Potential of Carbon Nanodots (CNDs) in Cancer Treatment
Abstract
1. Introduction
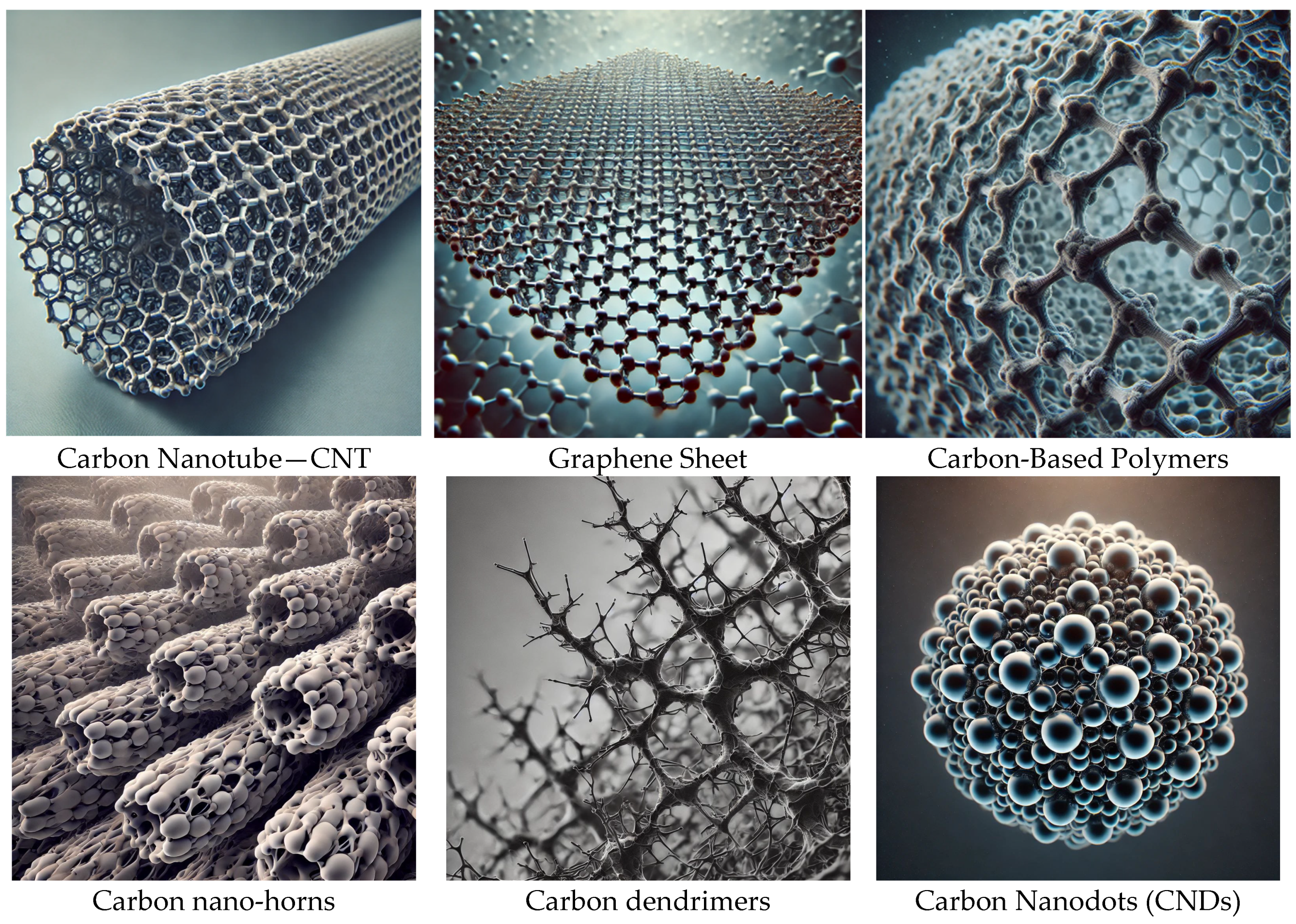
Definition and Characteristics of Carbon Nanodots
2. Overview of Cancer Treatment
Current Challenges in Cancer Treatment
3. Mechanisms of Action of Carbon Nanodots in Cancer Treatment
Cellular Uptake and Intracellular Localization
4. Applications of Carbon Nanodots in Cancer Treatment
Drug Delivery Systems
5. Biocompatibility and Toxicity of Carbon Nanodots
In Vitro and In Vivo Studies
6. Future Perspectives and Challenges
Clinical Translation and Regulatory Hurdles
Funding
Data Availability Statement
Conflicts of Interest
References
- Sekar, R.; Basavegowda, N.; Jena, S.; Jayakodi, S.; Elumalai, P.; Chaitanyakumar, A.; Somu, P.; Baek, K.-H. Recent Developments in Heteroatom/Metal-Doped Carbon Dot-Based Image-Guided Photodynamic Therapy for Cancer. Pharmaceutics 2022, 14, 1869. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Dunphy, A.; Anike, M.S.; Belperain, S.; Patel, K.; Chiu, N.H.; Jia, Z. Recent Advances in Carbon Nanodots: A Promising Nanomaterial for Biomedical Applications. Int. J. Mol. Sci. 2021, 22, 6786. [Google Scholar] [CrossRef] [PubMed]
- Gong, X.; Wang, Z.; Zhang, L.; Dong, W.; Wang, R.; Liu, Y.; Song, S.; Hu, Q.; Du, F.; Shuang, S. A Novel Carbon-Nanodots-Based Theranostic Nano-Drug Delivery System for Mitochondria-Targeted Imaging and Glutathione-Activated Delivering Camptothecin. Colloids Surf. B Biointerfaces 2022, 218, 112712. [Google Scholar] [CrossRef] [PubMed]
- Malhan, A.; Guleria, M.; Das, U.; Singh, S.; Prajapati, B.G.; Mohite, P.; Bhattacharya, S.; Chidrawar, V.R.; Puri, A.; Datta, D. Navigating the Future of Cancer Management through Carbon Nanodots: A Review. Nano-Struct. Nano-Objects 2024, 39, 101217. [Google Scholar] [CrossRef]
- Bartkowski, M.; Zhou, Y.; Nabil Amin Mustafa, M.; Eustace, A.J.; Giordani, S. CARBON DOTS: Bioimaging and Anticancer Drug Delivery. Chem. A Eur. J. 2024, 30, e202303982. [Google Scholar] [CrossRef]
- Kapat, K.; Semwal, N.; Chillarge, A.; Aswani, A. Multifunctional Carbon Nanodot-Based Advanced Diagnostics and Therapeutics. Adv. Ther. 2023, 6, 2300189. [Google Scholar] [CrossRef]
- Lamba, R.; Yukta, Y.; Mondal, J.; Kumar, R.; Pani, B.; Singh, B. Carbon Dots: Synthesis, Characterizations, and Recent Advancements in Biomedical, Optoelectronics, Sensing, and Catalysis Applications. ACS Appl. Bio Mater. 2024, 7, 2086–2127. [Google Scholar] [CrossRef]
- Dhamodharan, D.; Byun, H.-S.; Shree, M.V.; Veeman, D.; Natrayan, L.; Stalin, B. Carbon Nanodots: Synthesis, Mechanisms for Bio-Electrical Applications. J. Ind. Eng. Chem. 2022, 110, 68–83. [Google Scholar] [CrossRef]
- Kumara, B.N.; Kalimuthu, P.; Prasad, K.S. Synthesis, Properties and Potential Applications of Photoluminescent Carbon Nanoparticles: A Review. Anal. Chim. Acta 2023, 1268, 341430. [Google Scholar] [CrossRef]
- Ratre, P.; Nazeer, N.; Kumari, R.; Thareja, S.; Jain, B.; Tiwari, R.; Kamthan, A.; Srivastava, R.K.; Mishra, P.K. Carbon-Based Fluorescent Nano-Biosensors for the Detection of Cell-Free Circulating MicroRNAs. Biosensors 2023, 13, 226. [Google Scholar] [CrossRef]
- Wang, H.; Wang, Q.; Wang, Q.; Dong, W.; Liu, Y.; Hu, Q.; Song, X.; Shuang, S.; Dong, C.; Gong, X. Metal-Free Nitrogen-Doped Carbon Nanodots as an Artificial Nanozyme for Enhanced Antibacterial Activity. J. Clean. Prod. 2023, 411, 137337. [Google Scholar] [CrossRef]
