Design and Fabrication of Capillary-Driven Flow Device for Point-Of-Care Diagnostics
Abstract
:1. Introduction
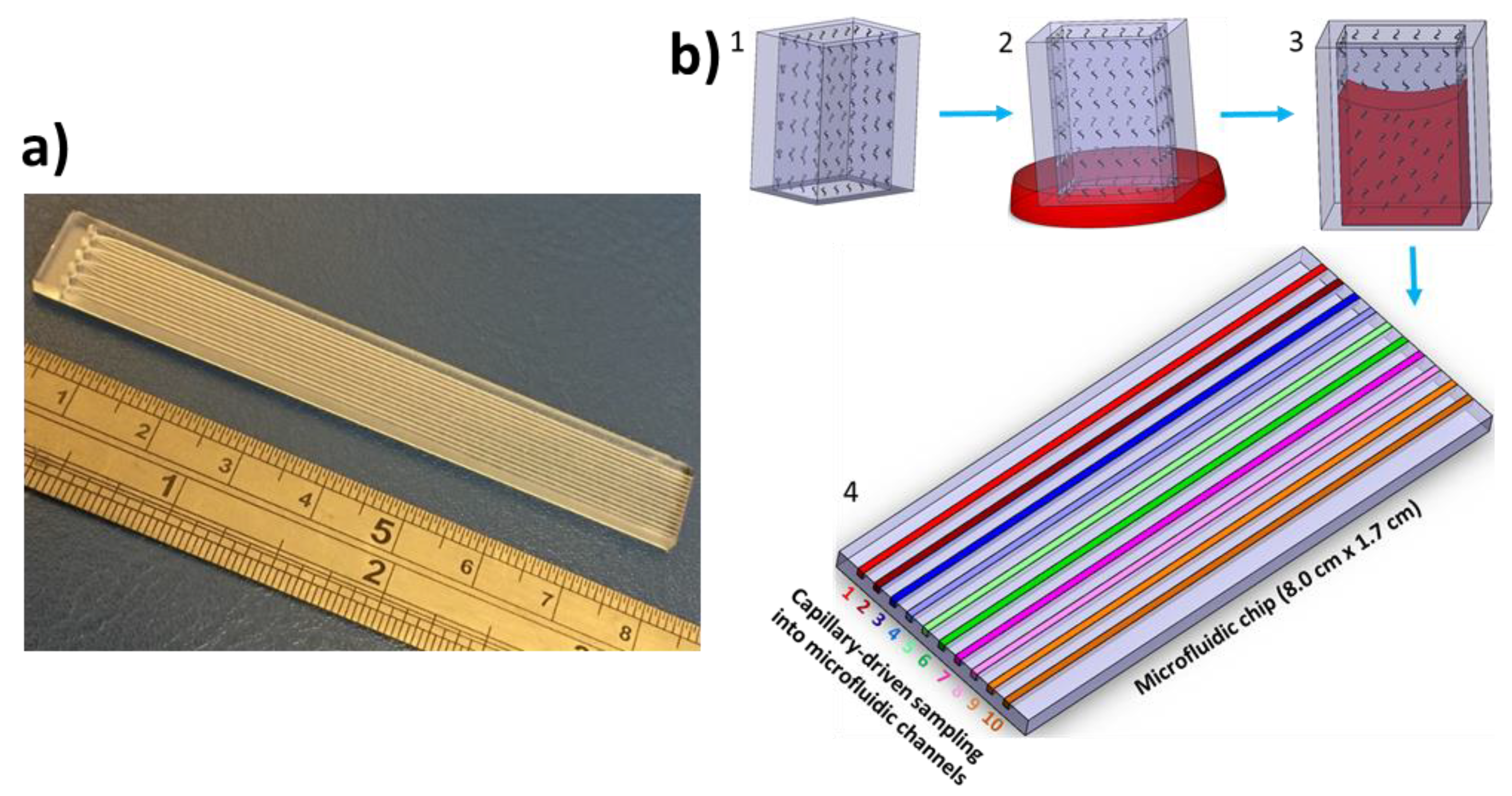
2. Experimental
3. Results and Discussion
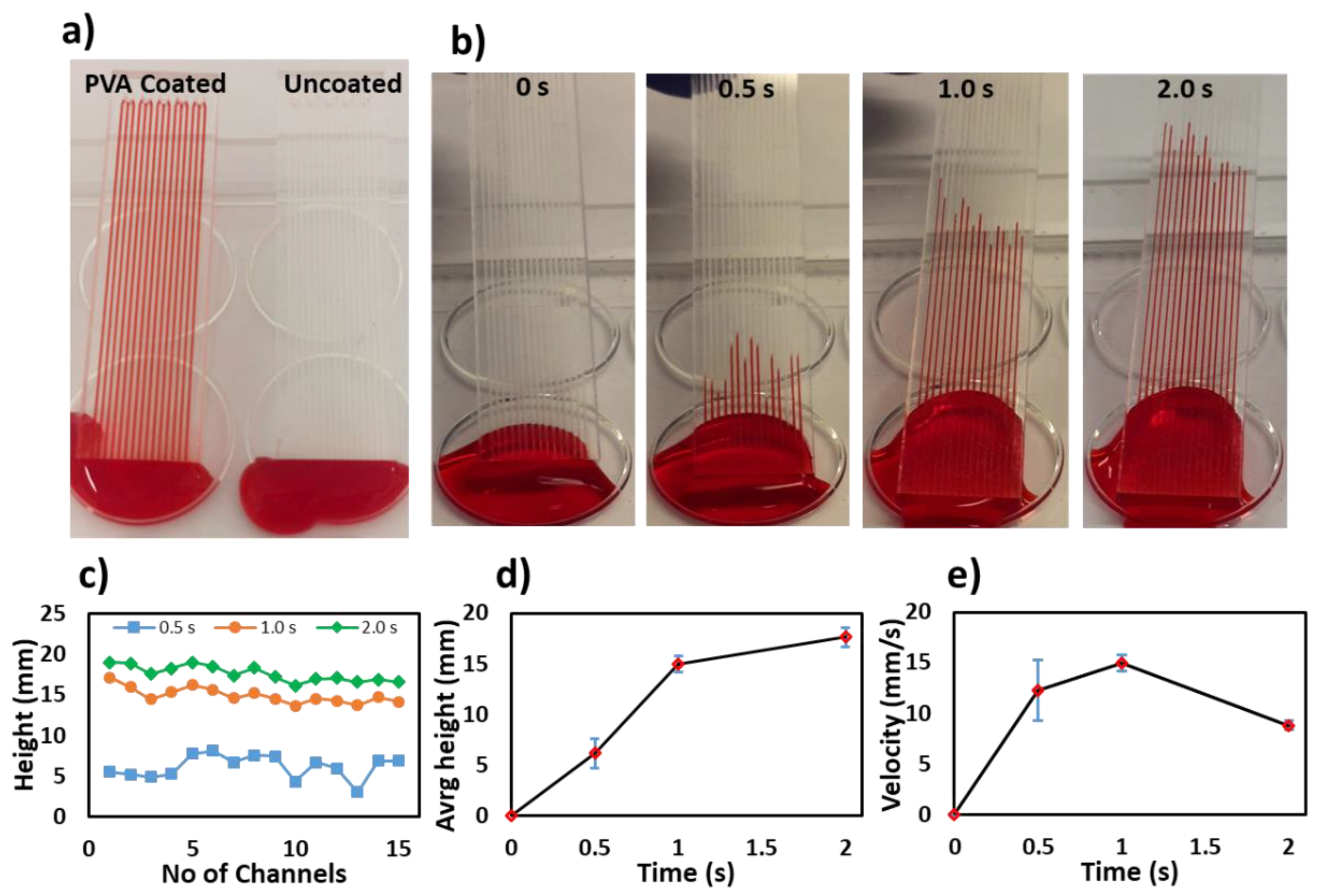
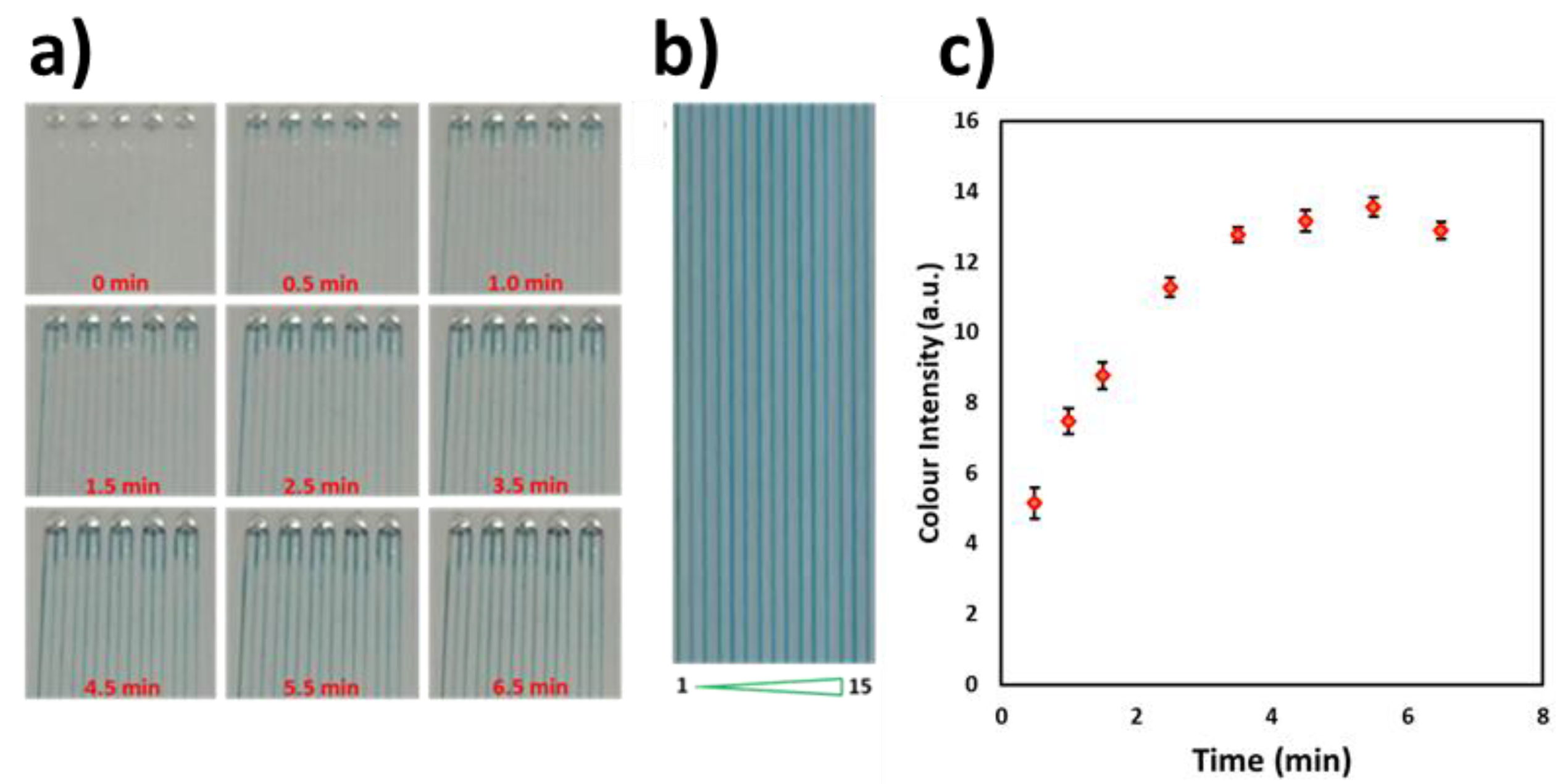
3.1. Characterization of the PVA Coating in Microchannels
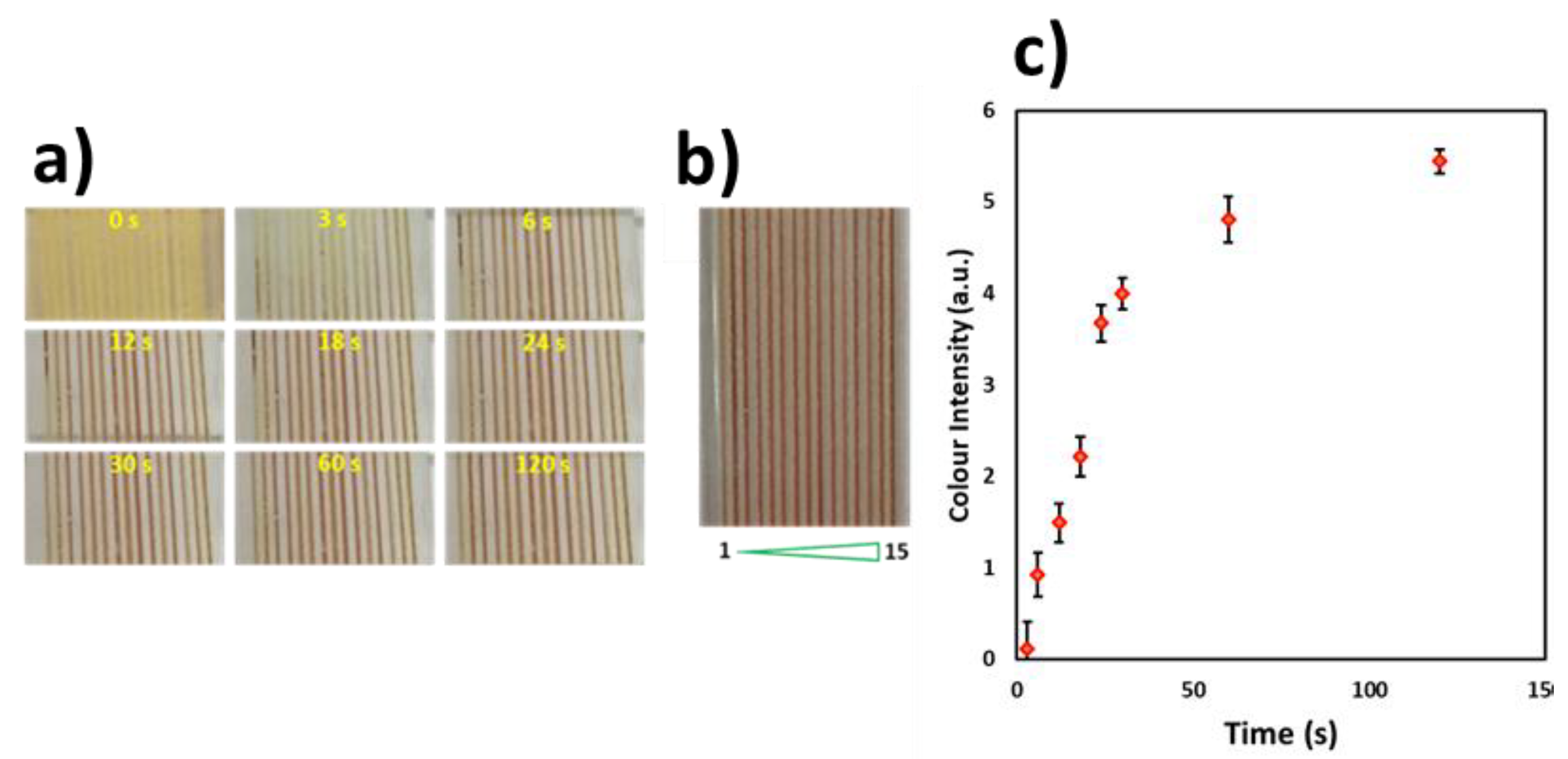
3.2. Characterization of Reagent Cross-Linking inside the Microchannels
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Stange, M.; Dreyer, M.E.; Rath, H.J. Capillary driven flow in circular cylindrical tubes. Phys. Fluids 2003, 15, 2587–2601. [Google Scholar] [CrossRef]
- Hassan, S.-U.; Zhang, X. Microfluidics as an Emerging Platform for Tackling Antimicrobial Resistance (AMR): A Review. Curr. Anal. Chem. 2020, 16, 41–51. [Google Scholar] [CrossRef] [Green Version]
- Liu, Z.; Banaei, N.; Ren, K. Microfluidics for Combating Antimicrobial Resistance. Trends Biotechnol. 2017, 35, 1129–1139. [Google Scholar] [CrossRef] [PubMed]
