myocardial Infarction. Cardiol. Res. 2016, 7, 146–151. [Google Scholar] [CrossRef][Green Version]
- Ling, S.H.; San, P.P.; Lam, H.K.; Nguyen, H.T. Hypoglycemia detection: Multiple regression-based combinational neural logic approach. Soft Comput. 2017, 21, 543–553. [Google Scholar] [CrossRef]
- San, P.P.; Ling, S.H.; Nguyen, H.T. Deep learning framework for detection of hypoglycemic episodes in children with type 1 diabetes. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2016, 2016, 3503–3506. [Google Scholar]
- Cordeiro, R.; Karimian, N.; Park, Y. Hyperglycemia Identification Using ECG in Deep Learning Era. Sensors 2021, 21, 6263. [Google Scholar] [CrossRef]
- Nguyen, L.L.; Su, S.; Nguyen, H.T. Identification of hypoglycemia and hyperglycemia in type 1 diabetic patients using ECG parameters. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2012, 2012, 2716–2719. [Google Scholar] [PubMed]
- Porumb, M.; Stranges, S.; Pescapè, A.; Pecchia, L. Precision Medicine and Artificial Intelligence: A Pilot Study on Deep Learning for Hypoglycemic Events Detection based on ECG. Sci. Rep. 2020, 10, 170. [Google Scholar] [CrossRef]
- Lipponen, J.A.; Kemppainen, J.; Karjalainen, P.A.; Laitinen, T.; Mikola, H.; Kärki, T.; Tarvainen, M.P. Dynamic estimation of cardiac repolarization characteristics during hypoglycemia in healthy and diabetic subjects. Physiol. Meas. 2011, 32, 649–660. [Google Scholar] [CrossRef]
- Olde Bekkink, M.; Koeneman, M.; de Galan, B.E.; Bredie, S.J. Early Detection of Hypoglycemia in Type 1 Diabetes Using Heart Rate Variability Measured by a Wearable Device. Diabetes Care 2019, 42, 689–692. [Google Scholar] [CrossRef]
- Amanipour, R.; Nazeran, H.; Reyes, I.; Franco, M.; Haltiwanger, E. The effects of blood glucose changes on frequency-domain measures of HRV signal in type 1 diabetes. In Proceedings of the CONIELECOMP 2012, 22nd International Conference on Electrical Communications and Computers, Cholula, Puebla, Mexico, 27–29 February 2012; pp. 50–54. [Google Scholar]
- Gordin, D.; Forsblom, C.; Rönnback, M.; Groop, P.H. Acute hyperglycaemia disturbs cardiac repolarization in Type 1 diabetes. Diabet Med. 2008, 25, 101–105. [Google Scholar] [CrossRef]
- Robinson, R.T.; Harris, N.D.; Ireland, R.H.; Lee, S.; Newman, C.; Heller, S.R. Mechanisms of abnormal cardiac repolarization during insulin-induced hypoglycemia. Diabetes 2003, 52, 1469–1474. [Google Scholar] [CrossRef] [PubMed]