- Yi, W.; Khalid, A.; Arshad, N.; Asghar, M.S.; Irshad, M.S.; Wang, X.; Yi, Y.; Si, J.; Hou, X.; Li, H.R. Recent Progress and Perspective of an Evolving Carbon Family From 0D to 3D: Synthesis, Biomedical Applications, and Potential Challenges. ACS Appl. Bio Mater. 2023, 6, 2043–2088. [Google Scholar] [CrossRef] [PubMed]
- Hassanvand, Z.; Jalali, F.; Nazari, M.; Parnianchi, F.; Santoro, C. Carbon Nanodots in Electrochemical Sensors and Biosensors: A Review. ChemElectroChem 2021, 8, 15–35. [Google Scholar] [CrossRef]
- Kush, P.; Kumar, P.; Singh, R. Functionalized Carbon Nanostructures in Cancer Diagnosis and Therapy. In Handbook of Functionalized Carbon Nanostructures: From Synthesis Methods to Applications; Barhoum, A., Deshmukh, K., Eds.; Springer International Publishing: Cham, Switzerland, 2024; pp. 2091–2130. ISBN 978-3-031-32150-4. [Google Scholar]
- Soerjomataram, I.; Bray, F. Planning for Tomorrow: Global Cancer Incidence and the Role of Prevention 2020–2070. Nat. Rev. Clin. Oncol. 2021, 18, 663–672. [Google Scholar]
- Singh, G.; Kaur, H.; Sharma, A.; Singh, J.; Alajangi, H.K.; Kumar, S.; Singla, N.; Kaur, I.P.; Barnwal, R.P. Carbon Based Nanodots in Early Diagnosis of Cancer. Front. Chem. 2021, 9, 669169. [Google Scholar]
- Frick, C.; Rumgay, H.; Vignat, J.; Ginsburg, O.; Nolte, E.; Bray, F.; Soerjomataram, I. Quantitative Estimates of Preventable and Treatable Deaths from 36 Cancers Worldwide: A Population-Based Study. Lancet Glob. Health 2023, 11, e1700–e1712. [Google Scholar]
- Bray, F.; Laversanne, M.; Sung, H.; Ferlay, J.; Siegel, R.L.; Soerjomataram, I.; Jemal, A. Global Cancer Statistics 2022: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA A Cancer J. Clin. 2024, 74, 229–263. [Google Scholar] [CrossRef]
- Rahib, L.; Wehner, M.R.; Matrisian, L.M.; Nead, K.T. Estimated Projection of US Cancer Incidence and Death to 2040. JAMA Netw. Open 2021, 4, e214708. [Google Scholar]
- Morgan, E.; Arnold, M.; Gini, A.; Lorenzoni, V.; Cabasag, C.J.; Laversanne, M.; Vignat, J.; Ferlay, J.; Murphy, N.; Bray, F. Global Burden of Colorectal Cancer in 2020 and 2040: Incidence and Mortality Estimates from GLOBOCAN. Gut 2023, 72, 338–344. [Google Scholar] [CrossRef]
- Rumgay, H.; Arnold, M.; Ferlay, J.; Lesi, O.; Cabasag, C.J.; Vignat, J.; Laversanne, M.; McGlynn, K.A.; Soerjomataram, I. Global Burden of Primary Liver Cancer in 2020 and Predictions to 2040. J. Hepatol. 2022, 77, 1598–1606. [Google Scholar]
- Zhou, X.; Guo, Z.; Liu, S.; Chen, Z.; Wang, Y.; Yang, R.; Li, X.; Ma, K. Transcriptomics and Molecular Docking Reveal the Potential Mechanism of Lycorine against Pancreatic Cancer. Phytomedicine 2024, 122, 155128. [Google Scholar] [CrossRef] [PubMed]
- Menendez, J.A.; Lupu, R. Fatty Acid Synthase: A Druggable Driver of Breast Cancer Brain Metastasis. Expert. Opin. Ther. Targets 2022, 26, 427–444. [Google Scholar] [CrossRef]
- Vlahopoulos, S.A. Divergent Processing of Cell Stress Signals as the Basis of Cancer Progression: Licensing NFκB on Chromatin. Int. J. Mol. Sci. 2024, 25, 8621. [Google Scholar] [CrossRef]
- Jiménez, R.; Constantinescu, A.; Yazir, M.; Alfonso-Triguero, P.; Pequerul, R.; Parés, X.; Pérez-Alea, M.; Candiota, A.P.; Farrés, J.; Lorenzo, J. Targeting Retinaldehyde Dehydrogenases to Enhance Temozolomide Therapy in Glioblastoma. Int. J. Mol. Sci. 2024, 25, 11512. [Google Scholar] [CrossRef] [PubMed]