- Ramalingam, N.; Warkiani, M.E.; Ramalingam, N.; Keshavarzi, G.; Hao-Bing, L.; Hai-Qing, T.G. Numerical and experimental study of capillary-driven flow of PCR solution in hybrid hydrophobic microfluidic networks. Biomed. Microdevices 2016, 18, 68. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Chou, T.-C.; Kang, N.; Kang, H.; Chen, J.; Baek, K.I.; Wang, W.; Ding, Y.; Di Carlo, D.; Tai, Y.-C.; et al. A Rapid Capillary-Pressure Driven Micro-Channel to Demonstrate Newtonian Fluid Behavior of Zebrafish Blood at High Shear Rates. Sci. Rep. 2017, 7, 1980. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bamshad, A.; Nikfarjam, A.; Sabour, M.H. Capillary-based micro-optofluidic viscometer. Meas. Sci. Technol. 2018, 29, 095901. [Google Scholar] [CrossRef]
- He, F.; Wang, Y.; Jin, S.; Nugen, S.R. Development of a capillary-driven, microfluidic, nucleic acid biosensor. Sens. Transducers 2011, 13, 150–158. [Google Scholar]
- Fuchiwaki, Y.; Takaoka, H. UV-laser-assisted modification of poly(methyl methacrylate) and its application to capillary-driven-flow immunoassay. J. Micromech. Microeng. 2015, 25, 75008. [Google Scholar] [CrossRef]
- Uchiyama, Y.; Okubo, F.; Akai, K.; Fujii, Y.; Henares, T.G.; Kawamura, K.; Yao, T.; Endo, T.; Hisamoto, H. Combinable poly(dimethyl siloxane) capillary sensor array for single-step and multiple enzyme inhibitor assays. Lab Chip 2012, 12, 204–208. [Google Scholar] [CrossRef]