- Kaze, A.D.; Yuyun, M.F.; Erqou, S.; Fonarow, G.C.; Echouffo-Tcheugui, J.B. Severe Hypoglycemia and Incidence of QT Interval Prolongation Among Adults with Type 2 Diabetes. J. Clin. Endocrinol. Metab. 2022, 107, e2743-50. [Google Scholar] [CrossRef]
- van Noord, C.; Sturkenboom, M.C.; Straus, S.M.; Hofman, A.; Kors, J.A.; Witteman, J.C.; Stricker, B.H. Serum glucose and insulin are associated with QTc and RR intervals in nondiabetic elderly. Eur. J. Endocrinol. 2010, 162, 241–248. [Google Scholar] [CrossRef][Green Version]
- Laitinen, T.; Lyyra-Laitinen, T.; Huopio, H.; Vauhkonen, I.; Halonen, T.; Hartikainen, J.; Niskanen, L.; Laakso, M. Electrocardiographic alterations during hyperinsulinemic hypoglycemia in healthy subjects. Ann. Noninvasive Electrocardiol. 2008, 13, 97–105. [Google Scholar] [CrossRef]
- Marfella, R.; Nappo, F.; De Angelis, L.; Siniscalchi, M.; Rossi, F.; Giugliano, D. The effect of acute hyperglycaemia on QTc duration in healthy man. Diabetologia 2000, 43, 571–575. [Google Scholar] [CrossRef] [PubMed]
- Bathula, R.; Hughes, A.D.; Panerai, R.; Potter, J.; Thom, S.A.M.; Francis, D.P.; Shore, A.C.; Kooner, J.; Chaturvedi, N. Indian Asians have poorer cardiovascular autonomic function than Europeans: This is due to greater hyperglycaemia and may contribute to their greater risk of heart disease. Diabetologia 2010, 53, 2120–2128. [Google Scholar] [CrossRef]
- Bouzid, Z.; Al-Zaiti, S.S.; Bond, R.; Sejdić, E. Remote and wearable ECG devices with diagnostic abilities in adults: A state-of-the-science scoping review. Heart Rhythm. 2022, 19, 1192–1201. [Google Scholar] [CrossRef] [PubMed]
| Variables | Median (IQR)/N (%) |
|---|---|
| Age, median (IQR) | 64 (55–72) |
| Male, n (%) | 27 (54.0) |
| Race | |
| White | 29 (58.0) |
| Black | 10 (20.0) |
| Asian | 2 (4.0) |
| Latino | 2 (4.0) |
| Height (cm), median (IQR) | 172 (163–180) |
| Weight (Kg), median (IQR) | 83.6 (70.2–96.3) |
| BMI, median (IQR) | 27.9 (25.4–29.7) |
| Diagnosis at admission | |
| Cardiovascular | 13 (26.0) |
| CNS | 11 (22.0) |
| Respiratory | 7 (14.0) |
| Infectious | 6 (12.0) |
| Gastrointestinal | 4 (8.0) |
| Metabolic | 4 (8.0) |
| Others | 5 (10.0) |
| Normal | Dysglycemia | p-Value | |
|---|---|---|---|
| R–R interval (s) | 0.74 ± 0.52 | 0.66 ± 0.50 | <0.001 |
| P–Q interval (s) | 0.13 ± 0.07 | 0.16 ± 0.09 | <0.001 |
| Q–R interval (s) | 0.08 ± 0.06 | 0.07 ± 0.05 | <0.001 |
| R–S interval (s) | 0.04 ± 0.03 | 0.05 ± 0.03 | <0.001 |
| S–T interval (s) | 0.25 ± 0.08 | 0.32 ± 0.09 | <0.001 |