- Gupta, J.; Jalil, A.T.; Abd Alzahraa, Z.H.; Aminov, Z.; Alsaikhan, F.; Ramírez-Coronel, A.A.; Ramaiah, P.; Najafi, M. The Metformin Immunoregulatory Actions in Tumor Suppressionand Normal Tissues Protection. CMC 2024, 31, 5370–5396. [Google Scholar] [CrossRef]
- Zhang, Y.; Gao, W.; Ma, Y.; Cheng, L.; Zhang, L.; Liu, Q.; Chen, J.; Zhao, Y.; Tu, K.; Zhang, M. Integrating Pt Nanoparticles with Carbon Nanodots to Achieve Robust Cascade Superoxide Dismutase-Catalase Nanozyme for Antioxidant Therapy. Nano Today 2023, 49, 101768. [Google Scholar] [CrossRef]
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Parkin, D.M.; Piñeros, M.; Znaor, A.; Bray, F. Cancer Statistics for the Year 2020: An Overview. Int. J. Cancer 2021, 149, 778–789. [Google Scholar] [CrossRef]
- Cao, X.; Cao, L.; Zhang, W.; Lu, R.; Bian, J.-S.; Nie, X. Therapeutic Potential of Sulfur-Containing Natural Products in Inflammatory Diseases. Pharmacol. Ther. 2020, 216, 107687. [Google Scholar] [CrossRef]
- Arafat, M.; Sakkal, M.; Beiram, R.; AbuRuz, S. Nanomedicines: Emerging Platforms in Smart Chemotherapy Treatment—A Recent Review. Pharmaceuticals 2024, 17, 315. [Google Scholar] [CrossRef]
- Yang, P.; Xu, Y.; Zhi, X.; Li, R.; Wang, B.; Liu, R.; Dai, Z.; Qian, L. Photodynamically Tumor Vessel Destruction Amplified Tumor Targeting of Nanoparticles for Efficient Chemotherapy. ACS Nano 2024, 18, 12933–12944. [Google Scholar] [CrossRef]
- Cheng, Z.; Li, M.; Dey, R.; Chen, Y. Nanomaterials for Cancer Therapy: Current Progress and Perspectives. J. Hematol. Oncol. 2021, 14, 85. [Google Scholar] [CrossRef]
- Huang, M.; Lu, J.-J.; Ding, J. Natural Products in Cancer Therapy: Past, Present and Future. Nat. Prod. Bioprospect. 2021, 11, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Elmore, L.W.; Greer, S.F.; Daniels, E.C.; Saxe, C.C.; Melner, M.H.; Krawiec, G.M.; Cance, W.G.; Phelps, W.C. Blueprint for Cancer Research: Critical Gaps and Opportunities. CA A Cancer J. Clin. 2021, 71, 107–139. [Google Scholar] [CrossRef]
- Najafi, M.; Majidpoor, J.; Toolee, H.; Mortezaee, K. The Current Knowledge Concerning Solid Cancer and Therapy. J. Biochem. Mol. Toxicol. 2021, 35, e22900. [Google Scholar] [CrossRef] [PubMed]
- Ostańska, E.; Aebisher, D.; Bartusik-Aebisher, D. The Potential of Photodynamic Therapy in Current Breast Cancer Treatment Methodologies. Biomed. Pharmacother. 2021, 137, 111302. [Google Scholar] [CrossRef]
- Lau, K.H.; Tan, A.M.; Shi, Y. New and Emerging Targeted Therapies for Advanced Breast Cancer. Int. J. Mol. Sci. 2022, 23, 2288. [Google Scholar] [CrossRef] [PubMed]
- Garg, P.; Malhotra, J.; Kulkarni, P.; Horne, D.; Salgia, R.; Singhal, S.S. Emerging Therapeutic Strategies to Overcome Drug Resistance in Cancer Cells. Cancers 2024, 16, 2478. [Google Scholar] [CrossRef]
- Zhong, L.; Li, Y.; Xiong, L.; Wang, W.; Wu, M.; Yuan, T.; Yang, W.; Tian, C.; Miao, Z.; Wang, T. Small Molecules in Targeted Cancer Therapy: Advances, Challenges, and Future Perspectives. Signal Transduct. Target. Ther. 2021, 6, 201. [Google Scholar] [CrossRef]
- Labrie, M.; Brugge, J.S.; Mills, G.B.; Zervantonakis, I.K. Therapy Resistance: Opportunities Created by Adaptive Responses to Targeted Therapies in Cancer. Nat. Rev. Cancer 2022, 22, 323–339. [Google Scholar] [CrossRef]
- Blagosklonny, M.V. Selective Protection of Normal Cells from Chemotherapy, While Killing Drug-Resistant Cancer Cells. Oncotarget 2023, 14, 193–206. [Google Scholar] [CrossRef]