- Fujii, Y.; Henares, T.G.; Kawamura, K.; Endo, T.; Hisamoto, H. Bulk- and surface-modified combinable PDMS capillary sensor array as an easy-to-use sensing device with enhanced sensitivity to elevated concentrations of multiple serum sample components. Lab Chip 2012, 12, 1522. [Google Scholar] [CrossRef]
- Huang, C.; Jones, B.J.; Bivragh, M.; Jans, K.; Lagae, L.; Peumans, P. A Capillary-Driven Microfluidic Device for Rapid DNA Detection with Extremely Low Sample Consumption. In Proceedings of the 17th International Conference on Miniaturized Systems for Chemistry and Life Sciences, µTAS 2013 Conference, Freiburg, Germany, 27–31 October 2013; pp. 191–193. [Google Scholar]
- Epifania, R.; Soares, R.R.G.; Pinto, I.F.; Chu, V.; Conde, J.P. Capillary-driven microfluidic device with integrated nanoporous microbeads for ultrarapid biosensing assays. Sens. Actuators B Chem. 2018, 265, 452–458. [Google Scholar] [CrossRef]
- Madadi, H.; Casals-Terre, J.; Mohammadi, M. Self-driven filter-based blood plasma separator microfluidic chip for point-of-care testing. Biofabrication 2015, 7, 025007. [Google Scholar] [CrossRef] [PubMed]