| P–R interval (s) | 0.21 ± 0.09 | 0.23 ± 0.10 | <0.001 |
| Q–T interval (s) | 0.37 ± 0.13 | 0.44 ± 0.15 | <0.001 |
| P–Q amplitude (mV) | 0.13 ± 0.05 | 0.15 ± 0.07 | <0.001 |
| Q–R amplitude (mV) | 0.68 ± 0.46 | 0.56 ± 0.43 | <0.001 |
| R–S amplitude (mV) | 0.75 ± 0.56 | 0.71 ± 0.49 | <0.001 |
| Q–S amplitude (mV) | 0.07 ± 0.05 | 0.05 ± 0.04 | <0.001 |
| S–T amplitude (mV) | 0.64 ± 0.43 | 0.58 ± 0.34 | <0.001 |
| P–R slope (mV/s) | 0.61 ± 0.58 | 0.81 ± 0.79 | <0.001 |
| P–Q slope (mV/s) | −1.14 ± 0.53 | −1.08 ± 0.58 | <0.001 |
| Q–S slope (mV/s) | −0.31 ± 0.27 | −0.12 ± 0.08 | <0.001 |
| S–T slope (mV/s) | 5.92 ± 5.91 | 4.64 ± 4.95 | <0.001 |
| R–T slope (mV/s) | −0.68 ± 0.60 | −0.58 ± 0.68 | <0.001 |
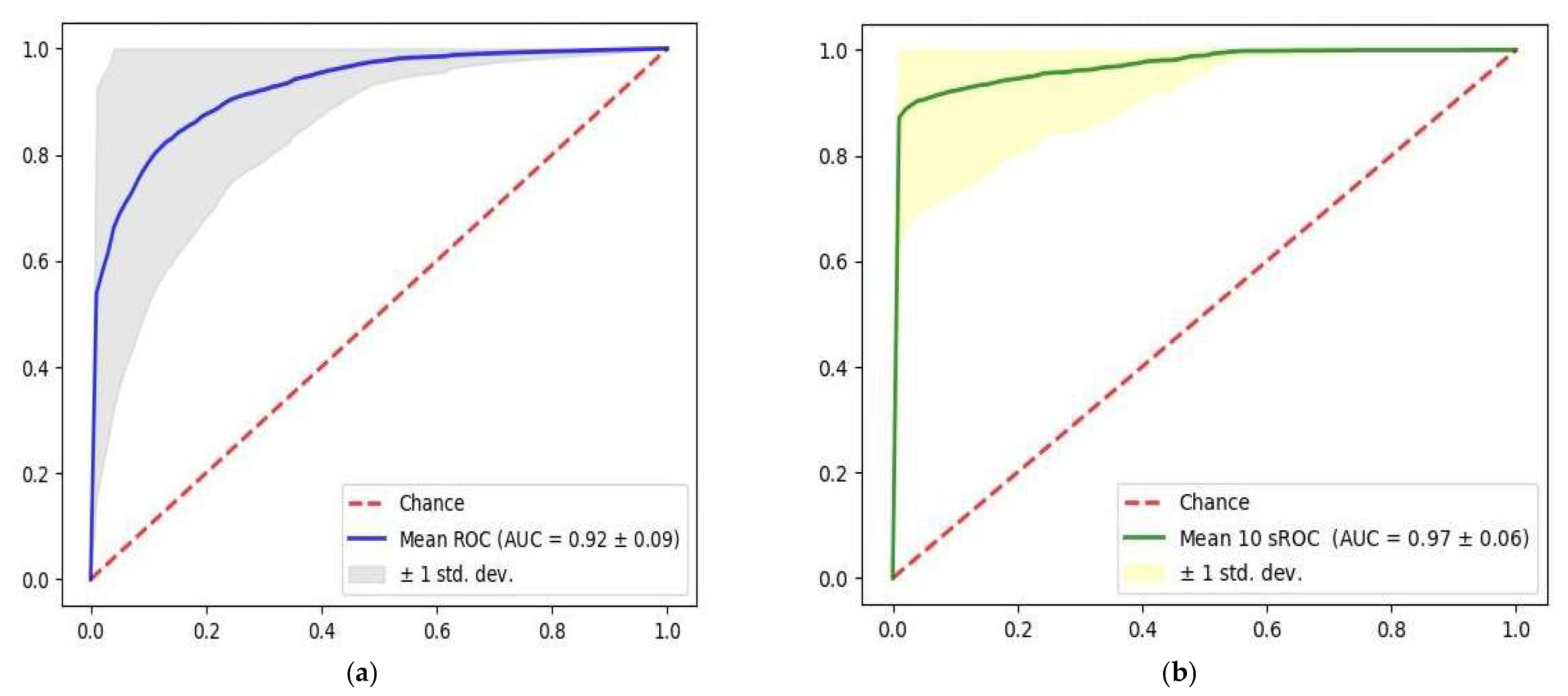
| Oc-SVM | AUC | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|---|
| Single heartbeat | 0.92 ± 0.09 | 0.92 ± 0.10 | 0.84 ± 0.04 | 0.85 ± 0.03 | 0.92 ± 0.09 |
| 10 s | 0.97 ± 0.06 | 0.97 ± 0.09 | 0.96 ± 0.04 | 0.96 ± 0.04 | 0.97 ± 0.09 |
| ECG Features | F-Score |
|---|---|
| R–R interval | 591 |
| R–S amplitude | 271 |
| P–T amplitude | 153 |
| Q–R amplitude | 150 |
| Q–T interval | 98 |
| S–T slope | 97 |
| R–T amplitude | 76 |
| R–S interval | 76 |
| P–S amplitude | 72 |
| P–Q amplitude | 69 |
| P–R slope | 69 |
| R–T slope | 69 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chiu, I.-M.; Cheng, C.-Y.; Chang, P.-K.; Li, C.-J.; Cheng, F.-J.; Lin, C.-H.R. Utilization of Personalized Machine-Learning to Screen for Dysglycemia from Ambulatory ECG, toward Noninvasive Blood Glucose Monitoring. Biosensors 2023, 13, 23. https://doi.org/10.3390/bios13010023
Chiu I-M, Cheng C-Y, Chang P-K, Li C-J, Cheng F-J, Lin C-HR. Utilization of Personalized Machine-Learning to Screen for Dysglycemia from Ambulatory ECG, toward Noninvasive Blood Glucose Monitoring. Biosensors. 2023; 13(1):23. https://doi.org/10.3390/bios13010023
Chicago/Turabian StyleChiu, I-Min, Chi-Yung Cheng, Po-Kai Chang, Chao-Jui Li, Fu-Jen Cheng, and Chun-Hung Richard Lin. 2023. "Utilization of Personalized Machine-Learning to Screen for Dysglycemia from Ambulatory ECG, toward Noninvasive Blood Glucose Monitoring" Biosensors 13, no. 1: 23. https://doi.org/10.3390/bios13010023
APA StyleChiu, I.-M., Cheng, C.-Y., Chang, P.-K., Li, C.-J., Cheng, F.-J., & Lin, C.-H. R. (2023). Utilization of Personalized Machine-Learning to Screen for Dysglycemia from Ambulatory ECG, toward Noninvasive Blood Glucose Monitoring. Biosensors, 13(1), 23. https://doi.org/10.3390/bios13010023