- Ciepła, J.; Smolarczyk, R. Tumor Hypoxia Unveiled: Insights into Microenvironment, Detection Tools and Emerging Therapies. Clin. Exp. Med. 2024, 24, 235. [Google Scholar] [CrossRef] [PubMed]
- Debela, D.T.; Muzazu, S.G.; Heraro, K.D.; Ndalama, M.T.; Mesele, B.W.; Haile, D.C.; Kitui, S.K.; Manyazewal, T. New Approaches and Procedures for Cancer Treatment: Current Perspectives. SAGE Open Med. 2021, 9, 20503121211034366. [Google Scholar] [CrossRef] [PubMed]
- Tian, C.; Chen, Z. Immune Therapy: A New Therapy for Acute Myeloid Leukemia. Blood Sci. 2023, 5, 15–24. [Google Scholar] [CrossRef]
- Chen, H.; Luo, K.; Xie, C.; Zhou, L. Nanotechnology of Carbon Dots with Their Hybrids for Biomedical Applications: A Review. Chem. Eng. J. 2024, 496, 153915. [Google Scholar]
- Ahmad, M.A.; Aung, Y.; Widati, A.A.; Sakti, S.C.W.; Sumarsih, S.; Irzaman, I.; Yuliarto, B.; Chang, J.; Fahmi, M.Z. A Perspective on Using Organic Molecules Composing Carbon Dots for Cancer Treatment. Nanotheranostics 2023, 7, 187. [Google Scholar] [CrossRef]
- Rahchamandi, S.Y.R.; Mirhadi, E.; Gheybi, F.; Kazemi-Beydokhti, A.; Jaafari, M.R.; Mostafavi, E.; Kesharwani, P.; Sahebkar, A.; Alavizadeh, S.H. Engineering Carbon-Based Nanomaterials for the Delivery of Platinum Compounds: An Innovative Cancer Disarming Frontier. Environ. Res. 2024, 262, 119933. [Google Scholar] [CrossRef]
- Bhattacharya, T.; Shin, G.H.; Kim, J.T. Carbon Dots: Opportunities and Challenges in Cancer Therapy. Pharmaceutics 2023, 15, 1019. [Google Scholar] [CrossRef]
- Prajapati, B.G.; Pandey, V.; Sharma, S.; Patel, S.; Shah, D.P.; Kapoor, D.U. Carbon Nanodots: An Illuminating Paradigm in Production, Characterization, and Oncological Targeting Methodologies—A Review. BioNanoScience 2024, 14, 4322–4341. [Google Scholar]
- Chaitanya, M.V.N.L.; Ramanunny, A.K.; Babu, M.R.; Gulati, M.; Vishwas, S.; Singh, T.G.; Chellappan, D.K.; Adams, J.; Dua, K.; Singh, S.K. Journey of Rosmarinic Acid as Biomedicine to Nano-Biomedicine for Treating Cancer: Current Strategies and Future Perspectives. Pharmaceutics 2022, 14, 2401. [Google Scholar] [CrossRef]
- Zygouri, P.; Tsiodoulos, G.; Angelidou, M.; Papanikolaou, E.; Athinodorou, A.-M.; Simos, Y.V.; Spyrou, K.; Subrati, M.; Kouloumpis, A.; Kaloudi, A.S. Graphene Oxide and Oxidized Carbon Nanodiscs as Biomedical Scaffolds for the Targeted Delivery of Quercetin to Cancer Cells. Nanoscale Adv. 2024, 6, 2860–2874. [Google Scholar] [CrossRef]
- Sun, L.; Zhao, Y.; Peng, H.; Zhou, J.; Zhang, Q.; Yan, J.; Liu, Y.; Guo, S.; Wu, X.; Li, B. Carbon Dots as a Novel Photosensitizer for Photodynamic Therapy of Cancer and Bacterial Infectious Diseases: Recent Advances. J. Nanobiotechnol. 2024, 22, 210. [Google Scholar] [CrossRef]
- Guo, Q.; Li, L.; Gao, G.; Liu, R.; Einaga, Y.; Zhi, J. Nanodiamonds Inhibit Cancer Cell Migration by Strengthening Cell Adhesion: Implications for Cancer Treatment. ACS Appl. Mater. Interfaces 2021, 13, 9620–9629. [Google Scholar] [CrossRef] [PubMed]
- Cilingir, E.K.; Sankaran, M.; Garber, J.M.; Vallejo, F.A.; Bartoli, M.; Tagliaferro, A.; Vanni, S.; Graham, R.M.; Leblanc, R.M. Surface Modification of Carbon Nitride Dots by Nanoarchitectonics for Better Drug Loading and Higher Cancer Selectivity. Nanoscale 2022, 14, 9686–9701. [Google Scholar] [CrossRef] [PubMed]
- Rai, M.; Ingle, A.P.; Törős, G.; Prokisch, J. Assessing the Efficacy of Carbon Nanodots Derived from Curcumin on Infectious Diseases. Expert. Rev. Anti-Infect. Ther. 2024, 22, 1107–1121. [Google Scholar] [CrossRef] [PubMed]