- Lade, R.K.; Hippchen, E.J.; Macosko, C.W.; Francis, L.F. Dynamics of Capillary-Driven Flow in 3D Printed Open Microchannels. Langmuir 2017, 33, 2949–2964. [Google Scholar] [CrossRef] [PubMed]
- Gervais, L.; Delamarche, E. Toward one-step point-of-care immunodiagnostics using capillary-driven microfluidics and PDMS substrates. Lab Chip 2009, 9, 3330. [Google Scholar] [CrossRef]
- Delamarche, E.; Temiz, Y.; Gökçe, O.; Arango, Y. Precision Diagnostics for Mobile Health Using Capillary-driven Microfluidics. Chim. Int. J. Chem. 2017, 71, 385. [Google Scholar] [CrossRef]
- Lapierre, F.; Gooley, A.; Breadmore, M. Principles around Accurate Blood Volume Collection Using Capillary Action. Langmuir 2017, 33, 14220–14225. [Google Scholar] [CrossRef]
- Reis, N.M.; Pivetal, J.; Loo-Zazueta, A.L.; Barros, J.; Edwards, A. Lab on a Stick: Multi-Analyte Cellular Assays in a Microfluidic Dipstick. Lab Chip 2016, 16, 2891–2899. [Google Scholar] [CrossRef] [Green Version]