- Behera, S.P.; Saxena, R.K. Nanodiamonds Inhibit Scratch-Wound Repair in Lung Epithelial Cell Monolayers by Blocking Cell Migration and Inhibiting Cell Proliferation. Toxicol. Lett. 2021, 341, 83–93. [Google Scholar] [CrossRef]
- Brindhadevi, K.; Garalleh, H.A.; Alalawi, A.; Al-Sarayreh, E.; Pugazhendhi, A. Carbon Nanomaterials: Types, Synthesis Strategies and Their Application as Drug Delivery System for Cancer Therapy. Biochem. Eng. J. 2023, 192, 108828. [Google Scholar] [CrossRef]
- Tok, K.; Barlas, F.B.; Bayır, E.; Şenışık, A.M.; Zihnioglu, F.; Timur, S. One Step Synthesis of Tryptophan-Isatin Carbon Nano Dots and Bio-Applications as Multifunctional Nanoplatforms. Colloids Surf. B Biointerfaces 2025, 114533. [Google Scholar] [CrossRef]
- Naghib, S.M.; Ahmadi, B.; Mikaeeli Kangarshahi, B.; Mozafari, M.R. Chitosan-Based Smart Stimuli-Responsive Nanoparticles for Gene Delivery and Gene Therapy: Recent Progresses on Cancer Therapy. Int. J. Biol. Macromol. 2024, 278, 134542. [Google Scholar] [CrossRef]
- Ramalho, M.J.; Serra, É.; Loureiro, J.A.; Pereira, M.C. Repurposing Gemcitabine for Glioblastoma Treatment: The Role of Drug-Conjugates and Nanoparticles as Drug Delivery Systems. J. Drug Deliv. Sci. Technol. 2024, 96, 105714. [Google Scholar] [CrossRef]
- Ibrahim, I.; Ayariga, J.; Xu, J.; Robertson, B.K.; Ajayi, O. Exploring the Synergy of Carbon. Nanodots in Enhancing Cannabidiol Delivery and Therapeutic Efficacy: A Comprehensive Review. Microbiol. Immunol. 2023. [Google Scholar] [CrossRef]
- Calabrese, G.; De Luca, G.; Nocito, G.; Rizzo, M.G.; Lombardo, S.P.; Chisari, G.; Forte, S.; Sciuto, E.L.; Conoci, S. Carbon Dots: An Innovative Tool for Drug Delivery in Brain Tumors. Int. J. Mol. Sci. 2021, 22, 11783. [Google Scholar] [CrossRef]
- Debnath, S.K.; Srivastava, R. Drug Delivery with Carbon-Based Nanomaterials as Versatile Nanocarriers: Progress and Prospects. Front. Nanotechnol. 2021, 3, 644564. [Google Scholar]
- Nocito, G.; Calabrese, G.; Forte, S.; Petralia, S.; Puglisi, C.; Campolo, M.; Esposito, E.; Conoci, S. Carbon Dots as Promising Tools for Cancer Diagnosis and Therapy. Cancers 2021, 13, 1991. [Google Scholar] [CrossRef] [PubMed]
- Pandey, V.K.; Tripathi, A.; Taufeeq, A.; Dar, A.H.; Samrot, A.V.; Rustagi, S.; Malik, S.; Bhattacharya, T.; Kovacs, B.; Shaikh, A.M. Significance and Applications of Carbon Dots in Anti Cancerous Nanodrug Conjugate Development: A Review. Appl. Surf. Sci. Adv. 2024, 19, 100550. [Google Scholar] [CrossRef]
- Pourmadadi, M.; Abbasi, P.; Eshaghi, M.M.; Bakhshi, A.; Manicum, A.-L.E.; Rahdar, A.; Pandey, S.; Jadoun, S.; Díez-Pascual, A.M. Curcumin Delivery and Co-Delivery Based on Nanomaterials as an Effective Approach for Cancer Therapy. J. Drug Deliv. Sci. Technol. 2022, 78, 103982. [Google Scholar] [CrossRef]
- Rajput, S.; Sharma, P.K.; Malviya, R.; Kaushik, N. Curcumin-Enclosed Nanoparticles for Cancer Therapy. Curr. Nutr. Food Sci. 2024, 20, 615–635. [Google Scholar] [CrossRef]
- Arvapalli, D.M.; Sheardy, A.T.; Bang, J.J.; Wei, J. Antiproliferative and ROS Regulation Activity of Photoluminescent Curcumin-Derived Nanodots. ACS Appl. Bio Mater. 2021, 4, 8477–8486. [Google Scholar] [CrossRef]
- Serag, E.; Helal, M.; El Nemr, A. Curcumin Loaded onto Folic Acid Carbon Dots as a Potent Drug Delivery System for Antibacterial and Anticancer Applications. J. Clust. Sci. 2024, 35, 519–532. [Google Scholar] [CrossRef]
- Aguilera, E.C.; Vachon, A.; Plourde, M. Comparative Pharmacokinetic of Curcuminoids Formulations with an Omega-3 Fatty Acids Monoglyceride Carrier: A Randomized Cross-over Triple-Blind Study. Nutrients 2022, 14, 5347. [Google Scholar] [CrossRef]
- Sengar, P.; Chauhan, K.; Hirata, G.A. Progress on Carbon Dots and Hydroxyapatite Based Biocompatible Luminescent Nanomaterials for Cancer Theranostics. Transl. Oncol. 2022, 24, 101482. [Google Scholar]
- Sajjadi, M.; Nasrollahzadeh, M.; Jaleh, B.; Soufi, G.J.; Iravani, S. Carbon-Based Nanomaterials for Targeted Cancer Nanotherapy: Recent Trends and Future Prospects. J. Drug Target. 2021, 29, 716–741. [Google Scholar] [CrossRef] [PubMed]
- Kasouni, A.I.; Chatzimitakos, T.G.; Troganis, A.N.; Stalikas, C.D. Citric Acid-Based Carbon Dots: From Revealing New Insights into Their Biological Properties to Demonstrating Their Enhanced Wound Healing Potential by in Vitro and in Vivo Experiments. Mater. Today Commun. 2021, 26, 102019. [Google Scholar] [CrossRef]
- Pooresmaeil, M.; Javanbakht, S.; Namazi, H.; Shaabani, A. Application or Function of Citric Acid in Drug Delivery Platforms. Med. Res. Rev. 2022, 42, 800–849. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Barroso, S.; Jacobo-Martín, A.; Navarro-Baena, I.; Hernández, J.J.; Navio, C.; Rodríguez, I.; Wannemacher, R. On the Nature of Solvothermally Synthesized Carbon Nanodots. J. Mater. Chem. C 2021, 9, 16935–16944. [Google Scholar] [CrossRef]
- Olla, C.; Cappai, A.; Porcu, S.; Stagi, L.; Fantauzzi, M.; Casula, M.F.; Mocci, F.; Corpino, R.; Chiriu, D.; Ricci, P.C.; et al. Exploring the Impact of Nitrogen Doping on the Optical Properties of Carbon Dots Synthesized from Citric Acid. Nanomaterials 2023, 13, 1344. [Google Scholar] [CrossRef]
- Dutta, A.; Dahiya, A.; Prakash, A.; Agrawala, P.K. Acute Toxicity of Diallyl Sulfide Derived from Allium Sativum (Garlic) in Mice and Its Possible Mechanisms. Phytomedicine Plus 2021, 1, 100084. [Google Scholar] [CrossRef]
- Dutta, A.; Trolles-Cavalcante, S.T.; Cleetus, A.; Marks, V.; Schechter, A.; Webster, R.D.; Borenstein, A. Surface Modifications of Carbon Nanodots Reveal the Chemical Source of Their Bright Fluorescence. Nanoscale Adv. 2021, 3, 716–724. [Google Scholar] [CrossRef]
- Bashar, M.A.; Hamed, A.; El-Tabakh, M.A.; Hashem, A.H.; Zaki, A.A.; Al-Askar, A.A.; Abou-Amra, E.S.; El-Beeh, M.E.; Mehany, A.B.; Shaaban, M. Anticancer, Antimicrobial, Insecticidal and Molecular Docking of Sarcotrocheliol and Cholesterol from the Marine Soft Coral Sarcophyton Trocheliophorum. Sci. Rep. 2024, 14, 28028. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Niu, C.; Qu, Y.; Sun, X.; Wang, K. Selective Activation of TRPA1 Ion Channels by Nitrobenzene Skin Sensitizers DNFB and DNCB. J. Biol. Chem. 2022, 298, 101555. [Google Scholar] [CrossRef]
- Parvin, N.; Kumar, V.; Joo, S.W.; Mandal, T.K. Emerging Trends in Nanomedicine: Carbon-Based Nanomaterials for Healthcare. Nanomaterials 2024, 14, 1085. [Google Scholar] [CrossRef]
- Onyancha, R.B.; Ukhurebor, K.E.; Aigbe, U.O.; Mogire, N.B.; Chanzu, I.; Kitoto, V.A.; Kusuma, H.S.; Darmokoesoemo, H. A Review of the Capabilities of Carbon Dots for the Treatment and Diagnosis of Cancer-Related Diseases. J. Drug Deliv. Sci. Technol. 2022, 78, 103946. [Google Scholar] [CrossRef]