- Pivetal, J.; Pereira, F.M.; Barbosa, A.I.; Castanheira, A.P.; Reis, N.M.; Edwards, A. Covalent immobilisation of antibodies in Teflon-FEP microfluidic devices for the sensitive quantification of clinically relevant protein biomarkers. Analyst 2017, 142, 959–968. [Google Scholar] [CrossRef] [Green Version]
- Barbosa, A.I.; Gehlot, P.; Sidapra, K.; Edwards, A.; Reis, N.M. Portable smartphone quantitation of prostate specific antigen (PSA) in a fluoropolymer microfluidic device. Biosens. Bioelectron. 2015, 70, 5–14. [Google Scholar] [CrossRef] [Green Version]
- Barbosa, A.I.; Castanheira, A.P.; Edwards, A.; Reis, N.M. A lab-in-a-briefcase for rapid prostate specific antigen (PSA) screening from whole blood. Lab Chip 2014, 14, 2918–2928. [Google Scholar] [CrossRef] [Green Version]
- Castanheira, A.P.; Barbosa, A.I.; Reis, N.M.; Edwards, A. Multiplexed femtomolar quantitation of human cytokines in a fluoropolymer microcapillary film. Analyst 2015, 140, 5609–5618. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Das, S.; Kumar, N.; Vishweswaraiah, R.; Haldar, L.; Gaare, M.; Singh, V.K.; Puniya, A.K. Microbial based assay for specific detection of β-lactam group of antibiotics in milk. J. Food Sci. Technol. 2014, 51, 1161–1166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hassan, S.