- Shen, C.-L.; Liu, H.-R.; Lou, Q.; Wang, F.; Liu, K.-K.; Dong, L.; Shan, C.-X. Recent Progress of Carbon Dots in Targeted Bioimaging and Cancer Therapy. Theranostics 2022, 12, 2860. [Google Scholar] [CrossRef] [PubMed]
- Jose, S.; Anaswara, K.P.; Mathew, A.A.; Varghese, M.; Balachandran, M. Biomass Carbon Dots: Illuminating New Era in Antimicrobial Defense and Cancer Combat. BioNanoScience 2025, 15, 170. [Google Scholar] [CrossRef]
- Naik, G.G.; Pratap, R.; Mohapatra, D.; Shreya, S.; Sharma, D.K.; Parmar, A.S.; Patra, A.; Sahu, A.N. From Phytomedicine to Photomedicine: Quercetin-Derived Carbon Nanodots—Synthesis, Characterization and Healthcare Applications. J. Mater. Sci. 2023, 58, 13744–13761. [Google Scholar] [CrossRef]
- Bartoli, M.; Marras, E.; Tagliaferro, A. Computational Investigation of Interactions between Carbon Nitride Dots and Doxorubicin. Molecules 2023, 28, 4660. [Google Scholar] [CrossRef]
- Shao, X.; Wang, C.; Wang, C.; Bai, M.; Hou, T.; Wang, X.; Yan, C.; Guan, P.; Hu, X. Novel Photocatalytic Carbon Dots: Efficiently Inhibiting Amyloid Aggregation and Quickly Disaggregating Amyloid Aggregates. Nanoscale 2024, 16, 8074–8089. [Google Scholar] [CrossRef]

| Characteristic | Top-Down Approach | Bottom-Up Approach | References |
|---|---|---|---|
| Materials | Bulk carbon materials (graphite, CNTs, coal, etc.) | Small organic molecules (citric acid, glucose, urea, etc.) | [14] |
| Synthesis Method | Physical methods, such as fragmentation, oxidation, and etching, and chemical methods, including molecular self-assembly, carbonization, and hydrothermal synthesis | Molecular self-assembly, carbonization, hydrothermal synthesis | [13] |
| Control over Size | Limited size control, often polydisperse | High precision in size and shape control | [11] |
| Cost | High cost due to energy-intensive processes (e.g., laser ablation) | More cost-effective with relatively lower energy consumption | [13] |
| Applications | Mass production, composite materials, electronic applications | Biomedical applications, bioimaging, drug delivery | [9] |
| Cancer Type | Mortality Rate (%) | Common Treatments | Medications Used | Challenges | References |
|---|---|---|---|---|---|
| Lung Cancer | 25 | Chemotherapy, Surgery, Immunotherapy | Cisplatin, Pembrolizumab | Late diagnosis, resistance to therapy | [17] |
| Breast Cancer | 15 | Surgery, Radiotherapy, Hormonal Therapy | Tamoxifen, Trastuzumab | Variability in tumor subtypes | [18] |
| Colorectal Cancer | 10 | Surgery, Chemotherapy, Targeted Therapy | 5-FU, Bevacizumab | High recurrence rates | [21] |
| Pancreatic Cancer | 10 | Chemotherapy, Surgery | Gemcitabine, FOLFIRINOX | Poor prognosis, aggressive nature | [20] |
| Liver Cancer | 8 | Surgery, Targeted Therapy | Sorafenib, Lenvatinib | Limited treatment options | [17] |
| Criterion | Traditional Treatments (Chemotherapy/Radiotherapy) | Emerging Therapies | References |
|---|---|---|---|
| Selectivity and Systemic Toxicity | Limited selectivity leads to significant systemic toxicity, impacting both cancerous and healthy cells | Enhanced selectivity is aimed at reducing off-target effects and minimizing systemic toxicity | [37,38] |
| Drug Resistance | High incidence of drug resistance due to non-specific mechanisms and tumor heterogeneity, which frequently reduces long-term efficacy | Still vulnerable to cancer cell evolution, potentially necessitating combination treatments to address resistance mechanisms | [38,40] |
| Tumor Recurrence | High recurrence risk, largely attributed to residual cancer cells that survive initial treatment | Potential for reduced recurrence exists with effective targeting | [43] |
| Challenges in Drug Delivery | Predominantly affected by systemic exposure that results in collateral damage to normal tissues | Hindered by complex transport pathways, including size and geometry mismatches, adhesive tumor microenvironments (TMEs), and rapid clearance by the reticuloendothelial system (RES) | [44] |
| Mechanism | Effect on Cancer Cells | Outcome | Reference |
|---|---|---|---|
| Cytotoxicity | Induction of oxidative stress and production of reactive oxygen species (ROS) induces damage to DNA and proteins | Promotes cancer cell apoptosis | [45,46] |
| Enhanced Drug Solubility | Improvement in the solubility of chemotherapeutic drugs, facilitating tumor site delivery | Increases therapeutic efficacy | [46,53] |
| Enhancement of Adjunct Therapies | Augmentation of the effects of chemotherapy, radiation, gene, and immunotherapy | Enhances cancer cell response to treatment | [54] |
| Modulation of MAPK Pathway | Disruption of growth signaling pathways, leading to reduced cell proliferation | Inhibits cancer cell growth and enhances treatment response | [52] |
| Cellular Uptake of CNDs | Internalization of CNDs via endocytic pathways | Facilitates efficient drug delivery within cells | [45] |
| Membrane Interaction | Insertion into the membrane, wrapping, pore formation, and aggregation | Improves tumor targeting or induces cytotoxicity depending on interaction type | [46] |
| Application | Description | Benefits | Reference |
|---|---|---|---|
| Drug delivery to tumor sites | CNDs can be utilized to deliver chemotherapeutic agents directly to tumor sites. | Enhances treatment efficacy while minimizing systemic side effects. | [59] |
| Imaging and theragnostic | CNDs serve as imaging agents for fluorescence imaging, detecting gene expression, and monitoring drug delivery. | Addresses the demand for theragnostic agents by integrating diagnostic and therapeutic functions. | [60] |
| Overcoming barriers of traditional approaches | CNDs can enhance the effectiveness of photosensitizers, drugs, and genes in treatment strategies. | Improves therapeutic response and overcomes limitations of conventional treatments. | [61] |
| Passive targeting via enhanced permeability and retention (EPR) effect | CNDs endow photothermal agents with imaging capability, achieving passive targeting through the EPR effect. | Enables selective accumulation in tumor tissues while reducing impact on healthy cells. | [59] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alibrahem, W.; Helu, N.K.; Oláh, C.; Prokisch, J. Potential of Carbon Nanodots (CNDs) in Cancer Treatment. Nanomaterials 2025, 15, 560. https://doi.org/10.3390/nano15070560
Alibrahem W, Helu NK, Oláh C, Prokisch J. Potential of Carbon Nanodots (CNDs) in Cancer Treatment. Nanomaterials. 2025; 15(7):560. https://doi.org/10.3390/nano15070560
Chicago/Turabian StyleAlibrahem, Walaa, Nihad Kharrat Helu, Csaba Oláh, and József Prokisch. 2025. "Potential of Carbon Nanodots (CNDs) in Cancer Treatment" Nanomaterials 15, no. 7: 560. https://doi.org/10.3390/nano15070560
APA StyleAlibrahem, W., Helu, N. K., Oláh, C., & Prokisch, J. (2025). Potential of Carbon Nanodots (CNDs) in Cancer Treatment. Nanomaterials, 15(7), 560. https://doi.org/10.3390/nano15070560