-U.; Zhang, X. Design and Fabrication of Optical Flow Cell for Multiplex Detection of β-lactamase in Microchannels. Micromachines 2020, 11, 385. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hassan, S.-U.; Gielien, F.; Niu, X.; Edel, J.B. Controlled one dimensional oscillation of the Belousov–Zhabotinsky reaction confined within microchannels. RSC Adv. 2012, 2, 6408–6410. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hassan, S.-u.; Zhang, X. Design and Fabrication of Capillary-Driven Flow Device for Point-Of-Care Diagnostics. Biosensors 2020, 10, 39. https://doi.org/10.3390/bios10040039
Hassan S-u, Zhang X. Design and Fabrication of Capillary-Driven Flow Device for Point-Of-Care Diagnostics. Biosensors. 2020; 10(4):39. https://doi.org/10.3390/bios10040039
Chicago/Turabian StyleHassan, Sammer-ul, and Xunli Zhang. 2020. "Design and Fabrication of Capillary-Driven Flow Device for Point-Of-Care Diagnostics" Biosensors 10, no. 4: 39. https://doi.org/10.3390/bios10040039
APA StyleHassan, S.-u., & Zhang, X. (2020). Design and Fabrication of Capillary-Driven Flow Device for Point-Of-Care Diagnostics. Biosensors, 10(4), 39. https://doi.org/10.3390/bios10040039




